This cohort study identifies social determinants of health patterns and estimates their associations with US children’s mental health, cognition, and physical health.
Key Points
Question
What are the underlying patterns of the multidimensional social determinants of health (SDOH), and what are their associations with individual mental health, cognition, and physical health outcomes in children?
Findings
In this cohort study of 10 504 children, significant disparities in child developmental health outcomes were observed across 4 patterns of SODH: (1) affluence, (2) high-stigma environment, (3) high socioeconomic deprivation, and (4) high crime and drug sale rates coupled with lower education and densely populated areas. The worst mental health, cognitive performance, and physical health outcomes were found in the high socioeconomic deprivation group (pattern 3).
Meaning
The SDOH patterns analyzed in this study were able to capture and quantify the multidimensional nature of SDOH that children experience, and the finding that socioeconomic deprivation was associated with the worst outcomes should guide more targeted public health and social policies to address causes of child development disparities.
Abstract
Importance
Social determinants of health (SDOH) influence child health. However, most previous studies have used individual, small-set, or cherry-picked SDOH variables without examining unbiased computed SDOH patterns from high-dimensional SDOH factors to investigate associations with child mental health, cognition, and physical health.
Objective
To identify SDOH patterns and estimate their associations with children’s mental, cognitive, and physical developmental outcomes.
Design, Setting, and Participants
This population-based cohort study included children aged 9 to 10 years at baseline and their caregivers enrolled in the Adolescent Brain Cognitive Development (ABCD) Study between 2016 and 2021. The ABCD Study includes 21 sites across 17 states.
Exposures
Eighty-four neighborhood-level, geocoded variables spanning 7 domains of SDOH, including bias, education, physical and health infrastructure, natural environment, socioeconomic status, social context, and crime and drugs, were studied. Hierarchical agglomerative clustering was used to identify SDOH patterns.
Main Outcomes and Measures
Associations of SDOH and child mental health (internalizing and externalizing behaviors) and suicidal behaviors, cognitive function (performance, reading skills), and physical health (body mass index, exercise, sleep disorder) were estimated using mixed-effects linear and logistic regression models.
Results
Among 10 504 children (baseline median [SD] age, 9.9 [0.6] years; 5510 boys [52.5%] and 4994 girls [47.5%]; 229 Asian [2.2%], 1468 Black [14.0%], 2128 Hispanic [20.3%], 5565 White [53.0%], and 1108 multiracial [10.5%]), 4 SDOH patterns were identified: pattern 1, affluence (4078 children [38.8%]); pattern 2, high-stigma environment (2661 children [25.3%]); pattern 3, high socioeconomic deprivation (2653 children [25.3%]); and pattern 4, high crime and drug sales, low education, and high population density (1112 children [10.6%]). The SDOH patterns were distinctly associated with child health outcomes. Children exposed to socioeconomic deprivation (SDOH pattern 3) showed the worst health profiles, manifesting more internalizing (β = 0.75; 95% CI, 0.14-1.37) and externalizing (β = 1.43; 95% CI, 0.83-2.02) mental health problems, lower cognitive performance, and adverse physical health.
Conclusions
This study shows that an unbiased quantitative analysis of multidimensional SDOH can permit the determination of how SDOH patterns are associated with child developmental outcomes. Children exposed to socioeconomic deprivation showed the worst outcomes relative to other SDOH categories. These findings suggest the need to determine whether improvement in socioeconomic conditions can enhance child developmental outcomes.
Introduction
Social determinants of health (SDOH), the “conditions in which people are born, grow, live, work, and age,”1,2 can affect health outcomes,3,4,5 including mental, cognitive, and physical well-being.6,7 Children are raised in neighborhoods with diverse SDOH profiles, including high poverty levels and unemployment; rural settings; limited access to quality health care, nutritious food, clean water, or educational opportunities; and increased exposure to crime and drug sales, and these SDOH are linked to an array of developmental problems, including mental health disorders,7,8,9,10,11,12 suicidal behaviors,13,14,15 cognitive performance,6,7,16 and physical health issues.10,17 Unraveling the complex relationships between SDOH and child development is crucial to understanding which SDOH combinations are associated with which developmental outcomes. Without such information, it is not possible to devise effective, targeted policies and interventions.
Current measurement tools are unable to capture the multidimensionality of SDOH. Most SDOH measures are composite indices, such as the Area Deprivation Index (ADI)18 and Social Vulnerability Index (SVI),19 that depend on an arbitrarily selected small set of SDOH variables and provide only generic and numeric vulnerability levels. These indices oversimplify the intricate clustering of SDOH and their potentially different effects on child health, forcing policymakers to attempt broad, and therefore more expensive, SDOH-focused interventions to mitigate health disparities. Moreover, previous research primarily correlates SDOH with broader county- and state-level outcomes4,20,21 instead of measuring individual-level child health directly,13,14,15,22,23 thereby increasing the risks of ecological fallacy.
The purpose of this study was to fill this critical knowledge gap by using innovative methodologies that capture and analyze the multidimensional nature of SDOH and uncover their associations with individual-level child mental health, cognition, and physical health outcomes. We hypothesized that distinct SDOH patterns exist, with different implications for child development and health outcomes.
Methods
Participants
This cohort study used data from the Adolescent Brain Cognitive Development (ABCD) Study, which recruited a diverse sample of children aged 9 to 10 years from 21 sites across the US, including urban, rural, and mountainous areas. The multistage probability sampling recruitment and oversampling for schools with more than 10% Black children by approximately 50% provided a close approximation to national sociodemographics based on age, sex, race and ethnicity, socioeconomic status, and urbanicity.24 Data were collected from September 1, 2016, to April 24, 2021.25 Institutional review boards at each study site approved the research protocol, with central institutional review board approval granted by the University of California, San Diego. All participants provided written informed consent.26 Children and parents completed surveys regarding child developmental outcomes and household socioeconomic characteristics. More details about recruitment and sampling strategies are described elsewhere.25 We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Measures
SDOH Exposure
The ABCD Study linked population-level SDOH characteristics to children by using primary residential addresses.27 Therefore, the input measures are at the individual level. We systematically reviewed major SDOH conceptual frameworks from the World Health Organization,1 Healthy People 2030,28 the US Agency for Healthcare Research and Quality,29 and the US Centers for Disease Control and Prevention2 to select SDOH variables. We added 4 indicators regarding state-level implicit bias to account for structural stigma27,30 and variables used to construct common SDOH indices, including the Opportunity Atlas,31 Child Opportunity Index,32 ADI,33,34,35 and SVI,19 to be comparable with prior research.
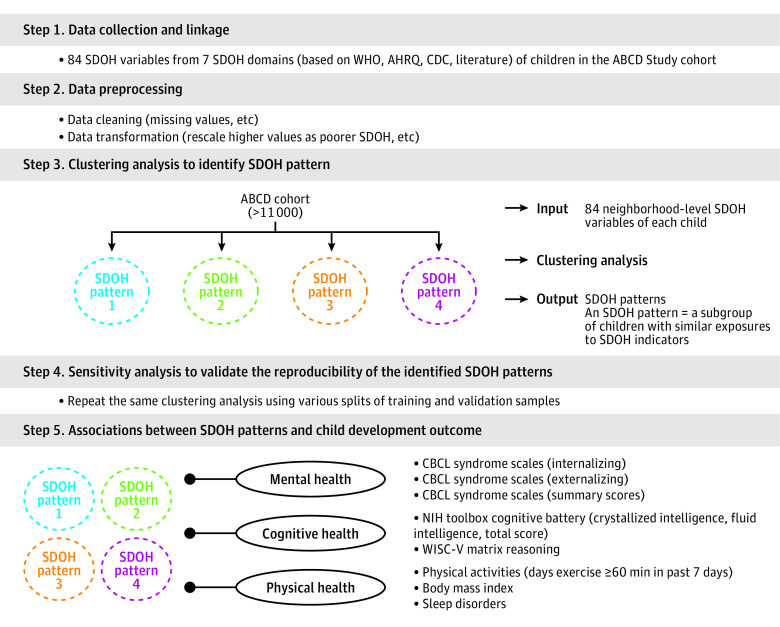
We included 84 neighborhood-level SDOH variables across the following 7 SDOH domains (Figure 1; eMethods 1 and eTable 1 in Supplement 1): (1) bias (4 variables, eg, implicit attitudes toward race, explicit attitudes toward immigrant status), (2) education (11 variables, eg, availability of educational resources, number of early childhood centers), (3) physical and health infrastructure (16 variables, eg, percentage of mobile homes, crowded housing conditions), (4) natural environment (10 variables, eg, access to healthy food, walkability index), (5) socioeconomic status (27 variables, eg, poverty rate, residents without a high school diploma), (6) social context (8 variables, eg, proportion of people older than 65 years, people with disabilities), and (7) crime and drugs (11 variables, eg, county-level counts of arrests, state laws related to marijuana possession and use) (eMethods 1 in Supplement 1).
Figure 1. Study Pipeline.
ABCD, Adolescent Brain Cognitive Development; AHRQ, Agency for Healthcare Research and Quality; CBCL, Child Behavior Checklist; CDC, Centers for Disease Control and Prevention; NIH, National Institutes of Health; SDOH, social determinants of health; WHO, World Health Organization; WISC-V, Wechsler Intelligence Scale for Children.
Child Mental Health, Cognitive Performance, and Physical Health
All outcome measures are described in eMethods 2 in Supplement 1. We included measures of child psychopathology and suicidal ideation and behaviors assessed at baseline (wave 1) and 1-year (wave 2) and 2-year (wave 3) follow-up. Internalizing (eg, anxious, withdrawn, somatic complaints), externalizing (eg, rule breaking, aggressive behaviors), and social (eg, thoughts, social, attention) problems were assessed using the caregiver-reported Child Behavior Checklist (CBCL), which is an empirically validated and widely used assessment.36,37,38,39 We also included the CBCL Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) (DSM-5)–oriented symptom subscales for depression, anxiety, attention deficit hyperactivity disorder, somatic problems, opposition behaviors, and conduct problems. Raw scores on this measure were converted to t scores, with a t score >60 representing a clinically significant disorder.36,37 The computerized version of the Kiddie Schedule for Affective Disorders and Schizophrenia for DSM-5 (Lifetime Version)40 was used to identify suicidal ideation and suicide attempts endorsed by either the child or caregiver.
The psychometrically sound National Institutes of Health Toolbox Cognition Battery41 was used to assess cognitive function in children,42,43,44 including 7 domain-specific cognitive tests from 2 categories (crystallized intelligence and fluid intelligence).45,46,47,48,49 We calculated the fully corrected crystallized cognition composite scores (derived from 2 subtests of the cognition battery: the picture vocabulary test and oral reading recognition test) and fluid cognition composite scores (derived from 5 subtests of the cognition battery: the card sort, flanker inhibitory control and attention test, picture sequence memory test, list-sorting working memory test, and pattern comparison processing speed test). We also used the Wechsler Intelligence Scale for Children (WISC-V),50 which measures nonverbal intelligence. We included 3 measures of physical health outcomes: body mass index (BMI), frequency of regular exercise for 60 minutes (days with ≥60-minute exercise in the past 7 days at survey), and sleep disorders (using the Sleep Disturbance Scale for Children,51 including subscores of 6 subdomains and composite score).
Covariates
We controlled for age, sex, and race and ethnicity reported in the baseline caregiver-completed ABCD Study Parent Demographics Survey. Race and ethnicity were based on baseline caregiver-reported categories from a list of provided terms and are included to account for the social construct that reflects youths’ experiences and exposure to social advantages and oppression.
Statistical Analysis
Data Preprocessing and Missing Data
Among the 84 candidate SDOH variables for clustering analysis, 82 were continuous variables and 2 were categorical variables (converted to binary values). The percentage of missingness was small, ranging between 5% and 8% (eTable 1 in Supplement 1). Since data are not missing at random (eFigure 1 in Supplement 1), multiple imputations may not be reliable.52 Therefore, we only included children with complete SDOH data in the primary analysis to minimize bias. All continuous variables were z score scaled to eliminate artifactual effects caused by variables being measured on different scales. Finally, we obtained an SDOH variable vector for each child.
SDOH Pattern Identification
We applied the hierarchical agglomerative clustering algorithm to derive SDOH patterns using individual-level child SDOH vectors. The optimal cluster number was determined by considering cluster separation in the dendrogram, 14 cluster measurements using the NbClust package,53 and cluster separation in t-distributed stochastic neighbor embedding54 (eMethods 3 in Supplement 1). Each resultant cluster represents a specific SDOH pattern of individuals with similar SDOH profiles.
Sensitivity Analyses for SDOH Pattern Stability
We evaluated the stability of the identified SDOH patterns by conducting 3 sensitivity analyses (eMethods 4 in Supplement 1). First, we assessed whether excluding the 1306 children with any missing values from the analysis changed SDOH patterns. Second, we repeated the hierarchical agglomerative clustering and replicated the SDOH patterns using data from only the 9137 unique neighborhoods of residence for children in the sample, thereby avoiding any double counting of neighborhoods. Third, we conducted a robustness check of the study samples.
SDOH Pattern Interpretation
We visualized the resultant SDOH patterns using bar charts, depicting the proportion of disadvantaged children across different variables defined as exposure to more than 75% of the vulnerability level in the 82 continuous SDOH variables. For categorical variables, ie, marijuana law type and census tract urban classification, we used chord diagrams to illustrate their distribution across SDOH patterns.
We also compared baseline demographic, health data, and individual SDOH variables of children across the identified SDOH patterns, using analysis of variance tests (for continuous values) and χ2 tests (for categorical values). Multiple comparisons were adjusted using the Bonferroni correction. A 2-tailed P < .05 was considered the threshold for statistical significance.
Exploring Associations Between SDOH Patterns and Children’s Developmental Outcomes
We estimated the associations between the identified SDOH patterns and children’s health outcomes using mixed-effects linear regression models (for continuous outcomes) and mixed-effects logistic regression models (for binary outcomes). These models included study sites as a random effect to adjust the clustering design and age, sex, and race and ethnicity as covariates. We fitted models for mental health outcomes at baseline and 1-year and 2-year follow-up and for cognitive and physical outcomes at baseline due to data availability.
All statistical analyses were performed using Python, version 3.7 (Python Software Foundation) and R, version 4.1 (R Foundation for Statistical Computing) software. Clustering models were implemented based on Python packages scikit-learn, version 0.23.2 and scipy, version 1.5.3. The t-SNE algorithm was implemented based on the Python package scikit-learn, version 0.23.2. The R package NbClust was used to calculate measures of clusters to determine the optimal cluster number in hierarchical agglomerative clustering. Linear mixed-effects models and logistic mixed-effects models were fitted using lme4 in R. All other statistical tests were performed using R. Chord diagrams were created using the R package circlize. Other data visualization, including bar plots and forest plots, were generated using the Python package matplotlib, version 3.0.
Results
Descriptive Statistics
The ABCD Study cohort included 10 504 children (median [SD] age, 9.9 [0.6] years) with complete SDOH information. Of the studied participants, 5510 were boys (52.5%) and 4994 girls (47.5%), and 229 were Asian (2.2%), 1468 Black (14.0%), 2128 Hispanic (20.3%), 5565 White (53.0%), and 1108 multiracial (10.5%) (Table 1).
Table 1. Baseline Characteristics of the Study Cohort Across Social Determinants of Health (SDOH) Patterns.
| Characteristica | All participants (N = 10 504) | SDOH pattern,b No. (%) | |||||
|---|---|---|---|---|---|---|---|
| 1 (n = 4078) | 2 (n = 2661) | 3 (n = 2653) | 4 (n = 1112) | P valuec | Bonferroni-corrected P value | ||
| Age, mean (SD), y | 9.9 (0.6) | 9.9 (0.6) | 9.9 (0.6) | 9.9 (0.6) | 9.9 (0.6) | <.001 | .02 |
| Sex | |||||||
| Female | 4994 (47.5) | 1907 (46.8) | 1250 (47.0) | 1288 (48.5) | 549 (49.4) | .29 | >.99 |
| Male | 5510 (52.5) | 2171 (53.2) | 1411 (53.0) | 1365 (51.5) | 563 (50.6) | ||
| Parents’ education (less than bachelor’s degree) | 4176 (39.8) | 766 (18.8) | 981 (36.9) | 1754 (66.1) | 675 (60.7) | .01 | .32 |
| Race and ethnicity | |||||||
| Asian | 229 (2.2) | 141 (3.5) | 15 (0.6) | 19 (0.7) | 54 (4.9) | <.001 | <.001 |
| Black | 1468 (14.0) | 178 (4.4) | 219 (8.2) | 999 (37.7) | 72 (6.5) | ||
| Hispanic | 2128 (20.3) | 449 (11.0) | 246 (9.2) | 760 (28.6) | 673 (60.5) | ||
| White | 5565 (53.0) | 2890 (70.9) | 1889 (71.0) | 577 (21.7) | 209 (18.8) | ||
| Multiracial | 1108 (10.5) | 416 (10.2) | 291 (10.9) | 297 (11.2) | 104 (9.4) | ||
| Parents’ marital status | |||||||
| Married | 7177 (68.3) | 3306 (81.1) | 2035 (76.5) | 1179 (44.4) | 657 (59.1) | <.001 | <.001 |
| Single parent | 2651 (25.2) | 647 (15.9) | 501 (18.8) | 1181 (44.5) | 322 (29.0) | ||
| Living with partner | 597 (5.7) | 119 (2.9) | 115 (4.3) | 251 (9.5) | 112 (10.1) | ||
| Annual household income, $ | |||||||
| <50 000 | 2776 (26.4) | 382 (9.4) | 588 (22.1) | 1356 (51.1) | 450 (40.5) | <.001 | <.001 |
| 50 000-100 000 | 2775 (26.4) | 978 (24.0) | 966 (36.3) | 606 (22.8) | 225 (20.2) | ||
| >100 000 | 4082 (38.9) | 2480 (60.8) | 969 (36.4) | 351 (13.2) | 282 (25.4) | ||
Variables including participants’ demographic characteristics and family mental health history records were not used in clustering analysis for SDOH pattern identification.
Social determinants of health patterns: 1, affluent community; 2, high-stigma environment; 3, high socioeconomic deprivation; 4, high crime and drug sales, low education, high population density.
Comparisons across all 4 SDOH patterns were performed using analysis of variance for continuous variables and χ2 test for categorical variables. A 2-tailed P < .05 was considered as the threshold for statistical significance.
Four Distinct SDOH Patterns
Four child clusters were identified (eResults 1 and eFigures 2 and 3 in Supplement 1). Each cluster indicates a unique SDOH pattern (Figure 2; eFigures 4 and 5 and eTable 2 in Supplement 1).
Figure 2. Characteristics of the Identified Social Determinants of Health (SDOH) Patterns.

Each bar shows the proportion of children with disadvantaged status in each (continuous) SDOH variable across SDOH patterns. Children with disadvantaged SDOH are those who have worse SDOH exposures than 75% of the population with regard to a specific SDOH variable. eFigure 4 in Supplement 1 provides more detailed information. ECE indicates early childhood education; SES, socioeconomic status.
Pattern 1
In SDOH pattern 1, 4078 children (38.8%) lived in affluent communities characterized by higher socioeconomic status, low structural stigma, moderate crime rates, and good academic performance (eg, highest third-grade reading and math proficiency). These children had easy access to healthy food, a healthier environment (eg, good air quality, low heat exposures), low social vulnerability (eg, lowest single-parent family rates, uncrowded housing, lowest minority populations), and moderate population density and walkability (Figure 2A).
Pattern 2
In SDOH pattern 2, 2661 children (25.3%) lived in a high-stigma environment that was marked by the highest implicit bias and discrimination toward women and sexual and gender minority groups and low college enrollment. These children lived in a poor environment for industrial pollutants, ozone, heat exposure, and particulate matter with a diameter less than 2.5 μm. The largest proportion of these children were aged 17 years or younger. This pattern included mobile homes and group quarters (eg, nursing homes, military barracks) and had the lowest number of white-collar workers, homeowners, and urbanicity characteristics (eg, lowest population density, lowest walkability, not close to highways) (Figure 2B).
Pattern 3
In SDOH pattern 3, 2653 children (25.3%) lived in a high socioeconomic deprivation environment that was characterized by the highest rates in most metrics of the ADI (eg, family income, income disparity, low home value, unemployment rates, high poverty rates, high single-family proportion, no telephone), SVI (eg, poverty rates, highest disabled population proportion), and Child Opportunity Index (eg, lowest health insurance, lowest reading and math proficiency, large public assistance–dependent family proportion) but the lowest Opportunity Atlas social mobility scores. Children in this pattern experienced the highest levels of racism and discrimination toward immigrants and the most severe lead exposure (Figure 2C).
Pattern 4
In SDOH pattern 4, 1112 children (10.6%) lived in environments characterized by high crime and drug sales, low education, and high population density. These children experienced the highest crime and drug sale rates, school poverty, air pollution (the highest amount of airborne microparticles), crowded housing, population density, and minority populations and the lowest levels of educational attainment and resources (eg, the lowest high school graduation rates and available early childhood education centers), access to a healthy environment (eg, lowest greenspace access), and homeownership rates (Figure 2D).
There are distinct racial and ethnic differences across SDOH patterns. Most White children were from affluent communities (pattern 1, 2890 [70.9%]) and high-stigma environments (pattern 2, 1889 [71.0]). Conversely, areas of high socioeconomic deprivation (pattern 3) revealed a much higher representation of Black (999 [37.7%]) and Hispanic (760 [28.6%]) children than their Asian counterparts (19 [0.7%]). Hispanic children were overrepresented in high-crime, low-education, and densely populated areas (pattern 4, 673 [60.5%]). Results of sensitivity analyses replicated the 4-cluster structure in the primary analyses and confirmed its robustness (eResults 2 and eFigures 6-8 in Supplement 1).
Child Health Disparities Across SDOH Patterns
Significant differences in associated child developmental outcomes were found across the SDOH patterns (Table 2; Figure 3; eFigures 9-11 and eTable 3 in Supplement 1). Children living in SDOH pattern 3 (high socioeconomic deprivation) had the worst health outcomes relative to the other 3 SDOH patterns, including more mental health issues, suicidal behaviors, lower cognitive performance, and poor physical health (Table 2), even after adjusting for covariates (Figure 3; eFigure 11 and eTable 3 in Supplement 1).
Table 2. Baseline Mental Health, Cognitive, and Physical Health Outcomes Across Social Determinants of Health (SDOH) Patterns.
| Characteristic | All participants (N = 10 504) | SDOH pattern, mean (SD)a | P value | Bonferroni-corrected P value | |||
|---|---|---|---|---|---|---|---|
| 1 (n = 4078) | 2 (n = 2661) | 3 (n = 2653) | 4 (n = 1112) | ||||
| Mental health outcomes | |||||||
| CBCL internalizing problems | |||||||
| Anxious and depressed | 53.46 (5.91) | 53.29 (5.69) | 53.95 (6.56) | 53.36 (5.72) | 53.13 (5.40) | <.001 | <.001 |
| Withdrawn and depressed | 53.47 (5.72) | 53.06 (5.20) | 53.62 (5.93) | 54.01 (6.24) | 53.30 (5.54) | <.001 | <.001 |
| Somatic complaints | 54.89 (6.04) | 54.42 (5.68) | 55.44 (6.37) | 55.18 (6.16) | 54.61 (6.05) | <.001 | <.001 |
| Social problems | 52.76 (4.68) | 52.26 (4.20) | 52.93 (4.91) | 53.40 (5.15) | 52.58 (4.37) | <.001 | <.001 |
| Total score | 45.68 (10.27) | 44.52 (9.77) | 46.43 (10.21) | 47.08 (10.96) | 44.80 (9.91) | <.001 | <.001 |
| CBCL externalizing problems | |||||||
| Rule-breaking behaviors | 52.74 (4.83) | 52.11 (4.13) | 52.80 (4.77) | 53.79 (5.80) | 52.39 (4.38) | <.001 | <.001 |
| Aggressive behaviors | 52.79 (5.46) | 52.34 (4.87) | 53.05 (5.70) | 53.39 (6.16) | 52.39 (4.94) | <.001 | <.001 |
| Total score | 48.43 (10.59) | 47.78 (10.24) | 49.43 (10.78) | 48.70 (10.83) | 47.74 (10.58) | <.001 | <.001 |
| CBCL problem behaviors | |||||||
| Thought problems | 53.77 (5.86) | 53.45 (5.48) | 54.39 (6.28) | 54.08 (6.27) | 52.76 (4.86) | <.001 | <.001 |
| Attention problems | 53.86 (6.11) | 53.41 (5.69) | 54.21 (6.43) | 54.45 (6.56) | 53.31 (5.51) | <.001 | <.001 |
| Total score | 45.81 (11.26) | 44.67 (10.75) | 46.98 (11.10) | 46.94 (11.95) | 44.52 (11.20) | <.001 | <.001 |
| Suicidal behaviors, No (%) | |||||||
| Suicide attempt | 161 (1.5) | 43 (1.1) | 42 (1.6) | 57 (2.1) | 19 (1.7) | .004 | .16 |
| Suicide ideation | 1308 (12.5) | 515 (12.6) | 348 (13.1) | 318 (12.0) | 127 (11.4) | .45 | >.99 |
| Cognitive outcomes | |||||||
| Crystallized intelligence | |||||||
| Picture vocabulary | 52.34 (11.02) | 53.60 (11.45) | 51.62 (10.89) | 50.91 (10.11) | 52.89 (11.23) | <.001 | <.001 |
| Oral reading recognition | 49.37 (11.58) | 50.17 (11.74) | 49.30 (11.61) | 48.20 (11.05) | 49.35 (11.94) | <.001 | <.001 |
| Total score | 50.97 (11.28) | 52.23 (11.59) | 50.48 (11.18) | 49.42 (10.58) | 51.25 (11.48) | <.001 | <.001 |
| Fluid intelligence | |||||||
| Flanker inhibitory control | 46.06 (9.18) | 46.37 (9.36) | 45.38 (8.90) | 45.99 (8.94) | 46.78 (9.63) | <.001 | <.001 |
| List-sorting working memory | 49.49 (9.95) | 50.13 (9.73) | 49.49 (9.49) | 48.60 (10.36) | 49.29 (10.68) | <.001 | <.001 |
| Dimensional change card sort | 47.51 (9.69) | 48.83 (10.44) | 47.12 (9.23) | 45.98 (8.72) | 47.27 (9.44) | <.001 | <.001 |
| Pattern comparison processing speed | 45.42 (14.27) | 46.82 (14.28) | 44.56 (13.69) | 43.76 (14.58) | 46.30 (14.37) | <.001 | <.001 |
| Picture sequence memory | 49.56 (11.04) | 49.84 (11.24) | 49.64 (10.83) | 48.93 (10.77) | 49.87 (11.34) | .009 | .10 |
| Total score | 45.87 (11.26) | 47.13 (11.67) | 45.16 (10.84) | 44.42 (10.75) | 46.46 (11.40) | <.001 | <.001 |
| Cognitive intelligence total score | 47.81 (11.27) | 49.40 (11.54) | 47.10 (10.91) | 45.90 (10.59) | 48.30 (11.81) | <.001 | <.001 |
| WISC-V matrix reasoning total score | 9.89 (2.97) | 10.39 (2.80) | 10.15 (2.87) | 8.99 (3.03) | 9.59 (3.16) | <.001 | <.001 |
| Physical health outcomes | |||||||
| General physical health | |||||||
| Days exercise ≥60 min in past 7 d | 3.52 (2.31) | 3.81 (2.22) | 3.64 (2.37) | 3.06 (2.33) | 3.23 (2.26) | <.001 | <.001 |
| BMI | 18.79 (4.23) | 17.96 (3.47) | 18.31 (3.91) | 20.08 (4.94) | 19.86 (4.70) | <.001 | <.001 |
| Sleep disorders scale | |||||||
| Disorders of initiating and maintaining sleep | 11.73 (3.72) | 11.41 (3.50) | 12.11 (4.03) | 12.13 (3.83) | 11.00 (3.22) | <.001 | <.001 |
| Sleep breathing disorders | 3.76 (1.24) | 3.61 (1.03) | 3.73 (1.21) | 4.00 (1.49) | 3.78 (1.28) | <.001 | <.001 |
| Disorders of arousal | 3.44 (0.92) | 3.42 (0.80) | 3.47 (0.96) | 3.48 (1.09) | 3.35 (0.75) | <.001 | .002 |
| Sleep-wake transition disorders | 8.18 (2.61) | 8.14 (2.49) | 8.29 (2.71) | 8.18 (2.73) | 8.05 (2.53) | .04 | .33 |
| Disorders of excessive somnolence | 6.94 (2.42) | 6.75 (2.15) | 7.05 (2.49) | 7.23 (2.80) | 6.65 (2.14) | <.001 | <.001 |
| Sleep hyperhidrosis | 2.44 (1.19) | 2.38 (1.03) | 2.46 (1.25) | 2.52 (1.32) | 2.46 (1.25) | <.001 | <.001 |
| Total score | 36.48 (8.19) | 35.72 (7.14) | 37.11 (8.71) | 37.55 (9.25) | 35.28 (7.32) | <.001 | <.001 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CBCL, Child Behavior Checklist; WISC-V, Wechsler Intelligence Scale for Children.
Pattern 1, affluent community; pattern 2, high-stigma environment; pattern 3, high socioeconomic deprivation; pattern 4, high crime and drug sales, low education, high population density.
Figure 3. Associations Between the Identified Social Determinants of Health (SDOH) Patterns and Mental Health and Suicidal Behavior Outcomes of Children.

Child mental health outcomes were measured based on Child Behavior Checklist (CBCL) symptom scales (continuous)36,37 and self-reported suicidal behaviors using the self-administered computerized version of the Kiddie Schedule for Affective Disorders and Schizophrenia for DSM-5 (Lifetime Version).40 A higher value on a CBCL symptom scale indicates worse mental illness of the child. For continuous outcomes (ie, CBCL symptom scales), β (95% CI) and P values were estimated based on linear mixed-effects regression analyses, adjusting for baseline age, sex, and race and ethnicity and including a random-effects term to account for within-site clustering. For binary outcomes (ie, suicidal behaviors), β (95% CI) and P values were estimated based on mixed-effects logistic regressions analyses, adjusting for baseline age, sex, and race and ethnicity and including a random-effects term to account for within-site clustering. P values can be found in eTable 3 in Supplement 1.
Specifically, children living in SDOH pattern 3 had the most severe internalizing problems (β = 0.75; 95% CI, 0.14-1.37; P = .02), externalizing problems (β = 1.43; 95% CI, 0.83-2.02; P < .001), social problems (β = 0.63; 95% CI, 0.36-0.90; P < .001), and mental health problems (ie, CBCL total score: β = 1.16; 95% CI, 0.50-1.81; P < .001) relative to the other 3 SDOH patterns (Figure 3; eTable 3 in Supplement 1). In addition, SDOH pattern 3 was associated with children’s poorer cognitive performance (Figure 4; eTable 3 in Supplement 1), including lower crystallized intelligence (β = −1.60; 95% CI, −2.27 to −0.92; P < .001), fluid intelligence (β = −1.84, 95% CI, −2.52 to −1.16; P < .001), cognitive intelligence total score (β = −2.08; 95% CI, −2.75 to −1.41; P < .001), and WISC-V reasoning score (β = −0.56; 95% CI, −0.73 to −0.40; P < .001). Furthermore, these children were the least active, as evidenced by a lower probability of exercising 60 minutes in the past 7 days (β = −0.33; 95% CI, −0.46 to −0.20; P < .001), a higher BMI (β = 1.01; 95% CI, 0.77-1.25; P < .001), and overall sleep disorder problems (β = 0.77; 95% CI, 0.29-1.25; P = .002) (eFigure 11 and eTable 3 in Supplement 1).
Figure 4. Associations Between the Identified Social Determinants of Health (SDOH) Patterns and Cognitive Outcomes of Children.

Cognitive intelligence total score was calculated as the summation of crystallized intelligence and fluid intelligence scores for children. For each score, a higher value indicates better cognitive health of the child. For continuous outcomes (ie, CBCL symptom scales), β (95% CI) and P values were estimated based on linear mixed-effects regression analyses, adjusting for baseline age, sex, and race and ethnicity and including a random-effects term to account for within-site clustering. For binary outcomes (ie, suicidal behaviors), β (95% CI) and P values were estimated based on mixed-effects logistic regressions analyses, adjusting for baseline age, sex, and race and ethnicity and including a random-effects term to account for within-site clustering. P values can be found in eTable 3 in Supplement 1.
Conversely, children residing in SDOH pattern 1 (affluent communities) had better developmental outcomes, including fewer mental health issues, fewer suicide attempts, higher cognitive scores, and better physical health (Figure 3, Figure 4; eFigure 11 and eTable 3 in Supplement 1). After accounting for covariates, SDOH pattern 1 was associated with fewer internalizing problems (β = −0.71; 95% CI, −1.26 to −0.15; P = .01), externalizing problems (β = −1.39; 95% CI, −1.92 to −0.85; P < .001), social problems (β = −0.53; 95% CI, −0.77 to −0.29; P < .001), thought problems (β = −0.44; 95% CI, −0.75 to −0.13; P = .005), attention problems (β = −0.36; 95% CI, −0.68 to −0.04; P = .03), and overall mental health problems (β = −1.27; 95% CI, −1.86 to −0.68; P < .001) and a lower likelihood of suicide attempts (β = −0.39; 95% CI, −0.76 to −0.02; P = .04) (Figure 3; eTable 3 in Supplement 1). Cognitively, children in SDOH pattern 1 showed the best cognitive performances (Figure 4), including crystallized intelligence (β = 2.23; 95% CI, 1.62-2.84; P < .001), fluid intelligence (β = 2.22; 95% CI, 1.62-2.83; P < .001), cognitive intelligence total score (β = 2.72; 95% CI, 2.11-3.33; P < .001), and WISC-V reasoning score (β = 0.62; 95% CI, 0.46-0.77; P < .001). Physically, children in SDOH pattern 1 engaged in more 60-minute exercise (β = 0.31; 95% CI, 0.19-0.42; P < .001), had lower BMIs (β = −0.97; 95% CI, −1.19 to −0.76; P < .001), and had a lower sleep disorders total score (β = −0.71; 95% CI, −1.14 to −0.28; P < .001) (eFigure 11 and eTable 3 in Supplement 1).
Children living in a pattern 2 (high stigma) or pattern 3 (high crime and drug sales, low education, and high population density) environment exhibited lower cognitive abilities (SDOH pattern 2, cognitive intelligence total score: β = −1.11 [95% CI, −1.82 to −0.41; P = .002]; SDOH pattern 4, WISC-V score: β = −0.47 [95% CI, −0.79 to −0.15; P = .005]) relative to the other patterns (Figure 4), with children in SDOH pattern 4 also showing lower levels of physical activity (β = −0.22; 95% CI, −0.45 to 0.01; P = .06), high BMI (β = 1.01; 95% CI, 0.54-1.47; P < .001), and worse sleep quality (β = −0.93; 95% CI, −1.83 to −0.02; P = .046) than the other 3 SDOH patterns (eFigure 11 and eTable 3 in Supplement 1).
Discussion
Our cohort study used machine learning techniques to identify multifaceted SDOH patterns from a wide spectrum of 84 population-level SDOH indicators and estimated their associations with child development. Children in areas of high socioeconomic deprivation experienced the worst developmental outcomes, while those living in affluent areas reported better mental health, cognitive, and physical health outcomes. Additionally, children residing in high-stigma environments and areas characterized by higher crime rates and drug sales, lower education attainment, and higher population density had lower cognitive performance (cognitive intelligence, reasoning scores), higher BMI, and more sleep disorders, underscoring the association of heterogeneous outcomes of SDOH with child development.
Our approach transcends the traditional scales or single-index methods that predominate in the literature but have been incapable of capturing the interconnected and multidimensional SDOH and associating them with specific health and developmental outcomes. We estimated the collective influence of co-occurring SDOH patterns on child development, setting a foundation for more precise, targeted health care policy planning and implementation.55
Our SDOH findings reflect distinct racial and ethnic differences. White children were overrepresented in affluent and high-stigma environments, whereas Black and Hispanic children were overrepresented in socioeconomically deprived areas, derived from discriminatory housing policies and resource accessibility56 and reflecting systemic racism and socioeconomic marginalization that restrict Black and Hispanic children’s access to opportunities.57 The higher rates of crime, low education, and dense populations in areas populated by Hispanic and Black residents may influence the mental, cognitive, and physical health of these children, as suggested by prior studies.58,59,60 These findings suggest, but are not proof, that socioeconomic deprivation may have a detrimental association with many child developmental outcomes.61 Factors such as restricted access to educational resources and cognitive stimulation, poor nutrition, limited opportunities for physical activity, and exposure to environmental stressors, may potentially disrupt sleep patterns,62,63,64,65 worsen mental health, and increase the risk of suicide attempts.66 Compared with other SDOH patterns, children living in highly stigmatizing environments exhibited lower cognitive abilities consistent with the possibility that chronic stress67 (which alters hypothalamic-pituitary-adrenal axis function and increases cortisol levels68), limited access to quality education,69 and inadequate health care and nutrition can negatively affect brain development and cognitive function.70
Children living in areas characterized by high crime and drug sales, low education, and high population density were observed to exhibit both lower cognitive function and insufficient physical activity compared with the other SDOH patterns. The chronic stress in these communities,71,72 coupled with limited access to basic resources,73 can hinder cognitive development and discourage physical activity, deteriorating overall cognition and activity levels.
Strengths and Limitations
The strengths of this study lie in the use of a data-driven approach, facilitating the identification of nuanced high-dimensional patterns of SDOH and their varied associations with child development. Our measures of child developmental outcomes are comprehensive and consistent with the gold standards of child mental, cognitive, and physical health assessments. We focused on linking area-based SDOH to individual-level outcomes, thereby minimizing the likelihood of ecological fallacy.74,75,76,77
However, the study also has limitations. First, outcome measures were self-reported and may be biased by underreporting or discrepancies in reports by the child or parents.78 Second, the ABCD Study sample is not nationally representative, covering 17 states across 21 study sites. Consequently, our results may not apply to all US children. Third, our SDOH data, constrained by the available ABCD-linked external data, may not cover all potential SDOH variables. However, the selection of the 84 SDOH variables is theoretically79,80,81,82 and empirically80 sound. Additionally, we focused on bias and stigma calculated using objective state-level indicators of social policies and prejudicial attitudes, with the goal of capturing broad societal and institutional biases. Such measures were not intended to consider individual-level bias derived from self-reported discrimination. Consequently, we may have overlooked influences arising from personal bias experiences and their interaction with structural factors. Fourth, there were missing data for some variables in the clustering models. Despite these limitations, our study contributes valuable insights and prompts further investigation into the role of SDOH in children’s health outcomes.
Conclusions
In this cohort study, we derived 4 SDOH patterns that quantify and express multidimensional SDOH and then linked these patterns to differences in child development and health outcomes. By linking specific outcomes to specific SDOH patterns, our findings emphasize the need for targeted interventions to tackle potential causes of adverse health and developmental outcomes, especially in children with greater socioeconomic deprivation. A holistic approach involving efforts of policymakers and health care practitioners is crucial to nurturing child resilience and promoting health equity.
eMethods 1. Social Determinants of Health Variables
eMethods 2. Detailed Measures of Study Outcomes
eMethods 3. Determination of the Optimal Cluster Number
eMethods 4. Sensitivity Analyses
eResults 1. Determination of the Optimal Number of Clusters (ie, SDOH Patterns) in the Primary Analysis
eResults 2. Sensitivity Analysis to Validate the Stability and Reproducibility of SDOH Patterns
eReferences
eFigure 1. An Illustration of Missing Values in the Child × SDOH Variable Matrix
eFigure 2. Dendrogram for SDOH Pattern Identification in the Primary Analysis
eFigure 3. Visualization of SDOH Patterns in 2D t-SNE Space
eFigure 4. Characteristics of the Identified Social Determinants of Health (SDOH) Patterns (With Detailed Information)
eFigure 5. Association Between SDOH Patterns With Marijuana State Law Types and Census Tract Urban Classification
eFigure 6. Results of Sensitivity Analysis to Dropped Samples Due to Missing Values
eFigure 7. Results of Sensitivity Analysis at the Neighborhood Level
eFigure 8. Results of Sensitivity Analysis to Include Data Samples
eFigure 9. Forest Plot Showing Associations Between the Identified Social Determinants of Health (SDOH) Patterns and Mental Health and Suicidal Behavior Outcomes of Children at 1-Year Follow-Up
eFigure 10. Forest Plot Showing Associations Between the Identified Social Determinants of Health (SDOH) Patterns and Mental Health and Suicidal Behavior Outcomes of children at 2-Year Follow-Up
eFigure 11. Forest Plot Showing Associations Between the Identified Social Determinants of Health (SDOH) Patterns and Physical Health Outcomes of Children
eTable 1. The SDOH Variables Used for SDoH Pattern Identification
eTable 2. Characteristics in SDOH Variables by the Identified SDOH Patterns
eTable 3. P Values of Associations Between the Identified SDOH Patterns and Mental Health, Cognition, and Physical Health Outcomes
Data Sharing Statement
References
- 1.A conceptual framework for action on the social determinants of health. World Health Organization ; 2010. Accessed February 22, 2023. https://www.who.int/publications/i/item/9789241500852
- 2.Social determinants of health at CDC. Centers for Disease Control and Prevention ; 2022. Accessed February 22, 2023. https://www.cdc.gov/about/sdoh/index.html
- 3.Murray CJL, Atkinson C, Bhalla K, et al. ; U.S. Burden of Disease Collaborators . The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591-608. doi: 10.1001/jama.2013.13805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kolak M, Bhatt J, Park YH, Padrón NA, Molefe A. Quantification of neighborhood-level social determinants of health in the continental United States. JAMA Netw Open. 2020;3(1):e1919928. doi: 10.1001/jamanetworkopen.2019.19928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marmot M. Social determinants of health inequalities. Lancet. 2005;365(9464):1099-1104. doi: 10.1016/S0140-6736(05)71146-6 [DOI] [PubMed] [Google Scholar]
- 6.Bradley RH, Corwyn RF. Socioeconomic status and child development. Annu Rev Psychol. 2002;53:371-399. doi: 10.1146/annurev.psych.53.100901.135233 [DOI] [PubMed] [Google Scholar]
- 7.McLoyd VC. Socioeconomic disadvantage and child development. Am Psychol. 1998;53(2):185-204. doi: 10.1037/0003-066X.53.2.185 [DOI] [PubMed] [Google Scholar]
- 8.Duncan GJ, Brooks-Gunn J, Klebanov PK. Economic deprivation and early childhood development. Child Dev. 1994;65(2 spec No.):296-318. doi: 10.2307/1131385 [DOI] [PubMed] [Google Scholar]
- 9.Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. Pediatrics. 2010;125(1):75-81. doi: 10.1542/peds.2008-2598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodman E, Slap GB, Huang B. The public health impact of socioeconomic status on adolescent depression and obesity. Am J Public Health. 2003;93(11):1844-1850. doi: 10.2105/AJPH.93.11.1844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tracy M, Zimmerman FJ, Galea S, McCauley E, Stoep AV. What explains the relation between family poverty and childhood depressive symptoms? J Psychiatr Res. 2008;42(14):1163-1175. doi: 10.1016/j.jpsychires.2008.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wadsworth ME, Achenbach TM. Explaining the link between low socioeconomic status and psychopathology: testing two mechanisms of the social causation hypothesis. J Consult Clin Psychol. 2005;73(6):1146-1153. doi: 10.1037/0022-006X.73.6.1146 [DOI] [PubMed] [Google Scholar]
- 13.Steelesmith DL, Fontanella CA, Campo JV, Bridge JA, Warren KL, Root ED. Contextual factors associated with county-level suicide rates in the United States, 1999 to 2016. JAMA Netw Open. 2019;2(9):e1910936. doi: 10.1001/jamanetworkopen.2019.10936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suk R, Hong YR, Wasserman RM, et al. Analysis of suicide after cancer diagnosis by US county-level income and rural vs urban designation, 2000-2016. JAMA Netw Open. 2021;4(10):e2129913. doi: 10.1001/jamanetworkopen.2021.29913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kandula S, Martinex-Alés G, Rutherford C, et al. County-level estimates of suicide mortality in the USA: a modelling study. Lancet Public Health. 2023;8(3):e184-e193. doi: 10.1016/S2468-2667(22)00290-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amezcua L, Rivera VM, Vazquez TC, Baezconde-Garbanati L, Langer-Gould A. Health disparities, inequities, and social determinants of health in multiple sclerosis and related disorders in the US: a review. JAMA Neurol. 2021;78(12):1515-1524. doi: 10.1001/jamaneurol.2021.3416 [DOI] [PubMed] [Google Scholar]
- 17.Chen E, Martin AD, Matthews KA. Understanding health disparities: the role of race and socioeconomic status in children’s health. Am J Public Health. 2006;96(4):702-708. doi: 10.2105/AJPH.2004.048124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible—The Neighborhood Atlas. N Engl J Med. 2018;378(26):2456-2458. doi: 10.1056/NEJMp1802313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Flanagan BE, Gregory EW, Hallisey EJ, Heitgerd JL, Lewis B. A social vulnerability index for disaster management. J Homel Secur Emerg Manag. 2011;8(1): 0000102202154773551792. doi: 10.2202/1547-7355.1792 [DOI] [Google Scholar]
- 20.Chantarat T, Van Riper DC, Hardeman RR. The intricacy of structural racism measurement: a pilot development of a latent-class multidimensional measure. EClinicalMedicine. 2021;40:101092. doi: 10.1016/j.eclinm.2021.101092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chantarat T, Van Riper DC, Hardeman RR. Multidimensional structural racism predicts birth outcomes for Black and White Minnesotans. Health Serv Res. 2022;57(3):448-457. doi: 10.1111/1475-6773.13976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Venkataramani AS, Bair EF, O’Brien RL, Tsai AC. Association between automotive assembly plant closures and opioid overdose mortality in the United States: a difference-in-differences analysis. JAMA Intern Med. 2020;180(2):254-262. doi: 10.1001/jamainternmed.2019.5686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duncan SC, Duncan TE, Strycker LA. A multilevel analysis of neighborhood context and youth alcohol and drug problems. Prev Sci. 2002;3(2):125-133. doi: 10.1023/A:1015483317310 [DOI] [PubMed] [Google Scholar]
- 24.Feldstein Ewing SW, Chang L, Cottler LB, Tapert SF, Dowling GJ, Brown SA. Approaching retention within the ABCD study. Dev Cogn Neurosci. 2018;32:130-137. doi: 10.1016/j.dcn.2017.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.ABCD Research Consortium . Adolescent Brain Cognitive Development Study (ABCD)—annual release 4.0 #1299. National Institute of Mental Health Data Archive. Deposited October 2021.
- 26.Clark DB, Fisher CB, Bookheimer S, et al. Biomedical ethics and clinical oversight in multisite observational neuroimaging studies with children and adolescents: the ABCD experience. Dev Cogn Neurosci. 2018;32:143-154. doi: 10.1016/j.dcn.2017.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fan CC, Marshall A, Smolker H, et al. Adolescent Brain Cognitive Development (ABCD) study Linked External Data (LED): protocol and practices for geocoding and assignment of environmental data. Dev Cogn Neurosci. 2021;52:101030. doi: 10.1016/j.dcn.2021.101030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Healthy People 2030: social determinants of health. US Department of Health and Human Services . Accessed February 22, 2023. https://health.gov/healthypeople/priority-areas/social-determinants-health (2023).
- 29.About SDOH in healthcare. Agency for Healthcare Research and Quality . Accessed February 22, 2023. https://www.ahrq.gov/sdoh/about.html (2023).
- 30.Hatzenbuehler ML, Weissman DG, McKetta S, et al. Smaller hippocampal volume among Black and Latinx youth living in high-stigma contexts. J Am Acad Child Adolesc Psychiatry. 2022;61(6):809-819. doi: 10.1016/j.jaac.2021.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chetty R, Friedman JN, Hendren N, Jones MR, Porter SR. The opportunity atlas: mapping the childhood roots of social mobility. National Bureau of Economic Research ; 2018. Accessed February 22, 2023. https://www.nber.org/papers/w25147 doi: 10.3386/w25147 [DOI]
- 32.Acevedo-Garcia D, McArdle N, Hardy EF, et al. The child opportunity index: improving collaboration between community development and public health. Health Aff (Millwood). 2014;33(11):1948-1957. doi: 10.1377/hlthaff.2014.0679 [DOI] [PubMed] [Google Scholar]
- 33.Singh GK, Siahpush M. Increasing inequalities in all-cause and cardiovascular mortality among US adults aged 25-64 years by area socioeconomic status, 1969-1998. Int J Epidemiol. 2002;31(3):600-613. doi: 10.1093/ije/31.3.600 [DOI] [PubMed] [Google Scholar]
- 34.Singh GK. Area deprivation and widening inequalities in US mortality, 1969-1998. Am J Public Health. 2003;93(7):1137-1143. doi: 10.2105/AJPH.93.7.1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singh GK, Azuine RE, Siahpush M, Kogan MD. All-cause and cause-specific mortality among US youth: socioeconomic and rural-urban disparities and international patterns. J Urban Health. 2013;90(3):388-405. doi: 10.1007/s11524-012-9744-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. ASEBA; 2001. [Google Scholar]
- 37.Barch DM, Albaugh MD, Avenevoli S, et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: rationale and description. Dev Cogn Neurosci. 2018;32:55-66. doi: 10.1016/j.dcn.2017.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Achenbach TM. The Achenbach System of Empirically Based Assessment (ASEBA): Development, Findings, Theory, and Applications. University of Vermont, Research Center for Children, Youth, & Families; 2009. [Google Scholar]
- 39.Karcher NR, Barch DM. The ABCD Study: understanding the development of risk for mental and physical health outcomes. Neuropsychopharmacology. 2021;46(1):131-142. doi: 10.1038/s41386-020-0736-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barch DM, Albaugh MD, Baskin-Sommers A, et al. Demographic and mental health assessments in the adolescent brain and cognitive development study: updates and age-related trajectories. Dev Cogn Neurosci. 2021;52:101031. doi: 10.1016/j.dcn.2021.101031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weintraub S, Bauer PJ, Zelazo PD, et al. I. NIH Toolbox Cognition Battery (CB): introduction and pediatric data. Monogr Soc Res Child Dev. 2013;78(4):1-15. doi: 10.1111/mono.12031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gershon RC, Wagster MV, Hendrie HC, Fox NA, Cook KF, Nowinski CJ. NIH toolbox for assessment of neurological and behavioral function. Neurology. 2013;80(11)(suppl 3):S2-S6. doi: 10.1212/WNL.0b013e3182872e5f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bleck TP, Nowinski CJ, Gershon R, Koroshetz WJ. What is the NIH Toolbox, and what will it mean to neurology? Neurology. 2013;80:874-875. [DOI] [PubMed] [Google Scholar]
- 44.Hodes RJ, Insel TR, Landis SC; NIH Blueprint for Neuroscience Research . The NIH Toolbox: setting a standard for biomedical research. Neurology. 2013;80(11)(suppl 3):S1. doi: 10.1212/WNL.0b013e3182872e90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zelazo PD, Anderson JE, Richler J, Wallner-Allen K, Beaumont JL, Weintraub S. II. NIH Toolbox Cognition Battery (CB): measuring executive function and attention. Monogr Soc Res Child Dev. 2013;78(4):16-33. doi: 10.1111/mono.12032 [DOI] [PubMed] [Google Scholar]
- 46.Weintraub S, Dikmen SS, Heaton RK, et al. Cognition assessment using the NIH Toolbox. Neurology. 2013;80(11)(suppl 3):S54-S64. doi: 10.1212/WNL.0b013e3182872ded [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Luciana M, Bjork JM, Nagel BJ, et al. Adolescent neurocognitive development and impacts of substance use: overview of the adolescent brain cognitive development (ABCD) baseline neurocognition battery. Dev Cogn Neurosci. 2018;32:67-79. doi: 10.1016/j.dcn.2018.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Heaton RK, Akshoomoff N, Tulsky D, et al. Reliability and validity of composite scores from the NIH Toolbox Cognition Battery in adults. J Int Neuropsychol Soc. 2014;20(6):588-598. doi: 10.1017/S1355617714000241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gershon RC, Slotkin J, Manly JJ, et al. IV. NIH Toolbox Cognition Battery (CB): measuring language (vocabulary comprehension and reading decoding). Monogr Soc Res Child Dev. 2013;78(4):49-69. doi: 10.1111/mono.12034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wechsler D. Wechsler Intelligence Scale for Children–Fifth Edition (WISC-V). Pearson; 2014. [Google Scholar]
- 51.Bruni O, Ottaviano S, Guidetti V, et al. The Sleep Disturbance Scale for Children (SDSC). construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5(4):251-261. doi: 10.1111/j.1365-2869.1996.00251.x [DOI] [PubMed] [Google Scholar]
- 52.Li P, Stuart EA, Allison DB. Multiple imputation: a flexible tool for handling missing data. JAMA. 2015;314(18):1966-1967. doi: 10.1001/jama.2015.15281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Charrad M, Ghazzali N, Boiteau V, Niknafs A. NbClust: an R package for determining the relevant number of clusters in a data set. J Stat Softw. 2014;61:1-36. doi: 10.18637/jss.v061.i06 [DOI] [Google Scholar]
- 54.Van der Maaten L, Hinton G. Visualizing data using t-SNE. J Mach Learn Res. 2008;9:2579-2605. [Google Scholar]
- 55.Zhang Y, Khullar D, Wang F, et al. Socioeconomic variation in characteristics, outcomes, and healthcare utilization of COVID-19 patients in New York City. PLoS One. 2021;16(7):e0255171. doi: 10.1371/journal.pone.0255171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ejlskov L, Antonsen S, Wulff JN, et al. Multilevel interactions between family and neighbourhood socioeconomic indices in childhood and later risks of self-harm and violent criminality in Denmark: a national cohort study. Lancet Public Health. 2023;8(2):e99-e108. doi: 10.1016/S2468-2667(22)00292-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sanders M, Winston J, Rochester SE. Most Black children live in neighborhoods that lack amenities associated with child well-being. Child Trends blog. February 24, 2023. Accessed February 22, 2023. https://www.childtrends.org/blog/most-black-children-live-in-neighborhoods-that-lack-amenities-associated-with-child-well-being
- 58.Deighton J, Lereya ST, Casey P, Patalay P, Humphrey N, Wolpert M. Prevalence of mental health problems in schools: poverty and other risk factors among 28 000 adolescents in England. Br J Psychiatry. 2019;215(3):565-567. doi: 10.1192/bjp.2019.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Patalay P, Moulton V, Goodman A, Ploubidis GB. Cross-domain symptom development typologies and their antecedents: results from the UK Millennium Cohort Study. J Am Acad Child Adolesc Psychiatry. 2017;56(9):765-776.e2. doi: 10.1016/j.jaac.2017.06.009 [DOI] [PubMed] [Google Scholar]
- 60.Ziebold C, Evans-Lacko S, Rezende Andrade MC, et al. Childhood poverty and mental health disorders in early adulthood: evidence from a Brazilian cohort study. Eur Child Adolesc Psychiatry. 2023;32(5):903-914. doi: 10.1007/s00787-021-01923-2 [DOI] [PubMed] [Google Scholar]
- 61.Mani A, Mullainathan S, Shafir E, Zhao J. Poverty impedes cognitive function. Science. 2013;341(6149):976-980. doi: 10.1126/science.1238041 [DOI] [PubMed] [Google Scholar]
- 62.Basner M, McGuire S. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and effects on sleep. Int J Environ Res Public Health. 2018;15(3):519. doi: 10.3390/ijerph15030519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Duncan GJ, Magnuson K, Votruba-Drzal E. Moving beyond correlations in assessing the consequences of poverty. Annu Rev Psychol. 2017;68:413-434. doi: 10.1146/annurev-psych-010416-044224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Henry A, Katsoulis M, Masi S, et al. The relationship between sleep duration, cognition and dementia: a Mendelian randomization study. Int J Epidemiol. 2019;48(3):849-860. doi: 10.1093/ije/dyz071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lê-Scherban F, Wang X, Boyle-Steed KH, Pachter LM. Intergenerational associations of parent adverse childhood experiences and child health outcomes. Pediatrics. 2018;141(6):141. doi: 10.1542/peds.2017-4274 [DOI] [PubMed] [Google Scholar]
- 66.Li Z, Page A, Martin G, Taylor R. Attributable risk of psychiatric and socio-economic factors for suicide from individual-level, population-based studies: a systematic review. Soc Sci Med. 2011;72(4):608-616. doi: 10.1016/j.socscimed.2010.11.008 [DOI] [PubMed] [Google Scholar]
- 67.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20-47. doi: 10.1007/s10865-008-9185-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10(6):434-445. doi: 10.1038/nrn2639 [DOI] [PubMed] [Google Scholar]
- 69.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453-1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 70.Lynch-Smith M, Bleich SN, Sommers BD. New federal efforts to address food and nutrition insecurity. JAMA Health Forum. 2022;3(11):e224914. [DOI] [PubMed] [Google Scholar]
- 71.Rakesh D, Zalesky A, Whittle S. Assessment of parent income and education, neighborhood disadvantage, and child brain structure. JAMA Netw Open. 2022;5(8):e2226208. doi: 10.1001/jamanetworkopen.2022.26208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Taylor MJ, Freeman D, Lundström S, Larsson H, Ronald A. Heritability of psychotic experiences in adolescents and interaction with environmental risk. JAMA Psychiatry. 2022;79(9):889-897. doi: 10.1001/jamapsychiatry.2022.1947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Berger N, Lewis D, Quartagno M, Njagi EN, Cummins S. Longitudinal associations between perceptions of the neighbourhood environment and physical activity in adolescents: evidence from the Olympic Regeneration in East London (ORiEL) study. BMC Public Health. 2019;19(1):1760. doi: 10.1186/s12889-019-8003-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Idrovo AJ. Three criteria for ecological fallacy. Environ Health Perspect. 2011;119(8):A332. doi: 10.1289/ehp.1103768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Piantadosi S, Byar DP, Green SB. The ecological fallacy. Am J Epidemiol. 1988;127(5):893-904. doi: 10.1093/oxfordjournals.aje.a114892 [DOI] [PubMed] [Google Scholar]
- 76.Schwartz S. The fallacy of the ecological fallacy: the potential misuse of a concept and the consequences. Am J Public Health. 1994;84(5):819-824. doi: 10.2105/AJPH.84.5.819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sedgwick P. Understanding the ecological fallacy. BMJ. 2015;351:h4773. doi: 10.1136/bmj.h4773 [DOI] [PubMed] [Google Scholar]
- 78.Janiri D, Doucet GE, Pompili M, et al. Risk and protective factors for childhood suicidality: a US population-based study. Lancet Psychiatry. 2020;7(4):317-326. doi: 10.1016/S2215-0366(20)30049-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Social determinants of health. World Health Organization; 2022. Accessed February 22, 2023. https://www.who.int/health-topics/social-determinants-of-health [Google Scholar]
- 80.Xiao Y, Yip PSF, Pathak J, Mann JJ. Association of social determinants of health and vaccinations with child mental health during the COVID-19 pandemic in the US. JAMA Psychiatry. 2022;79(6):610-621. doi: 10.1001/jamapsychiatry.2022.0818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hammond G, Joynt Maddox KE. A theoretical framework for clinical implementation of social determinants of health. JAMA Cardiol. 2019;4(12):1189-1190. doi: 10.1001/jamacardio.2019.3805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shim RS, Compton MT. Addressing the social determinants of mental health: if not now, when? if not us, who? Psychiatr Serv. 2018;69(8):844-846. doi: 10.1176/appi.ps.201800060 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods 1. Social Determinants of Health Variables
eMethods 2. Detailed Measures of Study Outcomes
eMethods 3. Determination of the Optimal Cluster Number
eMethods 4. Sensitivity Analyses
eResults 1. Determination of the Optimal Number of Clusters (ie, SDOH Patterns) in the Primary Analysis
eResults 2. Sensitivity Analysis to Validate the Stability and Reproducibility of SDOH Patterns
eReferences
eFigure 1. An Illustration of Missing Values in the Child × SDOH Variable Matrix
eFigure 2. Dendrogram for SDOH Pattern Identification in the Primary Analysis
eFigure 3. Visualization of SDOH Patterns in 2D t-SNE Space
eFigure 4. Characteristics of the Identified Social Determinants of Health (SDOH) Patterns (With Detailed Information)
eFigure 5. Association Between SDOH Patterns With Marijuana State Law Types and Census Tract Urban Classification
eFigure 6. Results of Sensitivity Analysis to Dropped Samples Due to Missing Values
eFigure 7. Results of Sensitivity Analysis at the Neighborhood Level
eFigure 8. Results of Sensitivity Analysis to Include Data Samples
eFigure 9. Forest Plot Showing Associations Between the Identified Social Determinants of Health (SDOH) Patterns and Mental Health and Suicidal Behavior Outcomes of Children at 1-Year Follow-Up
eFigure 10. Forest Plot Showing Associations Between the Identified Social Determinants of Health (SDOH) Patterns and Mental Health and Suicidal Behavior Outcomes of children at 2-Year Follow-Up
eFigure 11. Forest Plot Showing Associations Between the Identified Social Determinants of Health (SDOH) Patterns and Physical Health Outcomes of Children
eTable 1. The SDOH Variables Used for SDoH Pattern Identification
eTable 2. Characteristics in SDOH Variables by the Identified SDOH Patterns
eTable 3. P Values of Associations Between the Identified SDOH Patterns and Mental Health, Cognition, and Physical Health Outcomes
Data Sharing Statement