Abstract
Background
Clinical benefit of molnupiravir (MPV) in coronavirus disease 2019 (COVID-19)–infected subpopulations is unclear.
Methods
We used a matched cohort study design to determine the rate of hospitalization or death within 30 days of COVID-19 diagnosis among MPV treated and untreated controls. Participants were nonhospitalized, previously uninfected Veterans with a first confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection between 1 January and 31 August 2022, who were prescribed MPV within 3 days of COVID-19 diagnosis, and matched individuals who were not prescribed MPV.
Results
Among 1459 matched pairs, the incidence of hospitalization/death was not different among MPV treated versus untreated controls (48 vs 44 cases; absolute risk difference [ARD], 0.27; 95% confidence interval [CI], −.94 to 1.49). No benefit was observed among those >60 or ≤60 years old (ARD, 0.27; 95% CI, −1.25 to 1.79 vs ARD, −0.29; 95% CI, −1.22 to 1.80), those with specific comorbidities, or by vaccination status. A significant benefit was observed in asymptomatic but not in symptomatic persons (ARD, −2.80; 95% CI, −4.74 to −.87 vs ARD, 1.12; 95% CI −.31 to 2.55). Kaplan-Meier curves did not show a difference in proportion of persons who were hospitalized or died among MPV treated compared with untreated controls (logrank P = .7).
Conclusions
MPV was not associated with a reduction in hospitalization or death within 30 days of COVID-19 diagnosis. A subgroup of patients presenting without symptoms experienced a benefit.
Keywords: COVID-19, SARS-CoV-2, death, hospitalization, molnupiravir
In previously uninfected, nonhospitalized, high-risk persons with COVID-19, molnupiravir use is not associated with a significant reduction in hospitalization or death within 30 days of COVID-19 diagnosis. A subgroup of patients presenting without symptoms might experience a benefit.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the resultant coronavirus disease 2019 (COVID-19) remain a major global concern over 3 years after the first cases were reported. Vaccination is by far the most important strategy in reducing the burden of disease with current vaccines providing high level of protection against severe or critical disease [1–8]. However, immunity wanes over time [9] and breakthrough infections among fully vaccinated persons have been reported [10–14]. Previous therapeutic agents, including convalescent plasma [15], interleukin 6 (IL-6) blockers [16–18], remdesivir [19, 20], monoclonal antibodies [21–24], and systemic corticosteroids [25], among others, have shown modest benefits in clinical outcomes, often in select subgroups of patients. In December 2021, 2 novel oral antiviral agents, nirmatrelvir/ritonavir (NMV/r) and molnupiravir (MPV), were granted emergency use authorization by the Food and Drug Administration for treatment of early symptomatic patients with mild to moderate COVID-19 at high risk of progression to severe disease [26–29]. While early clinical trials have demonstrated a benefit in clinical outcomes, the effect has not been uniform or experienced by all demographic and clinical subgroups.
In a phase 3 double-blind, randomized, placebo-controlled trial in symptomatic, unvaccinated, nonhospitalized adults with mild to moderate disease who had at least 1 risk factor for disease progression, MPV treatment initiated within 5 days of symptom onset was associated a significant reduction in hospitalization or death by day 29 compared with the placebo group [30]. However, observational and real-world studies have reported mixed results, with some studies demonstrating reduction in the risk of severe disease or death [31, 32], while others have not demonstrated a clear benefit [33, 34]. In a large observational study from Israel including 2661 patients at high risk for severe COVID-19 who received molnupiravir and 2661 propensity score-matched controls, molnupiravir was not associated with a significant reduction in the risk of the severe COVID-19 or COVID-19–specific mortality (hazard ratio, 0.83; 95% confidence interval [CI], .57–1.21). However, in subgroup analyses, older persons and inadequately vaccinated persons experienced a benefit [34]. We undertook this study to determine the effect of MPV treatment upon hospitalization and death in a previously uninfected, nonhospitalized, high-risk population. Because many drugs approved under emergency use authorization may be prescribed to patients who do not meet the specific approval criteria, and because our goal was to determine the effectiveness of MPV in the real-world setting, we used a more inclusive population who received MPV for the treatment of COVID-19 as described in the “Methods” section.
METHODS
Study Setting
Department of Veterans Affairs (VA) created a national COVID-19 Shared Data Resource, which contains detailed demographic, clinical, laboratory, vital status, and episodes-of-care information on all veterans with a laboratory-confirmed diagnosis of SARS-CoV-2 infection and receipt of a SARS-CoV-2 vaccine within the VA. Veterans who are tested or vaccinated outside VA are captured by patient self-report (presentation of a vaccination card) or through insurance claims data. The VA COVID-19 Shared Data Resource is updated regularly with information derived from multiple validated sources [8, 11, 35–37].
Study Population
We used a matched cohort design to emulate a hypothetical target trial closely mimicking a recently published randomized controlled trial, with some changes to reflect the real-world prescription patterns for MPV [30]. This strategy has been used by us and others in previous analyses of the VA COVID-19 Shared Data Resource database [38, 39] (Supplementary Table 1). Eligible individuals were those in the VA COVID-19 Shared Data Resource with at least 2 episodes of care in the VA health care system within the last 2 years, who had a first confirmed SARS-CoV-2 infection between 1 January and 31 August 2022, and were free of an outcome event (hospitalization or death) within 3 days of testing positive. Those who were hospitalized in the 60-days period prior to the index COVID-19 test date were ineligible (to exclude persons at high risk of hospitalization from other causes), as were those who received MPV after diagnosis. While those with no comorbidities were excluded from the previously published randomized controlled trial, we opted to include this population to determine the effectiveness of MPV in a real-world setting.
Among the individuals meeting the eligibility criteria, we matched those who were prescribed MPV within 3 days of COVID-19 diagnosis date with those who were not prescribed MPV. Controls were matched 1:1 on age (5-year blocks), race, sex, body mass index, Charlson Comorbidity Index, VA facility where MPV was prescribed, and vaccination status. Individuals in the control group who were prescribed MPV after the match date and their corresponding matched case were excluded. Those pairs who received the other oral antiviral drug NMV/r after the match date were also removed. Molnupiravir was most frequently prescribed in the usual recommended dose (800 mg every 12 hours), although it should be noted that we did not have the data to measure adherence.
Primary Outcome Measure
Our primary outcome measure was hospitalization or death within 30 days of the index COVID-19 diagnosis date. We allowed a 3-day window from the time of COVID-19 diagnosis to be included in either group. We chose the COVID-19 test date as the reference point because this is more accurately confirmed than the onset of symptoms, which is more subjective and subject to recall bias, and because we also intended to determine the role of MPV in asymptomatic individuals.
Statistical Analysis
We calculated the incidence of hospitalization or admission among the MPV-treated versus the untreated group. Absolute risk difference (ARD) between the 2 groups along with 95% CIs were estimated using logistic regression models fit using generalized estimating equations to account for correlated outcomes within each matched pair [40]. The overall absolute difference between the groups, as well as for various substrata of the population by age, sex, body mass index, presence of various comorbidities, and vaccination status were tabulated and graphed. Kaplan-Meier curves were generated to demonstrate the difference in hospitalization or death over time among those treated with NMV/r and untreated controls. Logrank test was used to calculate P values between groups. A P value of <.05 was considered statistically significant.
Ethical Considerations
The study was approved by the Institutional Review Board at the VA Pittsburgh Healthcare System. A waiver of informed consent was granted for the study.
RESULTS
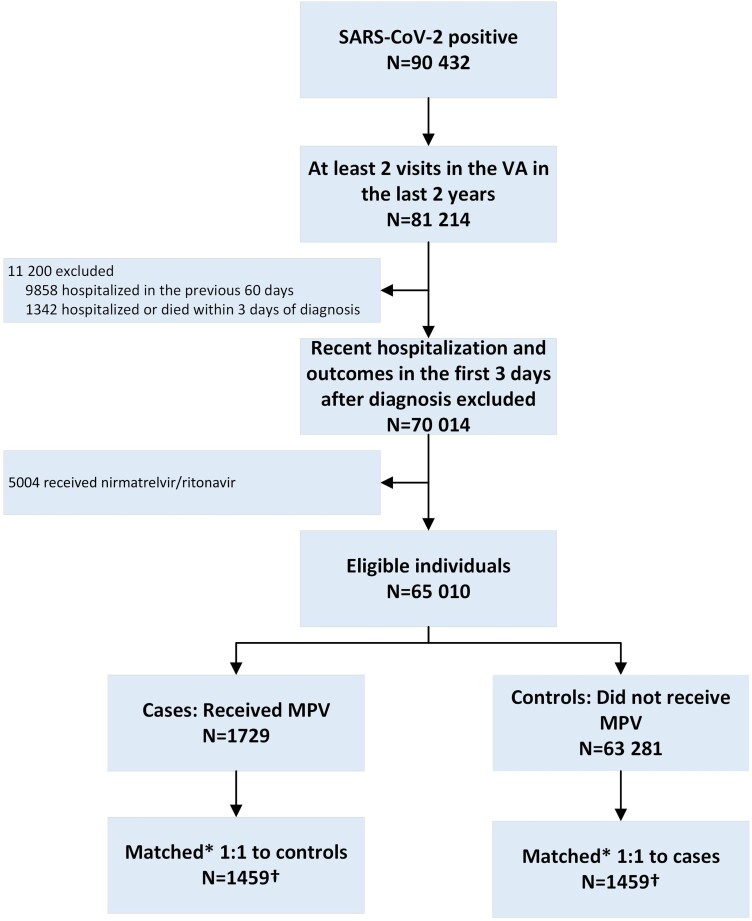
Among 90 432 persons with a confirmed first SARS-CoV-2 positive test between 1 January and 31 August 2022, we identified 65 010 persons who met the eligibility criteria as described above. Of those, 1459 were prescribed MPV and 63 281 were not prescribed MPV. Twenty-six individuals were excluded who started MPV >3 days after the match date and 3 individuals were excluded who started NMV/r during the study period. Corresponding matches for these 29 individuals were also excluded. The final primary analysis dataset included 1459 matched pairs of MPV-treated cases and controls (Figure 1).
Figure 1.
Study flowsheet. *Matched on age (5-year blocks), race, sex, body mass index, Charlson Comorbidity Index, VA station where prescribed, and vaccination status. †Twenty-six individuals and corresponding matches excluded who started MPV >3 days after match date and 3 excluded who started nirmatrelvir/ritonavir during study period. Abbreviations: MPV, molnupiravir; VA, Department of Veterans Affairs health care facility.
Baseline characteristics of the cohort before and after matching are presented in Table 1. After matching, the median age in each group was 69 years, 92% were male, and 20% were black. Mean body mass index was 31 kg/m2, median Charlson Comorbidity Index score was 1, 14% were unvaccinated or had not completed a primary SARS-CoV-2 vaccination series, while 64% had completed a primary series and had received a booster dose of the vaccine. Median number of days from diagnosis to first prescription of MPV was 0 days (interquartile range 0–1), and 82% in the treated group versus 65% in the untreated group were symptomatic at presentation (Table 1).
Table 1.
Baseline Characteristics of the Molnupiravir Analysis Cohort
| Characteristic | Before Matching | Matched Cohort | ||||
|---|---|---|---|---|---|---|
| MPV Group | Controls | P Value | MPV Group | Controls | SMD | |
| n = 1729 | n = 63 281 | n = 1459 | n = 1459 | |||
| Median age, y (IQR) | 69.4 (60.6–75.5) | 57.1 (43.8–68.9) | <.0001 | 69.4 (60.7–75.3) | 69.6 (60.6–75.1) | −0.0014 |
| Male sex, % | 89.71 | 73.01 | <.0001 | 91.84 | 91.84 | 0 |
| Race, % | <.0001 | 0 | ||||
| White | 71.14 | 54.45 | 75.94 | 75.94 | ||
| Black | 21.57 | 19.90 | 20.49 | 20.49 | ||
| Other/unknown | 7.29 | 25.64 | 3.56 | 3.56 | ||
| Body mass index, kg/m2 | ||||||
| Mean (SD) | 30.6 (6.3) | 30.7 (6.6) | .79 | 31.1 (6.3) | 30.9 (6.1) | −0.0333 |
| Body mass index category, % | <.0001 | 0 | ||||
| ≤ 25 | 15.33 | 12.08 | 12.61 | 12.61 | ||
| > 25–30 | 29.84 | 24.23 | 30.23 | 30.23 | ||
| > 30 | 44.65 | 35.63 | 47.98 | 47.98 | ||
| Missing | 10.18 | 28.06 | 9.18 | 9.18 | ||
| Median Charlson Comorbidity Index score (IQR) | 2 (1–4) | 1 (0–2) | <.0001 | 2 (1–4) | 2 (1–4) | 0 |
| Comorbidities at or before baseline, % | ||||||
| Diabetes | 47.95 | 25.21 | <.0001 | 46.06 | 44.69 | −0.0275 |
| Cardiovascular disease | 58.42 | 28.76 | <.0001 | 57.23 | 50.17 | −0.1419 |
| Chronic kidney disease | 26.32 | 10.69 | <.0001 | 23.99 | 21.18 | −0.0672 |
| Chronic lung disease | 27.18 | 13.44 | <.0001 | 26.53 | 24.81 | −0.0392 |
| Cancer diagnosis | 25.04 | 13.48 | <.0001 | 23.92 | 26.39 | 0.0569 |
| Vaccination status at baseline, % | <.0001 | 0 | ||||
| Unvaccinated or primary series incomplete | 14.75 | 42.75 | 14.19 | 14.19 | ||
| Primary series completed | 22.79 | 24.75 | 22.00 | 22.00 | ||
| Primary series plus booster | 62.46 | 32.50 | 63.81 | 63.81 | ||
| Geographical location, % | <.0001 | 0.0921 | ||||
| City/town | 6.48 | 5.17 | 6.72 | 6.58 | ||
| Small town/rural | 5.03 | 3.36 | 5.28 | 3.56 | ||
| Urban | 74.09 | 69.37 | 74.23 | 73.41 | ||
| Unknown | 14.40 | 22.10 | 13.78 | 16.45 | ||
| Median No. of days to first prescription (IQR) | 0 (0–1) | … | 0 (0–1) | … | 0 | |
| Symptomatic at baseline, % | 82.07 | 55.32 | <.0001 | 82.04 | 65.39 | −0.3853 |
| Asymptomatic at baseline, % | 17.93 | 44.68 | <.0001 | 17.96 | 34.61 | 0.3853 |
Abbreviations: IQR, interquartile range; MPV, molnupiravir; SMD, standardized mean difference.
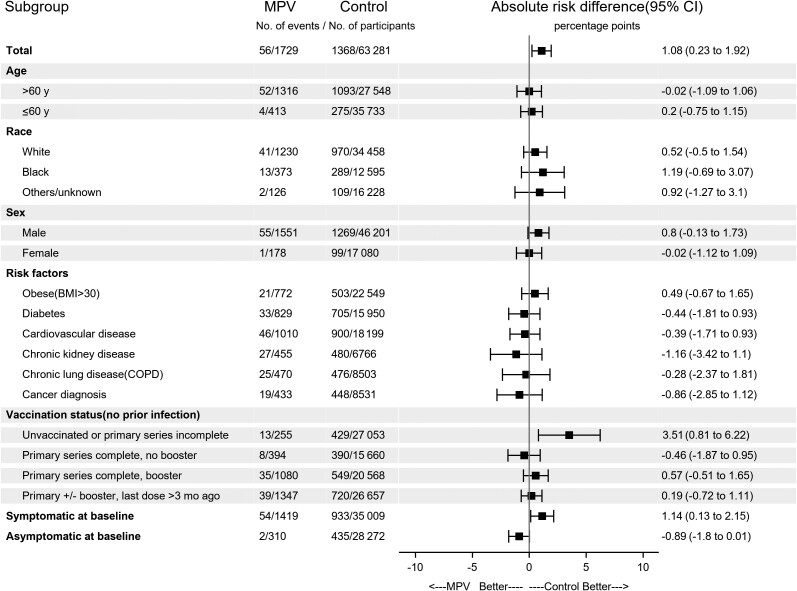
In the unmatched cohorts, a higher incidence of hospitalization or death was observed among those who were prescribed MPV (ARD, 1.08; 95% CI, .23–1.92; Figure 2 and Supplementary Table 2). In the matched groups analysis, the incidence of hospitalization or death was not significantly different among the 2 groups (48 vs 44 events; ARD, −0.27; 95% CI, −.94 to 1.49).
Figure 2.
Incidence of hospitalization or death within 30 days and absolute risk difference among patients who received molnupiravir and controls. Results for the full cohort before matching. Abbreviations: BMI, body mass index; CI, confidence interval; COPD, chronic obstructive pulmonary disease; MPV, molnupiravir.
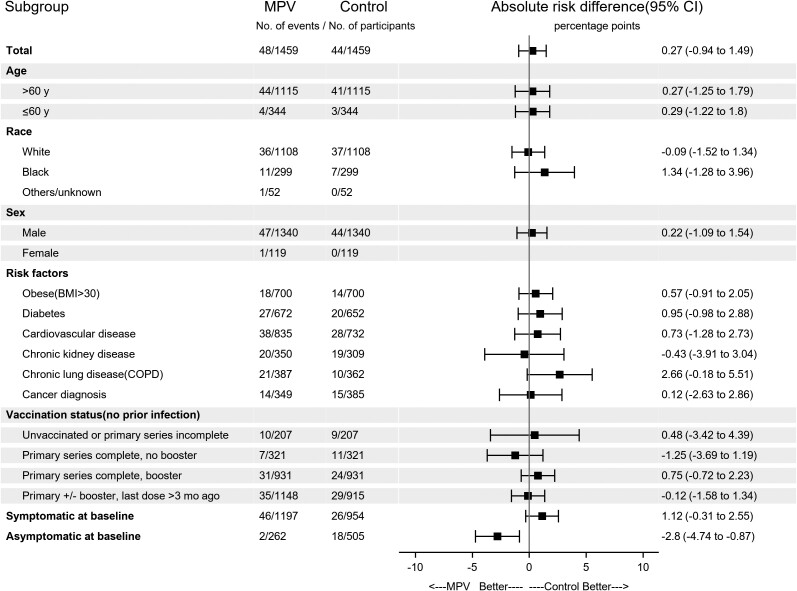
No benefit from MPV treatment was observed among those older than 60 or ≤60 years old (ARD, 0.27; 95% CI, −1.25 to 1.79 vs ARD, 0.29; 95% CI, −1.22 to 1.80). Similarly, no benefit was observed among those prescribed MPV who were unvaccinated/incompletely vaccinated, completed a primary series without a booster dose, or those who had received a booster dose after completing the primary vaccination series. Those with obesity, diabetes mellitus, cardiovascular disease, chronic kidney or lung disease, or a cancer diagnosis who were prescribed MPV also did not experience a benefit. However, a significant benefit was observed among asymptomatic persons who received MPV (ARD, −2.8; 95% CI, −4.74 to −.87) but not among those who were symptomatic at baseline (ARD, 1.12; 95% CI, −.31 to 2.55; Figure 3 and Supplementary Table 3).
Figure 3.
Incidence of hospitalization or death within 30 days and absolute risk difference among patients who received molnupiravir and controls. Results for the matched groups. Abbreviations: BMI, body mass index; CI, confidence interval; COPD, chronic obstructive pulmonary disease; MPV, molnupiravir.
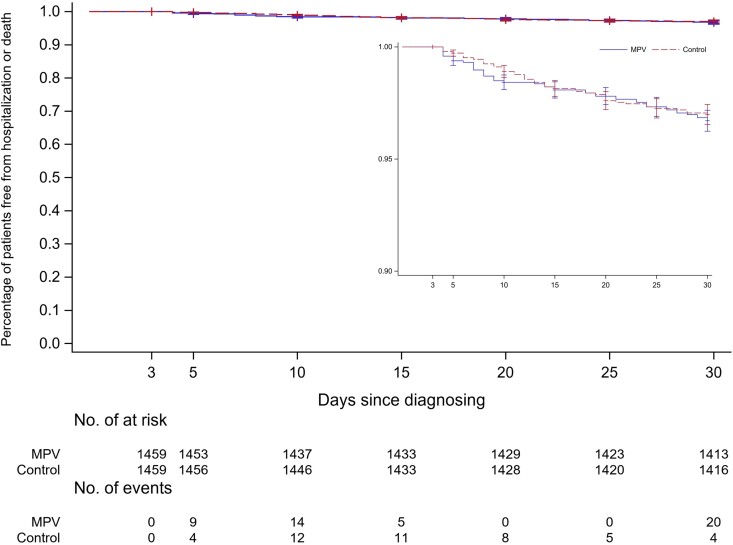
Kaplan-Meier curves did not show a significant reduction in proportion of persons who were hospitalized or died among those treated with MPV compared with untreated controls (logrank P = .7; Figure 4).
Figure 4.
Kaplan-Meier curves depicting percentage of patients without hospitalization or death among those treated with molnupiravir and untreated controls (inset: magnification of the graph to show details). Logrank P = .67. Abbreviation: MPV, molnupiravir.
Additional Analyses
We repeated the entire analyses using a 2-day eligibility period for inclusion after COVID-19 diagnosis (Supplementary Figure 1). Baseline characteristics of this cohort before and after matching are presented in Supplementary Table 4. The incidence of hospitalization or death and ARDs among treated and untreated groups are presented in Supplementary Figure 2 for unmatched groups and Supplementary Figure 3 for the matched groups. Kaplan-Meier curves for this comparison are presented in Supplementary Figure 4. All results were generally similar to our primary analyses.
DISCUSSION
MPV and NMV/r are oral antiviral agents against COVID-19 with demonstrated efficacy in clinical trials in preventing progression to severe disease or death among those with early and mild disease who are at risk of progression to severe disease. In real-world studies, MPV effectiveness has been demonstrated in some, but not all, studies. In our large, real-world study, we did not observe a clear overall benefit in a national, high-risk population except in a subgroup of individuals who were asymptomatic at presentation.
In the full cohort before matching, individuals who received MPV had a greater risk of hospitalization or death compared with those who did not receive MPV. This can be explained by the demographic and clinical characteristics of the overall groups before matching. Those who were prescribed MPV were significantly older, had a much higher burden of comorbidities, and more likely to be symptomatic at presentation. These factors placed them in a much higher risk category for adverse outcomes from COVID-19. In the matched cohort, there was no statistically significant difference in hospitalization or death between the treated and untreated groups. While the groups were well matched on age and comorbidities, a higher proportion of those who were prescribed MPV were symptomatic at presentation. No benefit in outcomes was observed in the symptomatic individuals. On the other hand, asymptomatic individuals who were prescribed MPV experienced a significant reduction in hospitalization or death. This suggests that the benefit from MPV may be limited to those with the mildest form of disease at presentation who are prescribed MPV early in the course of the illness.
Previous studies of MPV have shown mixed results [30–34]. While a randomized clinical trial demonstrated significant overall benefit, subgroup analyses revealed benefit among those with >3 days after symptoms onset, those who were obese, white race, and female [30]. In a larger observational study, no overall benefit was observed; however, in subgroup analyses, only older and inadequately vaccinated individuals experienced a benefit [34]. Our study reaffirms most of the previous findings demonstrating a benefit of MPV only in a subgroup of infected individuals who are asymptomatic at the time of presentation.
Our results have significant policy and practice implications. It is critical to identify the specific populations who will benefit from new treatments for any given disease. With COVID-19, this is particularly important due to the misinformation, disinformation, and early missteps in recommending effective treatment and prevention strategies [41–44]. Our results add to the growing evidence that MPV may be effective only in asymptomatic individuals or mild disease and when given early in the course of illness. Prescribing MPV only to those who may expect a benefit can prevent untoward adverse events and lower the costs of therapy.
Strengths of our study include a large national population at high risk of disease progression, validated data extraction methods and database, a strong study design emulating a target trial, and extensive longitudinal data availability. Certain limitations also need to be noted. While we emulated a target trial, it may still not be equivalent of a randomized clinical trial in balancing confounders. While Veterans are an optimal population for the study question due to the high risk of disease progression, they may not be representative of the general population. Veterans are older and predominantly male and have a higher burden of comorbidities than the general population. There may be some Veterans who sought care outside the VA healthcare system; however, only a small fraction of Veterans are “dual users.” In one study of Veterans requiring multiple hospital admissions, only 3% of those >65 years old and 8% of those <65 years were dual users [45]. We included only those individuals with a first positive COVID-19 test. However, a significant proportion of the population may have had previously undiagnosed infection, particularly those who were asymptomatic. We were unable to assess previously undiagnosed infection and its impact on outcomes.
In conclusion, MPV use was not associated with an overall reduction in short-term hospitalization or mortality. A benefit was observed in a subset of patients with COVID-19 who were asymptomatic at presentation. Further studies are needed to clarify its role in other subgroups.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Supplementary Material
Contributor Information
Adeel A Butt, Veterans Affairs Pittsburgh Healthcare System, Pittsburgh, Pennsylvania, USA; Department of Medicine, Weill Cornell Medicine, New York, New York, USA; Department of Medicine, Weill Cornell Medicine, Doha, Qatar; Department of Population Health Sciences, Weill Cornell Medicine, New York, New York, USA; Department of Population Health Sciences, Weill Cornell Medicine, Doha, Qatar; Hamad Medical Corporation, Doha, Qatar.
Peng Yan, Veterans Affairs Pittsburgh Healthcare System, Pittsburgh, Pennsylvania, USA.
Obaid S Shaikh, Veterans Affairs Pittsburgh Healthcare System, Pittsburgh, Pennsylvania, USA; Department of Medicine, Division of Gastroenterology, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Saad B Omer, Institute for Global Health, Yale University, New Haven, Connecticut, USA.
Florian B Mayr, Clinical Research, Investigation, and Systems Modeling of Acute Illness Center, Department of Critical Care Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania, USA; Department of Critical Care Medicine, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania, USA.
Victor B Talisa, Clinical Research, Investigation, and Systems Modeling of Acute Illness Center, Department of Critical Care Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania, USA; Department of Critical Care Medicine, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania, USA.
Notes
Author contributions. A. A. B. contributed study concept and study design, and drafting of the manuscript. P. Y. acquired data. P. Y. and A. A. B. performed data analysis. A. A. B., V. B. T., P. Y., O. S. S., S. B. O., and F. B. M. critically revised the manuscript for important intellectual content. All authors gave final approval of the article. A. A. B. and P. Y. had complete access to the data at all times and accept responsibility for the integrity of this article.
Acknowledgments . This study was supported by data created by the Veterans Affairs (VA) COVID-19 Shared Data Resource and resources and facilities of the Department of Veterans Affairs Informatics and Computing Infrastructure, VA HSR RES 13-457. This material is also the result of work supported with resources and the use of facilities at the VA Pittsburgh Healthcare System, Veterans Health Foundation of Pittsburgh, and the central data repositories maintained by the VA Information Resource Center, including the Corporate Data Warehouse.
Disclaimer. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the funding agencies.
Financial support. None.
Data sharing. This study used data created and maintained by the Veterans Health Administration, Department of Veterans Affairs. These data are freely available to approved individuals upon fulfilling the specified requirements through the Department of Veterans Affairs. Requests for data must be directed to the Veterans Health Administration at the Department of Veterans Affairs. Any request must fulfil all requirements for data sharing according to the existing laws, regulations, and policies of the Department of Veterans Affairs.
References
- 1. Abu-Raddad LJ, Chemaitelly H, Butt AA. Effectiveness of the BNT162b2 COVID-19 vaccine against the B.1.1.7 and B.1.351 variants. N Engl J Med 2021; 385:187–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baden LR, El Sahly HM, Essink B, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med 2021; 384:403–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N Engl J Med 2020; 383:2603–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Walsh EE, Frenck RW Jr, Falsey AR, et al. Safety and immunogenicity of two RNA-based COVID-19 vaccine candidates. N Engl J Med 2020; 383:2439–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Anderson EJ, Rouphael NG, Widge AT, et al. Safety and immunogenicity of SARS-CoV-2 mRNA-1273 vaccine in older adults. N Engl J Med 2020; 383:2427–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dagan N, Barda N, Kepten E, et al. BNT162b2 mRNA COVID-19 vaccine in a nationwide mass vaccination setting. N Engl J Med 2021; 384:1412–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Voysey M, Clemens SAC, Madhi SA, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021; 397:99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Butt AA, Omer SB, Yan P, Shaikh OS, Mayr FB. SARS-CoV-2 vaccine effectiveness in a high-risk national population in a real-world setting. Ann Intern Med 2021; 174:1404–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chemaitelly H, Tang P, Hasan MR, et al. Waning of BNT162b2 vaccine protection against SARS-CoV-2 infection in Qatar. N Engl J Med 2021; 385:e83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Butt AA, Khan T, Yan P, Shaikh OS, Omer SB, Mayr F. Rate and risk factors for breakthrough SARS-CoV-2 infection after vaccination. J Infect 2021; 83:237–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Butt AA, Yan P, Shaikh OS, Mayr FB. Outcomes among patients with breakthrough SARS-CoV-2 infection after vaccination in a high-risk national population. EClinicalMedicine 2021; 40:101117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Butt AA, Nafady-Hego H, Chemaitelly H, et al. Outcomes among patients with breakthrough SARS-CoV-2 infection after vaccination. Int J Infect Dis 2021; 110:353–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alishaq M, Nafady-Hego H, Jeremijenko A, et al. Risk factors for breakthrough SARS-CoV-2 infection in vaccinated healthcare workers. PLoS One 2021; 16:e0258820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hacisuleyman E, Hale C, Saito Y, et al. Vaccine breakthrough infections with SARS-CoV-2 variants. N Engl J Med 2021; 384:2212–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shen C, Wang Z, Zhao F, et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA 2020; 323:1582–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fernandez-Ruiz M, Lopez-Medrano F, Perez-Jacoiste Asin MA, et al. Tocilizumab for the treatment of adult patients with severe COVID-19 pneumonia: a single-center cohort study. J Med Virol 2021; 93:831–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Somers EC, Eschenauer GA, Troost JP, et al. Tocilizumab for treatment of mechanically ventilated patients with COVID-19. Clin Infect Dis 2021; 73:e445–e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Price CC, Altice FL, Shyr Y, et al. Tocilizumab treatment for cytokine release syndrome in hospitalized patients with coronavirus disease 2019: survival and clinical outcomes. Chest 2020; 158:1397–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of COVID-19—final report. N Engl J Med 2020; 383:1813–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Goldman JD, Lye DCB, Hui DS, et al. Remdesivir for 5 or 10 days in patients with severe COVID-19. N Engl J Med 2020; 383:1827–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dougan M, Nirula A, Azizad M, et al. Bamlanivimab plus etesevimab in mild or moderate COVID-19. N Engl J Med 2021; 385:1382–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lundgren JD, Grund B, Barkauskas CE, et al. A neutralizing monoclonal antibody for hospitalized patients with COVID-19. N Engl J Med 2021; 384:905–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gottlieb RL, Nirula A, Chen P, et al. Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial. JAMA 2021; 325:632–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Weinreich DM, Sivapalasingam S, Norton T, et al. REGEN-COV antibody combination and outcomes in outpatients with COVID-19. N Engl J Med 2021; 385:e81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Group RC, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med 2021; 384:693–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Food and Drug Administration . Coronavirus (COVID-19) update: FDA authorizes additional oral antiviral for treatment of COVID-19 in certain adults, 2021. www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-additional-oral-antiviral-treatment-covid-19-certain. Accessed 5 January 2022.
- 27. Food and Drug Administration . Coronavirus (COVID-19) update: FDA authorizes first oral antiviral for treatment of COVID-19, 2021. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-first-oral-antiviral-treatment-covid-19. Accessed 5 January 2022.
- 28. Food and Drug Administration . Emergency use authorization 105 (paxlovid), 2021. https://www.fda.gov/media/155049/download. Accessed 5 January 2022.
- 29. Food and Drug Administration . Emergency use authorization 108 (molnupiravir), 2021. https://www.fda.gov/media/155053/download. Accessed 5 January 2022.
- 30. Jayk Bernal A, Gomes da Silva MM, Musungaie DB, et al. Molnupiravir for oral treatment of COVID-19 in nonhospitalized patients. N Engl J Med 2022; 386:509–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Johnson MG, Puenpatom A, Moncada PA, et al. Effect of molnupiravir on biomarkers, respiratory interventions, and medical services in COVID-19 : a randomized, placebo-controlled trial. Ann Intern Med 2022; 175:1126–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wai AK, Chan CY, Cheung AW, et al. Association of molnupiravir and nirmatrelvir-ritonavir with preventable mortality, hospital admissions and related avoidable healthcare system cost among high-risk patients with mild to moderate COVID-19. Lancet Reg Health West Pac 2023; 30:100602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Khoo SH, FitzGerald R, Saunders G, et al. Molnupiravir versus placebo in unvaccinated and vaccinated patients with early SARS-CoV-2 infection in the UK (AGILE CST-2): a randomised, placebo-controlled, double-blind, phase 2 trial. Lancet Infect Dis 2023; 23:183–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Najjar-Debbiny R, Gronich N, Weber G, et al. Effectiveness of molnupiravir in high risk patients: a propensity score matched analysis. Clin Infect Dis 2023; 76:453.–. [DOI] [PubMed] [Google Scholar]
- 35. Butt AA, Yan P, Shaikh OS, Mayr FB, Omer SB. Rate and risk factors for severe/critical disease among fully vaccinated persons with breakthrough severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in a high-risk national population. Clin Infect Dis 2022; 75:e849–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mayr FB, Talisa VB, Shaikh O, Yende S, Butt AA. Effectiveness of homologous or heterologous COVID-19 boosters in veterans. N Engl J Med 2022; 386:1375–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mayr FB, Talisa VB, Castro AD, Shaikh OS, Omer SB, Butt AA. COVID-19 disease severity in US veterans infected during omicron and Delta variant predominant periods. Nat Commun 2022; 13:3647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ioannou GN, Locke ER, O'Hare AM, et al. COVID-19 vaccination effectiveness against infection or death in a national U.S. health care system: a target trial emulation study. Ann Intern Med 2022; 175:352–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Butt AA, Talisa VB, Shaikh OS, Omer SB, Mayr FB. Relative vaccine effectiveness of a SARS-CoV-2 mRNA vaccine booster dose against the omicron variant. Clin Infect Dis 2022; 75:2161–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. SAS Institute . Estimating the risk (proportion) difference for matched pairs data with binary response. https://support.sas.com/kb/46/997.html. Accessed 18 October 2022.
- 41. Furlan L, Caramelli B. The regrettable story of the “COVID kit” and the “early treatment of COVID-19” in Brazil. Lancet Reg Health Am 2021; 4:100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Abdelmalek SMA, Mousa A. Azithromycin misuse during the COVID-19 pandemic: a cross-sectional study from Jordan. Infect Drug Resist 2022; 15:747–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Romer D, Winneg KM, Jamieson PE, Brensinger C, Jamieson KH. Misinformation about vaccine safety and uptake of COVID-19 vaccines among adults and 5–11-year-olds in the United States. Vaccine 2022; 40:6463–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lee SK, Sun J, Jang S, Connelly S. Misinformation of COVID-19 vaccines and vaccine hesitancy. Sci Rep 2022; 12:13681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. West AN, Charlton ME, Vaughan-Sarrazin M. Dual use of VA and non-VA hospitals by veterans with multiple hospitalizations. BMC Health Serv Res 2015; 15:431. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.