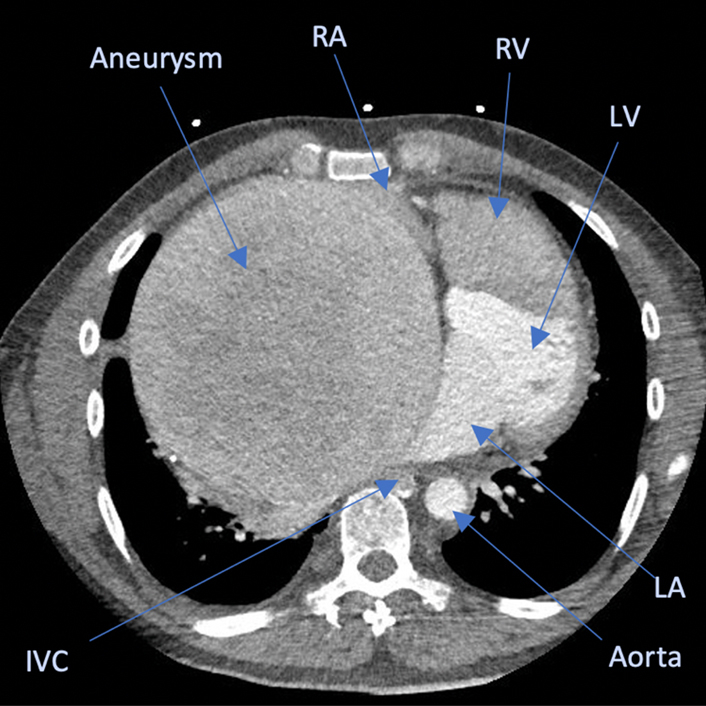
CTA image of the coronary artery fistula aneurysm compressing all adjacent structures.
Central Message.
First reporting of a hybrid Amplatz plug coronary fistula closure followed by surgical excision of a gigantic CAVF aneurysm.
Case Presentation
A 37-year-old man presented with supraventricular tachycardia, exercise intolerance, and lower limb edema. He reported a 2-year history of dyspnea, palpitations, and signs of superior vena cava syndrome. Transthoracic echocardiography and computed tomography angiography diagnosed a large coronary artery fistula. It originated from the proximal left circumflex coronary artery traveling through the transverse sinus behind the main pulmonary artery and aorta, into a gigantic aneurysm within the walls of the secundum septum embryonic folding (splaying the left and right atriums) and draining into the right atrium (RA) (Video 1). A 15-cm fistula aneurysm caused almost complete obstruction of the superior vena cava, inferior vena cava, right pulmonary veins, and right pulmonary artery (Figure 1, A). The Research Ethics Board of Nova Scotia Health approved the study protocol and publication of data (1,029,235; April 19, 2023). The patient provided informed written consent for the publication of the study data.
Figure 1.
A, Computed tomography angiography (CTA) image of the coronary artery fistula aneurysm. The large structure occupying most of the right side of the thorax is the giant aneurysm arising from the left circumflex coronary artery fistula and it is compressing the adjacent structures. B, Follow-up CTA 8 months postoperatively shows resolution of all obstruction and normalization of heart size. C and D, Images of the coronary catheterization before (C) and after (D) Amplatz device implantation. The perfusion of left coronary branches improved after Amplatz device implantation. The device is visualized occluding the fistula. RA, Right atrium; RV, right ventricle; LV, left ventricle; IVC, inferior vena cava; LA, left atrium.
Intervention
A hybrid approach was utilized during the index hospitalization by first occluding the fistula (Amplatz plug) and subsequently resecting the aneurysm on cardiopulmonary bypass (CPB), to ensure adequate myocardial protection. Using a telescoping technique,1 the plug was deployed proximal to the fistula aneurysm, angiographically occluding flow through the fistula. This immediately improved left-sided coronary artery filling (Figure 1, C and D) and decreased the central venous pressure (38-24 mm Hg).
A sternotomy was immediately performed on CPB via peripheral cannulation because the aneurysm was adjacent to the sternum. Innominate vein cannulation was added for upper body drainage. Successful antegrade cardioplegic arrest occurred without the need to manually occlude the fistula (plug resistance to flow). The fistula aneurysm was opened between the superior vena cava and aorta. All accessible aneurysmal free wall tissue was resected. The proximal fistula was identified, and the 2-cm orifice (Figure 2, B) primarily oversewed with the Amplatz still in situ. The 5-mm aneurysm exit site into the RA (Figure 2, C) was primarily closed. The aneurysmal wall attached to the RA and left atrium aspects of the splayed interatrial septum was reapproximated with interrupted sutures. The patient was weaned off CPB with normal biventricular function. One week later, reoperation was needed to evacuate an 8-cm thrombus in the interatrial secundum septum. The space was successfully reobliterated with bioglue. Due to the large remaining proximal fistula inlet, our institutional approach was to discharge the patient on warfarin and acetylsalicylic acid indefinitely for embolic prophylaxis. Eight-month postoperative computed tomography angiography showed resolution of all obstruction and normalization of heart size. The patient was completely asymptomatic at follow-up.
Figure 2.
A, Image showing the aneurysm between the ascending aorta and the right atrium (RA). B, Image of the coronary fistula inlet occluded by the Amplatz device. C, Image shows the coronary fistula outlet into the right atrium. SVC, Superior vena cava.
Discussion
To our knowledge this is the first description of hybrid closure of coronary arteriovenous fistula (CAVF) with percutaneous closure to facilitate coronary protection and aneurysm resection during surgical intervention. CAVF is a rare abnormal communication between a coronary artery and adjacent vessels or cardiac chambers with an incidence of 0.2% to 1.2%.2 Eventually, CAVF can result in coronary/fistula aneurysm formation due to ongoing left-to-right shunting. Therapeutic interventions are indicated on presence of symptoms, significant left-to-right shunt, or coronary ischemia.3 Management goals are to stop the left-to-right shunting proximal to fistula aneurysms while ensuring unobstructed TIMI 3 coronary flow. Surgical ligation has been the standard for the treatment of CAVF. However, with technological advancements, interventional closure of fistulas that do not influence distal coronary perfusion has become the preferred strategy.4 Transcatheter therapy won't relieve compressive effects of coronary aneurysms.
The Achilles heel of surgical CAVF ligation is myocardial protection. Once CPB is initiated, the venous drainage results in negative pressure in the right-sided chambers, potentially accentuating coronary steal and myocardial ischemia. Unoccluded, the fistula will also steal cardioplegia, resulting in ineffective myocardial protection, even with retrograde cardioplegia. Therefore, we elected to occlude the proximal fistula percutaneously with the Amplatz plug before embarking on the surgical aneurysm resection in our patient, without the need of coronary artery bypass graft surgery as described by Iacona and colleagues.5 Once the plug was deployed, coronary flow to the left coronary artery normalized (Figure 1, D), allowing effective cardioplegic arrest. The plug was left in situ, creating a shorter remaining proximal fistula stump to communicate with the left coronary system.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Footnotes
Read at the 103rd Annual Meeting of The American Association for Thoracic Surgery, Los Angeles, California, May 6-9, 2023.
Supplementary Data
Coronary aneurysm computed tomography angiography video prerepair. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00280-8/fulltext.
References
- 1.Sumaya W., Horne D., Chen R., Elkhateeb O. Novel telescope anchoring technique for closure of gigantic coronary fistulae using 3-dimensional printing for planning. Cardiovasc Interv. 2022;15:896–897. doi: 10.1016/j.jcin.2022.01.024. [DOI] [PubMed] [Google Scholar]
- 2.Challoumas D., Pericleous A., Dimitrakaki I.A., Danelatos C., Dimitrakakis G. Coronary arteriovenous fistulae: a review. Int J Angiol. 2014;23:1–10. doi: 10.1055/s-0033-1349162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liberthson R.R., Sagar K., Berkoben J.P., Weintraub R.M., Levine F.H. Congenital coronary arteriovenous fistula. Report of 13 patients, review of the literature and delineation of management. Circulation. 1979;59:849–854. doi: 10.1161/01.cir.59.5.849. [DOI] [PubMed] [Google Scholar]
- 4.Ata Y., Turk T., Bicer M., Yalcin M., Ata F., Yavuz S. Coronary arteriovenous fistulas in the adults: natural history and management strategies. J Cardiothorac Surg. 2009;4:62. doi: 10.1186/1749-8090-4-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iacona G.M., Patel S., Bakaeen F.G., Ghandour H., Stewart R.D., Svensson L.G., et al. Surgery for aneurysmal coronary artery fistulas to the coronary sinus in adults: a case series. JACC Case Rep. 2022;4 doi: 10.1016/j.jaccas.2022.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Coronary aneurysm computed tomography angiography video prerepair. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00280-8/fulltext.




