Pediatric and adult beating heart simulator.
Central Message.
The development of a low-cost beating heart simulator may broaden access to cardiac surgery training.
Perspective.
A beating heart simulator with high-fidelity beating heart simulations was developed at a lower cost compared to simulators currently on the market. This simulator reproduces systole, unlike other simulators that merely inflate and deflate pig hearts.
Pediatric and adult cardiac surgery specialties have specifics that are not shared with other surgical specialties (Videos 1 and 2). Many of these are difficult to learn due to their rarity, the length of training programs, and other essential factors, such as working hour regulations. Therefore, beating heart simulator–based training is an alternative pathway for advancing surgical training for the next generation of cardiac surgeons and increasing their exposure to rare and more complex surgical cases in a patient-safe environment. A beating heart simulator has been developed to reproduce systole and diastole using porcine heart-lung complexes and inexpensive parts to offer a low-cost simulator option for cardiac training (Figures 1 and 2).
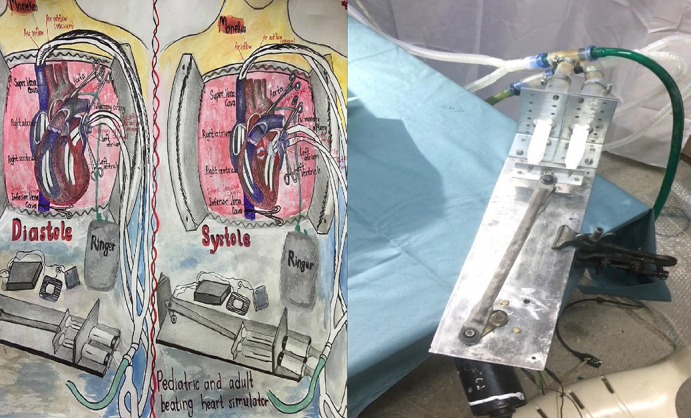
Figure 1.
Pediatric and adult beating heart simulator.
Figure 2.

Pediatric and adult beating heart simulator (winshield wiper mechanism, syringes, one-way valves, and tubes).
Background
A web search to identify different cardiac surgical simulators revealed only a few options. One challenge is the difficulty in developing a high-fidelity cardiac surgical simulator that can be incorporated into cardiac surgical training at a low cost to allow its widespread use.
All high-fidelity simulators have one thing in common: they can reproduce a real-case scenario. High-fidelity surgical scenarios can be achieved through the use of live tissue, as there currently is no available material that accurately represents living tissue. Artificial organs used in simulations are far from actual tissues. Even 3-dimensional printing is insufficient at producing artificial organs that can substitute for living tissues in high-fidelity simulations. Although artificial tissues can be used early in resident training, they are not applicable for more advanced training because they simply do not feel real when handling, dissecting, suturing, or moving. While remaining a good choice for simple demonstrations of surgical case scenarios, artificial tissues should not be used for surgical resident/fellow training.
One difference between operations performed on a beating heart simulator and operations performed on a porcine heart-lung complex without using a simulator is the high fidelity of the simulations. For example, one can place a purse-string suture on a standstill porcine heart atrium, but the experience differs from placing a purse-string on a beating heart simulator when the atrium and the whole heart are rapidly moving. The most crucial advantage of beating heart simulators is that they create a realistic environment for such procedures as placing purse-strings and cannulation on a beating heart, starting cardiopulmonary bypass, performing off-pump coronary artery bypass grafting (CABG), performing lung transplantation, and other procedures.
Some research papers have suggested that cardiothoracic surgical trainees are not allowed to perform complex cardiac surgical cases in adult and pediatric patients. Therefore, in the US, after completing classical cardiac surgical training, fellows continue their training in a super fellowship (non–ACGME-accredited fellowship programs in the US or a similar position as a trainee outside the US) to broaden their operative experience.1,2 Even after that, exposure to complex cases continues in an apprenticeship model. For example, many trainees in the US do not regularly perform aortic cases, mitral valve cases, and other complex cardiac surgical cases. Similarly, it is rare to see a fellow perform the most complex pediatric cardiac surgical cases as an operating surgeon, influencing the trainees' future independent practice. In most cases, both pediatric and adult cardiac surgery fellowship graduates work as junior cardiac surgeons after joining groups of cardiac surgeons and continue their training under the guidance and mentorship of more experienced surgeons. For example, an arterial switch operation for transposition of great arteries is considered a complex procedure, and fellows are often forbidden from performing this procedure as an operating surgeon. However, with a low-cost beating heart simulator, the steps of the switch operation (eg, coronary artery reimplantation) can be reproduced on the simulator. Coronary artery reimplantation is the most critical step during this complicated procedure, and it can be simulated on a simulator in a patient-safe environment until a fellow feels comfortable doing it, providing a maximally safe environment for the patient.
Ultimately, repetition is an integral part of surgical training. Beating heart simulator–based training can provide a limitless number of repetitions. Adding simulator-based training to cardiac surgical training may improve the quality of the training and help produce more qualified cardiac surgeons, especially for rare surgical cases performed mainly by attending surgeons during the fellowship/residency. Fellows can perform such surgeries on a simulator repeatedly until they feel comfortable and only then transfer that knowledge/skill set to an actual patient. This strategy would decrease the number of surgical mistakes made by residents/fellows, improving the results for patients and the entire team. Conditions are worse outside the US, where surgical and cardiac surgical training is considered to be more hands-on with more autonomy.3 Outside the US, surgical/cardiac surgical training is less hands-on with less autonomy; therefore, beating heart simulator–based training could solve this global problem, potentially leading to more qualified cardiac surgical graduates worldwide.
Methods
Previous research on simulation-based cardiac surgical training has been conducted. The simulator training took place at 8 thoracic surgical residency programs, the Cardiac Surgery Simulation Consortium was formed, and a curriculum was produced, which is available on the website of the Thoracic Surgery Directors Association (TSDA). Under an Agency for Healthcare Research and Quality grant (R18HS020451), the Consortium created a 39-session curriculum to assess whether a simulator curriculum could possibly improve resident training and thereby contribute to surgical patient safety.4 Training modules using the Ramphal simulator were created covering cardiopulmonary bypass, CABG, aortic valve replacement, massive air embolism, acute intraoperative aortic dissection, and sudden deterioration in cardiac function. Twenty-seven residents participated in this simulator cardiac surgical training using the curriculum and modules provided by the Consortium. The residents demonstrated improvement with practice repetitions that resulted in excellent final scores for each module. The aforementioned study concluded that overall performance in component tasks and complete surgical procedures improved during simulation-based training, and that simulation-based training provides the necessary skill set for managing adverse events and can help produce safer surgeons.4, 5
To be most useful in training, high-fidelity simulators should recreate the natural movements of the heart—systole, diastole, contraction, and relaxation—while having the properties of real organs. Existing commercial cardiac surgical simulators have challenges in meeting these needs.
There are 2 commercially available cardiac surgical simulators: the Ramphal6 simulator, now produced by KindHeart, and a simulator produced by the Chamberlain Group. The KindHeart simulator uses porcine hearts from vendors and butchers, and no animals are sacrificed explicitly for simulation purposes. Both simulators recreate cardiac activity. The Ramphal simulator uses inflatable balloons placed into the ventricles that simulate systole and diastole. However, the cardiac activity does not appear realistic because when the balloon inflates, the heart is stimulated to go into the diastolic phase, and thus the heart size increases. When the balloons then deflate, the heart returns to its starting size, whereas a real heart contracts noticeably during systole, and heart size decreases.
The Ramphal simulator has no contraction component; it only inflates and deflates. It is a great simulator, but the contractions do not appear natural. The Chamberlain simulator uses an artificial heart made from synthetic material unsuitable for high-fidelity simulations and training. One problem is the high cost of these simulators, and most cardiac surgical departments cannot purchase them. Thus, they have limited implementation. Both simulators have value, but there is a need for a high-fidelity and low-cost cardiac surgical training simulator.
Results
To overcome the challenges exhibited by the commercial models, pediatric and adult beating heart simulators were invented in a home garage using car parts and other low-cost items. The result was a realistic beating heart ready for any cardiac surgical procedure or complication simulation. The simulator has different speeds, and different heart rhythms can be reproduced. It also can be connected to a PC via different computer programs. Real-time cardiovascular monitoring also can be provided. Any pediatric or adult cardiac surgical procedure and its complications can be simulated using specifically written scenarios.
No other pediatric or adult beating heart simulators are currently available that offer such realistic presentations, and there is no information regarding pediatric beating heart simulators that use porcine hearts. Our pediatric version of the simulator will be the first yet reported to use porcine hearts. It uses a specially designed and manufactured mechanism that leads to systole and diastole, with a noticeable myocardial contraction; it also uses real live tissue purchased from butchers.
This low-cost simulator uses old car parts, simple electrical parts, tubing, valves, and other low-cost items (Figures 2 and 3). Because the simulator has no complicated mechanical or electrical parts, it is practical and potentially broadly applicable. The simulator prototype uses air pressure to inflate the atriums and the ventricles, simulating diastole, and a vacuum to deflate the atria and the ventricles to the neutral position of the cadaveric heart. These structures then move beyond the neutral position to recreate a ventricular contraction. Thus, the system needs a source of pressurized air to inflate and a vacuum to forcefully deflate the heart chambers, which is achieved via medical syringes. The air moves in and out of the heart via tubing, and the tubes are placed in the right and left ventricles. There are 4 main tubing elements, including 2 elements for inflation and 2 for deflation. Two pipes are placed into the ventricle, one to inflate the heart and the other to deflate the heart, simulating diastole and systole. A car wiper motor is used to move the syringe plunger. Because the original motor was relatively weak and overheated rapidly, a more durable version was developed. The electrical supply is 110V and 220V inputs tuned to 6 to 12V for the wiper motor. The control panel can regulate the voltage and thus the speed and force of the wiper motor to simulate faster or slower heartbeats. The simulator also has a one-way valve system such that when the syringe is depressed, the valve opens on one side and closes on the other side so that the air escapes from the syringe inflating the heart chambers. When the syringe comes out, the outflow valve opens and the inflow valve closes, leading to withdrawal of air and creation of a vacuum in the heart chambers. This action leads to perfect systole and diastole (Figure 4, Figure 5, Figure 6, Figure 7).
Figure 3.

Syringes with one-way valves and tubes.
Figure 4.

Pediatric beating heart simulator, diastole.
Figure 5.
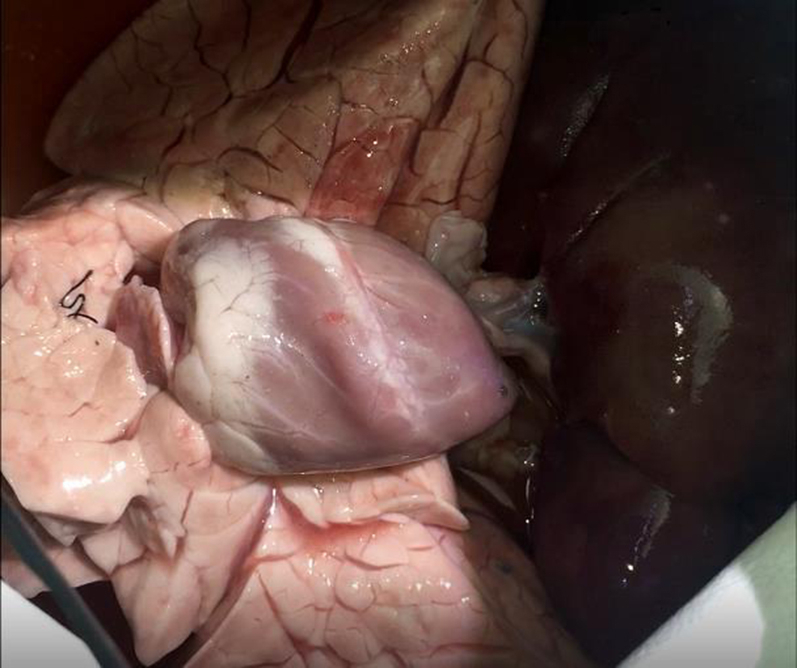
Pediatric beating heart simulator, systole.
Figure 6.

Adult beating heart simulator, diastole.
Figure 7.

Adult beating heart simulator, systole
The simulation experiments used varying inflation and deflation pressures. Inflation with greater air pressure caused the diastolic phase to appear more rapid; the same applied to air deflation, with the greater vacuum and volume of air deflated, the more rapid the systolic phase and the more forceful the contraction. However, if weaker and slower contractions are required, such as when coming out of cardiopulmonary bypass and noticing the first heart contractions, the inflation pressure, amount of inflated air, vacuum, and amount of deflated air all can be decreased. Although wall tension is not measured, this could be done in the future to obtain more information on physiology. Simulated systolic and diastolic timing could vary depending on the speed the simulator is set at. If the motor's speed (in this case, a windshield wiper motor) is increased, the mechanism moves faster, decreasing the time to inflate and then deflate the heart chambers, which disrupts systolic and diastolic timing. Besides size, there are several specific differences between adult and pediatric cardiac surgical simulations. The mechanism used is the same; however, for the pediatric simulations, smaller diameter tubing is used, less inflated air is needed, and less vacuum force for air suction is needed.
Some specific challenges arose while building this simulator. During diastole, the air can escape from the heart through the aortic and pulmonary valves. This was prevented via retrograde simulated blood flow into the aorta and pulmonary artery, which closes the aortic and pulmonary valves and simulates aortic and pulmonary artery blood flows. This simulated blood flow is very important if the simulator has an aortic cannulation component. Having a pressurized aorta with artificial blood makes aortic work possible, allowing realistic procedures like purse-string placement and canulation. Air leakage from the superior or inferior vena cava is prevented by isolating these veins from the right atrium via an internal plug or clamping them.
In addition, during the current simulation runs scenarios, there was no pressure feedback; however, when the simulator is modified and connected to a computer via an Arduino microcontroller, it will be possible to simulate the vital signs or different cardiac rhythms. For example, in the event of sudden deterioration of cardiac function, it will be possible to simulate the actual heart behavior and vital signs related to this condition. It was also determined that more vacuum force is needed for the left ventricle to simulate systolic contraction and less vacuum force is needed for the right ventricle; therefore, a stronger vacuum source, and probably larger syringes, will be used in the future.
It takes only a short time to prepare for a simulation. The simulator is assembled with all the lines and valves, the retrograde perfusion system, the computer, and the mannequin chest part ready to introduce the heart-lung complex. Then the simulator lines (inflation and deflation lines) are introduced into the heart through the posterior side of the left atrium into the left ventricle and through the superior or inferior vena cava into the right ventricle. In addition, 2 retrogradely perfused lines are placed into the aorta and pulmonary artery. Preparation for the simulation should take less than 30 minutes and can be done by one person.
Because this simulator is meant to be low-cost, where porcine hearts are procured is also important. Costs of porcine hearts, lungs, and heart-lung complexes vary depending on country. Although fresh porcine hearts are available from multiple online vendors that specialize in supplying living tissues for training purposes and can provide certification regarding the absence of animal-borne diseases (often necessary if one is planning to bring living animal tissues to the hospital), these can be costly, whereas porcine organs purchased from a butcher might not be. The easiest way to preserve organs and keep them reusable for a more significant number of residents and fellows to practice on the simulator on multiple occasions is to wash porcine hearts or other parts, like heart-lung complexes, in soapy water and then refrigerate or freeze them until they are needed.
Discussion
It is hypothesized that this simulator model can be used for adult and pediatric cardiac surgery training, especially in institutions with a low caseload or difficulty providing adequate autonomy to residents as operating surgeons while maintaining a low cost of simulations and a patient-safe training environment. Cardiac surgery trainees may be dissatisfied with their operative experience.7 One reason for this could be insufficient time during training for exposure to all types of surgical cases. Autonomy may vary based on the training site. Use of a simulator allows training in critical parts of the surgical procedures in a patient-safe environment. For example, coronary artery reimplantation during the arterial switch operation for the transposition of the great arteries can be reproduced. The same applies to any pediatric or adult cardiac surgical procedure that requires a high repetition volume to achieve excellence. Learning surgical skills ultimately requires repetition, which is currently deficient due to work hour regulations, less hands-on training, and decreased autonomy. The incorporation of simulator-based training in residency/fellowship programs on a regular basis may lead to more competent cardiac surgical residency graduates, which will positively affect cardiac surgical outcomes.
This simulator offers an opportunity to work on internal parts of the heart, such as valves, cords, and myocardium. Any known cardiac surgical procedure can be performed; for example a CABG procedure becomes super high-fidelity because the coronary arteries are perfused retrogradely through the aorta via the simulator's retrograde aortic perfusion system. Perfusion in this simulator uses a simple i.v. perfusion system, the same system used for pulmonary artery retrograde perfusion. This simulator has no extra high-cost components, which makes it broadly applicable. The same simulator airflow system can be used for inhalation and exhalation to achieve maximal fidelity of the procedures with the lungs moving, inflating, and deflating. This may be an important addition for cases that do not involve respiratory arrest, such as off-pump CABG. All these features make this simulator an excellent candidate for trainees.
Once it was built, the simulator was used to perform several procedures to access and demonstrate its effectiveness. Two individuals performed the procedures. The procedures performed using an adult model were blood vessel dissection using electrocautery and scissors while using the beating heart simulator, aortic and atrial purse-string suturing and subsequent cannulation (with the aorta and pulmonary artery retrogradely perfused with artificial blood), and off-pump CABG. Procedures performed using a pediatric model include blood vessel dissection using electrocautery, scissors while using the beating heart simulator, aortic and atrial purse-string suturing, and subsequent cannulation, with the aorta and pulmonary artery retrogradely perfused with artificial blood. The simulator is appropriate for both intracardiac and epicardial procedures/repairs.
The simulator has yet to be applied to a broader audience. The next step will be an application of the simulator to a broader audience of pediatric and adult cardiac surgical residents, fellows, attending, and medical students interested in cardiac surgery. Hopefully, the final results will demonstrate the effectiveness of this low-cost beating heart simulator in allowing cardiac surgeons practice in a patient safe environment, impacting cardiac training for the next generation.
Footnotes
Disclosures: The author reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Supplementary Data
Adult beating heart simulator video. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00215-8/fulltext.
Pediatric beating heart simulator video. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00215-8/fulltext.
References
- 1.Bergquist C.S., Brescia A.A., Watt T.M.F., Pienta M.J., Bolling S.F. Super fellowships among cardiothoracic trainees: prevalence and motivations. Ann Thorac Surg. 2021;111:1724–1729. doi: 10.1016/j.athoracsur.2020.05.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stoica S.C., Campbell D.N. Results of consecutive training procedures in pediatric cardiac surgery. J Cardiothorac Surg. 2010;5:105. doi: 10.1186/1749-8090-5-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah A.M., Siddiqui E., Holmes S.D., Okoh A., Abdullah M., Deatrick K., et al. Trends in the traditional cardiothoracic surgery resident operative experience for cardiac cases: an analysis of Accreditation Council for Graduate Medical Education case logs. J Thorac Cardiovasc Surg. 2021;161:1064–1075. doi: 10.1016/j.jtcvs.2020.11.168. [DOI] [PubMed] [Google Scholar]
- 4.Feins R.H., Burkhart H.M., Conte J.V., Coore D.N., Fann J.I., Hicks G.L., et al. Simulation-based training in cardiac surgery. Ann Thorac Surg. 2017;103:312–321. doi: 10.1016/j.athoracsur.2016.06.062. [DOI] [PubMed] [Google Scholar]
- 5.Mokadam N.A., Fann J.I., Hicks G.L., Nesbitt J.C., Burkhart H.M., Conte J.V., et al. Experience with the cardiac surgery simulation curriculum: results of the resident and faculty survey. Ann Thorac Surg. 2017;103:322–328. doi: 10.1016/j.athoracsur.2016.06.074. [DOI] [PubMed] [Google Scholar]
- 6.Ramphal P.S., Coore D.N., Craven M.P. A high fidelity tissue-based cardiac surgical simulator. Eur J Cardio Thorac Surg. 2005;27:910–916. doi: 10.1016/j.ejcts.2004.12.049. [DOI] [PubMed] [Google Scholar]
- 7.Cerqueria R.J., Heuts S., Gollmann-Tepeköylü C., Syrjälä S.O., Keijzers M., Zientara A., et al. Challenges and satisfaction in cardiothoracic surgery residency programmes: insights from a Europe-wide survey. Interact Cardiovasc Thorac Surg. 2021;23:167–173. doi: 10.1093/icvts/ivaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Adult beating heart simulator video. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00215-8/fulltext.
Pediatric beating heart simulator video. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00215-8/fulltext.



