Abstract
Objective
Even though severe tricuspid regurgitation is not uncommon after cardiac transplantation, primary severe tricuspid regurgitation is rare. We present such a case with additional complexities.
Methods
The patient was 44-year-old man with a HeartWare durable left ventricular assist device (Heartware Inc) who received a temporary right ventricular assist device (RVAD) with a ProtekDuo cannula (LivaNova Inc USA) for refractory ventricular fibrillation and underwent a heart transplant as United Network for Organ Sharing Status 1, in the presence of partially compensated cardiogenic shock, renal failure. Given complex re-operative surgery in a volume-overloaded patient with unknown pulmonary vascular resistance, an RVAD cannula was preserved and re- inserted during cardiac transplant. Postoperatively he required hemodialysis, had severe primary tricuspid regurgitation discovered after RVAD removal and developed Enterobacter mediastinitis. He underwent complex tricuspid valve repair for flail tricuspid leaflet due to ruptured papillary muscle likely due to RVAD cannula injury, after multiple mediastinal washouts and was followed by delayed chest reconstruction.
Results
The patient is doing well, 6 months after discharge to home, asymptomatic, without re-admissions, on renal recovery path, with no tricuspid regurgitation and good biventricular function.
Conclusions
Replacing the tricuspid valve in presence of hemodialysis catheter, immunosuppression and mediastinitis could be high risk for endocarditis. Even though we have short-term follow-up, tricuspid valve repair can be an effective way of managing primary severe regurgitation especially when there is a desire or need to avoid valve replacement.
Key Words: tricuspid regurgitation, tricuspid repair, heart failure, heart transplant, right ventricular assist device

Complex repair of TV for flail anterior leaflet after heart transplant.
Central Message.
Complex repair of a tricuspid valve for severe tricuspid regurgitation may be favored over replacement in some patients after heart transplant.
Perspective.
Primary severe tricuspid regurgitation in a recent heart transplant with active mediastinitis, in a newly dialysis-dependent patient is a unique situation. Valve replacement may be more predictable but risks endocarditis, structural degeneration. A failed repair may lead to longer cardiopulmonary bypass in a sick patient if intraoperative failure or reentry through reconstructed chest if late failure.
Many patients who undergo heart transplantation are medically complex and may present in cardiogenic shock. Such patients often require mechanical circulatory support to bridge to transplant, which may need to be continued during the immediate posttransplant period. The rate of potential complications increases with the use of mechanical circulatory support, most commonly related to hematologic, neurologic, and limb complications1; however, direct damage to vessels and the heart may occur.
In this case, we present a patient who underwent heart transplant and likely experienced damage to the tricuspid valve (TV) as a result of right ventricular assist device (RVAD) cannula placement. Consent was obtained from the patient for publication of study data; this study was exempt from the Washington University Institutional Review Board.
Clinical Summary
A 44-year-old man with nonischemic cardiomyopathy treated with HeartWare Ventricular Assist System (HeartWare Inc) implantation, presented in refractory ventricular fibrillation resulting in cardiogenic shock. A Protek Duo (LivaNova USA Inc) percutaneous RVAD was placed to provide biventricular support.
He was upgraded to status 1, and when an appropriate heart became available he underwent redo sternotomy, HeartWare Ventricular Assist System explantation, and heart transplant. The RVAD cannula was kept to the side and reinserted directly during right-sided anastomoses. He was extubated on postoperative day 1 but required hemodialysis. On postoperative day 11, the RVAD was removed. Severe tricuspid regurgitation (TR) with a flail leaflet causing moderate RV dilatation and mild RV dysfunction was found on the first surveillance transthoracic echocardiogram. This was managed conservatively with a plan to intervene after the patient recovered. One month posttransplant, the patient developed Enterobacter mediastinitis infection requiring multiple extensive debridements with an open chest for several weeks. Once the cultures cleared, we proceeded with tricuspid intervention.
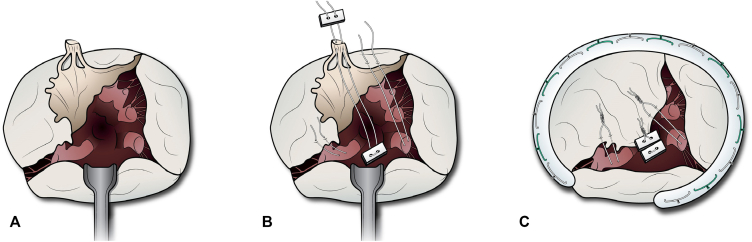
In the operating room, the mediastinum was accessed by reopening the wound. There were few adhesions, and the right-sided structures were easily identified. The aorta had minimal room and was dissected distally to allow cannulation. Once dissection was complete, the patient was placed on cardiopulmonary bypass using aortic and bicaval cannulation. We performed the operation without aortic crossclamping to avoid further insult to the RV. The right atrium was opened and the flail anterior leaflet was identified. Two polytetrafluoroethylene (PTFE) sutures were passed through medial and inferior papillary muscles and then passed through the anterior TV leaflet edge 5 mm from each side of the prolapse, in horizontal mattress fashion and left loose. A pledgeted PTFE suture was placed in a horizontal mattress through the interventricular septum underneath the septal leaflet, passed through the fibrous union of the anterior leaflet cords without crossing the cords of the septal leaflet, and was tied down. The remaining 2 PTFE sutures were then tied at the level of the annulus, visually estimating the plane of the annulus. This served as a backup safety mechanism to avoid anterior leaflet prolapse in the case of undoing of the primary repair. Tricuspid annuloplasty was performed using a 26-mm Tricuspid Physio ring (Edwards Lifesciences) (Figure 1). Saline test showed minimal leak. The right atrium was closed and cardiopulmonary bypass was weaned off. Intraoperative transesophageal echocardiogram showed TR reduced to trace (Figure 2) with a mean gradient of 2 mm Hg.
Figure 1.
Complex repair of the tricuspid valve (TV) showing the flail anterior leaflet (A) and the pledgeted polytetrafluoroethylene (PTFE) suture (B) placed in a horizontal mattress fashion through the interventricular septum underneath the septal leaflet and passed through the fibrous union of the anterior leaflet cords without crossing the cords of the septal leaflet, 2 PTFE sutures passed through medial and inferior papillary muscles through the anterior TV leaflet edge 5 mm from each side of the prolapse. C, TV after all sutures were tied.
Figure 2.
A, Transthoracic echocardiogram demonstrating flail tricuspid leaflet with dilated right ventricle. Transesophageal echocardiogram showing severe tricuspid regurgitation (B) and trace tricuspid regurgitation after complex repair (C).
Two days later, the chest was closed with omental coverage of the mediastinum, pectoralis major muscle advancement flaps, and sternal and rib plating by plastic surgery. The patient was discharged home a month after.
Six months after discharge, he is doing well with good biventricular function, no TR, and showing encouraging signs of renal recovery. Because cardiac biopsies may disrupt the complex repair, rejection is monitored with serial transthoracic echocardiogram and blood tests for gene expression profiling, a validated diagnostic tool to monitor for rejection in patients undergoing transplant.
Discussion
TV replacement in the presence of a hemodialysis catheter, immunosuppression, and mediastinitis could present high risk for endocarditis along with a reduced quality and expectancy of life.2,3 Thus, we opted for complex TV repair over replacement. Despite short-term follow-up in this case, complex TV repair for a mechanical issue can be an effective means of managing severe TR, especially when there is need to avoid replacement.
TR is the most common valvular issue for heart transplant recipients and may result in life-limiting symptoms.4 Often, it is due to RV dysfunction following transplant that may improve with time; however, TR may be due to mechanical issues.5
Overall, TR is a common problem in patients who have undergone heart transplant. It is often clinically inconsequential, but strong consideration should be given to intervention when it is severe and due to a mechanical issue. Even in medically complex situations, repair may be possible and could be encouraged.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires that editors and reviewers disclose conflicts of interest and decline handling manuscripts for which they have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Acknowledgments
We thank Chrystie Tyler, graphic designer/ medical illustrator at department of Surgery, Washington University School of Medicine, Saint Louis, for the drawings.
Footnotes
Informed Consent: Consent was obtained from the patient.
IRB: This study was exempt from the Washington University Institutional Review Board.
References
- 1.Mandawat A., Rao S.V. Percutaneous mechanical circulatory support devices in cardiogenic shock. Circ Cardiovasc Interv. 2017;10:e004337. doi: 10.1161/CIRCINTERVENTIONS.116.004337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bishawi M., Zanotti G., Shaw L., MacKenzie M., Castleberry A., Bartels K., et al. Tricuspid valve regurgitation immediately after heart transplant and long-term outcomes. Ann Thorac Surg. 2019;107:1348–1355. doi: 10.1016/j.athoracsur.2018.10.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson C.A., Shernan S.K., Leacche M., Rawn J.D., Paul S., Mihaljevic T., et al. Severity of intraoperative tricuspid regurgitation predicts poor late survival following cardiac transplantation. Ann Thorac Surg. 2004;78:1635–1642. doi: 10.1016/j.athoracsur.2004.05.028. [DOI] [PubMed] [Google Scholar]
- 4.Kwon M.H., Shemin R.J. Tricuspid valve regurgitation after heart transplantation. Ann Cardiothorac Surg. 2017;6:270–274. doi: 10.21037/acs.2017.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Veen K., Papageorgiou G., Zijderhand C., Brugts J., Mokhles M., Manintveld O., et al. The clinical Impact and long-term outcome of tricuspid regurgitation in patients with orthotopic heart transplantation. J Heart Lung Transplant. 2020;39:S291–S292. [Google Scholar]