An estimated 1 in 3 adults1—and 1 in 8 children2—worldwide have the form of chronic liver disease presently known as NAFLD.3 NAFLD is associated with an increased risk of cirrhosis, an important contributor to the growing incidence of liver cancer and a leading indication for liver transplantation.4 Does the US, the largest health care market by many measures, have a growing talent base to address the sheer magnitude of fatty liver disease and associated complications?
As illustrated in Figure 1, recent searches on Indeed.com, a major careers website, revealed ~33 open jobs associated with NAFLD, the acronym presently most associated with fatty liver disease. For the phrase “fatty liver”? There are 126 open jobs.
FIGURE 1.
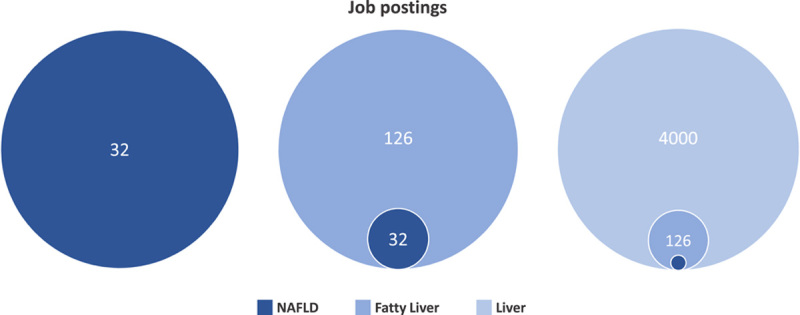
Job postings on Indeed.com associated with NAFLD, fatty liver, and liver in 2023.
What happens when we zoom out and search for just the word “liver”? We see ~4000 open jobs.
Thus, even though NAFLD prevalence dominates other liver diseases proportionally, the open postings for fatty liver-oriented roles seem trivial compared with overall liver-associated ones.
Figure 2 illustrates what happens when we zoom out more broadly to other disease and public health risk categories, recognizing that they may overlap or may involve dual diagnoses. Similar searches revealed over 120,000 open jobs associated with the word “cancer”. For the phrase “heart disease?” Just shy of 34,000 open jobs. For the word diabetes? Just over 23,000 jobs.
FIGURE 2.
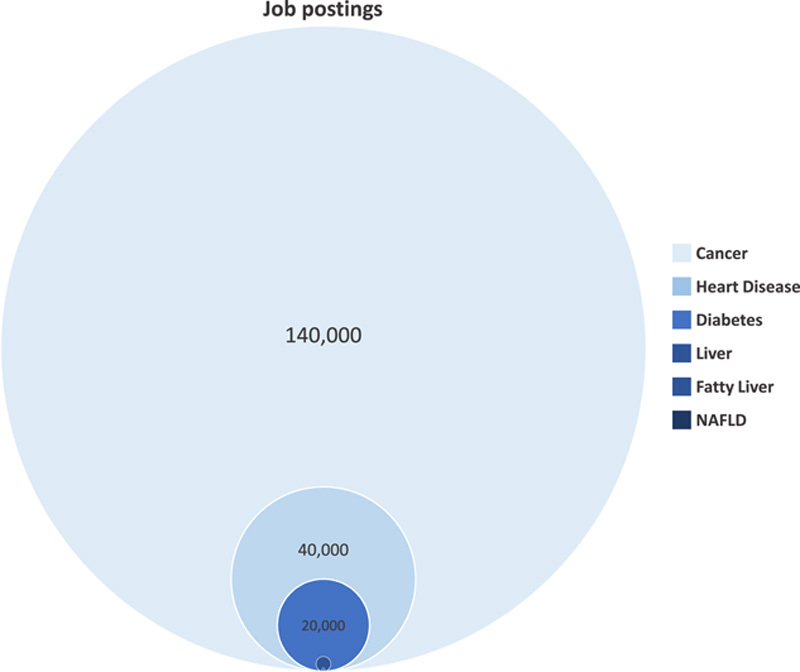
Job postings on Indeed.com associated with cancer, heart disease, diabetes, liver, fatty liver, and NAFLD in 2023.
Compared with most disease categories with relatively high mortality (eg, cancer, heart disease, and diabetes), we can see that fatty liver disease in and of itself is not—yet—widely recruiting and broadly developing a global disease-specific “community of practice”. Given the considerable overlap that exists between NAFLD and these other disease entities, there could be indirect liver benefits from these larger job markets. However, we submit that a disease-centric approach that considers fatty liver disease as a standalone entity, and not largely a byproduct of others, would facilitate more substantive research and management efforts that can make a strong impact on disease burden and patient outcomes.
Cognitive anthropologist Jean Lave and educational theorist Etienne Wenger introduced the framing of a “community of practice (CoP)” in 1991.5 They define a CoP as a group of people who “share a concern or a passion for something they do and learn how to do it better as they interact regularly”.5 In public health and health systems, CoPs are often considered and studied within the context of individual workplaces,6 such as a hospital. In other fields—and occasionally in public health and health systems7,8—CoPs are also understood to be global.
Healthy, vibrant CoPs focused on any one public health risk—both global and local—would include paid, professional clinical and research positions. Moreover, we believe that CoPs —global and local—should also include other related professional and volunteer roles. Volunteer roles might include caregivers for the ailing and elderly, unpaid community health workers, or peer advocates assisting those who share a common health risk. Additional paid, professional roles mitigating an identified public health risk might include trainers and educators, community health workers, program officers with NGOs, and dedicated fundraising and development professionals. Extending beyond a disease or health-risk-focused CoP, we anticipate seeing broader communities of interest encompassing common comorbidities.
These examples are meant to be illustrative, not exhaustive. Viewed together, global and local CoPs have several overlapping and aligned roles working over multiple time periods (from exigencies to long-term strategies), generating broader social attention, ultimately drawing increased talent and funding to manage and mitigate the public health threat.9
There are a few educated guesses for why there is such a small CoP for fatty liver disease. They include low overall awareness among broader stakeholders within health systems, public health, and industry; patients—or even health practitioners—not fully appreciating the seriousness of the disease; the perception that multidisciplinary care pathways, all but necessary for addressing fatty liver disease, are likely less profitable or too complicated to implement for US health systems; hurdles for coverage from third-party payers, whether public (government health funds) or private (insurance); and a low sense of urgency due to the slowly progressive course of fatty liver disease, unlike certain noncommunicable diseases (eg, heart disease and many forms of cancer) or among communicable infections (eg, sexually transmitted and respiratory). Most likely, a combination of all of these contributes to the (presently) slow growth of the fatty liver disease CoP.
Fortunately, the global CoP focused on fatty liver disease is not starting from zero. As observed from our analysis of the US, there are some paid professional roles focused on this public health risk. Yet, compared with other disease categories (eg, cancer and heart disease) and even other forms of high mortality and/or morbidity health risks (eg, occupational health and safety), the observable CoP is much smaller and has a much lower overall network effect.
For fatty liver disease, the largest—though still small—established segment of a CoP is among clinical medical positions. Patient advocacy groups have been formed in some countries. Adjacent to clinicians and patient groups sits a modest, though focused, community of researchers and epidemiologists. It is small enough that, globally, many fatty liver disease researchers and epidemiologists are on a first-name basis with one another.
This nascent global CoP (Figure 3) already has some established NGOs including patient advocacy groups and excellent professional associations— just not many in comparison to other major disease categories. Nevertheless, the fatty liver disease CoP presently lacks a long-tenured cadre of highly successful fundraising and development professionals focused on this disease category, when compared with similar career tracks offered in other areas. Still, given the sheer magnitude of the morbidity and mortality reach of fatty liver disease, we believe that all of the types of roles and institutions observed, with respect to other high-mortality disease categories, can, should, and must grow in relation to fatty liver disease.
FIGURE 3.
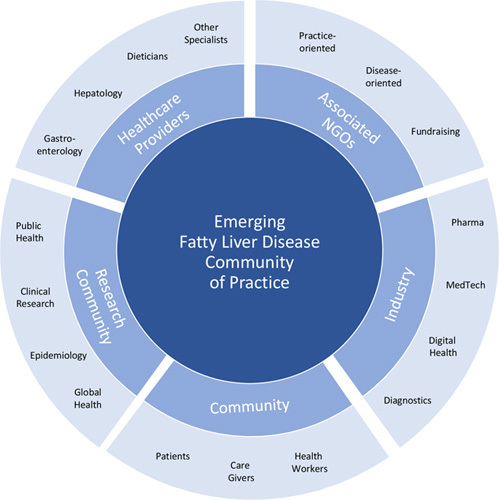
The nascent global community of practice for fatty liver disease.
Enhancing this nascent CoP faces a Catch-22. Professional talent usually wishes to be paid. Even volunteers are usually trained and coordinated by paid talent. Until there is a sufficient network effect from a fatty-liver disease-focused CoP, funding—whether from industry, government, or third-party payers—will often be directed toward other public health risk categories. These include those disease categories that no longer exhibit high rates of mortality in high-income countries, yet continue to have a CoP vested in securing continued funding. Of course, the hurdles and barriers noted must be addressed.
An emerging strategy to grow the fatty liver disease CoP on a global scale is simple, but not easy. It should focus on what we have (eg, patients, clinicians, researchers, and epidemiologists) and draw funding for what this pre-existing CoP requires to dramatically improve health outcomes (eg, multi-country collaborations, more trials that are more inclusive, and multidisciplinary interventions). In parallel, it should generate the adjacent roles needed to grow the global fatty liver disease CoP, increase the CoP’s network effect (measured through roles and funding), and, over time, demonstrate the CoP’s efficacy (measured by reducing the overall burden of fatty liver disease and improving patient outcomes).
Those of us in this effort are already behaving very much like a start-up, forming small teams of professionals with transferable skills from past success in other arenas, securing modest funding, testing proofs of concept, and booking early wins (and failures). Early wins, in particular, will contribute to securing additional funding for research for both pharmacological therapies and nonpharmacological interventions, in line with the global fatty liver disease research priorities agenda.10
Like many start-ups, this team will grow and change over time. Unlike many start-ups, however, our long-term success will be measured in part through: (1) introducing multidisciplinary models of care, (2) fostering health systems-level change, (3) reducing the burden of disease, and (4) growing the global fatty liver disease-centered CoP.
Job postings? Forthcoming funders? More needed! Potential partners and stakeholders? Anticipate our calls.
Acknowledgments
ACKNOWLEDGMENTS
Jeffrey V. Lazarus acknowledges support to ISGlobal from the grant CEX2018-000806-S funded by MCIN/AEI/10.13039/501100011033 and the “Generalitat de Catalunya” through the CERCA Program, outside of this work. Alina M. Allen acknowledges grants support to her institution from the National Institutes of Health (NIH) (DK128127), outside of this work.
CONFLICTS OF INTEREST
Jeffrey V. Lazarus acknowledges grants and speaker fees from AbbVie, Gilead Sciences, MSD, and Roche Diagnostics to his institution, speaker fees from Intercept, Janssen, Novo Nordisk, and ViiV, and consulting fees from Novavax, outside of this work. Zobair M. Younossi acknowledges consulting fees from Quest, Abbott, Astra Zeneca, Bristol-Myers Squibb, Gilead Sciences, Intercept, Madridgal, Merck, Novo Nordisk, and Siemens Healthineers, outside of this work. Alina M. Allen acknowledges grant support to her institution from Novo Nordisk, Pfizer, and Target Pharma and advisory board participation for Novo Nordisk, outside of this work. Christopher J. Kopka has no conflicts of interest to disclose.
Footnotes
Abbreviation: CoP, community of practice.
Contributor Information
Jeffrey V. Lazarus, Email: jeffrey.lazarus@isglobal.org.
Christopher J. Kopka, Email: chriskopka@yahoo.com.
Zobair M. Younossi, Email: zobair.younossi@inova.org.
Alina M. Allen, Email: allen.alina@mayo.edu.
REFERENCES
- 1.Younossi ZM, Golabi P, Paik JM, Henry A, Van Dongen C, Henry L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology. 2023;77:1335–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sweeny KF, Lee CK. Nonalcoholic fatty liver disease in children. Gastroenterol Hepatol. 2021;17:1335–47. [PMC free article] [PubMed] [Google Scholar]
- 3.Wong VW, Lazarus JV. Prognosis of MAFLD vs. NAFLD and implications for a nomenclature change. J Hepatol. 2021;75:1284–91. [DOI] [PubMed] [Google Scholar]
- 4.Cheemerla S, Balakrishnan M. Global epidemiology of chronic liver disease. Clinical Liver Disease. 2021;17:365–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge: Cambridge University Press; 1991. doi: 10.1017/CBO9780511815355. [DOI] [Google Scholar]
- 6.Terry DR, Nguyen H, Peck B, Smith A, Phan H. Communities of practice: a systematic review and meta-synthesis of what it means and how it really works among nursing students and novices. J Clin Nurs. 2020;29:370–80. [DOI] [PubMed] [Google Scholar]
- 7.Li LC, Grimshaw JM, Nielsen C, Judd M, Coyte PC, Graham ID. Use of communities of practice in business and health care sectors: a systematic review. Implementation Sci. 2009;4:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silverstein A, Benson A, Gates C, Nguyen D. Global community of practice: a means for capacity and community strengthening for health professionals in low- and middle-income countries. J Glob Health. 2022;12:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazarus JV, Mark HE, Anstee QM, Arab JP, Batterham RL, Castera L, et al. Advancing the global public health agenda for NAFLD: a consensus statement. Nature Rev Gastroenterol Hepatol. 2022;19:60–78. [DOI] [PubMed] [Google Scholar]
- 10.Lazarus JV, Mark HE, Allen AM, Arab JP, Carrieri P, Noureddin M, et al. A global research priority agenda to advance public health responses to fatty liver disease. J Hepatol. 2023; in press. [DOI] [PubMed] [Google Scholar]


