Abstract
Introduction
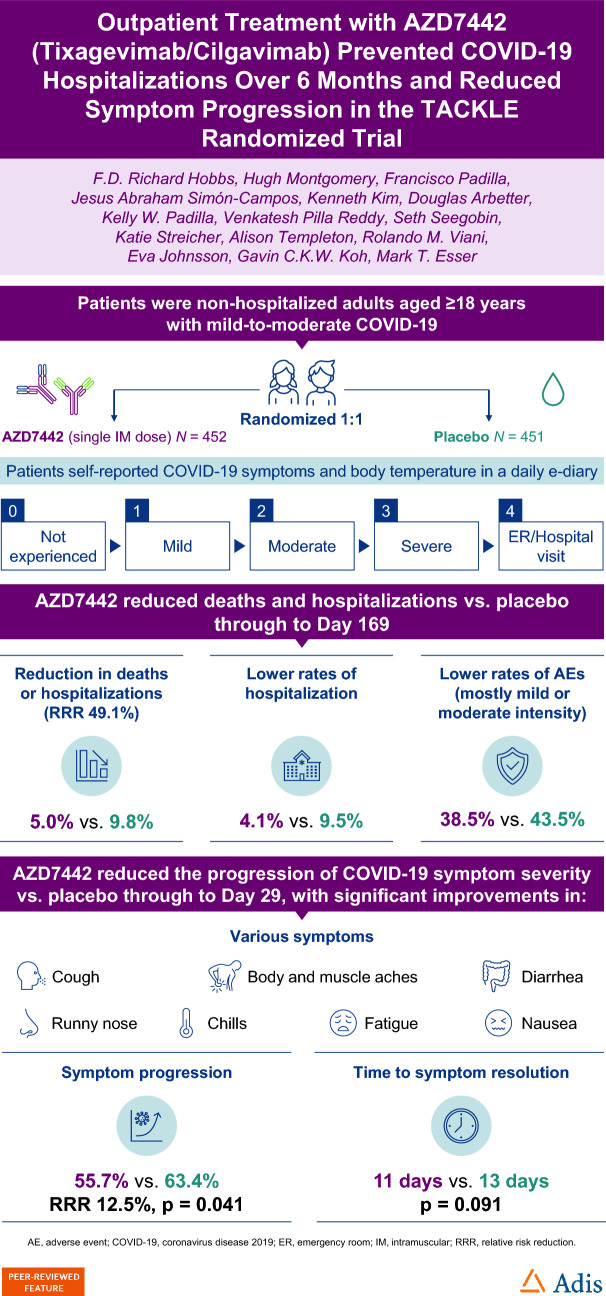
We assessed effects of AZD7442 (tixagevimab/cilgavimab) on deaths from any cause or hospitalizations due to coronavirus disease 2019 (COVID-19) and symptom severity and longer-term safety in the TACKLE adult outpatient treatment study.
Methods
Participants received 600 mg AZD7442 (n = 452) or placebo (n = 451) ≤ 7 days of COVID-19 symptom onset.
Results
Death from any cause or hospitalization for COVID-19 complications or sequelae through day 169 (key secondary endpoint) occurred in 20/399 (5.0%) participants receiving AZD7442 versus 40/407 (9.8%) receiving placebo [relative risk reduction (RRR) 49.1%; 95% confidence interval (CI) 14.5, 69.7; p = 0.009] or 50.7% (95% CI 17.5, 70.5; p = 0.006) after excluding participants unblinded before day 169 for consideration of vaccination). AZD7442 reduced progression of COVID-19 symptoms versus placebo through to day 29 (RRR 12.5%; 95% CI 0.5, 23.0) and improved most symptoms within 1–2 weeks. Over median safety follow-up of 170 days, adverse events occurred in 174 (38.5%) and 196 (43.5%) participants receiving AZD7442 or placebo, respectively. Cardiac serious adverse events occurred in two (0.4%) and three (0.7%) participants receiving AZD7442 or placebo, respectively.
Conclusions
AZD7442 was well tolerated and reduced hospitalization and mortality through 6 months, and symptom burden through 29 days, in outpatients with mild-to-moderate COVID-19.
Clinical Trial Registration
Clinicaltrials.gov, NCT04723394. (https://beta.clinicaltrials.gov/study/NCT04723394).
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1007/s40121-023-00861-7.
Keywords: COVID-19, Hospitalization, Monoclonal antibodies, SARS-CoV-2, Symptoms, AZD7442, Tixagevimab, Cilgavimab
Plain Language Summary
Antibodies are proteins produced by the body’s immune system to specifically combat foreign substances, such as viruses. Tixagevimab and cilgavimab are a pair of antibodies that bind to a specific part of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19). When they bind to the virus, they reduce its ability to cause disease. These antibodies were tested in a clinical trial to see if they could prevent people with COVID-19 from being hospitalized or dying. Around 900 adults took part in this clinical trial. These people all had COVID-19 but were not sick enough to be in hospital. Half of this group were treated with a dose of tixagevimab and cilgavimab, given as two injections. The other half received a placebo (injections that look exactly like the tixagevimab and cilgavimab injections but contain no medicine). The study found that, over 6 months, people with COVID-19 who received tixagevimab and cilgavimab were less likely to need to go to hospital than people who received the placebo. They were also less likely to die of COVID-19. Tixagevimab and cilgavimab also helped to improve COVID-19 symptoms. People who received the antibodies saw their symptoms improve faster than people who received the placebo. They were also less likely to have symptoms that got worse. Most people felt better within 1–2 weeks of getting treatment. No safety issues were found with tixagevimab and cilgavimab compared with placebo.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40121-023-00861-7.
Key Summary Points
| Why carry out this study? |
| There is a continuing need for effective coronavirus disease 2019 (COVID-19) treatments to prevent severe disease and persistent symptoms, and reduce risk of hospitalization and death in at-risk individuals. |
| The TACKLE phase 3 outpatient treatment study showed that a single 600 mg intramuscular administration of AZD7442 (tixagevimab/cilgavimab) within 7 days of symptom onset significantly reduced progression to severe COVID-19 or death through day 29. Here, we present secondary efficacy endpoints and longer-term safety data. |
| What was learned from this study? |
| In unvaccinated individuals with mild-to-moderate COVID-19, 600 mg of AZD7442 reduced death from any cause and COVID-19-related hospitalization through 6 months and reduced COVID-19 symptom burden through 29 days; however, the study was conducted prior to emergence of Omicron. |
| AZD7442 was well tolerated through 6 months, safety was consistent with prior studies, and there was no increased risk of cardiac severe adverse events. |
| These extended follow-up data confirm the findings of the TACKLE primary analysis and suggest that intramuscular administration of virus-specific antibodies can be used to treat patients with mild-to-moderate COVID-19 in an outpatient setting. |
Digital Features
This article is published with digital features, including a graphical abstract, to facilitate understanding of the article. To view digital features for this article go to: 10.6084/m9.figshare.23968905.
Introduction
Coronavirus disease 2019 (COVID-19) continues to have a significant impact on healthcare systems [1], and morbidity rates, including hospitalizations and self-reported long COVID, remain substantially high [2, 3]. Furthermore, while vaccination against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection reduces severe disease risk, breakthrough infections may still result in prolonged COVID-19 symptoms [4], with 200 million individuals globally estimated to currently experience or have previously experienced post-acute sequelae of COVID-19 (“long COVID”) [5]. Persistent health issues following COVID-19, such as cardiovascular disease, diabetes, and mental health disorders, add to the healthcare burden [6–8]. There is, therefore, a continuing need for effective COVID-19 treatments to prevent severe disease, persistent symptoms, hospitalization, and death in at-risk individuals such as older adults, those with multiple comorbidities, and those who are immunocompromised [9–12].
AZD7442 is a combination of two extended-half-life monoclonal antibodies (tixagevimab and cilgavimab) that bind to the SARS-CoV-2 spike protein receptor-binding domain [13]. AZD7442 demonstrated residual in vitro neutralization activity against the original SARS-CoV-2 and variants of concern [13]. In the primary analysis of the phase 3 TACKLE outpatient treatment study, 600 mg intramuscular (IM) AZD7442 was well tolerated and significantly reduced progression to severe COVID-19 or death through day 29 by 50.5% when administered within 7 days of symptom onset [14].
Here, we present additional data from the TACKLE study, describing secondary efficacy results, longer-term safety, and an analysis of AZD7442 for reducing self-reported COVID-19 symptom severity, symptom progression, and time to symptom resolution.
Methods
Study Design and Participants
TACKLE was a phase 3, randomized, double-blind, placebo-controlled, multicenter, outpatient treatment study conducted at 95 sites worldwide (clinicaltrials.gov identifier: NCT04723394) [14].
The study was conducted in accordance with the Good Clinical Practice guidelines and the Declaration of Helsinki, Council for International Organizations of Medical Sciences International Ethical guidelines, applicable International Conference on Harmonisation Good Clinical Practice guidelines, and all applicable laws and regulations. The protocol was reviewed and approved by an institutional review board or ethics committee at the respective study sites (Table S1). No identifiable patient data have been included in this manuscript.
Participants were nonhospitalized adults aged ≥ 18 years with documented, laboratory-confirmed SARS-CoV-2 infection, and a World Health Organization Clinical Progression Scale score of > 1 to < 4, who had not received a COVID-19 vaccine. Participants were randomized 1:1 and within 7 days of onset of COVID-19 symptoms were administered 600 mg AZD7442 (consecutive 3 ml IM injections of 300 mg tixagevimab and 300 mg cilgavimab) or saline placebo (two consecutive 3 ml IM injections). Participants who received study drug could request to be unblinded any time after day 30 to consider receiving a COVID-19 vaccine and remain in the study.
Recruitment for this trial took place between 28 January 2021 and 22 July 2021 [14], when the dominant SARS-CoV-2 variants were Alpha and Delta. The study had a follow-up period of 457 days. The primary efficacy endpoint, and safety data through to day 29, have been reported (primary data cutoff: 21 August 2021) [14]. Herein, we report secondary data (extended data cutoff: 14 January 2022) for participants who completed at least 169 days of follow-up. There were no formal assessments between day 169 and day 365. At the time of the extended data cutoff, most participants had not reached day 365 and therefore have 169 days recorded as their follow-up time.
Outcomes and Procedures
The key secondary efficacy endpoint was a composite of either death from any cause or hospitalization for COVID-19 complications or sequelae through to day 169. Hospitalization was defined as ≥ 24 h of acute care in a hospital or similar acute care facility, including emergency rooms (ERs), temporary facilities instituted (due to a shortage of hospital beds) to address the medical needs of those with severe COVID-19 during the pandemic, and appropriate home care settings.
Safety was assessed on the basis of the incidence of adverse events (AEs), serious AEs (SAEs), and AEs of special interest (including anaphylaxis and other serious hypersensitivity reactions). Serious AEs and AE severity ratings are defined in the Supplementary Appendix.
Additional secondary efficacy endpoints included an assessment of participant-reported COVID-19 symptoms through to day 29. Participants self-reported their COVID-19 symptoms and temperature each evening in an e-diary, which was reviewed by study staff with each participant at study visits. Participants used the diary to self-report on the following symptoms: temperature; shortness of breath; difficulty breathing; chills; cough; fatigue; muscle aches; body aches; headache; loss of taste; loss of smell; sore throat; congestion; runny nose; nausea; vomiting; and diarrhea. Symptom severity was self-reported using a protocol-defined scoring system as follows: 0, not experienced; (1) mild (no interference with daily activity); (2) moderate (some interference with daily activity); (3) severe (significant; prevents daily activity); (4) ER or hospital visit. Progression of COVID-19-associated symptoms through to day 29 was defined as an increase in severity of ≥ 1 COVID-19-associated symptoms by a score of ≥ 1 from baseline. Duration of fever through day 29 was defined as the last day in the participant-reported e-diary on which a temperature of > 37.8 °C was recorded or a potentially antipyretic drug, such as acetaminophen or ibuprofen, was taken.
AZD7442 pharmacokinetics were assessed as described previously [14].
Statistical Analysis
Efficacy analyses were performed using the modified full analysis set (mFAS), comprising all participants in the FAS (all randomized participants who received study drug) who were administered study drug within 7 days of symptom onset and were not hospitalized at baseline (day 1) for isolation purposes. Safety analyses were performed using the safety analysis set, comprising all participants who received study drug, regardless of baseline hospitalization status (hospitalization was only allowed for isolation purposes due to requirements in Japan and Russia). AZD7442 pharmacokinetics were determined using the pharmacokinetic analysis set, comprising all participants who received AZD7442 with ≥ 1 quantifiable serum pharmacokinetic observation.
The key secondary efficacy endpoint was analyzed when all participants completed their day 169 visit using a Cochran–Mantel–Haenszel (CMH) test stratified by time of study drug dosing from symptom onset (≤ 5 versus > 5 days) and risk of progression to severe COVID-19 (high versus low). Participants who were unblinded and/or received a COVID-19 vaccine after day 30 were included in the analysis. Participants who discontinued or were lost to follow-up before day 169 were considered missing. Sensitivity analyses were performed whereby missing response data were imputed using a multiple imputation method with placebo event rates and observed event rates. Another sensitivity analysis was performed that excluded participants who were unblinded prior to day 169 for consideration of COVID-19 vaccination by considering them as missing. A subgroup analysis was performed according to participants’ baseline SARS-CoV-2 serostatus (positive or negative). Kaplan–Meier curves were used to summarize time to key secondary endpoint events up to day 169, and a Cox proportional hazards model was used to generate a hazard ratio (HR) and 95% confidence interval (CI), with the stratification factors included as covariates. The difference between the groups was assessed via a stratified log-rank test. Absence of data following participants’ withdrawal/lost to follow-up was treated as missing and censored at the date of last known status.
The proportion of participants who underwent different types of hospitalization, and the duration of hospital and intensive care unit (ICU) stay, were analyzed descriptively.
The proportion of participants with progression through to day 29 of ≥ 1 COVID-19-associated symptoms to worse severity than recorded before start of treatment was compared using a stratified CMH test. Only participants with a baseline severity score < 4 were included in the symptoms analysis; participants with missing baseline severity scores were excluded. Missing symptom data for those who were hospitalized or died due to any cause before day 29 were imputed as symptom progression; this rule was added post hoc. COVID-19 symptom severity assessments were based on symptom severity scores through to day 29, including the day of dosing with AZD7442 or placebo. Least squares mean differences overall and by visit were calculated using a mixed model for repeated measures assuming a first-order autoregressive covariance structure. Missing symptom data for those who were hospitalized or died were imputed as a severity score of ER or hospital visit.
Time to symptom resolution was compared using Kaplan–Meier and Cox proportional hazards methods. Follow-up time (T) was calculated as follows:
T = (date of symptom resolution − date of first dosing + 1) when the participant scored “no symptom” on any symptoms except for cough, fatigue, and headache, which could be scored as “mild/moderate” or “no symptom” by participants with a baseline total severity score > 3; vomiting was excluded from the analysis. Participants who died or had COVID-19-related hospitalization before day 29 were censored at day 29 to conservatively prevent inflation of the treatment effect. Participants who did not experience resolution of symptoms were censored at the date of last known status up to day 29 (i.e. T = date of last known status up to day 29 − date of dosing + 1).
Duration of fever through to day 29 was compared using a two-sided Wilcoxon rank sum test at an alpha level of 5%. The Hodges–Lehmann estimate and its 95% CI for the location shift between the two groups are presented.
The primary endpoint and four supportive estimands and key secondary endpoint were tested in a hierarchical order for control of multiplicity. Analysis of the primary endpoint and supportive estimands reached significance [14]; hence, the key secondary endpoint was tested once participants reached day 169 as described above. p values for other secondary endpoints should be considered nominal.
Safety was analyzed descriptively, except for analysis of time to COVID-19 reinfection post-day 29 to day 169, which was analyzed by Kaplan–Meier, including events coded as recurrent COVID-19.
Results
Participants
A total of 903 participants were randomized, dosed, and included in the FAS (452 in the AZD7442 group and 451 in the placebo group) (Fig. S1). Of these, 413 in the AZD7442 group and 421 in the placebo group were included in the mFAS; 39 in the AZD7442 group and 30 in the placebo group were excluded from the mFAS because they were hospitalized at baseline for isolation purposes (in Japan or Russia) or were randomized ≥ 7 days post symptom onset.
Baseline characteristics were similar between the groups (Table 1). Mean age was 46.1 years [standard deviation (SD) 15.2] and 116 (12.8%) participants were aged ≥ 65 years, 455 (50.4%) were female, 559 (61.9%) were white, and 801 (88.7%) had at least one comorbidity considered to be a risk factor for severe COVID-19.
Table 1.
Participant demographics and baseline clinical characteristics (FAS)
| Characteristic | AZD7442 (N = 452) | Placebo (N = 451) | Total (N = 903) |
|---|---|---|---|
| Age, mean (SD), years | 46.3 (15.4) | 45.9 (15.0) | 46.1 (15.2) |
| Aged ≥ 65 years, n (%) | 59 (13.1) | 57 (12.6) | 116 (12.8) |
| Sex, female, n (%) | 239 (52.9) | 216 (47.9) | 455 (50.4) |
| Hispanic/Latino ethnicity, n (%) | 230 (50.9) | 238 (52.8) | 468 (51.8) |
| Race, n (%) | |||
| White | 285 (63.1) | 274 (60.8) | 559 (61.9) |
| American Indian/Alaska Native | 100 (22.1) | 115 (25.5) | 215 (23.8) |
| Asian | 30 (6.6) | 21 (4.7) | 51 (5.6) |
| Black or African American | 16 (3.5) | 20 (4.4) | 36 (4.0) |
| Not reported | 21 (4.6) | 21 (4.7) | 42 (4.7) |
| BMI, mean (SD), kg/m2 | 28.9 (5.5) | 29.2 (6.6) | 29.0 (6.0) |
| Time from symptom onset to randomization, mean (SD), days | 4.9 (1.6) | 5.0 (1.6) | 5.0 (1.6) |
| Serum for SARS-CoV-2 serology, n (%) | |||
| Positive | 60 (13.3) | 68 (15.1) | 128 (14.2) |
| Negative | 383 (84.7) | 376 (83.4) | 759 (84.1) |
| Missing data | 9 (2.0) | 7 (1.6) | 16 (1.8) |
| At high risk of progression to severe COVID-19,a n (%) | 405 (89.6) | 406 (90.0) | 811 (89.8) |
| Comorbidities considered to be risk factors for severe COVID-19, n (%) | 401 (88.7) | 400 (88.7) | 801 (88.7) |
| Obesity (BMI > 30 kg/m2) | 195 (43.1) | 193 (42.8) | 388 (43.0) |
| Current or former smoker | 180 (39.8) | 184 (40.8) | 364 (40.3) |
| Hypertension | 137 (30.3) | 121 (26.8) | 258 (28.6) |
| Diabetes | 53 (11.7) | 56 (12.4) | 109 (12.1) |
| Chronic lung disease/asthma | 58 (12.8) | 50 (11.1) | 108 (12.0) |
| Cardiovascular disease | 42 (9.3) | 38 (8.4) | 80 (8.9) |
| Cancer | 19 (4.2) | 15 (3.3) | 34 (3.8) |
| Chronic kidney disease | 10 (2.2) | 9 (2.0) | 19 (2.1) |
| Chronic liver disease | 7 (1.5) | 14 (3.1) | 21 (2.3) |
| Immunocompromised state | 22 (4.9) | 24 (5.3) | 46 (5.1) |
| Range of baseline symptom severity scores | 0–4 | 0–4 | 0–4 |
| Participants with available baseline symptom severity score < 4,b n/N (%) | 305/413 (73.8) | 322/421 (76.5) | 627/834 (75.2) |
| Unblinded after 30 days and decided to receive a COVID-19 vaccine before day 169, n/N (%) | 118/413 (28.6) | 129/421 (30.6) | 247/834 (29.6) |
Data cutoff, 14 January 2022. The FAS comprised all randomized participants who received study drug
BMI body mass index, COVID-19 coronavirus disease 2019, FAS full analysis set, mFAS modified FAS, SD standard deviation, SARS-CoV-2 severe acute respiratory syndrome coronavirus 2
aDefined as aged ≥ 65 years at randomization, or aged < 65 years with at least one of the following comorbidities: cancer, chronic lung disease or moderate-to-severe asthma, obesity (BMI > 30 kg/m2), hypertension, cardiovascular disease (including history of stroke), diabetes, chronic kidney disease, chronic liver disease, immunocompromised state, sickle cell disease, or smoker (current or former)
bAmong participants in mFAS
In the mFAS, 305 (73.8%) and 322 (76.5%) participants in the AZD7442 and placebo groups, respectively, had an available baseline symptom severity score of < 4 and were included in the symptoms analysis (108 and 99 participants, respectively, were excluded). In total, 118 (28.6%) and 129 (30.6%) participants in the AZD7442 and placebo groups, respectively, were unblinded after 30 days and decided to receive a COVID-19 vaccine before day 169.
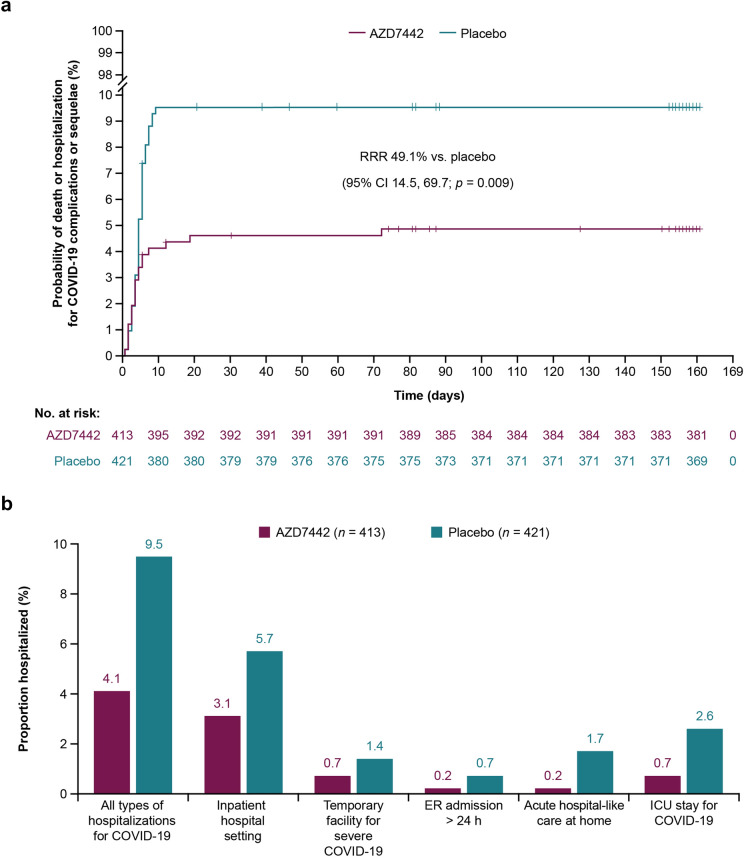
Death from Any Cause or Hospitalization for COVID-19 Complications or Sequelae through to Day 169
Death from any cause or hospitalization for COVID-19 complications or sequelae through to day 169 occurred in 20 of 399 (5.0%) versus 40 of 407 (9.8%) participants receiving AZD7442 versus placebo, respectively, translating into a relative risk reduction (RRR) of 49.1% (95% CI 14.5, 69.7; p = 0.009). Fourteen participants from each group were not included in the analysis due to missing data. Compared with the primary analysis at day 29, there was one additional death (at day 76) of a participant in the AZD7442 arm (due to underlying gastric cancer; not considered treatment related). Kaplan–Meier analysis showed divergence between the treatment groups through 169 days (HR 0.50; 95% CI 0.29, 0.85; log-rank p = 0.0094) (Fig. 1a).
Fig. 1.
a Probability of death or hospitalization for COVID-19 complications or sequelae and b type of hospitalizations through to day 169 (mFAS). Kaplan–Meier curves for time to death from any cause or first hospitalization for COVID-19 complications or sequelae up to day 169 were generated for the two study interventions. Hazard ratio was obtained from a Cox proportional hazards model, with time from symptom onset (≤ 5 versus > 5 days) and risk of progression to severe COVID-19 (high versus low) as covariates. The difference between the groups was assessed via a stratified log-rank test. Vertical lines on the Kaplan–Meier curves represent censored patients. The mFAS comprised all randomized participants who received study drug ≤ 7 days from symptom onset and were not hospitalized at baseline (day 1) for isolation purposes. CI confidence interval, COVID-19 coronavirus disease 2019, ER emergency room, ICU intensive care unit, mFAS modified full analysis set, RRR relative risk reduction
The key secondary outcome is supported by the results of multiple imputation analyses that imputed missing data based on the placebo event rate (RRR 46.9; 95% CI 10.6, 68.5; p = 0.014) and observed event rate (RRR 49.5; 95% CI 14.8, 70.0; p = 0.008). The sensitivity analysis that excluded participants who were unblinded before day 169 for consideration of COVID-19 vaccination also demonstrated a supportive RRR of 50.7% [20 of 295 (6.8%) versus 40 of 292 (13.7%) participants in the AZD7442 and placebo groups, respectively; 95% CI 17.5, 70.5; p = 0.006]. Among baseline seronegative participants, the RRR was 58.6% [16 of 339 (4.7%) versus 39 of 340 (11.5%) participants in the AZD7442 and placebo groups, respectively; 95% CI 27.6, 76.4; p = 0.001].
Reductions in all hospitalization types or acute hospital-like care at home through to day 169 were observed with AZD7442 versus placebo (Fig. 1b). Mean (SD) and median (interquartile range) durations of hospital stay with AZD7442 were 14.9 (10.8) and 14.0 (7.0–19.0) days, respectively, versus 12.7 (9.1) and 10.0 (8.5–14.5) days, respectively, with placebo. In the small proportion of participants admitted to ICU for COVID-19, the mean (SD) and median (interquartile range) durations of ICU admission with AZD7442 were 8.3 (0.6) and 8.0 (8.0–9.0) days, respectively, versus 12.8 (13.7) and 9.0 (6.0–12.0) days, respectively, with placebo.
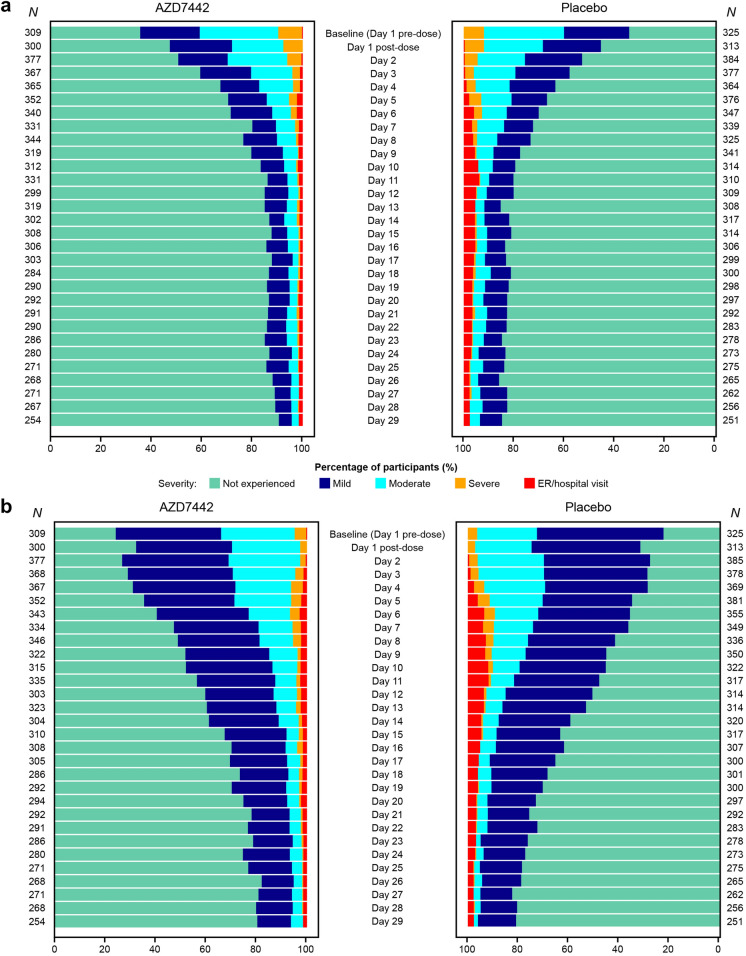
Severity and Progression of COVID-19 Symptoms through to Day 29
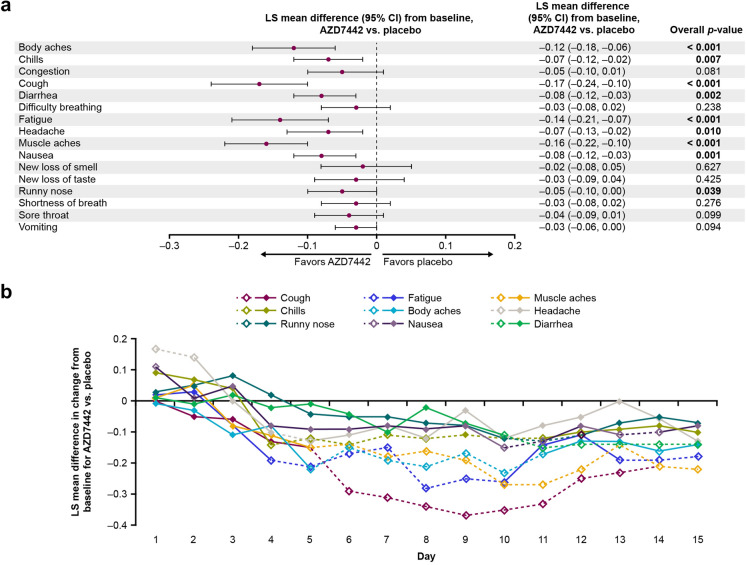
AZD7442 reduced the progression of COVID-19 symptom severity versus placebo. Progression of ≥ 1 COVID-19 symptoms to a worse severity score through to day 29 occurred in 170 (55.7%) participants in the AZD7442 group versus 204 (63.4%) participants in the placebo group, translating into an RRR of 12.5% (95% CI 0.5, 23.0; p = 0.041). Median Kaplan–Meier time to symptom resolution through to day 29 also showed a numerical improvement with AZD7442 versus placebo [11 (95% CI 10, 13) versus 13 (95% CI 11, 15) days; p = 0.091].
Analysis of individual symptoms per study day suggested a more rapid reduction in severity for several symptoms with AZD7442 versus placebo (Figs. 2, S2). Over 29 days, the overall mean improvement from baseline in severity of body aches, chills, cough, diarrhea, fatigue, headache, muscle aches, nausea, and runny nose was greater with AZD7442 versus placebo (Fig. 3a). Most symptoms improved with AZD7442 versus placebo within 1–2 weeks post-dose (Fig. 3b). A numerical improvement was observed in median duration of fever through to day 29 with AZD7442 versus placebo [8.0 versus 11.5 days; Hodges–Lehmann Estimate −1.0 (95% CI −2.0, 0.0; p = 0.155)].
Fig. 2.
Proportion of participants at each symptom severity level by study day for a muscle aches and b cough (mFAS). The mFAS comprised all randomized participants who received study drug ≤ 7 days from symptom onset and were not hospitalized at baseline (day 1) for isolation purposes. ER emergency room, mFAS modified full analysis set
Fig. 3.
LS mean difference in symptom severity change from baseline with AZD7442 versus placebo a overall through to day 29 and b daily through to day 15 (mFAS). Symptoms that improved with AZD7442 versus placebo (p < 0.05) through to day 29 in a are displayed daily through to day 15 in b. Timepoints where symptoms improved significantly with AZD7442 versus placebo are indicated with open circles and dashed lines. Fever was analyzed differently from all other symptoms and is therefore not included in this figure. The mFAS comprised all randomized participants who received study drug ≤ 7 days from symptom onset and were not hospitalized at baseline (day 1) for isolation purposes. CI confidence interval, LS least squares, mFAS modified full analysis set
Safety
Median (range) safety follow-up in this analysis was 170 (1–330) days in the AZD7442 group and 170 (1–326) days in the placebo group. AEs were reported by 174 (38.5%) participants in the AZD7442 group and 196 (43.5%) participants in the placebo group (Table 2). Most AEs were mild or moderate in both the AZD7442 and placebo groups.
Table 2.
Adverse events through to day 169 (safety analysis set)
| Event, n (%)a | AZD7442 (N = 452) | Placebo (N = 451) |
|---|---|---|
| Any AE | 174 (38.5) | 196 (43.5) |
| Mild | 84 (18.6) | 82 (18.2) |
| Moderate | 54 (11.9) | 61 (13.5) |
| Severe | 26 (5.8) | 34 (7.5) |
| Any AE with outcome of death | 7 (1.5) | 6 (1.3) |
| Acute left ventricular failure | 1 (0.2) | 0 |
| Sudden cardiac death | 1 (0.2) | 0 |
| COVID-19 pneumonia | 2 (0.4) | 4 (0.9) |
| COVID-19 | 1 (0.2) | 1 (0.2) |
| Septic shock | 0 | 1 (0.2) |
| Colorectal cancer metastatic | 1 (0.2) | 0 |
| Gastric cancer | 1 (0.2) | 0 |
| Any SAE (including death) | 40 (8.8) | 61 (13.5) |
| Cardiac SAE | 2 (0.4) | 3 (0.7) |
| Any treatment-related AEb | 23 (5.1) | 21 (4.7) |
| Any AE leading to study withdrawal | 5 (1.1) | 7 (1.6) |
| Most common AEs | ||
| COVID-19 pneumonia | 26 (5.8) | 49 (10.9) |
| Diarrhea | 8 (1.8) | 5 (1.1) |
| Injection site pain | 8 (1.8) | 11 (2.4) |
| Type 2 diabetes mellitus | 8 (1.8) | 5 (1.1) |
| COVID-19c | 7 (1.5) | 15 (3.3) |
| Vaccination complication | 7 (1.5) | 9 (2.0) |
| Headache | 7 (1.5) | 4 (0.9) |
| Diabetes mellitus inadequate control | 7 (1.5) | 4 (0.9) |
| Any AESId | 15 (3.3) | 15 (3.3) |
| Injection site pain | 8 (1.8) | 11 (2.4) |
Data cutoff, 14 January 2022. The safety analysis set comprised all participants who received study drug, regardless of baseline hospitalization status (hospitalization was only allowed for isolation purposes)
AE adverse event, AESI AE of special interest, COVID-19 coronavirus disease 2019, SAE serious AE
aParticipants with multiple events in the same category are counted only once in that category, and participants with events in more than one category are counted once in each of those categories
bPossibly related, as assessed by the investigator
cReported after day 29 [most of these AEs were sequelae from the index COVID-19; COVID-19 re-infection was confirmed in 1 (0.2%) participant in each of the AZD7442 and placebo groups]
dIncludes anaphylaxis and other hypersensitivities, injection site pain, injection site erythema, and injection site discomfort
In both groups, the most common AE was COVID-19 pneumonia. AEs of COVID-19, representing the deterioration of pre-existing COVID-19 after day 29, were reported by 7 (1.5%) participants in the AZD7442 group and 15 (3.3%) participants in the placebo group. One participant in the AZD7442 group (0.2%) and one participant in the placebo group (0.2%) had a COVID-19 AE that was judged by the investigator to be a new infection (occurring at days 157 and 158, respectively); all other COVID-19 AEs were considered to be sequelae from the index event.
SAEs were reported by 40 (8.8%) participants in the AZD7442 group and 61 (13.5%) participants in the placebo group. Cardiac SAEs were reported by two (0.4%) participants receiving AZD7442 and three (0.7%) participants receiving placebo. Investigators reported seven (1.5%) deaths in the AZD7442 group [three (0.7%) of which were COVID-19 deaths] versus six (1.3%) in the placebo group (all COVID-19 deaths). Other deaths reported in the AZD7442 group were acute left ventricular failure, sudden cardiac death, metastatic colorectal cancer, and gastric cancer, each in one participant (0.2%). No SAEs or deaths were considered by the investigators to be treatment related.
Pharmacokinetics
AZD7442 serum concentrations were evident 6 months after administration (Fig. S3). Geometric mean (geometric SD) serum concentrations of AZD7442 were 38.2 (± 2.3) µg/ml at day 29 and 13.4 (± 2.1) µg/ml at day 169.
Discussion
In this extended analysis of the TACKLE study, a 600-mg IM dose of AZD7442 administered within 7 days of symptom onset provided protection against death or hospitalization for COVID-19 complications or sequelae through 6 months in unvaccinated individuals with mild-to-moderate COVID-19. A significant RRR of 49.1% was calculated (95% CI 14.5, 69.7; p = 0.009), which was supported by the results of multiple imputation analyses that imputed missing data based on placebo event rates and observed event rates, a sensitivity analysis that excluded participants who were unblinded for consideration of COVID-19 vaccination, and a subgroup analysis of participants who were seronegative at baseline. Most of the hospitalizations or deaths occurred within 29 days of COVID-19 symptom onset, with one additional death recorded in the AZD7442 group at day 76 (due to underlying gastric cancer).
Reducing the hospitalization risk is important as hospital admission for COVID-19 is associated with markedly higher risks for hospital readmission, multi-organ dysfunction, and death compared with the general population [15, 16]. There were fewer admissions to hospital or other acute care facilities through to day 169 among participants receiving AZD7442 versus placebo. Among participants who were admitted to ICU, durations of admission were shorter in the AZD7442 versus the placebo group (mean 8.3 versus 12.3 days; median 8.0 versus 9.0 days), indicating that fewer of these participants required intensive care for more severe disease, or died, than those receiving placebo. Our findings on reducing hospitalization risk and ICU length of stay also have broader clinical and patient-centric importance, given that hospitalization is known to be associated with several hospital-acquired complications, such as hospital-acquired infections [17], generalized deconditioning [18], and exacerbation of patients’ emotions and feelings of depression and anxiety [19], and increasing ICU length of stay is associated with higher 1-year mortality [20].
Previous reports have described how COVID-19 disrupts several aspects of daily living, including broad daily activities, leisure and social life, and employment, as well as its psychological/emotional and physical limitations [21]. Furthermore, acute infection and more severe disease have been reported to have a substantial impact on health-related quality of life [22]. In TACKLE, analysis of participant e-diaries showed that AZD7442 prevented the progression of COVID-19 symptoms through 29 days and may have hastened symptom improvement, allowing individuals with mild-to-moderate COVID-19 to recover and return to normal activities faster, with less chance of disease progression.
In this extended analysis, AZD7442 was well tolerated through 6 months and exhibited a safety profile consistent with the primary analysis [14] and other trials investigating AZD7442 [23, 24]. Based on observations from the PROVENT trial, the question was raised as to whether AZD7442 may increase the risk of cardiac SAEs [25]. In this extended analysis of the TACKLE study, the number of cardiac SAEs reported in the AZD7442 group was unchanged from the primary analysis, and no cardiac SAEs in either group were judged by the investigators to be treatment related. Moreover, cardiac SAEs were infrequent overall (AZD7442, n = 2, 0.4%; placebo, n = 3, 0.7%) and occurred in participants at elevated risk of a cardiovascular event (aged > 65 years, cardiac history, and hypertension). These data, therefore, support earlier analyses indicating that there is no plausible mechanism by which AZD7442 elevates the risk of cardiac SAEs [26].
Limitations include standard of care variations across regions, such as local amendments that allow ivermectin (Brazil) and favipiravir (Hungary). In Russia and Japan, hospitalization at baseline was required for isolation purposes; to mitigate the risk of repeat observation bias, efficacy analyses were performed using an mFAS that excluded participants in the FAS hospitalized at baseline (day 1) for isolation purposes. Secondary endpoints, except the key secondary endpoint, were not controlled for type 1 error inflation. There was a relatively high enrollment in Mexico, but no country-level stratification was specified. By contrast, there was a low enrollment of Black and African American participants, who are disproportionately affected by COVID-19 [27]. Furthermore, study recruitment of participants older than 65 years of age, who are at risk for severe COVID-19, was limited mainly due to prioritization of older adults for COVID-19 vaccination when the study was enrolling. Symptom severity was self-reported by participants and not clinically assessed. Participant recruitment for this trial took place between January and July 2021, when the dominant SARS-CoV-2 variants were Alpha and Delta, with follow-up in the current 6-month analysis occurring up to 14 January 2022. The efficacy of AZD7442 against the Omicron variant could therefore not be determined. Recent analyses demonstrated AZD7442’s residual in vitro neutralization activity against Omicron sublineages through to BA.5 [13, 28–35], although in vitro studies indicate that it does not neutralize BQ.1.1 (an Omicron BA.5 subvariant) or XBB (an Omicron BA.2 subvariant) [36].
Conclusion
In individuals with mild-to-moderate COVID-19, outpatient treatment with a single 600 mg IM administration of AZD7442 was well tolerated, provided protection from hospitalization or death through 6 months, and prevented symptom progression through 29 days.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the trial participants, their families, and all investigators involved in this study. Marius Albulescu and Karen Near of AstraZeneca were involved in the study design of TACKLE.
Medical Writing Assistance
Medical writing support was provided by Matthew Young, DPhil, Shaun W. Foley, BSc (Hons), and Rob Campbell, PhD, of Core Medica, London, UK, supported by AstraZeneca according to Good Publication Practice guidelines.
Author Contributions
All authors contributed to data interpretation, drafting, and providing critical review of the manuscript drafts, and all approved the final version for submission. F.D. Richard Hobbs, Jesus Abraham Simón-Campos, Hugh Montgomery, Francisco Padilla, and Kenneth Kim were investigators for the study and involved in data acquisition. Douglas Arbetter, Alison Templeton, and Seth Seegobin analyzed the data, and Douglas Arbetter takes responsibility for the accuracy of the data analysis. Kelly W. Padilla takes responsibility for the integrity of the data.
Funding
This study, and the journal’s Rapid Service fee, were supported by AstraZeneca.
Data Availability
Data underlying the findings described in this manuscript may be requested in accordance with AstraZeneca’s data sharing policy described at https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure. AstraZeneca Group of Companies allows researchers to submit a request to access anonymized patient level clinical data, aggregate clinical or genomics data (when available), and anonymized clinical study reports through the Vivli web-based data request platform.
Declarations
Conflict of Interest
F.D. Richard Hobbs reports funding from AstraZeneca to cover meeting attendances and the operationalization of TACKLE in the UK as the UK principal investigator; has received funding from UK Research and Innovation and the National Institute for Health and Care Research (NIHR) for national Urgent Public Health COVID-19 trials, and as director of the NIHR Applied Research Collaboration, Oxford Thames Valley, and investigator on the Oxford Biomedical Research Centre (BRC) and NIHR MedTech. Hugh Montgomery is supported by the NIHR’s BRC at University College London Hospitals. He has received consultation fees from AstraZeneca and has consulted for Millfield Medical Electronics Ltd. on the development of a new Closed Circuit Continuous Positive Airway Pressure machine. Francisco Padilla has received personal fees and grants from Amgen, AstraZeneca, Boehringer Ingelheim, Ferrer, Kowa, Medix, Merck, Merck Sharp and Dohme, Novartis, Pfizer, Sanofi, Servier, and Silanes. Jesus Abraham Simón-Campos reports serving on advisory boards for Atea and Eli Lilly; and serves as a speaker for Pfizer, AstraZeneca, Roche, and Regeneron. Kenneth Kim has received research grants for the conduct of the TACKLE trial; reports funding from Regeneron, Eli Lilly, Merck, Pfizer, and Adagio; and serves as a speaker for Regeneron. Douglas Arbetter, Venkatesh Pilla Reddy, Seth Seegobin, Katie Streicher, Rolando M. Viani and Mark T. Esser are employees of, and hold or may hold stock in, AstraZeneca. Kelly W. Padilla was an employee of AstraZeneca at the time of this study and is now an employee of Immunovant, New York, NY, USA. Kelly W. Padilla holds stock in AstraZeneca, GSK (prior employee) and Trulab Inc (board member). Gavin C.K.W. Koh was an employee of AstraZeneca at the time of this study and is now an employee of Generate Biomedicines, Somerville, MA, USA. Gavin C.K.W. Koh holds stock in GSK. Eva Johnsson was an employee of AstraZeneca at the time of this study and is now an employee of Grunenthal, Stockholm, Sweden. Alison Templeton was an employee of AstraZeneca at the time of this study and is now an employee of Regeneron Pharmaceuticals, Inc, Uxbridge, UK.
Ethical Approval
The study adhered to Good Clinical Practice guidelines and the Declaration of Helsinki, Council for International Organizations of Medical Sciences International Ethical guidelines, applicable International Conference on Harmonisation Good Clinical Practice guidelines, and all applicable laws and regulations. All participants provided informed, written consent.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Our World in Data. Coronavirus (COVID-19) hospitalizations. 2022. https://ourworldindata.org/covid-hospitalizations. Accessed 8 Nov 2022.
- 2.Office for National Statistics. Direct and indirect health impacts of COVID-19 in England: emerging Omicron impacts. 2022. https://www.gov.uk/government/publications/direct-and-indirect-health-impacts-of-covid-19-in-england-emerging-omicron-impacts/direct-and-indirect-health-impacts-of-covid-19-in-england-emerging-omicron-impacts. Accessed 8 Nov 2022.
- 3.Centers for Disease Control and Prevention. COVID-NET: COVID-19-associated hospitalization surveillance network. 2022. https://gis.cdc.gov/grasp/covidnet/covid19_5.html. Accessed 8 Nov 2022.
- 4.Antonelli M, Penfold RS, Merino J, et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case–control study. Lancet Infect Dis. 2022;22:43–55. doi: 10.1016/S1473-3099(21)00460-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: a meta-analysis and systematic review. J Infect Dis. 2022;226(9):1593–1607. doi: 10.1093/infdis/jiac136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xie Y, Al-Aly Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol. 2022;10(5):311–321. doi: 10.1016/S2213-8587(22)00044-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xie Y, Xu E, Al-Aly Z. Risks of mental health outcomes in people with COVID-19: cohort study. BMJ. 2022;376:e068993. doi: 10.1136/bmj-2021-068993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28(3):583–590. doi: 10.1038/s41591-022-01689-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tenforde MW, Self WH, Adams K, et al. Association between mRNA vaccination and COVID-19 hospitalization and disease severity. JAMA. 2021;326(20):2043–2054. doi: 10.1001/jama.2021.19499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Juthani PV, Gupta A, Borges KA, et al. Hospitalisation among vaccine breakthrough COVID-19 infections. Lancet Infect Dis. 2021;21(11):1485–1486. doi: 10.1016/S1473-3099(21)00558-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021;21(1):855. doi: 10.1186/s12879-021-06536-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The OpenSAFELY Collaborative. Green A, Curtis H, et al. Describing the population experiencing COVID-19 vaccine breakthrough following second vaccination in England: a cohort study from OpenSAFELY. BMC Med. 2022;20(1):243. doi: 10.1186/s12916-022-02422-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loo YM, McTamney PM, Arends RH, et al. The SARS-CoV-2 monoclonal antibody combination, AZD7442, is protective in nonhuman primates and has an extended half-life in humans. Sci Transl Med. 2022;14(635):eabl8124. doi: 10.1126/scitranslmed.abl8124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montgomery H, Hobbs FDR, Padilla F, et al. Efficacy and safety of intramuscular administration of tixagevimab-cilgavimab for early outpatient treatment of COVID-19 (TACKLE): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet Respir Med. 2022;10(10):985–996. doi: 10.1016/S2213-2600(22)00180-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhaskaran K, Rentsch CT, Hickman G, et al. Overall and cause-specific hospitalisation and death after COVID-19 hospitalisation in England: a cohort study using linked primary care, secondary care, and death registration data in the OpenSAFELY platform. PLoS Med. 2022;19(1):e1003871. doi: 10.1371/journal.pmed.1003871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Subramaniam A, Lim ZJ, Ponnapa Reddy M, Shekar K. Systematic review and meta-analysis of the characteristics and outcomes of readmitted COVID-19 survivors. Intern Med J. 2021;51(11):1773–1780. doi: 10.1111/imj.15350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stewart S, Robertson C, Kennedy S, et al. Personalized infection prevention and control: identifying patients at risk of healthcare-associated infection. J Hosp Infect. 2021;114:32–42. doi: 10.1016/j.jhin.2021.03.032. [DOI] [PubMed] [Google Scholar]
- 18.Falvey JR, Mangione KK, Stevens-Lapsley JE. Rethinking hospital-associated deconditioning: proposed paradigm shift. Phys Ther. 2015;95(9):1307–1315. doi: 10.2522/ptj.20140511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alzahrani N. The effect of hospitalization on patients' emotional and psychological well-being among adult patients: an integrative review. Appl Nurs Res. 2021;61:151488. doi: 10.1016/j.apnr.2021.151488. [DOI] [PubMed] [Google Scholar]
- 20.Moitra VK, Guerra C, Linde-Zwirble WT, Wunsch H. Relationship between ICU length of stay and long-term mortality for elderly ICU survivors*. Crit Care Med. 2016;44(4):655–662. doi: 10.1097/CCM.0000000000001480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rofail D, McGale N, Podolanczuk AJ, et al. Patient experience of symptoms and impacts of COVID-19: a qualitative investigation with symptomatic outpatients. BMJ Open. 2022;12(5):e055989. doi: 10.1136/bmjopen-2021-055989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poudel AN, Zhu S, Cooper N, et al. Impact of Covid-19 on health-related quality of life of patients: a structured review. PLoS ONE. 2021;16(10):e0259164. doi: 10.1371/journal.pone.0259164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levin MJ, Ustianowski A, De Wit S, et al. Intramuscular AZD7442 (tixagevimab–cilgavimab) for prevention of Covid-19. N Engl J Med. 2022;386(23):2188–2200. doi: 10.1056/NEJMoa2116620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.ACTIV-3-Therapeutics for Inpatients with COVID-19 (TICO) Study Group Tixagevimab–cilgavimab for treatment of patients hospitalised with COVID-19: a randomised, double-blind, phase 3 trial. Lancet Respir Med. 2022;10(10):972–984. doi: 10.1016/S2213-2600(22)00215-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Piszczek J, Murthy S, Afra K. Cardiac and vascular serious adverse events following tixagevimab-cilgavimab. Lancet Respir Med. 2023;11(1):e5–e6. doi: 10.1016/S2213-2600(22)00452-0. [DOI] [PubMed] [Google Scholar]
- 26.Maselkar S, Kiazand A, Templeton A, Montgomery H, Esser MT. Cardiac and vascular serious adverse events following tixagevimab-cilgavimab—Author's reply. Lancet Respir Med. 2023;11(1):e7–e8. doi: 10.1016/S2213-2600(22)00450-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Phiri P, Delanerolle G, Al-Sudani A, Rathod S. COVID-19 and Black, Asian, and minority ethnic communities: a complex relationship without just cause. JMIR Public Health Surveill. 2021;7(2):e22581. doi: 10.2196/22581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tuekprakhon A, Nutalai R, Dijokaite-Guraliuc A, et al. Antibody escape of SARS-CoV-2 Omicron BA.4 and BA.5 from vaccine and BA.1 serum. Cell. 2022;185(14):2422–33 e13. doi: 10.1016/j.cell.2022.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Case JB, Mackin S, Errico JM, et al. Resilience of S309 and AZD7442 monoclonal antibody treatments against infection by SARS-CoV-2 Omicron lineage strains. Nat Commun. 2022;13(1):3824. doi: 10.1038/s41467-022-31615-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lusvarghi S, Pollett SD, Neerukonda SN, et al. SARS-CoV-2 BA.1 variant is neutralized by vaccine booster-elicited serum but evades most convalescent serum and therapeutic antibodies. Sci Transl Med. 2022;14(645):eabn8543. doi: 10.1126/scitranslmed.abn8543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dejnirattisai W, Huo J, Zhou D, et al. SARS-CoV-2 Omicron-B.1.1.529 leads to widespread escape from neutralizing antibody responses. Cell. 2022;185(3):467–84.e15. doi: 10.1016/j.cell.2021.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.VanBlargan LA, Errico JM, Halfmann PJ, et al. An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by therapeutic monoclonal antibodies. Nat Med. 2022;28(3):490–495. doi: 10.1038/s41591-021-01678-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou T, Wang L, Misasi J, et al. Structural basis for potent antibody neutralization of SARS-CoV-2 variants including B.1.1.529. Science. 2022;376(6591):eabn8897. doi: 10.1126/science.abn8897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cao Y, Yisimayi A, Jian F, et al. BA.2.12.1, BA.4 and BA.5 escape antibodies elicited by Omicron infection. Nature. 2022;608:593–601. doi: 10.1038/s41586-022-04980-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu MY, Carr EJ, Harvey R, et al. WHO's Therapeutics and COVID-19 Living Guideline on mAbs needs to be reassessed. Lancet. 2022:S0140-6736(22)01938-9 [DOI] [PMC free article] [PubMed]
- 36.Imai M, Ito M, Kiso M, et al. Efficacy of antiviral agents against omicron subvariants BQ.1.1 and XBB. N Engl J Med. 2023;388(1):89–91. doi: 10.1056/NEJMc2214302. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data underlying the findings described in this manuscript may be requested in accordance with AstraZeneca’s data sharing policy described at https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure. AstraZeneca Group of Companies allows researchers to submit a request to access anonymized patient level clinical data, aggregate clinical or genomics data (when available), and anonymized clinical study reports through the Vivli web-based data request platform.