Abstract
Objective
This study aims to evaluate the characteristics and outcomes of patients who fulfilled extracorporeal membrane oxygenation cardiopulmonary resuscitation (E-CPR) selection criteria during in-hospital cardiac arrest (IHCA).
Design
This is a nested cohort study.
Setting
Code blue data were collected across seven hospitals in Australia between July 2017 and August 2018.
Participants
Participants who fulfilled E-CPR selection criteria during IHCA were included.
Main outcome measures
Return of spontaneous circulation and survival and functional outcome at hospital discharge. Functional outcome was measured using the modified Rankin scale, with scores dichotomised into good and poor functional outcome.
Results
Twenty-three (23/144; 16%) patients fulfilled E-CPR selection criteria during IHCA, and 11/23 (47.8%) had a poor outcome. Patients with a poor outcome were more likely to have a non-shockable rhythm (81.8% vs. 16.7%; p = 0.002), and a longer duration of CPR (median 12.5 [5.5, 39.5] vs. 1.5 [0.3, 2.5] minutes; p < 0.001) compared to those with a good outcome. The majority of patients (18/19 [94.7%]) achieved sustained return of spontaneous circulation within 15 minutes of CPR. All five patients who had CPR >15 minutes had a poor outcome.
Conclusion
Approximately one in six IHCA patients fulfilled E-CPR selection criteria during IHCA, half of whom had a poor outcome. Non-shockable rhythm and longer duration of CPR were associated with poor outcome. Patients who had CPR for >15 minutes and a poor outcome may have benefited from E-CPR. The feasibility, effectiveness and risks of commencing E-CPR earlier in IHCA and among those with non-shockable rhythms requires further investigation.
Keywords: Extracorporeal membrane oxygenation, Cardiopulmonary resuscitation, Cardiac arrest, Intensive care
1. Introduction
In-hospital cardiac arrest (IHCA) is a sudden life-threatening emergency effecting approximately 3000 Australians each year.1 Despite treatment advances, survival rates have only marginally improved over time,[2], [3], [4] with larger registry studies reporting survival to hospital discharge to be approximately 20–25%.2,5,6 Although, most survivors appear to have a good functional outcome, recovery is variable and many survivors are left with significant disability.7,8
There is growing interest in the use of novel therapies to improve outcomes of patients who experience IHCA. In recent years, there has been a 10-fold increase in the utilisation of extracorporeal membrane oxygenation (ECMO) during cardiac arrests that are refractory to conventional cardiopulmonary resuscitation (CPR),9 referred to as ECMO-CPR (E-CPR). E-CPR is a complex, resource-intensive and costly intervention that requires a team of highly trained healthcare professionals.10,11 Accordingly, it is not universally available. Multiple cohort studies have shown E-CPR to be associated with increased rates of survival to hospital discharge and improved neurological outcomes when compared to conventional CPR.[12], [13], [14] However, the majority of these studies are small, single centre studies with heterogenous cohorts and therefore have a high risk of bias. There is an absence of rigorous randomised controlled trials evaluating E-CPR following IHCA.15 There is currently no consensus regarding appropriate selection criteria, and it is unclear which patients may benefit from E-CPR.10 In addition, the optimal timing of E-CPR for IHCA remains unknown11 although guidelines suggest establishing E-CPR within 60 minutes of IHCA.10,16
We have previously reported the epidemiology of ward-based IHCAs in Australian hospitals with established rapid response teams (RRTs), as well as the hospital discharge and long-term outcomes from the Australia and New Zealand Cardiac Arrest Outcomes and Determinants of ECMO (ANZ-CODE) study.7,8,17 The primary aim of this present study was to evaluate the characteristics and outcomes of ANZ-CODE study participants who fulfilled selection criteria for E-CPR during IHCA. The second aim was to compare the characteristics of patients who had a good functional outcome with those who had a poor functional outcome to better understand which patients may benefit from E-CPR during IHCA.
2. Methods
2.1. Study design
This was a nested cohort study within ANZ-CODE, a multicentre prospective observational study conducted between July 2017 and August 2018.17 Ethical approval was obtained at the lead site (Austin Health; HREC/16/Austin/168) and locally at all participating sites.
2.2. Setting and participant selection
The ANZ-CODE study methodology has been described in detail elsewhere.17 In brief, code blue and RRT data were collected prospectively across seven, acute, metropolitan hospitals in Australia during the study period. Patients were included if they were ≥18 years old, admitted as an acute care hospital in-patient and experienced IHCA. Patients were excluded if there was a documented “not for resuscitation” order in place prior to the IHCA or if they suffered a cardiac arrhythmia requiring electrical cardioversion but no external cardiac compressions. Non-ward-based cardiac arrests, such as those occurring in the emergency department, cardiac catheterisation laboratory, operating theatres and intensive care unit were also excluded.
For this present study, we included ANZ-CODE participants who fulfilled predefined E-CPR selection criteria during IHCA. We performed a search of existing literature[18], [19], [20], [21], [22], [23], [24], [25] and sought local expert opinion in order to define the E-CPR selection criteria prior to commencement of the ANZ-CODE study (Table 1). We included criteria that could be used by clinicians in real time to facilitate decisions regarding patients’ suitability for E-CPR during IHCA.
Table 1.
Extracorporeal membrane oxygenation cardiopulmonary resuscitation (E-CPR) selection criteria.
| E-CPR selection criteria |
|---|
| Age 18–70 years old |
| Independent with activities of daily living prior to index hospital admission |
| Charlson comorbidity index <5 |
No major pre-existing comorbidity including:
|
| No documented limits of care prior to in-hospital cardiac arrest |
| Witnessed in-hospital cardiac arrest |
Two of the participating sites were dedicated, high-volume (>30 cases per year) ECMO centres providing state-wide referral services for Victoria and New South Wales, two sites were low-volume (<20 cases per year) ECMO centres and three site performed ECMO infrequently.
2.3. Data collection and management
Patient demographic data included age, gender, independence with activities of daily living (ADL) before the index hospital admission, Charlson comorbidity index (CCI), organ system associated with the admission diagnosis and any documented limitation to treatment before the IHCA. Clinical and cardiac arrest characteristics included, duration of hospital admission before the IHCA, whether the IHCA was witnessed, initial arrest rhythm, total duration of CPR and the implementation of E-CPR.
We evaluated the outcomes of the IHCA including return of spontaneous circulation (ROSC) and, survival and functional outcome at hospital discharge. Functional outcome was measured using the modified Rankin scale (mRS), a 7-point disability scale ranging from 0 (no symptoms or disability) to 6 (death). The mRS scores were dichotomised into good functional outcome (mRS score ≤3) and poor functional outcome (mRS score ≥4).26
Data were collected prospectively through medical chart review using a standardised case report form and data dictionary.17 Data were transferred to the lead investigators via a secure, encrypted online platform (AARNET Cloudstor File Sender). For patients who experienced two or more IHCA during the study period, data from the first event were analysed for this study.
2.4. Statistical analysis
Categorical data were expressed as counts and percentages, and continuous data were summarised using mean ± standard deviation (SD) or median (interquartile range) according to data type and distribution. Comparisons between groups were made using chi-squared or Fisher's exact test (where numbers were small) for categorical variables and student's t-test or Mann–Whitney ‘U’ test as appropriate for continuous variables. All p-values were two-tailed with p < 0.05 considered statistically significant. Analyses were conducted using SPSS version 25 (IBM SPSS Inc, Armonk, NY).
3. Results
3.1. Participants who fulfilled predefined E-CPR selection criteria during IHCA
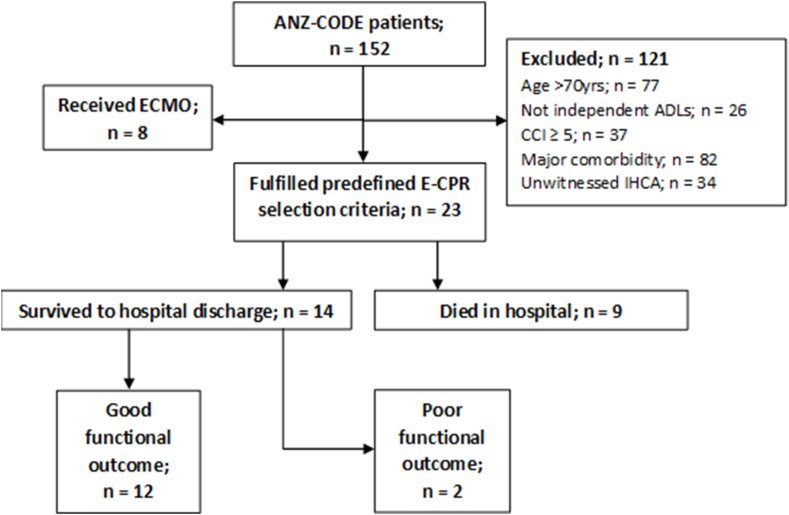
Twenty-three (23/144; 16%) ANZ-CODE patients fulfilled the predefined E-CPR selection criteria during IHCA. The primary reason for exclusion of the remaining 121 (84%) patients was the presence of one or more major comorbidity, closely followed by age over 70 years old (Fig. 1). The mean (SD) age of the patients who fulfilled the predefined selection criteria for E-CPR during IHCA was 60.0 (±7.7) years, 18 (78.3%) were male and approximately half had a cardiovascular condition associated with their hospital admission (Table 2). The median time to IHCA was 4.0 (2.0, 6.0) days after admission. Six (26.1%) IHCA occurred within “usual business hours” (i.e., Monday to Friday between 8am and 6pm). There was a median of 1.0 (1.0, 7.0) patient per hospital that fulfilled the predefined E-CPR selection criteria during IHCA throughout the 12-month study period.
Fig. 1.
Flow of participants through the study.
ANZ-CODE = Australia and New Zealand cardiac arrest outcomes and determinants of extracorporeal membrane oxygenation; E-CPR = extracorporeal membrane oxygenation cardiopulmonary resuscitation; ADLs = activities of daily living; CCI = Charlson comorbidity Index; IHCA = in-hospital cardiac arrest.
Table 2.
Demographics and cardiac arrest characteristics for patients who fulfilled and those who did not fulfil predefined E-CPR selection criteria.
| Demographics, cardiac arrest characteristics and outcomes | Total; n = 144 | Fulfilled E-CPR selection criteria; n = 23 | Did not fulfil E-CPR selection criteria; n = 121 | p-value |
|---|---|---|---|---|
| Age (years); mean ± SD | 70.6 ± 13.9 | 60.0 ± 7.7 | 72.6 ± 13.9 | <0.001 |
| Male gender; n (%) | 94 (65.3) | 18 (78.3) | 76 (62.8) | 0.15 |
| Charlson Comorbidity Index; median (IQR) | 3 (1, 5) | 1 (0, 1) | 3 (1, 5) | <0.001 |
| System of admission; n (%) | 0.83 | |||
| Cardiovascular System | 58 (40.3) | 11 (47.8) | 47 (38.8) | |
| Central Nervous System | 14 (9.7) | 1 (4.3) | 13 (10.7) | |
| Respiratory System | 14 (9.7) | 2 (8.7) | 12 (9.9) | |
| Gastrointestinal System | 24 (16.7) | 6 (26.1) | 18 (14.9) | |
| Musculoskeletal System | 7 (4.9) | 1 (4.3) | 6 (5.0) | |
| Other | 27 (18.8) | 2 (16.7) | 25 (20.7) | |
| Initial arrest rhythm; n (%) | 0.09 | |||
| Asystole | 46 (31.9) | 3 (13.0) | 43 (35.5) | |
| PEA | 52 (36.1) | 8 (34.8) | 44 (36.4) | |
| VT | 13 (9.0) | 3 (13.0) | 10 (8.3) | |
| VF | 15 (10.4) | 3 (13.0) | 12 (9.9) | |
| Other | 9 (6.3) | 3 (13.0) | 6 (5.0) | |
| Unknown | 9 (6.3) | 3 (13.0) | 6 (5.0) | |
| CPR duration (minutes); median (IQR) | 6.0 (2.0, 17.0) | 4.0 (1.5, 13.8) | 7.0 (2.8, 18.0) | 0.22 |
| Arrest Outcome; n (%) | 0.08 | |||
| Did not achieve ROSC | 42 (29.2) | 4 (17.4) | 38 (31.4) | |
| Intermittent ROSC | 11 (7.6) | 0 (0) | 11 (9.1) | |
| Sustained ROSC | 91 (63.2) | 19 (82.6) | 72 (59.5) | |
| Discharge disposition; n (%) | 0.15 | |||
| Died during arrest | 47 (32.6) | 4 (17.4) | 43 (35.5) | |
| Died in intensive care | 28 (19.4) | 5 (21.7) | 23 (19.0) | |
| Died in hospital | 10 (6.9) | 0 (0) | 10 (8.3) | |
| Discharged home | 37 (25.7) | 10 (43.5) | 27 (22.3) | |
| Discharged to rehabilitation | 10 (6.9) | 2 (8.7) | 8 (6.6) | |
| Discharged to nursing home | 5 (3.5) | 0 (0) | 5 (4.1) | |
| Hospital transfer | 7 (4.9) | 2 (8.7) | 5 (4.1) | |
| Functional outcome at discharge; n (%) | 0.006 | |||
| Good functional outcome (mRS ≤ 3) | 41 (28.5) | 12 (52.2) | 29 (24.0) | |
| Poor functional outcome (mRS ≥ 4) | 103 (71.5) | 11 (47.8) | 92 (76.0) |
E-CPR = extracorporeal membrane oxygenation cardiopulmonary resuscitation; SD = standard deviation; IQR = interquartile range; PEA = pulseless electrical activity; VT = ventricular tachycardia; VF = ventricular fibrillation; CPR = cardiopulmonary resuscitation; ROSC = return of spontaneous circulation; mRS = modified Rankin Scale.
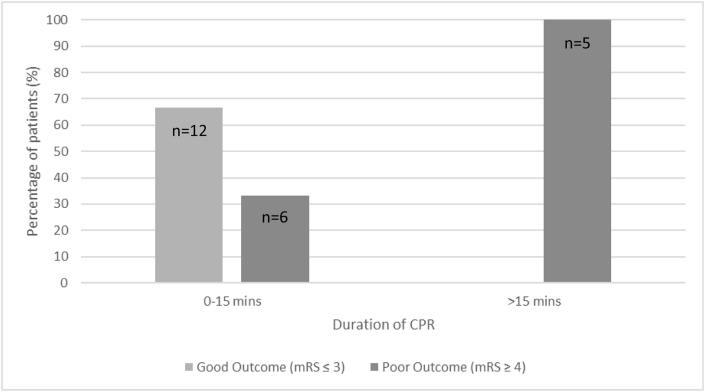
Of the 23 patients who fulfilled the predefined E-CPR selection criteria during IHCA, 11 (47.8%) patients had a poor outcome at hospital discharge. Patients with a poor outcome were more likely to have a non-shockable initial rhythm (81.8% vs. 16.7%; p = 0.002), and a longer duration of CPR (median 12.5 [5.5, 39.5] vs. 1.5 [0.3, 2.5] minutes; p < 0.001) compared to those who had a good outcome. Sustained ROSC was achieved in 19/23 (82.6%) patients (Table 3). The median duration of CPR of patients who achieved sustained ROSC was 3.0 (0.75, 5.5) minutes compared with 40.5 (28.5, 45.5) minutes for patients who did not achieve sustained ROSC (p = 0.003). The majority of patients (18/19 [94.7%]) who achieved sustained ROSC did so within the first 15 minutes of CPR. A good functional outcome occurred in 12/18 (66.7%) of patients with a CPR duration of ≤ 15minutes. Five patients had a duration of CPR of >15 minutes, all of whom had a poor outcome at hospital discharge (Fig. 2), including four who died during the arrest and one who was discharged to rehabilitation with moderate to severe disability.
Table 3.
Demographics, cardiac arrest characteristics and outcome of patients experiencing in-hospital cardiac arrest who fulfilled predefined E-CPR selection criteria.
| Demographics, cardiac arrest characteristics and outcomes | Total; n = 23 | Good Outcome (mRS ≤3); n = 12 | Poor Outcome (mRS ≥4); n = 11 | p-value |
|---|---|---|---|---|
| Age (years); mean ± SD | 60.0 ± 7.7 | 58.0 ± 8.3 | 62.2 ± 6.6 | 0.20 |
| Male gender; n (%) | 18 (78.3) | 11 (91.7%) | 7 (63.6%) | 0.16 |
| Charlson Comorbidity Index; median (IQR) | 1 (0, 1) | 1 (0.5, 1) | 0 (0, 1) | 0.35 |
| System of admission; n (%) | 0.06 | |||
| Cardiovascular System | 11 (47.8) | 8 (66.7) | 3 (27.3) | |
| Central Nervous System | 1 (4.3) | 0 (0) | 1 (9.1) | |
| Respiratory System | 2 (8.7) | 0 (0) | 2 (18.2) | |
| Gastrointestinal System | 6 (26.1) | 2 (16.7) | 4 (36.4) | |
| Musculoskeletal System | 1 (4.3) | 0 (0) | 1 (9.1) | |
| Other | 2 (16.7) | 2 (16.7) | 0 (0) | |
| Initial arrest rhythm; n (%) | 0.002 | |||
| Asystole | 3 (13.0) | 2 (16.7) | 1 (9.1) | |
| PEA | 8 (34.8) | 0 (0) | 8 (72.7) | |
| VT | 3 (13.0) | 3 (25.0) | 0 (0) | |
| VF | 3 (13.0) | 3 (25.0) | 0 (0) | |
| Other | 3 (13.0) | 2 (16.7) | 1 (9.1) | |
| Unknown | 3 (13.0) | 2 (16.7) | 1 (9.1) | |
| CPR duration (minutes); median (IQR) | 4.0 (1.5, 13.8) | 1.5 (0.3, 2.5) | 12.5 (5.5, 39.5) | <0.001 |
| Arrest Outcome; n (%) | 0.037 | |||
| Did not achieve ROSC | 4 (17.4) | 0 (0) | 4 (36.4) | |
| Intermittent ROSC | 0 (0) | 0 (0) | 0 (0) | |
| Sustained ROSC | 19 (82.6) | 12 (100) | 7 (63.6) | |
| Discharge disposition; n (%) | <0.001 | |||
| Died during arrest | 4 (17.4) | 0 (0) | 4 (17.4) | |
| Died in intensive care | 5 (21.7) | 0 (0) | 5 (21.7) | |
| Discharged home | 10 (43.5) | 10 (43.5) | 0 (0) | |
| Discharged to rehabilitation | 2 (8.7) | 0 (0) | 2 (8.7) | |
| Hospital transfer | 2 (8.7) | 2 (8.7) | 0 (0) |
E-CPR = extracorporeal membrane oxygenation cardiopulmonary resuscitation; mRS = modified Rankin Scale; SD = standard deviation; IQR = interquartile range; PEA = pulseless electrical activity; VT = ventricular tachycardia; VF = ventricular fibrillation; CPR = cardiopulmonary resuscitation; ROSC = return of spontaneous circulation.
Fig. 2.
Duration of cardiopulmonary resuscitation and outcome of patients who fulfilled predefined extracorporeal membrane oxygenation cardiopulmonary resuscitation (E-CPR) selection criteria.
CPR = cardiopulmonary resuscitation; E-CPR = extracorporeal membrane oxygenation cardiopulmonary resuscitation; mRS = modified Rankin scale.
3.2. Participants who received extracorporeal support following IHCA
No patients who fulfilled the predefined E-CPR criteria during IHCA received ECPR during the study period. However, five patients received ECMO later in their ICU admission for refractory cardiogenic shock, refractory ventricular tachycardia or haemodynamic instability. Two of these patients survived to hospital discharge with a good functional outcome, both of who were fitted with ventricular assist device as a bridge to heart transplant. Three patients who did not fulfil the predefined E-CPR criteria received E-CPR during IHCA, one of whom was over 70 years old and two had unwitnessed IHCAs, all of these patients had a poor outcome and died in ICU.
Overall, 3/152 (2.0%) participants received E-CPR during IHCA, and a further 5/152 (3.3%) who fulfilled E-CPR selection criteria during IHCA, who subsequently had a long duration of CPR and a poor outcome.
4. Discussion
4.1. Key findings
In this nested cohort study of ANZ-CODE study participants, we found approximately one in six patients fulfilled predefined E-CPR selection criteria during IHCA. Few events occurred during business hours and, on average, they occurred once per year in participating hospitals. Of the patients who fulfilled predefined E-CPR selection criteria during IHCA, half had a poor outcome. Patients with a poor outcome were more likely to have a non-shockable rhythm and a longer duration of CPR compared to patients with a good outcome. The majority of patients achieved sustained ROSC and did so within the first 15 minutes of CPR. Two thirds of patients who had a CPR duration of ≤15 minutes had a good outcome, whereas the five patients who had a CPR duration >15 minutes all had a poor outcome. E-CPR was performed in only 2% of IHCAs in our cohort.
4.2. Comparisons with previous studies
Few studies have explored the number of patients that may potentially be eligible for E-CPR following IHCA. Although we found that one in six patients fulfilled E-CPR selection criteria during IHCA, only 3.3% of patients in our cohort subsequently had a CPR duration ≥15 minutes and a poor outcome and may have benefited from E-CPR. Comparatively, two small, single-centre, retrospective studies found that 8% and 11% of patients fulfilled criteria for E-CPR following IHCA.27,28 Differences in the selection criteria used in these studies as well as variation in patient, cardiac arrest, and hospital characteristics may account for the disparity in percentages reported. We included only ward-based IHCA, whereas one study included patients from all inpatient areas,27 and the other included only patients who experienced IHCA in the emergency department.28 Both studies used a lower maximum age limit than our study, excluding patients aged over 65 years old.27,28
Among patients who fulfilled our predefined E-CPR selection criteria during IHCA, we found those with non-shockable rhythms and a longer duration of CPR had a worse outcome at hospital discharge. This is consistent with results from previous studies of conventional CPR following IHCA.5,[32], [33], [34] In our study, most patients fulfilling our predefined E-CPR selection criteria during IHCA and had a poor outcome, had a pulseless electrical activity (PEA) arrest rhythm. Many E-CPR programs and studies exclude patients with non-shockable rhythms due to the poor outcomes following conventional CPR. However, the prognostic significance of non-shockable rhythms in patients who receive E-CPR remains unclear.35,36 A recent systematic review and meta-analysis of E-CPR following IHCA found that patients with shockable rhythms had a higher likelihood of survival to hospital discharge than those with non-shockable rhythms.37 A similar trend was found in a study by Pabst et al., but importantly, they found that 23% of patients with a PEA arrest rhythm survived to hospital discharge compared with 0% of those with asystole.36 In contrast, a retrospective review by Marinacci et al. found no association between arrest rhythm and survival outcome; however, this study did not include patients with asystole.35 Currently, there is insufficient evidence to exclude patients with a PEA arrest from E-CPR. For patients who are relatively young, independent and have few comorbidities, the benefits of E-CPR may outweigh the risks.
Among observational studies, a shorter duration of CPR before E-CPR implementation was associated with improved rates of survival and favourable neurological outcome.[37], [38], [39], [40] Haneya et al., found 70% of patients with a “low flow” time (i.e., time from commencing CPR to initiation of E-CPR) of less than 15 minutes survived to hospital discharge, decreasing to 48% for 15–30 minutes, 27% for 30–45 minutes and 11% for 45–60 minutes.41 Combined, these studies and our findings suggest that the decision to implement E-CPR should be made as early as possible in the resuscitation efforts. A recent consensus statement from the Extracorporeal Life Support Organisation (ELSO) also states that it is reasonable to consider commencing E-CPR cannulation after 10–15 minutes of failed conventional resuscitation efforts.10
Despite the participation of two dedicated, high-volume ECMO centres, E-CPR was performed in only 2% of IHCAs in our study. The patients who received ECPR did not fulfil all of our predefined selection criteria and all had a poor outcome. There is currently no consensus regarding the most appropriate selection criteria for ECPR.20 Inconsistent reporting and heterogeneity of selection criteria and outcomes across studies significantly limit the ability to compare results, and the predictive effect of individual selection criteria on survival and functional outcome remains unknown.18,20 Given the potential benefit of earlier deployment of ECPR, it stands to reason that the selection criteria used should be relatively simple and able to be performed quickly in an emergency situation whilst ensuring patients with the best chance of a good outcome are captured.
We found few patients who fulfilled our predefined E-CPR selection criteria experienced IHCA within “usual business hours.” We also found that the frequency of patients who fulfilled the selection criteria was low for each hospital. This raises questions regarding the feasibility of implementing this specialised and resource intensive treatment in low-volume ECMO centres.25,29 There may also be more risk associated with implementing E-CPR outside of usual business hours with one study reporting lower survival and higher complication rates with E-CPR on weekends compared to weekdays.30 Studies have also shown that patients who receive E-CPR in dedicated high-volume ECMO centres may have better outcomes.31 Until further research is conducted and conclusions drawn regarding appropriate indications and potential benefits of E-CPR, it remains an experimental procedure within the limited resources of the general hospital setting.
4.3. Study strengths and limitations
This is one of the first prospective, multicentre studies to explore the number of patients who may be appropriate for E-CPR during IHCA. Our E-CPR selection criteria were informed by a detailed literature search and expert opinion. Our study provides insights into the outcomes of patients who might be appropriate for E-CPR, which may inform the design of future interventional studies. However, this study has a number of limitations. Due to the low frequency of IHCA in our cohort the sample size was relatively small. We included only metropolitan hospitals with established RRTs and ward-based IHCA, which may limit the generalisability of our results. The exclusion of IHCAs occurring in the emergency department, cardiac catheter laboratory, operating theatre and intensive care unit and cardiac catheter laboratory means our study likely underestimates the number of patients who may fulfil the selection criteria for E-CPR during IHCA, and we are unable to make comment on frequency of IHCA occurring in these areas. We collected data relating to the organ system of admission; however, information regarding the cause and potential reversibility of the IHCA was unavailable. The decision-making processes related to initiation of E-CPR or the withdrawal of life-sustaining treatments were not evaluated in this study.
4.4. Implications for clinical practice
We identified three important implications for clinical practice. First, we found a small group of patients who were relatively young, functionally independent, free of comorbidities, had witnessed IHCAs, with non-shockable rhythms who had a poor outcome, raising the question as to whether they may have benefited from E-CPR. Second, we found that all patients who had CPR for longer than 15 minutes had a poor outcome. Current guidelines suggest that E-CPR should be established within 60 minutes of arrest. However, if our findings were true of a broader population of patients, this suggests E-CPR should be initiated earlier in resuscitation efforts to minimise “low flow” time. Lastly, IHCA among patients fulfilling our selection criteria for E-CPR was uncommon, particularly during usual business hours. This poses significant challenges outside of specialised, high-volume ECMO centres in relation to the feasibility of E-CPR deployment.
4.5. Areas for future research
There is an urgent need for large, high quality prospective E-CPR studies in order to identify prognostic factors associated with neurologically intact survival and the optimal timing of E-CPR for IHCA. In particular, such research should focus on outcomes of E-CPR among suitable patients with witnessed arrest with non-shockable rhythm, as well as the feasibility and risk:benefit ratio of commencing E-CPR earlier during IHCA.
5. Conclusion
Approximately one in six patients who experienced IHCA fulfilled predefined E-CPR selection criteria during IHCA. Poor outcome was seen in half of these patients and associated with a non-shockable rhythm and longer CPR duration. The majority of patients achieved sustained ROSC in the first 15 minutes of CPR. A small number of patients who had CPR for greater than 15 minutes had a poor outcome. The feasibility, effectiveness and risks of commencing E-CPR earlier in IHCA and among those with non-shockable rhythms warrant further investigation.
Conflict of interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or non-for-profit sectors.
Credit author statement
DJ conceived the study. GP analysed the data and wrote the first draft. All authors provided input into the study, the writing and approved the final draft.
Acknowledgements
ANZ-CODE management committee
Daryl Jones, Carol Hodgson Glenn Eastwood, Gemma Pound, Lisa Higgins, Andrew Hilton, Rinaldo Bellomo
Sites and Site Investigators
The Alfred Hospital: Jasmin Board, Emma-Leah Martin, Judit Orosz, Andrew Udy; The Austin Hospital: Phil Marsh, Helen Young, Leah Peck; Cabrini Malvern: Shannon Simpson, David Brewster; Frankston Hospital: Sachin Gupta, Cameron Green; Gold Coast University Hospital: Maimoonbe Gough, Brent Richards; Royal Prince Alfred Hospital: Lucy Wells; David Gattas, Jennifer Coakley, Heidi Buhr; Footscray Hospital: Gerard Fennessy, Sam Bates, John Mulder.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ccrj.2023.05.006.
Contributor Information
G. Pound, Email: gemma.pound@monash.edu.
C.L. Hodgson, Email: carol.hodgson@monash.edu.
The ANZ-CODE Investigators. ANZ-CODE management committee:
Daryl Jones, Carol Hodgson, Glenn Eastwood, Gemma Pound, Lisa Higgins, Andrew Hilton, and Rinaldo Bellomo
Sites and Site Investigators:
Jasmin Board, Emma-Leah Martin, Judit Orosz, Andrew Udy, Phil Marsh, Helen Young, Leah Peck, Shannon Simpson, David Brewster, Sachin Gupta, Cameron Green, Maimoonbe Gough, Brent Richards, Lucy Wells, David Gattas, Jennifer Coakley, Heidi Buhr, Gerard Fennessy, Sam Bates, and John Mulder
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.Jones D.A., Pound G., Eastwood G.E., Hodgson C.L. Estimate of annual in-hospital cardiac arrests in Australia. Crit Care Resusc. 2021;23(4):427. doi: 10.51893/2021.4.L. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson L.E., Chan P.S., Tang F., Nallamothu B.K., Girota S., Perman S.M., et al. Long-term survival trends of medicare patients after in-hospital cardiac arrest: insights from get with the guidelines-resuscitation. Resuscitation. 2018;123:58–64. doi: 10.1016/j.resuscitation.2017.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Girotra S., Nallamothu B.K., Spertus J.A., Li Y., Krumholz H.M., Chan P.S., et al. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367(20):1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Straney L.D., Bray J.E., Finn J., Bernard S. Trends in intensive care unit cardiac arrest admissions and mortality in Australia and New Zealand. Crit Care Resusc. 2014;16(2):104–111. [PubMed] [Google Scholar]
- 5.Nolan J.P., Soar J., Smith G.B., Gwinnutt C., Parrott F., Power S., et al. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom national cardiac arrest audit. Resuscitation. 2014;85(8):987–992. doi: 10.1016/j.resuscitation.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Peberdy M.A., Kaye W., Ornato J.P., Larkin G.L., Nadkarni V., Mancini M.E., et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58(3):297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 7.Pound G.M., Jones D., Eastwood G.M., Paul E., Hodgson C.L., ANZ-CODE Investigators Survival and functional outcome at hospital discharge following in-hospital cardiac arrest (IHCA): a prospective multicentre observational study. Resuscitation. 2020;155:48–54. doi: 10.1016/j.resuscitation.2020.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Pound G.M., Jones D., Eastwood G.M., Paul E., Hodgson C.L., ANZ-CODE Investigators Long-term functional outcome and quality of life following in-hospital cardiac arrest - a longitudinal cohort study. Crit Care Med. 2022;50(1):61–71. doi: 10.1097/CCM.0000000000005118. [DOI] [PubMed] [Google Scholar]
- 9.Richardson A.S., Schmidt M., Bailey M., Pellegrino V.A., Rycus P.T. ECMO Cardio-Pulmonary Resuscitation (ECPR), trends in survival from an international multicentre cohort study over 12-years. Resuscitation. 2017;112:34–40. doi: 10.1016/j.resuscitation.2016.12.009. [DOI] [PubMed] [Google Scholar]
- 10.Richardson A.S.C., Tonna J.E., Nanjayya V., Nixon P., Abrams D.C., Raman L., et al. Extracorporeal cardiopulmonary resuscitation in adults. Interim guideline consensus statement from the extracorporeal life support organization. Asaio J. 2021;67(3):221–228. doi: 10.1097/MAT.0000000000001344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soar J., Maconochie I., Wyckoff M.H., Olasveengen T.M., Singletary E.M., Greif R., et al. 2019 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Circulation. 2019;140(24):e826–e880. doi: 10.1161/CIR.0000000000000734. [DOI] [PubMed] [Google Scholar]
- 12.Ahn C., Kim W., Cho Y., Choi K., Jang B., Lim T.H. Efficacy of extracorporeal cardiopulmonary resuscitation compared to conventional cardiopulmonary resuscitation for adult cardiac arrest patients: a systematic review and meta-analysis. Sci Rep. 2016;6 doi: 10.1038/srep34208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang G.N., Chen X.F., Qiao L., Mei Y., Lv J., Huang X., et al. Comparison of extracorporeal and conventional cardiopulmonary resuscitation: a meta-analysis of 2 260 patients with cardiac arrest. World J Emerg Med. 2017;8(1):5–11. doi: 10.5847/wjem.j.1920-8642.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miraglia D., Miguel L.A., Alonso W. Extracorporeal cardiopulmonary resuscitation for in- and out-of-hospital cardiac arrest: systematic review and meta-analysis of propensity score-matched cohort studies. J Am Coll Emerg Physicians Open. 2020;1(4):342–361. doi: 10.1002/emp2.12091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Link M.S., Berkow L.C., Kudenchuk P.J., Halperin H.R., Hess E.P., Moitra V.K., et al. Part 7: adult advanced cardiovascular life support: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S444–S464. doi: 10.1161/CIR.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 16.Michels G., Wengenmayer T., Hagl C., Dohmen C., Bottiger B.W., Bauersachs J., et al. Recommendations for extracorporeal cardiopulmonary resuscitation (eCPR): consensus statement of DGIIN, DGK, DGTHG, DGfK, DGNI, DGAI, DIVI and GRC. Clin Res Cardiol. 2019;108(5):455–464. doi: 10.1007/s00392-018-1366-4. [DOI] [PubMed] [Google Scholar]
- 17.Australia and New Zealand Cardiac Arrest Outcome and Determinants of ECMO (ANZ-CODE) Investigators The epidemiology of in-hospital cardiac arrests in Australia: a prospective multicentre observational study. Crit Care Resusc. 2019;21(3):180–187. [PubMed] [Google Scholar]
- 18.Burrell A.J.C., Bennett V., Serra A.L., Pellegrino V.A., Romero L., Fann E., et al. Venoarterial extracorporeal membrane oxygenation: a systematic review of selection criteria, outcome measures and definitions of complications. J Crit Care. 2019;53:32–37. doi: 10.1016/j.jcrc.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 19.Tonna J.E., Selzman C.H., Girotra S., Presson A.P., Thiagarajan R.R., Becker L.B., et al. Patient and institutional characteristics influence the decision to use extracorporeal cardiopulmonary resuscitation for in-hospital cardiac arrest. J Am Heart Assoc. 2020;9(9) doi: 10.1161/JAHA.119.015522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karve S., Lahood D., Diehl A., Burrell A., Tian D.H., Southwood T., et al. The impact of selection criteria and study design on reported survival outcomes in extracorporeal oxygenation cardiopulmonary resuscitation (ECPR): a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med. 2021;29(1):142. doi: 10.1186/s13049-021-00956-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koen J., Nathanaël T., Philippe D. A systematic review of current ECPR protocols. A step towards standardisation. Resusc Plus. 2020;3 doi: 10.1016/j.resplu.2020.100018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hadaya J., Dobaria V., Aguayo E., Kwon O.J., Sanaiha Y., Hyunh A., et al. National trends in utilization and outcomes of extracorporeal support for in- and out-of-hospital cardiac arrest. Resuscitation. 2020;151:181–188. doi: 10.1016/j.resuscitation.2020.02.034. [DOI] [PubMed] [Google Scholar]
- 23.Hodgson C.L., Anderson S., Salimi F., Bernard S., Board J.V., Brodie D., et al. October 2020. The EXCEL registry 2020 annual report, Monash University, Australian and New Zealand Intensive Care Research Centre. Report No 2, 30 pages. [Google Scholar]
- 24.Guglin M., Sira M., Joshi S., Shringi S. Outcomes of veno-arterial extracorporeal membrane oxygenation for in-hospital cardiac arrest. Cardiol Rev. 2022;30(2):75–79. doi: 10.1097/CRD.0000000000000371. [DOI] [PubMed] [Google Scholar]
- 25.Abrams D., Garan A.R., Abdelbary A., Bacchetta M., Bartlett R.H., Beck J., et al. Position paper for the organization of ECMO programs for cardiac failure in adults. Intensive Care Med. 2018;44(6):717–729. doi: 10.1007/s00134-018-5064-5. [DOI] [PubMed] [Google Scholar]
- 26.Nolan J.P., Berg R.A., Andersen L.W., Bhanji F., CHan P.S., Donnino M.W., et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the utstein resuscitation registry template for in-hospital cardiac arrest: a consensus report from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia) Resuscitation. 2019;144:166–177. doi: 10.1016/j.resuscitation.2019.08.021. [DOI] [PubMed] [Google Scholar]
- 27.Harrogate S., Stretch B., Seatter R., Finney S., Singer B. A retrospective analysis of inpatient cardiac arrests over one year at a tertiary heart attack and cardiothoracic centre identifying potential candidates for an inpatient extracorporeal cardiopulmonary resuscitation service. J Intensive Care Soc. 2020;21(2):105–110. doi: 10.1177/1751143719848660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iwashita M., Waqanivavalagi S., Merz T., Jones P. Eligibility criteria for extracorporeal cardiopulmonary resuscitation at Auckland City Hospital: a retrospective cohort study. Emerg Med Australasia (EMA) 2020;32(6):960–966. doi: 10.1111/1742-6723.13649. [DOI] [PubMed] [Google Scholar]
- 29.Fulcher B.J., Nicholson A.J., Linke N.J., Berkovic D., Hodgson C.L. The perceived barriers and facilitators to implementation of ECMO services in acute hospitals. Intensive Care Med. 2020;46(11):2115–2117. doi: 10.1007/s00134-020-06187-z. [DOI] [PubMed] [Google Scholar]
- 30.Lee D.S., Chung C.R., Jeon K., Park C., Suh G.Y., Song Y.B., et al. Survival after extracorporeal cardiopulmonary resuscitation on weekends in comparison with weekdays. Ann Thorac Surg. 2016;101(1):133–140. doi: 10.1016/j.athoracsur.2015.06.077. [DOI] [PubMed] [Google Scholar]
- 31.Barbaro R.P., Odetola F.O., Kidwell K.M., Paden M.L., Bartlett R.H., Davis M.M., et al. Association of hospital-level volume of extracorporeal membrane oxygenation cases and mortality. Analysis of the extracorporeal life support organization registry. Am J Respir Crit Care Med. 2015;191(8):894–901. doi: 10.1164/rccm.201409-1634OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fernando S.M., Tran A., Cheng W., Rochwerg B., Taljaard M., Vaillancourt C., et al. Pre-arrest and intra-arrest prognostic factors associated with survival after in-hospital cardiac arrest: systematic review and meta-analysis. BMJ. 2019;367:l6373. doi: 10.1136/bmj.l6373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hessulf F., Karlsson T., Lundgren P., Aune S., Stromsoe A., Kallestedt M.S., et al. Factors of importance to 30-day survival after in-hospital cardiac arrest in Sweden - a population-based register study of more than 18,000 cases. Int J Cardiol. 2018;255:237–242. doi: 10.1016/j.ijcard.2017.12.068. [DOI] [PubMed] [Google Scholar]
- 34.Cohn A.C., Wilson W.M., Yan B., Joshi S.B., Heily M., Morley P., et al. Analysis of clinical outcomes following in-hospital adult cardiac arrest. Intern Med J. 2004;34(7):398–402. doi: 10.1111/j.1445-5994.2004.00566.x. [DOI] [PubMed] [Google Scholar]
- 35.Marinacci L.X., Mihatov N., D’Alessandro D.A., Villavicencio M.A., Roy N., Raz Y., et al. Extracorporeal cardiopulmonary resuscitation (ECPR) survival: a quaternary center analysis. J Card Surg. 2021;36(7):2300–2307. doi: 10.1111/jocs.15550. [DOI] [PubMed] [Google Scholar]
- 36.Pabst D., Brehm C.E. Is pulseless electrical activity a reason to refuse cardiopulmonary resuscitation with ECMO support? Am J Emerg Med. 2018;36(4):637–640. doi: 10.1016/j.ajem.2017.09.057. [DOI] [PubMed] [Google Scholar]
- 37.D’Arrigo S., Cacciola S., Dennis M., Jung C., Kagawa E., Antonelli M., et al. Predictors of favourable outcome after in-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation: a systematic review and meta-analysis. Resuscitation. 2017;121:62–70. doi: 10.1016/j.resuscitation.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 38.Debaty G., Babaz V., Durand M., Gaide-Chevronnay L., Fournel E., Blancher M., et al. Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest. A systematic review and meta-analysis. Resuscitation. 2017;112:1–10. doi: 10.1016/j.resuscitation.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 39.Ryu J.A., Cho Y.H., Sung K., Choi S.H., Yang J.H., Choi J., et al. Predictors of neurological outcomes after successful extracorporeal cardiopulmonary resuscitation. BMC Anesthesiol. 2015;15:26. doi: 10.1186/s12871-015-0002-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Komeyama S., Takagi K., Tsuboi H., Tsuboi S., Morita Y., Yoshida R., et al. The early initiation of extracorporeal life support may improve the neurological outcome in adults with cardiac arrest due to cardiac events. Intern Med. 2019;58(10):1391–1397. doi: 10.2169/internalmedicine.0864-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haneya A., Philipp A., Diez C., Schopka S., Bein T., Zimmermann M., et al. A 5-year experience with cardiopulmonary resuscitation using extracorporeal life support in non-postcardiotomy patients with cardiac arrest. Resuscitation. 2012;83(11):1331–1337. doi: 10.1016/j.resuscitation.2012.07.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.