Abstract
Background
Shared decision-making (SDM), the process of engaging patients in their healthcare decisions, is an integral component of personalized medicine. The use of SDM in real-world allergy and asthma care in the United States (US) is unknown. Cross-sectional surveys of allergists and patients in a US population were conducted to assess the use and perceptions of SDM and SDM tools in real-world allergy and asthma care.
Methods
Allergists (N = 101) who were members of the American College of Allergy Asthma & Immunology (ACAAI) and who were also Dynata (a marketing research firm) research partners or in the Allergy & Asthma Network customer database completed an online survey from February–March 2022. Adult patients (N = 110) with asthma, allergy, and/or eczema in the United States who were participants of online research panels hosted by Dynata completed on online survey from February 1–7, 2022.
Results
Based on their own definition, 98% of the allergists reported familiarity with SDM, and 79% reported using it frequently. Allergists reported using SDM with an average of 44% of their patients. The most commonly used tool was the Immunotherapy SDM toolkit (40%); 43% had not used any SDM tool. Among allergists not using SDM or using it infrequently (n = 19), 42% considered it too time-consuming and 37% believed their patients have low health literacy. Of the surveyed patients, 25% reported their provider used SDM “frequently” or “occasionally” when being treated for allergies, asthma, or eczema, and 22% reported using SDM tools with their provider at some point. The most commonly used tool was the Asthma and Allergy Symptom Test (60%). Among patients whose allergists used SDM infrequently or never (n = 56), 70% reported they would be likely to ask their allergist to use SDM more often.
Conclusion
Survey responses revealed a disconnect between allergists and patients regarding SDM use. Barriers to SDM are consistent with those across the healthcare industry. Patients clearly expressed their desire for SDM.
Keywords: Rhinitis, Allergic, Asthma, Eczema, Decision making, Shared, Perception
Introduction
Shared decision-making (SDM) between healthcare providers and patients is now an integral part of personalized medicine. SDM is the process of actively engaging patients to make the best healthcare decision for the patient, not simply a good bedside manner, presenting treatment options, or even the use of a SDM tool. The role of the healthcare provider in SDM is to provide expertise on treatment options, benefits and harms of options, and treatment expectations, whereas patients provide input on their values and preferences related to treatment, as well as previous related medical experiences.1 SDM can empower and engage patients in their disease management, yet patients may need to be made aware that they have the right to engage in their own healthcare decisions. In addition, some vulnerable or marginalized patients may feel that their voice does not matter or is not being heard, and some patients may feel that the healthcare provider knows best so they should simply accept what they are told regarding their healthcare management.2,3 Thus, healthcare providers need to actively invite the patient to engage in the SDM process.
Adherence to treatment is critical to successful health outcomes, and patient preferences and expectations influence adherence.4,5 Thus, SDM conversations to fully explore these patient-related factors are particularly important for chronic disease, such as asthma, where adherence to treatment tends to decrease over time.4,6 Accordingly, SDM has been shown to improve adherence to asthma medications and asthma outcomes.7, 8, 9, 10 There is currently little information on the impact of SDM in other chronic allergic diseases (eg, allergic rhinitis or eczema).11
There are several SDM tools for asthma and other allergic diseases available through the American College of Allergy, Asthma & Immunology (ACAAI) website and other sources.12, 13, 14, 15, 16, 17, 18, 19 Although more validated SDM tools are needed in allergy, the tools that are available are applicable to diseases that would presumably be relevant to most allergists (ie, asthma, allergy immunotherapy, urticaria). The level of awareness and use of SDM and allergy- and asthma-specific SDM tools among allergists and patients with asthma or allergic diseases is unknown. Therefore, cross-sectional surveys of allergists and patients in a US population were conducted to assess the use and perceptions of SDM and SDM tools in real-world allergy and asthma care.
Methods
Survey methodology
The link to the online allergist survey was emailed to US allergists who were members of ACAAI and who were also Dynata research partners or in the Allergy & Asthma Network (AAN) customer database. Dynata is a marketing research firm. The allergist survey was conducted between February 10-March 11, 2022. The patient survey was made available online from February 1–7, 2022, to patients in the United States who were participants of online research panels hosted by Dynata.
The allergist and patient surveys and all study procedures were reviewed by an institutional review board (Advarra, Columbia, MD), and both surveys were given exemption status. The project was designed to comply with suggested quality standards for survey reporting in medical literature. Participants of both surveys gave consent within the surveys that they had read and understood the disclosure and agreed to the requirements to participate in the research. Survey data was linked to the research panel database using numeric identifiers so the identity of the panelist was always protected. For completing the surveys, allergist and patient participants were entered into a drawing for a $100 gift card.
Participant eligibility criteria
To participate in the allergist survey, participants had to be 25 years of age or older, be a physician specializing in allergy/asthma, be practicing for at least 3 years, and treat 26 or more asthma, allergy, and/or eczema patients per month.
To participate in the patient survey, patients had to be 18 years of age or older, be treated for asthma, allergies and/or eczema/atopic dermatitis in the last 12 months, and usually see an allergist for asthma, allergies, or eczema.
Survey characteristics
The allergist survey contained 25 questions (eTable 1) and the patient survey contained 22 questions (eTable 2) to determine the extent to which SDM tools were being used, understand which tools were being used and which were used most, and determine reasons, benefits, or barriers to using SDM tools.
Within the surveys, a definition of SDM was given to the participants. In the allergist survey, the definition was given after the questions assessing SDM awareness and usage and was therefore self-assessed based on their own perceived definition of SDM. The definition was then provided before the remaining section that assessed benefits and barriers to SDM. In contrast, the SDM definition in the patient survey was given before any questions were asked regarding SDM. The provided definition of SDM was as follows:
“Shared decision-making occurs when a healthcare provider and a patient work together to make a healthcare decision that is best for the patient. The optimal decision takes into account evidence-based information about available options, the provider's knowledge and experience, and the patient's values and preferences. Both healthcare professionals and patients benefit from using shared decision-making.
- Benefits to Physicians and Allergists:
-
•Improved quality of care delivered
-
•Increased patient satisfaction
-
•
- Benefits to Patients:
-
•Improved patient care experience
-
•Improved patient adherence to treatment recommendations
-
•Builds a trusting and lasting relationship between health care professionals and patients”
-
•
Analysis
The participation goal was to reach 100 completions for each survey. Analyses of the survey results were descriptive only. Categorical questions are reported as percentages of the survey participants.
Results
Participant characteristics
A total of 101 participants completed the allergist survey; the majority (60%) were ages 35–54 years, 71% were men, 44% were in practice for over 20 years, and 81% were in community-based/private practice (eTable 3). Nearly all participants (>90%) were members of the American Academy of Allergy, Asthma & Immunology (AAAAI) and the ACAAI (eTable 3).
A total of 110 participants completed the patient survey; 63% were women, 61% were ages 25–55 years, 64% identified as White, 23% identified as Black, and 19% identified as Hispanic (eTable 4). Nearly all participants (96%) reported being treated for allergies in the last 12 months, followed by asthma (34%), eczema (16%), and COVID-19 (16%). All participants reported that they usually see an allergist for their asthma, allergies, and/or eczema.
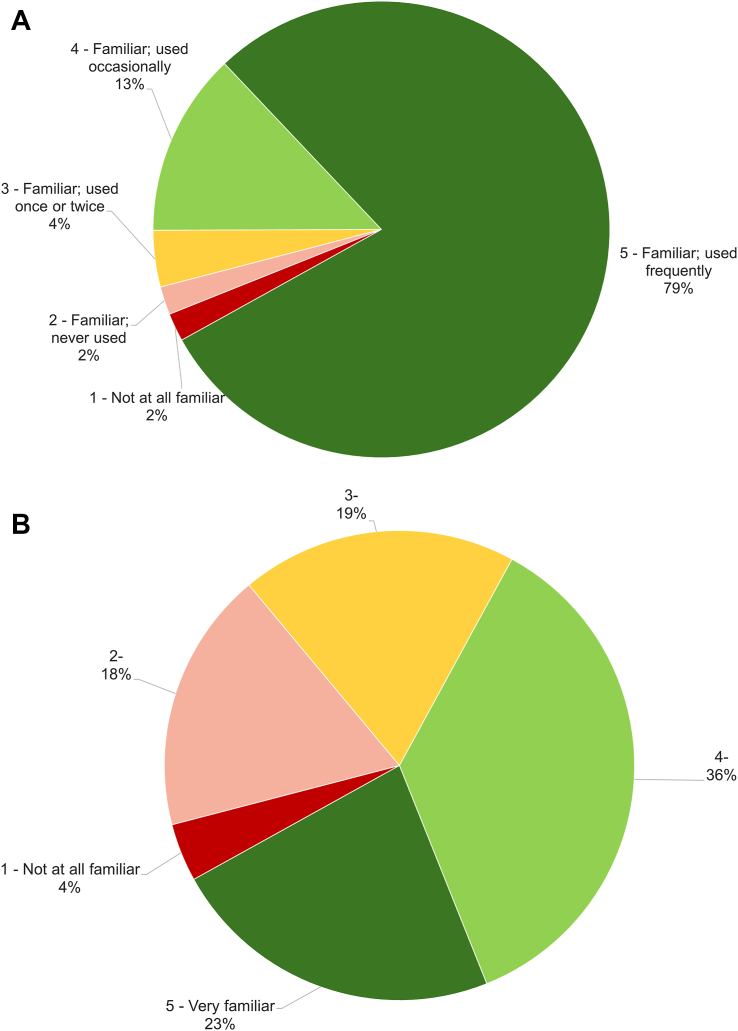
Reported use of SDM among allergists
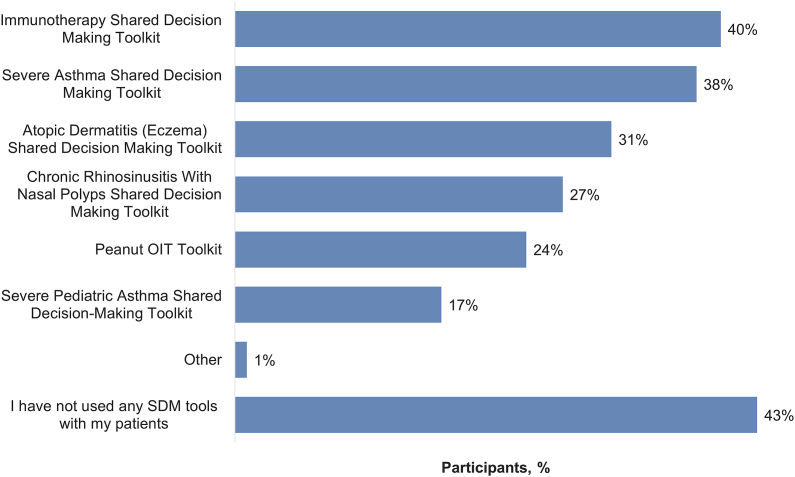
Nearly all (98%, n = 99) of the surveyed allergists reported being familiar with the concept of SDM based on their own definition, and 79% reported using it frequently (Fig. 1A). The surveyed allergists who reported using SDM (n = 97) indicated that they used it with an average of 44% of their patients with asthma, allergy, and eczema in the past 12 months. Allergists were somewhat less familiar with SDM tools (Fig. 1B). Among those who were familiar with SDM tools (n = 95), the most commonly used tool was the Immunotherapy SDM toolkit (40%); 43% had not used any SDM tools with their patients (Fig. 2).
Fig. 1.
Percentage of surveyed allergists (N = 101) reporting familiarity of A) concept of SDM based on their own definition and B) SDM tools. Familiarity with SDM tools was assessed on a scale of 1 (not at all familiar) to 5 (very familiar). SDM, shared decision-making
Fig. 2.
Percentage of surveyed allergists reporting using SDM tools specific for allergy and asthma practice in the past 12 months that are available on the American College of Allergy, Asthma & Immunology website. Data are from the subset of allergists who indicated they were familiar with SDM tools (n = 95). OIT, oral immunotherapy; SDM, shared decision-making
Benefits and barriers of SDM identified by allergists
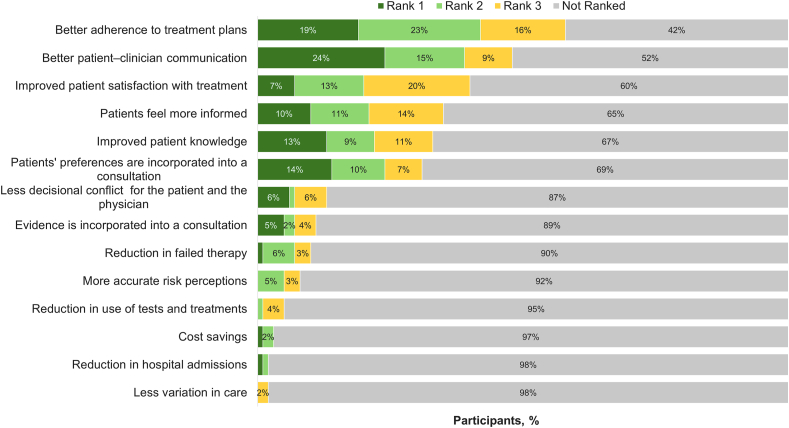
The top benefits of SDM as ranked by surveyed allergists are shown in Fig. 3.
Fig. 3.
Ranking of SDM benefits by surveyed allergists (N = 101). Participants selected their top 3 benefits. Rank 1 indicates most important. SDM, shared decision-making
Among allergists who reported not using SDM or using it infrequently (n = 19), 42% considered it too time-consuming, 37% believed their patients have low health literacy, 32% needed more information on SDM, and 32% believed their patients prefer the allergist make recommendations (Table 1).
Table 1.
Percentage of surveyed allergists reporting specific reasons for not using SDM or using it infrequently.
| Reason | Survey Participants n = 19a |
|---|---|
| SDM is too time-consuming | 42% |
| My patients have low health literacy and lack the knowledge, skills and confidence to communicate, navigate the health system and engage in SDM | 37% |
| I'm not very familiar with SDM; I need more information | 32% |
| My patients prefer that I make recommendations to them | 32% |
| The SDM tools are difficult to use | 26% |
| My patients have not asked to be more involved | 26% |
| My patients' conditions are complex; patients would not understand treatments well enough to make decisions on their own | 26% |
| I have limited or no access to up-to-date, high-quality evidence | 16% |
| My patients' conditions are simple; there is no need for SDM | 16% |
| I just don't like SDM; I prefer to use other methods | 5% |
| My colleagues have advised me against using SDM | 5% |
| Using SDM would raise my patients' anxiety levels | 0 |
| Other reasons (Please specify) | 0 |
| No particular reason | 5% |
SDM, shared decision-making.
Data are from the subset of allergists who are not using SDM or using it infrequently
Perceptions of SDM identified by allergists
Overall, 59% of allergists said they were “very likely” or “likely” to recommend the ACAAI SDM tools to colleagues. Although 99% of the allergists who reported using SDM believe their patients had a positive experience when SDM was used, responses from the open-ended comment section indicate that allergists believe SDM is a great tool, but it is not appropriate for all their patients. The allergists expressed beliefs that patients don't care or forget what is being explained, or that it takes too much time to educate a patient, or that the patient just wants the allergist to make the decision.
Reported use of SDM among patients
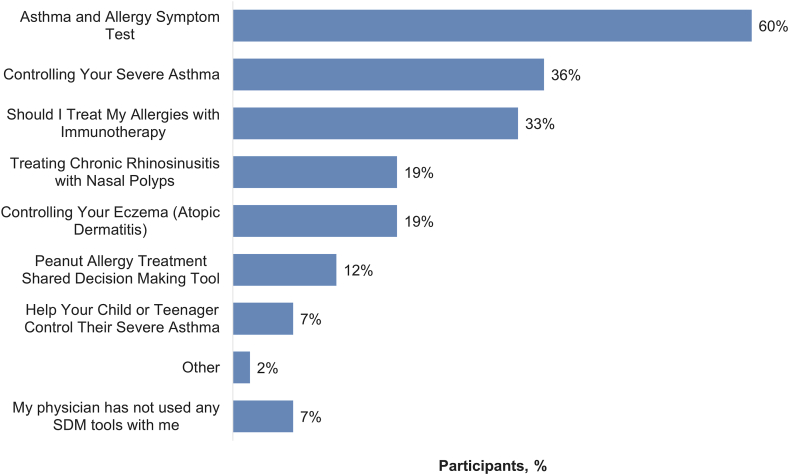
Of the 110 patient survey participants, 60% of patients reported as least some familiarity with the concept of SDM, and 25% reported using SDM “frequently” or “occasionally” when being treated for allergies, asthma, or eczema. Only 22% reported ever using SDM tools at some point with their healthcare professional. The highest reported use of SDM tools was by patients ages 18–39 years (32%) and those with high school or less education (32%) (eTable 5). The most commonly reported SDM tool used in the past 12 months was the Asthma and Allergy Symptom Test (60%; Fig. 4).
Fig. 4.
Percentage of surveyed patients reporting using SDM tools specific for allergy and asthma practice in the past 12 months that are available on the American College of Allergy, Asthma & Immunology website. Data are from the subset of patients whose allergist had used SDM (n = 42). SDM, shared decision-making
Of the patients unfamiliar with SDM (n = 44), 68% reported they would be interested in learning more about SDM. Interest in learning more about SDM was expressed by a high percentage of Black (89%) patients and those with at least a Bachelor's degree (85%).
Benefits and barriers of SDM identified by patients
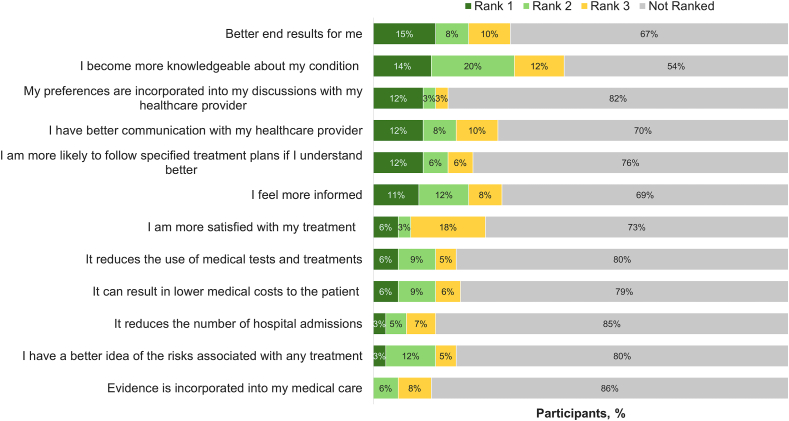
The benefits of SDM as ranked by patients are shown in Fig. 5.
Fig. 5.
Ranking of SDM benefits by surveyed patients. Participants selected their top 3 benefits. Rank 1 indicates most important. Data are from the subset of patients who indicated they were familiar with SDM (n = 66). SDM, shared decision-making
Of the patients who indicated they were unfamiliar with SDM (n = 44), 55% reported they would be likely to ask their allergist about SDM, and of patients whose allergists use SDM infrequently or never (n = 56), 70% reported they would be likely to ask their allergist to use it more often. Of those who indicated they were unlikely to ask their allergist to use SDM or to use it more frequently (n = 11), the most common reported reasons were “I don't know enough about SDM; I need more information”, “I would prefer that my allergist make recommendations to me; I don't need/want to have input”, and “My condition is simple to treat and SDM is not necessary” (Table 2).
Table 2.
Percentage of surveyed patients reporting specific reasons for not asking allergist to use SDM or use it more frequently.
| Reason | Survey Participants n = 11a |
|---|---|
| I don't know enough about SDM; I need more information | 27% |
| I would prefer that my allergist make recommendations to me; I don't need/want to have input | 27% |
| My condition is simple to treat and SDM is not necessary | 27% |
| I am not interested in being more involved in deciding about treatment options | 18% |
| I think my allergist would feel insulted and think I doubt his/her medical competence | 18% |
| I have heard about other people having bad experiences using SDM with their allergist | 0 |
| I would expect that SDM tools would be difficult to use | 0 |
| I would expect that SDM is too time-consuming | 0 |
| My condition is complex; I would not understand the treatment options well enough to make decisions for myself | 0 |
| Other reasons | 9% |
| No particular reason | 18% |
SDM, shared decision-making.
Data are from the subset of patients who are unlikely to ask their allergist about SDM or ask their allergist to use SDM more frequently
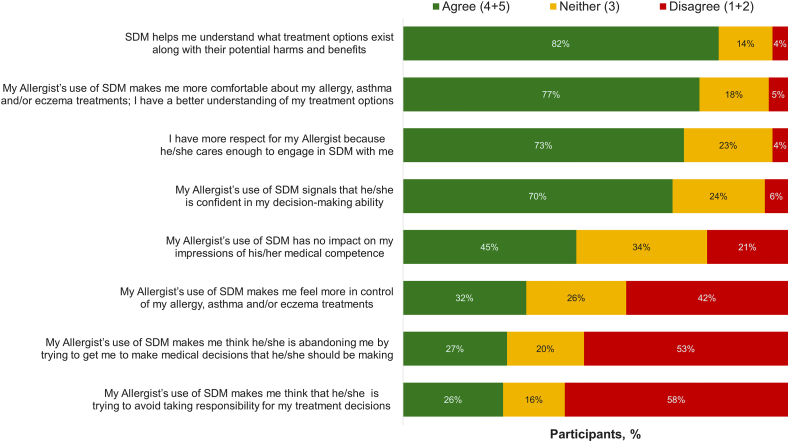
Perceptions of SDM identified by patients
Most (82%) patients agree that SDM helps them to understand what treatment options exist along with their potential harms and benefits (Fig. 6). Responses from the open-ended comment section indicate that patients are overwhelmingly positive about the concept of SDM because it makes them feel more in control of their treatment. Many claim they have been involved in SDM previously but did not know the formal name. Some patients indicated hesitation about SDM because they don't want to make stressful medical decisions or because they believe there's only one treatment option.
Fig. 6.
Percentage of surveyed patients (N = 110) reporting agreement with statements about allergists' use of SDM. SDM, shared decision-making
Discussion
Responses to the surveys indicate that allergists believe they are engaging in SDM based on their perception of what SDM entails, yet their reported use of SDM tools and patient reporting of the frequency of SDM use suggest there is room for improvement. When questioned about their familiarity and use of SDM (before a definition of SDM was stated in the survey), nearly all of the surveyed allergists claimed to be familiar with SDM, and 79% reported using it frequently. However, surveyed allergists also reported using SDM with less than half of their patients, approximately 20% used SDM infrequently or not at all, and more than 40% of those who claimed familiarity with SDM tools were not using them. In comparison, only about one-quarter of surveyed patients reported using SDM or SDM tools when being treated for their allergies, asthma, or eczema. Perceptions of SDM assessed in the surveys revealed that allergists and patients recognize SDM increases the patient's knowledge of their disease and improves physician/patient communication. Patients indicated they wanted their allergists to use SDM or use it more, yet barriers remain on both sides.
The discordance between reported use of SDM by the surveyed allergists and patients indicates that there is a disconnect in the perceived use of SDM. The surveyed allergists believe that they are practicing SDM, but they may not be practicing patient-recognized SDM. Discordance between clinician- and patient-perceived SDM is not uncommon.20,21 Interestingly, several studies that used validated measures to compare patient or caregiver-perceived SDM versus independent observer-perceived SDM for the same consultation visit, found that patient- and observer-measured levels of SDM also generally do not correlate with each other.22, 23, 24, 25 Together, these data indicate that physicians and patients can have quite different perceptions of a consultation, which often do not correlate with objective measures of SDM that have been evaluated by an independent observer. This suggests that the perceptions of the SDM participants may be influenced by previous consultation experiences and the subjective opinion of their physician/patient relationship.
There were some common perceived barriers to SDM expressed by both allergists and patients, the most striking of which was the belief that the patient prefers the allergist to make the decisions without patient input. Surveyed allergists reported that they do not use SDM because their patients have low health literacy and are not able to understand their complex disease. These expressed beliefs reiterate that some allergists and patients assume that SDM is not necessary because the patient is incapable or does not want to be involved with their healthcare decisions, and the patient should simply accept that their physician knows best without question. Such beliefs are well-known barriers to SDM, in general.2,26, 27, 28 This perception stems from a misunderstanding of SDM. SDM is not intended as a conversation about mechanism of action of different treatments or disease pathogenesis on par to a conversation between medical colleagues, or simply educating the patient about treatment pros and cons. SDM is about obtaining the patient's point of view. The patient alone knows their own preferences and perceptions, and SDM is meant to draw out those preferences and perceptions that will affect the patient's disease management.26 Not all patients will want to participate in SDM when they are approached with the concept,29 but finding out the patient's willingness to participate is in itself part of SDM. Such patient passivity is a barrier that may be overcome by the use of SDM tools since they are specifically designed to engage patient participation.30 Indeed, a pooled analysis of 16 studies found that use of SDM tools significantly alleviated patient passiveness toward involvement in decision-making.31 Since 2016, there have been a number of SDM tools developed for allergic diseases.12, 13, 14, 15, 16, 17, 18, 19 The survey results indicate that these allergy-specific SDM tools are currently underutilized and corroborate findings from a healthcare provider survey conducted in 2019 which found that 67% of allergists had not ever used any of the available allergy immunotherapy SDM aids.32 The reason given was mainly lack of awareness, although 18% of allergists reported they simply did not need it.32
The top barrier identified by surveyed allergists who were not using SDM or using it infrequently was that SDM is too time-consuming. In the United States, where healthcare is typically fee-for-service, this is an understandable concern, and it is another well-recognized barrier to SDM.27,28 A review of 10 studies found that use of SDM tools only increased a typical consultation visit by 7.5% (2.6 min).31 Face-to-face SDM time with the allergist may be alleviated by involving staff and distributing SDM tools to the patient before or after the clinic visit.19,26
A limitation of the surveys is that part of the allergist survey participants and all of the patient participants were recruited through the market research firm, Dynata and may not be generalizable to the general population with asthma and allergy. The small sample sizes also limit the generalizability of the results. In contrast, the strength of the Dynata patient panel is that it is required to be representative of the general US population in regard to demographics. Another limitation is that the allergists surveyed were not those who were treating the patient survey participants. Thus, the perceived disconnect between allergist and patient perceptions of SDM are on a general level and may differ among individual allergist and patient relationships.
Survey responses revealed a disconnect between allergists and their patients regarding SDM use, as well as barriers to SDM that are consistent across the healthcare industry in general. Thus, more extensive training of allergists, as well as staff, is needed regarding what SDM is and how to engage patients across socioeconomic and education backgrounds. To further this training initiative, the ACAAI, AAAAI, and Allergy & Asthma Network have SDM resources for the patient and allergist on their websites.12,33,34 Participants of the patient survey clearly expressed their desire for SDM to be better educated about their disease and treatment and feel more in control of their care. Successful SDM is a win-win for patients and allergists since disease outcomes may be improved, and patients will be pleased and satisfied with their disease management.
Abbreviations
AAAAI, American Academy of Allergy, Asthma & Immunology; ACAAI, American College of Allergy, Asthma & Immunology; SDM, shared decision-making.
Acknowledgements
Medical writing and editorial assistance were provided by Erin P. Scott, PhD, of Scott Medical Communications, LLC. This assistance was funded by the Allergy & Asthma Network.
Funding source
Funding for the surveys was provided by the Allergy & Asthma Network.
Role of the funding source
Allergy & Asthma Network contributed to the drafting of the survey, interpretation of the results, writing and reviewing of the manuscript, and the decision to submit the article for publication.
Availability of data
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Author contributions
J. Eghrari-Sabet contributed to the drafting of the survey, interpretation of the results, writing and reviewing of the manuscript, and the decision to submit the article for publication. D. Williams contributed to interpretation of the results, writing and reviewing of the manuscript, and the decision to submit the article for publication. D. A. Bukstein contributed to interpretation of the results, writing and reviewing of the manuscript, and the decision to submit the article for publication. T. Winders contributed to the drafting of the survey, interpretation of the results, writing and reviewing of the manuscript, and the decision to submit the article for publication. D. D. Gardner contributed to the drafting of the survey, interpretation of the results, writing and reviewing of the manuscript, and the decision to submit the article for publication.
Competing of interest
J. Eghrari-Sabet has nothing to disclose D. Williams serves on the board of directors for Allergy & Asthma Network. D.A. Bukstein has served as a consultant for AstraZeneca, Regeneron, and TEVA. T. Winders has nothing to disclose. D.D. Gardner has nothing to disclose.
Ethics statement
The surveys were reviewed by an institutional review board (Advarra, Columbia, MD) given exemption status. Survey data was linked to the research panel database using numeric identifiers so the identity of the panelist was always protected.
Authors’ consent for publication
All authors agreed to submit the manuscript for publication.
Confirmation of unpublished work
The manuscript is original, has not been published before, is not currently being considered for publication elsewhere, and has not been posted to a preprint server.
Footnotes
Full list of author information is available at the end of the article
Supplementary data to this article can be found online at https://doi.org/10.1016/j.waojou.2023.100828.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Blaiss M.S., Steven G.C., Bender B., Bukstein D.A., Meltzer E.O., Winders T. Shared decision making for the allergist. Ann Allergy Asthma Immunol. 2019;122:463–470. doi: 10.1016/j.anai.2018.08.019. [DOI] [PubMed] [Google Scholar]
- 2.Joseph-Williams N., Elwyn G., Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Counsel. 2014;94:291–309. doi: 10.1016/j.pec.2013.10.031. [DOI] [PubMed] [Google Scholar]
- 3.George M., Arcia A., Chung A., Coleman D., Bruzzese J.M. African Americans want a focus on shared decision-making in asthma adherence interventions. Patient. 2020;13:71–81. doi: 10.1007/s40271-019-00382-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ma Q., Luo G., Zhou X., et al. Self-reported reasons for treatment non-adherence in Chinese asthma patients: a 24-week prospective telephone follow-up study. Clin Res J. 2016;12:262–268. doi: 10.1111/crj.12525. [DOI] [PubMed] [Google Scholar]
- 5.Losi S., Berra C.C.F., Fornengo R., Pitocco D., Biricolti G., Federici M.O. The role of patient preferences in adherence to treatment in chronic disease: a narrative review. Drug Target Insights. 2021;15:13–20. doi: 10.33393/dti.2021.2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vähätalo I., Ilmarinen P., Tuomisto L.E., et al. 12-year adherence to inhaled corticosteroids in adult-onset asthma. ERJ Open Res. 2020:6. doi: 10.1183/23120541.00324-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilson S.R., Strub P., Buist A.S., et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010;181:566–577. doi: 10.1164/rccm.200906-0907OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fiks A.G., Mayne S.L., Karavite D.J., et al. Parent-reported outcomes of a shared decision-making portal in asthma: a practice-based RCT. Pediatrics. 2015;135:e965–e973. doi: 10.1542/peds.2014-3167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu T.L., Taylor Y.J., Mahabaleshwarkar R., Blanchette C.M., Tapp H., Dulin M.F. Shared decision making and time to exacerbation in children with asthma. J Asthma. 2018;55:675–683. doi: 10.1080/02770903.2017.1378357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tapp H., Shade L., Mahabaleshwarkar R., Taylor Y.J., Ludden T., Dulin M.F. Results from a pragmatic prospective cohort study: shared decision making improves outcomes for children with asthma. J Asthma. 2017;54:392–402. doi: 10.1080/02770903.2016.1227333. [DOI] [PubMed] [Google Scholar]
- 11.Steven G.C. Shared decision making in allergic rhinitis: an approach to the patient. Ann Allergy Asthma Immunol. 2020;125:268–272. doi: 10.1016/j.anai.2020.06.032. [DOI] [PubMed] [Google Scholar]
- 12.Practice management center. American College of Allergy, Asthma, & Immunology. Available at: https://college.acaai.org/practice-management/?toolkit_categories=clinical-tools. Accessed August 23, 2022.
- 13.Leonard SE, Wysocki T, Clay CF, Fuzzell L, Shirley ED. Environmental allergies: should my child get allergy shots? Nemours' Center for Healthcare Delivery Science. Available at: https://www.nemours.org/content/dam/nemours/wwwv2/filebox/research/Environmental%20Allergies%20Decision%20Aid.pdf. Accessed August 23, 2022.
- 14.What is the best treatment option for my severe asthma? CHEST, ACAAI, Allergy & Asthma Network. Available at: http://severeasthmatreatments.chestnet.org/. Accessed August 23, 2022.
- 15.Gagne M.E., Legare F., Moisan J., Boulet L.P. Development of a patient decision aid on inhaled corticosteroids use for adults with asthma. J Asthma. 2016;53:964–974. doi: 10.3109/02770903.2016.1166384. [DOI] [PubMed] [Google Scholar]
- 16.Urticaria shared decision making aid. Global Allergy & Airways Patient Platform. Available at: https://gaapp.org/urticaria-shared-decision-making/. Accessed August 23, 2022.
- 17.Allergies: Should I take allergy shots? Healthwise, Inc. Available at: https://www.healthwise.net/ohridecisionaid/Content/StdDocument.aspx?DOCHWID=aa69795. Accessed August 23, 2022.
- 18.Allergies: Should I take shots for insect sting allergies? Healthwise, Inc. Available at: https://www.healthwise.net/ohridecisionaid/Content/StdDocument.aspx?DOCHWID=rt1299. Accessed August 23, 2022.
- 19.Greenhawt M., Shaker M., Winders T., et al. Development and acceptability of a shared decision-making tool for commercial peanut allergy therapies. Ann Allergy Asthma Immunol. 2020;125:90–96. doi: 10.1016/j.anai.2020.01.030. [DOI] [PubMed] [Google Scholar]
- 20.Keshtgar A., Cunningham S.J., Jones E., Ryan F.S. Patient, clinician and independent observer perspectives of shared decision making in adult orthodontics. J Orthod. 2021;48:417–425. doi: 10.1177/14653125211007504. [DOI] [PubMed] [Google Scholar]
- 21.Sapir T., Moreo K.F., Greene L.S., et al. Assessing patient and provider perceptions of factors associated with patient engagement in asthma care. Ann Am Thorac Soc. 2017;14:659–666. doi: 10.1513/AnnalsATS.201608-602OC. [DOI] [PubMed] [Google Scholar]
- 22.Evong Y., Chorney J., Ungar G., Hong P. Perceptions and observations of shared decision making during pediatric otolaryngology surgical consultations. J Otolaryngol Head Neck Surg. 2019;48:28. doi: 10.1186/s40463-019-0351-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geessink N.H., Ofstad E.H., Olde Rikkert M.G.M., van Goor H., Kasper J., Schoon Y. Shared decision-making in older patients with colorectal or pancreatic cancer: determinants of patients' and observers' perceptions. Patient Educ Counsel. 2018;101:1767–1774. doi: 10.1016/j.pec.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 24.Kasper J., Heesen C., Köpke S., Fulcher G., Geiger F. Patients' and observers' perceptions of involvement differ. Validation study on inter-relating measures for shared decision making. PLoS One. 2011;6 doi: 10.1371/journal.pone.0026255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diendéré G., Farhat I., Witteman H., Ndjaboue R. Observer ratings of shared decision making do not match patient reports: an observational study in 5 family medicine practices. Med Decis Making. 2021;41:51–59. doi: 10.1177/0272989X20977885. [DOI] [PubMed] [Google Scholar]
- 26.Joseph-Williams N., Lloyd A., Edwards A., et al. Implementing shared decision making in the NHS: lessons from the MAGIC programme. Br Med J. 2017;357:j1744. doi: 10.1136/bmj.j1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zeuner R., Frosch D.L., Kuzemchak M.D., Politi M.C. Physicians' perceptions of shared decision-making behaviours: a qualitative study demonstrating the continued chasm between aspirations and clinical practice. Health Expect. 2015;18:2465–2476. doi: 10.1111/hex.12216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Légaré F., Thompson-Leduc P. Twelve myths about shared decision making. Patient Educ Counsel. 2014;96:281–286. doi: 10.1016/j.pec.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 29.Levinson W., Kao A., Kuby A., Thisted R.A. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20:531–535. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shaker M., Hsu Blatman K., Abrams E.M. Engaging patient partners in state-of-the-art allergy care: finding balance when discussing risk. Ann Allergy Asthma Immunol. 2020;125:252–261. doi: 10.1016/j.anai.2020.01.029. [DOI] [PubMed] [Google Scholar]
- 31.Stacey D., Legare F., Lewis K., et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:Cd001431. doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Winders T., DuBuske L., Bukstein D.A., Meltzer E.O., Wallace D., Rance K. Shifts in allergy practice in a COVID-19 world: implications of pre-COVID-19 national health care provider and patient surveys of treatments for nasal allergies. Allergy Asthma Proc. 2021;42:301–309. doi: 10.2500/aap.2021.42.210035. [DOI] [PubMed] [Google Scholar]
- 33.Allergy Office Practice. American Academy of Allergy Asthma & Immunology. Available at: https://education.aaaai.org/allergy-office-practice/AOP. Accessed August 23, 2022.
- 34.What is shared decision making for asthma and allergies? Allergy & Asthma Network. Available at: https://allergyasthmanetwork.org/health-a-z/shared-decision-making/. Accessed August 23, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.