Abstract
COVID-19 has posed formidable challenges as a significant global health crisis. Its complexity stems from factors like viral contagiousness, population density, social behaviors, governmental regulations, and environmental conditions, with interpersonal interactions and large-scale activities being particularly pivotal. To unravel these complexities, we used a modified SEIR epidemiological model to simulate various outbreak scenarios during the holiday season, incorporating both inter-regional and intra-regional human mobility effects into the parameterization scheme. In addition, evaluation metrics were used to evaluate the accuracy of the model simulation by comparing the congruence between simulated results and recorded confirmed cases. The findings suggested that intra-city mobility led to an average surge of 57.35% in confirmed cases of China, while inter-city mobility contributed to an average increase of 15.18%. In the simulation for Tianjin, China, a one-week delay in human mobility attenuated the peak number of cases by 34.47% and postponed the peak time by 6 days. The simulation for the United States revealed that human mobility played a more pronounced part in the outbreak, with a notable disparity in peak cases when mobility was considered. This study highlights that while inter-regional mobility acted as a trigger for the epidemic spread, the diffusion effect of intra-regional mobility was primarily responsible for the outbreak. We have a better understanding on how human mobility and infectious disease epidemics interact, and provide empirical evidence that could contribute to disease prevention and control measures.
Keywords: COVID-19, Modified SEIR model, Human mobility, Parameterization scheme
1. Introduction
COVID-19 is a serious global public health emergency with a devastating impact on the society, this pandemic not only brought an unprecedented crisis to socio-economic order, but it also posed a monumental challenge to global health systems (Jain et al., 2022; Nicola et al., 2020; Lian et al., 2020; Kraemer et al., 2020). The virus spread is influenced by multiple complex factors, such as infectivity, population density, social activities, protective measures, sanitation, government controls, and environmental aspects (Cheng et al., 2020; Qiu et al., 2020; Honein et al., 2020; Hamidi et al., 2020; Huang et al., 2020). Interpersonal communication significantly contributes to the virus's spread, and large-scale human activities correlate significantly with epidemic spread (Prem et al., 2020; Hu et al., 2021; Yang et al., 2020).
Many models have upgraded the traditional SIR model for simulating complex scenarios (He et al., 2020; Yang et al., 2020). Huang et al. (2020) combined statistical and dynamic climate prediction methods in atmospheric science with a modified SEIR model of infectious disease transmission dynamics to develop a COVID-19 global pandemic prediction system. The system incorporates government control and isolation, congregation and indoor transmission, seasonal and environmental impacts, virus mutation and vaccination parameter schemes (Liu et al., 2021; Huang et al., 2021). Furthermore, Chen et al. (2020) constructed a COVID-19 transmission dynamics model with multiple population groups and multiple transmission modes using multidisciplinary methods such as mathematical modeling, epidemiology, and genomics. Meanwhile, incorporating human mobility into such models is essential due to its significant impact on disease spread (Drake et al., 2020). Studies have demonstrated a close link between mobility and infection rates, with reduced mobility potentially curbing case growth (Li, 2020; Prem et al., 2020; Hu et al., 2021; Jia et al., 2020).
Many studies have shown that the spread of epidemics is affected by factors related to human mobility. However, it is currently unclear to what extent human mobility factors influence the epidemic spread. In this study, human mobility factors are integrated into the modified SEIR model to measure its impact on the epidemic. Epidemics during the Spring Festival in China and Christmas in the US are simulated separately, assessing both intra-regional and inter-regional mobility contributions to disease spread. We introduce a delay in human mobility, simulating control measures' effects, and propose a possible mobility impact mechanism on epidemic transmission. The model's effectiveness is confirmed using various evaluation metrics. Overall, this research enhances the existing research on the relationship of human mobility and epidemic spread, providing a scientific foundation for disease control and prevention strategies.
2. Materials and methods
2.1. Data source
This study utilizes the COVID-19 dataset from the Center for Systems Science and Engineering at Johns Hopkins University (Dong et al., 2020), accessible through their GitHub repository (https://github.com/CSSEGISandData/COVID-19). Data on confirmed cases, daily recoveries, and deaths in China are sourced from the National Health Commission (http://www.nhc.gov.cn/). China's human mobility data comes from Baidu's migration platform (http://qianxi.baidu.com) and traffic website (https://jiaotong.baidu.com), while the mobility data of US is obtained from the Department of Transportation's Bureau of Transportation Statistics (https://www.bts.dot.gov/covid-19).
2.2. The modified SEIR model
We employed the second version of the Global Prediction System for the COVID-19 Pandemic (GPCP) proposed by Lanzhou University for our epidemiological simulations. This advanced version expands on the SEIR model to better simulate and predict epidemics. It recognizes seven disease states: susceptible (S), protected (P), exposed (E), infected (I), quarantined (Q), recovered (R), and deaths (D). The coefficients α, β, γ, δ, λ, and κ signify rates of protection, transmission, average latent period inversion, infection-to-quarantine transition, variable recovery, and variable mortality, respectively. The model is built on the following equations:
2.3. Inter-regional human mobility parameterization scheme
This scheme incorporates human mobility between regions by factoring in both inflow and outflow of susceptible and exposed individuals. The quantities Min and Mout denote population flow into and out of a given region. Ein and Eout represent estimated exposed individuals flowing in and out of the region, whereas Sin and Sout represent estimated susceptible individuals flowing in and out of the region. Elocal and Emove represent the changes in the number of exposed individuals within a specific region and the changes in the number of exposed individuals during the process of population inflow and outflow, respectively. Similarly, Slocal and Smove represent the same for the susceptible population. Kin and Kout are trainable parameters, and N is the total population of a region at time t. The model equation for inter-regional human mobility is as follows:
2.4. Intra-regional human mobility parameterization scheme
Increased intra-regional mobility accelerates the chance of transmission sources interacting with susceptible individuals, possibly causing a higher infection risk. The susceptible population in a region grows by PT[t] per time unit, while the protected population decreases by the same amount. In the parameterization scheme for intra-regional human mobility, the changes between the susceptible and protected populations are considered. Here, the susceptible population primarily refers to individuals in a susceptible state, indicating those who have the opportunity to come into contact with infected individuals and are prone to infection. The protected population mainly represents those with a higher level of immunity due to vaccination or those with a relatively lower risk of infection due to certain restrictive measures. Moreover, in the intra-regional mobility scheme, since only the mobility of people within the region is considered, it is assumed that the total population of the area remains constant. Kre is a trainable parameter. The model equation for intra-regional human mobility is as follows:
2.5. Inter-regional and intra-regional human mobility parameterization scheme
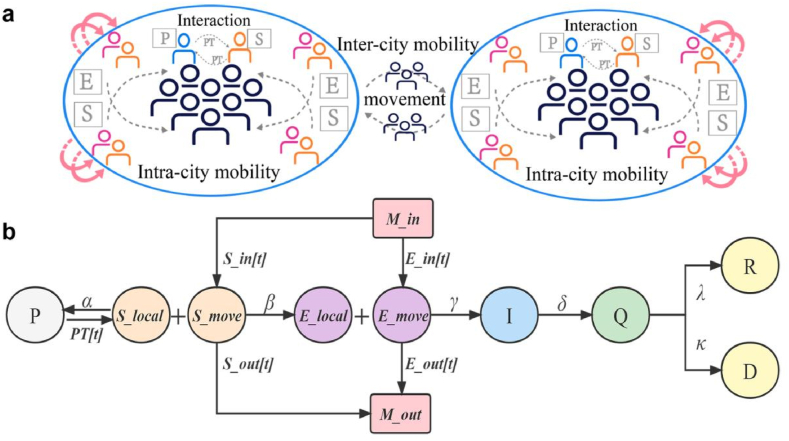
Fig. 1a illustrates the integration of both inter-regional and intra-regional human mobility into our model, accounting for their collective impact on epidemic spread. The finalized 'Inter-regional and Intra-regional human mobility model' framework is depicted in Fig. 1b, with Kre、Kin、Kout as trainable parameters.
Fig. 1.
The inter-regional and intra-regional human mobility simulation scheme. a The transmission process of the epidemic influenced by human mobility. b The modified inter-regional and intra-regional human mobility model scheme that integrates human mobility parameters.
2.6. Evaluation metrics
This study evaluates simulation accuracy using Mean Relative Error (MRE), Pearson Correlation Coefficient (PCC), and Root Mean Squared Error (RMSE). PCC gauges the linear relationship between two curves, MRE measures prediction variations relative to real values, and RMSE provides an aggregate evaluation of prediction precision.
3. Results
3.1. Empirical analysis of human mobility and COVID-19
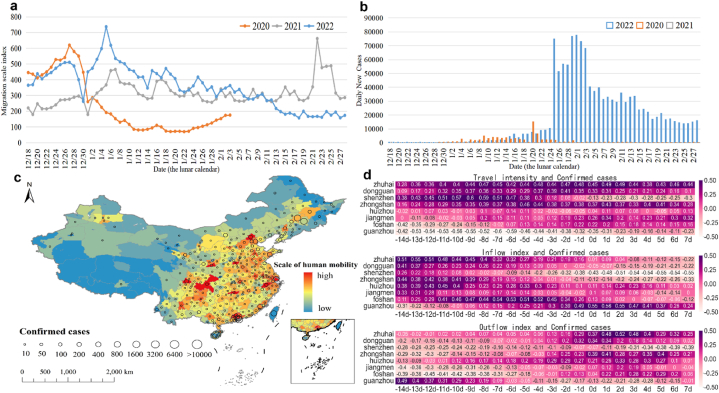
In 2022, with the relative easing of pandemic restrictions, human mobility in China increased significantly, rising by 193.3% compared to 2020, and 46.5% compared to 2021 (Fig. 2a). A major COVID-19 outbreak occurred during the 2022 Spring Festival, resulting in a nationwide increase in new cases by over 631.43% within a month (Fig. 2b). Correlation analysis between confirmed cases and travel intensity, inflow and outflow indices in Guangdong during this period, showed significant correlations, most notably when human mobility lagged by 7 days (Fig. 2d). A positive correlation was found between confirmed cases and both travel intensity and the inflow index, whereas a negative correlation existed with the outflow index. Fig. 2c displays the spatial distribution of new cases and the average mobility scale index from January 20 to March 30, 2022, revealing that regions with higher incidence rates corresponded to areas of greater mobility.
Fig. 2.
Empirical analysis of human mobility and COVID-19 during the Chinese New Year period. a The national human mobility index from 2020 to 2022. b The number of newly confirmed cases nationwide from 2020 to 2022. c The spatial distribution of confirmed cases and human mobility scale in 2022. d The correlation analysis between the number of confirmed cases in the cities of Guangdong province and the travel intensity, inflow index and outflow index.
3.2. Simulation results for cities in China
In Fig. 3, this study illustrates inter-city mobility simulations for China. For some cities in Guangdong province with high population outflow, the inter-city mobility negatively influences the epidemic spread. This adverse effect arises primarily from the high numbers of departing exposed and susceptible individuals. In most other cities, inflow and outflow populations are comparable. On average, inter-city mobility increases case numbers by 15.18% (Supplementary Fig. A1a). To reflect control measure impacts, simulations with delayed human mobility were conducted, revealing that such delays resulted in a slight decrease in peak case numbers and minimal impact on peak arrival time (Supplementary Fig. A2).
Fig. 3.
The simulation of daily new cases considering inter-city human mobility. The red dashed line represents the simulated curve generated by the scheme considering inter-city human mobility, with circles corresponding to daily reported confirmed cases. The blue solid line represents the simulation result without considering inter-city human mobility.
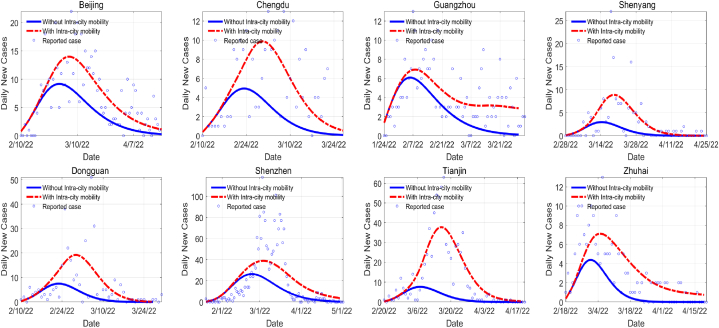
In the intra-city mobility simulation (Fig. 4), considering human mobility results in significantly higher case numbers than the simulation without mobility, with an average increase of 57.35%, outstripping inter-city mobility contributions (Supplementary Fig. A1b). Furthermore, mobility lag time significantly impacts results (Supplementary Fig. A3). In the simulation of Tianjin city in China, delaying human mobility has a significant effect on the COVID-19 outbreak. In particular, a delay of five days, one week, two weeks, and three weeks reduces the peak number of cases by 23.86%, 34.47%, 71.59%, and 90.15%, respectively. Meanwhile, the time required to reach the peak is delayed by 4, 6, 13, and 19 days, respectively. Current results indicate that the intra-city mobility has a greater impact on amplifying epidemic transmission dynamics than inter-city mobility. When an external infection source interacts with local populations, intra-city mobility becomes the primary epidemic driver.
Fig. 4.
The simulation of daily new cases considering intra-city human mobility. The red dashed line represents the simulated curve generated by the scheme considering intra-city human mobility, with circles corresponding to daily reported confirmed cases. The blue solid line represents the simulation result without considering intra-city human mobility.
Simulations considering both inter-city and intra-city mobility accurately capture reported confirmed cases, showing a notable concordance (Supplementary Fig. A4). This study emphasizes that intra-regional mobility, which primarily influences virus spread within a region, has a larger impact than inter-regional mobility. By adjusting human mobility scheduling, we demonstrate the effects of control measures. Advancing human mobility timing increases contact between individuals across regions, raising transmission rates and confirmed cases. In contrast, control measures that delay mobility reduce exposure risk and help mitigate the impact of an upcoming peak in the epidemic.
3.3. Simulation results for states in US
During the 2021 Christmas season, the US experienced a substantial COVID-19 outbreak, with cases increasing by 443.06% within one month, approximately 2.27 times the incidence recorded in the corresponding period of 2020 (Supplementary Fig. A5). This study simulates the outbreak across 36 states, using only intra-regional human mobility data due to lack of inter-regional data. As illustrated in Supplementary Fig. A6-A7, our model effectively captures COVID-19 spread dynamics. We further quantified human mobility's impact on outbreaks in US states, showing that intra-state mobility increased case numbers by 72.04% on average (Supplementary Fig. A8). Comparisons of peak cases simulated with and without mobility considerations show an average difference of nearly 6992 individuals and a maximum difference of 36,807 (Supplementary Fig. A9).
3.4. Evaluation of simulation results for China
Table 1 presents the evaluation results of simulating confirmed cases in China, and incorporating human mobility into our model generally improved its fitting capabilities. Of the three schemes, the inter-city and intra-city model performed best, with average MRE, PCC, and RMSE values of 0.02449, 0.99486, and 27.31250, respectively. These high scores underscore the importance of considering both inter-regional and intra-regional mobility in disease transmission modeling, and highlight the effectiveness of the combined inter-regional and intra-regional mobility scheme.
Table 1.
Evaluation of simulation results for the confirmed cases of China.
| City | Inter-City Scheme |
Intra-City Scheme |
Inter-City and Intra-City Scheme |
||||||
|---|---|---|---|---|---|---|---|---|---|
| MRE | PCC | RMSE | MRE | PCC | RMSE | MRE | PCC | RMSE | |
| Guangzhou | 0.00563 | 0.99419 | 16.2 | 0.00219 | 0.99854 | 6.2 | 0.00339 | 0.99573 | 9.9 |
| Shenzhen | 0.10110 | 0.98594 | 160.2 | 0.08903 | 0.98658 | 155.1 | 0.06693 | 0.99143 | 117.2 |
| Dongguan | 0.05220 | 0.99162 | 22.2 | 0.05161 | 0.99618 | 23.1 | 0.03170 | 0.99559 | 12.7 |
| Zhuhai | 0.02869 | 0.99738 | 8.2 | 0.04822 | 0.98248 | 16.7 | 0.01619 | 0.99645 | 5.4 |
| Beijing | 0.01434 | 0.99295 | 26.7 | 0.00836 | 0.99899 | 16.2 | 0.00913 | 0.99641 | 18.5 |
| Tianjin | 0.03869 | 0.98090 | 68.9 | 0.01744 | 0.99563 | 35.9 | 0.01897 | 0.98962 | 40.8 |
| Shenyang | 0.05121 | 0.99577 | 9.7 | 0.03486 | 0.99721 | 6.8 | 0.04573 | 0.99596 | 8.8 |
| Chengdu | 0.00626 | 0.99763 | 8.6 | 0.00552 | 0.99618 | 7.6 | 0.00384 | 0.99769 | 5.2 |
| Average | 0.03727 | 0.99205 | 40.0875 | 0.03215 | 0.99397 | 33.4500 | 0.02449 | 0.99486 | 27.31250 |
3.5. Evaluation of simulation results for US
Table 2 displays the evaluation results of our simulation of confirmed cases in the US, emphasizing the model's exceptional performance, as detailed within the table. It accurately reflected the trend in case numbers during this period and aligned well with the reported cases, showing its ability to effectively capture the outbreak's dynamics in the US.
Table 2.
Evaluation of simulation results for the confirmed cases of US.
| State | MRE | RMSE | State | MRE | RMSE | State | MRE | RMSE |
|---|---|---|---|---|---|---|---|---|
| Alabama | 0.01032 | 13248.5 | Kentucky | 0.00793 | 10777.6 | Ohio | 0.00289 | 9825.6 |
| Arizona | 0.01013 | 20753.4 | Louisiana | 0.00730 | 10087.7 | Oklahoma | 0.01611 | 17259.7 |
| Arkansas | 0.00565 | 4541.0 | Maryland | 0.01644 | 15716.6 | Oregon | 0.00850 | 6041.5 |
| California | 0.00299 | 29684.5 | Massachusetts | 0.00696 | 12409.4 | Pennsylvania | 0.00261 | 8101.1 |
| Colorado | 0.00283 | 4341.7 | Minnesota | 0.01225 | 20184.4 | South Carolina | 0.01490 | 21557.7 |
| Connecticut | 0.00473 | 4393.4 | Mississippi | 0.01183 | 10091.5 | Tennessee | 0.00470 | 9744.1 |
| Delaware | 0.00297 | 863.0 | Missouri | 0.00644 | 11224.3 | Texas | 0.00613 | 42225.1 |
| Florida | 0.00978 | 58887.3 | Nevada | 0.01378 | 9737.4 | Utah | 0.01399 | 13372.3 |
| Hawaii | 0.01133 | 2435.9 | New Jersey | 0.00401 | 8550.2 | Virginia | 0.00506 | 10010.2 |
| Illinois | 0.00426 | 16440.0 | New Mexico | 0.00673 | 3882.2 | Washington | 0.01740 | 24743.4 |
| Indiana | 0.00956 | 17093.7 | New York | 0.00365 | 18920.5 | West Virginia | 0.00842 | 4194.0 |
| Iowa | 0.00545 | 4605.7 | North Carolina | 0.00870 | 24248.3 | Wisconsin | 0.01727 | 29278.2 |
4. Conclusion
Large-scale human mobility can easily cause widespread transmission of epidemics during holiday periods. This study considers the influence of human social behaviors such as inter-regional and intra-regional human mobility in the constructed model schemes. Simulations revealed an average case increase of 57.35% due to intra-city mobility and 15.18% due to inter-city mobility in Chinese cities. The delayed duration of human mobility has a significant effect on the intra-city human mobility simulation results. In the simulation for Tianjin, China, a one-week delay reduces peak case numbers by 34.45% and postpones the peak by 6 days. A two-week delay further cuts peak numbers by 71.59% and pushes the peak back by 13 days. In the simulation for states of US, intra-regional human mobility led to an average increase of 72.04% in the number of cases. The performance of the evaluation metrics in both the simulation results for China during the Spring Festival and the simulation results for the US during the Christmas demonstrates the efficacy of the constructed scheme. Our study also provides a summary of the primary triggers and transmission routes of epidemics during holiday seasons. The results indicate that intra-regional human mobility plays a significant role in the epidemiological modeling of COVID-19. Given that the spread of COVID-19 is significantly dependent on the dynamics of human mobility, the majority of preventative measures can manifest as changes in human mobility patterns. While intra-regional human mobility determines the response time for the spread of infections within regions, inter-regional human mobility primarily reflects the inflow time of external sources of infection from other regions. This study investigates the connection between human mobility and epidemic spread, supplementing existing research, and it also provides a basis for early warnings and insights for disease prevention and control.
5. Discussion
The model constructed in this study can effectively simulate the spread of epidemics using human mobility data. Despite the fact that the model incorporates control measures based on changes in human mobility, it has limitations due to potential biases in the COVID-19 dataset resulting from disparities in regional reporting schemes. And the study did not account for transnational city and country transmissions, which may exhibit distinct spatial patterns and necessitate further investigation. In addition, our model may overestimate infections in regions with high human mobility and underestimate infections in regions with lower human mobility, highlighting the need for additional research on the spatial variations of epidemic transmission due to human mobility. In this study, we only considered the impact of human mobility on the spread of infectious diseases. Other influencing factors, such as economic and medical standards, vary significantly across regions and can also affect the transmission patterns of diseases in different areas. Future research needs to consider these various factors comprehensively. Aspects such as indirect transmission processes during human mobility and environmental factors affecting the spread of the disease also require further consideration. Furthermore, epidemic models have developed greatly in recent years, the majority of these models still only capture the time-dynamic growth of the number of cases and do not adequately capture the two-dimensional epidemic and diffusion processes of infectious diseases. Further research and discussion are needed on the spatio-temporal diffusion of the impact of human mobility on infectious diseases in the future.
Funding
This study was supported by the Frontier of Interdisciplinary Research on Monitoring and Prediction of Pathogenic Microorganisms in the Atmosphere (XK2022DXC005, L2224041), the Self-supporting Program of Guangzhou Laboratory (SRPG22-007), the Gansu Province Intellectual Property Program (Oriented Organization) Project (22ZSCQD02), and the Fundamental Research Funds for the Central Universities (lzujbky-2022-kb10).
Authors’ contributions
Han Li: Conceptualization, Data curation, Methodology, Formal analysis, Visualization, Writing-Original Draft; Jianping Huang: Conceptualization, Methodology, Writing-Original Draft, Supervision, Funding acquisition, Project administration; Xinbo Lian: Methodology, Software, Formal analysis, Investigation, Writing-Review & Editing; Yingjie Zhao: Methodology, Software, Formal analysis, Writing-Review & Editing; Wei Yan: Investigation, Software, Formal analysis; Li Zhang: Software, Investigation; Licheng Li: Methodology, Supervision; All of the authors contributed to the discussion and interpretation of the manuscript. All authors read and approved the final manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors acknowledge the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University for providing the COVID-19 data.
Handling Editor: Dr Yiming Shao
Footnotes
Peer review under responsibility of KeAi Communications Co., Ltd.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.idm.2023.10.001.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- Cheng V.C.C., Wong S.C., Chuang V.W.M., So S.Y.C., Chen J.H.K., Sridhar S.…Yuen K.Y. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. Journal of Infection. 2020;81(1):107–114. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen T.M., Rui J., Wang Q.P., Zhao Z.Y., Cui J.A., Yin L. A mathematical model for simulating the phase-based transmissibility of a novel coronavirus. Infectious Dis. Poverty. 2020;9(1):1–8. doi: 10.1186/s40249-020-00640-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. The Lancet Infectious Diseases. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake T.M., Docherty A.B., Weiser T.G., Yule S., Sheikh A., Harrison E.M. The effects of physical distancing on population mobility during the COVID-19 pandemic in the UK. The Lancet Digital Health. 2020;2(8):e385–e387. doi: 10.1016/S2589-7500(20)30134-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi S., Sabouri S., Ewing R. Does density aggravate the COVID-19 pandemic? Early findings and lessons for planners. Journal of the American Planning Association. 2020;86(4):495–509. [Google Scholar]
- He S., Peng Y., Sun K. SEIR modeling of the COVID-19 and its dynamics. Nonlinear Dynamics. 2020;101:1667–1680. doi: 10.1007/s11071-020-05743-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honein M.A., Christie A., Rose D.A., Brooks J.T., Meaney-Delman D., Cohn A.…Williams I. Summary of guidance for public health strategies to address high levels of community transmission of SARS-CoV-2 and related deaths, December 2020. Morbidity and Mortality Weekly Report. 2020;69(49):1860. doi: 10.15585/mmwr.mm6949e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J., Zhang L., Liu X., Wei Y., Liu C., Lian X.…Zhang T. Global prediction system for COVID-19 pandemic. Science Bulletin. 2020;65(22):1884. doi: 10.1016/j.scib.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Z., Huang J., Gu Q., Du P., Liang H., Dong Q. Optimal temperature zone for the dispersal of COVID-19. Science of the Total Environment. 2020;736 doi: 10.1016/j.scitotenv.2020.139487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J., Liu X., Zhang L., Zhao Y., Wang D., Gao J.…Liu C. The oscillation-outbreaks characteristic of the COVID-19 pandemic. National Science Review. 2021;8(8):nwab100. doi: 10.1093/nsr/nwab100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Z., Wu Y., Su M., Xie L., Zhang A., Lin X., Nie Y. Population migration, spread of COVID-19, and epidemic prevention and control: Empirical evidence from China. BMC Public Health. 2021;21:1–12. doi: 10.1186/s12889-021-10605-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain N., Hung I.C., Kimura H., Goh Y.L., Jau W., Huynh K.L.A.…Huy N.T. The global response: How cities and provinces around the globe tackled covid-19 outbreaks in 2021. The Lancet Regional Health-Southeast Asia. 2022;4 doi: 10.1016/j.lansea.2022.100031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia J.S., Lu X., Yuan Y., Xu G., Jia J., Christakis N.A. Population flow drives spatio-temporal distribution of COVID-19 in China. Nature. 2020;582(7812):389–394. doi: 10.1038/s41586-020-2284-y. [DOI] [PubMed] [Google Scholar]
- Kraemer M.U., Yang C.H., Gutierrez B., Wu C.H., Klein B., Pigott D.M.…Scarpino S.V. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368(6490):493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X. Association between population mobility reductions and new COVID-19 diagnoses in the United States along the urban–rural gradient, February–April, 2020. Preventing Chronic Disease. 2020;17 doi: 10.5888/pcd17.200241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lian X., Huang J., Huang R., Liu C., Wang L., Zhang T. Impact of city lockdown on the air quality of COVID-19-hit of Wuhan city. Science of the Total Environment. 2020;742 doi: 10.1016/j.scitotenv.2020.140556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Huang J., Li C., Zhao Y., Wang D., Huang Z., Yang K. The role of seasonality in the spread of COVID-19 pandemic. Environmental Research. 2021;195 doi: 10.1016/j.envres.2021.110874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C.…Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. International Journal of Surgery. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prem K., Liu Y., Russell T.W., Kucharski A.J., Eggo R.M., Davies N.…Klepac P. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: A modelling study. The Lancet Public Health. 2020;5(5):e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu Y., Chen X., Shi W. Impacts of social and economic factors on the transmission of coronavirus disease 2019 (COVID-19) in China. Journal of Population Economics. 2020;33:1127–1172. doi: 10.1007/s00148-020-00778-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z., Zeng Z., Wang K., Wong S.S., Liang W., Zanin M.…He J. Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions. Journal of Thoracic Disease. 2020;12(3):165. doi: 10.21037/jtd.2020.02.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.