Abstract
Objectives
Almost a quarter of the global burden of disease and mortalities is attributable to environmental causes, the magnitude of which is projected to increase in the near future. However, in many low- and middle-income settings, there remains a large gap in the synthesis of evidence on climate-sensitive health outcomes. In India, now the world’s most populous country, little remains known about the impacts of climate change on various health outcomes. The objective of this study is to better understand the challenges faced in conducting climate change and health research in Puducherry, India.
Design and setting
In this study, we employed key informant interviews to deepen the understanding of the perceived research barriers in Puducherry. The findings were analysed using data-driven qualitative thematic analysis to elaborate the major perceived barriers to conducting environmental health research.
Participants
This study was conducted among 16 public health professionals, including medical researchers, and professionals involved in environmental policies and planning in Puducherry.
Results
We identify three key barriers faced by public health professionals as key stakeholders, namely: (1) political and institutional barriers; (2) education and awareness barriers; and (3) technical research barriers. We show there is a need, from the professionals’ perspective, to improve community and political awareness on climate change and health; strengthen technical research capacity and collaboration among researchers; and strengthen health surveillance, resource allocation and access to health data for research.
Conclusion
Evidence informed policies and interventions are a key element in the adaptation response for countries. In the context of the paucity of data on environmental health from India, despite recognised climate change related health vulnerabilities, these findings could contribute to the development and improvement of relevant interventions conducive to a strong research environment.
Keywords: public health, qualitative research, epidemiology
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study identifies crucial challenges faced in conducting environmental health research by public health professionals for the first time.
The findings draw on the experiences of respected experts who are well placed in the climate change and health sphere.
The sample was restricted to Puducherry district and not representative of the entire Union Territory of Puducherry, much less India as a whole.
The sample is restricted to the opinions of a selected group of experts and we could not include the experiences and perspectives of other public health professionals or stakeholders.
Introduction
An ever-growing body of research has irrefutably shown the global health impacts of climate change through both direct and indirect exposure pathways.1 2 Multiple risk and vulnerability factors determine the population resilience and adaptive capacity, from sociopolitical, demographic and biological factors to infrastructure, urban planning, health information systems and health workforce.2 3 Given the regional variations in climate systems, the health impacts of climate change differ between and within countries and communities, mediated by interconnected socioeconomic and environmental determinants of health.4 5 Non-communicable diseases, such as respiratory diseases, cardiovascular diseases (CVDs) and mental health conditions, have been recognised as growing climate-sensitive health outcomes, in addition to other communicable diseases like vector-borne and water-borne diseases and malnutrition.3 6
With the rapid pace of climate change, the health impacts attributable to it are also projected to increase.7 Strengthening the adaptive capacity of countries is therefore an essential component of the climate change response.8 Timely public health interventions can do much to protect population health from the potential adverse health impacts of climate change.9 Low- and middle-income countries (LMICs), such as India, remain disproportionately affected by climate impacts, with a critical need to strengthen the healthcare response to climate impacts.10 11 One of the key steps in the regional or local adaptation response is assessing the true burden of the health impacts within the population of that location.12 However, owing to the complexity of the relationship between climate change and health, identifying and estimating this association remain one of the biggest global and environmental health challenges, especially in LMICs.11
In India, the existing health and social disparities within the population make it one of the most vulnerable to climate change impacts, compounded by climatic diversity.13–16 There have been recent efforts from the Government of India to focus on climate change and health, as evinced by the recent addition of a health mission to the National Action Plan on Climate Change (NAPCC). This led to the formulation of the National Action Plan on Climate Change and Human Health (NAPCCHH) and the drive for State Action Plans for Climate Change and Human Health (SAPCCHH).17 18 The government recognises several diseases as climate sensitive in these official documents. However, public health engagement, action and research on health impacts of climate change are limited in India, especially given the magnitude of climate impacts to which it is vulnerable.19 20
Medical and public health professionals, hereafter referred to as health professionals, play an important role in researching, managing and responding to climate change impacts on health. Along with being considered credible sources of information, these groups of professionals also have the capacity for scientific inquiries into the climate change attributable impacts of health.21–24 Globally, there is an acknowledged need to train health professionals to engage in, study and manage health impacts of climate change. There are few studies assessing stakeholder perceptions on climate change and health,14 25 26 and even fewer studies looking at specific barriers to research on this topic.27 28 Given the present gaps in this domain, especially in LMICs, it is particularly salient to better understand research barriers and needs, as perceived by health professionals.25–27 29
The aim of this study is to understand some of the contextual barriers to environmental health action and research among two relevant professional groups in Puducherry, India. We focused our study on: (1) medical professionals, both in active research and practising; and (2) members of the Department of Science, Technology and Environment (DSTE) working on climate change in Puducherry. As this study is a part of a larger project on CVDs and climate change in India, we also highlighted the specific challenges and barriers to conducting research on CVDs.
Methods
Study setting
This study employed key informant interviews following a semistructured interview guide. The methods have been described in detail elsewhere. Briefly, the geographical focus of our study was Puducherry district, which lies on the south-eastern coast of India, with a population of 950 289, as per the Government of India 2011 Census.30 Puducherry has one main State government run tertiary care hospital and medical college, along with several private clinics and primary care health centres. It is also home to the Central Government Jawaharlal Institute of Postgraduate Medical Education and Research, an ‘Institute of National Importance’ and tertiary care referral hospital. Within the DSTE, there also exists a specialised Puducherry Climate Change Cell with the aim to integrate knowledge about climate change and facilitate the NAPCC implementation, including the state specific Action Plan.31
Data collection and analysis
Sixteen semistructured interviews were conducted between January and March 2022 with participants from Puducherry. Fourteen interviews were conducted in-person and two were conducted virtually over Zoom. Using purposive sampling based on prior connections followed by snowball sampling, we invited medical professionals (research or practicing) and DSTE staff working on the Puducherry State Action Plan for Climate Change (hereon referred to as environmentalists). Interviews continued until information saturation was reached in the interviews or we had interviewed all the relevant target participants, as in the case of the DSTE staff. The full interview guide and framework with the main categories has been given in the online supplemental table S1.
bmjopen-2023-073381supp001.pdf (224.4KB, pdf)
Eleven of the participants had a medical background and were working as either practising physicians or researchers. Within the doctors, we mainly targeted cardiologists, emergency medicine or general medicine physicians who were involved in areas relevant to our study. The majority of the participants was male, with only three females, out of which only one had a medical background. Half of the participants were practising physicians, while the other half were researchers. The participant profile is presented in table 1 and further described in Ref 32.
Table 1.
Profile of participants interviewed in this study
| Sector/background | n | Females (n) | Males (n) | Age range (years) | Range of experience (years) |
| Medicine (in-practice) | 8 | 0 | 8 | 32–51 | 3–20 |
| Research (medical) | 3 | 1 | 2 | 40–44 | 11–20 |
| Research (environment/governmental) | 5 | 2 | 3 | 28–53 | 4–30 |
The interviews, conducted by S.S., lasted between 15 to 50 min and were audio recorded with informed consent using a voice recorder. Field notes taken to optimise the interview guide and note key topics. R.L. was a passive observer and facilitator for three interviews. We used an a priori developed interview guide with broad and open-ended questions to allow participants to freely bring up and discuss relevant topics. All interview recordings were assigned a number prior to transcription to ensure anonymity throughout the analysis process. Verbatim transcription and analysis was done using the MaxQDA software V.2018.1 (VERBI Software, Berlin, Germany) by S.S.
For the analysis, a combination of deductive and inductive thematic analysis was used as described by Gale et al.33 Broad themes were developed based on the aim, framework and interview guide, as discussed below. During analysis, major themes were inductively developed for emerging topics, which we then clearly defined. After familiarisation with the transcripts, an initial codebook was developed from coding the three interviews with the richest data; the remaining interviews were indexed and coded further. The codes were classified into categories, subthemes and themes. The final analytical matrix included three themes. S.S. and T.L. independently validated the codebook with the three main interviews and agreed on the final framework matrix that considered all relevant codes. The matrix was then used to chart relevant quotes supporting our findings and draw comparisons between participants.
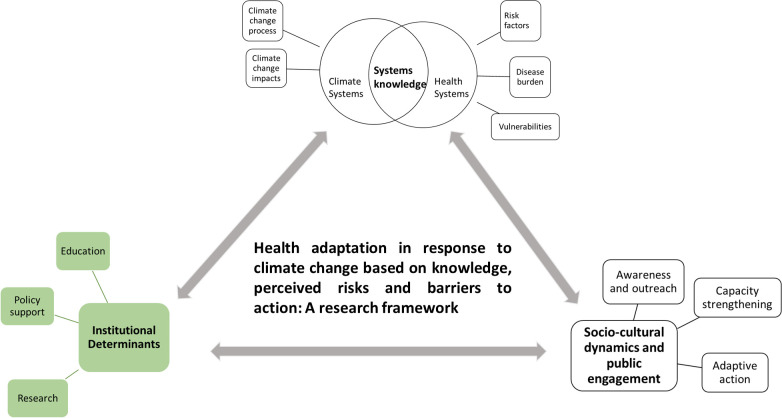
The conceptual framework for climate change risk perceptions developed by van Eck et al 34 and the framework for health inequalities proposed by Rudolph et al 35 were used as a base for our analytical framework, shown in figure 1. While there are three major themes, this paper focuses only on the theme of ‘Institutional determinants’. The findings from the two other themes have been elaborated elsewhere. Within the context of this paper, ‘institution’ is used as a broad term covering all governmental structures, including policy, education and occupation. We identify how these determinants can be perceived as barriers to environmental health research. The framework matrix with relevant themes and categories has been provided in online supplemental table S2. Additional supporting quotes have also been provided in the online supplemental material.
Figure 1.
A framework for health adaptation action in the context of climate change based on level of knowledge, perceived health risks, policy and institutional support and public engagement. The circled part highlights the thematic areas we focus on in this work, namely institutional determinants and its challenges.
Ethical consideration
There was no prior relationship between the researchers and participants. Before the interview, the researcher went over the informed consent form, which was then signed by both parties. S.S., the main researcher, is an Indian PhD candidate supervised by a team of international experts based mainly in Switzerland. R.L. is also Indian national based in Puducherry. Additionally, all the quotes presented in this analysis have been assigned only by serial number to ensure anonymity.
Patient and public involvement
As we employed a combination of purposive and snowball sampling, some participants were involved in helping us identify suitable participants to interview. Beyond that, no members of the public were involved in the design, conduct, reporting or dissemination plan of our research.
Results
Overall, there are four main themes that emerged from this research, which are presented in figure 2. We first report participants’ knowledge regarding climate change and health policies, followed by their perceived institutional barriers to research, namely political, educational and technical barriers. As this study is part of a larger study examining climate change impacts on CVDs, we also highlight barriers specific to climate change and CVD research.
Figure 2.
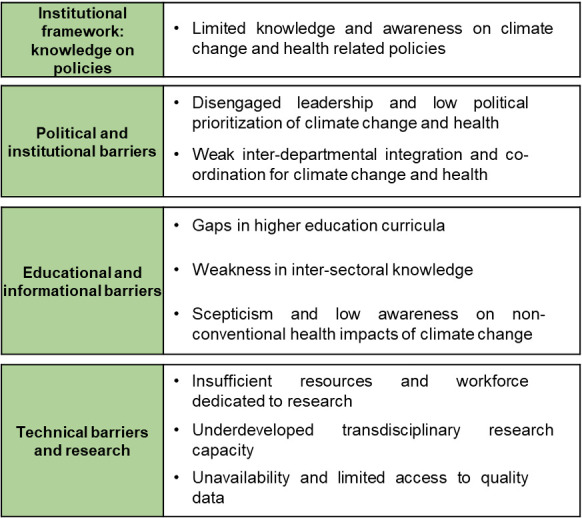
An overview of the thematic framework and salient findings for the four themes explored in this paper. The four main themes are: (1) institutional framework: knowledge on policies; (2) political and institutional; (3) educational and informational; and (4) technical research barriers.
Institutional framework: knowledge on policies
Limited knowledge and awareness on climate change and health related policies
We found limited awareness among the participants about climate change and health-related policies, such as the NAPCC, NAPCCHH and SAPCCHH. Aside from the environmentalists, who worked on it, only three medical professionals who worked on one of the Action Plans were aware of it. Four participants expressed belief about the non-inclusion of climate change in disease-specific policies and the lack of integrated climate change and health policies and guidelines.
Our country has different policy, environmental policy, health policy. But I have doubt whether health policy has any component of climate change. So, it needs to be incorporated in a health policy of national importance as well as the state, but currently, this element is not in place, that is my feeling. #8, Environmentalist.
One of the environmentalist also mentioned challenges in integrating climate change in development plans. These were thought to be made primarily from a socioeconomic development perspective, although there were ongoing efforts to include the economic co-benefits of climate change adaptation in the development plans.
The challenge is that the government sectoral officers are not aware of how the climate adaptations need to be integrated into their developmental plans. Because whenever they plan for a project, they plan it from the socioeconomic development perspective. #7, Environmentalist.
Political and institutional barriers
Disengaged leadership and low political prioritisation of climate change and health
Political leadership that did not consider health impacts of climate change as a pressing matter was perceived as one of the barriers to conducting research on the topic. Several participants mentioned how climate change was seen as future concern by policy-makers and the general public, rather than viewed as a cause for immediate concern. A few participants also mentioned the slim likelihood of decision-makers actually being aware of it. One participant described the issue as being ‘not mainstream enough’ to warrant focused work, contributing to the perceived low priority assigned to environmental health research.
Many participants felt that the governmental focus was inclined towards non-health impacts of climate change. The most pressing climate change impacts, which also influence research focus, were thought to be pollution, coastal sensitivity and natural resource depletion and degradation, especially in the context of Puducherry as a coastal region. Additionally, existing sectoral programmes already running were seen as a hindrance to focusing on climate change related programmes by one participant.
The problem is everybody has to understand at the level of the minister or the secretaries. So many programmes are there. Not only about climate change, other programmes are there so they do not focus much on (climate change) programmes… Actually, what I have seen for the past 2–3 years, they don’t care much about climate. #1, Practicing physician/policy advisor.
Despite climate change being recognised as a health risk factor, there was a clear disconnect between on-paper government plans and practice when it came to environmental health research. The challenges India faces from other vulnerabilities, including unmet nutritional and economic needs, were perceived to outrank climate risks to health.
I'm an adviser to government of India on health related research. We did discuss a lot of things but we also touched upon climate and the effects of climate on health… That was considered as an important topic, but we didn't dwell much upon how to take it forward because there are more pressing problems. #15, Practicing physician/academic.
Weak interdepartmental integration and coordination for climate change and health
The compartmentalisation of topics within institutes or sectors was seen as a barrier to conducting interdisciplinary research by the participants. One participant discussed the newly formed Puducherry Climate Change and Health Action Plan (2022), which aims to bring together a multisectoral team, under the leadership of the health ministry, to focus on health impacts of climate change.
However, apart from one participant, most others voiced a perceived need for an independent, coordinating body focused on environmental health, incorporating a research agenda. Partially, this was due to climate change being thought of an added responsibility for health professionals and vice versa for environmentalists, especially for those working in the government. As highlighted by a few participants, officials were likely to prioritise their primary work profile over the added responsibility of climate change and health research. Another concern in the existing scenario was intersectoral, collaborative research being dependant on higher officials being receptive to their junior employees researching a topic not entirely within the scope of their respective department.
Especially government departments, they are loaded with a lot of work. Today, an officer comes in, he has to do his own work, not the work that other departments asks us to do… #9, Environmentalist.
Several participants mentioned the Puducherry Climate Change cell created in response to address climate change impacts. However, despite that, one medical researcher mentioned the current difficulties in collaborating on climate change and health. Several participants also mentioned the need to improving coordination between the sectors, with a dedicated head of climate change and health.
Intersectoral body and there should be one decision maker. So now, everybody is like the leader in the particular sector, but if they need the support from other one, that coordination may be lacking… There won't be any one dedicated person for the climate change. So they will be in charge of multiple departments. For example, somebody’s going to be in charge of immunization or the child health. So their priority will be child health obviously. #3, Medical doctor/academic.
Educational and informational barriers
Gaps in climate change and health in higher education curricula
One of the strongest emergent themes, referred to by most participants, was the need for environmental health education, either by incorporating climate change in the health curriculum or health impacts of climate change in the environmental curriculum in universities and schools. The prevalent feeling was the source of climate change and health literacy needs to be from multiple sources, with formal education being the most important one. Most participants also felt that at present there was a disconnect between environmental and health education, as a result of which there was a relatively low level of awareness on climate change impacts on health.
Education system need to be addressed from beginning… Even the medical college students who are completing five years courses, I do not see any syllabus which contains impact on health by the climate change even though it is very important…my son is studying medical-medicine, but I guess I just go through the syllabus, but nothing is there. #8, Environmentalist.
All the environmentalists professed to never having specifically studied health impacts of climate change during the course of their education. On the other hand, the health professionals expressed incongruent views on climate change-health education. While one mentioned having studied climate sensitive diseases in medical school, another denied ever having been taught the link between climate change and various diseases.
Continuing education courses specific for health impacts of climate change were suggested by a few participants as potential options to bridge the gap between the environment and health. Two participants also suggested including short courses on this topic for all people working on topics related to climate change, health, adaptation and resilience.
Weakness in intersectoral information dissemination
Many of the participants mentioned having little to no awareness on climate change-health related research unless actively searching for it, pointing to the scope for improving related education and science dissemination, especially among the scientific community. Environmental risk factors were not commonly associated with health inherently, partially attributed the low scientific exposure on the topic.
CVDs were seen as a ‘silent’ disease, with many people are not trained to look for symptoms, much less correlate them to weather conditions, all suggesting the need for improved CVD literacy and awareness on the topic. On the other hand, many participants were open to changing theirs current schools of thought on risk factors for health to include climate change, conditional to being informed by global research on the topic.
If there is research or it’s already proven in other countries, ’so this is a risk factor it is a good idea to add’ but [before adding anything], I think some data or there should be some routine surveillance or monitoring system should be there. … even within the medical circle, people may not be aware how much is the contribution of climate change to the heart disease or for any disease for that case… I don't think our administrators or even our clinicians are that much thinking about the impact of climate change, and [heart disease]. #3, Medical doctor/academic.
Scepticism and low awareness on non-conventional health impacts of climate change
As alluded to previously, health impacts of climate change are often not explicit, making it a challenge to research or focus the research agenda on for several reasons. One participant described how the slow pace of climate impacts leads people to think it will not immediately affect health, unless the impacts are drastic.
…The problem has to become so severe, like you have air pollution in Delhi, then people will act. Climate change affects the life slowly it’s not drastic… that is one of the reasons I feel. And slowly if you get some data and keep on generating awareness not only among the public, but also within the scientific community, then slowly things will be better. #3, Medical doctor/academic.
For researchers, an additional challenge of convincing funders or collaborators on the health impacts of climate change also emerged. One participant described the difficulty researchers had separating environmental risks from other common health risk factors. Scepticism when attempting to research health impacts of climate change was also encountered. Confounding from other risk factors and potential ecological bias was seen as the roots of this uncertainty.
Maybe for six, seven years, I have been trying to do some work on climate change and environmental health. Every time I write a proposal I'm criticized largely telling that "how is it going to work?… And one other problem I see with the research with climate change or any environmental thing, it’s ecological effects. So people ask “how can you attribute this to only this, why not to this?“, " Why not to lifestyle, why only to climate change?” So this direct relationship is not there. #4, Medical doctor/ academic.
Diseases such as malaria, with historical links to stagnant water as breeding grounds, have been etched into public knowledge and further perpetrated through mass awareness campaigns, intervention programmes and research. The slow developing nature of CVDs and the prevalent categorisation of CVDs as solely lifestyle diseases was mentioned by many participants as potential barriers to research. One participant described how CVDs are commonly reduced to lifestyle diseases with the onus of risk management on the individual rather than a “willingness to see the invisible factors”. The multifactorial nature of CVDs was thought to add to the difficulty of identifying climate attributable impacts. Another participant described how clinicians especially do not see the need to focus on environmental risk factors for CVDs, believing it ineffective in reducing the overall burden.
Non-communicable diseases, because we are not quantifying that and because of the long latent period of the incident, you're not able to quantify directly to environment or climate change. So definitely, hypertension, cardiovascular disease, all these probably diabetes also because of the changing food pattern, but I don't think—you cannot separate climate change from any of the health effects or any of the non-communicable diseases. Also related to stress caused by climate change. #2, Medical doctor/ academic.
The need for regional studies was also stressed on as there seemed likely to be a disconnect in comparing national-level or global-level problems with health impacts of climate change on a local level. Participants described the attitude of “this does not affect us” among the public when it came to climate change especially. A few participants expressed belief and hope that the temperature-CVD association was an upcoming topic of interest for the government and public alike.
Technical barriers to research
Insufficient resources and workforce dedicated to research
Resource allocation, especially financial, for climate change-health research was described as a barrier, especially by researchers. Along with inconsistent funding from the government, one of the problems mentioned was lack of adequate trained personnel. This was partially linked to the need to relieve the research expectations from already overburdened doctors. There was also a need to have trained personnel for digitalisation and categorisation of health data in order to create a digital state-level health database.
Some participants, referred to the low percentage of the annual budget of India allocated to health along with the need to increase this. One participant described funds earmarked for climate change-health research institutionally, along with optimism that this would lead to future research opportunities.
Yes, for recent years even ICMR (Indian Council of Medical Research) has called for proposals on this environment related, uh, this one. ICMR is one of the largest body which is for the research organisation as well as for the academic institutes like us. So, clearly, they are given a separate block of funding for climate change and [health]. That means the funds are available. #3, Medical doctor/academic.
However, this was countered by the notion that most of the funds are directed to central government institutes as opposed to smaller research institutes. A participant also alluded to misappropriation of research funding at an institutional level. Another participant spoke about the need to involve university students in research along with concern that most students do not get access to funding or research opportunities. There was a feeling that most students remain unaware of opportunities for funding or that funds do not ultimately reach the students aiming to conduct research. Another participant also described the prioritisation of more immediate health burdens and curative research as opposed to preventative research for the directing of funds or resources. This was supported by the opinion expressed by an environmentalist on climate change being viewed as a problem for the future as opposed to the present.
So though we focus on vaccination and other things, but still, the budget still flows more for the curative aspects rather than the preventive part. So for instance, the climate change is more of like, you prevent this—the future heart attacks or some other diseases. You have to focus on the prevention. #3, Medical doctor/academic.
Underdeveloped transdisciplinary research capacity
Alongside education, the need to build more technical capacity among researchers was also mentioned as one of the biggest challenges by participants. Despite a potential interest and willingness from researchers, the lack of training and expertise in climate change-health research was strongly expressed. This was tied in with the expressed desire for mentorship, both to facilitate increased awareness among the scientific and medical community as well as increased regional research on health impacts of climate change.
Yeah, more than research, I would tell it as people are aware and willing to do it, but here is more of capacity building… Let’s say if I want to work on vector-borne disease, I know who to approach…but when it comes to climate change, that linking is absent. … So actually, even if I'm interested and I want to work on it, there are a lot of hurdles which have to be crossed… So I have to be given an opportunity to work on it, or I feel somebody has to mentor me to work on it. So what we call as, starting trouble, you know is there. Once I think somebody starts, we will be going into it…. #4, Medical doctor/ academic.
Some participants had the belief that larger research institutes or relevant ministries could be drafted to provide training to the smaller educational institutes or local government bodies. There was a sense of “duty” attached to studying all aspects of climate change impacts for the environmentalists in Puducherry tied in with a search for a starting point.
Research slowed by unavailability and limited access to quality data
Participants described critical gaps in monitoring, surveillance and database development, all of which were perceived to hamper research conduction, especially for health data. First, merging health data from the many healthcare facilities within Puducherry was seen as a challenge. There was an expressed need to bring together health data for the entire UT in a single system, including public and private healthcare facilities.
Second, some participants mentioned the state-level government health-monitoring database. However, participants described this as being limited to selected diseases from all the government run primary healthcare centres, with limited information on the private sector or secondary and tertiary care hospitals. A few participants described the lack of disease-specific categorisation of health outcomes, making it an added challenge in conducting health-related research.
Third, participants also perceived private medical colleges and healthcare facilities as reluctant to share data with the government, with a felt need to enhance governmental efforts to work on the state-wide database. Fourth, on a related note, concerns about data quality were mentioned by several participants. Part of the reason for an unwillingness to share data by healthcare facilities was thought to be due to potentially inaccurate or poor quality data.
They're all afraid of like somebody will find a fault with that. So because they don't have manpower to look at the accurate or clean the data, okay, so somebody shares and later they find their mistake, and they will be answerable to the higher authority. So that’s the usual reason we do not to share the data, the insecurity. #3, Medical doctor/academic.
Another challenge shared was the slow, ongoing effort to digitalise the data. Participants described as feeling unmotivated to start research at the cost of manually sorting through thousands of paper records, unless there was a way to guarantee research output. This was also relate to a challenge of medical professionals being overburdened with work.
There is not even a digitalization… Many hospital doesn't have digitalized MRD [medical records department]. For example, I was doing a study, retrospective study, collecting infective endocarditis data for past 10 years, there are more than 1000 files. How can I go through the 1000 files? It’s not possible. #13, Practicing physician.
Surveillance of diseases was mentioned as ongoing work. Diabetes, hypertension, cervical cancer and other ‘notifiable’ diseases like infectious diseases were described as being under surveillance.
Discussion
This research examined barriers faced in conducting climate change and health research by key stakeholders in Puducherry. The localised findings relatively remain relevant for India and can be extrapolated to other LMIC settings.28 Four main themes emerged from this research, which are discussed below.
First, we found limited knowledge of relevant policies, especially among the participants with a medical background. In recent years, there have been a lot of strides taken in the Indian policy space with pertaining to climate change and health, such as the addition of the Health Pillar to the NAPCC and the subsequent development of the NAPCCHH and mandates for the development of the state-level action plans for climate change and health.17 18 Although the Health Pillar is a relatively recent addition (2015), there was still a substantial lack of awareness on the NAPCC as well as the health mission in general, which we present as a key area for strengthening. Knowledge of such policies, especially if they can provide a framework to support-related research, is a useful tool to advance the research agenda on climate change and health.36 37 Health system vulnerabilities are already being seen in Puducherry and active knowledge of such policies can also be used by relevant stakeholders to develop resilience focused interventions. This includes communicating the severity of the problem to the policy-makers, who generally lack the political will to divert resources to non-apparent problems, alluded to by the participants in this study and identified in other studies.38 39
Second, participants perceived climate change and health as a topic lacking political support and prioritisation. Most political efforts are thought to be focused on mitigation measures such as air pollution control, with little importance given to health adaptation and healthcare resilience. The participants believed that the health impacts of climate change were not a political priority or seen as urgent. Similar findings have been elucidated in other studies which also found public health leadership on climate change to be fragmented.27 40 Further efforts to inform the decision-makers on the importance of health adaptation might contribute to more evidence informed climate change and health policies.41 42 As an added justification for health cobenefits of mitigation can be introduced through multiple pathways, including air pollution, lifestyle modification, health surveillance or research programmes in development or related policies.43 44
Participants also highlighted weaknesses in interdepartmental coordination for working on climate change and health. We found almost unanimous support for a separate intersectoral body focused specifically on climate change and health. Methodological challenges in the light of limited technical knowledge and adequate intersectorial coordination and support for transdisciplinary capacity that we found have also been reported elsewhere.29 45 A recent study on the knowledge, attitudes and practices related to climate change and health among the Indian health workforce found intermediate or delayed health impacts of climate change less commonly identified.26 This could also support the development of regional, national or even international research networks facilitating knowledge sharing and transfer, including research methodology support.29
The siloed operations of ‘health’ and ‘climate change’ were also seen as a research barrier. This was partially due to the unclear division of responsibilities and fragmented institutional focus, as also seen in other studies.29 40 46 A study examining the challenges for the Californian public health sector in climate change found the compartmentalisation and lack of intersectorial coordination to limit work on intersectoral issues such as climate change and health.27 Our findings point to the need to have regular national level conferences or improved science dissemination systems to communicate climate adaptation related research or plans between and across sectors.
Third, participants perceived gaps in formal education and training on climate change and health. Our respondents had varied views regarding education on climate change or its health impacts; however, the need to improve this was clearly described by participants in this study. The need for strengthening capacity and education has been a common finding in several other studies. Globally, there is a critical gap and scope for improvement in the education on health impacts of climate change, especially for medical practitioners.25 27 47–54 A study comparing medical curriculums across the world found inconsistencies between environmental changes, health and community needs, with Indian and Chinese students especially having a gap in the inclusion of planetary health in medical schools.50 The inclusion of planetary health from an early stage for medical students leads to a more active role of physicians in educating their patients about climate risks.50 55 However, there is a need to validate the results in future studies given the inconsistencies in the views we found on climate change-health education. The emphasis on cure rather that prevention, which has shown to reduce long-term healthcare costs, could support the need for Puducherry to focus on the preventative aspects, largely through education and awareness.24 We also found scepticism and low awareness on the non-conventional health impacts of climate change, such as CVDs. These health impacts were thought to be viewed as ‘invisible’ compared with more conventional or immediate impacts, such as air pollution or extreme events. This is also a commonly identified challenge to climate change and health research, accompanied by insufficient education about climate systems during the course of school or university education.26 56
Fourth, technical research barriers we found included insufficient data, capacity, human and financial resources. Data barriers remain common challenges in public health research, despite efforts to facilitate improvements.57 58 As Puducherry has the advantage of a relatively small size and well-connected healthcare facilities, efforts need to be taken to improve a central, disease-specific data collection system, incorporating all the healthcare facilities in the state.59 Facilitating training to build local data analysis expertise and capacity would contribute to more region specific research on the topic.60 As was also made apparent in this study, other studies have shown that health impacts of climate change are a relatively new concept and not inherently associated with climate, potentially explaining the uncertainties and scepticism expressed by our participants, especially for diseases that do not warrant a visit to the doctor.61 62 On the positive side, the expressed desire of participants to learn more about it and make changes to the healthcare system and policies based on robust, conclusive evidence implies a willingness to adapt and implement changes in how the region tackles health impacts of climate change.49 63 Resource and funding constraints are one of the most common barriers to public health research, especially in LMICs and there remains a critical need to address this gap.64
At present, little is known on CVD impacts of climate change in India. Our related study from Puducherry found a high attributable burden of non-optimal temperature to CVD mortality, suggesting a need for similar studies from around the country.65 66 The CVD-specific challenges we identified here are comparable to the general health challenges. Awareness among the medical community on the environmental risk factors of CVDs will be instrumental in furthering this research agenda, while awareness among policy-makers will help raise the political prioritisation of CVD impacts of climate change.24 67 68
Limitations
First, the sample was restricted to Puducherry district and not representative of the entire Union Territory of Puducherry, much less India as a whole, although the projected population for Puducherry is 1.25 million in 2021, comparable to a few smaller countries or global regions.69 The results might thus only reflect the studied context and participants. Second, while we chose to focus on the medical community and DSTE representatives working on climate change, we did not include the experiences and perspectives of other public health professionals or stakeholders. Third, we do not highlight the opportunities for increasing research on climate change and health as many of these are very often interconnected with barriers. However, we do discuss potential recommendations given by stakeholders. Nonetheless, the results of this study could be useful for the research community and policy-makers alike to strengthen climate change and health research and engagement.
Conclusion
There is a great need to fill the gap in research on the impacts of climate change on various health outcomes in India, especially in light of the vulnerabilities it faces. By highlighting some crucial barriers to environmental health research faced by relevant professionals, we present potential intervention points for consideration. Insufficient awareness on health impacts of climate change and perceived need to improve research capacity through collaborative work; and challenges in data availability emerged as the largest barriers to conducting research on this topic in Puducherry. We outlined the gaps and scope for addressing these through improved policy awareness; informed leadership and evidence informed climate change and health policies; research capacity strengthening and transdisciplinary research and communication network; improved education on climate change and health on all levels; and addressing data barriers in climate change through improved monitoring and evaluation systems. The key findings could contribute to supporting and strengthening evidence-informed climate resilient healthcare systems. In addition, it would also serve to inform and strengthen the research and institutional support for environmental health research in the future both in India and globally.
Supplementary Material
Acknowledgments
The authors would like to extend their sincere gratitude to all the participants who made this study possible.
Footnotes
Contributors: SS, MR, MAD, JU and GC conceptualised and planned the study. SS and RL acquired and provided access to the data. RL facilitated the interviews. SM and SS designed the study. TTL validated the codes and codebook. OC, SS and SM conceptualised and structured the framework. SS wrote the main manuscript with inputs from all authors. The final manuscript has been revised by all authors.GC and SS are the guarantors of this study.
Funding: SS has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No 801076, through the SSPH+ Global PhD Fellowship Programme in Public Health Sciences (GlobalP3HS) of the Swiss School of Public Health and from the Joint South Africa and Swiss Chair in Global Environmental Health. OC has been funded by the Swiss Government Excellence Scholarship (ESKAS) (reference no. 2020 0742).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. All data relevant to the study are included in the article or uploaded as supplementary information. All relevant data from this study have been included in the Supplementary material. As this is a qualitative study with a small number of key informants, making the full dataset and interview transcripts available to a wider audience could potentially breach the confidentiality commitment made to the participants during the process of obtaining informed consent as well as to the ethics committees that approved this study. Therefore, these data will not be made available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the Institute Ethics Committee (Human Studies) of the Indira Gandhi Medical College and Research Institute (A Government of Puducherry Institution); No. 318/IEC-31/IGM&RI/PP/2021 and by the Ethics Committee Northwest and Central Switzerland; Statement ID- AO_2020_00034. The methodology used in this project abided by the principles laid out in the Declaration of Helsinki and the Consolidated criteria for Reporting Qualitative research checklist. All participants were verbally explained the project and its objectives as well as being provided information sheets. All participants were made aware of their right to refuse participation at any point prior to publication of the study. Signed informed consent was obtained from all participants prior to the interviews, with participants retaining one copy.
References
- 1. Rocque RJ, Beaudoin C, Ndjaboue R, et al. Health effects of climate change: an overview of systematic reviews. BMJ Open 2021;11:e046333. 10.1136/bmjopen-2020-046333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cissé G, McLeman R, Adams H, et al. health, wellbeing, and the changing structure ofCommunities . In: Pörtner D-O, Tignor M, Poloczanska ES, et al., eds. Climate Change 2022: Impacts,Adaptation andVulnerability. Contribution of Working Group II to the Sixth Assessment Reportof the Intergovernmental Panel on Climate Change. Cambridge, UK and New York, NY, USA: IPCC, 2022: 1041–170. 10.1017/9781009325844 [DOI] [Google Scholar]
- 3. WHO . Climate change and health. fact sheets. 2021. Available: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health
- 4. Patz JA, Campbell-Lendrum D, Holloway T, et al. Impact of regional climate change on human health. Nature 2005;438:310–7. 10.1038/nature04188 [DOI] [PubMed] [Google Scholar]
- 5. Watts N, Amann M, Arnell N, et al. The 2020 report of the lancet Countdown on health and climate change: responding to converging crises. Lancet 2021;397:129–70. 10.1016/S0140-6736(20)32290-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cissé G. Food-borne and water-borne diseases under climate change in Low- and middle-income countries: further efforts needed for reducing environmental health exposure risks. Acta Trop 2019;194:181–8. 10.1016/j.actatropica.2019.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rocha J. Climate change and its impacts on health, environment and economy, in One Health. Elsevier, 2022: 253–79. [Google Scholar]
- 8. Wise RM, Fazey I, Stafford Smith M, et al. Reconceptualising adaptation to climate change as part of pathways of change and response. Global Environmental Change 2014;28:325–36. 10.1016/j.gloenvcha.2013.12.002 [DOI] [Google Scholar]
- 9. Haines A, Ebi KL, Smith KR, et al. Health risks of climate change: act now or pay later. Lancet 2014;384:1073–5. 10.1016/S0140-6736(14)61659-7 [DOI] [PubMed] [Google Scholar]
- 10. Kjellstrom T. Climate change, direct heat exposure, health and well-being in low and middle-income countries. Glob Health Action 2009;2:2. 10.3402/gha.v2i0.1958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Scheelbeek PFD, Dangour AD, Jarmul S, et al. The effects on public health of climate change adaptation responses: a systematic review of evidence from Low- and middle-income countries. Environ Res Lett 2021;16:073001. 10.1088/1748-9326/ac092c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ebi KL, Kovats RS, Menne B. An approach for assessing human health vulnerability and public health interventions to adapt to climate change. Environ Health Perspect 2006;114:1930–4. 10.1289/ehp.8430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gioli G, Khan T, Scheffran J. Climatic and environmental change in the Karakoram: making sense of community perceptions and adaptation strategies. Reg Environ Change 2014;14:1151–62. 10.1007/s10113-013-0550-3 [DOI] [Google Scholar]
- 14. Tripathi V, Akhtar R, Preetha GS. Perceptions regarding climate change and its health impact: reflections from a community-based study in India. Indian J Community Med 2021;46:206–9. 10.4103/ijcm.IJCM_120_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nayak S, Takemi T. Assessing the impact of climate change on temperature and precipitation over India. In: Sumi T, Kantoush SA, Saber M, eds. Wadi Flash Floods, Natural Disaster Science and Mitigation Engineering: DPRI reports., T. Singapore, 2022. 10.1007/978-981-16-2904-4 [DOI] [Google Scholar]
- 16. Dagdeviren H, Elangovan A, Parimalavalli R. Climate change, monsoon failures and inequality of impacts in South India. J Environ Manage 2021;299:S0301-4797(21)01617-0. 10.1016/j.jenvman.2021.113555 [DOI] [PubMed] [Google Scholar]
- 17. National Action Plan for Climate Change and Human Health, G.o.I . Ministry of Health and Family Welfare. 2018. [Google Scholar]
- 18. GOI, G.o.I . India’s national action plan on climate change. 2009. [DOI] [PMC free article] [PubMed]
- 19. Bush KF, Luber G, Kotha SR, et al. Impacts of climate change on public health in India: future research directions. Environ Health Perspect 2011;119:765–70. 10.1289/ehp.1003000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Singh PK, Dhiman RC. Climate change and human health: Indian context. J Vector Borne Dis 2012;49:55–60.:55. [PubMed] [Google Scholar]
- 21. Gill M, Stott R. Health professionals must act to tackle climate change. Lancet 2009;374:1953–5. 10.1016/S0140-6736(09)61830-4 [DOI] [PubMed] [Google Scholar]
- 22. Roberts I, Stott R, Climate and Health Council executive . Doctors and climate change. BMJ 2010;341:bmj.c6357. 10.1136/bmj.c6357 [DOI] [PubMed] [Google Scholar]
- 23. Moser AM, Stigler FL, Haditsch B. Physicians' responsibility for planetary health. Lancet Planet Health 2017;1:S2542-5196(17)30023-2. 10.1016/S2542-5196(17)30023-2 [DOI] [PubMed] [Google Scholar]
- 24. Sainsbury P, Charlesworth K, Madden L, et al. Climate change is a health issue: what can doctors do. Intern Med J 2019;49:1044–8. 10.1111/imj.14380 [DOI] [PubMed] [Google Scholar]
- 25. Hathaway J, Maibach EW. Health implications of climate change: a review of the literature about the perception of the public and health professionals. Curr Environ Health Rep 2018;5:197–204. 10.1007/s40572-018-0190-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sambath V, Narayan S, Kumar P, et al. Adithya Pradyumna, knowledge, attitudes and practices related to climate change and its health aspects among the Healthcare workforce in India – A cross-sectional study. J Climate Change Health 2022;6:100147. 10.1016/j.joclim.2022.100147 [DOI] [Google Scholar]
- 27. Gould S, Rudolph L. Challenges and opportunities for advancing work on climate change and public health. Int J Environ Res Public Health 2015;12:15649–72. 10.3390/ijerph121215010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mallen E, Joseph HA, McLaughlin M, et al. Overcoming barriers to successful climate and health adaptation practice: notes from the field. Int J Environ Res Public Health 2022;19:7169. 10.3390/ijerph19127169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Leal Filho W, Morgan EA, Godoy ES, et al. Implementing climate change research at universities: barriers, potential and actions. Journal of Cleaner Production 2018;170:269–77. 10.1016/j.jclepro.2017.09.105 [DOI] [Google Scholar]
- 30. GOI . Census of India- Puducherry. Government of India, 2011. [Google Scholar]
- 31. DTEE . Puducherry Climate Change Cell. Available: https://dste.py.gov.in/PCCC/PCCC_Projects.html [Google Scholar]
- 32. Shrikhande SS, Merten S, Cambaco O, et al. Climate change and health?”: knowledge and perceptions among key Stakeholders in Puducherry, India. Int J Environ Res Public Health 2023;20:4703. 10.3390/ijerph20064703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gale NK, Heath G, Cameron E, et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13:117. 10.1186/1471-2288-13-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. van Eck CW, Mulder BC, van der Linden S. Climate change risk perceptions of audiences in the climate change Blogosphere. Sustainability 2020;12:7990. 10.3390/su12197990 [DOI] [Google Scholar]
- 35. Rudolph L, Gould S. Climate change and health inequities: A framework for action. Ann Glob Health 2015;81:432–44. 10.1016/j.aogh.2015.06.003 [DOI] [PubMed] [Google Scholar]
- 36. Crouzat E, Arpin I, Brunet L, et al. Researchers must be aware of their roles at the interface of Ecosystem services science and policy. Ambio 2018;47:97–105. 10.1007/s13280-017-0939-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. van Valkengoed AM, Perlaviciute G, Steg L. Relationships between climate change perceptions and climate adaptation actions: policy support, information seeking, and behaviour. Climatic Change 2022;171. 10.1007/s10584-022-03338-7 [DOI] [Google Scholar]
- 38. Hussey LK, Arku G. Conceptualizations of climate-related health risks among health experts and the public in Ghana. Soc Sci Med 2019;223:40–50. 10.1016/j.socscimed.2019.01.026 [DOI] [PubMed] [Google Scholar]
- 39. Austin SE, Ford JD, Berrang-Ford L, et al. Enabling local public health adaptation to climate change. Soc Sci Med 2019;220:236–44. 10.1016/j.socscimed.2018.11.002 [DOI] [PubMed] [Google Scholar]
- 40. Biesbroek R, Klostermann J, Termeer C, et al. Barriers to climate change adaptation in the Netherlands. Clim Law 2011;2:181–99. 10.1163/CL-2011-033 [DOI] [Google Scholar]
- 41. Oxman AD, Lewin S, Lavis JN, et al. SUPPORT tools for evidence-informed health policymaking (STP) 15: engaging the public in evidence-informed policymaking. Health Res Policy Sys 2009;7:1–9. 10.1186/1478-4505-7-S1-S15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Uzochukwu B, Onwujekwe O, Mbachu C, et al. The challenge of bridging the gap between researchers and policy makers: experiences of a health policy research group in engaging policy makers to support evidence informed policy making in Nigeria. Global Health 2016;12:67. 10.1186/s12992-016-0209-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Haines A. Health Co-benefits of climate action. Lancet Planetary Health 2017;1:e4–5. 10.1016/S2542-5196(17)30003-7 [DOI] [PubMed] [Google Scholar]
- 44. Haines A, McMichael AJ, Smith KR, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: overview and implications for policy makers. The Lancet 2009;374:2104–14. 10.1016/S0140-6736(09)61759-1 [DOI] [PubMed] [Google Scholar]
- 45. Xun WW, Khan AE, Michael E, et al. Climate change epidemiology: methodological challenges. Int J Public Health 2010;55:85–96. 10.1007/s00038-009-0091-1 [DOI] [PubMed] [Google Scholar]
- 46. Eisenack K, Moser SC, Hoffmann E, et al. Explaining and overcoming barriers to climate change adaptation. Nature Clim Change 2014;4:867–72. 10.1038/nclimate2350 [DOI] [Google Scholar]
- 47. Yang L, Liao W, Liu C, et al. Associations between knowledge of the causes and perceived impacts of climate change: A cross-sectional survey of medical, public health and nursing students in universities in China. Int J Environ Res Public Health 2018;15:2650. 10.3390/ijerph15122650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kotcher J, Maibach E, Miller J, et al. Views of health professionals on climate change and health: a multinational survey study. Lancet Planet Health 2021;5:e316–23. 10.1016/S2542-5196(21)00053-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Corner A. PSYCHOLOGY science literacy and climate views. Nature Clim Change 2012;2:710–1. 10.1038/nclimate1700 [DOI] [Google Scholar]
- 50. Omrani OE, Dafallah A, Paniello Castillo B, et al. Envisioning planetary health in every medical curriculum: an international medical student organization’s perspective. Med Teach 2020;42:1107–11. 10.1080/0142159X.2020.1796949 [DOI] [PubMed] [Google Scholar]
- 51. Whitley CT, Takahashi B, Zwickle A, et al. Sustainability behaviors among college students: an application of the VBN theory. Environmental Education Research 2018;24:245–62. 10.1080/13504622.2016.1250151 [DOI] [Google Scholar]
- 52. Chaplin G, Wyton P. Student engagement with Sustainability: understanding the value-action gap. Int J Sustain High Educat 2014;15:404–17. 10.1108/IJSHE-04-2012-0029 [DOI] [Google Scholar]
- 53. Greibe Andersen J, Karekezi C, Ali Z, et al. Perspectives of local community leaders, health care workers, volunteers, policy makers and academia on climate change related health risks in Mukuru informal settlement in Nairobi, Kenya-A qualitative study. IJERPH 2021;18:12241.:22. 10.3390/ijerph182212241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Eagle L, Low D, Case P, et al. Attitudes of undergraduate business students toward Sustainability issues. Int J Sustainab High Educat 2015;16:650–68. 10.1108/IJSHE-04-2014-0054 [DOI] [Google Scholar]
- 55. Shaman J, Knowlton K. The need for climate and health education. Am J Public Health 2018;108:S66–7. 10.2105/AJPH.2017.304045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. McMichael AJ. Impediments to comprehensive research on climate change and health. Int J Environ Res Public Health 2013;10:6096–105. 10.3390/ijerph10116096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. van Panhuis WG, Paul P, Emerson C, et al. A systematic review of barriers to data sharing in public health. BMC Public Health 2014;14:.:1144. 10.1186/1471-2458-14-1144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lazem M, Sheikhtaheri A. Barriers and Facilitators for disease Registry systems: a mixed-method study. BMC Med Inform Decis Mak 2022;22:97. 10.1186/s12911-022-01840-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Lakshmanasamy Ravivarman PK. A10 medically certified causes of death and risk factors in mortality, Puducherry district, India 2016-19. BMC Proc 2019;15. [Google Scholar]
- 60. Levison MM, Butler AJ, Rebellato S, et al. Development of a climate change vulnerability assessment using a public health lens to determine local health Vulnerabilities: an Ontario health unit experience. Int J Environ Res Public Health 2018;15:2237. 10.3390/ijerph15102237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Valois P, Blouin P, Ouellet C, et al. The health impacts of climate change: A continuing medical education needs assessment framework. J Contin Educ Health Prof 2016;36:218–25. 10.1097/CEH.0000000000000084 [DOI] [PubMed] [Google Scholar]
- 62. Herrmann A, Sauerborn R. General practitioners' perceptions of heat health impacts on the elderly in the face of climate Changea qualitative study in Baden-Wurttemberg, Germany. Int J Environ Res Public Health 2018;15:843. 10.3390/ijerph15050843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Paterson J, Berry P, Ebi K, et al. Health care facilities resilient to climate change impacts. Int J Environ Res Public Health 2014;11:13097–116. 10.3390/ijerph111213097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Shumba CS, Lusambili AM. Not enough Traction: barriers that aspiring researchers from Low- and middle-income countries face in global health research. Journal of Global Health Economics and Policy 2021;1:1. 10.52872/001c.25802 [DOI] [Google Scholar]
- 65. Shrikhande SS, Pedder H, Röösli M, et al. Non-optimal apparent temperature and cardiovascular mortality: the association in puducherry, india between 2010 and 2020. In Review [Preprint] 2022. 10.21203/rs.3.rs-1697787/v1 [DOI] [PMC free article] [PubMed]
- 66. Bhatia M, Dixit P, Kumar M, et al. Impending epidemic of cardiovascular diseases among lower socioeconomic groups in India. Lancet Healthy Longev 2021;2:e314–5. 10.1016/S2666-7568(21)00080-5 [DOI] [PubMed] [Google Scholar]
- 67. Sheffield PE, Durante KT, Rahona E, et al. Emerging roles of health care providers to mitigate climate change impacts: A perspective from East Harlem, New York. Health Hum Rights 2014;16:113–21. [PMC free article] [PubMed] [Google Scholar]
- 68. Dupraz J, Burnand B. Role of health professionals regarding the impact of climate change on health-an exploratory review. Int J Environ Res Public Health 2021;18:3222. 10.3390/ijerph18063222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. GovernmentOfPuducherry . About Puducherry District, Available: https://puducherry-dt.gov.in/history
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-073381supp001.pdf (224.4KB, pdf)
Data Availability Statement
No data are available. All data relevant to the study are included in the article or uploaded as supplementary information. All relevant data from this study have been included in the Supplementary material. As this is a qualitative study with a small number of key informants, making the full dataset and interview transcripts available to a wider audience could potentially breach the confidentiality commitment made to the participants during the process of obtaining informed consent as well as to the ethics committees that approved this study. Therefore, these data will not be made available.