Abstract
This paper explores the role of political stability in explaining the cross-country variation of Covid-19 pandemic outcomes. Based on the international evidence, we find that lower pre-Covid-19 levels of political stability are associated with worse Covid-19 pandemic outcomes. Politically unstable countries are more likely to suffered significantly higher morbidity and mortality. Further analysis shows that political stability only matters in countries prepared with requisite medical capacity to deal with health emergencies. We also find that political stability is more crucial in countries with higher poverty rates. Overall, to combat Covid-19 and the subsequential collective threats successfully, the national authorities should pay more attention to maintain political stability.
Keywords: Political stability, Covid-19, Morbidity and mortality
1. Introduction
The Covid-19 pandemic has spread rapidly and enveloped around the world with increasing morbidity and mortality. Wide range of policy measures have been deployed including Covid-19 surveillance and testing [1,2]; lockdowns and social distancing [[3], [4], [5]]; raising public health awareness on behavioral health affairs [6,7]; building trust through risk communication and community engagement [8]; reaching Covid-19 vaccination targets [9,10] and so on.
Although policy measures deployed by governments have been similar in many regions, countries are in very different situations. Some countries have not only contained the Covid-19 pandemic but also resumed near normal economic activity in the short run, while others are still struggling in deepening crisis. Why have these countries responded remarkably better than others? What explains the among-countries variation of the pandemic outcomes?
Previous studies have identified a number of factors to explain this variation, including differences in cognitive biases [11,12]; predisposition to comply with regulations [13,14]; public trust [15,16]; access to and use of Covid-19 diagnostics, therapeutics and vaccines [17,18]; reliable information [19]; economic and demographic character [20]. Literature have also addressed diverse aspects of the politics of Covid-19 and related issues [21,22].
This paper sheds light on the above questions by exploring the link between political stability and the Covid-19 pandemic. Though limited evidence exists on how political stability influences Covid-19 pandemic outcomes, relevant studies have proven that social conflict, government stability, political regimes, and political corruption badly affect public health.
As for the effects of social conflicts on public health, there are four channels: first, social conflict destroys the medical capacity. In Myanmar, many healthcare workers stopped working, a part of ‘Civil Disobedience Movement’ as a peaceful, non-violent protest against the military coup [23]. Social conflict also destroys infrastructure including water, electricity and health care, which are essential to public health [24,25]. Second, social conflict makes international cooperation unlikely, while joint prevention and control are essential in a bid to conquer pandemic [26,27]. Third, some studies suggest that social conflict exacerbates migration flow, which may in turn aggravate the spread of virus [28]. Fourth, psychological stress caused by social conflict makes people more vulnerable to diseases in Lebanon [29] and in Czechia and Romania [30]. As for government instability, government instability ruins the trust in policy makers and officials and undermines people's compliance with pandemic containment policies [31,32]. As for political regimes, democratic political institutions are considered as an disadvantage in responding quickly to pandemics [33,34]. As for political corruption, political corruption has been recognized as a threat to achieving health goals [35,36]. The non-governmental organization Transparency International has warned that political corruption hampers health care, particularly for infectious diseases [37].
On the basis of documents available, this paper examines the affect of political stability on Covid-19 pandemic outcomes. To this end, we conduct a unified analysis to examine the role of political stability in explaining the cross-country variation of the Covid-19 pandemic morbidity and mortality. To this end, we use ICRG (International Country Risk Guide) political risk rating as the measure of political stability for each country. It is done by assigning points to a preset group of factors, including government stability, socioeconomic conditions, investment profile, internal conflict, external conflict, corruption, military in politics, religious tensions, law and order, ethnic tensions, democratic accountability, and bureaucracy quality.
We find political stability as a major determinant of the Covid-19 Pandemic Outcomes. To the best of our knowledge, this is the first paper directly establishing the link between political stability and Covid-19. Further, our analysis uses the countries' poverty status to explore heterogeneity in the effects of political stability. Since the start of the Covid-19 pandemic there is a large literature explaining the key factors driving and restraining the pandemic. Although the impact of the Covid-19 pandemic is largest for the world's poorest [38], only a few of this research took poverty status into consideration. Emerging evidence shows that exposure to infection is unequal. Poorer communities that live in overcrowded, substandard housing and use shared modes of transport are challenged in adhering to preventive measures [39,40] and exposed to the health risks of epidemics [41]. People in low-paid sectors have been more exposed to covid-19 as telecommuting is not feasible and their face-to-face jobs cannot be done from home [[42], [43], [44]]. Poorer communities have also been more vulnerable to severe disease once infected because of higher levels of pre-existing illness and less access to affordable health care [45]. Additionally, recent research identified the extra costs involve in having children at home for longer without access to vital free services [46,47]. Since the fight against the Covid-19 pandemic is entangled in the fight against political instability and poverty, it means that poverty, Covid-19 and political instability form a deadly trangle [48].
Our findings yield some important insights. First, we establish that political stability may be a major determinant of Covid-19 pandemic outcomes. Countries plagued with worse political stability have suffered higher morbidity and mortality. Second, we find that political stability only matters in countries prepared with requisite medical capacity to deal with health emergencies. Third, we find that political stability is more crucial in countries facing serious poverty. After presenting a range of robustness tests based on alternative measures of variables and different specifications, our findings hold true.
This study provides at least two contributions to existing literature. First, by identifying political stability as an additional source of the cross-country variation of Covid-19 pandemic outcomes, we contribute to the efforts to develop better understanding of pandemics. New interventions are needed to maintain political stability as countries continue to combat Covid-19 and the subsequential collective threats. Correspondingly, by quantifying additional costs of political instability, we contribute to debates on the politics of pandemics. Second, we analyze the deadly triangle formed by poverty, political instability and pandemic. Political instability worsens the pandemic as well as increases poverty, while these problems are in return destabilizing for the political situation and may become more so. By showing the results vary according to the poverty status of countries, we present a possible approach to break the deadly triangle which is to maintain political stability.
The remainder of our paper is organized as follows. Section 2 presents our empirical methodology. Section 3 describes data and variables used in our analysis. Section 4 presents and interprets empirical findings. Section 5 concludes.
2. Methodology
To examine the relationship between political stability and the Covid-19 pandemic, we estimate the following OLS specification:
| (1) |
Where CR is the Covid-19 pandemic cumulative case rate, a measure of pandemic outcomes. For robustness test, we re-estimate our model using an alternative definition of pandemic outcomes, the Covid-19 pandemic cumulative death rate (DR). PS is the key dependent variable corresponding to political stability indicator. X consists of control variables that are likely to impact the Covid-19 pandemic morbidity or mortality.
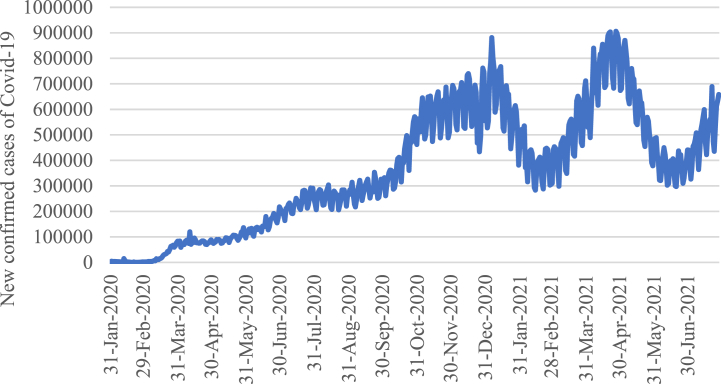
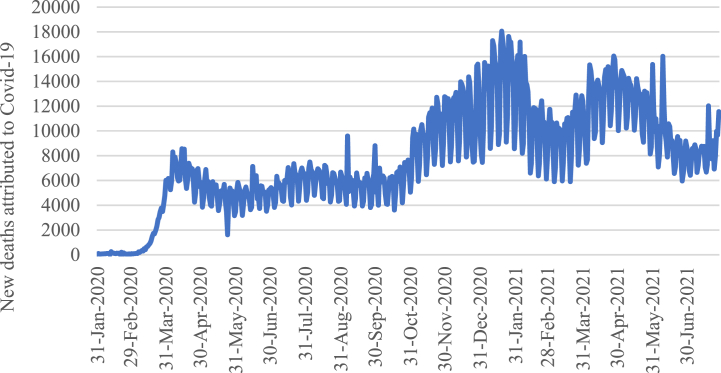
A definitive cross-country analysis cannot be done until the Covid-19 pandemic has been eradicated, as is also noted in Ozkan et al. (2021) [49]. However, we can still retrieve sufficient information to examine the link between Covid-19 pandemic and political stability once we figure out the periodic features of the pandemic. As in Fig. 1 and Fig. 2, the whole world has passed the peak of two waves of Covid-19 pandemic in terms of both new cases and new deaths. The first wave ended by February 2021 and the second wave ended by May 2021. Accordingly, we carry out our empirical analysis using the Covid-19 pandemic cumulative case rate (CR) on the two corresponding dates respectively: Feb 29, 2021, and May 31, 2021.
Fig. 1.
7-day rolling average of new confirmed cases of Covid-19 worldwide.
Fig. 2.
7-day rolling average of new deaths of Covid-19 worldwide.
3. Data and variables
We construct a cross-section database set including 83 countries and regions to analyze the effect of political stability on the Covid-19 pandemic (Appendix 1). The following briefly discusses database sources and variable definitions.
3.1. The Covid-19 pandemic
Morbidity describes the general severity degree of Covid-19 pandemic outcomes, which is defined as the 7-day rolling average of cumulative number of cases per 100,000 population due to Covid-19 by Feb 29, 2021 (CR1) and May 31, 2021 (CR2). The data on Covid-19 are retrieved from John Hopkins CSSE GitHub Data Source, which provides daily updates of the number of Covid-19 cases globally (Table 1).
Table 1.
Descriptive statistics.
| Variable | Obs | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| CR1 | 83 | 3398.600 | 3144.464 | 17.601 | 11547.730 |
| CR2 | 83 | 5047.155 | 4328.301 | 52.574 | 15527.510 |
| PS | 83 | 66.479 | 16.533 | 0.000 | 87.125 |
| Hospital bed | 83 | 34.96 | 27.42 | 2.000 | 130.50 |
| Stringency | 83 | 61.193 | 10.845 | 29.611 | 83.073 |
| Test-case rate | 83 | 141.153 | 365.996 | 3.033 | 2377.558 |
| Urbanization | 83 | 68.896 | 20.100 | 16.937 | 100.000 |
| Population growth | 83 | 102.518 | 109.928 | −95.419 | 492.116 |
| Trade | 83 | 90.240 | 59.361 | 27.095 | 387.103 |
| GDP per capita | 83 | 11.745 | 2.324 | 7.429 | 17.831 |
| GDP growth | 83 | 2.297 | 2.037 | −3.467 | 6.838 |
| Human development | 83 | 80.000 | 12.749 | 48.300 | 95.700 |
Notes: This table reports the descriptive statistics for main variables used in our analysis. Variable definitions are presented in Appendix 2.
3.2. Political stability
We use ICRG political risk rating (PS) for 2020 as the measure of political stability. The higher the rating point, the greater the political stability. Data for alternative years has been used to conduct robustness tests, including 2019 (PS2019) and average from 2018 to 2020 (PSaverage). The ICRG model for forecasting country risks was created in 1980 by the editors of International Reports. In 1992, ICRG became an integral part of the PRS Group's services to international business community, providing ratings for 140 countries and regions and is widely used in country risks analysis [[50], [51], [52]].
3.3. Control variables
Pandemic morbidity and mortality are closely linked with medical capacity so that we control for the number of hospital beds per 1000 population (Hospital bed) [53]. We use Stringency, Government Response Stringency Index retrieving from Oxford Covid-19 Government Response Tracker to capture the strictness of government policy response [54].
Under-reporting is an important concern when analyzing morbidity and mortality. The numbers of Covid-19 cases and deaths are likely to be under-reported due to insufficient tests especially at the early stage when the testing ability was still weak. Following Gelfand et al. (2021) [55], we use tests conducted per new confirmed case of Covid-19 (Test-case rate) as the primary proxy for under-reporting. A low ratio of tests to cases suggest that a country was mostly testing people with symptoms and the level of under-reporting may be high.
The condition can be quite different in rural areas compared with urban areas. For one thing, the population density and mobility in rural areas are remarkably lower, which helps to interrupt transmission of virus. For another, rural areas with relatively poor health infrastructures may not be able to handle infections, leading to higher mortality. We control for urban population as percentage of population (Urbanization) to feature these urban-rural differences. Considering the virus spread through international trade, we incorporate trade volume (Trade) expressed as exports and imports of goods and services as percentage of GDP. In addition, we incorporate population growth (Population growth) to capture population characteristics, and GDP per capita (GDP per capita), GDP growth rate (GDP growth) as well as Human development index (Human development) to control for economic conditions. All the control variables are by the latest pre-Covid-19 years for which data are available.
4. Political stability and the Covid-19 pandemic
4.1. Main results
Table 2 presents our empirical results from estimating Eq. (1). Column (1) and (2) report the baseline specifications corresponding to case rates on Feb 29, 2021 (CR1) and May 31, 2021 (CR2) separately, which only include control variables. In Column (3) and (4), we incorporate the key dependent variable PS. Explanatory power of specifications gets better after incorporating PS, as can be seen in R2. We find a negative and significant relation between the Covid-19 case rate (both CR1 and CR2) and PS, suggesting countries plagued with political instability are likely to suffer from higher Covid-19 morbidity.
Table 2.
Political stability and Covid-19 morbidity.
|
VARIABLES |
(1) |
(2) |
(3) |
(4) |
|---|---|---|---|---|
| CR1 | CR2 | CR1 | CR2 | |
| PS | −66.947*** | −115.157*** | ||
| (-3.37) | (-4.19) | |||
| Hospital beds | −15.871 | −7.135 | −24.687* | −22.300 |
| (-1.08) | (-0.34) | (-1.76) | (-1.15) | |
| Stringency | 26.264 | 50.693 | 12.496 | 27.010 |
| (0.73) | (0.98) | (0.37) | (0.57) | |
| Test-case rate | −2.614*** | −2.871** | −2.789*** | −3.173*** |
| (-2.94) | (-2.26) | (-3.35) | (-2.76) | |
| Urbanization | 21.545 | 42.545 | 11.141 | 24.650 |
| (0.93) | (1.29) | (0.51) | (0.82) | |
| Trade | 11.796* | 17.789** | 11.301** | 16.938** |
| (1.98) | (2.09) | (2.03) | (2.20) | |
| Population growth | −5.196 | −4.651 | −5.482 | −5.143 |
| (-1.33) | (-0.83) | (-1.50) | (-1.02) | |
| GDP per capita | −168.747 | −151.895 | −233.489* | −263.260 |
| (-1.27) | (-0.80) | (-1.86) | (-1.52) | |
| GDP growth | 31.411 | 98.640 | −4.221 | 37.348 |
| (0.15) | (0.33) | (-0.02) | (0.14) | |
| Human development | 79.255** | 86.086 | 137.056*** | 185.511*** |
| (2.03) | (1.54) | (3.39) | (3.32) | |
| Constant | −3731.547 | −6789.314 | −1096.654 | −2256.948 |
| (-0.98) | (-1.25) | (-0.30) | (-0.45) | |
| Observations | 83 | 83 | 83 | 83 |
| R-squared | 0.370 | 0.319 | 0.456 | 0.453 |
| F test | 5.31e-05 | 0.000573 | 1.39e-06 | 1.67e-06 |
| r2_a | 0.293 | 0.235 | 0.380 | 0.376 |
| F | 4.767 | 3.797 | 6.029 | 5.951 |
Notes: This table reports our regression results to assess the impact of political stability on Covid-19 case rates by Feb 29, 2021 (CR1) and May 31, 2021 (CR2). The specifications are estimated by OLS regression. Variable definitions are presented in Appendix 2. T-statistics are in parentheses. ***, **, * denote the significance level at 1%, 5%, and 10%, respectively. We estimate multicollinearity via the variance inflation factors for our model. A variance inflation factor of above 5 generally means that a model has high multicollinearity which is biasing the estimates and standard errors. Appendix 3 shows that no variables had problematic multicollinearity.
4.2. Heterogeneity tests
Considering the impact of political stability on Covid-19 morbidity varies meaningfully across countries, we conduct two sets of subgroup analyses to test the potential heterogeneity.
4.2.1. Public health capacity, political stability, and Covid-19 pandemic
Medical resource and capacity play a fundamental role in the battle against pandemics. In fact, the strength of the state capacity and public health programs matter more than the form of government in face of a pandemic. It is a legitimate inference that the impact of political stability on the Covid-19 pandemic could be different across countries depending on medical capacity.
We test the heterogeneity based on medical capacity measured by the number of hospital beds per 10,000 population (Hospital beds) for each country. Country i is classified as a “Below (Above or equal to) the median” subgroup if the Hospital beds is smaller (equal to or larger) than the medial value of the corresponding number of all countries.
Table 3 reports the heterogeneity results based on medical capacity. Columns (1) and (3) present the empirical results for the “Above or equal to the median” subgroup. The estimated relation between political stability and Covid-19 morbidity is negative and significant at 1% level. As for the “Below the median” subgroup, the coefficients of PS are insignificantly negative in Columns (2) and (4). These findings point to an adverse impact of political stability on Covid-19 case rates only exists in the “Above or equal to the median” subgroup, which verifies that political stability only matters in countries prepared with requisite medical capacity to address health emergencies.
Table 3.
Public health capacity, political stability, and Covid-19 morbidity.
|
VARIABLES |
(1) |
(2) |
(3) |
(4) |
|---|---|---|---|---|
| CR1 |
CR1 |
CR2 |
CR2 |
|
| ( ≥ 2.76) | (<2.76) | ( ≥ 2.76) | (<2.76) | |
| PS | −92.583*** | −36.822 | −147.539*** | −55.212 |
| (-4.10) | (-0.90) | (-5.00) | (-0.95) | |
| Hospital beds | −23.733 | −157.847 | −32.171 | −260.407* |
| (-1.40) | (-1.52) | (-1.46) | (-1.77) | |
| Stringency | 59.293 | −10.839 | 83.528 | −20.175 |
| (1.39) | (-0.19) | (1.50) | (-0.25) | |
| Test-case rate | −3.521*** | −1.204 | −2.892* | −1.831 |
| (-2.95) | (-0.89) | (-1.85) | (-0.95) | |
| Urbanization | −9.448 | 57.443 | 7.330 | 81.835 |
| (-0.34) | (1.53) | (0.20) | (1.54) | |
| Trade | 18.715*** | −8.045 | 28.388*** | −11.238 |
| (2.89) | (-0.74) | (3.36) | (-0.73) | |
| Population growth | −8.160 | −3.914 | −12.345* | −0.092 |
| (-1.59) | (-0.64) | (-1.84) | (-0.01) | |
| GDP per capita | −270.782 | −157.005 | −272.101 | −162.069 |
| (-1.32) | (-0.91) | (-1.02) | (-0.66) | |
| GDP growth | −180.094 | −160.614 | −158.185 | −248.047 |
| (-0.66) | (-0.56) | (-0.44) | (-0.61) | |
| Human development | 261.928*** | 87.721 | 255.906** | 157.604 |
| (3.26) | (1.14) | (2.44) | (1.44) | |
| Constant | −10,819.398 | 1212.203 | −7434.726 | −1049.040 |
| (-1.43) | (0.21) | (-0.75) | (-0.13) | |
| Observations | 42 | 41 | 42 | 41 |
| R-squared | 0.657 | 0.393 | 0.648 | 0.421 |
| F test | 5.72e-05 | 0.0781 | 8.21e-05 | 0.0483 |
| r2_a | 0.547 | 0.191 | 0.534 | 0.228 |
| F | 5.944 | 1.943 | 5.706 | 2.182 |
Notes: This table reports the heterogeneity results from subgroup regressions to assess the impact of political stability on Covid-19 case rate by Feb 29, 2021 (CR1) and May 31, 2021 (CR2). The grouping variable is the number of hospital beds per 10,000 population. The specifications are estimated by OLS regression. Variable definitions are presented in Appendix 2. T-statistics are in parentheses. ***, **, * denote the significance level ate 1%, 5%, and 10%, respectively.
4.2.2. Poverty, political stability, and Covid-19 pandemic
The impact of Covid-19 is not shared equally and the vulnerable are left disproportionately exposed to the virus. A survey in 2020 has found infection rate to be as high as 94% among some people living in precarious situations in Paris, indicating that Covid-19 is more easily spread among people living in poor conditions [56]. Indeed, the rich have some ability to save themselves because they are far more accessible to appropriate accommodation and healthcare tools, while the poor are in greater need of government assistances as they are powerless against the pandemic. Since political stability is the prerequisite for the effective functioning of governments, political stability should matter more to countries facing serious poverty.
Therefore, we infer that the impact of political stability on the Covid-19 pandemic morbidity vary with poverty. We utilize the share of the population living in extreme poverty (Poverty) as the measure of poverty levels. Country i is classified as a “Below (Above or equal to) the median” subgroup if the Poverty is smaller (equal to or larger) than the medial value of the corresponding number of all countries.
Table 4 reports the heterogeneity results based on poverty. Columns (1) and (3) present the empirical results for the “Above or equal to the median” subgroup, the estimated relation between political stability and Covid-19 case rates are negative and significant at the 1% level. In contrast, the coefficients on PS is insignificant for the “Below the median” subgroup in Columns (2) and (4). Our findings indicate an adverse impact of political stability on Covid-19 pandemic outcomes only exists in the “Above or equal to the median” subgroup, which suggests that political stability matters more in countries facing serious poverty. We conclude that the authorities in politically stable countries, do better to fix healthcare inequality and exclusion, and protect the vulnerable from Covid-19.
Table 4.
Poverty, political stability, and Covid-19 morbidity.
|
VARIABLES |
(1) |
(2) |
(3) |
(4) |
|---|---|---|---|---|
| CR1 |
CR1 |
CR2 |
CR2 |
|
| ( ≥ 3.55) | (<3.55) | ( ≥ 3.55) | (<3.55) | |
| PS | −121.161*** | 3.285 | −163.136*** | −51.172 |
| (-4.69) | (0.09) | (-4.33) | (-0.98) | |
| Hospital beds | −44.718* | −3.083 | −48.809 | −0.869 |
| (-1.89) | (-0.15) | (-1.41) | (-0.03) | |
| Stringency | −2.508** | −2.561* | −3.503** | −2.175 |
| (-2.15) | (-1.79) | (-2.06) | (-1.02) | |
| Test-case rate | −37.737 | 69.555 | −24.098 | 64.993 |
| (-0.78) | (1.17) | (-0.34) | (0.73) | |
| Urbanization | 5.657 | 6.890 | 5.083 | 33.272 |
| (0.17) | (0.23) | (0.11) | (0.73) | |
| Trade | 7.920 | 10.551 | 12.265 | 16.796 |
| (0.89) | (1.44) | (0.94) | (1.54) | |
| Population growth | −6.412 | −2.725 | −3.843 | −5.378 |
| (-1.12) | (-0.48) | (-0.46) | (-0.63) | |
| GDP per capita | −121.679 | −327.663* | −189.804 | −297.155 |
| (-0.66) | (-1.78) | (-0.71) | (-1.09) | |
| GDP growth | −81.629 | 15.598 | −45.062 | 76.946 |
| (-0.26) | (0.06) | (-0.10) | (0.21) | |
| Human development | 173.386*** | 132.907* | 262.667*** | 130.690 |
| (3.01) | (1.76) | (3.12) | (1.16) | |
| Constant | 3046.143 | −8778.591 | −100.549 | −5694.890 |
| (0.56) | (-1.17) | (-0.01) | (-0.51) | |
| Observations | 42 | 41 | 42 | 41 |
| R-squared | 0.631 | 0.433 | 0.609 | 0.265 |
| F test | 0.000155 | 0.0389 | 0.000337 | 0.405 |
| r2_a | 0.512 | 0.244 | 0.483 | 0.0204 |
| F | 5.302 | 2.289 | 4.824 | 1.083 |
Notes: This table reports the heterogeneity results from subgroup regressions to assess the impact of political stability on Covid-19 case rate by Feb 29, 2021 (CR1) and May 31, 2021 (CR2). The grouping variable is the share of the population living in extreme poverty. The specifications are estimated by OLS regression. Variable definitions are presented in Appendix 2. T-statistics are in parentheses. ***, **, * denote the significance level ate 1%, 5%, and 10%, respectively.
4.3. Robustness tests
4.3.1. Alternative measures for the Covid-19 pandemic
In this section, we use an alternative measure, the Covid-19 pandemic cumulative death rate by Feb 29, 2021 (DR1) and May 31, 2021 (DR2), to conduct robustness tests. The coefficients of PS are negative and significant at the 5% level in Columns (1) and (2) for Table 5, associated with the prediction that an increase in political stability contributes to decreasing Covid-19 mortality. Along with our main results, these results show that political stability helps to reduce both morbidity and mortality for the Covid-19 pandemic.
Table 5.
Political stability and Covid-19 mortality.
|
VARIABLES |
(1) |
(2) |
|---|---|---|
| DR1 | DR2 | |
| PS | −1.081** | −2.069** |
| (-2.14) | (-2.29) | |
| Hospital beds | −0.441 | −0.748 |
| (-1.24) | (-1.17) | |
| Stringency | 0.887 | 1.104 |
| (1.02) | (0.71) | |
| Test-case rate | −0.047** | −0.064* |
| (-2.22) | (-1.69) | |
| Urbanization | 0.058 | 0.550 |
| (0.10) | (0.55) | |
| Trade | 0.083 | 0.085 |
| (0.59) | (0.33) | |
| Population growth | −0.275*** | −0.443*** |
| (-2.96) | (-2.67) | |
| GDP per capita | −5.434* | −6.922 |
| (-1.70) | (-1.21) | |
| GDP growth | −1.482 | −0.054 |
| (-0.30) | (-0.01) | |
| Human development | 2.079** | 2.426 |
| (2.02) | (1.32) | |
| Constant | 24.769 | 94.239 |
| (0.27) | (0.57) | |
| Observations | 83 | 83 |
| R-squared | 0.342 | 0.270 |
| F test | 0.000451 | 0.00805 |
| r2_a | 0.250 | 0.168 |
| F | 3.737 | 2.659 |
Notes: This table reports the regression results to assess the impact of political stability on Covid-19 death rate by Feb 29, 2021 (DR1) and May 31, 2021 (DR2). The specifications are estimated by OLS regression. Variable definitions are presented in Appendix 2. T-statistics are in parentheses. ***, **, * denote the significance level ate 1%, 5%, and 10%, respectively.
4.3.2. Political stability indicator by different years
Given that countries are going through different stages of the Covid-19 pandemic, we use ICRG political risk rating by different dates to conduct robustness tests instead of 2020: 2019 (PS2019) and average from 2018 to 2020 (PSaverage). As presented in Table 6, the coefficients of PS2019 and PSaverage are negative and significant at the 1% level, suggesting political instability exacerbate Covid-19 morbidity.
Table 6.
Political stability and Covid-19 morbidity.
|
VARIABLES |
(1) |
(2) |
(3) |
(4) |
|---|---|---|---|---|
| CR1 | CR1 | CR2 | CR2 | |
| PS2019 | −63.705*** | −111.089*** | ||
| (-3.22) | (-4.06) | |||
| PSaverage | −63.707*** | −110.819*** | ||
| (-3.21) | (-4.04) | |||
| Hospital beds | −25.218* | −24.922* | −23.435 | −22.879 |
| (-1.78) | (-1.76) | (-1.20) | (-1.17) | |
| Stringency | 11.726 | 11.189 | 25.341 | 24.469 |
| (0.34) | (0.33) | (0.53) | (0.52) | |
| Test-case rate | −2.800*** | −2.802*** | −3.195*** | −3.199*** |
| (-3.34) | (-3.34) | (-2.76) | (-2.76) | |
| Urbanization | 12.488 | 12.553 | 26.752 | 26.905 |
| (0.57) | (0.57) | (0.88) | (0.89) | |
| Trade | 11.347** | 11.245** | 17.007** | 16.830** |
| (2.02) | (2.01) | (2.20) | (2.17) | |
| Population growth | −5.505 | −5.480 | −5.189 | −5.146 |
| (-1.50) | (-1.49) | (-1.02) | (-1.01) | |
| GDP per capita | −224.159* | −224.612* | −248.522 | −249.074 |
| (-1.78) | (-1.78) | (-1.43) | (-1.43) | |
| GDP growth | 0.347 | 2.259 | 44.471 | 47.930 |
| (0.00) | (0.01) | (0.17) | (0.18) | |
| Human development | 134.803*** | 134.686*** | 182.951*** | 182.510*** |
| (3.31) | (3.31) | (3.26) | (3.25) | |
| Constant | −1270.219 | −1251.646 | −2497.264 | −2475.467 |
| (-0.35) | (-0.34) | (-0.49) | (-0.49) | |
| Observations | 83 | 83 | 83 | 83 |
| R-squared | 0.449 | 0.449 | 0.446 | 0.445 |
| F test | 2.00e-06 | 2.05e-06 | 2.43e-06 | 2.61e-06 |
| r2_a | 0.373 | 0.372 | 0.369 | 0.368 |
| F | 5.876 | 5.867 | 5.795 | 5.767 |
Notes: This table reports the regression results to assess the impact of political stability on Covid-19 case rate by Feb 29, 2021 (CR1) and May 31, 2021 (CR2). We use ICRG political risk rating for 2019 (PS2019) as well as average from 2018 to 2020 (PSaverage) instead of 2020. The specifications are estimated by OLS regression. Variable definitions are presented in Appendix 2. T-statistics are in parentheses. ***, **, * denote the significance level ate 1%, 5%, and 10%, respectively.
4.3.3. Tobit regression
Because the dependent variables are left censored which may produce biased estimates, we re-estimate our base-line regression using the Tobit model and present the results in Table 7. The coefficients of PS in Columns (1) and (2) are significantly negative.
Table 7.
Tobit regression.
|
VARIABLES |
(1) |
(2) |
|---|---|---|
| CR1 | CR2 | |
| PS | −66.947*** | −115.157*** |
| (-3.61) | (-4.50) | |
| Hospital beds | −24.687* | −22.300 |
| (-1.89) | (-1.24) | |
| Stringency | 12.496 | 27.010 |
| (0.39) | (0.62) | |
| Test-case rate | −2.789*** | −3.173*** |
| (-3.59) | (-2.96) | |
| Urbanization | 11.141 | 24.650 |
| (0.55) | (0.88) | |
| Trade | 11.301** | 16.938** |
| (2.18) | (2.36) | |
| Population growth | −5.482 | −5.143 |
| (-1.61) | (-1.09) | |
| GDP per capita | −233.489** | −263.260 |
| (-2.00) | (-1.63) | |
| GDP growth | −4.221 | 37.348 |
| (-0.02) | (0.15) | |
| Human development | 137.056*** | 185.511*** |
| (3.64) | (3.57) | |
| Constant | −1096.654 | −2256.948 |
| (-0.32) | (-0.48) | |
| Observations | 83 | 83 |
| F test | 2.16e-07 | 2.67e-07 |
| Prob > chi2 | 0.0000 | 0.0000 |
| Pseudo R2 | 0.0321 | 0.0308 |
Notes: This table reports the regression results to assess the impact of political stability on Covid-19 case rate by Feb 29, 2021 (CR1) and May 31, 2021 (CR2). The specifications are estimated by Tobit regression. Variable definitions are presented in Appendix 2. T-statistics are in parentheses. ***, **, * denote the significance level ate 1%, 5%, and 10%, respectively.
5. Conclusions and discussions
This paper, through its use of a cross-section database set including 83 countries and regions, explores the role of political stability in explaining cross-country variations of Covid-19 pandemic outcomes. In accordance with expectation, we find that lower pre-Covid-19 levels of political stability are associated with worse Covid-19 pandemic outcomes. This basic result is compatible with recent findings from the literature that unstable political situations including social conflict [[23], [24], [25], [26], [27], [28], [29], [30]], government stability [31,32], and political corruption [[35], [36], [37]] badly affect public health.
However, the result conflicts with Cepaluni et al. (2020) and Cepaluni et al. (2021) to a certain extent, which argue that democratic political institutions to be a disadvantage in halting the pandemics [33,34]. According to ICRG political risk rating standards, higher degree of democracy is corresponding to higher level of political stability, which is associated with better Covid-19 pandemic outcomes as our result shows. The discrepancy occurred because the ICRG political risk rating is an aggregative measure of political stability, which is done by assigning points to a preset group of 12 factors, including the degree of democracy (democratic accountability). Thus, we could not reveal the relationship between political regimes and Covid-19 pandemic outcomes definitely.
Our study reconfirms the fundamental role of national medical capacity in the battle against public health emergencies. Though political stability is a major determinant of Covid-19 pandemic outcomes, it only matters in countries prepared with requisite medical capacity. In fact, strong national health systems and a competent public health workforce have been considered key conditions for the delivery of effective public health services for decades [57].
We also use national poverty status to analyze the heterogeneity in the effects of political stability on Covid-19 pandemic outcomes. Political stability is pivotal for pandemic management especially in countries with higher poverty rates. A potential reason is the poor are in greater need of government assistances as they are disproportionately exposed to the virus and far less accessible to appropriate health care services, and political stability is the prerequisite for the effective functioning of governments.
A key policy lesson is that measures deployed to tackle pandemics could be based on an understanding on how political instability affect national health systems functioning and individual behaviors. New interventions are needed to maintain political stability as countries continue to combat Covid-19 and the subsequential collective threats. For instance, Saudi coalition declared a ceasefire in bid to contain coronavirus, two weeks after the UN Secretary-General issued a global appeal to all belligerents to down their weapons to help halt the spread of the new coronavirus. Meanwhile, reorientation of health systems with strengthened ability to prepare for and respond to public health emergencies will be required to combat Covid-19 and the subsequential collective threats successfully, due to its fundamental role for public health emergency management.
As the poor are in greater need of government assistances in face of the threat of virus, policy measures and programs should integrate poverty status. Further, when we show the results vary according to the poverty status of countries, it means that maintaining political stability could be a possible approach to break the deadly triangle formed by poverty, political instability and pandemic, as it may both halt the pandemic and enhances economic growth, transforming the vicious circle into a virtuous circle.
Limitations of the data and methods warrant further discussion. First, the data on Covid-19 was collected during the first two waves of the pandemic, so that we cannot conduct the tests dynamically according to the changes of the pandemic and policy responses. Thus, this is not a definitive cross-country analysis, which cannot analyze the long-run effects of political stability on Covid-19 pandemic outcomes. Second, as a national level study, we neglect the heterogeneity among different regions within one country. Third, though we find a significant affect of political stability on Covid-19 pandemic outcomes, we have not empirically examined the multiple mechanisms.
In closing, we highlight with some open questions for potential follow-up research. First, an essential next step is to assess the effects of political stability on Covid-19 pandemic outcomes in the long run. Second, to assess whether the heterogeneity within countries is present, and how much, it is necessary to conduct the analysis in the specific countries, especially countries suffering from extreme poverty and political chaos. Third, comprehensive mechanism tests should be considered.
Data availability statement
Data will be made available on request.
Funding statement
This study had no funding support.
CRediT authorship contribution statement
Rui Gao: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. Hai-Hong Liu: Conceptualization, Formal analysis, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix tables
Appendix 1.
Sample
| CODE | COUNTRY | CODE | COUNTRY | CODE | COUNTRY |
|---|---|---|---|---|---|
| 1 | Albania | 29 | Greece | 57 | Panama |
| 2 | Argentina | 30 | Guatemala | 58 | Paraguay |
| 3 | Australia | 31 | Hungary | 59 | Peru |
| 4 | Bahrain | 32 | India | 60 | Philippines |
| 5 | Bangladesh | 33 | Indonesia | 61 | Poland |
| 6 | Belgium | 34 | Iraq | 62 | Portugal |
| 7 | Bolivia | 35 | Ireland | 63 | Qatar |
| 8 | Bulgaria | 36 | Israel | 64 | Romania |
| 9 | Belarus | 37 | Italy | 65 | Russia |
| 10 | Sri Lanka | 38 | Jamaica | 66 | Saudi Arabia |
| 11 | Chile | 39 | Japan | 67 | Serbia |
| 12 | Colombia | 40 | Kazakhstan | 68 | Singapore |
| 13 | Denmark | 41 | Jordan | 69 | Slovakia |
| 14 | Costa Rica | 42 | Kenya | 70 | Slovenia |
| 15 | Croatia | 43 | Korea, South | 71 | South Africa |
| 16 | Cuba | 44 | Kuwait | 72 | Zimbabwe |
| 17 | Cyprus | 45 | Latvia | 73 | Spain |
| 18 | Czechia | 46 | Lithuania | 74 | Sweden |
| 19 | Dominican Republic | 47 | Luxembourg | 75 | Switzerland |
| 20 | Ecuador | 48 | Madagascar | 76 | Togo |
| 21 | El Salvador | 49 | Malawi | 77 | Ukraine |
| 22 | Ethiopia | 50 | Mongolia | 78 | Turkey |
| 23 | Estonia | 51 | Morocco | 79 | US |
| 24 | Finland | 52 | Oman | 80 | Uganda |
| 25 | France | 53 | Netherlands | 81 | United Arab Emirates |
| 26 | Gambia | 54 | New Zealand | 82 | Uruguay |
| 27 | Germany | 55 | Norway | 83 | United Kingdom |
| 28 | Ghana | 56 | Pakistan |
Appendix 2.
Variable definitions
| Variable | Definition | Data Source |
|---|---|---|
| Covid-19 morbidity and mortality | ||
| CR | Covid-19 pandemic case rate: 7-day rolling average of cumulative number of cases per 100,000 population. | John Hopkins CSSE GitHub Data Source |
| DR | Covid-19 pandemic death rate: 7-day rolling average of cumulative number of deaths per 100,000 population. | |
| Political stability | ||
| PS | ICRG political risk rating. Political risk components include government stability, socioeconomic conditions, investment profile, internal conflict, external conflict, corruption, military in politics, religious tensions, law and order, ethnic tensions, democratic accountability, and bureaucracy quality. | ICRG reports |
| Control variables | ||
| GDP per capita | Gross Domestic Product per capita | World Bank |
| GDP growth | Gross Domestic Product growth rate | World Bank |
| Urbanization | Urban population as percentage of population | World Bank |
| Population growth | Exponential rate of growth of midyear population from year t-1 to t (expanded by 100 times) | World Bank |
| Trade | Sum of exports and imports of goods and services as percentage of Gross Domestic Product | World Bank |
| Hospital beds | Number of hospital beds per 1000 population | Our World in Data |
| Human development | A composite index measuring average achievement in three basic dimensions of human development: a long and healthy life, knowledge, and a decent standard of living. (expanded by 100 times) | United Nations Development Programme |
| Stringency | Government Response Stringency Index: composite measure based on 9 response indicators including school closures, workplace closures, and travel bans, rescaled to a value from 0 to 100 (100 = strictest response) | Oxford Covid-19 Government Response Tracker |
| Test-case rate | Tests conducted per new confirmed case of Covid-19, given as a rolling 7-day average | Our World in Data |
| Poverty | The share of the population living in extreme. This is a grouping variable which is not included in specifications. | |
Appendix 3.
Multicollinearity Analysis
| Variable | VIF | 1/VIF |
|---|---|---|
| PS | 1.45 | 0.690908 |
| Hospital beds | 1.98 | 0.505433 |
| Stringency | 1.83 | 0.546594 |
| Test-case rate | 1.25 | 0.802922 |
| Urbanization | 2.58 | 0.388178 |
| Trade | 1.46 | 0.682984 |
| Population growth | 2.16 | 0.463032 |
| GDP per capita | 1.14 | 0.878257 |
| GDP growth | 2.08 | 0.481311 |
| Human development | 3.56 | 0.281094 |
| Mean VIF | 1.95 | – |
References
- 1.Kozlakidis Z., Struelens M.J. Editorial: insights in coronavirus disease (Covid-19) - surveillance, prevention and treatment. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.998998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cirakli U., Dogan I., Gozlu M. The relationship between Covid-19 cases and Covid-19 testing: a panel data analysis on OECD countries. Journal of the Knowledge Economy. 2021;2021:1–14. doi: 10.1007/s13132-021-00792-z. [DOI] [Google Scholar]
- 3.Brodeur A., Clark A.E., Fleche S., et al. Covid-19, lockdowns and well-being: evidence from google trends. J. Publ. Econ. 2023;193 doi: 10.1016/J.JPUBECO.2020.104346. 2021 Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koh D. Covid-19 lockdowns throughout the world. Occup. Med. (Lond.) 2020 doi: 10.1093/occmed/kqaa073. 2020 May 2:kqaa073. [DOI] [Google Scholar]
- 5.Tran P., Tran L., Tran L. The influence of social distancing on Covid-19 mortality in US counties: cross-sectional study. JMIR Public Health Surveill. 2021;7(3) doi: 10.2196/21606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faus M., Alonso F., Javadinejad A., Useche S.A. Are social networks effective in promoting healthy behaviors? A systematic review of evaluations of public health campaigns broadcast on. Twitter. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.1045645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grantham J.L., Verishagen C.L., Whiting S.J., Henry C.J., Lieffers J.R. Evaluation of a social media campaign in Saskatchewan to promote healthy eating during the Covid-19 pandemic: social media analysis and qualitative interview study. J. Med. Internet Res. 2021;23 doi: 10.2196/27448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Warren G.W., Lofstedt R. Risk communication and Covid-19 in Europe: lessons for future public health crises. J. Risk Res. 2021;2021(5):1–15. doi: 10.1080/13669877.2021.1947874. [DOI] [Google Scholar]
- 9.Wiegel J.J. SARS-CoV-2 Vaccination: the time is now. Kidney360. 2021;2(9):1402–1404. doi: 10.34067/KID.0005352021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu K.W. Why is it necessary to improve Covid-19 vaccination coverage in older people? How to improve the vaccination coverage? Hum. Vaccines Immunother. 2023;19(2) doi: 10.1080/21645515.2023.2229704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halpern S.D., Truog R.D., Miller F.G. Cognitive bias and public health policy during the Covid-19 pandemic. JAMA, J. Am. Med. Assoc. 2020;324(4) doi: 10.1001/jama.2020.11623. [DOI] [PubMed] [Google Scholar]
- 12.Mohamed K., Yazdanpanah N., Saghazadeh A., Rezaei N. Cognitive biases affecting the maintenance of Covid-19 pandemic. Acta Biomed. 2021;92(2) doi: 10.23750/abm.v92i2.11073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cabrera-Álvarez P., Hornsey M.J., Lobera J. Determinants of self-reported adherence to Covid-19 regulations in Spain: social norms, trust and risk perception. Health Promot. Int. 2022;37(6):daac138. doi: 10.1093/heapro/daac138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mevorach T., Cohen J., Apter A. Keep Calm and Stay Safe: the relationship between anxiety and other psychological factors, media exposure and compliance with Covid-19 regulations. Int J Environ Res Public Health. 2021;18(6):2852. doi: 10.3390/ijerph18062852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stanica C., Crosby A., Larson S. Trust in government and Covid-19 response policy: a comparative approach. J. Comp. Pol. Anal.: Research and Practice. 2023;25:2. doi: 10.1080/13876988.2022.2103672. [DOI] [Google Scholar]
- 16.Vu V.T. Public trust in government and compliance with policy during Covid-19 pandemic: empirical evidence from Vietnam. Publ. Organ. Rev. 2021;21 doi: 10.1007/S11115-021-00566-W. [DOI] [Google Scholar]
- 17.Bright B., Babalola C.P., Sam-Agudu N.A., Onyeaghala A.A., Olatunji A., Aduh U., Sobande P.O., Crowell T.A., Tebeje Y.K., Phillip S., Ndembi N., Folayan M.O. Covid-19 preparedness: capacity to manufacture vaccines, therapeutics and diagnostics in sub-Saharan Africa. Global Health. 2021;17(1):24. doi: 10.1186/s12992-021-00668-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Narayanasamy S., Okware B., Muttamba W., Patel K., Duedu K.O., Ravi N., Ellermeier N., Shey M., Woods C.W., Sabiiti W. Global Inequity of Covid-19 Diagnostics: Challenges and Opportunities. J Epidemiol Community Health; 2022. Covid-19 clinical research coalition, virology, immunology, and diagnostics working group. jech-2022-219333. [DOI] [PubMed] [Google Scholar]
- 19.Anderson C.J., Hobolt S.B. Creating compliance in crisis: messages, messengers, and masking up in Britain. W. Eur. Polit. 2022;46:2. doi: 10.1080/01402382.2022.2091863. [DOI] [Google Scholar]
- 20.Sorci G., Faivre B., Morand S. Explaining among-country variation in Covid-19 case fatality rate. Sci. Rep. 2020;10 doi: 10.1038/s41598-020-75848-2. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parker R., Ferraz D. Politics and pandemics. Global Publ. Health. 2021;16:8–9. doi: 10.1080/17441692.2021.1947601. [DOI] [PubMed] [Google Scholar]
- 22.Daher-Nashif S. In sickness and in health: the politics of public health and their implications during the Covid-19 pandemic. Sociology Compass. 2021 doi: 10.1111/soc4.12949. [DOI] [Google Scholar]
- 23.Han S.M., Lwin K.S., Swe K.T., Gilmour S., Nomura S. Military coup during Covid-19 pandemic and health crisis in Myanmar. BMJ Glob. Health. 2021;6(4) doi: 10.1136/bmjgh-2021-005801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sowers J.L., Weinthal E., Zawahri N. Targeting environmental infrastructures, international law, and civilians in the new Middle Eastern wars. Secur. Dialog. 2017;48(5):410–430. doi: 10.1177/0967010617716615. [DOI] [Google Scholar]
- 25.Wise P.H., Barry M. Civil war & the global threat of pandemics. Daedalus. 2017;146(4):71–84. doi: 10.1162/DAED_a_00460. [DOI] [Google Scholar]
- 26.Carlson C.J., Albery G.F., Phelan A. Preparing international cooperation on pandemic prevention for the Anthropocene. BMJ Glob. Health. 2021;6(3) doi: 10.1136/bmjgh-2020-004254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taghizade S., Chattu V.K., Jaafaripooyan E., Kevany S. Covid-19 pandemic as an excellent opportunity for global health diplomacy. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.655021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Campos J.E., Lien D. Political instability and illegal immigration. J. Popul. Econ. 1995;8(1):23–33. doi: 10.1007/BF00172036. [DOI] [PubMed] [Google Scholar]
- 29.Jaspal R., Assi M., Maatouk I. Potential impact of the Covid-19 pandemic on mental health outcomes in societies with economic and political instability: case of Lebanon. Ment. Health Rev. 2020;25(3) doi: 10.1108/MHRJ-05-2020-0027. [DOI] [Google Scholar]
- 30.Creţan R., Light D. Covid-19 in Romania: transnational labour, geopolitics and the Roma ‘outsiders’. Eurasian Geogr. Econ. 2020 doi: 10.1080/15387216.2020.1780929. 61. [DOI] [Google Scholar]
- 31.Glik D.C. Risk communication for public health emergencies. Annu. Rev. Publ. Health. 2007;28 doi: 10.1146/annurev.publhealth.28.021406.144123. [DOI] [PubMed] [Google Scholar]
- 32.Abraham T. Lessons from the pandemic: the need for new tools for risk and outbreak communication. Emerg. Health Threats J. 2011;4 doi: 10.3402/ehtj.v4i0.7160. 7160-7160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cepaluni G., Dorsch M.T., Branyiczki R. Political regimes and deaths in the early stages of the Covid-19 pandemic. J. Publ. Financ. Public Choice. 2022;37(1):27–53. doi: 10.1332/251569121X16268740317724. [DOI] [Google Scholar]
- 34.Cepaluni G., Dorsch M., Dzebo S. Working paper; 2021. Populism, political regimes, and Covid-19 deaths.https://ssrn.com/abstract=3816398 ISBN: 1556-5068. [Google Scholar]
- 35.Garcia P.J. Corruption in global health: the open secret. Lancet. 2019;394(10214) doi: 10.1016/s0140-6736(19)32527-9. [DOI] [PubMed] [Google Scholar]
- 36.Kohler J.C., Bowra A. Exploring anti-corruption, transparency, and accountability in the world health organization, the united nations development programme, the world bank group, and the global fund to fight AIDS, tuberculosis and malaria. Glob. Health. 2020;16(1) doi: 10.1186/s12992-020-00629-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burki T. Corruption is an "ignored pandemic". Lancet Infect. Dis. 2019;19(5) doi: 10.1016/s1473-3099(19)30178-1. 471-471. [DOI] [PubMed] [Google Scholar]
- 38.World Bank . 2022. Global Economic Prospects.https://openknowledge.worldbank.org/server/api/core/bitstreams/1a18a651-c40b-5316-8898-bb3bd60ca390/content January 2022. [Google Scholar]
- 39.Buheji M., da Costa Cunha K., Beka G., Yein T.C. The extent of covid-19 pandemic socio-economic impact on global poverty. A global integrative multidisciplinary review. Am. J. Econ. 2020;10:213–224. doi: 10.5923/j.economics.20201004.02. [DOI] [Google Scholar]
- 40.Lancet India under Covid-19 lockdown. Lancet. 2020;395(10233):1315. doi: 10.1016/S0140-6736(20)30938-7. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Daras K., Alexiou A., Rose T.C., Buchan I., Taylor-Robinson D., Barr B. How does vulnerability to covid-19 vary between communities in England? Developing a small area vulnerability index (SAVI) Social Science Research Network. 2020;75(8) doi: 10.2139/ssrn.3650050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chetty R., Friedman J.N., Hendren N., Stepner M. How Did Covid-19 and Stabilization Policies Affect Spending and Employment? A New Real-Time Economic Tracker Based on Private Sector Data. National Bureau of Economic Research; Cambridge, MA: 2020. The opportunity insights team.https://www.nber.org/system/files/working_papers/w27431/revisions/w27431.rev1.pdf NBER Working Paper 27431. [Google Scholar]
- 43.Brussevich M., Dabla-Norris E., Khalid S. Who will bear the brunt of lockdown policies? Evidence from tele-workability measures across countries. IMF Working Paper. 2020:20–88. doi: 10.5089/9781513546285.001. [DOI] [Google Scholar]
- 44.Darvas Z. 2021. The unequal inequality impact of the Covid-19 pandemic.https://www.jstor.org/stable/pdf/resrep32250.pdf Working Papers 41764, Bruegel.Handle: RePEc:bre:wpaper:41764. [Google Scholar]
- 45.Whitehead M., Taylor-Robinson D., Barr B. Covid-19: we are not “all in it together”—less privileged in society are suffering the brunt of the damage. BMJ Opinion. 2020 https://blogs.bmj.com/bmj/2020/05/22/covid-19-we-are-not-all-in-it-together-less-privileged-in-society-are-suffering-the-brunt-of-the-damage/ 22 May 2020. [Google Scholar]
- 46.Hefferon C., Taylor C., Bennett D., Falconer C., Taylor-Robinson D. Priorities for the child public health response to the Covid-19 pandemic recovery in England. Arch. Dis. Child. 2020;106 doi: 10.1136/archdischild-2020-320214. 6:archdischild-2020-320214. [DOI] [PubMed] [Google Scholar]
- 47.Brewer M., Patrick R. Resolution Foundation; 2021. Pandemic Pressures: Why Families on Low Income Are Spending More during Covid-19.https://www.resolutionfoundation.org/app/uploads/2021/01/Pandemic-pressures.pdf [Google Scholar]
- 48.Sepahvand M., Verwimp P. Fighting Covid-19 amidst civil conflict: micro-level evidence from Burkina Faso. World Dev. 2023;170(106343):1–34. doi: 10.1016/j.worlddev.2023.106343. [DOI] [Google Scholar]
- 49.Ozkan A., Ozkan G., Yalaman A., Yildiz Y. Climate risk, culture and the Covid-19 mortality: a cross-country analysis. World Dev. 2021;141 doi: 10.1016/j.worlddev.2021.105412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hoti S., McAleer M., Shareef R. Modelling international tourism and country risk spillovers for Cyprus and Malta. Tourism Manag. 2007;28(6) doi: 10.1016/j.tourman.2007.02.014. [DOI] [Google Scholar]
- 51.Law S.H., Lim T.C., Ismail N.W. Institutions and economic development: a Granger causality analysis of panel data evidence. Econ. Syst. 2013;37(4):610–624. doi: 10.1016/j.ecosys.2013.05.005. [DOI] [Google Scholar]
- 52.Chen H., Liao H., Tang B.J., Wei Y.M. Impacts of OPEC's political risk on the international crude oil prices: an empirical analysis based on the SVAR models. Energy Econ. 2016;57:42–49. doi: 10.1016/j.eneco.2016.04.018. [DOI] [Google Scholar]
- 53.Sussman N. vol. 11. COVID Economics; 2020. https://www.researchgate.net/publication/341043555_Time_for_beds_Hospital_capacity_and_mortality_from_COVID-19 (Time for Bed(s): Hospital Capacity and Mortality from Covid-19). [Google Scholar]
- 54.Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T. How will country-based mitigation measures influence the course of the Covid-19 epidemic? The Lancet, Mar21. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gelfand M.J., Jackson J.C., Pan X., Nau D., Pieper D., Denison E.…Wang M. The relationship between cultural tightness-looseness and Covid-19 cases and deaths: a global analysis. Lancet Planet. Health. 2021;5(3):e135–e144. doi: 10.1016/s2542-5196(20)30301-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Roederer, T., Mollo, B., Vincent, C., et al., High seroprevalence of SARS-CoV-2 antibodies among people living in precarious situations in Ile de France, working paper. doi: 10.1101/2020.10.07.20207795. [DOI]
- 57.Van den Broucke S. Strengthening public health capacity through a health promotion lens. Health Promot. Int. 2017;32(5) doi: 10.1093/heapro/dax064. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.