Abstract
Background:
Previous studies found consistent associations between pregestational diabetes and birth defects. Given the different biological mechanisms for type 1 (PGD1) and type 2 (PGD2) diabetes, we used National Birth Defects Prevention Study (NBDPS) data to estimate associations by diabetes type.
Methods:
The NBDPS was a study of major birth defects that included pregnancies with estimated delivery dates from October 1997 to December 2011. We compared self-reported PGD1 and PGD2 for 29,024 birth defect cases and 10,898 live-born controls. For case groups with ≥5 exposed cases, we estimated adjusted odds ratios (aORs) and 95% confidence intervals (CIs) for the association between specific defects and each diabetes type. We calculated crude ORs (cORs) and 95% CIs with Firth's penalized likelihood for case groups with 3–4 exposed cases.
Results:
Overall, 252 (0.9%) cases and 24 (0.2%) control mothers reported PGD1, and 357 (1.2%) cases and 34 (0.3%) control mothers reported PGD2. PGD1 was associated with 22/26 defects examined and PGD2 was associated with 29/39 defects examined. Adjusted ORs ranged from 1.6 to 70.4 for PGD1 and from 1.6 to 59.9 for PGD2. We observed the strongest aORs for sacral agenesis (PGD1: 70.4, 32.3–147; PGD2: 59.9, 25.4–135). For both PGD1 and PGD2, we observed elevated aORs in every body system we evaluated, including central nervous system, orofacial, eye, genitourinary, gastrointestinal, musculoskeletal, and cardiac defects.
Conclusions:
We observed positive associations between both PGD1 and PGD2 and birth defects across multiple body systems. Future studies should focus on the role of glycemic control in birth defect risk to inform prevention efforts.
Keywords: birth defect, case–control study, pregestational diabetes, type 1 diabetes, type 2 diabetes
1 ∣. INTRODUCTION
In the United States, the prevalence of pregestational diabetes has increased in recent decades. From 2000 to 2010, the age-standardized prevalence of pregestational diabetes among deliveries increased from 0.65 per 100 births to 0.89 per 100 births, a relative change of 37% (Bardenheier et al., 2015). This increase is concerning given that diabetes is a known teratogen (Mills, 2010). Increased risks for defects of the cardiovascular, central nervous, genitourinary, and musculoskeletal systems have been observed in pregnancies of women with pregestational diabetes in National Birth Defects Prevention Study (NBDPS) analyses which combined pregestational type 1 and type 2 diabetes, including a recent analysis which used the same years as the current analysis (Correa et al., 2008; Tinker et al., 2020). Findings from the NBDPS are supported by studies in other populations (Arendt et al., 2021; Mowla, Gissler, Räisänen, & Kancherla, 2020; Yang, Cummings, O'Connell, & Jangaard, 2006). However, these analyses either analyzed pregestational type 1 and type 2 diabetes as one group or did not evaluate specific birth defects. Less is known about whether pregestational type 1 and type 2 diabetes confer different risks for specific defects.
Type 1 and type 2 diabetes both involve blood glucose regulation but have different underlying biological mechanisms. Type 1 diabetes is an autoimmune disorder resulting in the destruction of the beta cells in the pancreas which produce insulin, while type 2 diabetes is a metabolic disorder resulting in lowered insulin production or insulin resistance. Additionally, there are differences in the characteristics associated with type 1 and type 2 diabetes. Type 1 diabetes is more commonly diagnosed at a younger age, comprising greater than 85% of all diabetes diagnosed in children (Maahs, West, Lawrence, & Mayer-Davis, 2010). Type 2 diabetes, more commonly diagnosed in adulthood, has become increasingly diagnosed in children, with the incidence of both types of diabetes increasing (Mayer-Davis et al., 2017).
Existing studies that have evaluated birth defects associated with pregestational type 1 and type 2 diabetes separately have inconsistent results. Some report higher rates of birth defects among pregestational type 1 diabetes than pregestational type 2 diabetes (Lapolla et al., 2008; Murphy et al., 20170029; Peticca, Keely, Walker, Yang, & Bottomley, 2009), others report higher rates among type 2 diabetics (Clausen et al., 2005), and still others report that the two types are similarly associated with birth defects (Gonzalez-Gonzalez et al., 2008; Macintosh et al., 2006). Those who have studied associations with more specific defects have found both pregestational type 1 and type 2 diabetes to be associated with several, but not necessarily the same, birth defects (Arendt et al., 2021; Jovanovič et al., 2015).
In this study, we separately evaluated the association of pregestational type 1 and type 2 diabetes with 52 specific birth defects using data from the NBDPS. Given the large size of NBDPS, we assessed associations between each type of pregestational diabetes and specific birth defects.
2 ∣. METHODS
The NBDPS was a population-based case–control study of major structural birth defects, which included pregnancies ending on or after October 1, 1997 and with an estimated date of delivery on or before December 31, 2011. Birth defects surveillance systems in Arkansas, California, Georgia, Iowa, Massachusetts, North Carolina, New Jersey, New York, Texas, and Utah ascertained pregnancies affected by one or more eligible defect (cases) that were liveborn, stillborn, or induced terminations. Control infants were liveborn infants without major structural birth defects randomly selected from hospital records or birth certificates in the same geographic area and time-period as the cases (Reefhuis et al., 2015). Trained interviewers conducted a computer-assisted telephone interview to collect information from mothers of case and control infants on demographics, pregnancy history, medical conditions, medication use, and other exposures before and during pregnancy. All participating centers obtained institutional review board approval for the study and women provided informed consent.
A clinical geneticist reviewed clinical information for each case to ensure study eligibility. A second reviewer classified each case as having isolated, multiple, or complex defects. A case had an isolated status if there was one or more major defects in the same organ system (Rasmussen et al., 2003). A case had a multiple status if two or more apparently unrelated defects were diagnosed in different organ systems. A case had a complex status if a pattern of embryologically related major defects was present (Rasmussen et al., 2003; Reefhuis et al., 2015). Excluded from the study were cases with a known chromosomal or single-gene abnormality. Cardiac birth defects cases were further classified by cardiac phenotype, complexity, and presence of noncardiac defects (Botto et al., 2007). Oral clefts, glaucoma, cataracts, ventricular septal defects, and pulmonary valve stenosis were not ascertained by all sites for all years; we excluded controls when analyzing these case groups for sites and years with incomplete data (Reefhuis et al., 2015). Cases classified as unspecified atrial septal defects (ASD) were likely ASD secundum type and were counted as such in the analysis (Botto et al., 2007). For hypospadias, we restricted to male controls.
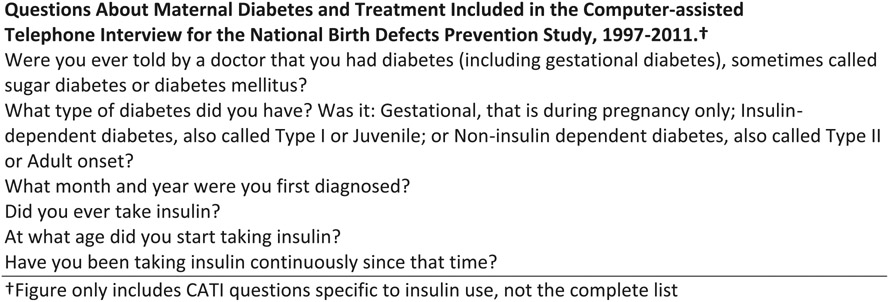
Mothers were asked whether they had ever been told by a doctor that they had diabetes. For those that reported diabetes, information on type, date of diagnosis, and medication use were collected (specific questions are shown in Figure 1). We defined pregestational type 1 diabetes and pregestational type 2 diabetes as a reported diagnosis prior to the estimated date of conception for the index pregnancy. We excluded any mothers who first reported a type 1 or type 2 diagnosis during the index pregnancy or during a previous pregnancy, as a diagnosis during pregnancy may suggest gestational diabetes. Mothers who reported pregestational type 1 diabetes but did not report using insulin continuously during pregnancy were excluded (74 cases; six controls), and women who reported an unknown diabetes type, or an unknown diagnosis date (407 cases; 102 controls). Women who reported gestational diabetes at any time were also excluded (2,512 cases; 823 controls). The reference group included mothers who did not report any type of diabetes (Figure 2).
FIGURE 1.
Questions about maternal diabetes and treatment included in the computer-assisted telephone interview for the National Birth Defects Prevention Study, 1997–2011
FIGURE 2.
Study population, exclusions, and pregestational type 1 and type 2 diabetes status among mothers in the National Birth Defects Prevention Study, 1997–2011
We analyzed associations between type 1 and type 2 diabetes and defects that had at least 50 cases. For defects with five or more exposed cases, we calculated adjusted odds ratios (aORs) and profile likelihood 95% confidence intervals (CIs) using unconditional logistic regression with Firth's penalized likelihood, while controlling for covariates identified a priori based on a review of the literature: maternal age at delivery (≤24, 25–29, ≥30 years), race/ethnicity (non-Hispanic White, other), education (high school or less, more than high school), pre-pregnancy body mass index (BMI) (kilograms/height in meters (Mills, 2010; <25, ≥25), and state of residence at birth (Firth, 1993; Karabon, 2020). Firth's penalized likelihood addresses issues of quasi-complete separation of data due to small sample size, reducing bias in the maximum likelihood estimation (Firth, 1993). For defects with three or four exposed cases, we calculated crude odds ratios (cORs) and exact 95% CIs. We did not calculate OR estimates for defects with fewer than three exposed cases. Our primary analysis included isolated and multiple birth defects together. Because isolated birth defects may differ etiologically from those associated with other major birth defects, we also calculated estimates for each birth defect among the subset of isolated cases (Rasmussen et al., 2003).
We conducted a sensitivity analysis to explore potential misclassification of diabetes type. Type 1 diabetes is more commonly diagnosed at a younger age, comprising greater than 85% of all diabetes diagnosed in children (Maahs et al., 2010). Given this, we restricted the sensitivity analysis to mothers who reported an age of diagnosis of type 1 diabetes at 20 years of age or younger. We conducted all analyses in SAS (9.4; SAS Corporation, Cary, NC).
3 ∣. RESULTS
Of the 39,922 infants in the analysis, 10,898 were controls and 29,024 were cases. Twenty-four (0.2%) mothers of control infants, and 252 (0.9%) mothers of case infants reported pregestational type 1 diabetes. Thirty-four (0.3%) mothers of control infants, and 357 (1.2%) mothers of case infants reported pregestational type 2 diabetes. The distribution of characteristics among controls by maternal diabetes status is presented in Table 1.
TABLE 1.
Selected characteristics of control mothers by reported pregestational diabetes status, National Birth Defects Prevention Study 1997–2011
| Pregestational type 1 diabetes (n = 24) |
Pregestational type 2 diabetes (n = 34) |
No diabetes (n = 10,840) |
|
|---|---|---|---|
| Maternal characteristic | n (%)a | n (%)a | n (%)a |
| Age at delivery (years) | |||
| ≤24 | 8 (33.3) | 7 (20.6) | 3,612 (33.3) |
| 25–29 | 10 (41.7) | 7 (20.6) | 3,013 (27.8) |
| 30+ | 6 (25) | 20 (58.8) | 4,215 (38.9) |
| Race/ethnicity | |||
| Non-Hispanic White | 18 (75.0) | 12 (35.3) | 6,376 (58.9) |
| Other | 6 (25.0) | 22 (64.7) | 4,458 (41.2) |
| Education | |||
| High school or less | 13 (54.2) | 17 (51.5) | 4,212 (39.8) |
| More than high school | 11 (45.8) | 16 (48.5) | 6,362 (60.2) |
| Prepregnancy BMI | |||
| Normal/underweight BMI < 25 | 14 (58.3) | 3 (9.4) | 6,305 (60.6) |
| Overweight/obese BMI ≥ 25 | 10 (41.7) | 29 (90.6) | 4,098 (39.4) |
| Periconceptional smokingb | |||
| Yes | 4 (16.7) | 7 (21.2) | 1,918 (18.1) |
| No | 20 (83.3) | 26 (78.8) | 8,698 (81.9) |
| Periconceptional folic acid-containing supplement useb | |||
| Yes | 13 (54.2) | 24 (70.6) | 5,688 (52.9) |
| No | 11 (45.8) | 10 (29.4) | 5,064 (47.1) |
| Parity (previous stillbirths and livebirths) | |||
| 0 | 15 (62.5) | 5 (14.7) | 4,375 (40.4) |
| 1+ | 9 (37.5) | 29 (85.3) | 6,449 (59.6) |
| Intended pregnancy | |||
| Yes | 7 (38.9) | 19 (67.9) | 5,208 (59.1) |
| No | 11 (61.1) | 9 (32.1) | 3,608 (40.9) |
| Hypertension | |||
| Yes | 9 (37.5) | 18 (52.9) | 1,368 (12.8) |
| No | 15 (62.5) | 16 (47.1) | 9,336 (87.2) |
Abbreviation: BMI, body mass index (weight in kg/height in m).
Numbers vary because of missing values.
Periconceptional defined as the month before through the third month of pregnancy.
We estimated ORs for pregestational type 1 diabetes and 26 birth defects, 19 of which were adjusted estimates and seven were crude estimates (Tables 2 and 3). Adjusted ORs for pregestational type 1 diabetes ranged from 1.6 to 70.4, with the strongest association observed for sacral agenesis (aOR: 70.4; 95% CI: 32.3–147.2). Additionally, pregestational type 1 diabetes was associated with all but one of the reported cardiac defects; the strongest association among cardiac defects was observed for heterotaxy (aOR: 13.5; 95% CI: 5.7–29.3). Additionally, we observed high aORs (OR ≥ 10) for intercalary and longitudinal limb deficiency (aOR: 13.6; 95% CI: 6.8–26.1) and double outlet right ventricle with transposition of the great arteries (aOR: 10.8; 95% CI: 3.4–27.6). Additionally, we observed high cORs for pregestational type 1 diabetes and holoprosencephaly (aOR: 10.0; 95% CI: 1.9–33.4) and truncus arteriosus (aOR: 11.9; 95% CI: 2.3–39.9).
TABLE 2.
Associations between pregestational type 1 and type 2 diabetes and noncardiac birth defects included in the National Birth Defects Prevention Study, 1997–2011
| No diabetes |
Pregestational type 1 diabetes |
Pregestational type 2 diabetes |
|||
|---|---|---|---|---|---|
| All |
All |
All |
|||
| Birth defect | Unexposeda | Type 1 exposeda |
Type 1 OR (95% CI)b |
Type 2 exposeda |
Type 2 OR (95% CI)b |
| Amniotic band sequence | 315 | 2 | NC | 4 | 4.1 (1.0, 11.5) |
| Central nervous system defects | |||||
| Anencephaly | 588 | 10 | 6.9 (2.9, 15.0) | 4 | 2.2 (0.6, 6.1) |
| Spina bifida | 1,162 | 2 | NC | 6 | 1.6 (0.6, 3.6) |
| Encephalocele | 205 | 4 | 8.8 (2.2, 26.0) | 3 | 4.7 (0.9, 15.0) |
| Holoprosencephaly | 136 | 3 | 10.0 (1.9, 33.4) | 7 | 14.4 (5.7, 32.4) |
| Dandy–Walker malformation | 168 | 1 | NC | 1 | NC |
| Hydrocephaly | 453 | 10 | 9.6 (4.4, 19.5) | 9 | 7.6 (3.4, 15.4) |
| Cerebellar hypoplasia | 55 | 0 | NC | 0 | NC |
| Eye defects | |||||
| Anophthalmia/microphthalmiac | 211 | 1 | NC | 4 | 6.0 (1.5, 17.2) |
| Congenital cataractsc,d | 329 | 0 | NC | 3 | 3.1 (0.6, 10.2) |
| Glaucoma | 170 | 1 | NC | 0 | NC |
| Anotia/microtia | 593 | 12 | 8.4 (3.8, 17.4) | 6 | 2.8 (1.0, 6.6) |
| Orofacial defects | |||||
| Cleft lip with palatec,d | 1,822 | 10 | 2.3 (1.1, 4.7) | 23 | 4.1 (2.3, 7.1) |
| Cleft lip onlyc,d | 1,005 | 2 | NC | 13 | 4.8 (2.4, 9.3) |
| Cleft palate onlyc,d | 1,432 | 15 | 4.1 (2.1, 7.8) | 19 | 4.4 (2.4, 7.8) |
| Choanal atresia | 148 | 1 | NC | 1 | NC |
| Gastrointestinal defects | |||||
| Anorectal atresia/stenosis | 946 | 11 | 5.4 (2.6, 10.8) | 11 | 4.4 (2.2, 8.2) |
| Small intestine atresia/stenosis | 438 | 0 | NC | 2 | NC |
| Esophageal atresia | 697 | 2 | NC | 10 | 5.3 (2.5, 10.6) |
| Duodenal atresia/stenosis | 221 | 0 | NC | 1 | NC |
| Biliary atresia | 180 | 2 | NC | 2 | NC |
| Cloacal exstrophy | 88 | 0 | NC | 0 | NC |
| Colonic atresia/stenosis | 58 | 0 | NC | 0 | NC |
| Genitourinary defects | |||||
| Hypospadiasc,d | 2,368 | 8 | 1.7 (0.7, 4.4) | 17 | 3.8 (1.8, 8.0) |
| Renal agenesis/hypoplasia | 166 | 3 | 8.2 (1.6, 27.3) | 5 | 8.3 (2.6, 21.2) |
| Bladder exstrophy | 65 | 0 | NC | 2 | NC |
| Musculoskeletal defects | |||||
| Transverse limb deficiency | 661 | 3 | 2.1 (0.4, 6.8) | 5 | 2.9 (1.0, 6.7) |
| Intercalary and longitudinal limb deficiency | 471 | 14 | 13.6 (6.8, 26.1) | 11 | 9.6 (4.6, 18.8) |
| Craniosynostosis | 1,450 | 6 | 1.6 (0.6, 3.8) | 4 | 0.9 (0.2, 2.5) |
| Diaphragmatic hernia | 802 | 2 | NC | 6 | 2.4 (0.9, 5.5) |
| Omphalocele | 400 | 2 | NC | 4 | 3.2 (0.8, 9.0) |
| Gastroschisis | 1,404 | 2 | NC | 2 | NC |
| Sacral agenesis | 65 | 12 | 70.4 (32.3, 147.0) | 11 | 59.9 (25.4, 135.0) |
Note: Bold font represents a statistically significant finding; italicized font represents a crude odds ratio.
Abbreviations: CI, confidence interval; NC, not calculated; OR, odds ratio.
The pregestational type 1 analysis included 24 exposed and 10,840 unexposed controls. The pregestational type 2 analyses included 34 exposed and 10,840 unexposed controls.
Crude ORs and Fisher's Exact 95% CIs are presented for defects groups with 3–4 exposed cases and are italicized. For defects with ≥5 exposed cases, Firth's penalized likelihood estimates were adjusted for mother's age, race/ethnicity, education, body mass index (weight in kg/height in m, and study center. Estimates are not provided for analyses with <3 exposed cases.
The number of controls differed for the following pregestational type 1 birth defect analyses: clefts (24 exposed and 10,707 unexposed controls), hypospadias (11 exposed and 5,528 unexposed male controls).
The number of controls differed for the following pregestational type 2 birth defect analyses: congenital cataracts and glaucoma (27 exposed and 9,220 unexposed controls), clefts (34 exposed and 10,707 unexposed controls), hypospadias (16 exposed and 5,528 unexposed male controls).
TABLE 3.
Associations between pregestational type 1 and type 2 diabetes and cardiac birth defects included in the National Birth Defects Prevention Study, 1997–2011
| No diabetes |
Pregestational type 1 diabetes |
Pregestational type 2 diabetes |
|||
|---|---|---|---|---|---|
| All |
All |
All |
|||
| Birth defect | Unexposeda | Type 1 exposeda |
Type 1 OR (95% CI)b |
Type 2 exposeda |
Type 2 OR (95% CI)b |
| Heterotaxy | 307 | 9 | 13.5 (5.7, 29.3) | 11 | 11.8 (5.4, 24.1) |
| Conotruncal defects | |||||
| Truncus arteriosus | 114 | 3 | 11.9 (2.3, 39.9) | 9 | 20.3 (8.7, 44.0) |
| Tetralogy of Fallot | 1,060 | 8 | 3.7 (1.6, 7.9) | 20 | 5.1 (2.8, 9.1) |
| d-TGA | 708 | 9 | 5.5 (2. 5, 11.4) | 4 | 1.8 (0.5, 5.1) |
| DORV-TGA | 174 | 5 | 10.8 (3.4, 27.6) | 3 | 5.5 (1.1, 17.7) |
| Conoventricular septal Defectc,d | 102 | 0 | NC | 6 | 22.6 (7.7, 60.5) |
| Atrioventricular septal defect | 324 | 7 | 9.4 (3.8, 20.7) | 10 | 12.5 (5.7, 25.2) |
| TAPVR | 272 | 2 | NC | 3 | 3.5 (0.7, 11.3) |
| LVOTO defects | |||||
| HLHS | 579 | 1 | NC | 9 | 4.9 (2.1, 10.3) |
| Coarctation of the aorta | 1,047 | 8 | 3.4 (1.4, 7.3) | 16 | 5.4 (2.9, 9.8) |
| Aortic stenosis | 467 | 4 | 3.9 (1.0, 11.3) | 8 | 5.8 (2.4, 12.7) |
| RVOTO defects | |||||
| Pulmonary atresia | 240 | 0 | NC | 6 | 6.0 (2.1, 14.2) |
| Pulmonary valve stenosisc,d | 1,389 | 12 | 3.8 (1.8, 7.8) | 16 | 3.6 (1.9, 6.6) |
| Tricuspid atresia | 160 | 2 | NC | 4 | 8.0 (2.0, 22.7) |
| Ebstein anomaly | 171 | 0 | NC | 1 | NC |
| Septal defects | |||||
| Perimembranous VSDc,d | 1,313 | 14 | 4.6 (2.1, 10.2) | 24 | 5.7 (3.0, 11.0) |
| Muscular VSD | 176 | 0 | NC | 1 | NC |
| Secundum or ASD NOS | 2,680 | 45 | 7.4 (4.4, 12.5) | 55 | 6.4 (4.0, 10.2) |
| Single ventricle | 141 | 3 | 9.6 (1.8, 32.2) | 12 | 29.6 (13.5, 61.7) |
Note: Bold font represents a statistically significant finding; italicized font represents a crude odds ratio.
Abbreviations: ASD, atrial septal defect; CI, confidence interval; DORV-TGA, double outlet right ventricle with transposition of the great arteries; d-TGA, d-transposition of the great arteries; HLHS, hypoplastic left heart syndrome; LVOTO, left ventricular outflow tract obstruction; NC, not calculated; OR, odds ratio; RVOTO, right ventricular outflow tract obstruction; TAPVR, total anomalous pulmonary venous return; VSD, ventricular septal defect.
The pregestational type 1 analysis included 24 exposed and 10,840 unexposed controls. The pregestational type 2 analyses included 34 exposed and 10,840 unexposed controls.
Crude ORs and Fisher's Exact 95% CIs are presented for defects groups with 3–4 exposed cases and are italicized. For defects with ≥5 exposed cases, Firth's penalized likelihood estimates were adjusted for mother's age, race/ethnicity, education, body mass index (weight in kg/height in m), and study center. Estimates are not provided for analyses with <3 exposed cases.
The number of controls differed for the following type 1 birth defect analyses: pulmonary valve stenosis (21 exposed, 10,401 unexposed controls) and perimembranous VSD (14 exposed and 9,792 unexposed controls).
The number of controls differed for the following type 2 birth defect analyses: conoventricular VSD (16 exposed and 6,340 unexposed controls), pulmonary valve stenosis (34 exposed and 10,401 unexposed controls), perimembranous VSD (16 exposed and 6,340 unexposed controls).
We estimated ORs for pregestational type 2 diabetes and 39 birth defect groups (Tables 2 and 3), of which 28 were adjusted and 11 were crude estimates. Adjusted ORs for pregestational type 2 diabetes ranged from 1.6 to 59.9. As with type 1 diabetes, we observed the strongest association for type 2 diabetes and sacral agenesis (aOR: 59.9; 95% CI: 25.4–135.2). All but two included cardiac birth defects (d-transposition of the great arteries and total anomalous pulmonary venous return) were associated with pregestational type 2 diabetes and the strongest association among cardiac defects was for single ventricle defect (aOR: 29.6; 95% CI: 13.5–61.7). We also observed aORs ≥10 for pregestational type 2 diabetes and holoprosencephaly (aOR: 14.4; 95% CI: 5.7–32.4), heterotaxy (aOR: 11.8; 95% CI: 5.4–24.1), truncus arteriosus (aOR: 20.3; 95% CI: 8.7–44.0), conoventricular septal defects (aOR: 22.6; 95% CI: 7.7–60.5), and atrioventricular septal defects (aOR: 12.5; 95% CI: 5.7–25.2).
For isolated cases, pregestational type 1 diabetes was significantly associated with 15 of the 19 assessed defects with aORs ranging from 3.2 to 328.0 (Tables S1 and S2). Pregestational type 2 diabetes was significantly associated with 17 of 27 isolated birth defects assessed with aORs ranging from 2.5 to 18.8. For both type 1 and type 2 diabetes, these estimates were generally similar to those from the main analysis in which both isolated and multiple cases were analyzed together.
Of the 276 mothers with pregestational type 1 diabetes in our main analysis, 76.1% (191 cases; 19 controls) were diagnosed at age 20 or younger. We saw no meaningful differences in OR estimates when we limited the analysis to mothers who were diagnosed at a younger age (data not shown).
4 ∣. DISCUSSION
We observed strong associations between pregestational diabetes of either type and most birth defects assessed. Pregestational type 1 diabetes had strong, statistically significant ORs for 22 defects. We observed strong, statistically significant ORs for pregestational type 2 diabetes and 29 defects. Most defects for which we observed increased risk were associated with both types of diabetes. For the defects with five or more exposed cases, adjusted estimates were similar regardless of diabetes type.
Pregestational diabetes is an established risk factor for birth defects. While pregestational diabetes and risk of birth defects has been studied previously, we were able to calculate estimates for specific major birth defects rather than overall groupings based on body system. Some studies have found higher rates of a combined birth defect outcome among women with pregestational type 1 diabetes compared with women with pregestational type 2 diabetes but did not explore specific birth defects (Lapolla et al., 2008; Murphy et al., 2017; Peticca et al., 2009). Gonzalez-Gonzalez et al. (2008) found similar associations for pregestational type 1 and type 2 diabetes and the risk of birth defects, but did not evaluate specific defects. In contrast, Clausen et al. (2005) observed that pregestational type 2 diabetes was more strongly associated with birth defects than pregestational type 1 diabetes.
Several studies have explored associations between each type of pregestational diabetes and specific defects (Arendt et al., 2021; Bánhidy, Acs, Puhó, & Czeizel, 2010; Jovanovič et al., 2015). Using data from the Hungarian Case–Control Surveillance System of Congenital Abnormalities, Bánhidy et al. (2010) observed that pregestational type 1 diabetes was associated with renal agenesis/dysgenesis, obstructive urinary tract defects, cardiovascular malformations, and caudal dysplasia sequence and that pregestational type 2 diabetes was associated with diaphragmatic defects. While we did not explore larger groupings of defects, we did observe a similar elevated association for type 1 diabetes and bilateral renal agenesis and associations between type 1 diabetes and 11 specific cardiac defects. However, we also observed elevated associations for type 2 diabetes and cardiac birth defects, which Bánhidy et al. (2010) did not. Lastly, Bánhidy et al. (2010) observed a significantly elevated association between pregestational type 2 diabetes and diaphragmatic hernia. We observed an aOR of 2.4, but the CI included the null value of 1.0.
Among women with pregestational type 2 diabetes, Jovanovič et al. (2015) found significantly elevated circulatory, cleft, digestive, facial, heart, integument, and nervous system defects compared with nondiabetics, and significantly elevated risk for pregestational type 1 diabetics and circulatory and heart defects, which we also observed. Among women with pregestational type 1 diabetes, Arendt et al. (2021) observed major heart defects, and major malformations of the eye, respiratory system, and digestive system. For mothers with pregestational type 2 diabetes, the highest prevalence of birth defects observed were for major congenital heart diseases, similar to our observations. Lastly, our findings are consistent with previously published findings using the same years of NBDPS data that combined type 1 and type 2 diabetes (Correa et al., 2008). For most defects, we found an elevated association for both type 1 and type 2 diabetes. However, we observed potential differences by type of diabetes and hypospadias.
Other studies have reported associations that we did not observe in our data. For example, a population-based national registry study found a positive association between spina bifida and pregestational diabetes (Mowla et al., 2020). We did not observe an increased risk of spina bifida in the present study nor did a previous study using NBDPS data that combined all pregestational diabetics (Tinker et al., 2020). Tinker et al. (2020) suggested that the lack of an effect observed in NBDPS may be at least partially explained by effect modification by folic acid. We did not explore this hypothesis in our study. Parker, Yazdy, Tinker, Mitchell, and Werler (2013) explored the relationship between spina bifida, pregestational diabetes, and folic acid use, finding that folic acid attenuates, but does not eliminate, the association between diabetes and spina bifida.
Our study had several strengths. NBDPS has a large sample size allowing us to analyze specific defects and control for potential confounders. While pregestational diabetes and risk of birth defects has been studied previously, our study included rare defects that smaller studies were unable to analyze. Our study utilized strict case classification by clinical geneticists' criteria using medical records, so we expect little outcome misclassification. We were also able to separately evaluate isolated cases of specific defects.
A limitation of this analysis is that we relied on maternal self-reported diabetes and timing of diagnosis. Although several studies have found high concordance between administrative data or medical records and self-reported chronic conditions, including diabetes (Fortin, Haggerty, Sanche, & Almirall, 2017; Jackson et al., 2014; Tisnado et al., 2006), some evidence suggests that self-reported diabetes status has high specificity but lower sensitivity (Day & Parker, 2013). There may have been underreporting of diabetes in NBDPS, only 0.2% of controls reported pregestational type 1 diabetes and 0.3% reported type 2 diabetes, which is lower than the 0.89% prevalence estimate from another national study (Bardenheier et al., 2015). Misclassification of diabetes type is likely (Seidu, Davies, Mostafa, de Lusignan, & Khunti, 2014; Shields et al., 2015). To reduce bias due to exposure misclassification, we excluded women who reported diabetes of unknown type. Additionally, since type 1 diabetes generally necessitates insulin replacement therapy (Shields et al., 2015), we excluded women who reported pregestational type 1 diabetes but did not report continuous insulin use from the time of diagnosis. To further assess potential bias associated with exposure misclassification, we conducted a sensitivity analysis restricted to mothers with pregestational type 1 diabetes diagnosis at 20 or younger. We found that a stricter exposure definition did not meaningfully change our results.
Given that pregestational type 1 and type 2 diabetes are rare exposures within NBDPS, we used Firth's penalized regression to estimate adjusted ORs. Even using this method, we observed imprecise estimates with wide 95% CIs. Given the number of statistical tests performed, some of the observed associations may be due to chance. The main analysis included 65 statistical tests; at α = 0.05, approximately three significant associations would be expected by chance alone (65 statistical tests * 0.05 = 3.25). We observed 53 such associations. Given that these associations were robust in sensitivity analyses, are biologically plausible, and are consistent with previous studies that did not use NBDPS data, it is unlikely that all results were due to statistical chance. In addition, previous studies, including a systematic review, found that poor glycemic control was associated with a greater than threefold risk for birth defects compared to optimal glycemic control among pregnant women with pregestational diabetes (Inkster et al., 2006). We did not have clinical information on diabetes control, such as fasting glucose measurement or glycated hemoglobin (HbA1c) and were therefore not able to explore effect modification by disease severity or glucose control. Additionally, while we controlled for some potential confounders, there may be residual confounding by measured or unmeasured factors.
Although the exact teratogenic mechanism is unknown, altered glucose metabolism is a potential mechanism through which both pregestational type 1 and type 2 diabetes may impact the risk of birth defects (Bardenheier et al., 2015). Dude, Badreldin, Schieler, and Yee (2021) found that higher periconception glycosylated hemoglobin in women with pregestational diabetes was significantly associated with major and minor congenital fetal anomalies. In our analysis, similar estimates for specific defects for both pregestational type 1 and type 2 diabetes support this potential mechanism. Therefore, it is important to emphasize control of diabetes before pregnancy for women with either pregestational type 1 or type 2 diabetes. A meta-analysis of 25 studies demonstrated that preconception care, including glucose monitoring, among women with diabetes reduced their risk of birth defects by 71% (Wahabi et al., 2020). Given that most birth defects occur early in the first trimester and a substantial proportion of pregnancies are unintended (61% of control mothers with pregestational type 1 diabetes and 32% of control mothers with pregestational type 2 diabetes in our analysis), post-pregnancy recognition may be too late to address birth defect risk factors. Thus, proper glycemic control should be emphasized for all diabetic women of reproductive age, regardless of pregnancy planning status.
Mothers with pregestational type 1 or type 2 diabetes are at high risk for having a pregnancy affected by a birth defect. Relatively similar associations with pregestational type 1 and pregestational type 2 diabetes and many different birth defects suggest that controlling high blood glucose provides an opportunity for prevention. Since pregestational diabetes of either type are relatively rare occurrences, more studies evaluating both types of pregestational diabetes and the role of their respective monitoring and glycemic control methods could help inform birth defect prevention interventions.
Supplementary Material
ACKNOWLEDGMENTS
We thank the participating families, scientists, and staff from the National Birth Defects Prevention Study sites. The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. This study was supported through Centers for Disease Control and Prevention cooperative agreements under PA #96043, PA #02081, FOA #DD09-001, FOA #DD13-003, and NOFO #DD18-001 to the Centers for Birth Defects Research and Prevention participating in the National Birth Defects Prevention Study and/or the Birth Defects Study To Evaluate Pregnancy exposures.
FUNDING INFORMATION
The manuscript reports findings from a study funded through a cooperative agreement from the Centers for Disease Control and Prevention (Grant number: U01/DD00048702). This study was supported through Centers for Disease Control and Prevention cooperative agreements under PA #96043, PA #02081, FOA #DD09-001, FOA #DD13-003, and NOFO #DD18-001 to the Centers for Birth Defects Research and Prevention participating in the National Birth Defects Prevention Study and/or the Birth Defects Study To Evaluate Pregnancy exposures.
Footnotes
Presented at the 2021 Society for Birth Defects Research and Prevention Meeting, Virtual, from June 24, 2021 to July 1, 2021.
CONFLICT OF INTEREST
The authors have no conflicts of interest or financial disclosures relevant to this manuscript. This analysis has been replicated by an independent analyst prior to publication. The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of the article at the publisher's website.
DATA AVAILABILITY STATEMENT
Study questionnaires and process for accessing the data used in this study are described at https://www.cdc.gov/ncbddd/birthdefects/nbdps-public-access-procedures.html. The code book may be made available upon request.
REFERENCES
- Arendt LH, Pedersen LH, Pedersen L, Ovesen PG, Henriksen TB, Lindhard MS, … Ramlau-Hansen CH (2021). Glycemic control in pregnancies complicated by pre-existing diabetes mellitus and congenital malformations: A Danish population-based Study. Clinical Epidemiology, 13, 615–626. 10.2147/CLEP.S298748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bánhidy F, Acs N, Puhó EH, & Czeizel AE (2010). Congenital abnormalities in the offspring of pregnant women with type 1, type 2 and gestational diabetes mellitus: A population-based case-control study. Congenital Anomalies, 50(2), 115–121. 10.1111/j.1741-4520.2010.00275.x [DOI] [PubMed] [Google Scholar]
- Bardenheier BH, Imperatore G, Devlin HM, Kim SY, Cho P, & Geiss LS (2015). Trends in pre-pregnancy diabetes among deliveries in 19 U.S. states, 2000-2010. American Journal of Preventive Medicine, 48(2), 154–161. 10.1016/j.amepre.2014.08.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botto LD, Lin AE, Riehle-Colarusso T, Malik S, Correa A, & National Birth Defects Prevention Study. (2007). Seeking causes: Classifying and evaluating congenital heart defects in etiologic studies. Birth defects research Part A, Clinical and Molecular Teratology, 79(10), 714–727. 10.1002/bdra.20403 [DOI] [PubMed] [Google Scholar]
- Clausen TD, Mathiesen E, Ekbom P, Hellmuth E, Mandrup-Poulsen T, & Damm P (2005). Poor pregnancy outcome in women with type 2 diabetes. Diabetes Care, 28(2), 323–328. 10.2337/diacare.28.2.323 [DOI] [PubMed] [Google Scholar]
- Correa A, Gilboa SM, Besser LM, Botto LD, Moore CA, Hobbs CA, … Reece EA (2008). Diabetes mellitus and birth defects. American Journal of Obstetrics and Gynecology, 199(3), 237.e1–237.e2379. 10.1016/j.ajog.2008.06.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day HR, & Parker JD (2013). Self-report of diabetes and claims-based identification of diabetes among Medicare beneficiaries. National Health Statistics Reports, 69, 1–14. [PubMed] [Google Scholar]
- Dude AM, Badreldin N, Schieler A, & Yee LM (2021). Periconception glycemic control and congenital anomalies in women with pregestational diabetes. BMJ Open Diabetes Research & Care, 9(1), e001966. 10.1136/bmjdrc-2020-001966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth D (1993). Bias reduction of maximum likelihood estimates. Biometrika, 80(1), 27–38. 10.2307/2336755 [DOI] [Google Scholar]
- Fortin M, Haggerty J, Sanche S, & Almirall J (2017). Self-reported versus health administrative data: Implications for assessing chronic illness burden in populations. A cross-sectional study. CMAJ Open, 5(3), E729–E733. 10.9778/cmajo.20170029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Gonzalez NL, Ramirez O, Mozas J, Melchor J, Armas H, Garcia-Hernandez JA, … Bartha JL (2008). Factors influencing pregnancy outcome in women with type 2 versus type 1 diabetes mellitus. Acta Obstetricia et Gynecologica Scandinavica, 87(1), 43–49. 10.1080/00016340701778732 [DOI] [PubMed] [Google Scholar]
- Inkster ME, Fahey TP, Donnan PT, Leese GP, Mires GJ, & Murphy DJ (2006). Poor glycated haemoglobin control and adverse pregnancy outcomes in type 1 and type 2 diabetes mellitus: Systematic review of observational studies. BMC Pregnancy and Childbirth, 6, 30. 10.1186/1471-2393-6-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JM, DeFor TA, Crain AL, Kerby TJ, Strayer LS, Lewis CE, … Margolis KL (2014). Validity of diabetes self-reports in the Women's health initiative. Menopause, 21(8), 861–868. 10.1097/GME.0000000000000189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovanovič L, Liang Y, Weng W, Hamilton M, Chen L, & Wintfeld N (2015). Trends in the incidence of diabetes, its clinical sequelae, and associated costs in pregnancy. Diabetes/Metabolism Research and Reviews, 31(7), 707–716. 10.1002/dmrr.2656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karabon P (2020). Rare events or non-convergence with a binary outcome? The power of Firth regression in PROC LOGISTIC. Proceedings of the SAS Global Forum. 4654–2020. Retrieved from https://www.sas.com/content/dam/SAS/support/en/sas-global-forum-proceedings/2020/4654-2020.pdf. [Google Scholar]
- Lapolla A, Dalfrà MG, Di Cianni G, Bonomo M, Parretti E, Mello G, & Scientific Committee of the GISOGD Group. (2008). A multicenter Italian study on pregnancy outcome in women with diabetes. Nutrition, Metabolism, and Cardiovascular Diseases: NMCD, 18(4), 291–297. 10.1016/j.numecd.2006.12.001 [DOI] [PubMed] [Google Scholar]
- Maahs DM, West NA, Lawrence JM, & Mayer-Davis EJ (2010). Epidemiology of type 1 diabetes. Endocrinology and Metabolism Clinics of North America, 39(3), 481–497. 10.1016/j.ecl.2010.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macintosh MC, Fleming KM, Bailey JA, Doyle P, Modder J, Acolet D, … Miller A (2006). Perinatal mortality and congenital anomalies in babies of women with type 1 or type 2 diabetes in England, Wales, and Northern Ireland: Population based study. BMJ, 333(7560), 177. 10.1136/bmj.38856.692986.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer-Davis EJ, Lawrence JM, Dabelea D, Divers J, Isom S, Dolan L, … SEARCH for Diabetes in Youth Study. (2017). Incidence trends of type 1 and type 2 diabetes among youths, 2002-2012. The New England Journal of Medicine, 376(15), 1419–1429. 10.1056/NEJMoa1610187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills JL (2010). Malformations in infants of diabetic mothers. Clinical and Molecular Teratology 25:385–94. 1982. Birth Defects Research. Part A, Clinical and Molecular Teratology, 88(10), 769–778. 10.1002/bdra.20757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowla S, Gissler M, Räisänen S, & Kancherla V (2020). Association between maternal pregestational diabetes mellitus and spina bifida: A population-based case-control study, Finland, 2000-2014. Birth Defects Research, 112(2), 186–195. 10.1002/bdr2.1624 [DOI] [PubMed] [Google Scholar]
- Murphy HR, Bell R, Cartwright C, Curnow P, Maresh M, Morgan M, … Lewis-Barned N (2017). Improved pregnancy outcomes in women with type 1 and type 2 diabetes but substantial clinic-to-clinic variations: A prospective nationwide study. Diabetologia, 60(9), 1668–1677. 10.1007/s00125-017-4314-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker SE, Yazdy MM, Tinker SC, Mitchell AA, & Werler MM (2013). The impact of folic acid intake on the association among diabetes mellitus, obesity, and spina bifida. American Journal of Obstetrics and Gynecology, 209(3), 239.e1–239.e2398. 10.1016/j.ajog.2013.05.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peticca P, Keely EJ, Walker MC, Yang Q, & Bottomley J (2009). Pregnancy outcomes in diabetes subtypes: How do they compare? A province-based study of Ontario, 2005-2006. Journal of Obstetrics and Gynaecology Canada, 31(6), 487–496. 10.1016/S1701-2163(16)34210-4 [DOI] [PubMed] [Google Scholar]
- Rasmussen SA, Olney RS, Holmes LB, Lin AE, Keppler-Noreuil KM, Moore CA, & National Birth Defects Prevention Study. (2003). Guidelines for case classification for the National Birth Defects Prevention Study. Birth Defects Research Part A, Clinical and Molecular Teratology, 67(3), 193–201. 10.1002/bdra.10012 [DOI] [PubMed] [Google Scholar]
- Reefhuis J, Gilboa SM, Anderka M, Browne ML, Feldkamp ML, Hobbs CA, … Honein MA (2015). The National Birth Defects Prevention Study: A review of the methods. Birth defects Research Part A, Clinical and Molecular Teratology, 103(8), 656–669. 10.1002/bdra.23384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidu S, Davies MJ, Mostafa S, de Lusignan S, & Khunti K (2014). Prevalence and characteristics in coding, classification and diagnosis of diabetes in primary care. Postgraduate Medical Journal, 90(1059), 13–17. 10.1136/postgradmedj-2013-132068 [DOI] [PubMed] [Google Scholar]
- Shields BM, Peters JL, Cooper C, Lowe J, Knight BA, Powell RJ, … Hattersley AT (2015). Can clinical features be used to differentiate type 1 from type 2 diabetes? A systematic review of the literature. BMJ Open, 5(11), e009088. 10.1136/bmjopen-2015-009088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinker SC, Gilboa SM, Moore CA, Waller DK, Simeone RM, Kim SY, … National Birth Defects Prevention Study. (2020). Specific birth defects in pregnancies of women with diabetes: National Birth Defects Prevention Study, 1997-2011. American Journal of Obstetrics and Gynecology, 222(2), 176.e1–176.e11. 10.1016/j.ajog.2019.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tisnado DM, Adams JL, Liu H, Damberg CL, Chen WP, Hu FA, … Kahn KL (2006). What is the concordance between the medical record and patient self-report as data sources for ambulatory care? Medical Care, 44(2), 132–140. 10.1097/01.mlr.0000196952.15921.bf [DOI] [PubMed] [Google Scholar]
- Wahabi HA, Fayed A, Esmaeil S, Elmorshedy H, Titi MA, Amer YS, … Sabr Y (2020). Systematic review and meta-analysis of the effectiveness of pre-pregnancy care for women with diabetes for improving maternal and perinatal outcomes. PLoS One, 15(8), e0237571. 10.1371/journal.pone.0237571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J, Cummings EA, O'Connell C, & Jangaard K (2006). Fetal and neonatal outcomes of diabetic pregnancies. Obstetrics and Gynecology, 108(3 Pt 1), 644–650. 10.1097/01.AOG.0000231688.08263.47 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Study questionnaires and process for accessing the data used in this study are described at https://www.cdc.gov/ncbddd/birthdefects/nbdps-public-access-procedures.html. The code book may be made available upon request.