A dual-lumen, percutaneous RVAD cannula placed via the RIJ versus left subclavian vein.
Central Message.
The dual-lumen percutaneous RVAD cannula can be safely placed via the left subclavian vein under fluoroscopic guidance as an alternative to the RIJ site.
Increased single-site venovenous (VV) extracorporeal membrane oxygenation (ECMO) use promotes awake, mobilized patients. The internal jugular vein is a safe, established site for dual-lumen ECMO cannula insertion with image guidance.1 Left internal jugular (LIJ) and left subclavian veins are alternative cannulation sites when the right internal jugular (RIJ) vein is inaccessible.2,3
During the COVID-19 pandemic, patients on VV ECMO experienced refractory cor pulmonale unresponsive to medical treatment.4 The Protek Duo (TandemLife) offers percutaneous right ventricular assist device (RVAD) support. Designed for RIJ placement, it assists patients until recovery or lung transplant by draining blood from the right atrium and returning it to the PA when connected to an ECMO circuit. An oxygenator is added for gas exchange. Previously, limited options existed for percutaneous, single-site RVAD placement when the RIJ vein was inaccessible.
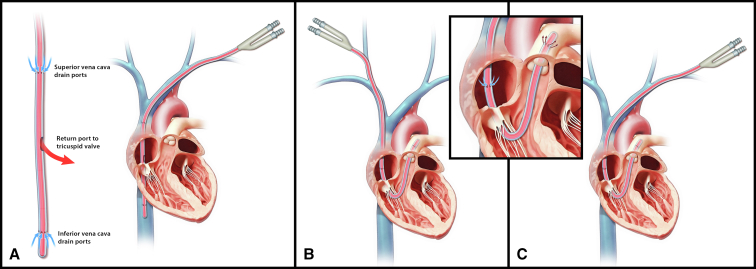
We present the use of the left subclavian vein as an alternative site for percutaneous dual-lumen cannula placement, connecting the right atrium to the pulmonary artery (PA), as part of an RVAD used to bridge a patient to lung transplant (Figure 1).
Figure 1.
A, Dual-lumen, bicaval, VV ECMO cannula percutaneously placed in the left subclavian vein. B, Dual-lumen, right atrial to PA cannula percutaneously placed in the standard position: RIJ vein, as part of an RVAD. C, Dual-lumen, right atrial to PA cannula percutaneously placed in the left subclavian vein, as part of an RVAD.
Materials and Methods
Institutional Review Board approval and written consent from patients were obtained for publication of this surgical technique (STUDY00004012, 04/02/2022).
Case Description
A 52-year-old man developed severe COVID-19–related acute respiratory distress syndrome. On day 5, he was remotely cannulated for VV ECMO using a right femoral vein multistage drainage cannula and a short single-stage, RIJ vein oxygenated return cannula, and transported to our ECMO center.
The patient's lung injury persisted, resulting in significant parenchymal destruction and refractory hypoxemia episodes. After 6 weeks, he developed COVID-19–related group 3 pulmonary hypertension, leading to right heart failure due to extensive pulmonary vasculature scarring.
To support the failing right ventricle, the patient was transitioned to a fluoroscopically guided RIJ percutaneous RVAD with an oxygenator using a Protek Duo. After 4 months of rehabilitation, the patient met institutional lung transplant criteria. However, he developed significant skin breakdown at the RIJ site resulting in bleeding and ongoing transfusion requirements. Concurrently, he had persistent multidrug-resident Klebsiella bacteremia. This prompted relocation of his cannula.
Surgical Technique
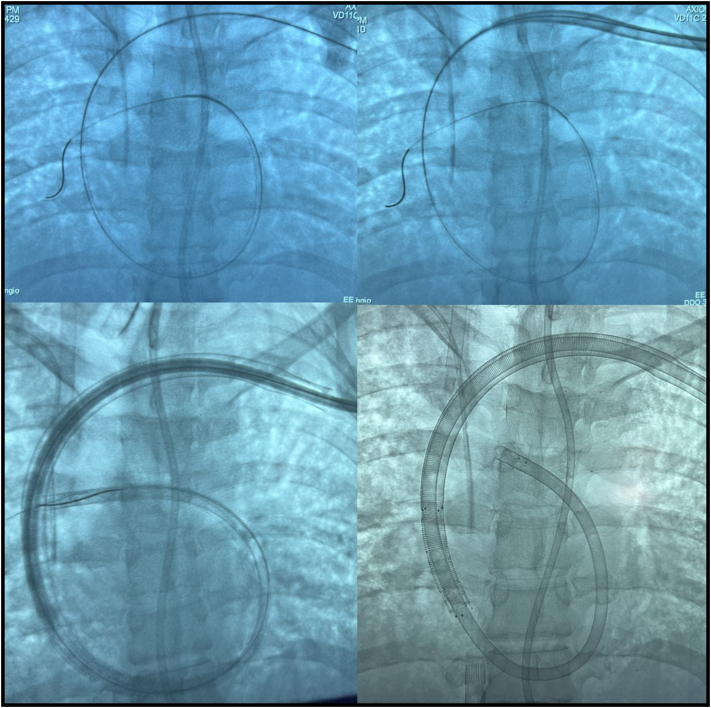
In the hybrid operating room, the patient was first transitioned to 2 sites: VV ECMO via the left IJ and right femoral veins. The existing RIJ vein percutaneous RVAD cannula was removed. Next, the left subclavian vein was accessed with a micropuncture needle and catheter. Under fluoroscopy, a Glidewire (Terumo) was advanced into the right lower lobe PA to provide extra purchase. This was exchanged over a catheter for an extra stiff, double-looped Lunderquist wire (Cook Medical). The site was serially dilated using the Avalon Elite Vascular access kit (Maquet GmbH) to 30F. Then a 31F, dual-lumen, right atrial to PA cannula was placed with the tip terminating in the PA (Figure 2). Flows were optimized (3.75 L/min), and subsequently oxygenation improved, with partial pressure of oxygen greater than 100 mm Hg.
Figure 2.
Fluoroscopic stepwise images of left subclavian vein cannulation with a percutaneous, dual-lumen right atrial to PA cannula.
On the new extracorporeal life support circuit, the patient's hemodynamics improved, and the bleeding at the RIJ cannulation site was then surgically controlled.
Postoperative Course
On the new circuit, his bacteremia resolved, and the RIJ site remained hemostatic. This allowed the patient to more easily participate in rehabilitation. Previously limited to ambulating 80 feet, the patient demonstrated remarkable progress by walking more than 1000 feet. Two weeks later, he underwent a double lung transplant on mechanical circulatory support. After a sweep gas trial on postoperative day zero, the patient was decannulated from ECMO. Two purse-string sutures were placed around the left subclavian vein site. The cannula was removed and the sutures were tied down sequentially in standard fashion. Adhering to institutional protocol, a postdecannulation venous ultrasound was performed within 48 hours, revealing no deep venous thrombosis. Nine months after initial presentation, the patient was discharged home and continues to thrive 1 year after the transplant.
Discussion
Left subclavian vein cannulation is a suitable alternative site for percutaneous placement of a dual-lumen RVAD cannula, providing improved mechanical right heart support compared with standard cannulation strategies for conventional VV ECMO.2,3 Additional benefits include preserved leg mobility and increased distance from the tracheostomy site, thereby lowering the risk of airway-related contamination.5 The left subclavian vein is preferred over the right because it makes a gentler turn into the superior vena cava, minimizing cannula kinking and associated flow limitations. However, this approach has limitations, such as the potential for obstructing venous drainage in the left upper extremity resulting in increased risk of left arm swelling and deep venous thrombosis.5 Routine postdecannulation venous ultrasounds can provide useful information in these patients.
Real-time fluoroscopy and proper wire selection are crucial for these endovascular procedures to be successful and safe. The former allows for continuous monitoring of wire position by a member of the surgical team during dilation and cannula placement. A Glidewire or the Safari wire (Boston Scientific), with its soft curved tip, can be initially used to reduce the risk of valvular or branch PA lumen injury. Afterward, they are exchanged over a catheter for the stiffer Lunderquist wire, which provides a safe platform for dilation and the over 270-degree turn required for cannula placement. Traversing the tricuspid and pulmonic valves during cannula placement carries the risk of valvular leaflet injury and structural damage. Adequate endovascular skills, an experienced cannulator, and real-time imaging are necessary for successful left subclavian vein cannulation.
When selecting the specific puncture site along the left subclavian vein, cannula depth and patient habitus must be considered. The drainage holes must align with the right atrium. Shallow positioning can result in ventricular abnormalities and significant pulmonary valve insufficiency, and excessive depth can lead to PA overload, hypertension, and hemorrhage. To facilitate dilation and prevent cannula kinking, it is important to avoid passage through the clavicular periosteum.
Transesophageal echocardiography can assist with cannula placement and monitoring, including assessing for valvular insufficiency and postcannulation right ventricle function. The Protek Duo and a cannula by Spectrum Medical (Cheltenham, UK) offer options for percutaneous right atrial to PA dual-lumen cannula placement.
Conclusions
In cases where internal jugular site cannulation is not available, left subclavian vein cannulation with real-time fluoroscopy is a technically challenging, but safe alternative for percutaneous RVAD placement.
Acknowledgments
Illustrations were provided by Andy Matlock, Department of Surgery, Emory School of Medicine.
Footnotes
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Funding: This project was supported by endowed research funds provided by Harriet and Burke Boger to Emory University School of Medicine.
Institutional Review Board number: STUDY00004012/Date approved: April 2, 2022.
Informed Consent Statement: The patient provided written informed consent for publication.
References
- 1.Bermudez C.A., Rocha R.V., Sappington R.L., Toyoda Y., Murray H.N., Boujoukos A.J. Initial experience with single cannulation for venovenous extracorporeal oxygenation in adults. Ann Thorac Surg. 2010;90:991–995. doi: 10.1016/j.athoracsur.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 2.Abrams D., Brodie D., Javidfar J., Brenner K., Wang D., Zwischenberger J., et al. Insertion of bicaval dual-lumen cannula via the left internal jugular vein for extracorporeal membrane oxygenation. ASAIO J. 2012;58:636–637. doi: 10.1097/MAT.0b013e31826feda5. [DOI] [PubMed] [Google Scholar]
- 3.Shafii A.E., McCurry K.R. Subclavian insertion of the bicaval dual lumen cannula for venovenous extracorporeal membrane oxygenation. Ann Thorac Surg. 2012;94:663–665. doi: 10.1016/j.athoracsur.2012.02.024. [DOI] [PubMed] [Google Scholar]
- 4.Bharat A., Querry M., Markov N.S., Kim S., Kurihara C., Garza-Castillon R., et al. Lung transplantation for patients with severe COVID-19. Sci Transl Med. 2020;12 doi: 10.1126/scitranslmed.abe4282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Javidfar J., Zaaqoq A.M., Yamashita M.H., Eschun G., Jacobs J.P., Heinsar S., et al. Venovenous extracorporeal membrane oxygenation in obese patients. JTCVS Tech. 2021;10:335–348. doi: 10.1016/j.xjtc.2021.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]