Abstract
Background
Programmed cell death receptor-1 (PD-1)-blocking antibodies are approved to treat metastatic or locally advanced cutaneous squamous cell carcinoma (CSCC) cases ineligible for curative surgery or radiation. Notwithstanding, some patients experience inadequate responses or severe immune-related adverse events (AEs), indicating the need for improved therapies. Cosibelimab is a high-affinity programmed cell death-ligand 1 (PD-L1)-blocking antibody that activates innate and adaptive immunity by blocking PD-L1 interaction with PD-1 and B7-1 receptors. It is an unmodified immunoglobulin G1 subtype with a functional Fc domain capable of inducing antibody-dependent cellular cytotoxicity and complement-dependent cytotoxicity. Here, we present results of the pivotal study of patients with metastatic CSCC from an open-label, multicenter, multiregional, multicohort, phase 1 trial of cosibelimab.
Methods
In this trial, participants with metastatic CSCC received cosibelimab 800 mg intravenously every 2 weeks. Primary endpoint was objective response rate (ORR) by independent central review using Response Evaluation Criteria in Solid Tumors, V.1.1. Secondary endpoints included duration of response (DOR) and safety.
Results
Objective response was observed in 37 of 78 participants (47.4% (95% CI: 36.0% to 59.1%)), with median follow-up of 15.4 months (range: 0.4 to 40.5) as of data cut-off. Median DOR was not reached (range: 1.4+ to 34.1+ months), with response ongoing in 73.0% of participants. Common treatment-emergent AEs (≥15%) were fatigue (26.9%), rash (16.7%), and anemia (15.4%). Eighteen participants (23.1%) experienced immune-related AEs (grade 3: n=2 (2.6%); no grade 4/5). No treatment-related deaths were reported.
Conclusions
Cosibelimab demonstrated clinically meaningful ORR and DOR and was associated with a manageable safety profile.
Trial registration number
Keywords: Immunotherapy, Programmed Cell Death 1 Receptor, Skin Neoplasms, Immune Checkpoint Inhibitors
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Cutaneous squamous cell carcinoma (CSCC) is the second most common form of skin cancer, and although it is often associated with a favorable prognosis, patients who present with locally advanced or metastatic CSCC (mCSCC) who are ineligible for curative surgery or radiation have limited treatment options. Although existing immunotherapies targeting programmed cell death receptor-1 (PD-1) have proven effective in mCSCC, some patients experience inadequate responses or severe immune-related adverse events (irAEs), and there remains an unmet need to improve outcomes and safety.
WHAT THIS STUDY ADDS
This pivotal phase 1 study demonstrates the safety and efficacy of a programmed cell death-ligand 1 (PD-L1)-targeting therapy with functional Fc domain, cosibelimab, in mCSCC. Cosibelimab treatment resulted in a robust and clinically meaningful objective response rate (ORR) with durable responses and a well-tolerated safety profile.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Cosibelimab is the first PD-L1-blocking antibody to demonstrate a robust and clinically meaningful ORR with durable responses as well as a manageable safety profile in patients with mCSCC. Given observed lower rates of irAEs compared with those reported for similar studies of PD-1-targeting agents, cosibelimab may address an area of unmet clinical need for effective and better tolerated treatments for patients with mCSCC who are ineligible for curative surgery or radiation.
Background
Cutaneous squamous cell carcinoma (CSCC) is the second most common form of skin cancer, making up ~20% of epithelial skin cancers.1–3 The incidence of CSCC is rapidly increasing globally owing to aging of the world’s population and increased exposure to risk factors such as ultraviolet radiation.1 4 5 However, CSCC remains a highly under-recognized disease, as it is excluded from most national cancer registries.6 In a 2020 study from the Netherlands, the authors estimated that European CSCC incidence rates would increase by 23% for men and 29% for women between 2017 and 2027.4 Similarly, the incidence of CSCC is increasing in the USA, UK, and Australia.1 7 8 This increase in incidence will be associated with corresponding increases in morbidity, mortality, public health burden, and social costs.3
Although patients with CSCC generally have a favorable prognosis and a high likelihood for long-term survival after surgical excision, which remains the standard treatment for localized CSCC, some may progress to locally advanced CSCC (laCSCC) or metastatic CSCC (mCSCC).3 Such patients may experience relapse, develop aggressive local lesions that are not candidates for approved therapies, or exhibit regional or distant metastases.3 9 Indeed, 17% of immunocompetent patients with high-risk CSCC may develop locoregional recurrence within 5 years after curative surgery and postoperative radiotherapy.10 Both laCSCC and mCSCC are associated with substantial morbidity and mortality, representing an area of unmet clinical need for effective and well-tolerated treatments.1 3
Before the approval of immunotherapies, the management of CSCC was challenging because existing therapies exhibited poor response rates, short durations of response, or poor safety profiles.11–13 The exceptionally high tumor mutational burden of CSCC with ultraviolet radiation-related mutations underpins sensitivity to immunotherapy.14 Programmed cell death-ligand 1 (PD-L1), which is often upregulated in CSCC tumors, is the primary ligand for programmed cell death receptor-1 (PD-1).15 Activation of PD-1 on T cells by PD-L1 on tumor cells leads to inhibition of cytokine production and the cytolytic activity of PD-1+, tumor-infiltrating T cells, thereby circumventing their destruction by the immune system.9 15–17 Indeed, increased PD-L1 expression in cancer cells is associated with risk of metastasis.18 Thus, inhibiting the interaction between PD-1 and PD-L1 has been shown to promote the immune response and result in antitumor activity.9 Together, these data support inhibition of the PD-1 and PD-L1 pathway as immunotherapy to treat CSCC. Currently, two PD-1-blocking antibodies are approved in the USA as monotherapy for patients with laCSCC or mCSCC ineligible for curative surgery or radiation.19 20 One of these, cemiplimab, has additional global approvals, including in the European Union and Australia.21 22 Although PD-1-blocking antibodies are effective in patients with CSCC, they can be associated with severe adverse events, indicating the need for efficacious agents that have better safety profiles.23 Differences have been noted between PD-1 inhibitors and PD-L1 inhibitors in the incidence of grade 3 or higher treatment-related adverse events (TRAEs), including immune-related adverse events (irAEs), with occurrence being lower for PD-L1 inhibitors.23–25 It is hypothesized that TRAEs and irAEs may be lower with anti-PD-L1 antibodies because the interaction between PD-1 and PD-L2 remains unaltered.23 25 With less blockade of the negative inhibitory signal, PD-L1 inhibitors might produce less autoimmunity relative to anti-PD-1 antibodies.23 25 Furthermore, PD-L2 also binds to repulsive guidance molecule b, which regulates respiratory immunity; this fact could explain why the incidences of some irAEs, such as pneumonitis, are higher with PD-1 inhibitors than with PD-L1 inhibitors.26 27 Although PD-L1 inhibitors have been approved for certain advanced tumors, none are currently approved for patients with CSCC.20
Cosibelimab is a high-affinity, fully human monoclonal antibody that binds to PD-L1; it restores adaptive immunity and engages innate immunity through sustained high tumor target occupancy that blocks PD-L1 interaction with PD-1 to reactivate T cells.28 29 Additionally, cosibelimab has a functional fragment crystallizable domain capable of inducing antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity against tumor cells.28 Preclinical pharmacology studies have shown that the affinity binding capability, relative inhibitory potential, and functional cellular activity of cosibelimab are consistent with a mechanism of action of blocking PD-L1.28 Toxicity and safety studies further support the investigation of cosibelimab in patients with advanced cancers, including CSCC. Here, we present efficacy and safety data for a cohort of patients with mCSCC from an open-label, multicenter, multiregional, multicohort, phase 1 trial of cosibelimab.
Methods
Participants
This ongoing, open-label, multicenter, multicohort trial was conducted in two parts. Part 1 was a dose-escalation study to evaluate fixed doses of cosibelimab monotherapy administered every 2 weeks (Q2W) or every 3 weeks (Q3W) in participants with advanced cancers. Part 2 enrolled participants into seven expansion cohorts on the basis of tumor type to assess the antitumor activity and safety of cosibelimab, including a pivotal cohort of participants with mCSCC. Eligible participants were aged ≥18 years with an Eastern Cooperative Oncology Group performance status (ECOG PS) of 0 or 1. Participants had a life expectancy of ≥3 months, adequate hematological and biological function by confirmed laboratory values, and histologically confirmed diagnosis of mCSCC not amenable to curative surgery or radiation. Nodal and/or distant disease was classified as metastatic disease in this study. Immunosuppressive doses of systemic medications or surgery requiring general anesthesia were discontinued or completed ≥2 weeks before study drug administration, and surgeries requiring local/epidural anesthesia were completed ≥72 hours before study drug administration. Female participants were required to be postmenopausal for ≥24 consecutive months, surgically incapable of bearing children, or using a reliable form of contraception. Male participants were also required to use contraception during the study treatment period and for ≥180 days after the last dose of study drug.
Key exclusion criteria included a history of severe hypersensitivity reactions to other monoclonal antibodies, prior immune checkpoint inhibitor therapy, or history of autoimmune disease. Individuals who required immunosuppressive doses of steroids, chemotherapy, radioactive or biological cancer therapy, or tyrosine kinase inhibitor therapy within 4 weeks before the first dose of study drug were also excluded. Individuals with allogeneic transplant within 6 months before the first dose of study drug; malignancy within the previous 2 years, except for locally curable cancers; or an active infection (viral, bacterial, or fungal) requiring intravenous antimicrobial therapeutic treatment within 28 days before the first dose of study drug were excluded. Lastly, individuals with a history of being positive for HIV, hepatitis B, or hepatitis C; those with current or previous interstitial lung disease; and those with a history of pneumonitis that required oral or intravenous steroids were excluded from the study.
Study design
The Consolidated Standards of Reporting Trials reporting guidelines were used in preparation of this report.30 In this pivotal study, of 96 participants with mCSCC screened for inclusion, 78 participants were enrolled and included in the analyses (online supplemental figure 1). There was no randomization, and neither participants nor study investigators were blinded. Dose selection was based on the results of dose escalation from Part 1 of the study and pharmacokinetic/target-occupancy modeling that predicted >99% tumor target occupancy of PD-L1 at steady-state trough concentrations with a cosibelimab 800 mg Q2W dosing regimen.31 Participants received a fixed dose of cosibelimab 800 mg by intravenous infusion over 60 min Q2W until confirmed complete response (CR), worsening progressive disease (PD), toxicity, or clinical deterioration and then entered the post-treatment follow-up period (online supplemental figure 2). Cosibelimab was administered on days 1 and 15 of each 28-day treatment cycle. Both the investigator and an independent central review (ICR) conducted end-of-cycle tumor assessments according to Response Evaluation Criteria in Solid Tumors, version 1.1 (RECIST V.1.1) between days 24 and 28 in cycles 2, 4, 6, and 8 and every three cycles thereafter. Investigator assessments informed the decision to treat participants with additional cycles or begin follow-up visits. Participants with worsening PD (defined as ≥10% increase in tumor burden volume from time of initial PD) and/or clinical deterioration were removed from treatment and followed for 3 months during follow-up visits 1 and 2. Participants with CR, partial response (PR), stable disease (SD), or non-worsening PD who did not have a grade ≥3 treatment-emergent adverse event (TEAE) that precluded further treatment were treated with additional cycles of cosibelimab. All participants who discontinued treatment, except for those who discontinued owing to PD, had tumor assessment scans at follow-up visits for up to 6 months or until relapse or initiation of a new therapy.
jitc-2023-007637supp001.pdf (114.8KB, pdf)
jitc-2023-007637supp002.pdf (75.8KB, pdf)
After participants stopped treatment and completed the necessary follow-up visits, they began survival follow-up, wherein they were contacted by telephone quarterly for survival and tumor treatment status. There were no participants lost to follow-up as of data cut-off.
A central laboratory analyzed the tumor samples for baseline PD-L1 expression using the PD-L1 IHC 22C3 pharmDx assay (SK00621-5; Agilent, Santa Clara, California, USA) to derive the percentage of tumor cells exhibiting cell surface PD-L1 before treatment.
The study was conducted according to the principles of the Declaration of Helsinki, the International Conference on Harmonisation (ICH) Good Clinical Practice guidelines outlined in the ICH E6 Tripartite Guideline, and the Code of Federal Regulations Title 21 (part 312) at the various participating sites, with approval of an independent ethics committee or institutional review board. Written informed consent was obtained from each participant before study enrollment.
Outcomes
The prespecified primary endpoint was objective response rate (ORR) assessed by ICR according to RECIST V.1.1. ORR was determined by the proportion of participants with a best overall response (BOR) of CR or PR in the intent-to-treat (ITT) population. Participants with BOR of SD, PD, or not evaluable (NE) were considered as not reaching an objective response of CR or PR. Secondary endpoints included duration of response (DOR) for participants with CR or PR assessed by ICR according to RECIST V.1.1, as well as incidence and severity of TEAEs according to the National Cancer Institute Common Terminology Criteria for Adverse Events, V.5.0. Safety assessments included clinical laboratory data, vital signs, electrocardiograms, ECOG PS evaluations, and physical examinations. An exploratory analysis of ORR by PD-L1 status (positive (≥1%), negative) was also performed. Data cut-off was November 18, 2021, for ORR and March 18, 2022, for DOR and all safety data, as predefined in the study’s statistical analysis plan.
Statistical analysis
A sample size of 75 provided at least 95% power to reject a null hypothesis of an ORR of 25% at a two-sided significance level ≤5% if the true ORR is 45%. The sample size was selected such that the lower limit of the two-sided 95% CI of the estimated ORR would represent a clinically meaningful response rate. The ORR was summarized by descriptive statistics and two-sided 95% CIs via the Exact (Clopper-Pearson) method.
Tumor response was assessed on radiologic scans according to RECIST V.1.1, and DOR was summarized for participants with confirmed responses. Time-to-event variables were summarized by Kaplan-Meier curves and estimates at the key landmark time point with 95% CI. All recorded adverse events were listed and tabulated for the worst Common Terminology Criteria grade by system organ class, preferred term, and dose and coded according to Medical Dictionary for Regulatory Activities (MedDRA), V.24.0. The incidence, relationship to therapy, and severity of TEAEs and the changes in clinical laboratory tests, ECOG PS, physical examination, vital signs, electrocardiograms, and immunogenicity results were summarized with descriptive statistics.
All statistical analyses were carried out with the statistical analysis software SAS, V.9.4 or higher.
Results
Participants
This clinical trial enrolled participants at 24 sites in eight countries, grouped regionally as Australia/New Zealand (57.7%), Europe (24.4%), South Africa (10.3%), and Thailand (7.7%; table 1). Overall, from September 2019 to May 2021, 78 participants with mCSCC were enrolled and received cosibelimab 800 mg Q2W, and all were included in the safety and ITT populations. Participants were predominantly man (75.6%) and had a median age of 71.6 years. Most participants had distant mCSCC (66.7%) and an ECOG PS of 1 (70.5%). Additionally, most participants had undergone prior cancer surgery (60.3%) and radiation therapy (65.4%), but the majority (91.0%) had not undergone prior systemic therapy for their malignancy. The median duration of follow-up was 15.4 months (range: 0.4 to 40.5).
Table 1.
Participant demographics and baseline characteristics
| Demographic, n (%)* | mCSCC (N=78) |
| Sex | |
| Female | 19 (24.4) |
| Male | 59 (75.6) |
| Median age | 71.6 (37–91) |
| <65 years | 22 (28.2) |
| ≥65 years | 56 (71.8) |
| Race | |
| White | 69 (88.5) |
| Asian | 6 (7.7) |
| Unknown | 2 (2.6) |
| Black or African American | 1 (1.3) |
| Ethnicity | |
| Not Hispanic or Latino | 73 (93.6) |
| Hispanic or Latino | 3 (3.8) |
| Unknown | 2 (2.6) |
| Country/region | |
| Australia/New Zealand | 45 (57.7) |
| Europe | 19 (24.4) |
| South Africa | 8 (10.3) |
| Thailand | 6 (7.7) |
| PD-L1 status | |
| PD-L1-positive (≥1%) | 37 (47.4) |
| PD-L1-negative | 18 (23.1) |
| Unknown | 23 (29.5) |
| ECOG PS | |
| 0 | 23 (29.5) |
| 1 | 55 (70.5) |
| Primary CSCC site | |
| Head/neck | 46 (59.0) |
| Extremity | 18 (23.1) |
| Trunk | 9 (11.5) |
| Other | 5 (6.4) |
| Type of metastatic disease | |
| Distant | 52 (66.7) |
| Nodal | 26 (33.3) |
| Prior cancer-related surgery | 47 (60.3) |
| Prior cancer-related radiotherapy | 51 (65.4) |
| Prior cancer-related systemic therapy | 7 (9.0) |
*Except for median age, which is presented as years (range).
CSCC, cutaneous squamous cell carcinoma; ECOG PS, Eastern Cooperative Oncology Group performance status; mCSCC, metastatic CSCC; PD-L1, programmed cell death-ligand 1.
Efficacy
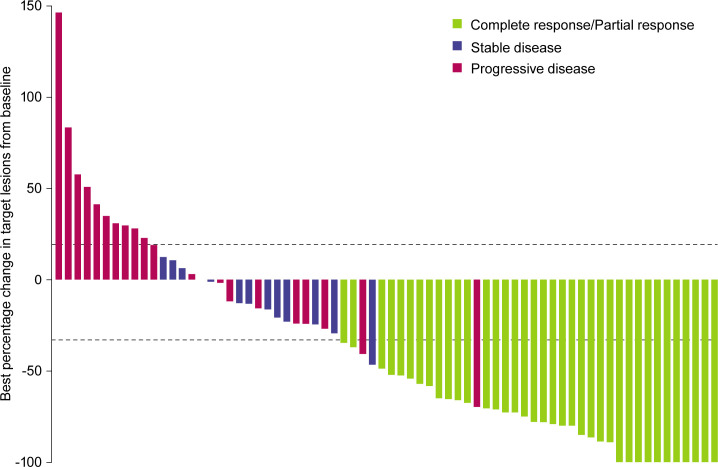
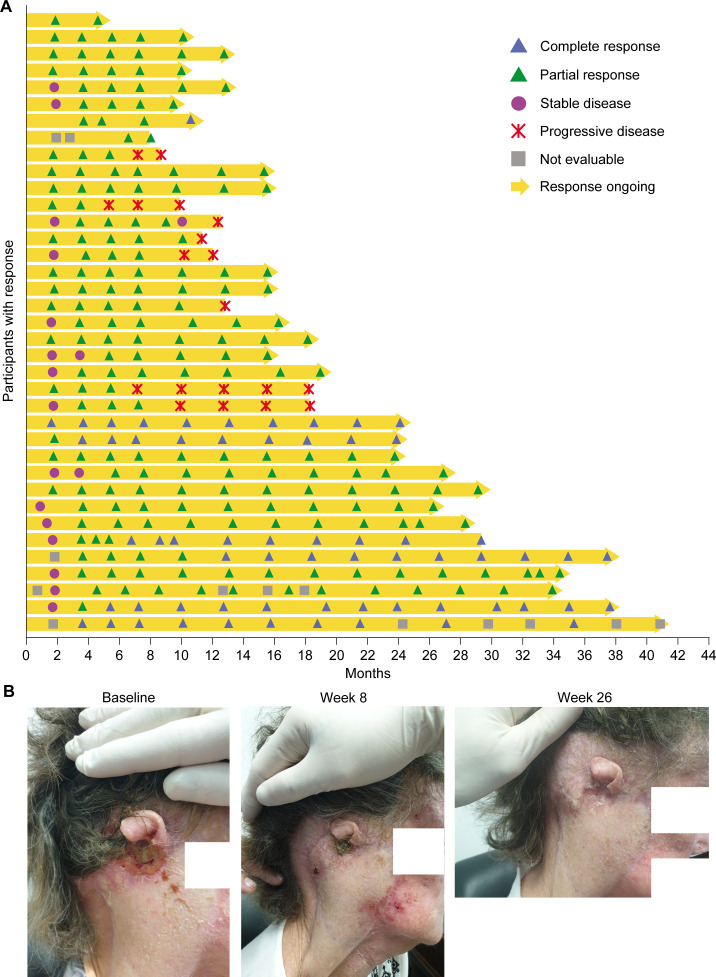
The confirmed ORR by ICR in the ITT population was 47.4% (95% CI: 36.0% to 59.1%), with robust and durable reductions in target lesions observed (table 2; figures 1,2). The median observed time to response was 1.9 months (range: 1.6 to 6.6). Of 37 participants who had an objective response, 6 achieved a CR and 31 achieved a PR as of the data cut-off. The median DOR was not reached (range: 1.4+ to 34.1+ months), with response ongoing in 73.0% of participants. The Kaplan-Meier-estimated probabilities of maintaining a response at 6, 12, and 24 months were 88.9%, 73.0%, and 73.0%, respectively.
Table 2.
Tumor response by ICR according to RECIST V.1.1
| Parameter, n (%)* | mCSCC (N=78) |
| Best overall response | |
| Complete response | 6 (7.7) |
| Partial response | 31 (39.7) |
| Stable disease | 12 (15.4) |
| Progressive disease | 21 (26.9) |
| Not evaluable | 8 (10.3) |
| ORR in ITT population, % (95% CI) | 47.4 (36.0 to 59.1) |
| ORR in modified ITT population, % (95% CI) | 48.7 (37.0 to 60.4)† |
| Response ongoing | 27 (73.0) |
| Median DOR, months (min, max) | NR (1.4+ to 34.1+) |
| Kaplan-Meier-estimated 6-month DOR probability, % (95% CI) | 88.9 (73.1 to 95.7) |
| Kaplan-Meier-estimated 12-month DOR probability, % (95% CI) | 73.0 (54.2 to 85.0) |
| Kaplan-Meier-estimated 24-month DOR probability, % (95% CI) | 73.0 (54.2 to 85.0) |
| Median duration of follow-up, months (95% CI) | 15.4 (12.0 to 21.0) |
*Unless otherwise denoted.
†Participants who died of COVID-19 before a post-baseline response assessment were excluded from ORR calculations in the modified ITT population.
DOR, duration of response; ICR, independent central review; ITT, intent-to-treat; mCSCC, metastatic cutaneous squamous cell carcinoma; NR, not reached; ORR, objective response rate; RECIST V.1.1, Response Evaluation Criteria in Solid Tumors, version 1.1.
Figure 1.
mCSCC best overall response to cosibelimab monotherapy. Best percentage change in the sum of target lesion diameters from baseline for participants who underwent tumor assessment by independent central review after treatment initiation (n=70). Figure excludes participants with a best overall response of not evaluable due to no post-baseline tumor assessment (n=8), which are included as non-responders in the calculation of ORR. Horizontal dashed lines indicate RECIST V.1.1 criteria for partial response (≥30% decrease in the sum of target lesion diameters) and progressive disease (≥20% increase in target lesion diameters). mCSCC, metastatic cutaneous squamous cell carcinoma; ORR, objective response rate; RECIST V.1.1, Response Evaluation Criteria in Solid Tumors, version 1.1.
Figure 2.
Effect of cosibelimab on time to response, DOR, and an individual case. (A) Time to response and DOR in responding participants who underwent tumor assessment by independent central review after treatment initiation (n=37). (B) Effect of cosibelimab monotherapy in a participant with mCSCC. An adult patient with a CSCC skin lesion at the right postauricular region at baseline (left), after 8 weeks (middle), and after 26 weeks (right) of treatment initiation with cosibelimab. CSCC, cutaneous squamous cell carcinoma; DOR, duration of response; mCSCC, metastatic CSCC.
Exploratory subgroup analyses by demographics are presented in online supplemental figure 3. Samples for baseline tumor PD-L1 status assessment were available for 55 (70.5%) of the 78 enrolled participants. The ORR by ICR was 45.9% (17 of 37) among participants with PD-L1-positive (≥1%) tumors and 44.4% (8 of 18) among participants with PD-L1-negative tumors, with durable responses observed regardless of PD-L1 status.
jitc-2023-007637supp003.pdf (298.3KB, pdf)
Safety
The most common TEAEs were fatigue (26.9%), rash (16.7%), and anemia (15.4%; table 3). Nine participants (11.5%) discontinued treatment owing to an adverse event, but of those, only 2 (2.6%) were considered related to cosibelimab treatment: 1 participant diagnosed with pemphigoid and 1 with hepatobiliary disorders (cholestasis and hepatic cytolysis). The only adverse event of grade 3 or higher that occurred in more than two participants was anemia (6.4%).
Table 3.
Summary of TEAEs
| TEAE, n (%) | Any grade (N=78) | Grade ≥3 (N=78) |
| Any | 76 (97.4) | 41 (52.6) |
| Immune-related TEAE | 18 (23.1) | 2 (2.6) |
| TEAEs, regardless of attribution, that led to discontinuation | 9 (11.5) | 8 (10.3) |
| Most common TEAEs (>10%), regardless of attribution | ||
| Fatigue | 21 (26.9) | 2 (2.6) |
| Rash | 13 (16.7) | 1 (1.3) |
| Anemia | 12 (15.4) | 5 (6.4) |
| Constipation | 11 (14.1) | — |
| Diarrhea | 11 (14.1) | — |
| Nausea | 10 (12.8) | — |
| Hypercalcemia | 9 (11.5) | 1 (1.3) |
| Hyponatremia | 9 (11.5) | 2 (2.6) |
| Localized infection | 9 (11.5) | 1 (1.3) |
| Peripheral edema | 9 (11.5) | — |
| Arthralgia | 8 (10.3) | — |
| Cellulitis | 8 (10.3) | 1 (1.3) |
| Cough | 8 (10.3) | — |
| Insomnia | 8 (10.3) | — |
| Pruritus | 8 (10.3) | — |
TEAE, treatment-emergent adverse event.
Adverse events led to death in 3 (3.8%) participants, all considered unrelated to cosibelimab treatment. Two participants died of COVID-19-related illness and one with a history of cardiovascular disease died of cardiac arrest. Most TRAEs were mild to moderate in severity, with 8 (10.3%) participants experiencing an event assessed as grade 3 (no participants experienced a TRAE higher than grade 3; online supplemental table 1). Among 18 (23.1%) participants experiencing irAEs, 2 (2.6%) were assessed as grade 3 (none were higher than grade 3; table 3).
jitc-2023-007637supp004.pdf (25.2KB, pdf)
Discussion
Advanced CSCC is a life-threatening condition, and patients with metastatic disease face a poor prognosis, with 10-year survival rates as low as 10% to 20%.14 32 Thus, the development of monoclonal antibodies directed against immune checkpoints represents a great advancement in the management of CSCC.14 Indeed, therapies targeting PD-1 on T effector cells have led to substantial improvements in CSCC treatment in terms of objective responses, survival, and quality of life.14 Moving forward, the use of immunotherapy such as checkpoint inhibitors will most likely become the gold standard in the management of CSCC.14 Still, treatment options are limited and new therapies are needed that have more tolerable adverse event profiles.14 20 33 To date, no PD-L1-targeted therapy has been approved for CSCC.21 34 Herein, we report results from a pivotal phase 1 study demonstrating the efficacy and safety of cosibelimab, an anti-PD-L1 monoclonal antibody, in participants with mCSCC.
Ultraviolet exposure, a major risk factor for CSCC, varies among geographic regions and, as expected, a large percentage of participants with mCSCC in this study came from regions with high levels of ultraviolet radiation and with a Caucasian background.1 4 35 However, the multiregional aspect of our trial most likely did not affect the underlying causality of mCSCC among participants. Treatment with cosibelimab 800 mg Q2W resulted in a robust and clinically meaningful ORR with durable responses in participants. Immunohistochemical analysis showed that cosibelimab was clinically active irrespective of baseline tumor PD-L1 status. This preliminary analysis suggests that PD-L1 cannot be used to predict clinical response of cosibelimab in patients with mCSCC. The ORR in the ITT population was 47.4% with an estimated probability of maintaining a response at 24 months of 73.0%, denoting the effectiveness and durability of cosibelimab. This durability of cosibelimab can be further characterized and confirmed with long-term follow-up, as those who did not meet criteria for response might experience clinical benefit.
The response rate of cosibelimab was similar to that of PD-1 inhibitors approved by regulatory authorities for the treatment of laCSCC and mCSCC.14 36–38 Immunotherapy is gradually gaining prominence in the management of CSCC; however, one of the challenges is reducing the toxicity profile.16 From a safety profile perspective, both a scientifically plausible rationale and reasonable evidence from published clinical data support the premise that certain serious toxicities known to occur with available anti-PD-1 antibodies can be avoided with the anti-PD-L1 antibody cosibelimab, possibly owing to the presence of the other PD-1 ligand, PD-L2, which may maintain some level of checkpoint signaling.23 In our study, cosibelimab resulted in mostly mild-to-moderate TRAEs; 10.3% of participants experienced grade 3 TRAEs, and there were no reports of grade 4 or 5 TRAEs. Moreover, only 23.1% of participants experienced irAEs, and only 2.6% experienced an event of grade 3 severity (no grade 4 or 5), rates that are lower than those reported in similar studies of PD-1-targeting agents.33 36 Similarly, the rate of grade ≥3 irAEs was lower than that reported in a neoadjuvant cemiplimab study in patients with resectable CSCC who received cemiplimab over a shorter duration of time.39 Overall, cosibelimab was well tolerated in patients with mCSCC.
Study limitations include the single-cohort design and duration of follow-up at data cut-off. Furthermore, although we conducted a subgroup analysis on the basis of PD-L1 expression levels, we did not analyze other potential biomarkers, including tumor mutational burden, limiting our findings and potential ability to identify patients who benefit the most or detect potential mechanisms of resistance to cosibelimab in mCSCC tumors. Additionally, immunocompromised patients were under-represented in our study population; therefore, we cannot comment on the efficacy of cosibelimab among such patients. However, there is a mechanistic rationale to study cosibelimab in immunocompromised patients in future trials, such as in patients with CSCC with concomitant chronic lymphoid leukemia, given the engagement of cosibelimab with natural killer cells through its functional Fc region inducing ADCC-mediated tumor cell lysis.
Despite these limitations, our data from this pivotal study of patients with mCSCC from an open-label, multicenter, multiregional, multicohort, phase 1 trial suggest that cosibelimab is associated with robust antitumor activity, durable responses, and a well-tolerated profile. Future data cut-off dates will provide more information on DOR and long-term safety and will be reported as results become available. In conclusion, these results support cosibelimab 800 mg Q2W as a potential treatment that is safe and effective for patients with mCSCC. Long-term follow-up of the study participants is ongoing to continue characterization of the safety and efficacy profile of cosibelimab. Additionally, this study is enrolling cohorts to evaluate cosibelimab as a treatment for patients with laCSCC and to evaluate cosibelimab with an alternative dosing regimen of 1200 mg Q3W.
Acknowledgments
The authors would like to thank the participants, their families, and all investigational site members involved in this study. Writing and editorial assistance were provided under the direction of the authors by Ella A Kasanga, PhD, and Claire Levine, MS, ELS, of MedThink SciCom.
Footnotes
Contributors: JO and JD conceptualized and supervised the administration of this study. PC, RL, DB, DLH, MM, JC, SF, AK, DRM, AM, VSh, HS, AT, M-AB-G, CC, SD, AD, OD, PK, IL, HM, EM-C, and VSr recruited patients, provided resources, and collected and analyzed the data. SA recruited patients, provided resources, and collected data. JO accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish. All authors contributed to data interpretation, as well as critical review, revision, and approval of the report.
Funding: This study was funded by Checkpoint Therapeutics.
Competing interests: PC has nothing to disclose. RL has received honoraria from AstraZeneca/MedImmune, Bristol Myers Squibb Foundation, MSD, and Sanofi; has served as a consultant and/or scientific advisor for AstraZeneca/MedImmune and Roche; and has received compensation for travel, accommodations, and other expenses from MSD. DB has nothing to disclose. DLH has served as a consultant and/or scientific advisor for Checkpoint Therapeutics. MM has nothing to disclose. SA has nothing to disclose. JC has nothing to disclose. SF has nothing to disclose. AK has nothing to disclose. DRM has nothing to disclose. AM has nothing to disclose. VSh has served as a speaker for Elekta. HS has nothing to disclose. AT has nothing to disclose. M-AB-G has served as a consultant and/or scientific advisor for BMS, Eisai, MSD, Novartis, and Pierre Fabre and has received research funding from Novartis. CC has received grant/research support from AstraZeneca, Novartis, and Roche. SD has received institutional research grants from BMS and MSD; has served as a consultant and/or scientific advisor for BMS, MSD, and Pierre Fabre; and has received compensation for congress attendance from BMS and MSD. AD has nothing to disclose. OD has nothing to disclose. PK has nothing to disclose. IL has financial or non-financial interests in Agenus, BMS, Janssen, MacroGenics, MSD, Pfizer, and Roche. HM has received honoraria from BMS, Merck Serono, MSD, Novartis, and Pierre Fabre; has received institutional support from BMS, Canceropole PACA, and Société Française de Dermatologie; has served as a consultant for BMS, Merck Serono, MSD, Novartis, and Pierre Fabre; has served on a data safety monitoring board/advisory board for Novartis and Pierre Fabre; and has received travel grants from Novartis and Pierre Fabre. EM-C has served as a consultant and/or scientific advisor for MBS, MSD, Novartis, Pierre Fabre, and Sanofi; has received honoraria from MBS, MSD, Novartis, Pierre Fabre, and Sanofi; and has received compensation for travel, accommodations, and other expenses from MSD. VSr has nothing to disclose. JO is an employee of Checkpoint Therapeutics and holds stocks and other ownership interests in the company; has served in leadership roles at Checkpoint Therapeutics; and has received compensation for travel, accommodations, and other expenses from Checkpoint Therapeutics. JD has served as a consultant and/or scientific advisor for Amgen, Bayer, BeiGene, Boehringer Ingelheim, Daiichi Sankyo, GlaxoSmithKline, Merck KGaA, Novartis, Novotech, Pfizer, Pierre Fabre, and Roche/Genentech; has served on a data safety monitoring board/advisory board for Boehringer Ingelheim and Pfizer; has served as a board director for Cancer Trials Australia and ANZSA; and has received institutional grant/research support from AstraZeneca/MedImmune, BeiGene, BMS, GlaxoSmithKline, Lilly, Novartis, and Roche.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The data supporting the findings of this study are available within the article and its supplementary materials. Any additional data requests are available upon reasonable request to the corresponding author.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was conducted according to the principles of the Declaration of Helsinki, the International Conference on Harmonisation (ICH) Good Clinical Practice guidelines outlined in the ICH E6 Tripartite Guideline, and the Code of Federal Regulations Title 21 (part 312) at the various participating sites, with approval of an independent ethics committee or institutional review board (Bellberry Human Research Ethics Committee: 2017-07-507; Comité de Ética de Investigación con medicamentos (CEIm) del Hospital Universitario 12 de Octubre: 20/285; Comite de Protecion des Personnes (CPP) Ouest II – Angers: 20.01120.202047; Eastern Health Human Research Ethics Committee: HREC/17/EH/125; Institutional Review Board/Faculty of Medicine, Chulalongkorn University: 079/2018; Komisja Bioetyczna przy Okręgowej Radzie Lekarskiej Wielkopolskiej Izby Lekarskiej: 142/2018; Maharaj Nakorn Chiang Mai Hospital, Research Ethics Committee: REC 60-346-14-1; Metro South Human Research Ethics Committee: HREC/2019/QMS/58441 (SR); New Zealand Northern B Health and Disability Ethics Committee: 17/NTB/164; Pharma-Ethics Independent Research Ethics Committee: 299/2018; University of The Witwatersrand (WITS), Johannesburg HREC: 191122984; Bioethics and Deontology Committee of the State Institution ‘V.T. Zaitsev Institute of General and Urgent Surgery of National Academy of Medical Sciences’ of Ukraine: 40; Local Ethics Committee at the Communal Non-Profit Enterprise of Sumy Regional Council, Sumy Regional Clinical Oncology Dispensary: 211/1). Written informed consent was obtained from each participant before study enrollment. Participants gave informed consent to participate in the study before taking part.
References
- 1. Palyca P, Koshenkov VP, Mehnert JM. Developments in the treatment of locally advanced and metastatic squamous cell carcinoma of the skin: a rising unmet need. Am Soc Clin Oncol Educ Book 2014:e397–404. 10.14694/EdBook_AM.2014.34.e397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Amaral T, Osewold M, Presser D, et al. Advanced cutaneous squamous cell carcinoma: real world data of patient profiles and treatment patterns. J Eur Acad Dermatol Venereol 2019;33 Suppl 8(suppl 8):44–51. 10.1111/jdv.15845 [DOI] [PubMed] [Google Scholar]
- 3. Stanganelli I, Spagnolo F, Argenziano G, et al. The Multidisciplinary management of cutaneous squamous cell carcinoma: a comprehensive review and clinical recommendations by a panel of experts. Cancers 2022;14:377. 10.3390/cancers14020377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tokez S, Hollestein L, Louwman M, et al. Incidence of multiple vs first cutaneous squamous cell carcinoma on a nationwide scale and estimation of future incidences of cutaneous squamous cell carcinoma. JAMA Dermatol 2020;156:1300–6. 10.1001/jamadermatol.2020.3677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lomas A, Leonardi-Bee J, Bath-Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol 2012;166:1069–80. 10.1111/j.1365-2133.2012.10830.x [DOI] [PubMed] [Google Scholar]
- 6. Wehner MR. Underestimation of cutaneous squamous cell carcinoma incidence, even in cancer registries. JAMA Dermatol 2020;156:1290–1. 10.1001/jamadermatol.2020.3678 [DOI] [PubMed] [Google Scholar]
- 7. Perera E, Gnaneswaran N, Staines C, et al. Incidence and prevalence of non-melanoma skin cancer in Australia: a systematic review. Australas J Dermatol 2015;56:258–67. 10.1111/ajd.12282 [DOI] [PubMed] [Google Scholar]
- 8. Jones OT, Ranmuthu CKI, Hall PN, et al. Recognising skin cancer in primary care. Adv Ther 2020;37:603–16. 10.1007/s12325-019-01130-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Patel R, Chang ALS. Immune checkpoint inhibitors for treating advanced cutaneous squamous cell carcinoma. Am J Clin Dermatol 2019;20:477–82. 10.1007/s40257-019-00426-w [DOI] [PubMed] [Google Scholar]
- 10. Porceddu SV, Bressel M, Poulsen MG, et al. Postoperative concurrent chemoradiotherapy versus postoperative radiotherapy in high-risk cutaneous squamous cell carcinoma of the head and neck: the randomized phase III TROG 05.01 trial. J Clin Oncol 2018;36:1275–83. 10.1200/JCO.2017.77.0941 [DOI] [PubMed] [Google Scholar]
- 11. Gold KA, Kies MS, William WN, et al. Erlotinib in the treatment of recurrent or metastatic cutaneous squamous cell carcinoma: a single-arm phase 2 clinical trial. Cancer 2018;124:2169–73. 10.1002/cncr.31346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Maubec E, Petrow P, Scheer-Senyarich I, et al. Phase II study of cetuximab as first-line single-drug therapy in patients with unresectable squamous cell carcinoma of the skin. J Clin Oncol 2011;29:3419–26. 10.1200/JCO.2010.34.1735 [DOI] [PubMed] [Google Scholar]
- 13. Montaudié H, Viotti J, Combemale P, et al. Cetuximab is efficient and safe in patients with advanced cutaneous squamous cell carcinoma: a retrospective, multicentre study. Oncotarget 2020;11:378–85. 10.18632/oncotarget.27434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Boutros A, Cecchi F, Tanda ET, et al. Immunotherapy for the treatment of cutaneous squamous cell carcinoma. Front Oncol 2021;11:733917. 10.3389/fonc.2021.733917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Twomey JD, Zhang B. Cancer immunotherapy update: FDA-approved checkpoint inhibitors and companion diagnostics. AAPS J 2021;23:39. 10.1208/s12248-021-00574-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ahmed SR, Petersen E, Patel R, et al. Cemiplimab-rwlc as first and only treatment for advanced cutaneous squamous cell carcinoma. Expert Review of Clinical Pharmacology 2019;12:947–51. 10.1080/17512433.2019.1665026 [DOI] [PubMed] [Google Scholar]
- 17. Maubec E. Update of the management of cutaneous squamous-cell carcinoma. Acta Derm Venereol 2020;100:5753. 10.2340/00015555-3498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kamiya S, Kato J, Kamiya T, et al. Association between PD-L1 expression and lymph node metastasis in cutaneous squamous cell carcinoma. Asia Pac J Clin Oncol 2020;16:e108–12. 10.1111/ajco.13102 [DOI] [PubMed] [Google Scholar]
- 19. LIBTAYO® . Regeneron Pharmaceuticals, Inc; 2021.
- 20. Vafaei S, Zekiy AO, Khanamir RA, et al. Combination therapy with immune checkpoint inhibitors (ICIs); a new frontier. Cancer Cell Int 2022;22:2. 10.1186/s12935-021-02407-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stratigos AJ, Garbe C, Dessinioti C, et al. European interdisciplinary guideline on invasive squamous cell carcinoma of the skin: part 2. Treatment. Eur J Cancer 2020;128:83–102. 10.1016/j.ejca.2020.01.008 [DOI] [PubMed] [Google Scholar]
- 22. LIBTAYO® (cemiplimab) . Australian product information. Sanofi-Aventis Australia Pty Ltd; 2020.
- 23. Wang Y, Zhou S, Yang F, et al. Treatment-related adverse events of PD-1 and PD-L1 inhibitors in clinical trials: a systematic review and meta-analysis. JAMA Oncol 2019;5:1008–19. 10.1001/jamaoncol.2019.0393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Baxi S, Yang A, Gennarelli RL, et al. Immune-related adverse events for anti-PD-1 and anti-PD-L1 drugs: systematic review and meta-analysis. BMJ 2018;360:k793. 10.1136/bmj.k793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pillai RN, Behera M, Owonikoko TK, et al. Comparison of the toxicity profile of PD-1 versus PD-L1 inhibitors in non-small cell lung cancer: a systematic analysis of the literature. Cancer 2018;124:271–7. 10.1002/cncr.31043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Khunger M, Rakshit S, Pasupuleti V, et al. Incidence of pneumonitis with use of programmed death 1 and programmed death-ligand 1 inhibitors in non-small cell lung cancer: a systematic review and meta-analysis of trials. Chest 2017;152:271–81. 10.1016/j.chest.2017.04.177 [DOI] [PubMed] [Google Scholar]
- 27. Spagnuolo A, Gridelli C. Comparison of the toxicity profile of PD-1 versus PD-L1 inhibitors in non-small cell lung cancer": is there a substantial difference or not? J Thorac Dis 2018;10(Suppl 33):S4065–8. 10.21037/jtd.2018.09.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gorelik L, Avgerinos G, Kunes Y, et al. Abstract 4606: Preclinical characterization of a novel fully human IgG1 anti-PD-L1 mAb CK-301. Cancer Res 2017;77(13_Supplement):4606. 10.1158/1538-7445.AM2017-4606 [DOI] [Google Scholar]
- 29. Lin L, Hilbert J, Gorelik L, et al. Semi-mechanistic PK and target-occupancy modeling to support dose justification for anti-PD-L1 clinical candidate CK-301 (cosibelimab) in oncology patients. Poster presented at: Society for Immunotherapy of Cancer 34th Annual Meeting; National Harbor, MD, 2019.. [Google Scholar]
- 30. Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c869. 10.1136/bmj.c869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lin L, Hillbert J, Gorelik L, et al. Semi-mechanistic PK and target-occupancy modeling to support dose justification for anti-PD-L1 clinical candidate CK-301 (TG-1501) in oncology patients [abstract P431]. Abstract presented at: Society for Immunotherapy of Cancer 34th Annual Meeting; National Harbor, MD, 2019.. [Google Scholar]
- 32. Greco S, Pugliese G, Rimini M, et al. Treatment of locally advanced and metastatic cutaneous squamous cell carcinoma. Recenti Prog Med 2021;112:69e–74e. 10.1701/3620.36035 [DOI] [PubMed] [Google Scholar]
- 33. Rischin D, Migden MR, Lim AM, et al. Phase 2 study of cemiplimab in patients with metastatic cutaneous squamous cell carcinoma: primary analysis of fixed-dosing, long-term outcome of weight-based dosing. J Immunother Cancer 2020;8:e000775. 10.1136/jitc-2020-000775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schmults CD, Blitzblau R, Aasi SZ, et al. NCCN guidelines® insights: squamous cell skin cancer, version 1.2022. J Natl Compr Canc Netw 2021;19:1382–94. 10.6004/jnccn.2021.0059 [DOI] [PubMed] [Google Scholar]
- 35. Cancer Council . UV index, Available: https://www.cancer.org.au/cancer-information/causes-and-prevention/sun-safety/uv-index [Accessed 24 May 2023].
- 36. Migden MR, Rischin D, Schmults CD, et al. PD-1 blockade with cemiplimab in advanced cutaneous squamous-cell carcinoma. N Engl J Med 2018;379:341–51. 10.1056/NEJMoa1805131 [DOI] [PubMed] [Google Scholar]
- 37. Grob J-J, Gonzalez R, Basset-Seguin N, et al. Pembrolizumab monotherapy for recurrent or metastatic cutaneous squamous cell carcinoma: a single-arm phase II trial (KEYNOTE-629). J Clin Oncol 2020;38:2916–25. 10.1200/JCO.19.03054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Maubec E, Boubaya M, Petrow P, et al. Phase II study of pembrolizumab as first-line, single-drug therapy for patients with unresectable cutaneous squamous cell carcinomas. J Clin Oncol 2020;38:3051–61. 10.1200/JCO.19.03357 [DOI] [PubMed] [Google Scholar]
- 39. Gross ND, Miller DM, Khushalani NI, et al. Neoadjuvant cemiplimab for stage II to IV cutaneous squamous-cell carcinoma. N Engl J Med 2022;387:1557–68. 10.1056/NEJMoa2209813 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2023-007637supp001.pdf (114.8KB, pdf)
jitc-2023-007637supp002.pdf (75.8KB, pdf)
jitc-2023-007637supp003.pdf (298.3KB, pdf)
jitc-2023-007637supp004.pdf (25.2KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The data supporting the findings of this study are available within the article and its supplementary materials. Any additional data requests are available upon reasonable request to the corresponding author.