Delayed excision of benign primary cardiac tumor in the setting of metastatic disease.
Central Message.
Preliminary diagnosis of cardiac tumor using history and imaging characteristics can justify surveillance over immediate operative intervention in the appropriate setting.
Primary cardiac tumors are rare lesions that are often benign. Incidence of these tumors in multiple autopsy series range from 0.2% to 0.4%.1 Pathology of benign cardiac tumors include myxoma, rhabdomyoma, fibroma, hemangioma, and lipoma.2,3 Cardiac lipomas account for ∼8.4% of these tumors and have been documented in all chambers of the heart and valve leaflets.1 Few cases to date have documented cardiac lipomas with papillary muscle involvement (see the E-References).
Case Report/Description
The patient provided written informed consent for publication of this report. The institutional review board (IRB) or equivalent ethics committee of the University of Oklahoma Health Science Center did not approve this study due to the IRB's policy that single case reports are not considered human subjects research and therefore due not require IRB approval.
A 46-year-old woman initially presented with abdominal pain and fullness. A computed tomography (CT) image of the abdomen and pelvis revealed a large pelvic mass, possible liver metastasis, and left ventricular filling defect (Figure 1, A). Transesophageal echocardiography confirmed a large echogenic mass along the midinferolateral wall of the left ventricle that appeared to be attached to underlying myocardium. The cardiac surgery team was consulted and ordered cardiac gated magnetic resonance imaging (MRI) to better characterize the mass. MRI finding was consistent with lipoma (Figure 1, B). With the likelihood of this mass being benign, the cardiac team recommended management of her gynecologic malignancy first and the patient underwent oncologic resection during her initial hospital admission. Final pathology was metastatic ovarian and endometrial adenocarcinoma. Her postoperative positron emission tomography scan did not show enhancement of the cardiac mass, which corroborated the theory of a benign lesion (Figure 1, C). At her 1-month follow-up appointment after her cancer operation it was emphasized that although the cardiac mass appeared benign, without pathologic evidence there was still a possibility of malignancy. The patient denied any symptoms and had no evidence of heart failure or embolization. Using preoperative MRI and transesophageal echocardiography the broad base of the tumor appeared to involve the mitral valve papillary muscle and resection would likely require removal of the papillary muscle with subsequent mitral valve replacement. Due to her ongoing cancer treatment, the patient elected to undergo close surveillance. One year into surveillance, she developed symptoms of feeling faint. Interval echocardiography showed increase in size of the mass. Her gynecology/oncology team confirmed the patient completed treatment and was in remission. After a long discussion of the risks and benefits of surgery, the patient elected to undergo resection with possible valve replacement.
Figure 1.
A, Cardiac computed tomography angiogram with evidence of filling defect in the left ventricle. B, Sagittal view of a cardiac magnetic resonance imaging study with a well-circumscribed mass seen in the left ventricle. C, Postoperative positron emission tomography with no evidence of increased activity in the heart.
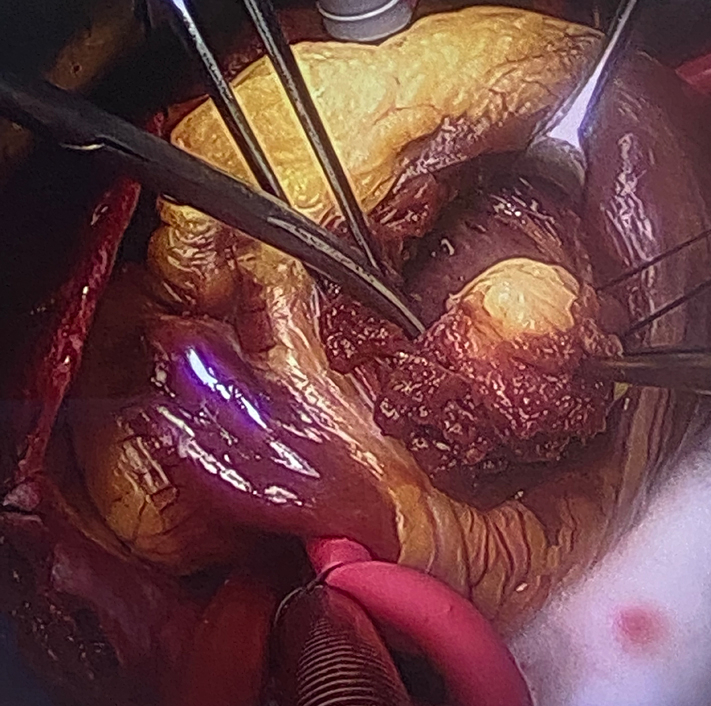
The operative approach started with a left atriotomy but its location made visualization across the mitral valve difficult. This led to a left ventriculotomy. With the heart arrested, we palpated the mass in the posterior ventricle wall and performed a ventriculotomy adjacent to the mass extending out to the apex. Once visualized, the mass did involve the anteromedial papillary muscle, chordal tissue, and myocardium. The tumor was removed en bloc with a significant portion of the anterior-medial papillary muscle. The mitral valve was dysfunctional and replaced with an On-X (On-X Life Technologies Inc) valve with posterior leaflet preservation. The patient tolerated the procedure well and was discharged home after an uncomplicated hospital course. Final pathology was consistent with benign intracardiac lipoma.
Comment
Cardiac tumors can vary in presentation from incidental in an asymptomatic patient to sudden death.4 The diagnosis of cardiac tumors is often based on patient history and imaging alone due to the difficulty of obtaining a biopsy. The imaging techniques that help delineate benign from malignant tumors include echocardiography, cardiac CT, and MRI.5 Definitive diagnosis cannot be made until surgery is performed and final pathology obtained. This creates a dilemma when a patient has an incidental finding of a cardiac tumor while being treated for malignancy. It is often hard to distinguish tumor from thrombus and although metastasis is the most common cardiac tumor, thrombus occurs at a much higher frequency.3 This raises a question: In an asymptomatic patient with metastatic cancer, is it safe to conclude whether or not a cardiac tumor is primary, secondary, malignant, benign, or even a thrombus based on imaging characteristics alone? Is a delay in treatment appropriate in certain situations? Our patient had multiple imaging modalities that suggested a primary benign cardiac tumor separate from her gynecologic malignancy. A positron-emission tomography–CT scan corroborated this theory when there was no cardiac enhancement. Because this cardiac tumor was discovered during her original malignancy workup, cardiac surveillance allowed her to undergo surgical resection, chemotherapy, and radiation without delay. History and imaging characteristics of a benign cardiac tumor in an asymptomatic patient provide satisfactory evidence to justify postponing treatment. To do so, communication is vital and confirming the patient understands his or her condition and the need for close surveillance is critical.
Footnotes
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
The Institutional Review Board (IRB) or equivalent ethics committee of the University of Oklahoma Health Science Center did not approve this study due to the IRB's policy that single case reports are not considered human subjects research and therefore due not require IRB approval.
Patient consent: The patient's informed consent was obtained for the publication of the following case report.
References
- 1.Shu S., Wang J., Zheng C. From pathogenesis to treatment, a systemic review of cardiac lipoma. J Cardiothorac Surg. 2021;16:1–7. doi: 10.1186/s13019-020-01379-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grebenc M.L., Rosado de Christenson M.L., Burke A.P., Green C.E., Galvin J.R. Primary cardiac and pericardial neoplasms: radiologic-pathologic correlation. Radiographics. 2000;20:1073–1103. doi: 10.1148/radiographics.20.4.g00jl081073. quiz 1110-1, 1112. [DOI] [PubMed] [Google Scholar]
- 3.Stojanovska J. Is it a cardiac tumor or a thrombus: an everlasting dilemma solved by radiomics analysis. Acad Radiol. 2022;29:S9–S10. doi: 10.1016/j.acra.2021.11.006. [DOI] [PubMed] [Google Scholar]
- 4.Poterucha T.J., Kochav J., O'Connor D.S., Rosner G.F. Cardiac tumors: clinical presentation, diagnosis, and management. Curr Treat Options Oncol. 2019;20:66. doi: 10.1007/s11864-019-0662-1. [DOI] [PubMed] [Google Scholar]
- 5.Paraskevaidis I.A., Michalakeas C.A., Papadopoulos C.H., Anastasiou-Nana M. Cardiac tumors. ISRN Oncol. 2011;2011 doi: 10.5402/2011/208929. [DOI] [PMC free article] [PubMed] [Google Scholar]
E-References
- Koshy A.N., Koshy G., Hardikar A.A. Intracardiac lipoma arising from the papillary muscle. J Card Surg. 2011;26:65–66. doi: 10.1111/j.1540-8191.2010.01156.x. [DOI] [PubMed] [Google Scholar]
- Anderson D.R., Gray M.R. Mitral incompetence associated with lipoma infiltrating the mitral valve. Br Heart J. 1988;60:169–171. doi: 10.1136/hrt.60.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y.S., Lee K.H., Choi S.J., Baek W.K. Cardiac lipoma arising from left ventricular papillary muscle: resect or not? J Thorac Cardiovasc Surg. 2018;156:244–246. doi: 10.1016/j.jtcvs.2018.01.040. [DOI] [PubMed] [Google Scholar]
- Prestipino F., Cammardella A.G., Chello M. Unconventional location for a cardiac lipoma: the anterior papillary muscle. J Cardiol Cases. 2016;14:71–73. doi: 10.1016/j.jccase.2016.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]



