Abstract
Background
Internal hernias are relatively rare and difficult to diagnose. Diagnostic delays lead to the progression of strangulation. In particular, pararectal fossa hernias are extremely rare. We encountered a case in which internal hernia occurred in the pararectal fossa.
Case presentation
An 87-year-old woman was referred to our hospital because of persistent lower abdominal pain and vomiting. Contrast-enhanced computed tomography revealed findings of intestinal ischemia, such as closed loop formation with reduced contrast effect on the left side of the rectum in the pelvis. Strangulation small bowel obstruction was diagnosed, and emergency laparotomy was performed. The small intestine was found to invade the peritoneal reflection on the left side of the rectum. The patient was finally diagnosed with pararectal fossa hernia. The incarcerated small intestine was released with no bowel resection. The 4-cm hernia phylum was observed and closed by simple suture. The patient had a good postoperative course without recurrence.
Conclusions
We encountered a very rare case of internal hernia in the left pararectal fossa. Preoperative diagnosis of this disease is difficult, but it should nevertheless be considered in cases in which the cause of the intestinal obstruction is unknown.
Keywords: Pararectal fossa hernia, Internal hernia, Intestinal obstruction, Perirectal fossa hernia
Background
Internal hernia is a rare condition that causes intestinal obstruction. It is defined as the herniation of an organ into an unusually large fossa, fovea, or foramen in the abdominal cavity [1]. Internal hernias are reported to comprise 0.2–5.8% of all cases of small bowel obstruction, which itself is a rare disease [2]. The diagnosis of internal hernia is difficult, and diagnostic delays lead to the progression of strangulation [3]. Particularly, among cases of internal hernia, cases of pararectal fossa hernias are extremely rare. We encountered a rare case in which internal hernia occurred in the pararectal fossa. Herein, we report the case with a review of the literature.
Case presentation
An 87-year-old woman presented with the chief complaint of lower abdominal pain and nausea. She was referred to our hospital with persistent lower abdominal pain and vomiting. On physical examination, mild tenderness was present in the lower abdomen. Blood test revealed elevated white blood cell count (12,200 /μl) and C-reactive protein levels (2.2 g/dl), with no other pertinent findings. The patient had diabetes and high blood pressure and had previously undergone total hysterectomy for uterine fibroids. Contrast-enhanced computed tomography showed beak-like changes in the small intestine, closed loop formation with reduced contrast effect, and localized ascites on the left side of the rectum in the pelvis (Fig. 1a, b). Strangulation small bowel obstruction was diagnosed, and emergency laparotomy was performed. The small intestine was found to invade the peritoneal reflection on the left side of the rectum (Fig. 2a, b). The final diagnosis was pararectal fossa hernia. The incarcerated small intestine was released, and no bowel resection of the same site was required because the intestinal blood flow disorder was reversible. The 4-cm hernia phylum was observed and closed by simple suture (Fig. 2b). The patient had a good postoperative course and no recurrence.
Fig. 1.
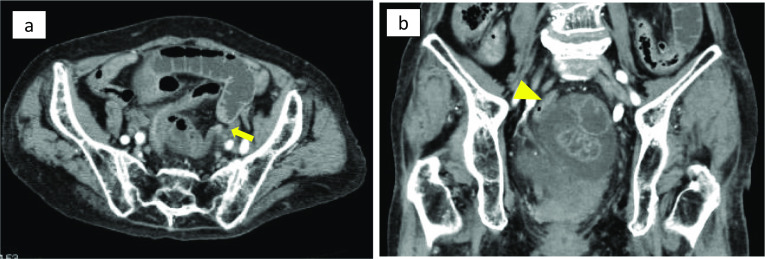
Computed tomography before treatment. a Abdominal computed tomography shows extensive small intestinal dilation and beak-like changes in the small intestine (arrow) on the left side of the pelvis. b A closed loop with reduced contrast effect is formed on the left side of the rectum (arrow head), and localized ascites is observed
Fig. 2.
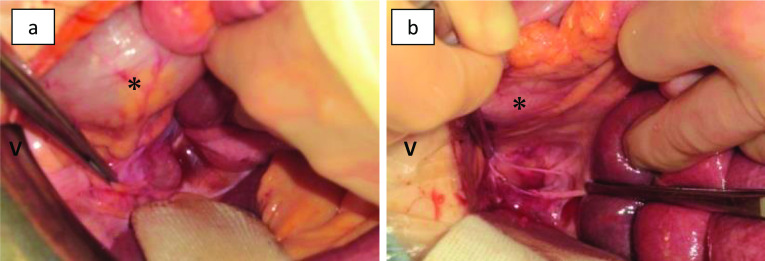
Intraoperative images. a The small intestine was stuck in the pararectal fossa on the left side of the rectum (asterisk). V = ventral side. b A 4-cm hernia orifice was found in the peritoneal reflection on the left side of the rectum (asterisk)
Discussion
Internal hernia is defined as the herniation of an organ into an unusually large fossa, fovea, or foramen in the abdominal cavity [1]. Internal hernias occur in 0.2–5.8% of all cases of small bowel obstruction [2, 4]. Particularly, paraduodenal fossa hernias are reported to be the most common (53%), followed by paracecal fossa hernias (13%), and Winslow foramen hernias and transverse mesenteric fossa hernias (8%) [3]. On the other hand, internal hernias in the pelvis, including the broad ligament of the uterus, Douglas fossa, and pararectal fossa, occur in < 6% of cases [3]. Furthermore, there are several cases of the broad ligament of the uterus reported as internal hernias in the pelvis [5, 6]. Thus, it can be concluded that the occurrence of internal hernia in the pararectal fossa is extremely rare.
A search on the PubMed and MEDLINE databases for literature published regarding “pararectal fossa hernia” or “perirectal fossa hernia” yielded a total of three studies [3, 7, 8] (Table 1). All previous cases were in middle-aged women, but our case was in a very elderly woman. In two cases, internal hernia occurred on the right side of the rectum, whereas in the other two (including our case), it occurred on the left side of the rectum. The latter two cases had a history of hysterectomy. The cause may be congenital or acquired, but congenital factors were suspected in the cases in which internal hernia occurred on the right side of the rectum considering the early age of onset and the absence of a history of surgery. On the other hand, the cases in which internal hernia occurred on the left side of the rectum were presumed to be associated with a history of gynecological surgery.
Table 1.
Previously reported cases of pararectal fossa hernia
| No. | Author | Reported year |
Age (y) | Sex | History of surgery | Position | Symptom | Hernia content | Surgical approach | Procedure |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Takeyama [3] | 2005 | 28 | Female | – | Right | Ileus | Bowel | Laparotomy | Suture |
| 2 | Yamashiro [7] | 2007 | 48 | Female | – | Right | Ileus | Bowel | Laparoscopy | Not detected |
| 3 | Walid [8] | 2010 | 48 | Female | Total hysterectomy | Left | Incidental | No content | Laparoscopy | Mesh |
| 4 | Our Case | 2021 | 87 | Female | Total hysterectomy | Left | Ileus | Bowel | Laparotomy | Suture |
A differential disease of pararectal fossa hernia includes pararectal hernia, a type of perineal hernia. Perineal hernia is defined as a pathological condition in which intra-abdominal organs protrude beyond the pelvic floor into the subcutaneous area of the perineum. A defect is found in the pelvic floor, which is composed of pelvic floor muscles, and it is considered to be a condition in which a hernia orifice is formed [9]. Internal hernias in the pelvis, including this case, are caused by defects up to the peritoneum, and should be distinguished from perineal hernias.
In this case, we performed laparotomy to release the strangulation and closed the hernia phylum with suture. In recent years, there have been cases in which laparoscopic surgery was performed for strangulated small bowel obstruction [10], and both laparoscopic surgery and laparotomy are considered as treatment options. Thus, it is important to determine which operative procedure is better based on the patient’s condition, including the status of small bowel obstruction, such as dilation of the intestinal tract.
Closure of the hernia phylum involves the use of ligation sutures and a repair method using a mesh [3, 8]. If the intestinal tract is necrotic, it is difficult to use the mesh owing to the possibility of infection. Thus, it is necessary to choose the appropriate closure method for hernia phylum based on the patient’s condition.
Conclusion
We present a case of pararectal fossa hernia, which is a very rare disease among the different types of internal hernias. Preoperative diagnosis is difficult, but a differential diagnosis of pelvic internal hernia should nevertheless be considered. In such cases, early surgery is desirable.
Acknowledgements
We thank Edanz Group (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author contributions
KM wrote the article. SS and JN edited the article. HB supervised the editing of the manuscript. YK, MO and NH collected the data and discussed the content of the manuscript. All authors read and approved the final manuscript.
Funding
This study was not funded.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. Kumamoto Chuo Hospital Ethics Committee approved this case report. The committee’s reference number: 202201–01.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Steinke CR. Internal hernia: three additional case reports. Arch Surg. 1932;25(5):909–925. doi: 10.1001/archsurg.1932.01160230092008. [DOI] [Google Scholar]
- 2.Newsom BD, Kukora JS. Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg. 1986;152(3):279–285. doi: 10.1016/0002-9610(86)90258-8. [DOI] [PubMed] [Google Scholar]
- 3.Takeyama N, Gokan T, Ohgiya Y, Satoh S, Hashizume T, Hataya K, et al. CT of internal hernias. Radiographics. 2005;25(4):997–1015. doi: 10.1148/rg.254045035. [DOI] [PubMed] [Google Scholar]
- 4.Suwa K, Yamagata T, Hanyu K, Suzuki T, Okamoto T, Yanaga K. Internal hernia through a peritoneal defect in the pouch of Douglas: report of a case. Int J Surg Case Rep. 2013;4(1):115–117. doi: 10.1016/j.ijscr.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haku T, Daidouji K, Kawamura H, Matsuzaki M. Internal herniation through a defect of the broad ligament of the uterus. Abdom Imaging. 2004;29(2):161–163. doi: 10.1007/s00261-003-0065-y. [DOI] [PubMed] [Google Scholar]
- 6.Fafet P, Souiri M, Ould Said H, Mattei M, Godlewski G. Internal hernia of the small intestine through a breach of the broad ligament, apropos of a case. Review of the literature. J Chir (Paris) 1995;132(6–7):314–317. [PubMed] [Google Scholar]
- 7.Yamashiro T, Samura H, Kinjo M, Iida G, Gibo M, Murayama S, et al. CT of internal hernia through a defect of the perirectal fossa. Abdom Imaging. 2007;32(3):320–322. doi: 10.1007/s00261-006-9087-y. [DOI] [PubMed] [Google Scholar]
- 8.Walid MS, Heaton RL. Pararectal and obturator hernias as incidental findings on gynecologic laparoscopy. Hernia. 2010;14(1):109–111. doi: 10.1007/s10029-009-0515-0. [DOI] [PubMed] [Google Scholar]
- 9.Stamatiou D, Skandalakis JE, Skandalakis LJ, Mirilas P. Perineal hernia: surgical anatomy, embryology, and technique of repair. Am Surg. 2010;76(5):474–479. doi: 10.1177/000313481007600513. [DOI] [PubMed] [Google Scholar]
- 10.Zerey M, Sechrist CW, Kercher KW, Sing RF, Matthews BD, Heniford BT. The laparoscopic management of small-bowel obstruction. Am J Surg. 2007;194(6):882–7; discussion 7–8. doi: 10.1016/j.amjsurg.2007.08.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.


