Abstract
PURPOSE
Early integration of pediatric palliative care (PPC) for children with cancer is critical to improving the quality of life of both the patient and family. Understanding physician perceptions of palliative care and perceived barriers to early integration is necessary to develop PPC in Brazil.
METHODS
The Assessing Doctors' Attitudes on Palliative Treatment survey was modified for use in Brazil. The survey was open from January 2022 to June 2022 and distributed to physicians of all specialties from participating institutions who treat children with cancer. Statistical analysis was complemented by qualitative analysis of open-ended responses.
RESULTS
A total of 272 respondents participated. Most respondents reported access to PPC experts for consultation (77.2%) and 34.5% indicated previous palliative care training. Physician knowledge of PPC was generally aligned with WHO guidance (median alignment, 93.0%; range, 80.5%-98.2%). However, about half (53.3%) felt comfortable addressing physical needs of patients receiving PPC, 35.3% addressing emotional needs, 25.8% addressing spiritual needs, and 33.5% addressing grief and bereavement needs. Most respondents (65.4%) felt palliative care should be involved from diagnosis, but only 10.3% stated that this occurred in their setting. The most important barriers identified were physician discomfort (89.0%), limited physician knowledge (88.6%), and lack of home-based services (83.8%).
CONCLUSION
Despite a strong understanding of the role of palliative care, physicians in Brazil reported low confidence delivering PPC to children with cancer. Additionally, physicians generally believed that PPC should be integrated earlier in the disease trajectory of children with cancer. This work will direct educational and capacity building initiatives to ensure greater access to high-quality PPC for children with cancer in Brazil to address patient and family suffering.
Physicians find barriers that exist in the early integration of palliative care for children with cancer in Brazil.
INTRODUCTION
Pediatric palliative care (PPC) is a critical component of childhood cancer care. Children with cancer experience considerable suffering—physical, psychological, social, and/or spiritual—that is often inadequately relieved.1,2 Studies demonstrate that children with cancer receiving palliative care have improved outcomes, including better symptom management, enhanced quality of life for patients and families, less intervention-focused care at the end of life, fewer deaths in the intensive care unit, and communication between health care professionals and patients/families.3-9 Accordingly, in 2014, the World Health Assembly unanimously passed resolution WHA67.19, declaring palliative care to be an ethical responsibility of health systems.10,11
CONTEXT
Key Objective
What are Brazilian physicians' knowledge and attitudes toward palliative care for children with cancer and the perceived barriers to early integration of care?
Knowledge Generated
Although physicians in Brazil who care for children with cancer had a general understanding of what is palliative care, they were uncomfortable in delivering palliative care services, especially in addressing the emotional, spiritual, and grief and bereavement needs of patients and their families. Additionally, there was a discrepancy between what was perceived as ideal timing of palliative care involvement and what was occurring in practice because of perceived barriers including physician knowledge and discomfort, along with lack of home-based services, among others.
Relevance
These findings will guide educational and capacity building initiatives to build skills delivering palliative care with the goal of improving the quality of life for all children with cancer in Brazil.
However, access to quality palliative care services for children remains limited globally, with more than 65% of countries having no known PPC.12 The greatest need for PPC lies in low- and middle-income countries (LMICs), where limited access to medications, training, national policies that include PPC, public awareness, and financial resources represent significant barriers to PPC delivery.13-15 This gap is of particular concern in childhood cancer care, as 90% of children with cancer live in LMICs.16,17
In 1998, the National Cancer Institute of the Ministry of Health in Brazil introduced an exclusive unit dedicated to palliative care in Rio de Janeiro, the Hospital do Câncer IV.18,19 The palliative care movement grew further in 2005 through the establishment of two key entities: the National Policy for Cancer Care,20 which recognized that palliative care should be integrated into oncologic care, and the National Academy of Palliative Care (ANCP),21 which supported the regularization of palliative care services.22-24 However, much of these efforts have focused on the provision of palliative care in adults.
The Assessing Doctors' Attitudes on Palliative Treatment (ADAPT) survey evaluates physician knowledge and perceptions of palliative care integration for children with cancer and has previously been used in 11 countries in Eastern Europe and Central Asia,25,26 and 17 Spanish-speaking countries in Central and South America.27,28 The objective of this study was to assess physician knowledge and attitudes of palliative care, timing of palliative care consultation, and barriers to the early integration of palliative care for children with cancer in Brazil to inform targeted PPC interventions.
METHODS
IRB Approval
The Office of Human Subjects Research Protections and Institutional Review Board at St Jude Children's Research Hospital (Memphis, TN) approved this study as category 2 exempted research including educational tests and survey procedures. Because of the legal requirements for performing multi-institutional research in Brazil, the National Research Ethics Commission in Brazil also approved the study followed by institutional ethical approval at each participating hospital. Voluntary completion of the survey was considered consent to participate in the study.
Instrument Development
The ADAPT survey was originally developed on the basis of the WHO guidance and a literature review of studies evaluating physician perceptions of palliative care.29-32 The survey was translated into Portuguese and assessed by a team of bilingual experts (A.F.O.d.L., D.A.G.A., P.L., and E.B.) to ensure appropriate syntax and comprehension. The survey then underwent iterative rounds of review to improve content validity and cultural sensitivity and was back-translated to English to confirm construct consistency. Next, five Portuguese-speaking physician representatives of the target specialties piloted the survey, with adjustments made on the basis of feedback. The final survey contained 66 questions, with 62 close-ended items using a 5-point Likert scale (strongly agree to strongly disagree) or a multiple-choice format with four open-ended questions (Data Supplement).
Instrument Distribution Strategy
The ADAPT survey was distributed electronically via the Qualtrics platform33 in Portuguese to physicians who treat children with cancer in Brazil. An institution leader was identified at each participating hospital who identified colleagues appropriate for the study and distributed the survey via email. Surveys were completed anonymously, and participation was optional at all centers. The survey was open from January 2022 to June 2022.
Statistical Analysis
Demographic data were reported via descriptive statistics. For analysis of multiple-choice questions, the 5-point Likert scale was also collapsed into three categories (often/always, sometimes, and never/rarely). To calculate physician alignment with WHO guidance, 15 statements were categorized as in alignment or not in alignment with WHO guidance for PPC (Data Supplement). Each item was marked correct if the respondent indicated moderate or strong alignment with the correct response. Each participant received an overall score for percent alignment on the basis of the number of correct responses of 15 maximum.
Qualitative Analysis
Free-text responses for open-ended questions were translated from Portuguese to English using Google Translate (A.G.) and approved by Portuguese native speakers (P.L., A.d.O.J., and E.B.). The qualitative codebook developed in previous ADAPT studies was used (Data Supplement). Codes were changed or added through iterative review of the free-text responses and memo-writing. Each free-text response served as the unit of analysis for coding. Thematic content analysis focused on components of palliative care, timing to palliative care consultation, and barriers to palliative care involvement in patient care. The qualitative data were managed using MAXQDA 2022 (VERBI Software, Berlin, Germany).34
RESULTS
Sample Demographics
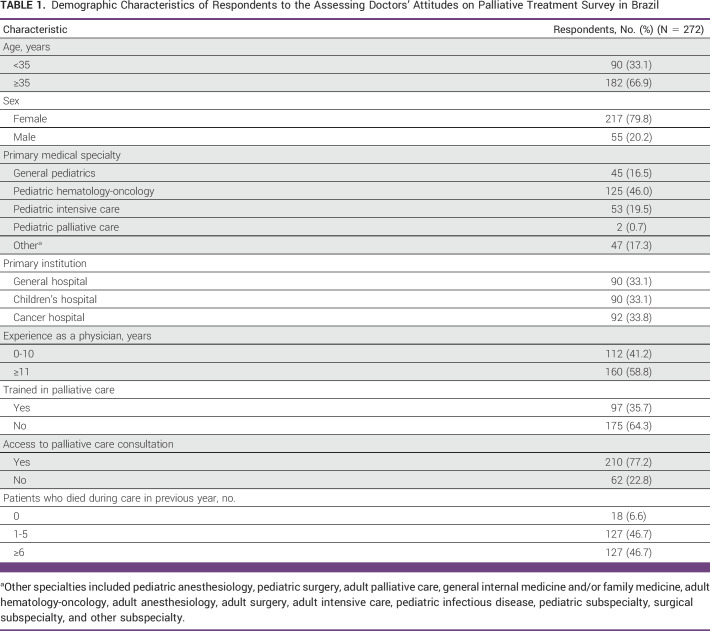
A total of 272 respondents from 14 Brazilian hospitals participated with a median institutional response rate of 53.4% (range, 19.8%-87.0%; Data Supplement). These institutions represented eight different states in Brazil, which make up over 50% of the population of Brazil (Data Supplement). Most respondents were age 35 years or older (66.9%), female (79.8%), and almost half practiced pediatric hematology and/or oncology (46.0%) (Table 1). Other common specialties included general pediatricians (16.5%) and pediatric intensivists (19.5%). The respondents were fairly distributed between general hospitals (33.1%), children's hospitals (33.1%), and dedicated cancer hospitals (33.8%). The majority (77.2%) reported access to a PPC consultation in their practice. Approximately one third of respondents (34.5%) indicated previous training in palliative care. Of those, the most common type of training was a rotation in medical school or postgraduate training (41.2%) or a certificate course (29.9%). Although three participants stated that they had done a residency or fellowship in palliative care, only two respondents identified as a PPC specialist (0.6%) (Data Supplement).
TABLE 1.
Demographic Characteristics of Respondents to the Assessing Doctors' Attitudes on Palliative Treatment Survey in Brazil
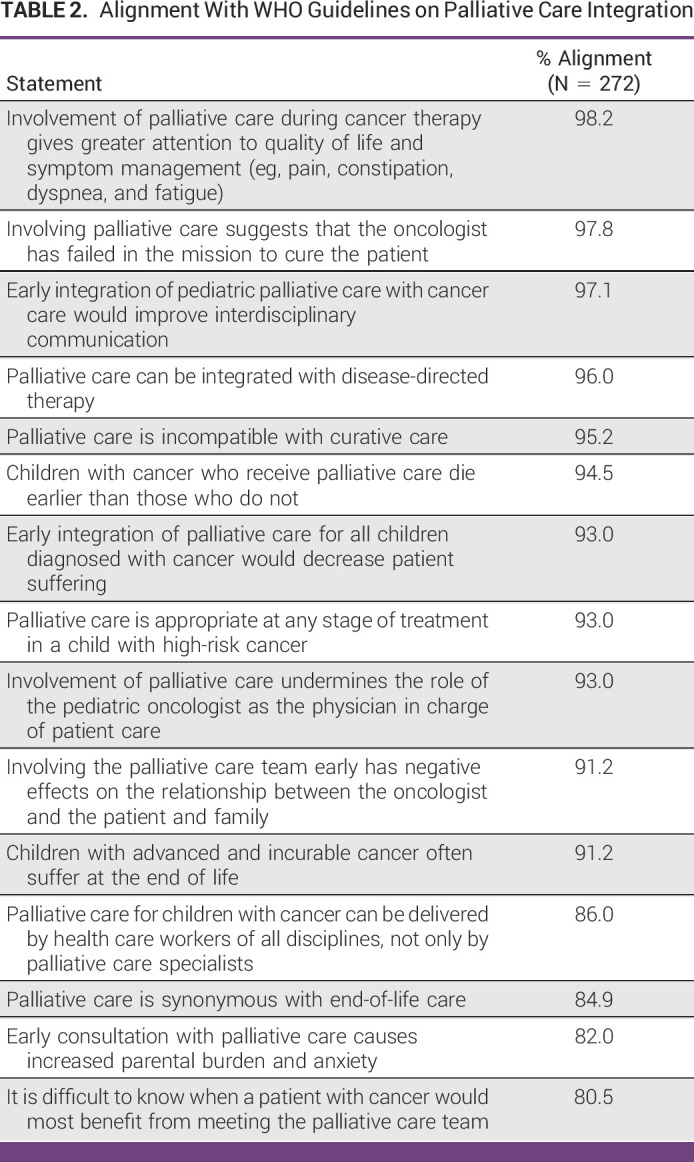
Alignment With WHO Guidance
Physicians demonstrated strong alignment with WHO guidance for PPC (≥90% correct for 11 of 15 statements, Table 2), with a median alignment of 93.0% (range, 80.5%-98.2%).
TABLE 2.
Alignment With WHO Guidelines on Palliative Care Integration
Palliative Care in Practice
Over half of respondents (53.3%) reported they felt confident assessing and treating the physical needs of pediatric patients with serious incurable illness. Physicians felt less confident assessing and treating emotional (35.3%) and spiritual needs (25.8%), as well as the grief and bereavement needs (33.5%) of families. Of respondents, 28.3% reported feeling burdened by their inability to control the suffering of patients at the end of life (Table 3).
TABLE 3.
Physician Confidence in Delivering Palliative Care Services
Most physicians (81.6%) agreed or strongly agreed with the statement that quality of life was often overlooked in the face of cancer-directed treatment. Additionally, 61.9% of respondents stated that in their setting, physicians continue to recommend cancer-directed treatment for children with incurable oncologic disease even when that treatment was unlikely to prolong a child's life.
Timing of Palliative Care Integration
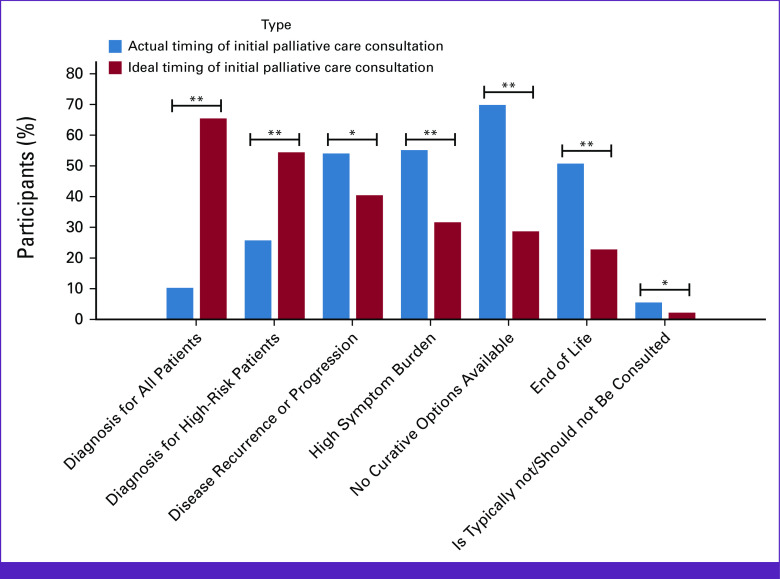
Approximately half (52.9%) of participants believed that palliative care involvement occurred too late in the treatment of children with cancer in their setting. Additionally, only 65.4% reported palliative care consultation was available when needed. When asked about the actual timing of initial palliative care consultation, physicians reported this often occurred when no curative options were available (69.9%; Fig 1). Other common times for initial consultation included when patients had a high symptom burden (55.2%), at disease recurrence or progression (54.0%), and at the end of life (50.7%). By contrast, when asked about the ideal timing of initial palliative care consultation, most physicians indicated that it should occur at diagnosis (65.4%) or for high-risk patients (54.4%).
FIG 1.
Ideal versus actual timing of initial palliative care consultation. Results of 272 physician respondents to the multiple-choice questions asking when an initial palliative care consultation for a child with cancer typically occurs in their practice setting and when they believe is the ideal time it should occur. Participants were able to choose all options that were applicable. The figure shows the percentage of participants who indicated each option. Statistical significance is demonstrated with either a single * for P values of <.05 and ** for values of <.001.
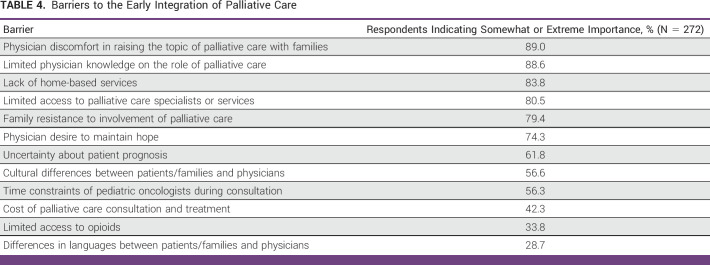
Barriers to Palliative Care Integration
Of 12 perceived barriers to early integration of palliative care mentioned in the survey, nine were indicated as being somewhat or extremely important by at least 50% of respondents (Table 4). The most frequent perceived barriers included physician discomfort (89.0%), limited physician knowledge (88.6%), lack of home-based services (83.8%), limited access to palliative care (80.5%), and family resistance (79.4%).
TABLE 4.
Barriers to the Early Integration of Palliative Care
Free-text responses elaborate highlighted physician knowledge/attitudes was a major barrier impeding early integration of palliative care, because of lack of knowledge of the team about the real meaning of palliation (Data Supplement). Delays in palliative care referral were attributed in part to resistance of the oncology team or obstinate oncologists who, as one participant described, “believe [they] know how to manage symptoms well.” Palliative care integration for children with cancer presented a unique dilemma for physicians, in part because of the team's hope, because it is a pediatric patient, that the patient will be cured of the disease.
Although less common, provision of palliative care was also felt by the respondents to be limited because of the knowledge and attitudes of family members and the wider society. Possible explanations for the perceived resistance of family members ranged from extreme religiosity or religious fanaticism in the family to intellectual limitation of family members. In a broader context, some physicians spoke of how the term palliative care “carries a very bad stigma in [their] society,” grounded in a general “lack of understanding about the scope and objectives of palliative care.”
Some free-text responses addressed a lack of access to palliative care specialists or services as a perceived barrier to early integration of palliative care in the qualitative responses. Physicians described the “lack of [a] structured palliative care service” and “small, specialized team(s) in palliative care,” possibly explained an “insufficient number of qualified personnel for this role.” Accordingly, delivery of PPC often fell on nonpalliative care specialists, in particular oncologists, who had to balance oncologic and palliative care duties: “The palliative care professional is also a pediatric oncologist.”
Even those who had access to palliative care services faced substantial institutional and systemic barriers. Institutional barriers were characterized by the high demand for palliative care services within most institutions, often leading to extremely overworked palliative care team[s]. Physicians also underlined a deficit in multidisciplinary collaboration: lack of multidisciplinary work among pediatric professionals, oncologists, and professionals responsible for palliative care. On a systems level, physicians also mentioned lack of teaching about PC in undergraduate and medical residency and a need for public policies to promote the health of critically ill patients.
Palliative Care Education
Most respondents (97.7%) demonstrated interest in more education on how to provide palliative care to their patients. Nearly all (99.0%) agreed that greater emphasis on palliative care education for doctors and other health care professionals is an important step in improving PPC access. Some participants further expressed how they wish educational initiatives to be implemented, including through distance learning and with a weekly workload accessible to doctors who work throughout the week.”
DISCUSSION
The WHO has called on all Member States to strengthen palliative care as a component of comprehensive care throughout the life course. However, global palliative care services remain inadequate to meet the palliative care needs of pediatric patients with cancer, especially in LMICs. In this study, we found that physicians in Brazil had high alignment to WHO guidance on PPC but were generally uncomfortable addressing the PPC needs of their patients. Additionally, most physicians believed that palliative care for pediatric patients with cancer should be integrated earlier than currently occurred in their practice. This study provides insight into physician perspectives on and identifies barriers to early integration of PPC for children with cancer in Brazil. These findings can be used to build capacity and education to address the discomfort in providing care to children and overcome the barriers identified. It is important to note that these findings were specific to children with cancer, and that further research is needed to understand perspectives and perceived barriers for children with nononcologic diagnoses.
Knowledge of the role of PPC among physicians caring for children with cancer in Brazil was robust. The overall median WHO alignment of 93.0% was higher than that seen in the rest of Latin America (83.0%).27 This high knowledge may be attributed to the steady progression of palliative care development in Brazil. Although many of our participants had no formal palliative care training, PPC access and availability in Brazil is relatively high compared with other countries,25-28 and PPC is considered a component of standard oncologic care. These findings suggest that national policies can advance palliative care knowledge among the medical community.
Despite a strong understanding of palliative care principles, limited physician knowledge and physician discomfort in raising the topic of palliative care were perceived as significant barriers to palliative care integration. These findings may be due to respondents' lack of confidence in delivering PPC services and not their knowledge of palliative care principles. Physicians in Brazil and Latin America were more confident in addressing the physical needs of patients, in comparison with providing emotional, spiritual, and/or grief and bereavement care to patients and family members, suggesting that symptom management is likely prioritized in training over other components, consistent with other Brazilian studies of physician knowledge.35,36 Further efforts are needed for educating, training, and practical experience for physicians caring for children with cancer in Brazil on how to address the emotional, spiritual, and grief and bereavement needs of patients and families beyond physical symptom management.
Another perceived barrier identified by the respondents was family resistance to palliative care involvement. However, this may reflect the feelings of the physician themselves that are transferred to the family more than feelings of the family. There is some evidence in the United States that shows that families are open to PPC involvement from diagnosis with proper introduction to the role of palliative care.37 More research is essential to understand parent and family perceptions of PPC in LMICs.
Barriers to PPC delivery in Brazil identified in this study should be addressed through targeted educational and training aimed at behavior change, such as improving provider communication with patients and families.38 All didactic components of PPC education should be paired with practical skills-based training targeting institution-/region-specific gaps in comfort. Palliative care principles should be embedded from the beginning of medical education to assure exposure regardless of specialist training. At the undergraduate medical student level, only 44 of 315 Brazilian medical schools offer courses in palliative care37 with over half of medical schools' course coordinators reporting insufficient or nonexistent priority given to education in palliative care.39
In addition, PPC training courses should be accessible and feasible for health care workers who are currently in practice, including physicians, nurses, social workers, and psychologists, to leverage the skills and resources of multidisciplinary professionals. The Education in Palliative and End-of-Life Care (EPEC)-Pediatrics program consists of a 24-module course delivered via virtual and in-person sessions. Postier et al40 found that 71.0% of participants saw clinical improvements in the care of children with serious illnesses at their own institutions from participation in EPEC-Pediatrics. The successful implementation of EPEC-Pediatrics is an example of how an educational intervention can increase knowledge as well as proficiency in practical applications of palliative care. This curriculum can be regionally adapted to target specific gaps in PPC delivery identified through research studies such as ADAPT, as has been done in other regions.41
Consistent with previous studies,42 findings in both Brazil and other Spanish-speaking countries in Latin America show that despite access to a PPC expert for consultation, current palliative care services are inadequate to care for all the patients in need of PPC. A recent analysis of palliative care in Latin America found similar results; despite growth of the number of services and acquired expertise, the number of services is not enough to cover needs.43 Therefore, dedicated clinical training opportunities should focus on the practical elements of care to increase capacity and strengthen services to cover the palliative care needs for children with cancer within Brazil.
Additional clinical opportunities such as residencies, fellowships, and externships dedicated to PPC should be made available to increase the palliative care workforce. Pastrana et al44 found both the proportion of medical schools with palliative care at the undergraduate level and the number of accredited physicians working in palliative care to be significantly associated with the number of palliative care services per million inhabitants in Latin America. A 2021 study45 identified 15 palliative medicine subspecialty programs in Brazil—the most of any country in Latin America. However, only one of these subspecialty programs is specific to pediatrics.
Alongside dedicating funds for palliative care specialists, institutions should prioritize formation of designated multidisciplinary palliative care teams including nursing, social work, child-life, and spiritual care experts.46 According to the ANCP in Brazil, <10% of Brazilian hospitals have a multidisciplinary palliative care team.47,48 Thus, progress in PPC relies on initiatives that train PPC professionals beyond physicians to support team-based PPC services. This expansion of PPC services should be accompanied by advocacy at the institutional and national levels to ensure the structural and financial sustainability of palliative care programs.49,50
This study has several limitations. Most participants are from specialized hospitals located in urban regions, especially in southern Brazil. We used an electronic, institution-specific distribution strategy, which may have excluded more remote, poorly resourced, or community-based centers. Thus, this study likely represents a best case scenario of palliative care knowledge and availability in the country. However, because pediatric oncology care is primarily concentrated in these hospitals/regions, we believe that this study is representative of PPC for children with cancer in the country. The target population of this survey were physicians who care for children with cancer as they are often the gatekeepers for consultation of other subspecialty services. However, nurses, psychologists, and social workers represent prominent figures in provision of care for children with cancer, and further research is necessary to investigate the perceptions of the entire multidisciplinary palliative care team. The perspectives of patients and their caregivers are also important viewpoints missing from this analysis.
To our knowledge, the ADAPT study is the largest to evaluate perceptions of PPC integration among physicians who care for children with cancer in Brazil. Across all specialties, Brazilian physicians had a robust understanding of palliative care concepts. However, physicians showed low confidence in delivering palliative care services, especially in addressing the emotional, spiritual, and grief and bereavement needs of patients and their families. In addition, physicians believed that palliative care should be integrated earlier in the care of children with cancer than typically occurred in their setting. Potential barriers that may impede earlier integration of PPC included limited physician knowledge, physician discomfort in raising the topic of palliative care with families, lack of home-based services, limited access to palliative care specialists or services, and perceived family resistance. Future interventions should include educational opportunities for physicians of all specialties to build skills delivering palliative care, more opportunities for PPC specialization, and establishing multidisciplinary palliative care teams, with the goal of improving the quality of life for all children with cancer in Brazil.
ACKNOWLEDGMENT
The authors acknowledge the incredible support of all the institutions and country leaders who were a part of the ADAPT Brazil team in assisting the distribution of the survey. These individuals include Dr Pablo Santiago, Dr Marcelo Milone, Dr Camila Cancela, Dr Lauro José Gregianin, Dr Carolina Madalena Souza Pinto Alvares, Dr Patrick Rezende Godinho, Dr Sarue Brizola Ocampos, Dr Viviany de Oliveria Viana, Dr Silviana Vieira Ramos Alves, Dr Joaquim Caetano de Aguirre Neto, Dr Gabriela Caus Fernandes Luiz Canali, and Eden Robertson.
André de Oliveira Junior
Employment: Hospital de Amor de Barretos
Travel, Accommodations, Expenses: St Jude Children's Research Hospital
Glaucia Regina Costa Murra
Employment: Barretos Cancer Hospital
Honoraria: Barretos Cancer Hospital
Travel, Accommodations, Expenses: Barretos Cancer Hospital
Monika L. Metzger
Research Funding: Seagen
Meenakshi Devidas
Honoraria: Novartis, Merck
Asya Agulnik
Research Funding: National Cancer Institute
No other potential conflicts of interest were reported.
PRIOR PRESENTATION
Presented in part at the International Society of Pediatric Oncology (SIOP) Conference, Barcelona, Spain, October 1, 2022.
SUPPORT
Supported by the American Lebanese Syrian Associated Charities.
M.J.M. and A.G. are cofirst authors.
AUTHOR CONTRIBUTIONS
Conception and design: Michael J. McNeil, Patricia Loggetto, Dileiny Antunes Geronutti Ayub, Allan Francisco Oliveira de Lima, Paola Friedrich, Monika L. Metzger, Asya Agulnik, Justin N. Baker
Financial support: Justin N. Baker
Administrative support: Patricia Loggetto, André de Oliveira Junior, Glaucia Regina Costa Murra, Paola Friedrich, Justin N. Baker
Provision of study materials or patients: Glaucia Regina Costa Murra, Aline Esmeraldo Andrade de Almeida, Julia Lopes Garcia, Anna Beatriz Costa Neves do Amaral, Iêda Cristina Cunha Ferreira e Fonseca
Collection and assembly of data: Michael J. McNeil, Patricia Loggetto, André de Oliveira Junior, Erica Boldrini, Glaucia Regina Costa Murra, Dileiny Antunes Geronutti Ayub, Allan Francisco Oliveira de Lima, Aline Esmeraldo Andrade de Almeida, Julia Lopes Garcia, Anna Beatriz Costa Neves do Amaral, Iêda Cristina Cunha Ferreira e Fonseca, Paola Friedrich, Meenakshi Devidas, Justin N. Baker
Data analysis and interpretation: Michael J. McNeil, Godwin Job, Dileiny Antunes Geronutti Ayub, Allan Francisco Oliveira de Lima, Paola Friedrich, Monika L. Metzger, Meenakshi Devidas, Asya Agulnik, Justin N. Baker
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
André de Oliveira Junior
Employment: Hospital de Amor de Barretos
Travel, Accommodations, Expenses: St Jude Children's Research Hospital
Glaucia Regina Costa Murra
Employment: Barretos Cancer Hospital
Honoraria: Barretos Cancer Hospital
Travel, Accommodations, Expenses: Barretos Cancer Hospital
Monika L. Metzger
Research Funding: Seagen
Meenakshi Devidas
Honoraria: Novartis, Merck
Asya Agulnik
Research Funding: National Cancer Institute
No other potential conflicts of interest were reported.
REFERENCES
- 1. Wolfe J, Grier HE, Klar N, et al. Symptoms and suffering at the end of life in children with cancer. N Engl J Med. 2000;342:326–333. doi: 10.1056/NEJM200002033420506. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Integrating Palliative Care and Symptom Relief Into Paediatrics: A WHO Guide for Health Care Planners, Implementers and Managers. Geneva: World Health Organization; 2018. [Google Scholar]
- 3. Snaman J, Kaye EC, Lu JJ, et al. Palliative care involvement is associated with less intensive end-of-life care in adolescent and young adult oncology patients. J Palliat Med. 2017;20:509–516. doi: 10.1089/jpm.2016.0451. [DOI] [PubMed] [Google Scholar]
- 4. Snaman J, McCarthy S, Wiener L, et al. Pediatric palliative care in oncology. J Clin Oncol. 2020;38:954–962. doi: 10.1200/JCO.18.02331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ullrich C, Lehmann L, London WB, et al. End-of-life care patterns associated with pediatric palliative care among children who underwent hematopoietic stem cell transplant. Biol Blood Marrow Transpl. 2016;22:1049–1055. doi: 10.1016/j.bbmt.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vern-Gross T, Lam CG, Graff Z, et al. Patterns of end-of-life care in children with advanced solid tumor malignancies enrolled on a palliative care service. J Pain Symptom Manage. 2015;50:305–312. doi: 10.1016/j.jpainsymman.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wolfe J, Hammel JF, Edwards KE, et al. Easing of suffering in children with cancer at the end of life: Is care changing? J Clin Oncol. 2008;26:1717–1723. doi: 10.1200/JCO.2007.14.0277. [DOI] [PubMed] [Google Scholar]
- 8. Kaye E, Friebert S, Baker JN. Early integration of palliative care for children with high-risk cancer and their families. Pediatr Blood Cancer. 2016;63:593–597. doi: 10.1002/pbc.25848. [DOI] [PubMed] [Google Scholar]
- 9. Levine DR, Mandrell BN, Sykes A, et al. Patients’ and parents’ needs, attitudes, and perceptions about early palliative care integration in pediatric oncology. JAMA Oncol. 2017;3:1214–1220. doi: 10.1001/jamaoncol.2017.0368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Resolution WHA67.19 Strengthening of palliative care as a component of comprehensive care throughout the life course. Sixty-Seventh World Health Assembly, Geneva, May 19–24, 2014. http://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_R19-en.pdf .
- 11.Connor SR, Morris C, Jaramillo E, et al. Global Atlas of Palliative Care. London: Global Atlas of Palliative Care; 2020. [Google Scholar]
- 12. Knapp C, Woodworth L, Wright M, et al. Pediatric palliative care provision around the world: A systematic review. Pediatr Blood Cancer. 2011;57:361–368. doi: 10.1002/pbc.23100. [DOI] [PubMed] [Google Scholar]
- 13. Caruso Brown AE, Howard SC, Baker JN, et al. Reported availability and gaps of pediatric palliative care in low- and middle-income countries: A systematic review of published data. J Palliat Med. 2014;17:1369–1383. doi: 10.1089/jpm.2014.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Downing J, Powell RA, Marston J, et al. Children’s palliative care in low- and middle-income countries. Arch Dis Child. 2016;101:85–90. doi: 10.1136/archdischild-2015-308307. [DOI] [PubMed] [Google Scholar]
- 15. Downing J, Boucher S, Daniels A, et al. Paediatric palliative care in resource-poor countries. Children. 2018;5:27. doi: 10.3390/children5020027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bhakta N, Force LM, Allemani C, et al. Childhood cancer burden: A review of global estimates. Lancet Oncol. 2019;20:e42–e53. doi: 10.1016/S1470-2045(18)30761-7. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization . CureAll Framework: WHO Global Initiative for Childhood Cancer. Geneva: World Health Organization; 2021. [Google Scholar]
- 18.Instituto Nacional de Câncer . Jornada discute importância dos cuidados paliativos para pacientes oncológicos [in Portugese] https://www.gov.br/inca/pt-br/assuntos/noticias/2021/jornada-discute-importancia-dos-cuidados-paliativos-para-pacientes-oncologicos. [Google Scholar]
- 19.Ministério da Saúde, Portaria no2439/GM de 08/12/2005 . Política Nacional de Atenção Oncológica. Brasil: Ministério da Saúde; 2005. [Google Scholar]
- 20.Academia Nacional de Cuidados Paliativos . ANCP and palliative care in Brazil [in Portugese] https://paliativo.org.br/cuidados-paliativos/cuidados-paliativos-no-brasil/ [Google Scholar]
- 21. Floriani CA. Palliative care in Brazil: A challenge to the health-care system. Palliat Care Res Treat. 2008;2:19–23. [Google Scholar]
- 22. Fonseca A, Fini D. An overview of Brazilian palliative care. Hos Pal Med Int Jnl. 2017;1:54–55. [Google Scholar]
- 23. Migowski A, Tavares de Moraes Atty A, Tomazelli JG, et al. 30 Years of oncological care in the Brazilian national health system. Rev Bras Cancerol. 2018;64:241–244. [Google Scholar]
- 24. Paiva CF, Santos TCF, Aperibense PGGdS, et al. Historical aspects in pain management in palliative care in an oncological reference unit. Rev Bras Enferm. 2021;74:e20200761. doi: 10.1590/0034-7167-2020-0761. [DOI] [PubMed] [Google Scholar]
- 25. Ehrlich BS, Movsisyan N, Batmunkh T, et al. A multicountry assessment in Eurasia: Alignment of physician perspectives on palliative care integration in pediatric oncology with World Health Organization guidelines. Cancer. 2020;126:3777–3787. doi: 10.1002/cncr.33001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ehrlich BS, Movsisyan N, Batmunkh T, et al. Barriers to the early integration of palliative care in pediatric oncology in 11 Eurasian countries. Cancer. 2020;126:4984–4993. doi: 10.1002/cncr.33151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McNeil MJ, Ehrlich BS, Wang H, et al. Physician perceptions of palliative care for children with cancer in Latin America. JAMA Netw Open. 2022;5:e221245. doi: 10.1001/jamanetworkopen.2022.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McNeil MJ, Ehrlich B, Wang H, et al. Ideal vs actual timing of palliative care integration for children with cancer in Latin America. JAMA Netw Open. 2023;6:e2251496. doi: 10.1001/jamanetworkopen.2022.51496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dalberg T, Jacob-Files E, Carney PA, et al. Pediatric oncology providers’ perceptions of barriers and facilitators to early integration of pediatric palliative care. Pediatr Blood Cancer. 2013;60:1875–1881. doi: 10.1002/pbc.24673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pifer PM, Farrugia MK, Mattes MD. Comparative analysis of the views of oncologic subspecialists and palliative/supportive care physicians regarding advanced care planning and end-of-life care. Am J Hosp Palliat Care. 2018;35:1287–1291. doi: 10.1177/1049909118763592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sanchez Varela AM, Johnson LM, Kane JR, et al. Ethical decision making about end-of-life care issues by pediatric oncologists in economically diverse settings. J Pediatr Hematol Oncol. 2015;37:257–263. doi: 10.1097/MPH.0000000000000271. [DOI] [PubMed] [Google Scholar]
- 32. Friedrichsdorf SJ, Remke S, Hauser J, et al. Development of a pediatric palliative care curriculum and dissemination model: Education in Palliative and End-of-Life Care (EPEC) Pediatrics. J Pain Symptom Manage. 2019;58:707–720.e3. doi: 10.1016/j.jpainsymman.2019.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qualtrics, version 2022. Seattle, WA, Qualtrics; 2005. https://www.qualtrics.com/ [Google Scholar]
- 34. Schönfelder W. CAQDAS and Qualitative Syllogism Logic-NVivo 8 and MAXQDA 10 compared. Forum Qual Soc Res. 2011;12:21. [Google Scholar]
- 35. Naufel LZ, Sarno MTCD, Alves MAJ. O conhecimento médico a respeito das diversas religiões nos cuidados pediátricos. Rev Paul Pediat. 2019;37:479–485. doi: 10.1590/1984-0462/;2019;37;4;00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Záu Serpa de Araujo L, Záu Serpa de Araujo C. Importance of education in palliative care. Palliat Med Care Int J. 2018;1:18–19. [Google Scholar]
- 37. Levine DR, Mandrell BN, Sykes A, et al. Patients' and parents' needs, attitudes, and perceptions about early palliative care integration in pediatric oncology. JAMA Oncol. 2017;3:1214–1220. doi: 10.1001/jamaoncol.2017.0368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Castro AA, Taquette SR, Marques NI. Cuidados paliativos: Inserção do ensino nas escolas médicas do Brasil. Rev Bras Educ Med. 2021;45:e56. [Google Scholar]
- 39. de Toledo AP, Priolli DG. Cuidados no Fim da Vida: O Ensino Médico no Brasil. Rev Bras Educ Med. 2012;36:109–117. [Google Scholar]
- 40. Postier A, Wolfe J, Hauser J, et al. Education in Palliative and End-of-Life Care-Pediatrics: Curriculum use and dissemination. J Pain Symptom Manage. 2022;63:349–358. doi: 10.1016/j.jpainsymman.2021.11.017. [DOI] [PubMed] [Google Scholar]
- 41. McNeil MJ, Ehrlich B, Yakimkova T, et al. Regional adaptation of the Education in Palliative and End-of-Life Care Pediatrics (EPEC-Pediatrics) curriculum in Eurasia. Cancer Med. 2023;12:3657–3669. doi: 10.1002/cam4.5213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sanchez Varela AM, Dussel V, Barfield R, et al. Perceived resources and barriers to pediatric palliative care AmongHealthCare practitioners attending the V Latin American Palliative Care Association (ALCP) meeting. J Pain Symptom Manage. 2011;41:306. [Google Scholar]
- 43. Pastrana T, Centeno C, De Lima L. Palliative care in Latin America from the professional perspective: A SWOT analysis. J Palliat Med. 2015;18:429–437. doi: 10.1089/jpm.2014.0120. [DOI] [PubMed] [Google Scholar]
- 44. Pastrana T, Torres-Vigil I, De Lima L. Palliative care development in Latin America: An analysis using macro indicators. Palliat Med. 2014;28:1231–1238. doi: 10.1177/0269216314538893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Pastrana T, De Lima L, Stoltenberg M, et al. Palliative medicine specialization in Latin America: A comparative analysis. J Pain Symptom Manage. 2021;62:960–967. doi: 10.1016/j.jpainsymman.2021.04.014. [DOI] [PubMed] [Google Scholar]
- 46. Freitas R, Costa de Oliveira L, Mendes GLQ, et al. Barreiras para o encaminhamento para o cuidado paliativo exclusivo: A percepção do oncologista. Saúde Debate. 2022;46:331–345. [Google Scholar]
- 47.Brazilian National Academy of Palliative Care . Panorama dos cuidados paliatives no Brasil. 2018. https://paliativo.org.br/wp-content/uploads/2018/10/Panorama-dos-Cuidados-Paliativos-no-Brasil-2018.pdf . [Google Scholar]
- 48. Laís Záu Serpa A, Carolina Záu Serpa A, Luiz Henrique Rosendo B, et al. Palliative care in the Brazilian health system. Palliat Med Care Int J. 2019;2:118–123. [Google Scholar]
- 49. Pettus KI, de Lima L. Palliative care advocacy: Why does it matter? J Palliat Med. 2020;23:1009–1012. doi: 10.1089/jpm.2019.0696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Pantilat SZ. Leveraging external resources to grow and sustain your palliative care program: A call to action. J Palliat Med. 2012;15:25–28. doi: 10.1089/jpm.2011.0280. [DOI] [PMC free article] [PubMed] [Google Scholar]