Abstract
The coronavirus disease 2019 (COVID-19) may have a negative impact on the sexual health of male adults. An online questionnaire survey was conducted among male adults from February 04, 2023 to March 15, 2023 to analyze the impact of COVID-19 on the sexual health of male adults in China.
Participants provided about their medical, social, lifestyle, and family situations information through questionnaires including the Brief Sexual Function Inventory (BSFI). Sexual function problems were defined based on predetermined cutoff values of the BSFI domain scores.
A total of 1,250 male adults were included with median age as 32 years. According to the analysis of statistical results, sexual drive and erections firm enough to have sexual intercourse were reported to be present only a few days or less last month among 14.8 % and 11.1 % of COVID-19 survivors, respectively. Compared with uninfected persons, COVID-19 survivors had significantly lower scores on all BSFI domains and an increased risk of problems with sexual drive and erectile. In multivariate models of COVID-19 survivors, age ≥30 years, rural resident, lower education level, manual worker, lower income, and shorter duration from recovery to survey date were significantly associated with poorer overall sexual function.
In this study, COVID-19 survivors was reported to have significantly poorer sexual function than uninfected persons. The COVID-19 may have had a significant impact on the sexual health of Chinese male adults. We need to focus on sexual dysfunction in COVID-19 survivors, and proactively provide effective interventions.
Keywords: COVID-19 pandemic, Sexual health, Sexual functioning, Erectile dysfunction, Men’s health, Questionnaire
1. Introduction
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was designated as a public health emergency of international concern (PHEIC) by the World Health Organization (WHO) on January 31, 2020 (Kang and Xu, 2020). In addition to pulmonary symptoms, the clinical manifestations of COVID-19 also demonstrate different degrees of extra-pulmonary organ damage (Gupta et al., 2020). Large-scale statistical analyses in multiple countries have shown that disease severity and mortality are higher in men than in women, and male sex does appear to be a risk factor for serious infections worldwide (Aleksanyan and Weinman, 2022, Nassau et al., 2022). It is well known that androgens have high serum concentrations in men, and the underlying mechanism of SARS-CoV-2 virus entry and the severity of resulting COVID-19 may be influenced by androgens (Auerbach and Khera, 2021, Okwan-Duodu et al., 2021). The unique deleterious effects of the virus on male reproduction and sexual function are becoming increasingly apparent (Pijls et al., 2021, White, 2020). Nearly a quarter of infected men have been reported to be infected with epididymo-orchitis (Best et al., 2021). Following recovery from COVID-19, some COVID-19 survivors developed erectile dysfunction (ED), and viral particles were even found in the penile tissue of COVID-19 survivors up to 7 months after infection (Kresch et al., 2021). These phenomena raise concerns about the sexual health of male COVID-19 survivors.
During the pandemic, most studies have been focused on women or both genders, or explored the impact of psychological problems caused by the lockdown on sexual function (Fang et al., 2021, Li et al., 2020). From January of 2023, China government announced the lift of strict prevention and control measures against COVID-19 infection. The COVID-19 pandemic in China entered a new phase with a large number of Chinese men being infected with the virus. It is important to understand the effects of SARS-CoV-2 on male sexual function so that prevention and treatment can be developed (Dubin et al., 2022).
An online questionnaire survey was conducted to investigate the impact of COVID-19 infection on the sexual function of Chinese men in an environment with loosened control measures.
2. Participants and methods
2.1. Participants inclusion
An online questionnaire survey was conducted from February 4, 2023 to March 15, 2023 at the Urology Center of Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine. The online questionnaire was created using a professional system (Wenjuanxing, https://www.wjx.cn), and the survey was administered through social media including WeChat (version 8; Tencent, Shenzhen, China) and Douyin (www.douyin.com); the questionnaire was also accessed by participants scanning the QR code on posters put up in Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine. To be included in this survey, participants had to be Chinese men (aged 18–80 years) with a history of sexual intercourse. Informed consent was obtained from participants before they began the questionnaire, which stated privacy protection, and the survey was anonymous. Participants completed the questionnaire using a mobile phone or personal computer. Ethical approval for this study was obtained from the Ethics Committee of Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine.
2.2. Questionnaires
The questionnaire consists of three parts. The first part was the basic personal information of the participants, including age, height, body mass index (BMI) (Wang et al., 2021), marital status, education background, occupation, monthly income, living habits, and history of sexual-function-enhancing medications.
The second part was the diagnosis and treatment history of COVID-19, including the diagnosis method of COVID-19 infection, the number of vaccine shots received, clinical symptoms, drugs used for treatment, and duration from recovery to survey date.
The third part was the Brief Sexual Functioning Inventory (BSFI). The BSFI is an 11-item questionnaire about sexual experiences in the past 30 days. The questionnaire consists of three functional domains (two items for drive, three items for erection, and two items for ejaculation), one problem assessment domain (one item for drive, erection, and ejaculation, respectively), and one overall sexual satisfaction item (O'Leary et al., 1995). Participants responded with ratings from 0 to 4, with 0 indicating the worst functioning, biggest problems, or least satisfaction, and 4 indicating the opposite. We use domain scores (range 0–4) and BSFI total score (sum of all values except sexual satisfaction, range 0–40) to measure the overall sexual functioning of participants. Domain score is the average rating of total items in the corresponding domain. Referring to the relevant literature on male sexual function, we calculated the total score of each domain from the BSFI score, and the cutoff values for caseness (problem) were defined as drive ≤3, erection ≤7, ejaculation ≤5, and satisfaction ≤1 to compare sexual problems between COVID-19 survivors and normative data (NORM) (Dahl et al., 2007). A combined sum score for drive, erection, and ejaculation (DEE) was created and the problem defined as DEE ≤10. A problem with overall sexual function was defined as the presence of either a satisfactory problem and/or a DEE problem (Bersvendsen et al., 2020).
Cronbach’s coefficient alpha was calculated to assess internal consistency: BSFI 0.926.
2.3. Data collection
The data from participants with wrong information, those with an unclear diagnosis of COVID-19 infection, and those who had not recovered or duration from recovery to survey date less than one month were excluded.
2.4. Medication enhancing sexual function
We collected information on the use of medications enhancing sexual function, including pro-erectile medications (including sidenafil and tadafil), traditional Chinese medicine (TCM) (e.g. Wuzi Yanzong pill, Liuwei Dihuang pill, Shenqi Dihuang decoction, etc.), and others. Five sets of categorical variables were constructed for COVID-19 survivors based on their medication use prior to infection: (1) no sexual function enhancing medication; (2) pro-erectile medication; (3) TCM; (4) concomitant use of pro-erectile medication and TCM; (5) other.
2.5. Statistics
Descriptive characteristics were presented as median (range) for age variables, number (percentage) for each categorical variable, and mean (standard deviation) for BSFI score. Independent sample t-test was used to compare the means among the data according to the data type. The resulting BSFI score was transformed into binary qualitative data according to the threshold, and age-stratified binary logistic regression was used to assess the association between the independent and outcome variables as odds ratios (OR) with 95 % confidence intervals. Age-adjusted and multivariable linear regression models were used to assess the association between the independent variables and the outcome variables, using the unstandardized regression coefficient beta with 95 % confidence intervals. Variables with p values ≤ 0.25 in the age-adjusted models were included as independent variables in the multivariate model (Bersvendsen et al., 2020), and a stepwise regression process was performed.
Effect sizes were used as a measure to assess the clinical significance and were reported as standardized mean differences, with the standard deviations of the NORM group as the denominator due to heteroskedasticity, and the equation: standardized mean difference (SMD) = . Effect size was considered as none (0–0.20), small (0.21–0.49), and moderate (ES ≥0.50) clinical significance(Schober et al., 2021).
A two-sided p values ≤ 0.05 was considered to indicate statistical significance. SPSS version 25 (IBM Corporation, Armonk, NY, USA) and SAS version 9.4 (SAS Institute, Cary, NC) was used as statistical software.
3. Results
3.1. Study sample characteristics
In total, 1398 male adults participated in the survey (Fig. 1). Based on the inclusion criteria, we excluded male participants with obviously incorrect information (n = 5), unclear diagnosis of COVID-19 infection (n = 76), not recovered (n = 15), and duration from recovery to survey date less than one month (n = 63). The remaining 1250 participants represented the sample included in the analyses. 1052 (84.1 %) males with previous COVID-19 infection constituted COVID-19 survivor group, and 198 (15.8 %) uninfected males constituted normative group (NORM).
Fig. 1.
Flow chart of the online questionnaire survey on adult male sexual function in China from February 4, 2023 to March 15, 2023.
The median age of COVID-19 survivors was 33 years (Table 1). 48.2 % males were normal body size (BMI ranged from 18.5 to 24 kg/m2), 57.2 % in a marital relationship, 18.0 % rural residents. Among them, 23.2 % were smokers, 43.6 % alcohol drinkers, and 58.7 % with exercise habits. 33.9 % of COVID-19 survivors had a master degree or above, 34.5 % public employees (including medical workers, teachers, and civil servants) which accounts for the largest proportion, and 62.9 % had an monthly income of more than 7,000 CNY. Among the COVID-19 survivor group, 74.8 % had received three or more vaccine shots, 46.3 % had been recovered from COVID-19 for 30–59 days when they participated in the survey, and 10.7 % had taken medications to enhance sexual function prior to infection.
Table 1.
Characteristics of NORM and COVID-19 survivors who participated in the online questionnaire in China from February 4, 2023 to March 15, 2023.
| NORM (n = 198) |
COVID-19 survivors (n = 1052) |
||
|---|---|---|---|
| Age, years | 29.5(19–62) | 33(18–69) | |
| BMIa | |||
| Underweight | 10(5.0) | 31(2.9) | |
| Normal | 109(55.0) | 508(48.2) | |
| Overweight | 68(34.3) | 399(37.9) | |
| Obesity | 11(5.5) | 114(10.8) | |
| In a marital relationship | 84(42.4) | 602(57.2) | |
| Rural resident | 57(28.8) | 189(18.0) | |
| Lifestyle behavior | |||
| Smokingb | 48(24.2) | 244(23.2) | |
| Drinkingb | 79(39.9) | 459(43.6) | |
| Exercisingc | 100(50.5) | 617(58.7) | |
| Highest academic degree | |||
| Junior middle school or lower | 9(4.6) | 24(2.3) | |
| Senior middle school and technical secondary school | 19(9.6) | 65(6.2) | |
| Undergraduate and junior college | 104(52.5) | 606(57.6) | |
| Master or above | 66(33.3) | 357(33.9) | |
| Occupation | |||
| Workers and peasants | 11(5.6) | 49(4.7) | |
| Students | 38(19.2) | 102(9.7) | |
| Medical workers, teachers and civil servants | 57(28.8) | 363(34.5) | |
| Company clerks | 38(19.2) | 244(23.2) | |
| Managers and self-employed people | 18(9.1) | 150(14.3) | |
| Retirees | 0(0) | 10(1.0) | |
| Service trades and salespeople | 10(5.1) | 34(3.2) | |
| Freelancing and other professions | 26(13.1) | 100(9.5) | |
| Monthly income, CNY | |||
| No income | 20(10.1) | 63(6.0) | |
| <1,000 | 24(12.1) | 39(3.7) | |
| 2,000–3,999 | 12(6.1) | 65(6.2) | |
| 4,000–6,999 | 33(16.7) | 223(21.2) | |
| ≥7,000 | 109(55.0) | 662(62.9) | |
| Medication to enhance sexual functiond | 24(12.1) | 102(9.7) | |
| Pro-erectile medication | 4(2.0) | 60(5.7) | |
| TCM | 14(7.0) | 13(1.2) | |
| Pro-erectile medication combines with TCM | 6(3.0) | 19(1.8) | |
| Others | 0 | 10(0.9) | |
| Number of vaccine shots receivede | |||
| None | 8(4.0) | 42(4.0) | |
| 1 | 9(4.6) | 24(2.3) | |
| 2 | 25(12.6) | 199(19.0) | |
| 3 | 126(63.6) | 733(69.7) | |
| >3 | 30(15.2) | 54(5.1) | |
| Duration from recovery to survey datef, days | |||
| 30–59 | 488(46.3) | ||
| 60–89 | 356(33.8) | ||
| ≥90 | 208(19.7) | ||
Data are presented as numbers (%) unless otherwise specified.
NROM normative data, COVID-19 Coronavirus Disease 2019, BMI body-mass index, CNY Chinese yuan, TCM Traditional Chinese medicine.
BMI classification is defined by Chinese cutoff points. Underweight: <18.5 kg/m2; Normal: 18.5–24 kg/m2; Overweight: 24–28 kg/m2; Obesity: ≥28 kg/m2.
Daily or occasionally.
Physical activity less than 150 min/week of moderate activity, or less than 75 min of strenuous activity.
Medications taken before infection with COVID-19. Pro-erectile medication includes sildenafil and tadalafil; TCM includes Wuzi Yanzong pill, Liuwei Dihuang pill, Shenqi Dihuang decoction and other formulas.
The COVID-19 vaccine.
Recovery was defined as the disappearance of symptoms of COVID-19 infection and negative nucleic acid test for two consecutive days.
The median age of NORM was 29.5 years. 55 % were normal body size, 42.4 % in a marital relationship, and 28.8 % rural residents. 24.2 % NORM parcipicants were smokers, 39.9 % alcohol drinkers, and 50.5 % with exercise habits. 33.3 % had a master degree or above, 28.8 % public employees which accounts for the largest proportion, and 55.0 % had an income of more than 7,000 CNY. Among the NORM group, 78.8 % had received three or more vaccine shots, and 12.1 % had taken medications to enhance sexual function prior to infection.
3.2. Sexual outcomes
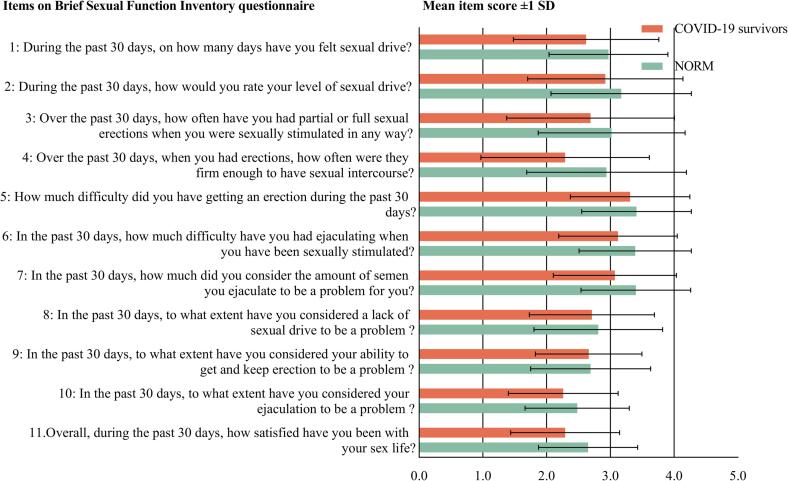
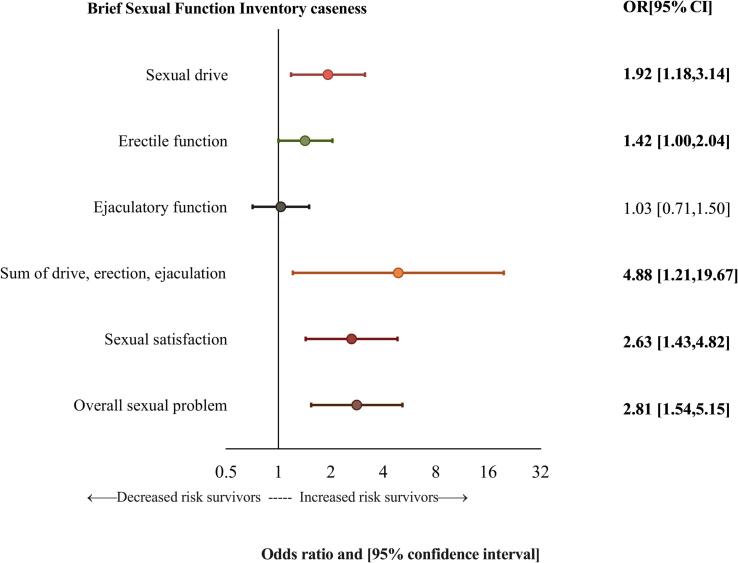
14.8 % of COVID-19 survivors reported sexual drive only a few days or less in the past 30 days, and 11.1 % of COVID-19 survivors reported erections firm enough to have sexual intercourse only a few times or less in the past 30 days. 15.9 % of survivors were mostly or very dissatisfied with their sexual life (Fig. 2). COVID-19 survivors had lower scores on all BSFI items and sexual domains compared to NORM (all p values < 0.05) (Fig. 3 and Table 2), and the differences in domain scores were clinically significant. The effect sizes of erectile function, ejaculatory function, overall sexual functioning, and sexual satisfaction increased with age among young and middle-aged people (18–49 years old). Among COVID-19 survivors, 18.82 % had sexual drive problems, 30.80 % had erectile problems, and 16.92 % had overall sexual problems (Table 3). The corresponding proportions among NORM were 10.61 %, 23.74 %, and 6.06 %. Compared with NORM, the probability of a sexual problem among COVID-19 survivors was 1.5 to 5 times increased for all domains except ejaculation (Fig. 4 and Table 3). Age-stratified comparisons with NORM showed the greatest increased risk for sexual drive problems among men 30–39 years old, and the greatest increased risk of erection, sexual satisfaction problems, and overall sexual problems among men aged 40–49 years (Table 3).
Fig. 2.
Males recovered from the coronavirus disease 2019 (COVID-19) response to the Brief Sexual Function Inventory (BSFI) items in China from February 4, 2023 to March 15, 2023.
Fig. 3.
Brief Sexual Function Inventory (BSFI) mean item score in males recovered from the novel coronavirus infection (n = 1052) and normative data (NORM) (n = 198) in China from February 4, 2023 to March 15, 2023. Score: question 1–7: 0–4 (never or poor function-always or good function); question 8–10: 0–4 (big problem – no problem); question 11: 0–4 (very unsatisfied – very satisfied).
Table 2.
BSFI outcomes (sexual function domains, total BSFI score, and sexual satisfaction) among male COVID-19 survivors and NORM in China from February 4, 2023 to March 15, 2023, overall and age-stratified.
| Sexual drive | Erectile function | Ejaculatory function | Problem assessment | Total BSFI score (overall sexual functioning) | Sexual satisfaction | ||
|---|---|---|---|---|---|---|---|
| Total sample | |||||||
| NORM (n = 198) | 2.56(0.72) | 2.96(0.72) | 3.40(0.78) | 3.04(1.07) | 29.95(6.6) | 2.97(0.93) | |
| COVID-19 survivors (n = 1,052) |
2.28(0.81) | 2.81(0.79) | 3.22(0.85) | 2.63(1.16) | 27.33(7.99) | 2.62(1.14) | |
| p valuea | <0.001 | 0.012 | 0.0051 | <0.001 | <0.001 | <0.001 | |
| SMDb | −0.40 | −0.21 | −0.23 | −0.38 | −0.40 | −0.38 | |
| 18–29 years | |||||||
| NORM (n = 99) | 2.61(0.78) | 3.02(0.67) | 3.49(0.72) | 3.26(0.99) | 31.06(5.7) | 3.03(1) | |
| COVID-19 survivors (n = 417) |
2.45(0.76) | 2.96(0.66) | 3.46(0.7) | 2.97(1.05) | 29.61(6.56) | 2.86(1.02) | |
| p valuea | 0.0647 | 0.4035 | 0.6841 | 0.012 | 0.0439 | 0.1329 | |
| SMDb | −0.20 | −0.09 | −0.04 | −0.30 | −0.25 | −0.17 | |
| 30–39 years | |||||||
| NORM (n = 41) | 2.70(0.55) | 3.07(0.73) | 3.39(0.84) | 2.89(1.14) | 30.07(6.91) | 3.00(0.89) | |
| COVID-19 survivors (n = 271) |
2.31(0.81) | 2.93(0.79) | 3.25(0.79) | 2.77(1.06) | 28.20(7.56) | 2.68(1.09) | |
| p valuea | 0.0038 | 0.2609 | 0.2774 | 0.489 | 0.1368 | 0.0744 | |
| SMDb | −0.70 | −0.20 | −0.17 | −0.11 | −0.27 | −0.36 | |
| 40–49 years | |||||||
| NORM (n = 24) | 2.54(0.83) | 3.11(0.56) | 3.46(0.87) | 3.24(0.95) | 31.04(7.07) | 3.08(0.72) | |
| COVID-19 survivors (n = 240) |
2.11(0.82) | 2.61(0.86) | 2.99(0.88) | 2.19(1.2) | 24.59(8.59) | 2.31(1.27) | |
| p valuea | 0.0139 | 0.0054 | 0.0133 | <0.001 | 0.0004 | 0.0036 | |
| SMDb | −0.52 | −0.89 | −0.54 | −1.11 | −0.91 | −1.08 | |
| >50 years | |||||||
| NORM (n = 34) | 2.28(0.61) | 2.56(0.82) | 3.09(0.74) | 2.46(1.09) | 25.79(6.95) | 2.71(0.87) | |
| COVID-19 survivors (n = 124) |
1.93(0.77) | 2.47(0.86) | 2.77(1.06) | 2.08(1.13) | 23.02(8.83) | 2.28(1.14) | |
| p valuea | 0.0154 | 0.5712 | 0.0976 | 0.0788 | 0.092 | 0.0469 | |
| SMDb | −0.58 | −0.11 | −0.43 | −0.35 | −0.40 | −0.49 | |
Range score possible: sexual drive 0–4, erectile function 0–4, ejaculatory function 0–4, problem assessment 0–4, total BSFI score 0–40, sexual satisfaction 0–4.
Bold type indicating statistical significance (p value < 0.05) or moderate clinical significance (effect size ≥ 0.50).
Data are presented as mean (SD) unless otherwise specified.
BSFI Brief Sexual Function Inventory, NORM normative data, COVID-19 coronavirus disease 2019, SMD standardized mean difference.
Select independent sample t-test or variance analysis according to data type.
Equation: SMD =.
Table 3.
Age-stratified odds ratios for BSFI caseness (problem) comparing COVID-19 survivors with normative controls in China from February 4, 2023 to March 15, 2023 using logistic regression models.
| Domain problem |
|||||||
|---|---|---|---|---|---|---|---|
| Sexual drive | Erectile function | Ejaculatory function | DEE | Sexual satisfaction |
Overall sexual problem |
||
| Total sample, n = 198 NORM/1,052 COVID-19 survivors | |||||||
| NORM | 21(10.61) | 47(23.74) | 43(21.72) | 2(1.01) | 12(6.06) | 12(6.06) | |
| COVID-19 survivors | 198(18.82) | 324(30.80) | 250(23.76) | 56(5.32) | 168(15.97) | 178(16.92) | |
| Odds ratio [95 % CI], reference = NORMa | 1.92[1.18,3.14] | 1.42[1.00,2.04] | 1.03[0.71,1.50] | 4.88[1.21,19.67] | 2.63[1.43,4.82] | 2.81[1.54,5.15] | |
| 18–29 years, n = 99 NORM/417 COVID-19 survivors | |||||||
| NORM | 9(9.09) | 20(20.2) | 16(16.16) | 0(0) | 7(7.07) | 7(7.07) | |
| COVID-19 survivors | 46(11.03) | 96(23.02) | 53(12.71) | 6(1.44) | 36(8.63) | 36(8.63) | |
| Odds ratio [95 % CI], reference = NORM | 1.24[0.59,2.62] | 1.18[0.69,2.03] | 0.76[0.41,1.39] | 3.14[0.18,56.26] | 1.24[0.54,2.88] | 1.24[0.54,2.88] | |
| 30–39 years, n = 41 NORM/271 COVID-19 survivors | |||||||
| NORM | 1(2.44) | 6(14.63) | 9(21.95) | 2(4.88) | 3(7.32) | 3(7.32) | |
| COVID-19 survivors | 52(19.19) | 74(27.31) | 55(20.3) | 12(4.43) | 40(14.76) | 44(16.24) | |
| Odds ratio [95 % CI], reference = cNORM | 9.50[1.28,70.69] | 2.19[0.88,5.43] | 0.9[0.41,2.01] | 0.9[0.19,4.18] | 2.19[0.65,7.46] | 2.46[0.73,8.33] | |
| 40–49 years, n = 24 NORM/240 COVID-19 survivors | |||||||
| NORM | 3(12.50) | 4(16.67) | 7(29.17) | 0(0) | 0(0) | 0(0) | |
| COVID-19 survivors | 61(25.42) | 98(40.83) | 92(38.33) | 22(9.17) | 65(27.08) | 68(28.33) | |
| Odds ratio [95 % CI], reference = NORM | 2.39[0.69,8.26] | 3.45[1.14,10.41] | 1.51[0.6,3.77] | 5.05[0.30,85.79] | 18.29[1.10,305.07] | 19.458[1.17,324.46] | |
| >50 years, n = 34 NORM/124 COVID-19 survivors | |||||||
| NORM | 8(23.53) | 17(50) | 11(32.35) | 0(0) | 2(5.88) | 2(5.88) | |
| COVID-19 survivors | 39(31.45) | 56(45.16) | 50(40.32) | 16(12.9) | 27(21.77) | 30(24.19) | |
| Odds ratio [95 % CI], reference = NORM | 1.49[0.62,3.58] | 0.82[0.39,1.76] | 1.41[0.63,3.15] | 10.49[0.61,179.50] | 4.45[1.00,19.78] | 5.10[1.16,22.58] | |
Bold type indicating statistical significance (p value < 0.05). Data are presented as numbers (%) unless otherwise specified.
NORM normative data, BSFI Brief Sexual Function Inventory, COVID-19 coronavirus disease 2019, DEE drive, erection, and ejaculation.
Age-adjusted.
Fig. 4.
Odds ratio and 95 % confidence interval [95 %] for Brief Sexual Function Inventory (BSFI) problem* among male recovered from the novel coronavirus infection in China from February 4, 2023 to March 15, 2023, reference = normative data (NORM). Asterisk indicates categorized as problem (caseness) if total score on current domain: sexual drive ≤ 3; erectile function ≤ 7; ejaculatory function ≤ 5; DEE (drive, erection, ejaculation) problems ≤ 10; sexual satisfaction ≤ 1; overall sexual problem = either DEE problem or overall satisfaction problem.
3.3. Sexual function enhancing medication
We analyzed the use of medications that enhance sexual function (prior to Covid-19 infection) (Table 1). Among the participants included in the analysis, 126 (10.1 %) males had taken medications to enhance sexual function, including 102 (8.2 %) COVID-19 survivors and 24 (1.9 %) NORM. Among the COVID-19 survivors, 13 (1.2 %) had taken TCM prior to infection, 60 (5.7 %) had taken pro-erectile medication, 19 (1.8 %) had taken both, and 10 (0.9 %) had taken other medications.
3.4. Factors associated with sexual outcomes
In the age-adjusted analysis, age ≥30 years, not in a marital relationship, rural resident, lower education level, manual workers, lower income, and shorter duration from recovery to survey date were significantly associated with decreased overall sexual functioning. Age ≥30 years, not in a marital relationship, rural resident, sedentary, lower education level, manual worker, lower income, not taking medications enhancing sexual function, not receiving three or more COVID-19 vaccine shots and shorter duration from recovery to survey date were significantly associated with lower sexual satisfaction (Table 4).
Table 4.
Association between BSFI outcomes (function domains, total BSFI score, and sexual satisfaction) and characteristics of COVID-19 survivors (n = 1,052) in China from February 4, 2023 to March 15, 2023, (A) age-adjusted and (B) multivariable linear regression models.
| Mean sum Sexual drive | Mean sum Erectile function | Mean sum Ejaculatory function | Mean sum Problem assessment | Total BSFI score (overall sexual functioning) | Sexual satisfaction | ||
|---|---|---|---|---|---|---|---|
| (A) Age-adjusted models | |||||||
| Age, years | |||||||
| 18–29 | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| 30–39 | −0.14[−0.26,−0.02] | −0.04[−0.15,0.08] | −0.22[−0.34,−0.09] | −0.20[−0.36,−0.03] | −1.41[−2.57,−0.25] | −0.18[−0.35,−0.01] | |
| 40–49 | −0.34[−0.47,−0.22] | −0.35[−0.48,−0.23] | −0.47[−0.6,−0.34] | −0.78[−0.95,−0.6] | −5.02[−6.23,−3.81] | −0.55[−0.73,−0.37] | |
| ≥50 | −0.53[−0.68,−0.37] | −0.50[−0.65,−0.34] | −0.70[−0.86,−0.53] | −0.89[−1.11,−0.67] | −6.60[−8.12,−5.07] | −0.58[−0.80,−0.35] | |
| BMIa | |||||||
| Underweight | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| Normal | −0.19[−0.48,0.09] | 0.16[−0.12,0.44] | 0.26[−0.03,0.56] | 0.15[−0.25,0.55] | 1.09[−1.69,3.86] | −0.06[−0.47,0.35] | |
| Overweight | −0.18[−0.48,0.11] | 0.22[−0.07,0.5] | 0.27[−0.03,0.57] | 0.20[−0.21,0.61] | 1.43[−1.41,4.26] | −0.04[−0.46,0.37] | |
| Obesity | −0.05[−0.37,0.26] | 0.32[0.01,0.63] | 0.37[0.04,0.70] | 0.38[−0.07,0.82] | 2.73[−0.35,5.80] | 0.02[−0.43,0.48] | |
| In a marital relationship | 0.10[−0.04, 0.24] | 0.18[0.05,0.32] | 0.11[−0.03,0.25] | 0.31[0.12,0.50] | 1.89[0.56,3.22] | 0.38[0.19,0.58] | |
| Rural resident | −0.28[−0.41,−0.16] | −0.3[−0.43,−0.18] | −0.29[−0.42,−0.16] | −0.44[−0.61,−0.26] | −3.37[−4.59,−2.15] | −0.25[−0.43,−0.07] | |
| Lifestyle behavior | |||||||
| Non-smoker | 0.06[−0.06,0.17] | 0.04[−0.07,0.15] | −0.05[−0.17,0.07] | −0.04[−0.20,0.12] | 0.01[−1.08,1.10] | 0.08[−0.08,0.24] | |
| Non-drinker | 0.03[−0.07,0.13] | 0.11[0.02,0.21] | 0.01[−0.09,0.11] | −0.01[−0.15,0.13] | 0.38[−0.56,1.32] | 0.12[−0.01,0.26] | |
| Sedentaryb | 0.04[−0.06,0.14] | −0.06[−0.15,0.04] | 0.01[−0.09,0.11] | −0.04[−0.17,0.10] | −0.18[−1.12,0.76] | −0.30[−0.43,−0.16] | |
| Highest academic degree | |||||||
| Junior middle school or lower | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| Senior middle school and technical secondary school | 0.70[0.34,1.07] | 0.66[0.31,1.01] | 0.51[0.13,0.89] | 0.68[0.17,1.18] | 6.44[2.94,9.94] | 0.86[0.35,1.38] | |
| Undergraduate and junior college | 0.90[0.58,1.22] | 0.82[0.51,1.13] | 0.62[0.29,0.95] | 1.04[0.59,1.48] | 8.60[5.53,11.67] | 1.15[0.69,1.60] | |
| Master or above | 0.93[0.61,1.25] | 0.93[0.61,1.24] | 0.72[0.39,1.06] | 1.24[0.79,1.69] | 9.82[6.71,12.93] | 1.27[0.81,1.73] | |
| Occupation | |||||||
| Workers and peasants | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| Students | 0.25[−0.02,0.52] | 0.52[0.26,0.78] | 0.68[0.40,0.95] | 1.09[0.72,1.47] | 6.71[4.14,9.28] | 0.68[0.3,1.06] | |
| Medical workers, teachers and civil servants | 0.39[0.15,0.62] | 0.68[0.46,0.91] | 0.68[0.44,0.92] | 1.13[0.80,1.45] | 7.57[5.34,9.81] | 1.01[0.68,1.34] | |
| Company clerks | 0.37[0.13,0.61] | 0.56[0.32,0.79] | 0.63[0.38,0.87] | 0.96[0.62,1.29] | 6.53[4.24,8.83] | 0.66[0.32,1.00] | |
| Managers and self-employed people | 0.22[−0.04,0.47] | 0.54[0.29,0.78] | 0.47[0.21,0.73] | 0.87[0.52,1.22] | 5.6[3.17,8.03] | 0.57[0.21,0.93] | |
| Retirees | 0.04[−0.51,0.6] | 0.27[−0.26,0.8] | 0.26[−0.3,0.82] | 0.59[−0.17,1.35] | 3.18[−2.07,8.44] | 0.96[0.19,1.73] | |
| Service trades and salespeople | 0.52[0.17,0.86] | 0.61[0.28,0.94] | 0.84[0.49,1.19] | 0.99[0.51,1.46] | 7.50[4.24,10.76] | 0.78[0.30,1.25] | |
| Freelancing and other professions | 0.43[0.16,0.70] | 0.41[0.15,0.67] | 0.53[0.26,0.81] | 0.86[0.49,1.23] | 5.74[3.19,8.29] | 0.71[0.33,1.08] | |
| Monthly income, CNY | |||||||
| No income | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| <2,000 | 0.25[−0.07,0.56] | 0.18[−0.12,0.48] | 0.16[−0.16,0.48] | 0.34[−0.10,0.78] | 2.38[−0.63,5.39] | 0.54[0.09,0.98] | |
| 2,000–3,999 | 0.06[−0.21,0.33] | −0.03[−0.23,0.29] | −0.33[−0.61,−0.05] | −0.15[−0.53,0.23] | −0.91[−3.53,1.71] | 0.29[−0.09,0.68] | |
| 4,000–6,999 | 0.20[−0.02,0.42] | 0.18[−0.04,0.40] | −0.06[−0.29,0.17] | −0.20[−0.51,0.11] | 0.22[−1.92,2.36] | 0.26[−0.06,0.58] | |
| ≥7,000 | 0.34[0.12,0.55] | 0.36[0.15,0.56] | 0.10[−0.12,0.31] | 0.12[−0.17,0.42] | 2.30[0.27,4.34] | 0.48[0.18,0.78] | |
| Medications to enhance sexual functionc | |||||||
| Pro-erectile medication | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| None | 0[−0.47,0.47] | −0.13[−0.59,0.33] | −0.02[−0.50,0.47] | −0.64[−1.29,0.02] | −2.33[−6.87,2.21] | −0.81[−1.46,−0.16] | |
| TCM | 0.20[−0.01,0.40] | 0.19[−0.01,0.39] | 0.24[0.03,0.45] | 0.37[0.08,0.65] | 2.53[0.55,4.51] | 0.62[0.33,0.9] | |
| Pro-erectile medication combines with TCM | 0.43[0.03,0.84] | −0.09[−0.49,0.30] | −0.29[−0.71,0.12] | 0.03[−0.53,0.59] | 0.09[−3.81,3.99] | 0.05[−0.51,0.61] | |
| Others | −0.23[−0.77,0.3] | −0.24[−0.76,0.28] | −0.51[−1.06,0.03] | −0.64[−1.38,0.10] | −4.13[−9.24,0.98] | −1.19[−1.92,−0.46] | |
| Number of vaccine shots receivedd | |||||||
| None | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| 1 | −0.16[−0.55,0.24] | −0.14[−0.53,0.24] | −0.34[−0.75,0.07] | −0.12[−0.67,0.43] | −1.78[−5.60,2.04] | 0.16[−0.40,0.72] | |
| 2 | 0.07[−0.19,0.34] | 0.15[−0.1,0.41] | 0.07[−0.20,0.34] | 0.31[−0.05,0.68] | 1.69[−0.84,4.22] | 0.34[−0.03,0.71] | |
| 3 | 0.10[−0.15,0.34] | 0.14[−0.10,0.38] | 0.06[−0.19,0.32] | 0.28[−0.07,0.62] | 1.56[−0.81,3.93] | 0.43[0.08,0.78] | |
| >3 | 0.07[−0.25,0.39] | 0.23[−0.08,0.54] | 0.18[−0.15,0.51] | 0.53[0.08,0.97] | 2.78[−0.29,5.84] | 0.66[0.21,1.11] | |
| Duration from recovery to survey datee, days | |||||||
| 30–59 | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| 60–89 | 0.09[−0.02,0.19] | 0.11[0.01,0.21] | 0.08[−0.03,0.19] | 0.22[0.07,0.37] | 1.32[0.31,2.33] | 0.06[−0.09,0.21] | |
| ≥90 | 0.50[0.37,0.62] | 0.37[0.25,0.5] | 0.26[0.13,0.39] | 0.67[0.5,0.85] | 4.64[3.43,5.85] | 0.70[0.52,0.87] | |
| |||||||
| Age, years | |||||||
| 18–29 | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| 30–39 | −0.17[−0.29,−0.04] | −0.08[−0.20,0.04] | −0.26[−0.39,−0.13] | −0.21[−0.38,−0.04] | −1.8[−2.99,−0.62] | −0.22[−0.41,−0.02] | |
| 40–49 | −0.31[−0.45,−0.17] | −0.38[−0.51,−0.24] | −0.5[−0.64,−0.36] | −0.74[−0.93,−0.55] | −5[−6.31,−3.69] | −0.55[−0.77,−0.33] | |
| ≥50 | −0.47[−0.65,−0.30] | −0.52[−0.69,−0.35] | −0.71[−0.89,−0.53] | −0.82[−1.06,−0.58] | −6.42[−8.06,−4.78] | −0.6[−0.87,−0.33] | |
| BMIa | |||||||
| Underweight | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| Normal | −0.19[−0.47,0.09] | 0.1[−0.28,0.48] | 0.87[−1.75,3.49] | ||||
| Overweight | −0.19[−0.48,0.09] | 0.1[−0.28,0.49] | 0.88[−1.80,3.55] | ||||
| Obesity | −0.02[−0.33,0.28] | 0.36[−0.06,0.78] | 2.79[−0.12,5.70] | ||||
| In a marital relationship | 0.14[−0.05,0.32] | ||||||
| Rural resident | −0.17[−0.3,−0.04] | −0.15[−0.27,−0.02] | −0.23[−0.36,−0.10] | −0.26[−0.43,−0.08] | −2.01[−3.21,−0.80] | ||
| Lifestyle behavior | |||||||
| No drinking | 0.10[0.01,0.19] | 0.12[−0.01,0.25] | |||||
| Sedentaryb | −0.23[−0.36,−0.1] | ||||||
| Highest academic degree | |||||||
| Junior middle school or lower | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| Senior middle school and technical secondary school | 0.52[0.15,0.89] | 0.40[0.04,0.76] | 0.22[−0.34,0.77] | 0.38[−0.13,0.88] | 3.93[0.43,7.43] | 0.58[0.09,1.08] | |
| Undergraduate and junior college | 0.74[0.4,1.070] | 0.47[0.15,0.80] | 0.75[0.41,1.10] | 0.65[0.19,1.10] | 5.38[2.24,8.52] | 0.82[0.37,1.26] | |
| Master or above | 0.80[0.45,1.14] | 0.56[0.23,0.90] | 0.46[0.19,0.73] | 0.75[0.27,1.22] | 6.14[2.87,9.40] | 0.87[0.41,1.33] | |
| Occupation | |||||||
| Workers and peasants | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| Students | 0.24[−0.08,0.55] | 0.62[0.31,0.93] | 0.25[−0.04,0.54] | 0.79[0.36,1.22] | 6.10[3.13,9.07] | 0.55[0.12,0.97] | |
| Medical workers, teachers and civil servants | 0.13[−0.1,0.37] | 0.49[0.26,0.72] | 0.22[−0.08,0.52] | 0.78[0.46,1.1] | 5.11[2.89,7.33] | 0.63[0.31,0.95] | |
| Company clerks | 0.17[−0.07,0.41] | 0.39[0.16,0.62] | 0.39[0.06,0.71] | 0.69[0.36,1.01] | 4.53[2.30,6.77] | 0.4[0.08,0.72] | |
| Managers and self-employed people | 0[−0.25,0.25] | 0.32[0.08,0.57] | 0.77[0.45,1.08] | 0.57[0.22,0.91] | 3.32[0.96,5.67] | 0.2[−0.14,0.54] | |
| Retirees | −0.07[−0.61,0.46] | 0.13[−0.39,0.65] | 0.56[0.32,0.80] | 0.36[−0.38,1.09] | 1.81[−3.25,6.86] | 0.49[−0.24,1.22] | |
| Service trades and salespeople | 0.37[0.04,0.69] | 0.5[0.18,0.82] | 0.49[0.25,0.74] | 0.83[0.38,1.28] | 6.21[3.1,9.31] | 0.48[0.04,0.93] | |
| Freelancing and other professions | 0.34[0.08,0.60] | 0.32[0.07,0.57] | 0.31[0.05,0.57] | 0.64[0.29,1.00] | 4.54[2.09,6.99] | 0.45[0.10,0.81] | |
| Monthly income, CNY | |||||||
| No income | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| <2,000 | 0.20[−0.10,0.50] | 0.13[−0.16,0.42] | 0.14[−0.18,0.45] | 0.27[−0.15,0.68] | 1.85[−1.00,4.70] | 0.41[0,0.82] | |
| 2,000–3,999 | 0.09[−0.18,0.35] | 0.11[−0.15,0.37] | −0.25[−0.53,0.03] | −0.1[−0.47,0.26] | −0.31[−2.83,2.22] | 0.26[−0.10,0.63] | |
| 4,000–6,999 | 0.24[−0.02,0.5] | 0.31[0.05,0.56] | 0.09[−0.18,0.36] | −0.13[−0.49,0.23] | 1.16[−1.32,3.63] | 0.26[−0.09,0.62] | |
| ≥7,000 | 0.33[0.07,0.59] | 0.43[0.18,0.68] | 0.24[−0.02,0.51] | 0.1[−0.25,0.46] | 2.71[0.27,5.14] | 0.41[0.06,0.76] | |
| Medications to enhance sexual functionc | |||||||
| Pro-erectile medication | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| None | −0.02[−0.47,0.44] | −0.06[−0.50,0.38] | 0.02[−0.46,0.50] | −0.61[−1.24,0.02] | −1.75[−6.09,2.59] | −0.72[−1.34,−0.10] | |
| TCM | 0.19[−0.01,0.39] | 0.22[0.03,0.41] | 0.28[0.07,0.48] | 0.38[0.11,0.65] | 2.72[0.86,4.59] | 0.64[0.38,0.91] | |
| Pro-erectile medication combines with TCM | 0.48[0.1,0.87] | −0.02[−0.4,0.36] | −0.24[−0.65,0.16] | 0.08[−0.45,0.61] | 0.56[−3.10,4.22] | 0.10[−0.42,0.63] | |
| Others | −0.30[−0.82,0.22] | −0.21[−0.71,0.3] | −0.45[−0.99,0.09] | −0.68[−1.39,0.03] | −4.15[−9.06,0.75] | −1.09[−1.79,−0.39] | |
| Duration from recovery to survey datee, daysf | |||||||
| 30–59 | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | 0 Ref. | |
| 60–89 | 0.07[−0.03,0.17] | 0.09[−0.01,0.19] | 0.06[−0.05,0.16] | 0.18[0.04,0.32] | 1.08[0.10,2.05] | 0.04[−0.10,0.18] | |
| ≥90 | 0.50[0.37,0.62] | 0.35[0.23,0.47] | 0.23[0.10,0.36] | 0.67[0.50,0.84] | 4.54[3.36,5.71] | 0.71[0.54,0.88] | |
Range score possible: sexual drive 0–4, erectile function 0–4, ejaculatory function 0–4, problem assessment 0–4, total BSFI score 0–40, sexual satisfaction 0–4.
Bold type indicating statistical significance (p value < 0.05).
Italic type indicating p value < 0.25.
Data are presented as unstandardized coefficient beta [95% Confidence Interval], unless otherwise specified.
BSFI Brief Sexual Function Inventory, COVID-19 coronavirus disease 2019, BMI body-mass index, CNY Chinese yuan, TCM Traditional Chinese medicine.
BMI classification is defined by Chinese cutoff points. Underweight: <18.5 kg/m2; Normal: 18.5–24 kg/m2; Overweight: 24–28 kg/m2; Obesity: ≥28 kg/m2.
Physical activity less than 150 min/week of moderate activity, or less than 75 min of strenuous activity.
Medications taken before infection with the novel coronavirus. Pro-erectile medication includes sildenafil or tadalafil as the main ingredient; TCM includes Wuzi Yanzong pill, Liuwei Dihuang pill, Shenqi Dihuang decoction and other formulas.
The COVID-19 vaccine.
Recovery was defined as the disappearance of symptoms of COVID-19 infection and negative nucleic acid test for two consecutive days.
Variables with p value ≤ 0.25 in the univariate analysis model of age adjustment were included into the multivariate model as independent variables, and a stepwise regression process was carried out.
In multivariate models, age ≥30 years, rural resident, lower education level, lower income, and shorter duration from recovery to survey date were associated with lower sexual drive. Age ≥30 years, rural resident, lower education level, manual worker, lower income, and shorter duration from recovery to survey date were significantly associated with decreased overall sexual functioning. Age ≥30 years, sedentary, lower education level, manual worker, lower income, not taking medications enhancing sexual function and shorter duration from recovery to survey date were significantly associated with lower sexual satisfaction (Table 4).
4. Discussion
This is the first study to compare sexual function between COVID-19 survivors and NORM during a pandemic after China government lifted strict lockdowns and loosened control measures. Some studies reported that during the COVID-19 pandemic, part of male adults have decreased sexual function (Fang et al., 2021, Pennanen-Iire et al., 2021). COVID-19 can cause erectile dysfunction (ED) through several factors, including endothelial dysfunction, prolonged hypoxia due to respiratory impairment, anxiety and depression, and endocrine disorders(Sansone et al., 2022), which has unique and detrimental effects on men's sexual health and erectile function (Hsieh et al., 2022, Sansone et al., 2021). These studies support our conclusion that COVID-19 has a significant impact on the sexual health of Chinese male adults. Effect sizes suggest that COVID-19 survivors may have worse sexual function compared with NORM. Of the COVID-19 survivors who participated in this survey, 16.92 % had overall sexual problems, with reduced sexual function and sexual satisfaction, compared to age-matched NORM.
Stratified by age, it was observed that Covid-19 impact on sexual function and sexual satisfaction increased from young to middle-aged, but decreased from middle-aged to elderly age group. Expectations of normal sexual function and sexual satisfaction may vary across different age groups (Capogrosso et al., 2019), probably one of the reasons contributing to the most striking differences between COVID-19 survivors and NORM in middle-aged group. In addition, younger COVID-19 survivors might have faster functional recovery before satisfaction was affected.
The associations found in the age-adjusted model reflect the interaction of multiple factors (social and physical) on sexual functioning, as also described in general population (McCabe et al., 2016, Mitchell et al., 2013). Manual workers who live in rural areas, with lower education levels and incomes, are more vulnerable to the pandemic impact socially and physically.
In the multivariate model, increasing age was significantly associated with lower sexual functioning, in line with earlier reports (Mitchell et al., 2013). In the elderly age group, decreased physical health, adverse effects of chronic diseases in the elderly, lower testosterone levels, and lack of a partner were found to be possible causes (McCabe et al., 2016).
Compared to infected individuals living in urban areas, overall sexual dysfunction was more pronounced among those living in rural areas. This could be explained by the relatively abundant medical resources available for COVID-19 treatment in urban areas (Li et al., 2022). During the pandemic period with medical resources constraints, urban residents had a higher chance of receiving medical support and drug treatment, which could relieve the symptoms caused by COVID-19 and even shorten the course of the illness, helping speed up recovery and reduce the negative impact on sexual function. Observational studies report that a lower education level influences the severity of COVID-19 in different populations (Hawkins et al., 2020, Niedzwiedz et al., 2020, Ribeiro et al., 2021). These studies support our conclusion that overall sexual dysfunction was more pronounced among those having a lower education level.
A three-month prospective observational follow-up study found that SARS-CoV-2 infection can cause persistent damage possibly due to pulmonary and/or extra-pulmonary diseases (Liang et al., 2020), and symptoms in a certain part of the population lasting for more than 12 weeks or even a year after the onset of the illness is classified as post-COVID-19 syndrome (Mehandru and Merad, 2022, Seeßle et al., 2022). Post-COVID-19 syndrome exhibits numerous complications involving virtually all systems in the human body that may impair erectile function through multiple pathogenic mechanisms (Sansone et al., 2022). Our results indicated that a respondent was more likely to suffer overall sexual dysfunction when it was closer in time from COVID-19 recovery. Sexual function was significantly improved in COVID-19 survivors whose recovery time was greater than three months. Currently, there is no evidence that SARS-CoV-2 causes persistent damage to sexual function.
Our study findings suggest that COVID-19 survivors who are sedentary report lower levels of sexual satisfaction compared to those who are physically active. However, sexual function was reported to be comparable between sedentary and physically active in COVID-19 survivor group. This is consistent with previous reports that inadequate physical activity is not associated with ED (Schimmer et al., 2001|). Sedentary survivors suffered a decline in sexual function that they believed more problematic compared with people who engage in regular exercise.
An interesting finding from our study is that among COVID-19 survivors who had taken medications to enhance sexual function prior to infection, those who took both TCM and pro-erectile medication showed less impact on their sexual drive compared to those who only took pro-erectile medication. However, there were no significant differences in terms of erectile and ejaculatory function. Among COVID-19 survivors who only took TCM, the majority were middle-aged (Capogrosso et al., 2019), and the decrease in sexual satisfaction may be related to their higher expectations after receiving TCM treatment. While TCM has been shown positive effects in preventing and treating COVID-19 (Xian et al., 2020, Zhao et al., 2021), it is still unknown whether it provides a certain extent of protection against reproductive system damage caused by COVID-19, which requires further investigation to clarify.
Currently, it is believed that COVID-19 affects male sexual function from multiple perspectives, including damaging male germ cells(Erbay et al., 2021), decreasing gonadal function (Ma et al., 2021), causing testicular inflammation (Xu et al., 2021), vascular damage (Sansone and Jannini, 2021) and mental health problems caused by the lockdown(Fang et al., 2021). Whether these effects are long-term or not remains unknown.
The BSFI is a validated tool with good psychometric properties. The use of the same tool for infected and uninfected participants is a significant advantage, particularly in research fields that utilize multiple assessment tools. When interpreting the results of this study, several limitations should be kept in mind. The number of uninfected participants was relatively small, partly due to the widespread occurrence of COVID-19 among Chinese males during the pandemic. This limitation is also a common issue in general population sexual behavior questionnaire studies. The outcomes of interest were based on patient-reported measurements, which may be influenced by recall difficulties (Bersvendsen et al., 2020). Online survey data collection resulted in a relatively smaller sample size of middle-aged and older individuals, leading to uncertainty in statistical analysis of effect sizes. Since the COVID-19 pandemic is still ongoing, the survey questionnaire had to be published online to reduce participants' exposure to the virus and better protect their privacy. Considering all the limitations mentioned above, our cross-sectional data-based findings do not represent the entire male population. Larger-scale studies are required to understand the impact of COVID-19 on male sexual function in the context of the current situation in China.
The significance of our research findings lies in the fact that during the new phase of the COVID-19 pandemic in China, although disease-related mortality rates were low, it was found that decreased sexual function and lower sexual satisfaction were associated with the infection. As the pandemic subsides, there may be a need to develop strategies for identifying long-term effects of the disease and providing additional healthcare support to fully address the impact of COVID-19 on male reproductive health.
5. Conclusion
Our research has found that sexual dysfunction is a concern for male COVID-19 survivors in China, while sexual function in the medical treatment of COVID-19 is an issue that can easily be overlooked. Therefore, doctors should closely monitor sexual function before, during, and after treatment to identify the sexual problems and their causes in COVID-19 survivors. By recognizing the importance of COVID-19 impact on male sexual function, we believe that more male COVID-19 survivors will have their sexual problems diagnosed, treated, and relieved potentially.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would especially thank the participants for sharing their time and experiences with us.
Funding
This work was supported by the National Natural Science Foundation of China (82174122).
Data availability
Data will be made available on request.
References
- Aleksanyan Y., Weinman J.P. Women, men and COVID-19. Soc Sci Med. 2022;294:114698. doi: 10.1016/j.socscimed.2022.114698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach J.M., Khera M. Testosterone's Role in COVID-19. J Sex Med. 2021;18(5):843–848. doi: 10.1016/j.jsxm.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bersvendsen H.S., Haugnes H.S., Dahl A.A., Fagerli U.-M., Fluge Ø., Holte H., Seland M., Wilsgaard T., Smeland K.B., Kiserud C.E. Sexual function in long-term male lymphoma survivors after high-dose therapy with autologous stem-cell transplantation. Bone Marrow Transplant. 2020;55(5):891–905. doi: 10.1038/s41409-019-0745-4. [DOI] [PubMed] [Google Scholar]
- Best J.C., Kuchakulla M., Khodamoradi K., Lima T.F.N., Frech F.S., Achua J., Rosete O., Mora B., Arora H., Ibrahim E., Ramasamy R. Evaluation of SARS-CoV-2 in Human Semen and Effect on Total Sperm Number: A Prospective Observational Study. World J Mens Health. 2021;39(3):489. doi: 10.5534/wjmh.200192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capogrosso P, Ventimiglia E, Boeri L, et al. Should We Tailor the Clinical Management of Erectile Dysfunction According to Different Ages. J Sex Med. 2019u. 16(7): 999-1004. [DOI] [PubMed]
- Dahl A.A., Bremnes R., Dahl O., Klepp O., Wist E., Fosså S.D. Is the sexual function compromised in long-term testicular cancer survivors. Eur Urol. 2007;52(5):1438–1447. doi: 10.1016/j.eururo.2007.02.046. [DOI] [PubMed] [Google Scholar]
- Dubin J.M., Bennett N.E., Halpern J.A. The adverse impact of COVID-19 on men's health. Curr Opin Urol. 2022;32(2):146–151. doi: 10.1097/MOU.0000000000000966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erbay G., Sanli A., Turel H., Yavuz U., Erdogan A., Karabakan M., Yaris M., Gultekin M.H. Short-term effects of COVID-19 on semen parameters: A multicenter study of 69 cases. Andrology. 2021;9(4):1060–1065. doi: 10.1111/andr.13019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang D, Peng J, Liao S, et al. An Online Questionnaire Survey on the Sexual Life and Sexual Function of Chinese Adult Men During the Coronavirus Disease 2019 Epidemic. Sex Med. 2021j. 9(1): 100293. [DOI] [PMC free article] [PubMed]
- Gupta A., Madhavan M.V., Sehgal K., Nair N., Mahajan S., Sehrawat T.S., Bikdeli B., Ahluwalia N., Ausiello J.C., Wan E.Y., Freedberg D.E., Kirtane A.J., Parikh S.A., Maurer M.S., Nordvig A.S., Accili D., Bathon J.M., Mohan S., Bauer K.A., Leon M.B., Krumholz H.M., Uriel N., Mehra M.R., Elkind M.S.V., Stone G.W., Schwartz A., Ho D.D., Bilezikian J.P., Landry D.W. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26(7):1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins R.B., Charles E.J., Mehaffey J.H. Socio-economic status and COVID-19-related cases and fatalities. Public Health. 2020;189:129–134. doi: 10.1016/j.puhe.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh T.C., Edwards N.C., Bhattacharyya S.K., Nitschelm K.D., Burnett A.L. The Epidemic of COVID-19-Related Erectile Dysfunction: A Scoping Review and Health Care Perspective. Sex Med Rev. 2022;10(2):286–310. doi: 10.1016/j.sxmr.2021.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Y., Xu S. Comprehensive overview of COVID-19 based on current evidence. Dermatol Ther. 2020;33(5):e13525. doi: 10.1111/dth.13525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kresch E., Achua J., Saltzman R., Khodamoradi K., Arora H., Ibrahim E., Kryvenko O.N., Almeida V.W., Firdaus F., Hare J.M., Ramasamy R. COVID-19 Endothelial Dysfunction Can Cause Erectile Dysfunction: Histopathological, Immunohistochemical, and Ultrastructural Study of the Human Penis. World J Mens Health. 2021;39(3):466. doi: 10.5534/wjmh.210055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Li G, Xin C, Wang Y, Yang S. Challenges in the Practice of Sexual Medicine in the Time of COVID-19 in China. J Sex Med. 2020k. 17(7). 1225-1228. [DOI] [PMC free article] [PubMed]
- Li J., Zhao N., Zhang H., Yang H., Yang J. Roles and Challenges for Village Doctors in COVID-19 Pandemic Prevention and Control in Rural Beijing, China: A Qualitative Study. Front Public Health. 2022;10 doi: 10.3389/fpubh.2022.888374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang L., Yang B., Jiang N., Fu W., He X., Zhou Y., Ma W.-L., Wang X. Three-month Follow-up Study of Survivors of Coronavirus Disease 2019 after Discharge. J Korean Med Sci. 2020;35(47):e418. doi: 10.3346/jkms.2020.35.e418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L., Xie W., Li D., Shi L., Ye G., Mao Y., Xiong Y., Sun H., Zheng F., Chen Z., Qin J., Lyu J., Zhang Y., Zhang M. Evaluation of sex-related hormones and semen characteristics in reproductive-aged male COVID-19 patients. J Med Virol. 2021;93(1):456–462. doi: 10.1002/jmv.26259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe M.P., Sharlip I.D., Lewis R., Atalla E., Balon R., Fisher A.D., Laumann E., Lee S.W., Segraves R.T. Risk Factors for Sexual Dysfunction Among Women and Men: A Consensus Statement From the Fourth International Consultation on Sexual Medicine 2015. J Sex Med. 2016;13(2):153–167. doi: 10.1016/j.jsxm.2015.12.015. [DOI] [PubMed] [Google Scholar]
- Mehandru S., Merad M. Pathological sequelae of long-haul COVID. Nat Immunol. 2022;23(2):194–202. doi: 10.1038/s41590-021-01104-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell K.R., Mercer C.H., Ploubidis G.B., Jones K.G., Datta J., Field N., Copas A.J., Tanton C., Erens B., Sonnenberg P., Clifton S., Macdowall W., Phelps A., Johnson A.M., Wellings K. Sexual function in Britain: findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3) Lancet. 2013;382(9907):1817–1829. doi: 10.1016/S0140-6736(13)62366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nassau D.E., Best J.C., Kresch E., Gonzalez D.C., Khodamoradi K., Ramasamy R. Impact of the SARS-CoV-2 virus on male reproductive health. BJU Int. 2022;129(2):143–150. doi: 10.1111/bju.15573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niedzwiedz C.L., O'Donnell C.A., Jani B.D., Demou E., Ho F.K., Celis-Morales C., Nicholl B.I., Mair F.S., Welsh P., Sattar N., Pell J.P., Katikireddi S.V. Ethnic and socioeconomic differences in SARS-CoV-2 infection: prospective cohort study using UK Biobank. BMC Med. 2020;18:160. doi: 10.1186/s12916-020-01640-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okwan-Duodu D., Lim E.C., You S., Engman D.M. TMPRSS2 activity may mediate sex differences in COVID-19 severity. Signal Transduct Target Ther. 2021;6(1):100. doi: 10.1038/s41392-021-00513-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Leary M.P., Fowler F.J., Lenderking W.R., Barber B., Sagnier P.P., Guess H.A., Barry M.J. A brief male sexual function inventory for urology. Urology. 1995;46(5):697–706. doi: 10.1016/S0090-4295(99)80304-5. [DOI] [PubMed] [Google Scholar]
- Pennanen-Iire C., Prereira-Lourenço M., Padoa A., Ribeirinho A., Samico A., Gressler M., Jatoi N.-A., Mehrad M., Girard A. Sexual Health Implications of COVID-19 Pandemic. Sex Med Rev. 2021;9(1):3–14. doi: 10.1016/j.sxmr.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pijls B.G., Jolani S., Atherley A., Derckx R.T., Dijkstra J.I.R., Franssen G.H.L., Hendriks S., Richters A., Venemans-Jellema A., Zalpuri S., Zeegers M.P. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: a meta-analysis of 59 studies. BMJ Open. 2021;11(1):e044640. doi: 10.1136/bmjopen-2020-044640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro K.B., Ribeiro A.F., Veras M., de Castro M.C. Social inequalities and COVID-19 mortality in the city of São Paulo, Brazil. Int J Epidemiol. 2021;50:732–742. doi: 10.1093/ije/dyab022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansone A., Jannini E.A. COVID-19 and Erectile Dysfunction: Endothelial Dysfunction and Beyond. World J Mens. Health. 2021;39(4):820–821. doi: 10.5534/wjmh.210081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansone A., Mollaioli D., Ciocca G., Colonnello E., Limoncin E., Balercia G., Jannini E.A. “Mask up to keep it up”: Preliminary evidence of the association between erectile dysfunction and COVID-19. Andrology. 2021;9(4):1053–1059. doi: 10.1111/andr.13003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansone A., Mollaioli D., Limoncin E., Ciocca G., Bắc N.H., Cao T.N., Hou G., Yuan J., Zitzmann M., Giraldi A., Jannini E.A. The Sexual Long COVID (SLC): Erectile Dysfunction as a Biomarker of Systemic Complications for COVID-19 Long Haulers. Sex Med Rev. 2022;10(2):271–285. doi: 10.1016/j.sxmr.2021.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schimmer A.D., Ali V., Stewart A.K., Imrie K., Keating A. Male sexual function after autologous blood or marrow transplantation. Biol Blood Marrow Transplant. 2001;7(5):279–283. doi: 10.1053/bbmt.2001.v7.pm11400950. [DOI] [PubMed] [Google Scholar]
- Schober P., Mascha E.J., Vetter T.R. Statistics From A (Agreement) to Z (z Score): A Guide to Interpreting Common Measures of Association, Agreement, Diagnostic Accuracy, Effect Size, Heterogeneity, and Reliability in Medical Research. Anesth Analg. 2021;133(6):1633–1641. doi: 10.1213/ANE.0000000000005773. [DOI] [PubMed] [Google Scholar]
- Seeßle J, Waterboer T, Hippchen T, et al. Persistent Symptoms in Adult Patients 1 Year After Coronavirus Disease 2019 (COVID-19): A Prospective Cohort Study. Clin Infect Dis. 2022{. 74(7). 1191-1198. [DOI] [PMC free article] [PubMed]
- Wang L., Zhou B., Zhao Z., Yang L., Zhang M., Jiang Y., Li Y., Zhou M., Wang L., Huang Z., Zhang X., Zhao L., Yu D., Li C., Ezzati M., Chen Z., Wu J., Ding G., Li X. Body-mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004–18. Lancet. 2021;398(10294):53–63. doi: 10.1016/S0140-6736(21)00798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A. Men and COVID-19: the aftermath. Postgrad Med. 2020;132(sup4):18–27. doi: 10.1080/00325481.2020.1823760. [DOI] [PubMed] [Google Scholar]
- Xian Y., Zhang J., Bian Z., Zhou H., Zhang Z., Lin Z., Xu H. Bioactive natural compounds against human coronaviruses: a review and perspective. Acta Pharm Sin b. 2020;10(7):1163–1174. doi: 10.1016/j.apsb.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H., Wang Z., Feng C., Yu W., Chen Y., Zeng X., Liu C. Effects of SARS-CoV-2 infection on male sex-related hormones in recovering patients. Andrology. 2021;9(1):107–114. doi: 10.1111/andr.12942. [DOI] [PubMed] [Google Scholar]
- Zhao Z., Li Y., Zhou L., Zhou X., Xie B., Zhang W., Sun J. Prevention and treatment of COVID-19 using Traditional Chinese Medicine: A review. Phytomedicine. 2021;85:153308. doi: 10.1016/j.phymed.2020.153308. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.