Abstract
Ubiquitously expressed in mammalian cells, the Kelch-like ECH-associated protein 1 (Keap1)–NF erythroid 2–related factor 2 (Nrf2) complex forms the evolutionarily conserved antioxidation system to tackle oxidative stress caused by reactive oxygen species. Reactive oxygen species, generated as byproducts of cellular metabolism, were identified as essential second messengers for T cell signaling, activation, and effector responses. Apart from its traditional role as an antioxidant, a growing body of evidence indicates that Nrf2, tightly regulated by Keap1, modulates immune responses and regulates cellular metabolism. Newer functions of Keap1 and Nrf2 in immune cell activation and function, as well as their role in inflammatory diseases such as sepsis, inflammatory bowel disease, and multiple sclerosis, are emerging. In this review, we highlight recent findings about the influence of Keap1 and Nrf2 in the development and effector functions of adaptive immune cells, that is, T cells and B cells, and discuss the knowledge gaps in our understanding. We also summarize the research potential and targetability of Nrf2 for treating immune pathologies.
Introduction
Mammalian cells have evolved to respond to various kinds of stress caused by adverse conditions, including oxidative stress due to the increased levels of free radicals. Cellular metabolism during the normal physiological state or pathological conditions results in the production of highly reactive free radicals such as superoxide radicals, hydrogen peroxide, hydroxyl radicals, and singlet oxygen as byproducts collectively called reactive oxygen species (ROS) (1). Traditionally thought to be detrimental to cell health, research from the last few decades has established ROS as important intermediates in maintaining immune cell signaling and activation (2). Whereas high levels of ROS lead to cellular damage and apoptosis, low ROS levels cause decreased cellular proliferation and impaired host defenses (3). Thus, it is not surprising that immune cells have mechanisms in place to strike a perfect redox balance and to modulate the levels of ROS differentially during their naive, activated, and effector stages for tailored immune responses (4).
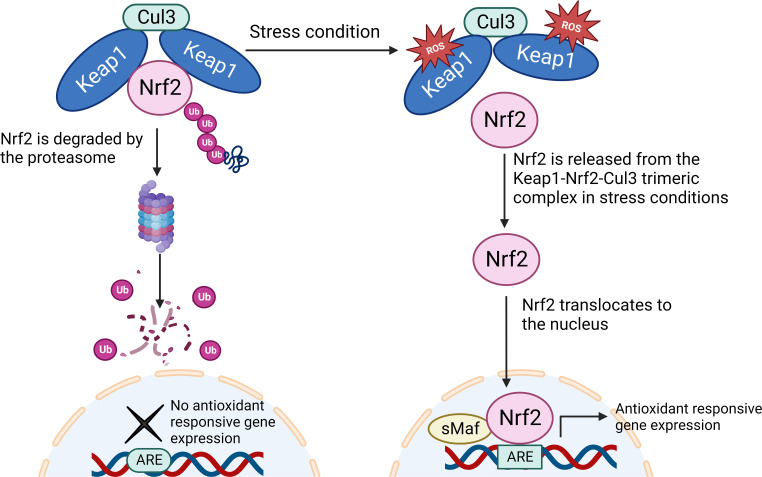
The ubiquitously expressed trimeric complex composed of Kelch-like ECH-associated protein 1 (Keap1), NF erythroid 2–related factor 2 (Nrf2), and cullin 3 (Cul3) proteins constitute the antioxidation system to maintain redox homeostasis in mammalian cells (Fig. 1). An imbalance in this system leads to susceptibility to drug-induced toxicity and oxidative stress–induced diseases such as acute lung injury, chronic obstructive pulmonary disease, diabetic nephropathy, heart failure, and cancer (5–9). Apart from the conventional antioxidation role, other functions of Keap1 and Nrf2, particularly in cancer cells, are well established. Additionally, several studies have reported newer functions of Keap1 and Nrf2 in the activation and functions of immune cells and how antioxidation contributes to inflammatory diseases such as sepsis and multiple sclerosis (MS) (10–13). Several studies, mostly in tumor cells, recognized that the Keap1–Nrf2 complex regulates cellular metabolism (14–16). In this review, we outline some of the newer developments about the roles of Keap1 and Nrf2 in the development and effector functions of cells of the adaptive immune system, that is, T lymphocytes and B lymphocytes. We also discuss the therapeutic potential of these proteins and identify the current knowledge gaps and possible new research directions.
FIGURE 1.
Overview of the Keap1–Nrf2 pathway.
Under homeostatic conditions, Nrf2, bound to a trimeric complex with Keap1 and Cullin3, is ubiquitinated and thence degraded by the 26S proteasome. During oxidative stress, the reactive cysteine residues in Keap1 bind to ROS or electrophilic toxins, causing a conformational change that impairs its ability to bind Nrf2. Nrf2 accumulates in the cytoplasm and then translocates into the nucleus where it activates the transcription of antioxidant-responsive genes. ARE, antioxidant response element; sMaf, small musculoaponeurotic fibrosarcoma. This figure was made in BioRender.com
The Keap1–Nrf2 complex
Keap1 serves as an intracellular sensor of stress. In conjunction with Cul3, Keap1 forms an E3 ubiquitin ligase complex (adaptor protein of Cul3) to control the stability and accumulation of Nrf2 (17, 18). Keap1 is a highly conserved protein abundantly expressed in different cell types and tissues (19, 20). During homeostatic conditions, in the absence of stress, Nrf2 gets ubiquitinated by the Keap1-Cul3-E3 ubiquitin ligase and gets degraded rapidly by the proteasome pathway such that the cellular activity of Nrf2 is suppressed (Fig. 1). Human Keap1 contains 27 cysteine residues that can be modified by alkylation or oxidoreduction reactions in the presence of electrophilic compounds during Nrf2 activation (20). During oxidative stress, the cysteine residues of Keap1 bind to the ROS or electrophilic toxins, causing conformational changes that lead to a poor binding affinity for Nrf2. Dislodged from the trimeric complex, Nrf2 is no longer ubiquitinated or degraded, leading to its accumulation in the cytosol (21) and then translocation into the nucleus where it activates the transcription of cytoprotective genes (22).
Nrf2 is the master transcription factor for controlling environmental stress responses. It is encoded by the gene NFE2L2 (NF, erythroid 2, like 2) and belongs to the cap’n’collar subfamily of basic leucine zipper transcription factors (23, 24). In vertebrates, these transcription factors are NFE2 (NF erythroid-derived 2) and the NFE2-related factors Nrf1, Nrf2, and Nrf3 (25). During oxidative and electrophilic stress, Nrf2 forms a dimer with small musculoaponeurotic fibrosarcoma (sMaf) proteins to form the sMaf-Nrf2 heterodimer, which recognizes the ARE (antioxidant response element) domain located in the promoter region of detoxification genes. This binding triggers the transcription of an array of genes including the cytoprotective genes (26–28), such as Nqo1 (NAD(P)H quinone oxidoreductase 1), HO-1 (heme oxygenase-1), SOD2 (superoxide dismutase 2), GCLC (glutamate-cysteine ligase catalytic subunit), and GSTP1 (GST pi 1) (21, 24).
Dysregulation of the antioxidation pathway causes or contributes to the development of multiple pathologies, including cancers and inflammatory diseases (24, 29). Mutations in Nrf2 and Keap1 genes are frequently found in various cancer types (30). Keap1 was shown to play a role in autophagy, apoptosis, NF-κB signaling, cell proliferation, and inflammation (31). In immune cells, Keap1 and Nrf2 play important roles in regulating the expression of genes involved in antioxidant defense, detoxification, as well as immune responses (28).
It is well known that innate immune cells provide a critical framework for mounting of the adaptive immune responses (32–36). Substantial research has established that Nrf2 is involved in regulating the numbers and function of innate immune cells such as dendritic cells (37, 38), neutrophils (13, 39), macrophages (13, 40), NK cells (41), and myeloid-derived suppressor cells (42). These findings have been covered extensively in previously published reviews (43, 44). More recent research has shed light on the contributions of the antioxidant pathway proteins in the development and immune functions of adaptive immune cells as well. In this review, we summarize the recent findings on the roles of Keap1 and Nrf2 in the development, immune functions, and metabolism of T cells and B cells, and highlight their potential as therapeutic targets for immune pathologies.
Keap1 and Nrf2 in lymphocyte development
Cells of the lymphoid lineage (T, B, and NK cells) and myeloid lineage (macrophages, granulocytes, dendritic cells, and myeloid-derived suppressor cells) are generated from self-renewing progenitors, that is, the hematopoietic stem cell (HSCs) in the bone marrow. One study reported that Nrf2 activation in HSCs skews hematopoietic differentiation toward the myeloid lineage at the cost of the lymphoid lineage cells (45). Using two different transgenic mouse strains, this study showed that the Keap1–Nrf2 system is highly functional in HSCs, and that Nrf2 activation in these cells causes reduced commitment of T cells and B cells while supporting the production of granulocytes and monocytes, particularly under stressed conditions, such as inflammation.
Early lymphoid progenitors develop into either T cells in the thymus or into B cells in the bone marrow and spleen. Although the role of Keap1 and Nrf2 in early T cell development is as yet undetermined, studies suggest that they do not participate in late T cell development, leading to the generation of single-positive CD4 and CD8 T cells. We and others observed that in mice, T cell–specific deletion of Keap1 or Nrf2 under the CD4 promoter (leading to deletion at the double-positive stage of thymocyte development) did not affect the CD4+ or CD8+ T cell compartments (11, 31). In the same mice, however, we observed reduced numbers of invariant NKT cells in the thymus and the peripheral organs. NKT cells, which express both TCR and surface receptors of NK cells (46, 47), are innate-like T cells that develop in the thymus after branching out at the double-positive stage. NKT cells have the characteristics of both adaptive immunity and innate immunity, and they harbor high levels of ROS (48). Interestingly, Keap1-deficient NKT cells with high Nrf2 activity show increased proliferation and a higher apoptotic rate in addition to low ROS levels (31). These developmental defects in Keap1-deficient NKT cells were rescued by depleting Nrf2. This study highlighted the importance of maintaining low Nrf2 activity and high ROS during NKT cell development. Promyelocytic leukemia zinc finger (PLZF) is the master transcription factor that is instrumental for NKT cell development (49). It is still unknown whether the Keap1–Nrf2 complex modulates PLZF levels and whether these antioxidation proteins also regulate the fate of other innate T cells such as γδ T cells and mucosal-associated invariant T cells.
Although there is evidence that Nrf2 and Keap1 participate in activation-driven B cell responses such as plasma cell differentiation and Ab generation (discussed in the next section), there are no direct studies that investigated the role of the antioxidation system in B cell development.
Keap1 and Nrf2 in lymphocyte functions
T cell activation
A newer role of the Nrf2–Keap1–Cul3 trimeric complex in T cell–mediated immunity is emerging (Fig. 2). Naive T cells, upon recognition of cognate Ag, receive TCR signaling and upregulate the expression of various activation markers and proliferative cytokine IL-2 as the first step of effector responses. Two different studies from the same group showed that the chemical induction of Nrf2 using tert-butylhydroquinone (tBHQ) in primary human CD4 T lymphocytes and Jurkat cells decreased the expression of the early activation markers such as CD25 and CD69, and consequently lowered the expression of IL-2 (50, 51). This decrease in the expression of activation markers with high Nrf2 correlated with impaired NF-κB transcriptional activity, which is critical for T cell activation (50, 51). Notably, two different chemical activators of Nrf2, tBHQ and 2-cyano-3,12 dioxooleana-1,9 diene-28-imidazolide (CDDO-Im), had differential effects on early T cell activation and IL-2 production, with some effects being Nrf2-independent (52). Thus, cell-specific conditional deletion or activation of Nrf2 might be a better tool for investigating cell-intrinsic biological functions of Nrf2 in T cells to rule out off-target effects.
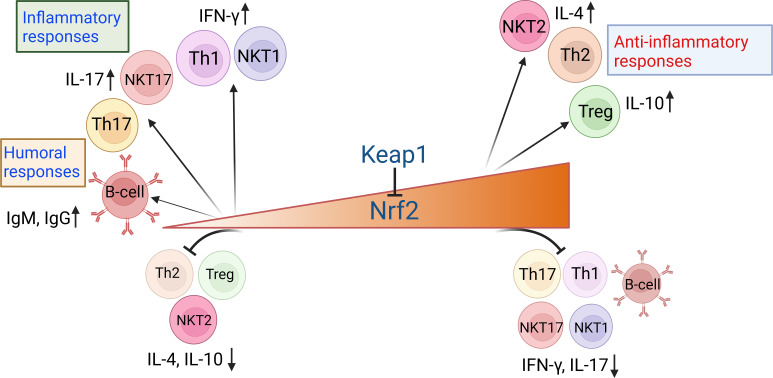
FIGURE 2.
Nrf2 levels influence proinflammatory and anti-inflammatory responses by adaptive immune cells.
The protein levels of Nrf2, negatively regulated by Keap1, play a deciding factor in T cell–mediated inflammatory responses. Nrf2 activation supports the differentiation of the Th2 subset, regulatory T cells (Tregs), and the NKT2 subset while inhibiting the differentiation of Th1, Th17, NKT1, and NKT17 subsets. Conversely, the absence of or low Nrf2 results in enhanced proinflammatory responses, characterized by the differentiation of Th1, Th17, NKT1, and NKT17 subsets, whereas subdued generation of Th2, Treg, and NKT2 subsets. Nrf2 activation levels also influence the generation of humoral responses. Whereas low Nrf2 levels favor T cell–dependent production of IgG and IgM Abs by activated B cells, high Nrf2 suppresses B cell responses such as the differentiation of germinal center B cells and plasma cells. Thus, Nrf2 negatively regulates T–cell mediated inflammatory responses and T-dependent B cell responses. This figure was made in BioRender.com.
Th cells and regulatory T cells
Activated CD4+ T cells undergo clonal expansion and differentiate into one of the Th cell subsets (e.g., Th1, Th2, Th17) to perform specialized functions (53). The chemical activation of Nrf2 using tBHQ and butylated hydroxyanisole (BHA) during in vitro T cell activation led to decreased production of Th1 cytokine IFN-γ and increased production of Th2 cytokines IL-4, IL-5, and IL-13, which correlated with suppressed DNA binding of T-bet and increased binding of GATA-binding protein 3 (GATA3), respectively (10). Further investigation with Th1 and Th2 differentiation assays or T cell inflammatory mouse models is needed to identify the role of Nrf2 in the skewing of the Th1/Th2 balance. However, in contrast to the murine cells, activation of Nrf2 by these compounds in the human T cells that were obtained from buffy coats of healthy donors did not alter the expression of proinflammatory or anti-inflammatory cytokines (54). Studies indicate the role of Nrf2 in the differentiation of inflammatory IL-17–producing Th17 cells. Noel et al. (11) reported that in mice with T cell–specific augmentation of Nrf2 activity by Keap1 deletion, the frequency of IFN-γ+ and IL-17+ CD4 T cells decreased in the kidneys. As expected, these mice were significantly less susceptible to acute kidney injury, and adoptive transfer of Nrf2-high T cells protected the wild-type (WT) mice and improved their survival.
Several studies thus far have indicated a protective role of Nrf2 in inflammation-driven pathology. Whereas high Nrf2 attenuates inflammation and in turn disease pathology, the absence of Nrf2 exacerbates inflammation. Evidence suggests that this is mainly mediated by modulation of Th differentiation by Nrf2 (55–59). Nrf2 activators such as triterpenoids and sulforaphane were shown to suppress experimental autoimmune encephalitis by inhibiting Th1 and Th17 responses (55, 56). Similarly, a protective role of Nrf2 was reported in a mixed granulocytic mouse model of asthma (57). The administration of sulforaphane reduced inflammation, upregulated antioxidants, and downregulated Th17 responses in the airways (57). Nrf2 activation using sodium butyrate led to the differentiation of regulatory T cells (Tregs) over Th17 cells, causing attenuation of autoimmune uveitis in an experimental mouse model (58). Consistently, deficiency of Nrf2 heightened Th17 responses and promoted lupus nephritis in mouse models. Furthermore, increased Th17 differentiation and increased phosphorylation of STAT3 were noted in Nrf2-depleted CD4 T cells in in vitro Th17 differentiation assays (59). In all, these studies indicate a role of Nrf2 in suppressing the differentiation of the inflammatory Th cell subsets (Fig. 2). In line with this, in scurfy mice that lack Tregs (and die due to multiorgan inflammation), systemic activation of Nrf2 by Keap1 deletion attenuated inflammation and improved survival mediated by decreased T cell activation and cytokine responses (60).
Contrary to the widely reported anti-inflammatory role of Nrf2 (10, 11, 52, 59), a handful of studies showed a proinflammatory function of Nrf2 in mouse models. One study reported that Nrf2 activation resulted in severe inflammation in the lungs and liver, loss of immune tolerance, and accumulation of IFN-γ–producing effector T cells, leading to death of the study mice (61). This discrepancy was probably due to the differences in the method used for modulating Nrf2 gene expression. Whereas the other studies either used chemical activators of Nrf2 (10, 52) or used CD4 T cell–specific knockout of Keap1 to activate Nrf2 (11), this study employed Foxp3-driven deletion of Keap1 (61). These mice depicted high neonatal fatality because apart from Tregs, Foxp3 is expressed by the epithelial cells (62). A study examining graft-versus-host disease during allogeneic hematopoietic cell transplantation in an experimental mouse model showed that Nrf2 knockout donor CD4 T cells induced an increase in Foxp3 expression and Treg abundance and less graft-versus-host mortality and morbidity compared with allogeneic hematopoietic cell transplantation from Nrf2 WT mice (63). One study reported that activation of Nrf2 using CDDO-Im induces an IL-22 response in murine CD4+ T cells by binding to the ARE motif of the aryl hydrocarbon receptor (64). Importantly, they also found that CDDO-Im acts differently in murine- and human-derived CD4+ T cells to modulate IL-17A responses such that Nrf2 activation inhibits the IL-17A response in MS patient–derived PBMCs. Although these findings undoubtedly add to the increasing body of important research in the realm of Nrf2 in immunobiology, they also point to the fact that Nrf2 can exert both proinflammatory and anti-inflammatory functions depending on the experimental system and the mode of Nrf2 activation, warranting further critical studies.
The direct role of Nrf2 in the generation of natural or induced Tregs is not very clear. Of importance, a comparison of Nrf2 expression between different T cell subsets generated by in vitro differentiation revealed that Foxp3+ Tregs have the highest levels of Nrf2 activity compared with Th0, Th1, Th2, and Th17 subsets. Thus, higher Nrf2 levels may promote Treg generation and favor regulatory responses. In mice with T cell–specific Keap1 deletion, the frequency of CD25+Foxp3+ Tregs was found to be increased, in conjunction with decreased inflammation and ischemic acute kidney injury (11). A recent study also documented an important role of CD4 T cell–specific Nrf2 in hepatic ischemia-reperfusion injury in orthotopic liver transplantation wherein adoptive transfer of Nrf2-knockout CD4 T cells worsened orthotopic liver transplantation injury in RAG2-knockout mice (65). Furthermore, CD4 T cell–specific Nrf2 signaling suppressed the proinflammatory Th1/Th17 cytokines and promoted Treg generation in vitro. These findings highlight the anti-inflammatory functions of Nrf2.
NKT cells
NKT cells are T cells of innate lineage, which recognize glycolipids through their invariant TCR and produce copious amounts of various cytokines in response. During development in the thymus, NKT cells are believed to develop into NKT1, NKT2, and NKT17, which are functionally similar to Th1, Th2, and Th17 cells, respectively (66). We previously reported that NKT cells harbor significantly higher levels of ROS even at a steady state compared with conventional T cells, particularly in NKT1 and NKT17 subsets, and that these high levels of ROS are important for the inflammatory functions of NKT cells (48). As expected, we noted that constitutively high Nrf2 activity in T cells in mice led to low ROS and a decreased frequency of NKT1 subsets, whereas NKT2 cells increased, which correlated with low IFN-γ+ NKT cells and higher IL-4+ NKT cells in these mice (31). Whether Nrf2 plays a similar role in the inflammatory functions of other innate T cells remains to be studied.
B lymphocytes
B cells are Ab-producing adaptive immune cells that provide humoral immunity. Upon recognition of an Ag, B cells undergo clonal expansion and differentiate into Ab-secreting plasma cells in a T cell–dependent or –independent manner (67). The more common T cell–dependent B cell responses are activated by complex Ags, resulting in the production of different Ab isotypes and long-term protection, whereas T cell–independent responses are activated by highly repetitive Ags and produce only IgM Abs, providing short-term protection (68). Research using genetic ablation of Nrf2 and its activators has revealed a possible impact of Nrf2 on B cell responses (Fig. 2).
Bertolotti et al. (69) first demonstrated that elevated oxidative stress and Nrf2 activation are important for T cell–independent terminal differentiation but not for the proliferation of activated B cells. LPS-activated B cells isolated from Nrf2-knockout mice had delayed plasma cell differentiation and IgM secretion, compared with the WT mice. Using the Nrf2 activator tBHQ, Bursley and Rockwell (70) reported similar results while investigating the effect of Nrf2 on T cell–independent B cell responses by activating B cells with LPS. Although neither tBHQ treatment nor genetic ablation of Nrf2 (Nrf2-null) affected the percentage of B cells in the spleen, the production of IgM increased in an Nrf2-dependent manner. However, tBHQ inhibited the differentiation and activation of B cells in an Nrf2-independent manner. Thus, Nrf2-independent mechanisms cannot be ruled out when using chemical activators of Nrf2.
In normal and malignant human B cells, oxidative stress inducer 15-deoxy-Δ12,14-PGJ2 (15d-PGJ2) upregulated the expression of HO-1, a cytoprotective enzyme, via Nrf2 activation (71). Interestingly, malignant B cells showed higher induction of HO-1 than did normal B cells. IgM and IgG levels in the plasma of Nrf2-null mice increased 3- to 4-fold, suggesting a role for HO-1 and/or Nrf2 in Ab production. However, isolated B cells from these mice only produced slightly more IgG and similar amounts of IgM upon stimulation compared with control mice, indicating that global disruption of Nrf2 might be affecting multiple cell types involved in Ab production. Interestingly, Nrf2-deficient mice exhibited increased expression of cyclooxygenase-2 (Cox-2) protein even without stimulation, which is critical for optimal Ab synthesis (72). Thus, elevated Ab levels in the absence of Nrf2 may be due to increased Cox-2 levels in B cells. Nrf2 was found to support the survival of human B lymphoblast cells (WiL2-NS) in vitro upon treatment with the chemical bisphenol A (BPA), but the mechanism is uncharacterized (73).
In contrast to the previous studies using LPS for B cell activation, in the collagen-induced arthritis mouse models, treatment with Nrf2 activator sulforaphane led to the suppression of CD138+ plasma cell differentiation and germinal center B cells associated with reduced expression of inflammatory cytokines (74). In line with this, in patients treated with dimethyl fumarate (DMF), a U.S. Food and Drug Administration–approved drug for the treatment of relapsing MS, decreased mature and memory B cells, as well as plasmablasts, and increased immature, transitional B cells were noted, indicating a shift from pathogenic to nonpathogenic B cell types (75). These findings indicate a regulatory role of Nrf2 in B cell responses (Fig. 2). Consistently, during chronic lung inflammation in mice exposed to nontypeable Haemophilus influenzae, Nrf2-null mice exhibited increased B cell responses such as plasma cell infiltration, Ag-specific Ab titers in serum, and expression of B cell activation/survival markers compared with WT mice (76). The variations in the functions and differentiation of B cells in these studies may be due to the discrepancies in the model systems employed and the method used for manipulating Nrf2. It is possible that chemical activators of Nrf2 could potentially affect the results through Nrf2-independent mechanisms. In contrast, alterations in the functioning of innate immune cells and T cells can occur and directly affect B cell responses when using in vivo mouse models. Therefore, to solidify the role of Keap1–Nrf2 pathway proteins in B cell effector functions, genetic ablation of Keap1 or Nrf2 in mice preferentially in a B cell–specific manner may provide more convincing and clear answers in the future.
Nrf2 in T cell and B cell metabolism
Similar to cancer cells, activated T cells turn metabolically active to meet the bioenergetic demands of rapid clonal expansion and subsequent effector responses (77). Metabolic processes often produce ROS as a byproduct, and high metabolic turnover leads to oxidative stress, which in turn upregulates the antioxidation pathway by Nrf2 activation (3). The Keap1–Nrf2 system is well known to modulate cell metabolism in cancer cells (reviewed in Refs. 15, 16). Studies focusing on its metabolic function in immune cells, however, are more recent (40, 78). In a first study about the role of the Keap1–Nrf2 system in T cell metabolism, we reported that Nrf2 regulates the development and homeostasis of NKT cells by altering glucose metabolism and mitochondrial biogenesis (31). In mice with T cell–specific deletion of Keap1, NKT cells with high Nrf2 displayed increased mitochondrial function, glucose uptake, and the expression of glucose transporter glucose transporter protein type 1 (GLUT1)) together with increased proliferation as well as increased apoptosis. Concurrent deletion of both Nrf2 and Keap1 reversed these metabolic changes, indicating that these defects were Nrf2 mediated (31). In line with our findings in NKT cells, another study found that Nrf2 activation in Tregs enhanced their glucose uptake and upregulated their mammalian target of rapamycin (mTOR) activity (61), indicating that Nrf2 partakes in metabolic modulation of T cells. More recently, a study showed that Nrf2 activation via 4-octyl itaconate in CD4 T cells isolated from synovial fluid resulted in a modest decrease in mitochondrial mass, mitochondrial ROS, and fatty acid but not the uptake of glucose (79). Given that Nrf2 is a well-known regulator of glucose and glutamine metabolism (14, 80), and T cell subsets rely heavily on these nutrients for their effector functions, further studies are necessary to examine whether and how Nrf2 modulates nutrient metabolism in these immune cell subsets.
Although there is still much to be learned about the metabolism of both T cells and B cells, we know more about T cell metabolism than B cell metabolism. ROS levels are upregulated in B cells upon activation by BCR engagement via multiple mechanisms, including mitochondrial ROS generation, NADPH oxidase enzymes (NOXes), and oxidative protein folding (81–84). This upregulation of ROS is important for BCR signaling and proliferation, and in determining B cell fate after activation (82, 83). A recent study showed that in patients of systemic lupus erythematosus, B cells harbor heightened levels of cytosolic ROS and increased expression of Nrf2 (85). At the pre-B developmental stage, upon expression of pre-BCR, these cells also undergo rapid proliferation with high uptake of glucose and enhanced mitochondrial ROS generation (86). During the L chain rearrangement, B cells also enter a metabolically quiescent stage that then changes upon their transition to immature B cells (86). The metabolic mechanism behind transition of immature B cells to mature naive B cells is uncharacterized. Metabolically quiescent naive B cells upon Ag stimulation undergo induction of both glycolysis and oxidative phosphorylation (87). However, whether Nrf2 modulates B cell metabolism during their development and/or differentiation remains to be deciphered.
Targeting Keap1–Nrf2 in T cells for therapeutic interventions
As discussed so far, Keap1–Nrf2 proteins clearly participate in regulating various aspects of the T and B cell immune cell functions. Thus, targeting this pathway seems to be a viable therapeutic option against T and B cell–associated malignancies (Table I). The approval of the Nrf2 activator DMF by the U.S. Food and Drug Administration in 2013 for the treatment of remitting or relapsing MS has invigorated further studies in the field. Increased oxidative stress and excessive inflammation mediated by CD4 T cells are linked to MS, a debilitating autoimmune disease of the CNS (88). Because the Keap1–Nrf2 system is a major regulator of ROS and also inflammatory responses, several natural and synthetic compounds that activate Nrf2 are being actively studied to develop therapies against MS, and several Nrf2 inducers are currently in clinical trials for the treatment of MS (reviewed in Ref. 12).
Table I. Summary of major Nrf2-activating drugs targeting T cell and B cell responses in various pathological conditions.
| Compound | Cell Type | Mechanism of Action | Conditions | References |
|---|---|---|---|---|
| BHA | Th1, Th2 | Electrophilic modification of Keap1 through Cys23, Cys151, Cys226, and Cys368 | Th1/Th2 balance in mice | (10, 114) |
| DMF | Th1, Th2, Th17, B cells | Electrophilic modification of Keap1-Cys151 | Multiple sclerosis | (41, 75, 89–95, 97–103, 111) |
| NaB | Tregs | Uncharacterized (potentially modifying Keap1 through Cys residues) | Autoimmune uveitis | (58) |
| Sulforaphane | Th1, Th17, B cells | Electrophilic modification of Keap1-Cys151 | Mixed granulocytic mouse model of asthma Collagen-induced arthritis mouse model |
(55–57, 74, 111) |
| tBHQ | Th1, Th2, B cells | Electrophilic modification of Keap1 through Cys23, Cys151, Cys273, Cys288, Cys226, and Cys368 | Th1/Th2 balance in mice IgM production by B cells |
(10, 50, 51, 70, 114) |
| Triterpenoids: CDDO-Im, CDDO-Me, CDDO-EA, CDDO-TFEA | Th1, Th17 | Electrophilic modification of Keap1 through Cys257, Cys288, Cys489, Cys513, and Cys613 and Tyr85 | Experimental autoimmune encephalomyelitis (CDDO-Me, CDDO-EA, and CDO-TFEA) Multiple Sclerosis (CDDO-Im) |
(52, 56, 64, 115, 116) |
| 4-Octyl itaconate | Th0 | Alkylation of Keap1 cysteine residues 151, 257, 288, 273, and 297 | Juvenile idiopathic arthritis | (56, 117) |
| A-1396076 | Th0 | Uncharacterized (selective binding to Keap1) | Rat adjuvant-induced arthritis IFN-α accelerated lupus nephritis Rat MOG experimental autoimmune Encephalomyelitis Rat collagen-induced arthritis Mouse GPI-induced arthritis Collagen Ab-induced arthritis Mouse OVA lung inflammation |
(104) |
BHA, butylated hydroxyanisole; CDDO, 1-(2-cyano-3-,12-dioxooleana-1,9(11)-dien-28-oyl); CDDO-EA, CDDO-ethyl amide; CDDO-Me, CDDO-methyl ester; CDDO-TFEA, CDDO-trifluoethylamide; MOG, myelin oligodendrocyte glycoprotein NaB, sodium butyrate.
Mechanistically, in MS patients, DMF is shown to have an immunosuppressive role with differential effects on the number and percentages of different subsets of immune cells (89) (reviewed Ref. (90). Studies show that DMF treatment decreases the total number of leukocytes and lymphocytes, which may induce lymphopenia in patients (41, 90–94). DMF selectively reduced the population of cytotoxic T cells (high CD4+/CD8+ T cell ratio), although there was an overall decrease in the number of both CD4+ and CD8+ T cells (95–98). DMF was also shown to reduce memory T cells and shift the balance from proinflammatory Th1/Th17 to an anti-inflammatory Th2 phenotype in MS patients (99). Additionally, DMF alters the metabolic profile of human T cells and restricts their antioxidative capacities by decreasing intracellular levels of glutathione (100). DMF is also shown to cause a shift toward an anti-inflammatory B cell phenotype with a decrease in mature, memory B cells as well as plasmablasts and an increase in immature, transitional B cells (75, 101–103).
A recent study showed that a potent and specific activator of Nrf2, named A-1396076, inhibits inflammation across several rodent models of autoimmunity by dampening Ag-dependent T cell activation (104). Studies have established a key role of Keap1–Nrf2 signaling in the dampening of acute and chronic inflammation in diseases such as rheumatoid arthritis, asthma, and atherosclerosis by maintaining mitochondrial function, restoring redox homeostasis, and suppressing inflammatory cytokine production (105). T cell–specific activation of Nrf2 provides significant protection against ischemia/reperfusion-induced acute kidney injury in mice, resulting in their improved survival. Similarly, the adoptive transfer of Nrf2-activated T cells to WT mice improved outcomes from acute kidney injury (11). Nrf2 is viewed as a potent therapeutic option for treating T cell–mediated inflammatory diseases such as inflammatory bowel disease/colitis. In fact, Nrf2 activation through different compounds has been shown to be beneficial in exerting a protective effect against colitis in experimental animal models (106–110), paving the way for the development of an effective therapeutic target against inflammatory bowel disease. Increasing numbers of clinical trials using Nrf2 activators are underway for treating an array of human diseases (reviewed in Refs. (111, 112).
Although there is plenty of research dedicated to the development of Nrf2 activators, the use of pharmacological inhibitors of Nrf2 in modulating T cell function is severely lacking. Some studies, albeit in cancer cells, showed the anticancer effect of Nrf2 inhibition (111). However, either the effect of this inhibition is unspecific or the underlying mechanism of the function of the inhibitors is unknown, highlighting the research gap that needs to be addressed before using these inhibitors to treat immune-mediated pathologies. Because of the pleiotropic functions of the Keap1–Nrf2 system, there may be potential off-target effects of these chemicals, making it challenging for drug development. With more studies and a better understanding of the mechanism of Nrf2 activation and its function, superior drugs with improved pharmacodynamic profiles could be developed to target specific diseases.
On the horizon
Although the broad immunomodulatory role of the antioxidation pathway or its proteins is now understood, its impact on specific immune cells is still ambiguous. A limitation of some of the existing studies is the usage of chemical activators that may have broad nonspecific targets. Although these studies certainly provide essential insight into the overall impact of Nrf2-modulating drugs in preclinical models for therapeutic potential, using them to identify cellular processes modulated by Nrf2 is not ideal. Another limitation of some of the existing studies is the usage of Nrf2-null animals to answer immunological questions. Because Keap1 and Nrf2 are ubiquitously expressed in all mammalian cells, dissecting their cell-intrinsic mechanisms in immune cells and how they contribute to disease outcome is a challenge. Using animal models with conditional T cell– or B cell–specific gene ablation or activation of Nrf2, Keap1, or both would be a much cleaner system for identifying cell-specific roles.
Studies investigating the role of antioxidation in B cell development are still awaited. Although much needs to be done to identify the impact of Keap1–Nrf2 on B cell development and B cell responses, their role in T cell development and functions is also not yet fully understood. Having identified that ROS levels are critical for innate-like NKT cell immune functions and that Keap1 and Nrf2 partake in their development, it will be interesting to see whether the same is true for other innate T cells, namely γδ T cells and MALT cells. Increasing evidence indicates a key role of Nrf2 in favoring the differentiation of CD4 T cells to Th2 and Treg subsets, while suppressing the Th1 and Th17 generation. However, the role of Nrf2 in the differentiation of CD4 T cells to Th9, Th22, or T follicular helper T cell subsets is undeciphered. Also undetermined is how the Keap1–Nrf2 complex contributes to CD8 T cell activation and/or cytotoxic functions. It is possible that this pathway modulates CD8 T cell responses in a manner similar to CD4 T cells when it is a T cell–specific mechanism.
Most of the studies identifying the immunomodulatory role of Keap1–Nrf2 are phenotypic. Mechanistically, much remains to be deciphered about how they manipulate immune cell functions. It would be interesting to see whether the Keap1–Nrf2 pathway cross-talks with the TCR-signaling pathway in activated T cells. Studies have shown that the decreased activation of T cells in Nrf2 activator–treated cells is because of decreased binding of NF-κB to the DNA. Further studies focusing on the crosstalk with other signaling cascades such as JAK-STAT pathways are warranted. Also, note that Nqo1 and other Nrf2 target genes also have NF-κB binding sites (113). Recent studies have established that metabolism is central to immune cell functions. Although Nrf2 is a well-known modulator of tumor cell metabolism, studies focusing on the role of Nrf2 in T cell or B cell metabolism are very rare. Thus, detailed studies are required to elucidate the molecular mechanisms involved at the frontier of Nrf2 and T cell biology. Some exciting prospects for the future would be to try to identify specific metabolites that can initiate this signaling pathway or that are regulated by this pathway to manipulate cellular functions. Further exploration and thorough characterization of the immunomodulatory effects of Nrf2 in a cell type– and experimental model–specific manner are essential before developing Nrf2 modulators as therapeutic interventions against various diseases.
Finally, although Nrf2 expression is known to be governed by Keap1, it is possible that some of the functions of Nrf2 could be independent of Keap1 and that Nrf2 may be regulated by Keap1-independent mechanisms in immune cells. In either case, more studies are needed to identify any such possibilities. By modulating various cellular processes ranging from antioxidation to metabolism, the Keap1–Nrf2 system has emerged as a key player in several cellular processes. Findings deciphering the contributions of Keap1–Nrf2 in immune cell functions only add to the importance of this complex in the maintenance of overall health and disease. In all, future studies deciphering the role of Nrf2 in immune cells will not only further our understanding of the fundamentals of T cell activation, but also provide novel considerations when designing therapies against T cell–mediated pathologies. There are numerous ongoing clinical trials using Nrf2-targeting drugs, which indicate that the Keap1–Nrf2 system is a promising pharmacological target.
Footnotes
This work was supported by startup funds to K.P. by Kansas State University and the University of Kansas Comprehensive Cancer Center, as well as by an institutional development award from the National Institute of General Medical Sciences through National Institutes of Health Grant K-INBRE P20 GM103418 to K.P. A.P. was supported by a postdoctoral award through National Institutes of Health Grant K-INBRE P20 GM103418. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. D.D. received a graduate student cancer research award from Johnson Cancer Research Center of Kansas State University.
- CDDO-Im
- 2-cyano-3, 12 dioxooleana-1, 9 diene-28-imidazolide
- Cul3
- cullin 3
- DMF
- dimethyl fumarate
- HO-1
- heme oxygenase 1
- HSC
- hematopoietic stem cell
- Keap1
- Kelch-like ECH-associated protein 1
- MS
- multiple sclerosis
- Nrf2
- NF erythroid 2–related factor 2
- ROS
- reactive oxygen species
- tBHQ
- tert-butylhydroquinone
- Treg
- regulatory T cell
- WT
- wild-type
Disclosures
The authors have no financial conflicts of interest.
References
- 1. Pizzino, G., Irrera N., Cucinotta M., Pallio G., Mannino F., Arcoraci V., Squadrito F., Altavilla D., Bitto A.. 2017. Oxidative stress: harms and benefits for human health. Oxid. Med. Cell. Longev. 2017: 8416763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yarosz, E. L., Chang C.-H.. 2018. The role of reactive oxygen species in regulating T cell-mediated immunity and disease. Immune Netw. 18: e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schieber, M., Chandel N. S.. 2014. ROS function in redox signaling and oxidative stress. Curr. Biol. 24: R453–R462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kesarwani, P., Murali A. K., Al-Khami A. A., Mehrotra S.. 2013. Redox regulation of T-cell function: from molecular mechanisms to significance in human health and disease. Antioxid. Redox Signal. 18: 1497–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Li, J., Baker J., Higham A., Shah R., Montero-Fernandez A., Murray C., Cooper N., Lucas C., Fox C., Singh D., Lea S.. 2022. COPD lung studies of Nrf2 expression and the effects of Nrf2 activators. Inflammopharmacology 30: 1431–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marzec, J. M., Christie J. D., Reddy S. P., Jedlicka A. E., Vuong H., Lanken P. N., Aplenc R., Yamamoto T., Yamamoto M., Cho H.-Y., Kleeberger S. R.. 2007. Functional polymorphisms in the transcription factor NRF2 in humans increase the risk of acute lung injury. FASEB J. 21: 2237–2246. [DOI] [PubMed] [Google Scholar]
- 7. Qin, Q., Qu C., Niu T., Zang H., Qi L., Lyu L., Wang X., Nagarkatti M., Nagarkatti P., Janicki J. S., et al. 2016. Nrf2-mediated cardiac maladaptive remodeling and dysfunction in a setting of autophagy insufficiency. Hypertension 67: 107–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tan, Y., Ichikawa T., Li J., Si Q., Yang H., Chen X., Goldblatt C. S., Meyer C. J., Li X., Cai L., Cui T.. 2011. Diabetic downregulation of Nrf2 activity via ERK contributes to oxidative stress-induced insulin resistance in cardiac cells in vitro and in vivo. Diabetes 60: 625–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yamaguchi, Y., Kamai T., Higashi S., Murakami S., Arai K., Shirataki H., Yoshida K.-I.. 2019. Nrf2 gene mutation and single nucleotide polymorphism rs6721961 of the Nrf2 promoter region in renal cell cancer. BMC Cancer 19: 1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rockwell, C. E., Zhang M., Fields P. E., Klaassen C. D.. 2012. Th2 skewing by activation of Nrf2 in CD4+ T cells. J. Immunol. 188: 1630–1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Noel, S., Martina M. N., Bandapalle S., Racusen L. C., Potteti H. R., Hamad A. R. A., Reddy S. P., Rabb H.. 2015. T lymphocyte-specific activation of Nrf2 protects from AKI. J. Am. Soc. Nephrol. 26: 2989–3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Michaličková, D., Hrnčíř T., Canová N. K., Slanař O.. 2020. Targeting Keap1/Nrf2/ARE signaling pathway in multiple sclerosis. Eur. J. Pharmacol. 873: 172973. [DOI] [PubMed] [Google Scholar]
- 13. Thimmulappa, R. K., Lee H., Rangasamy T., Reddy S. P., Yamamoto M., Kensler T. W., Biswal S.. 2006. Nrf2 is a critical regulator of the innate immune response and survival during experimental sepsis. J. Clin. Invest. 116: 984–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mitsuishi, Y., Taguchi K., Kawatani Y., Shibata T., Nukiwa T., Aburatani H., Yamamoto M., Motohashi H.. 2012. Nrf2 redirects glucose and glutamine into anabolic pathways in metabolic reprogramming. Cancer Cell 22: 66–79. [DOI] [PubMed] [Google Scholar]
- 15. Panieri, E., Telkoparan-Akillilar P., Suzen S., Saso L.. 2020. The NRF2/KEAP1 axis in the regulation of tumor metabolism: mechanisms and therapeutic perspectives. Biomolecules 10: 791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rojo de la Vega, M., Chapman E., Zhang D. D.. 2018. NRF2 and the hallmarks of cancer. Cancer Cell 34: 21–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lu, M.-C., Ji J.-A., Jiang Z.-Y., You Q.-D.. 2016. The Keap1–Nrf2-ARE pathway as a potential preventive and therapeutic target: an update. Med. Res. Rev. 36: 924–963. [DOI] [PubMed] [Google Scholar]
- 18. Taguchi, K., Yamamoto M.. 2017. The KEAP1-NRF2 system in cancer. Front. Oncol. 7: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dinkova-Kostova, A. T., Kostov R. V., Canning P.. 2017. Keap1, the cysteine-based mammalian intracellular sensor for electrophiles and oxidants. Arch. Biochem. Biophys. 617: 84–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kopacz, A., Kloska D., Forman H. J., Jozkowicz A., Grochot-Przeczek A.. 2020. Beyond repression of Nrf2: an update on Keap1. Free Radic. Biol. Med. 157: 63–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Suzuki, T., Muramatsu A., Saito R., Iso T., Shibata T., Kuwata K., Kawaguchi S.-I., Iwawaki T., Adachi S., Suda H., et al. 2019. Molecular mechanism of cellular oxidative stress sensing by Keap1. Cell Rep. 28: 746–758.e4. [DOI] [PubMed] [Google Scholar]
- 22. Suzuki, T., Yamamoto M.. 2017. Stress-sensing mechanisms and the physiological roles of the Keap1–Nrf2 system during cellular stress. J. Biol. Chem. 292: 16817–16824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Canning, P., Sorrell F. J., Bullock A. N.. 2015. Structural basis of Keap1 interactions with Nrf2. Free Radic. Biol. Med. 88(Pt B): 101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Taguchi, K., Yamamoto M.. 2020. The KEAP1-NRF2 system as a molecular target of cancer treatment. Cancers (Basel) 13: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sykiotis, G. P., Bohmann D.. 2010. Stress-activated cap’n’collar transcription factors in aging and human disease. Sci. Signal. 3: re3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Li, W., Yu S., Liu T., Kim J.-H., Blank V., Li H., Kong A.-N. T.. 2008. Heterodimerization with small Maf proteins enhances nuclear retention of Nrf2 via masking the NESzip motif. Biochim. Biophys. Acta 1783: 1847–1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Motohashi, H., O’Connor T., Katsuoka F., Engel J. D., Yamamoto M.. 2002. Integration and diversity of the regulatory network composed of Maf and CNC families of transcription factors. Gene 294: 1–12. [DOI] [PubMed] [Google Scholar]
- 28. Nguyen, T., Sherratt P. J., Pickett C. B.. 2003. Regulatory mechanisms controlling gene expression mediated by the antioxidant response element. Annu. Rev. Pharmacol. Toxicol. 43: 233–260. [DOI] [PubMed] [Google Scholar]
- 29. Deshmukh, P., Unni S., Krishnappa G., Padmanabhan B.. 2017. The Keap1–Nrf2 pathway: promising therapeutic target to counteract ROS-mediated damage in cancers and neurodegenerative diseases. Biophys. Rev. 9: 41–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Taguchi, K., Motohashi H., Yamamoto M.. 2011. Molecular mechanisms of the Keap1–Nrf2 pathway in stress response and cancer evolution. Genes Cells 16: 123–140. [DOI] [PubMed] [Google Scholar]
- 31. Pyaram, K., Kumar A., Kim Y.-H., Noel S., Reddy S. P., Rabb H., Chang C.-H.. 2019. Keap1–Nrf2 system plays an important role in invariant natural killer T cell development and homeostasis. Cell Rep. 27: 699–707.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Iwasaki, A., Medzhitov R.. 2015. Control of adaptive immunity by the innate immune system. Nat. Immunol. 16: 343–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jain, A., Pasare C.. 2017. Innate control of adaptive immunity: beyond the three-signal paradigm. J. Immunol. 198: 3791–3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sallusto, F., Lanzavecchia A.. 2002. The instructive role of dendritic cells on T-cell responses. Arthritis Res. 4(Suppl 3): S127–S132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bird, L. 2020. MDSC metabolite stuns T cells. Nat. Rev. Immunol. 20: 352–353. [DOI] [PubMed] [Google Scholar]
- 36. Srivastava, M. K., Sinha P., Clements V. K., Rodriguez P., Ostrand-Rosenberg S.. 2010. Myeloid-derived suppressor cells inhibit T-cell activation by depleting cystine and cysteine. Cancer Res. 70: 68–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yeang, H. X. A., Hamdam J. M., Al-Huseini L. M. A., Sethu S., Djouhri L., Walsh J., Kitteringham N., Park B. K., Goldring C. E., Sathish J. G.. 2012. Loss of transcription factor nuclear factor-erythroid 2 (NF-E2) p45-related factor-2 (Nrf2) leads to dysregulation of immune functions, redox homeostasis, and intracellular signaling in dendritic cells. J. Biol. Chem. 287: 10556–10564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Al-Huseini, L. M. A., Aw Yeang H. X., Sethu S., Alhumeed N., Hamdam J. M., Tingle Y., Djouhri L., Kitteringham N., Park B. K., Goldring C. E., Sathish J. G.. 2013. Nuclear factor-erythroid 2 (NF-E2) p45-related factor-2 (Nrf2) modulates dendritic cell immune function through regulation of p38 MAPK-cAMP-responsive element binding protein/activating transcription factor 1 signaling. J. Biol. Chem. 288: 22281–22288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Helou, D. G., Noël B., Gaudin F., Groux H., El Ali Z., Pallardy M., Chollet-Martin S., Kerdine-Römer S.. 2019. Cutting edge: Nrf2 regulates neutrophil recruitment and accumulation in skin during contact hypersensitivity. J. Immunol. 202: 2189–2194. [DOI] [PubMed] [Google Scholar]
- 40. Ryan, D. G., Knatko E. V., Casey A. M., Hukelmann J. L., Dayalan Naidu S., Brenes A. J., Ekkunagul T., Baker C., Higgins M., Tronci L., et al. 2022. Nrf2 activation reprograms macrophage intermediary metabolism and suppresses the type I interferon response. iScience 25: 103827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Diebold, M., Sievers C., Bantug G., Sanderson N., Kappos L., Kuhle J., Lindberg R. L. P., Derfuss T.. 2018. Dimethyl fumarate influences innate and adaptive immunity in multiple sclerosis. J. Autoimmun. 86: 39–50. [DOI] [PubMed] [Google Scholar]
- 42. Beury, D. W., Carter K. A., Nelson C., Sinha P., Hanson E., Nyandjo M., Fitzgerald P. J., Majeed A., Wali N., Ostrand-Rosenberg S.. 2016. Myeloid-derived suppressor cell survival and function are regulated by the transcription factor Nrf2. J. Immunol. 196: 3470–3478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. van der Horst, D., Carter-Timofte M. E., van Grevenynghe J., Laguette N., Dinkova-Kostova A. T., Olagnier D.. 2022. Regulation of innate immunity by Nrf2. Curr. Opin. Immunol. 78: 102247. [DOI] [PubMed] [Google Scholar]
- 44. Battino, M., Giampieri F., Pistollato F., Sureda A., de Oliveira M. R., Pittalà V., Fallarino F., Nabavi S. F., Atanasov A. G., Nabavi S. M.. 2018. Nrf2 as regulator of innate immunity: a molecular Swiss army knife! Biotechnol. Adv. 36: 358–370. [DOI] [PubMed] [Google Scholar]
- 45. Murakami, S., Shimizu R., Romeo P.-H., Yamamoto M., Motohashi H.. 2014. Keap1–Nrf2 system regulates cell fate determination of hematopoietic stem cells. Genes Cells 19: 239–253. [DOI] [PubMed] [Google Scholar]
- 46. Tupin, E., Kinjo Y., Kronenberg M.. 2007. The unique role of natural killer T cells in the response to microorganisms. Nat. Rev. Microbiol. 5: 405–417. [DOI] [PubMed] [Google Scholar]
- 47. Van Kaer, L., Joyce S.. 2005. Innate immunity: NKT cells in the spotlight. Curr. Biol. 15: R429–R431. [DOI] [PubMed] [Google Scholar]
- 48. Kim, Y.-H., Kumar A., Chang C.-H., Pyaram K.. 2017. Reactive oxygen species regulate the inflammatory function of NKT cells through promyelocytic leukemia zinc finger. J. Immunol Baltim Md 199: 3478–3487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Savage, A. K., Constantinides M. G., Han J., Picard D., Martin E., Li B., Lantz O., Bendelac A.. 2008. The transcription factor PLZF directs the effector program of the NKT cell lineage. Immunity 29: 391–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Turley, A. E., Zagorski J. W., Rockwell C. E.. 2015. The Nrf2 activator tBHQ inhibits T cell activation of primary human CD4 T cells. Cytokine 71: 289–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Zagorski, J. W., Turley A. E., Dover H. E., VanDenBerg K. R., Compton J. R., Rockwell C. E.. 2013. The Nrf2 activator, tBHQ, differentially affects early events following stimulation of Jurkat cells. Toxicol. Sci. 136: 63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Zagorski, J. W., Turley A. E., Freeborn R. A., VanDenBerg K. R., Dover H. E., Kardell B. R., Liby K. T., Rockwell C. E.. 2018. Differential effects of the Nrf2 activators tBHQ and CDDO-Im on the early events of T cell activation. Biochem. Pharmacol. 147: 67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zhu, J., Yamane H., Paul W. E.. 2010. Differentiation of effector CD4 T cell populations. Annu. Rev. Immunol. 28: 445–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Morzadec, C., Macoch M., Sparfel L., Kerdine-Römer S., Fardel O., Vernhet L.. 2014. Nrf2 expression and activity in human T lymphocytes: stimulation by T cell receptor activation and priming by inorganic arsenic and tert-butylhydroquinone. Free Radic. Biol. Med. 71: 133–145. [DOI] [PubMed] [Google Scholar]
- 55. Li, B., Cui W., Liu J., Li R., Liu Q., Xie X.-H., Ge X.-L., Zhang J., Song X.-J., Wang Y., Guo L.. 2013. Sulforaphane ameliorates the development of experimental autoimmune encephalomyelitis by antagonizing oxidative stress and Th17-related inflammation in mice. Exp. Neurol. 250: 239–249. [DOI] [PubMed] [Google Scholar]
- 56. Pareek, T. K., Belkadi A., Kesavapany S., Zaremba A., Loh S. L., Bai L., Cohen M. L., Meyer C., Liby K. T., Miller R. H., et al. 2011. Triterpenoid modulation of IL-17 and Nrf-2 expression ameliorates neuroinflammation and promotes remyelination in autoimmune encephalomyelitis. Sci. Rep. 1: 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Al-Harbi, N. O., Nadeem A., Ahmad S. F., AlThagfan S. S., Alqinyah M., Alqahtani F., Ibrahim K. E., Al-Harbi M. M.. 2019. Sulforaphane treatment reverses corticosteroid resistance in a mixed granulocytic mouse model of asthma by upregulation of antioxidants and attenuation of Th17 immune responses in the airways. Eur. J. Pharmacol. 855: 276–284. [DOI] [PubMed] [Google Scholar]
- 58. Chen, X., Su W., Wan T., Yu J., Zhu W., Tang F., Liu G., Olsen N., Liang D., Zheng S. G.. 2017. Sodium butyrate regulates Th17/Treg cell balance to ameliorate uveitis via the Nrf2/HO-1 pathway. Biochem. Pharmacol. 142: 111–119. [DOI] [PubMed] [Google Scholar]
- 59. Zhao, M., Chen H., Ding Q., Xu X., Yu B., Huang Z.. 2016. Nuclear factor erythroid 2-related factor 2 deficiency exacerbates lupus nephritis in B6/lpr mice by regulating Th17 cell function. Sci. Rep. 6: 38619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Suzuki, T., Murakami S., Biswal S. S., Sakaguchi S., Harigae H., Yamamoto M., Motohashi H.. 2017. Systemic activation of NRF2 alleviates lethal autoimmune inflammation in scurfy mice. Mol. Cell. Biol. 37: e00063-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Klemm, P., Rajendiran A., Fragoulis A., Wruck C., Schippers A., Wagner N., Bopp T., Tenbrock K., Ohl K.. 2020. Nrf2 expression driven by Foxp3 specific deletion of Keap1 results in loss of immune tolerance in mice. Eur. J. Immunol. 50: 515–524. [DOI] [PubMed] [Google Scholar]
- 62. Chen, G.-Y., Chen C., Wang L., Chang X., Zheng P., Liu Y.. 2008. Cutting edge: broad expression of the FoxP3 locus in epithelial cells: a caution against early interpretation of fatal inflammatory diseases following in vivo depletion of FoxP3-expressing cells. J. Immunol. 180: 5163–5166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Tsai, J. J., Velardi E., Shono Y., Argyropoulos K. V., Holland A. M., Smith O. M., Yim N. L., Rao U. K., Kreines F. M., Lieberman S. R., et al. 2018. Nrf2 regulates CD4+ T cell-induced acute graft-versus-host disease in mice. Blood 132: 2763–2774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Lin, X., Tawch S., Wong H. T., Roy S., Gaudino S., Castillo P., Elsegeiny W., Wakabayashi N., Oury T. D., Pociask D., et al. 2021. Nrf2 through aryl hydrocarbon receptor regulates IL-22 Response in CD4+ T cells. J. Immunol. 206: 1540–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kojima, H., Kadono K., Hirao H., Dery K. J., Kupiec-Weglinski J. W.. 2023. CD4+ T cell NRF2 signaling improves liver transplantation outcomes by modulating T cell activation and differentiation. Antioxid. Redox Signal. 38: 670–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wang, H., Hogquist K. A.. 2018. How lipid-specific t cells become effectors: the differentiation of iNKT subsets. Front. Immunol. 9: 1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Cyster, J. G., Allen C. D. C.. 2019. B cell responses: cell interaction dynamics and decisions. Cell 177: 524–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Hoffman, W., Lakkis F. G., Chalasani G.. 2016. B cells, antibodies, and more. Clin. J. Am. Soc. Nephrol. 11: 137–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Bertolotti, M., Yim S. H., Garcia-Manteiga J. M., Masciarelli S., Kim Y.-J., Kang M.-H., Iuchi Y., Fujii J., Vené R., Rubartelli A., et al. 2010. B- to plasma-cell terminal differentiation entails oxidative stress and profound reshaping of the antioxidant responses. Antioxid. Redox Signal. 13: 1133–1144. [DOI] [PubMed] [Google Scholar]
- 70. Bursley, J. K., Rockwell C. E.. 2020. Nrf2-dependent and -independent effects of tBHQ in activated murine B cells. Food Chem. Toxicol. 145: 111595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Bancos, S., Baglole C. J., Rahman I., Phipps R. P.. 2010. Induction of heme oxygenase-1 in normal and malignant B lymphocytes by 15-deoxy-Δ12,14-prostaglandin J2 requires Nrf2. Cell. Immunol. 262: 18–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ryan, E. P., Pollock S. J., Murant T. I., Bernstein S. H., Felgar R. E., Phipps R. P.. 2005. Activated human B lymphocytes express cyclooxygenase-2 and cyclooxygenase inhibitors attenuate antibody production. J. Immunol. 174: 2619–2626. [DOI] [PubMed] [Google Scholar]
- 73. Jang, J.-W., Lee J.-W., Yoon Y. D., Kang J.-S., Moon E.-Y.. 2020. Bisphenol A and its substitutes regulate human B cell survival via Nrf2 expression. Environ. Pollut. 259: 113907. [DOI] [PubMed] [Google Scholar]
- 74. Moon, S.-J., Jhun J., Ryu J., Kwon J. Y., Kim S.-Y., Jung K., Cho M.-L., Min J.-K.. 2021. The anti-arthritis effect of sulforaphane, an activator of Nrf2, is associated with inhibition of both B cell differentiation and the production of inflammatory cytokines. [Published erratum appears in 2021 PLoS One 16: e0256716.] PLoS One 16: e0245986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Traub, J., Traffehn S., Ochs J., Häusser-Kinzel S., Stephan S., Scannevin R., Brück W., Metz I., Weber M. S.. 2019. Dimethyl fumarate impairs differentiated B cells and fosters central nervous system integrity in treatment of multiple sclerosis. Brain Pathol. 29: 640–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Lugade, A. A., Vethanayagam R. R., Nasirikenari M., Bogner P. N., Segal B. H., Thanavala Y.. 2011. Nrf2 regulates chronic lung inflammation and B-cell responses to nontypeable Haemophilus influenzae. Am. J. Respir. Cell Mol. Biol. 45: 557–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Wang, R., Green D. R.. 2012. Metabolic reprogramming and metabolic dependency in T cells. Immunol. Rev. 249: 14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Ohl, K., Fragoulis A., Klemm P., Baumeister J., Klock W., Verjans E., Böll S., Möllmann J., Lehrke M., Costa I., et al. 2018. Nrf2 is a central regulator of metabolic reprogramming of myeloid-derived suppressor cells in steady state and sepsis. Front. Immunol. 9: 1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Rajendiran, A., Subramanyam S. H., Klemm P., Jankowski V., van Loosdregt J., Vastert B., Vollbach K., Wagner N., Tenbrock K., Ohl K.. 2022. NRF2/itaconate axis regulates metabolism and inflammatory properties of T cells in children with JIA. Antioxidants 11: 2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Heiss, E. H., Schachner D., Zimmermann K., Dirsch V. M.. 2013. Glucose availability is a decisive factor for Nrf2-mediated gene expression. Redox Biol. 1: 359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Cachat, J., Deffert C., Hugues S., Krause K.-H.. 2015. Phagocyte NADPH oxidase and specific immunity. Clin. Sci. (Lond.) 128: 635–648. [DOI] [PubMed] [Google Scholar]
- 82. Jang, K.-J., Mano H., Aoki K., Hayashi T., Muto A., Nambu Y., Takahashi K., Itoh K., Taketani S., Nutt S. L., et al. 2015. Mitochondrial function provides instructive signals for activation-induced B-cell fates. Nat. Commun. 6: 6750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Wheeler, M. L., Defranco A. L.. 2012. Prolonged production of reactive oxygen species in response to B cell receptor stimulation promotes B cell activation and proliferation. J. Immunol. 189: 4405–4416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Zhang, H., Wang L., Chu Y.. 2019. Reactive oxygen species: the signal regulator of B cell. Free Radic. Biol. Med. 142: 16–22. [DOI] [PubMed] [Google Scholar]
- 85. Gautam, P., Kaushal J., Sharma A., Bhatnagar A.. 2022. Proportion of B cell subsets and Nrf2 mediated redox regulation in systemic lupus erythematosus patients. Immunobiology 227: 152180. [DOI] [PubMed] [Google Scholar]
- 86. Stein, M., Dütting S., Mougiakakos D., Bösl M., Fritsch K., Reimer D., Urbanczyk S., Steinmetz T., Schuh W., Bozec A., et al. 2017. A defined metabolic state in pre B cells governs B-cell development and is counterbalanced by Swiprosin-2/EFhd1. Cell Death Differ. 24: 1239–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Akkaya, M., Traba J., Roesler A. S., Miozzo P., Akkaya B., Theall B. P., Sohn H., Pena M., Smelkinson M., Kabat J., et al. 2018. Second signals rescue B cells from activation-induced mitochondrial dysfunction and death. Nat. Immunol. 19: 871–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Steinman, L. 2009. A molecular trio in relapse and remission in multiple sclerosis. Nat. Rev. Immunol. 9: 440–447. [DOI] [PubMed] [Google Scholar]
- 89. Diebold, M., Galli E., Kopf A., Sanderson N. S. R., Callegari I., Benkert P., Gonzalo Núñez N., Ingelfinger F., Herms S., Cichon S., et al. 2022. High-dimensional immune profiling identifies a biomarker to monitor dimethyl fumarate response in multiple sclerosis. Proc. Natl. Acad. Sci. USA 119: e2205042119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Montes Diaz, G., Hupperts R., Fraussen J., Somers V.. 2018. Dimethyl fumarate treatment in multiple sclerosis: recent advances in clinical and immunological studies. Autoimmun. Rev. 17: 1240–1250. [DOI] [PubMed] [Google Scholar]
- 91. Buckle, G., Bandari D., Greenstein J., Gudesblatt M., Khatri B., Kita M., Repovic P., Riser E., Weinstock-Guttman B., Thrower B., et al. 2020. Effect of dimethyl fumarate on lymphocyte subsets in patients with relapsing multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 6: 2055217320918619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Longbrake, E. E., Mao-Draayer Y., Cascione M., Zielinski T., Bame E., Brassat D., Chen C., Kapadia S., Mendoza J. P., Miller C., et al. 2021. Dimethyl fumarate treatment shifts the immune environment toward an anti-inflammatory cell profile while maintaining protective humoral immunity. Mult. Scler. 27: 883–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Mehta, D., Miller C., Arnold D. L., Bame E., Bar-Or A., Gold R., Hanna J., Kappos L., Liu S., Matta A., et al. 2019. Effect of dimethyl fumarate on lymphocytes in RRMS: implications for clinical practice. Neurology 92: e1724–e1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Sweetser, M. T., Dawson K. T., Bozic C.. 2013. Manufacturer’s response to case reports of PML. N. Engl. J. Med. 368: 1659–1661. [DOI] [PubMed] [Google Scholar]
- 95. Fleischer, V., Friedrich M., Rezk A., Bühler U., Witsch E., Uphaus T., Bittner S., Groppa S., Tackenberg B., Bar-Or A., et al. 2018. Treatment response to dimethyl fumarate is characterized by disproportionate CD8+ T cell reduction in MS. Mult. Scler. 24: 632–641. [DOI] [PubMed] [Google Scholar]
- 96. Khatri, B. O., Garland J., Berger J., Kramer J., Sershon L., Olapo T., Sesing J., Dukic M., Rehn E.. 2015. The effect of dimethyl fumarate (Tecfidera™) on lymphocyte counts: a potential contributor to progressive multifocal leukoencephalopathy risk. Mult. Scler. Relat. Disord. 4: 377–379. [DOI] [PubMed] [Google Scholar]
- 97. Lückel, C., Picard F., Raifer H., Campos Carrascosa L., Guralnik A., Zhang Y., Klein M., Bittner S., Steffen F., Moos S., et al. 2019. IL-17+ CD8+ T cell suppression by dimethyl fumarate associates with clinical response in multiple sclerosis. Nat. Commun. 10: 5722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Spencer, C. M., Crabtree-Hartman E. C., Lehmann-Horn K., Cree B. A. C., Zamvil S. S.. 2015. Reduction of CD8+ T lymphocytes in multiple sclerosis patients treated with dimethyl fumarate. Neurol. Neuroimmunol. Neuroinflamm. 2: e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Wu, Q., Wang Q., Mao G., Dowling C. A., Lundy S. K., Mao-Draayer Y.. 2017. Dimethyl fumarate selectively reduces memory T cells and shifts the balance between Th1/Th17 and Th2 in multiple sclerosis patients. J. Immunol. 198: 3069–3080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Liebmann, M., Korn L., Janoschka C., Albrecht S., Lauks S., Herrmann A. M., Schulte-Mecklenbeck A., Schwab N., Schneider-Hohendorf T., Eveslage M., et al. 2021. Dimethyl fumarate treatment restrains the antioxidative capacity of T cells to control autoimmunity. Brain 144: 3126–3141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Li, R., Rezk A., Ghadiri M., Luessi F., Zipp F., Li H., Giacomini P. S., Antel J., Bar-Or A.. 2017. Dimethyl fumarate treatment mediates an anti-inflammatory shift in B cell subsets of patients with multiple sclerosis. J. Immunol. 198: 691–698. [DOI] [PubMed] [Google Scholar]
- 102. Lundy, S. K., Wu Q., Wang Q., Dowling C. A., Taitano S. H., Mao G., Mao-Draayer Y.. 2016. Dimethyl fumarate treatment of relapsing-remitting multiple sclerosis influences B-cell subsets. Neurol. Neuroimmunol. Neuroinflamm. 3: e211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Smith, M. D., Martin K. A., Calabresi P. A., Bhargava P.. 2017. Dimethyl fumarate alters B-cell memory and cytokine production in MS patients. Ann. Clin. Transl. Neurol. 4: 351–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Goess, C., Terrillon S., Mayo M., Bousquet P., Wallace C., Hart M., Mathieu S., Twomey R., Donnelly-Roberts D., Namovic M., et al. 2020. NRF2 activator A-1396076 ameliorates inflammation in autoimmune disease models by inhibiting antigen dependent T cell activation. J. Transl. Autoimmun. 4: 100079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Tu, W., Wang H., Li S., Liu Q., Sha H.. 2019. The anti-inflammatory and anti-oxidant mechanisms of the Keap1/Nrf2/ARE signaling pathway in chronic diseases. Aging Dis. 10: 637–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Gao, Y., Bai D., Zhao Y., Zhu Q., Zhou Y., Li Z., Lu N.. 2019. LL202 ameliorates colitis against oxidative stress of macrophage by activation of the Nrf2/HO-1 pathway. J. Cell. Physiol. 234: 10625–10639. [DOI] [PubMed] [Google Scholar]
- 107. Liu, X., Zhou W., Zhang X., Lu P., Du Q., Tao L., Ding Y., Wang Y., Hu R.. 2016. Dimethyl fumarate ameliorates dextran sulfate sodium-induced murine experimental colitis by activating Nrf2 and suppressing NLRP3 inflammasome activation. Biochem. Pharmacol. 112: 37–49. [DOI] [PubMed] [Google Scholar]
- 108. Park, D. D., Yum H.-W., Zhong X., Kim S. H., Kim S. H., Kim D.-H., Kim S.-J., Na H.-K., Sato A., Miura T., Surh Y.-J.. 2017. Perilla frutescens extracts protects against dextran sulfate sodium-induced murine colitis: NF-κB, STAT3, and Nrf2 as putative targets. Front. Pharmacol. 8: 482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Yalniz, M., Demirel U., Orhan C., Bahcecioglu I. H., Ozercan I. H., Aygun C., Tuzcu M., Sahin K.. 2012. Nadroparin sodium activates Nrf2/HO-1 pathway in acetic acid-induced colitis in rats. Inflammation 35: 1213–1221. [DOI] [PubMed] [Google Scholar]
- 110. Yang, L., Shen L., Li Y., Li Y., Yu S., Wang S.. 2017. Hyperoside attenuates dextran sulfate sodium-induced colitis in mice possibly via activation of the Nrf2 signalling pathway. J. Inflamm. (Lond.) 14: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Robledinos-Antón, N., Fernández-Ginés R., Manda G., Cuadrado A.. 2019. Activators and inhibitors of NRF2: a review of their potential for clinical development. Oxid. Med. Cell. Longev. 2019: 9372182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Yagishita, Y., Gatbonton-Schwager T. N., McCallum M. L., Kensler T. W.. 2020. Current landscape of NRF2 biomarkers in clinical trials. Antioxidants 9: 716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Wardyn, J. D., Ponsford A. H., Sanderson C. M.. 2015. Dissecting molecular cross-talk between Nrf2 and NF-κB response pathways. Biochem. Soc. Trans. 43: 621–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Abiko, Y., Miura T., Phuc B. H., Shinkai Y., Kumagai Y.. 2011. Participation of covalent modification of Keap1 in the activation of Nrf2 by tert-butylbenzoquinone, an electrophilic metabolite of butylated hydroxyanisole. Toxicol. Appl. Pharmacol. 255: 32–39. [DOI] [PubMed] [Google Scholar]
- 115. Meng, X., Waddington J. C., Tailor A., Lister A., Hamlett J., Berry N., Park B. K., Sporn M. B.. 2020. CDDO-imidazolide targets multiple amino acid residues on the Nrf2 adaptor, Keap1. J. Med. Chem. 63: 9965–9976. [DOI] [PubMed] [Google Scholar]
- 116. Magesh, S., Chen Y., Hu L.. 2012. Small molecule modulators of Keap1–Nrf2-ARE pathway as potential preventive and therapeutic agents. Med. Res. Rev. 32: 687–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Mills, E. L., Ryan D. G., Prag H. A., Dikovskaya D., Menon D., Zaslona Z., Jedrychowski M. P., Costa A. S. H., Higgins M., Hams E., et al. 2018. Itaconate is an anti-inflammatory metabolite that activates Nrf2 via alkylation of KEAP1. Nature 556: 113–117. [DOI] [PMC free article] [PubMed] [Google Scholar]