Key Clinical Message
Proteus syndrome is a rare genetic disease characterized by an asymmetrical growth of individual parts of the body and has only been described in single cases. This patient presented with recurrent manifestations of a laryngeal and hypopharyngeal lymphangioma, which were treated with laser surgery, systemic therapy, and sclerotherapy. The reported data depict the diagnosis and treatment in the department of otorhinolaryngology, head and neck surgery of the university hospital Heidelberg from 2019 until May 2023. The recurrent endoscopy of the upper airway was performed using a flexible HD‐endoscope and the Visera Elite video tower from Olympus, Hamburg. The 29‐year old female patient initially presented in February 2019 with stridor and exertional dyspnea due to a lymphatic malformation of the left larynx and hypopharynx. In April 2019 there was no improvement by sclerotherapy with Picibanil, so that systemic therapy with the PIK3CA inhibitor alpelisib was initiated (03–07/2020) and discontinued due to a high side effect profile. In the course of 2021–2023, three microlaryngoscopies with laser surgical resection and renewed sclerotherapy of the lymphangioma with Picibanil were carried out due to fluctuating findings. After these interventions a stable disease could be established until May 2023. Laser surgical therapy is currently described as the therapy of choice in lymphangiomas in the head and neck region and also showed the highest effectiveness in our patient. In case of airway obstruction in particular, it can bring rapid symptom relief. Alternatively, and with a lower surgical risk, local improvements have been reported by sclerotherapy, which was less effective in the presented case. Rare syndromic diseases require multidisciplinary collaboration. In the case of laryngeal lymphangiomatosis, other treatment options should be considered in addition to surgical excision, especially in the case of recurrence.
Keywords: head and neck, larynx, laser surgery, lymphangiomatosis, Proteus syndrome, rare diseases
Initial laryngoscopy of February 2019: Submucous tumorous mass with punctum maximum at the left supraglottis, reaching to the midline and the postcricoid region on both sides and along the aryepiglottic fold on the left, partially obstructing the sinus piriformis on the left, but with equal mobility of the vocal folds with complete glottic closure, but supraglottic constriction during phonation.

1. BACKGROUND
Proteus syndrome is a very rare disease caused by mutations in components of the phosphatidylinositol‐3‐kinase (PI3K)‐AKT signaling cascade. The most common mosaic gene alterations in patients with Proteus syndrome are in AKT1. 1 Proteus syndrome is characterized by a disproportionate, asymmetric overgrowth in a mosaic pattern in affected patients. 2 Symptoms may include progressive skeletal or vascular malformations including lymphatic malformations, benign and malignant tumors as well as skin lesions or even deep vein thrombosis or pulmonary embolism. 2
Lymphatic malformations are rare cystic malformations that develop of the lymphatic system in localized regions of the body. They commonly present in the head and neck region, but isolated laryngeal manifestation is extremely uncommon. 3 , 4 Symptoms are similar to any laryngeal mass, including dysphonia and dyspnea. Therapeutic options in the head and neck region are radiofrequency ablation, laser surgery, sclerotherapy, and classic surgical therapy. 5 In case of airway obstruction in particular, laser surgical resection can bring rapid symptom relief. Alternatively, and with a lower surgical risk, improvement and healing has also been achieved by sclerotherapy. 6
So far, only about 200 cases of Proteus syndrome were reported in the literature. Treatment options are mostly symptomatic and remain individual to each patient. 7
We report the case of a 29‐year‐old female, who was diagnosed with Proteus syndrome and presented with recurrent manifestations of a laryngeal and hypopharyngeal lymphangioma, which were treated with laser surgery, systemic therapy, and sclerotherapy due to fluctuating findings. A stable disease could be established until May 2023 after several interventions.
2. METHODS
The present work is a case report of a female patient who presented to our consultation for the first time at the age of 29 years. The follow‐up since the initial presentation was 4 years. The initial diagnosis of Proteus syndrome was made by genetic analysis of fatty tissue and clinical criteria according to Sapp et al. 1
The presented data and examinations represent the course of treatment in the department of otorhinolaryngology, head and neck surgery of the university hospital Heidelberg. The patient was seen and examined in intervals no longer than 3 months. The endoscopy of the upper airway was performed with the Visera Elite video tower from Olympus, Hamburg, Germany. As digital image processing system we used rpszene® from Rehder/Partner, Hamburg, Germany.
3. CASE PRESENTATION
The 29‐year‐old patient initially presented at our clinic in February 2019. The patient got the diagnosis of Proteus syndrome in 2013 at the age of 23 by mutation analysis from fatty tissue. The Proteus syndrome presented with increased vascular malformations, macrodactyly, thoracolumbar scoliosis, and lung ventilation disorders.
The vascular malformations included a lymphatic malformation in the region of the right adrenal gland, a lymphatic malformation of the spleen, and a venous malformation with aneurysmal dilatation of the right jugular vein as well as capillary malformations of the right breast.
In the patient's history, an unsafe neoplasm of the hemithorax was already surgically removed after birth, as was a cervical neoplasm. Hyperplasia of the digits II–IV on the right and II and III on the left also manifested directly postnatally. In addition, there was an aneurysmal expansion of the right internal jugular vein and thoracolumbar scoliosis. Multiple orthopedic procedures of the fingers and hands were performed in the course, up to amputation of digits II–IV right and II and III left. At the age of 16, a corrective operation was performed for pectus excavatum (Nuss procedure). In 2018 an immunosuppressive therapy with sirolimus was initiated but stopped after 2 months because of severe side effects and no effectiveness.
At the initial presentation the patient complained about exertional dyspnea and stridor, but no hoarseness. In the laryngoscopy a submucous mass revealed in parts of the larynx and hypopharynx with equal mobility of the vocal folds with complete glottic closure (Figure 1).
FIGURE 1.
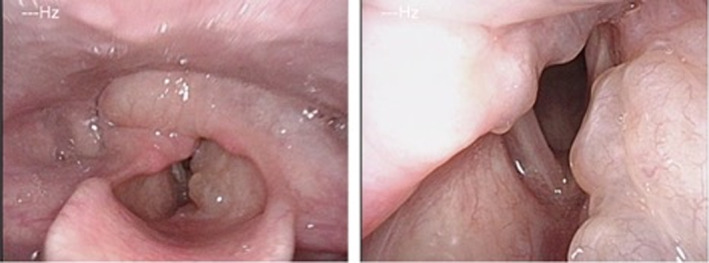
Initial laryngoscopy of February 2019.
An external magnet resonance imaging (MRI) scan revealed correlating findings with a contrast enhancement in the above‐mentioned regions (Figure 2).
FIGURE 2.
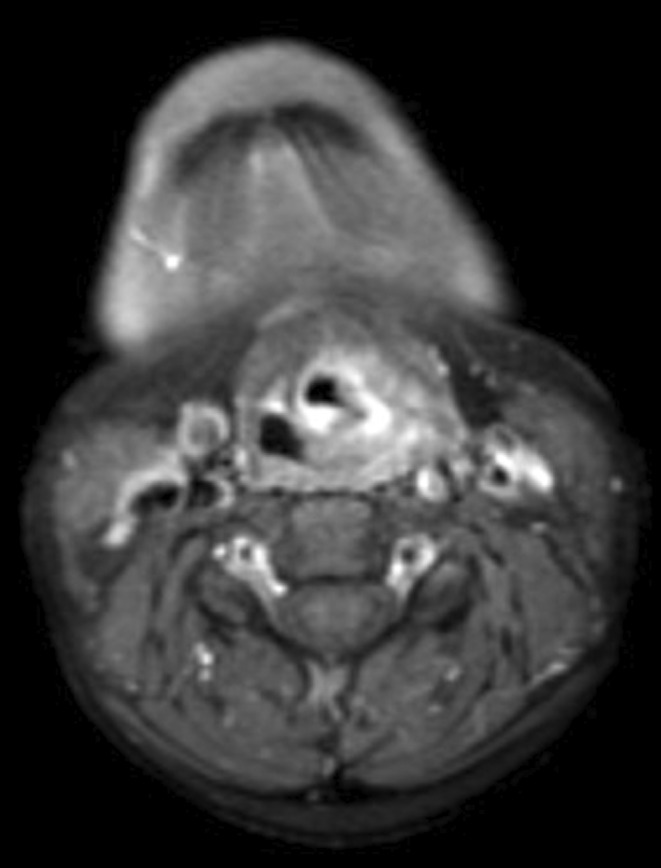
T1‐weighted MRI scan with gadolinium from October 2018.
Submucous tumorous mass with punctum maximum at the left supraglottis, reaching to the midline and the postcricoid region on both sides and along the aryepiglottic fold on the left, partially obstructing the sinus piriformis on the left, but with equal mobility of the vocal folds with complete glottic closure, but supraglottic constriction during phonation.
After an interdisciplinary conference, sclerotherapy was scheduled. The procedure was successfully performed in April 2019 by transcutaneous puncture on the left upper edge of the thyroid cartilage and injection of one unit of Picibanil under endoscopic and fluoroscopic control in general anesthesia.
After sclerotherapy, the patient recovered temporarily from exertional dyspnea and stridor. Another MRI scan in August 2019 and endoscopy revealed a mild improvement of the lymphangioma of the larynx. Ten months after the intervention, the patient developed increasing symptoms again, so that a therapy with the PI3K inhibitor alpelisib was started in March 2020. During this therapy, the patient developed extreme side effects, ultimately leading to discontinuation of therapy after 3 months. During systemic therapy the lymphatic malformations remained stable.
In May 2021, the laryngoscopy still showed the supraglottic malformation in the area of the left vocal fold, hypopharyngeal affecting the postcricoid region and the sinus piriformis on both sides (Figure 3).
FIGURE 3.
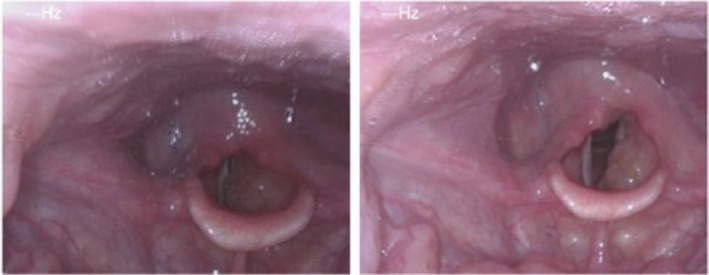
Laryngoscopy of March 2021.
Therefore, we performed a microlaryngoscopy with laser surgical resection in general anesthesia in June 2021. Histopathologic findings confirmed the diagnosis of a lymphatic malformation.
After the procedure the patient was monitored in our intensive care unit due to severe postoperative swelling. About 3 weeks later she reported a symptom relief, which lasted for about half a year.
In October 2021 there were again episodes of dyspnea on exertion and stridor and a return of the lymphangioma, so that microlaryngoscopy with renewed sclerotherapy (Picibanil) of the hypopharyngeal lymphangioma was performed under general anesthesia.
After the operation, the patient complained of increasing dyspnea and cervical tightness. Magnifying laryngoscopy also showed increasing left hypopharyngeal swelling, particularly in the area of the aryepiglottic fold. After being monitored in the intensive care unit and given steroids, the patient was discharged a few days later in an improved general condition.
Due to renewed recurrences and an increase in the lymphatic malformation, a microlaryngoscopy with laser surgical resection on the left postcricoid area was performed again in May 2022. After this, a stable disease could be achieved.
In March 2023, during a routine checkup, the patient reported altered sensation of the laryngeal area and an increase in the dyspnea, especially when exerting or after eating. Hoarseness also occurred intermittently.
The clinical laryngeal finding revealed a persistent but reduced left supraglottic and hypopharyngeal mass (Figure 4). Due to the recurring symptoms, a microlaryngoscopy with laser surgical resection of the left postcricoid area was performed under general anesthesia. About a week after the operation, the patient described an improvement of the symptoms. Further clinical controls have already been agreed in the course of the process. In the case of recurrent lymphangioma, a satisfactory laryngeal and hypopharyngeal finding could be established for the time being.
FIGURE 4.
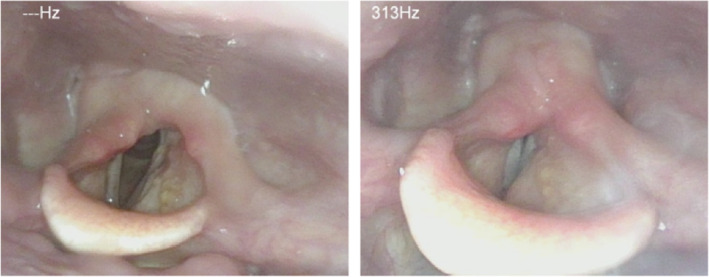
Laryngoscopy of March 2023. Hypopharyngeal with the Valsalva maneuver at most only slight and symmetrical thickening recognizable, subglottic space free. Pocket fold on the left still occupied by the lymphangioma.
4. DISCUSSION
Lymphangioma of the larynx is rare. Only few reports have been described in the literature. Our patient suffers from recurrent manifestations of a lymphangioma in the laryngeal and hypopharyngeal area due to Proteus syndrome.
Lymphatic malformations localized in the larynx area may require rapid therapy due to local complications. In most cases, intensified dyspnea is associated with infections, which should be aggressively treated with antibiotics and steroids. If there is no improvement, a tracheostomy may be necessary to secure the airway. 8 In addition to the clinical examination, imaging by means of computed tomography (CT) or MRI is essential in order to plan the procedure and to protect adjacent structures as best as possible. 8
Therapeutic options for lymphangiomas in the head and neck region are radiofrequency ablation, laser surgery, sclerotherapy, and classic surgical therapy. 5 In the laryngeal region lasers are mostly used to treat mucosal‐based lesions, as the traumatic effect on adjacent structures can be minimized compared to classic surgery and healing is usually rapid. 5 , 9 In our patient, laser surgical resection showed the highest effectiveness and brought symptom relief. We were able to excise the lesion without causing any damage to surrounding vital anatomical structures of the larynx and preserve its functions, using an endoscopic approach. Due to postoperative swelling the patient had to be monitored in our intensive care unit after the surgical procedures. Nevertheless, a tracheostomy was not necessary. Despite this, our patient suffered multiple recurrences of the lymphangioma. Hartl et al. also report a 94% risk of recurrence of lymphangiomas located at the base of the tongue, parapharyngeal space, and/or larynx in their 18 pediatric patients that were included in their study. 10
Alternatively, and with a lower surgical risk, high healing rates have also been achieved by sclerotherapy. 11 Especially Picibanil (OK‐432), which is a biologic preparation of lyophilized powder containing Streptococcus pyogenes Su strain cells (group A, Type 3) treated with benzylpenicillin potassium, has been widely used and accepted. 5 , 11 The treatment agent works by inducing an inflammatory response in the lesion through the release of cytokines and consequent endothelial damage. 5 The use of Picibanil in lymphatic malformations was first reported in 1987 by Ogita et al 12 Since then, a few cases have been reported in which partial to complete resolution of the lesions has been observed with the use of the drug. 13
The main disadvantage of sclerotherapy with Picibanil is the high risk of post‐procedural inflammation and swelling. 5 Our patient also suffered from swelling postoperatively and had to be temporarily monitored in the intensive care unit and had to be treated with steroids. In addition, multiple interventions are often required to achieve the desired effect and stabilization of the lymphatic malformation. 5 , 11
So far, there is no randomized study to compare the different treatment options. The therapeutic decision should therefore be made on an interdisciplinary basis and depends on the extent of the lymphatic malformation and its localization.
We reported this case because of the unusual site of involvement in isolation from the rest of the head and neck in an adult patient who suffers from Proteus syndrome.
5. CONCLUSION
Rare syndromic diseases require multidisciplinary collaboration. In the case of laryngeal lymphangiomatosis, treatment options should be considered carefully. Laser surgical treatment can bring rapid symptom relief but with the risk of damaging adjacent structures and functional loss. Sclerotherapy can be used with less surgical risk and functional damage but also has the risk of postinterventional swelling and requires usually multiple interventions to achieve symptom relief.
AUTHOR CONTRIBUTIONS
Christina Sauter: Conceptualization; data curation; writing – original draft. Veronika Kolb: Investigation; writing – review and editing. Nikolaus Bosch: Investigation; writing – review and editing. Cornelia Hornberger: Writing – review and editing. Peter Karl Plinkert: Resources; supervision. Ralph Hohenberger: Formal analysis; project administration; supervision; writing – review and editing.
FUNDING INFORMATION
This research did not receive any funding.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
ETHICS STATEMENT
In accordance to the ethics committee of the University of Heidelberg, no further ethic vote was necessary. The patient's written consent was gathered to publish the data and the pictures.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENT
Open Access funding enabled and organized by Projekt DEAL.
Sauter C, Kolb V, Bosch N, Hornberger C, Plinkert PK, Hohenberger R. Recurrent laryngeal lymphangiomatosis in a patient with Proteus syndrome: A case report. Clin Case Rep. 2023;11:e8073. doi: 10.1002/ccr3.8073
DATA AVAILABILITY STATEMENT
The present data are summarized in this paper (METHODS). The complete dataset can be obtained from the authors by interested readers upon formal request.
REFERENCES
- 1. Sapp JC, Buser A, Burton‐Akright J, Keppler‐Noreuil KM, Biesecker LG. A dyadic genotype‐phenotype approach to diagnostic criteria for Proteus syndrome. Am J Med Genet C Semin Med Genet. 2019;181(4):565‐570. doi: 10.1002/ajmg.c.31744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Organization for Rare Disorders (NORD) . Proteus Syndrome. https://rarediseases.org/rare‐diseases/proteus‐syndrome/. Published 2018, Accessed on: June 16, 2023
- 3. Gupta N, Goyal A, Singh PP, Sharma S. Isolated laryngeal lymphangioma: a rarity. Indian J Otolaryngol Head Neck Surg. 2011;63(Suppl 1):90‐92. doi: 10.1007/s12070-011-0210-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Seven H, Topuz E, Turgut S. Isolated laryngeal lymphangioma showing the symptoms of acute epiglottitis. Eur Arch Otorhinolaryngol. 2004;261(10):548‐550. doi: 10.1007/s00405-002-0486-6 [DOI] [PubMed] [Google Scholar]
- 5. Colbert SD, Seager L, Haider F, Evans BT, Anand R, Brennan PA. Lymphatic malformations of the head and neck‐current concepts in management. Br J Oral Maxillofac Surg. 2013;51(2):98‐102. doi: 10.1016/j.bjoms.2011.12.016 [DOI] [PubMed] [Google Scholar]
- 6. Hirunwiwatkul P. Radiofrequency tissue volume reduction: suggested treatment for lymphatic malformation. J Med Assoc Thai. 2004;87(7):834‐838. [PubMed] [Google Scholar]
- 7. Biesecker L. The challenges of Proteus syndrome: diagnosis and management. Eur J Hum Genet. 2006;14(11):1151‐1157. doi: 10.1038/sj.ejhg.5201638 [DOI] [PubMed] [Google Scholar]
- 8. Perkins JA, Manning SC, Tempero RM, et al. Lymphatic malformations: review of current treatment. Otolaryngol Head Neck Surg. 2010;142(6):795‐803.e1. doi: 10.1016/j.otohns.2010.02.026 [DOI] [PubMed] [Google Scholar]
- 9. Papsin BC, Evans JN. Isolated laryngeal lymphangioma: a rare cause of airway obstruction in infants. J Laryngol Otol. 1996;110(10):969‐972. doi: 10.1017/s0022215100135479 [DOI] [PubMed] [Google Scholar]
- 10. Hartl DM, Roger G, Denoyelle F, Nicollas R, Triglia JM, Garabedian EN. Extensive lymphangioma presenting with upper airway obstruction. Arch Otolaryngol Head Neck Surg. 2000;126(11):1378‐1382. doi: 10.1001/archotol.126.11.1378 [DOI] [PubMed] [Google Scholar]
- 11. Zhou Q, Zheng JW, Mai HM, et al. Treatment guidelines of lymphatic malformations of the head and neck. Oral Oncol. 2011;47(12):1105‐1109. doi: 10.1016/j.oraloncology.2011.08.001 [DOI] [PubMed] [Google Scholar]
- 12. Ogita S, Tsuto T, Nakamura K, Deguchi E, Tokiwa K, Iwai N. OK‐432 therapy for lymphangioma in children: why and how does it work? J Pediatr Surg. 1996;31(4):477‐480. doi: 10.1016/s0022-3468(96)90478-9 [DOI] [PubMed] [Google Scholar]
- 13. Luzzatto C, Midrio P, Tchaprassian Z, Guglielmi M. Sclerosing treatment of lymphangiomas with OK‐432. Arch Dis Child. 2000;82(4):316‐318. doi: 10.1136/adc.82.4.316 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The present data are summarized in this paper (METHODS). The complete dataset can be obtained from the authors by interested readers upon formal request.


