Abstract
Acute occlusion of celiomesenteric trunk variants such as a replaced common hepatic artery origin from a superior mesenteric artery can be catastrophic and requires immediate attention to reverse simultaneous mesenteric and hepatic ischemia and prevent death. We report the case of a 73-year-old woman with acute occlusion of her celiomesenteric trunk and proximal superior mesenteric artery who underwent successful endovascular repair with stent graft via brachial access. In the present case report, we describe a surgically relevant classification system of celiomesenteric trunk variants, highlight the feasibility of endovascular intervention in this uncommon scenario, and describe our technique.
Keywords: Celiacomesenteric trunk, Celiomesenteric trunk, Mesenteric ischemia, Replaced common hepatic artery
A replaced common hepatic artery (RCHA) from the superior mesenteric artery (SMA) is one of the variants of the celiomesenteric trunk and is rare, occurring in 1.13% of 19,013 cases in the largest systematic review of the literature.1 Patients with an RCHA can require vascular intervention for acute and chronic ischemia,2, 3, 4, 5, 6, 7 aneurysms,8,9 dissection,10 and median arcuate ligament syndrome.8 Reports of patients with mesenteric ischemia in the setting of a celiomesenteric trunk variant have described excellent clinical results with thoughtful and timely open and endovascular intervention.4,5,9,11 Other reports have acknowledged that mesenteric ischemia in a patient with a celiomesenteric trunk presents diagnostic and therapeutic challenges but that delay in definitive treatment has lethal consequences.3,6,12 We report the case of a 73-year-old woman with acute occlusion of her celiomesenteric trunk who underwent successful endovascular repair. She was cachectic, with months of food fear and weight loss, and presented with severe acute abdominal pain. Computed tomography (CT) angiography of the abdomen and pelvis demonstrated occlusion of her celiomesenteric trunk and proximal SMA. We successfully treated her celiomesenteric trunk occlusion with a balloon expandable stent graft using a telescoping technique via left brachial access. Postoperatively, she had complete and immediate resolution of her abdominal pain. Her case demonstrates that, with proper planning, endovascular therapy can be highly effective. Ethics approval was not required because this is a retrospective case report. The patient provided written informed consent for the report of her case details and imaging studies.
Comparing her case with those previously reported was challenging owing to the wide variety of descriptors used for the variant common hepatic artery anatomy. The terms currently used in the literature include replaced common hepatic artery (or RCHA), celiomesenteric trunk, celiacomesenteric trunk, and quadrification, among others.3,6,7,9,11,13 The aberrant origin of some of these arteries is likely related to the persistence of vitelline arteries during embryologic development.14 Previous classification systems of these anomalies failed to provide the level of anatomic detail required by surgeons and interventionists planning revascularization.14,15 Modern CT-based classification systems have benefitted from larger sample sizes and have begun to categorize the variant anatomy in more detail.16
The recent classification system by Tang et al17 presents five types of celiomesenteric trunk variants, with subcategories determined by the length of the common trunk and left gastric artery origin. Their report and classification system provide a good framework and illustrations for understanding the variants and articulating the reason for selecting a particular vascular repair. Five types were identified from their retrospective review of >5500 CT scans in which they evaluated variant patterns of the celiomesenteric trunk. The investigators defined the celiac trunk as an arterial trunk with at least two of the major branches of the normal celiac artery.17 A celiomesenteric trunk is defined as a single common trunk from the aorta and its branches, including the SMA and at least two major celiac branches. The five celiomesenteric trunk types are listed in the Table.17 Our patient had acute occlusion of a type IV celiomesenteric trunk. Because it was long type, the lesion was amenable to endovascular repair with a single stent graft. Prior studies reported treatment of a short celiomesenteric trunk type using kissing stents.11 The report of future interventions in terms of these celiomesenteric trunk types could be helpful.
Table I.
Types of celiomesenteric trunk
| Variable | Description |
|---|---|
| Type | |
| I | Hepatosplenic gastric mesenteric trunk |
| II | Hepatosplenic mesenteric trunk with separate left gastric artery origin from aorta |
| III | Gastrosplenic mesenteric trunk with common hepatic artery origin from aorta |
| IV | Hepatogastric splenic mesenteric trunk with splenic artery origin from aorta |
| V | Other |
| Celiomesenteric trunk length | Subtype according to gastric artery origin |
| Short | |
| Celiac trunk | |
| Long | |
| Abdominal aorta | |
| Single common trunk | |
| Other artery |
Data from Tang et al.17
Case report
A 73-year-old, frail-appearing woman was transferred to our institution for evaluation and treatment of severe abdominal pain, nausea, weight loss, and nonbloody diarrhea. She was a smoker and had chronic obstructive pulmonary disease, coronary artery disease, hypertension, hyperlipidemia, renal artery stenosis, and peripheral artery disease. Her body mass index was 13.7 kg/m2. She had a surgical history of laparoscopic cholecystectomy and right common iliac and left external iliac artery stent placement. She reported that the abdominal pain and food phobia had been getting worse, resulting in a 16-kg weight loss in the previous 5 months. On the day of presentation, her pain had become intractable and severe. On examination, she was afebrile, normotensive, and not tachycardic. She had pain out of proportion to the examination and no peritoneal signs. She had no leukocytosis. Her renal and liver function was normal, and she had no metabolic acidosis. Her albumin was low at 2.1 g/dL. A previous transfemoral mesenteric angiogram showed bilateral renal artery stenosis, SMA occlusion with reconstitution via the arc of Riolan, stenosis of the inferior mesenteric artery origin, a right common iliac artery stent, and a left external iliac artery stent (Fig 1). She underwent CT angiography of the abdomen and pelvis, which demonstrated occlusion of a type IV celiomesenteric trunk and proximal SMA with reconstitution of mid-distal SMA via the arc of Riolan (Fig 2). She received antiplatelet therapy, statin therapy, and systemic heparinization. Her symptoms, examination findings, and radiographic findings were consistent with acute mesenteric ischemia. She was a poor candidate for open revascularization because of her malnutrition, chronic obstructive pulmonary disease, coronary artery disease, and extensive severe aortoiliac disease. Thus, endovascular revascularization was selected. She underwent emergent open left brachial access, abdominal aortography, and celiomesenteric trunk stenting in a hybrid operating room.
Fig 1.
Abdominal aortogram demonstrating occlusion of celiomesenteric trunk and proximal superior mesenteric artery (SMA) with reconstitution of the mid- and distal SMA via the arc of Riolan from the stenotic inferior mesenteric artery. An incidental finding of bilateral renal artery stenosis can be seen. Note that the splenic artery is not seen owing to the aberrant origin directly from aorta, which was above the level of the flush catheter.
Fig 2.

Sagittal computed tomography (CT) angiogram demonstrating occlusion of celiomesenteric trunk with filling of the distal superior mesenteric artery (SMA).
She was transferred to the hybrid room table, placed in the supine position with the left arm outstretched. She was given 1 g of cefazolin (Ancef; SmithKline Beecham). After induction of monitored anesthesia care with sedation, the left brachial artery was evaluated with ultrasound, and the proximal brachial artery was selected for access in anticipation of the need for a 7F sheath in a patient with small arteries. The skin and subcutaneous tissue were infiltrated with 1% lidocaine. She underwent open left brachial artery exposure. The patient was given 5000 U of heparin, and the activated clotting time was monitored throughout the operation to maintain therapeutic anticoagulation. The left brachial artery was accessed with a micropuncture set, which was exchanged for a 5F, 11-cm sheath over a 0.035-in. stiff hydrophilic wire. The 0.035-in. stiff hydrophilic wire and flush catheter were advanced into the supraceliac aorta. A nonselective aortogram was performed. The sheath was exchanged for a 7F, 45-cm sheath, which was advanced into the supraceliac aorta. The celiomesenteric trunk was selected using the 0.035-in. stiff hydrophilic wire and multipurpose catheter. Selective arteriography confirmed successful selection of the celiomesenteric trunk and patency of the common hepatic artery and mid- to distal SMA (Fig 3). The wire was exchanged. The sheath and dilator were advanced into the celiomesenteric trunk origin. Percutaneous transluminal angioplasty of the occluded celiomesenteric trunk and proximal SMA was performed with a 4-mm × 60-mm balloon catheter (Fig 4). The severe residual stenosis of the celiomesenteric trunk was then treated with a balloon expandable stent graft measuring 6 mm × 39 mm (Fig 5). The completion arteriogram demonstrated no significant residual stenosis of the celiomesenteric trunk or SMA with excellent flow to the RCHA. All wires, catheters, and sheaths were removed. The brachial artery was closed transversely with interrupted 6-0 nonabsorbable monofilament sutures. Once flow was restored in the brachial artery, the patient had a strong palpable left radial artery pulse. The incision was closed in layers, and a compression wrap was applied. The patient tolerated the procedure well and was transferred to the postanesthesia care unit (PACU) in stable condition. In the PACU, she received 81 mg of aspirin and a 300-mg loading dose of clopidogrel. She reported immediate resolution of her abdominal pain and nausea in the PACU and was transferred to the intensive care unit for close hemodynamic monitoring in anticipation of fluid shifts. On the first postoperative day, she was pain free and tolerating a regular diet. Her electrolytes were carefully monitored to evaluate for the presence of refeeding syndrome. Her leukocytosis had resolved by postoperative day 2. Psyllium and probiotics were initiated, and patient was provided with protein and calorie goals. She was discharged to home with dual antiplatelet therapy after an uncomplicated recovery.
Fig 3.
Occlusion of celiomesenteric trunk.
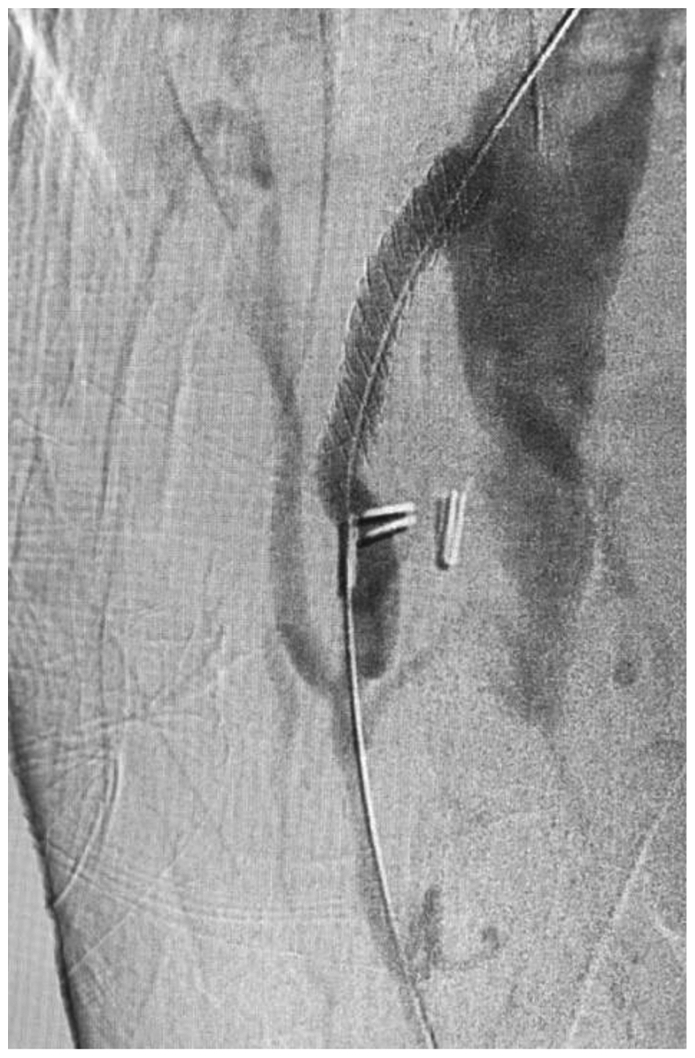
Fig 4.
Predilation of celiomesenteric trunk.
Fig 5.
Completion arteriogram demonstrating widely patent celiomesenteric trunk stent graft, common hepatic artery, and superior mesenteric artery (SMA).
Discussion
This case report highlights the occurrence of acute mesenteric ischemia due to celiomesenteric trunk occlusion in a frail patient with significant comorbidities. Clinically, she was a poor candidate for any open revascularization. Careful examination of the CT angiogram revealed that her lesion and anatomy were amenable to endovascular repair. A few technical points from our experience include that left brachial artery access afforded us an advantageous angle of approach. Also, because of the small size of her brachial arteries and the sheath size required, we opted for open exposure for access and closure. We used a telescoping technique to establish a secure working platform to allow for lesion navigation and treatment. Another option for access would have been common femoral artery access with the use of a steerable sheath. We pretreated the area of stenosis with slow gentle angioplasty using graded balloons to reduce the risk of dissection. This maneuver also allowed us to clearly define the origin of the common hepatic artery before stenting. We selected a covered balloon expandable stent to reduce the risk of distal embolization of periprocedural atheroemboli and long-term restenosis. Variations of our technique could have included the use of a filter wire and consideration of the use of a buddy wire to protect both the common hepatic and the SMA origins. Our patient received dual antiplatelet therapy. She also received close hemodynamic, urine output, and electrolyte monitoring in anticipation of visceral third spacing of fluid after revascularization. She had immediate resolution of her symptoms and recovered uneventfully.
Conclusions
Endovascular treatment of patients with mesenteric ischemia involving celiomesenteric trunk occlusive disease is an opportunity to provide a life-saving intervention that is immediately rewarding to both patient and surgeon. Early recognition of the specific anatomic variant and the need for urgent intervention is key. Our case presentation illustrates the clinical indicators that justify immediate intervention and the technical points of successful revascularization. We recommend the use of the term “celiomesenteric trunk” to describe this anatomic variant and its subtypes. We propose wide adoption of the CT-based classification system proposed by Tang et al17 to allow future case reports to produce a cohesive body of literature to inform decision making and guide optimal therapy.
Disclosure
None.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Suzuki T., Nakayasu A., Kawabe K., Takeda H., Honjo I. Surgical significance of anatomic variations of the hepatic artery. Am J Surg. 1971;122:505–512. doi: 10.1016/0002-9610(71)90476-4. [DOI] [PubMed] [Google Scholar]
- 2.Tasleem S.H., Younas F., Syed F.A., Mohuiddin I.T. Endovascular repair of common celiomesenteric trunk stenosis. VASA Z Gefasskrankheiten. 2010;39:341–343. doi: 10.1024/0301-1526/a000059. [DOI] [PubMed] [Google Scholar]
- 3.Fuentes G., Molina G.A., Jiménez M.A., et al. Intestinal ischemia in a patient with vascular malformation: a recipe for disaster. J Surg Case Rep. 2022;2022:rjac376. doi: 10.1093/jscr/rjac376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ratra A., Campbell S. Recurrent mesenteric ischemia from celiomesenteric trunk stenosis. Cureus. 2018;10 doi: 10.7759/cureus.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ayers N.P., Zacharias S.J., Abu-Fadel M.S., Hennebry T.A. Successful use of blunt microdissection catheter in a chronic total occlusion of a celiomesenteric artery. Catheter Cardiovasc Interv. 2007;69:546–549. doi: 10.1002/ccd.20954. [DOI] [PubMed] [Google Scholar]
- 6.Kueht M.L., Wu D.L., Mills J.L., Gilani R. Symptomatic celiomesenteric trunk: Variable presentations and outcomes in 2 patients. Tex Heart Inst J. 2018;45:35–38. doi: 10.14503/THIJ-16-6155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agarwal A.K., Youssef M.K., Doyle G.J., Wood C.P. Coeliomesenteric trunk stenosis--a rare variation causing mesenteric ischaemia. Eur J Vasc Endovasc Surg. 2000;20:405–406. doi: 10.1053/ejvs.2000.1202. [DOI] [PubMed] [Google Scholar]
- 8.Kalra M., Panneton J.M., Hofer J.M., Andrews J.C. Aneurysm and stenosis of the celiomesenteric trunk: a rare anomaly. J Vasc Surg. 2003;37:679–682. doi: 10.1067/mva.2003.37. [DOI] [PubMed] [Google Scholar]
- 9.Ailawadi G., Cowles R.A., Stanley J.C., et al. Common celiacomesenteric trunk: aneurysmal and occlusive disease. J Vasc Surg. 2004;40:1040–1043. doi: 10.1016/j.jvs.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 10.Boukoucha M., Yahmadi A., Znaidi H., Ben Khelifa R., Daghfous A. Spontaneous celiacomesenteric trunk dissection: case report. Int J Surg Case Rep. 2020;71:128–131. doi: 10.1016/j.ijscr.2020.04.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Date Y., Katoh H., Abe T., Nagamine H., Hara H., Kawase Y. Effective kissing stent to severe stenosis of the superior mesenteric artery replacing the common hepatic artery. CVIR Endovasc. 2018;1:18. doi: 10.1186/s42155-018-0025-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lovisetto F., Finocchiaro De Lorenzi G., Stancampiano P., et al. Thrombosis of celiacomesenteric trunk: report of a case. World J Gastroenterol. 2012;18:3917–3920. doi: 10.3748/wjg.v18.i29.3917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fakoya A.O.J., Aguinaldo E., Velasco-Nieves N.M., et al. A Unique communicating arterial branch between the celiac trunk and the superior mesenteric artery: a case report. Open Access Maced J Med Sci. 2019;7:2138–2141. doi: 10.3889/oamjms.2019.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hiatt J.R., Gabbay J., Busuttil R.W. Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg. 1994;220:50–52. doi: 10.1097/00000658-199407000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Michels N.A. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg. 1966;112:337–347. doi: 10.1016/0002-9610(66)90201-7. [DOI] [PubMed] [Google Scholar]
- 16.Bolintineanu Ghenciu L.A., Bolintineanu S.L., Iacob N., Zăhoi D.E. Clinical consideration of anatomical variations in the common hepatic arteries: an analysis using MDCT angiography. Diagn Basel Switz. 2023;13:1636. doi: 10.3390/diagnostics13091636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tang W., Shi J., Kuang L.Q., Tang S.Y., Wang Y. Celiomesenteric trunk: New classification based on multidetector computed tomography angiographic findings and probable embryological mechanisms. World J Clin Cases. 2019;7:3980–3989. doi: 10.12998/wjcc.v7.i23.3980. [DOI] [PMC free article] [PubMed] [Google Scholar]