Abstract
Exposure to intimate partner violence (IPV) incurs significant public health consequences. Understanding risk markers can accelerate prevention and response efforts, important in settings like Sub-Saharan Africa (SSA) where resources are scarce. In this study, four databases were searched to identify studies that examined risk markers for male-to-female physical IPV. With application of the socioecological model, we analyzed 11 risk markers for male physical IPV perpetration (with 71 effect sizes) and 16 risk markers for female physical IPV victimization (with 131 effect sizes) in SSA from 51 studies. For male IPV perpetration, we found medium-to-large effect sizes for six risk markers: perpetrating emotional abuse and sexual IPV, witnessing parental IPV, being abused as a child, cohabitating (not married), and exhibiting controlling behaviors. We found small effect sizes for substance use. Employment, age, marital status, and education were not significant risk markers. For female IPV victimization, a medium effect size was found for post-traumatic stress symptoms. Small effect sizes were found for reporting depressive symptoms, being abused as a child, witnessing parental IPV, and reporting drug and alcohol use. Rural residence, approval of violence, length of relationship, income, education, employment, age, marital status, and religiosity were not significant risk markers. Findings highlight opportunities for screening and intervention at the couple level, show the need to test and incorporate interventions for IPV in mental health treatment, and emphasize the importance of further research on sociodemographic risk markers and the interventions that target them.
Keywords: Africa, domestic violence, intimate partner violence, low- and middle-income countries, risk marker, socioecological model
Intimate partner violence (IPV)—acts of physical, sexual, or psychological harm in an intimate relationship (World Health Organization, 2017)—is a serious public health concern. Women are more likely to experience violence from intimate partners than from any other type of perpetrator (García-Moreno et al., 2013). As such, IPV affects around one-third of women globally (Devries, Mak, Bacchus, et al., 2013). A seminal World Health Organization (WHO) survey conducted in 15 sites across 10 countries with 24,097 girls and women between the ages of 15 and 49 found that 15% to 71% of women reported experiencing physical or sexual violence in their lifetime (Garcia-Moreno et al., 2006). Due to its numerous deleterious effects on health, mental wellness, and child wellbeing, IPV has been identified as a critical social determinant of health.
Rates of IPV vary significantly across country and industrialized/rural settings (Devries, Mak, Bacchus, et al., 2013; Garcia-Moreno et al., 2006), suggesting that cultural and sociopolitical factors influence risk markers for victimization and perpetration. Global IPV prevalence is highest in Sub-Saharan Africa (SSA), where rates reach 70% in some countries (Garcia-Moreno et al., 2006). SSA, a highly diverse region in Africa mostly located below the Sahara Desert, consists of four subregions (Eastern, Central, Western, and Southern Africa) that encompass 48 countries with over 1 billion inhabitants who speak around 1,500 languages (United Nations, 2020).
Most countries in SSA are categorized as low-income with half of the countries having one-third of the population living in poverty (Schoch & Lakner, 2020). Serving as key structures in the prevention of and response to IPV (Miller & McCaw, 2019), healthcare systems across SSA suffer from lack of funding, poor infrastructure, and scarce human and material resources. The Lancet Commission on the future of health in SSA identified social determinants of health as a critical area for action to improve healthcare systems and achieve health equity (Agyepong et al., 2017), and research on risk markers for IPV in SSA has proliferated in the last two decades. As expanding and implementing universal healthcare is a top priority to achieve the third United Nations Sustainable Development Goal by 2030 (Falchetta et al., 2020), a synthesis of the IPV literature is timely and needed to inform screening, prevention, and response efforts that can be integrated into burgeoning healthcare systems to improve health and mental health outcomes.
Theoretical Framework
Bronfenbrenner (1977) developed the socioecological framework to attend to the importance of the social environment on individual behaviors. A series of concentric circles represents levels in the environment. Others have adapted Bronfenbrenner’s model specifically to conceptualize violence (Heise, 1998; Krauss, 2006). The WHO has advocated for the use of an ecological model to understand almost all forms of interpersonal violence intervention and prevention to conceptualize violence as a public health problem (Krug et al., 2002). WHO’s model includes four social levels termed individual, relationship, community, and societal that align with Bronfenbrenner’s conceptual hierarchy. Heise (1998) pioneered the application of the ecological framework to violence against women and examined both local and cross-cultural literature to explore variables related to IPV perpetration and victimization. We applied the socioecological model because of its public health scope and ability to classify multifactorial risk markers into nested levels in social, community, relational (family), and individual spheres. Most studies examine risk factors at the individual level, although risk factors exist at all levels of the socioecological model.
Individual Factors
Factors related to the individual victim or offender are considered “individual” factors. IPV is related to multiple negative health and mental health disorders that, in turn, pose higher risk for IPV exposure. IPV can result in serious physical injury and, relatedly, having a poor health status or disability heightens risk for IPV (World Health Organization, 2016). A systematic review of IPV research in Africa included a review of 18 studies conducted from 2000 to 2010 addressing prevalence and risk markers for any form of IPV among pregnant women (Shamu et al., 2011). Shamu et al. (2011) found that for pregnant women, having a positive HIV status, history of violence, low socioeconomic status (SES), young age, alcohol use, and having more than five lifetime sexual partners were all risk markers for female IPV victimization at the individual level. A Demographic Health Survey report of IPV across 10 countries found that unintended pregnancy and terminated pregnancies were associated with IPV victimization in most studies (Hindin et al., 2008). They did not examine risk markers for perpetration or for male victimization and did not examine risk markers in other levels of the socioecological model. Another study in South Africa, which surveyed 340 pregnant women, found that women who were unemployed, had low education, and positive HIV status were more likely to be IPV victims (Hoque et al., 2009). However, other SSA research has not supported this assertion. A longitudinal study in Uganda for example, showed that having a positive HIV status and pregnancy status were not associated with IPV victimization (Kouyoumdjian et al., 2013).
Global reviews and meta-analyses of research that examined mental health disorders and IPV have found a strong correlation between IPV and common mental disorders (depression, anxiety, and Post-traumatic Stress Disorder [PTSD]; Capaldi et al., 2012; Devries, Mak, Garcia-Moreno, et al., 2013; Spencer et al., 2019; Trevillion et al., 2012). This relation is often bidirectional and has been confirmed through longitudinal analysis (Bacchus et al., 2018). A meta-analysis of 16 studies showed that, in comparison to women without mental disorders, women with PTSD, anxiety, or depression were at higher risk for experiencing IPV (Trevillion et al., 2012). Suicidality and alcohol use are additional individual risk markers that have been consistently linked to IPV (Capaldi et al., 2012; Devries, Mak, Garcia-Moreno et al., 2013; Devries et al., 2014; Kouyoumdjian et al., 2013). However, given the global focus of much of the previous research, many of these findings were not specific to SSA nor differentiated by location and cultural context. A meta-analysis of studies addressing gender-based violence in SSA from 2008 to 2019 found that women’s low educational attainment, depression, substance use, low SES, and having accepting attitudes toward gender-based violence were individual factors associated with IPV (Muluneh et al., 2021).
Relational Risk Markers
The meta-analysis discussed above (Muluneh et al., 2021) found that women married to men who had multiple sex partners were more likely to be IPV victims. In addition, they found that previous child and family violence were relational risk markers (Muluneh et al., 2021). A national population-based survey in eight SSA countries with 20,639 adults examined physical IPV victimization in both men and women (Andersson et al., 2007). While the strongest risk marker for both male and female victimization was having multiple sex partners, additional risk markers included having gender inequitable attitudes toward sexuality, acceptance of sexual violence, as well as having discrepancy in income between partners. WHO’s global survey across 10 countries (three of which were in SSA) with 24,097 women, found that male partners’ controlling behaviors are associated with their use of physical or sexual IPV in all countries (Garcia-Moreno et al., 2006). The global survey also indicated wide variability of the importance of male partner controlling behaviors in relationship to male perpetration, that reached almost 90% prevalence in SSA in contrast to other survey sites, suggesting presence of sociocultural influences that shape expectations for behaviors in relationships in SSA.
Studies have also established that individual factors, such as unemployment and having a low level of education, can intersect with relational dynamics in couples and families to leave women vulnerable to IPV victimization. Women in SSA have some of the lowest rates of secondary education globally with less than one-third of women over the age of 25 having achieved some secondary education (United Nations Development Programme (UNDP), 2020). Having a low SES, for example, can produce inequitable relationships where the male partner has a higher income and education, and women are economically dependent on them. Inequitable relationships such as these can be related to IPV. A South African study found that inequity in relationships (e.g., women being economically dependent on men) was significantly related to IPV (Zembe et al., 2015). In addition, a longitudinal analysis with data from 128 women in South Africa revealed that being in a relationship that was inequitable was also associated with IPV victimization (Jewkes et al., 2010).
Social/Community Risk Markers
Risk markers that extend beyond the individual and the relationship are likewise pertinent. For instance, socioeconomic and sociopolitical factors interact with IPV. Data from 46 low- and middle-income countries (LMICs) showed that women who were poorer, younger, and lived in rural areas were more likely to experience IPV victimization (Coll et al., 2020). SSA has experienced its first recession in two decades due to the COVID-19 pandemic, which has exacerbated poverty levels and inequity, and the recession has resulted in 32 million people living in extreme poverty (Selassie & Hakobyan, 2021). The UNDP (2016) developed the Gender Inequality Index using indices of reproductive choice and participation in decision-making and discovered a relation between poverty and gender inequality, which indicated that the countries with the lowest development indexes exhibited the highest rates of gender inequality. Many experts have asserted that family violence, such as IPV, cannot be fully understood without considering gender, power dynamics, and sexism (Heise, 1998; Yllö, 2006). Gender role dynamics that relate to IPV include: who holds power in familial relationships; whether masculinity is defined by dominance and aggression; if a culture endorses hypermasculinity; the extent to which women are perceived as being the property of men; and the cultural endorsement of physically punishing women (Heise, 1998).
The Present Study
The purpose of this study was to quantitatively synthesize the burgeoning body of literature on risk markers for victimization and perpetration of male-to-female physical IPV in SSA where IPV rates are among the highest. Our search was broad enough to encapsulate risk markers that spanned the different levels of the socioecological model to inform prevention and response options. Physical IPV is much more commonplace than sexual IPV (Devries, Mak, Bacchus, et al., 2013; Garcia-Moreno et al., 2006), even with consideration that sexual IPV is likely to be more stigmatized and therefore underreported. Many studies combine different types of IPV, although important differences between risk markers may exist. We have elected to examine risk markers for physical IPV to enhance specificity that can lead to more precise prevention and response recommendations. Fewer studies in SSA have examined risk markers for female perpetration of IPV. Therefore, we have only included studies that examined risk markers for male perpetration and female victimization. Through the use of a meta-analysis, we sought to examine all risk markers for male-to-female physical IPV in SSA identified in the literature. We purposively developed a diverse team of co-authors from the US, SSA, and Brazil to increase the likelihood that this meta-analysis was designed and interpreted accurately. All co-authors were involved in “shaping and determining the interpretation of findings” (Bent-Goodley, 2021, p. 4984).
Methods
Literature Search
To obtain studies to include in the analysis, standard procedures outlined by Card (2012) were followed. Database searches were utilized to identify studies to be included in the meta-analysis. Peer-reviewed journal articles, dissertations, and theses published between 1980 and March 2021 were identified from Proquest, Google Scholar, PubMed, and Web of Science. Boolean search terms were used that included search terms related to intimate relationships (marital OR spous* OR husband OR wife OR intimate partner OR relationship OR same-sex partner), violence (aggress* OR domestic violence OR abus* OR batter OR maltreat* OR violen*), risk markers (predictor OR risk OR factor OR path* OR correlate*), and Africa (Sub-Sahara* Africa OR Africa OR Algeria OR Angola OR Benin OR Botswana OR Burkina Faso OR Burundi OR Cabo Verde OR Cameroon OR Central African Republic OR Chad OR Comoros OR Democratic Republic of the Congo OR Republic of the Congo OR Cote d’Ivoire OR Djibouti OR Egypt OR Equatorial Guinea OR Eritrea OR Eswatini OR Ethiopia OR Gabon OR The Gambia OR Ghana OR Guinea OR Guinea-Bissau OR Kenya OR Lesotho OR Liberia OR Libya OR Madagascar OR Malawi OR Mali OR Mauritania OR Mauritius OR Morocco OR Mozambique OR Namibia OR Niger OR Nigeria OR Rwanda OR Saint Helena, Ascension, and Tristan da Cunha OR Sao Tome and Principe OR Senegal OR Seychelles OR Sierra Leone OR Somalia OR South Africa OR South Sudan OR Sudan OR Tanzania OR Togo OR Tunisia OR Uganda OR Zambia OR Zimbabwe). Lastly, hand-picking strategies from previous research on risk markers for IPV perpetration and victimization in SSA were also utilized to identify additional studies.
Inclusion and Exclusion Criteria
Articles were included in the study if they (a) examined risk markers for physical IPV, (b) examined male perpetration or female victimization of IPV, (c) included at least one bivariate effect size examining the relationship between IPV and a risk marker, (d) the sample was collected in a country in Africa, (e) examined adult relationships, and (f) were written in English.
Studies were excluded from the meta-analysis if they (a) did not examine physical IPV, (b) did not examine risk markers for male perpetration or female victimization, (c) did not include at least one bivariate effect size to be included in the study, (d) did not examine adult intimate relationships, or (e) were not written in English.
The database searches and hand-picking techniques identified a total of 5,187 articles. For the first round of screening, titles and abstracts were reviewed. If it was at all possible that studies could be included in the meta-analysis, they were included in the second round of screening. If it was clear that articles did not meet the inclusion criteria, they were removed during the first round of screening. A total of 4,281 studies were removed in the first round of screening, leaving 906 studies included in the second round of screening. The second round of screening consisted of full-article reviews to determine if the studies met the inclusion criteria. Ultimately, 855 studies were excluded in the second round of screening (see Figure 1). A total of 260 studies were excluded because they did not examine IPV at all, 215 were duplicates, 192 did not include at least one bivariate effect size examining the relationship between IPV and a risk marker, 111 did not look at physical IPV, 46 were qualitative studies or review articles, and 31 examined teen dating violence. A total of 51 studies, all of which were from SSA, met the inclusion criteria and were included in the meta-analysis.
Figure 1.
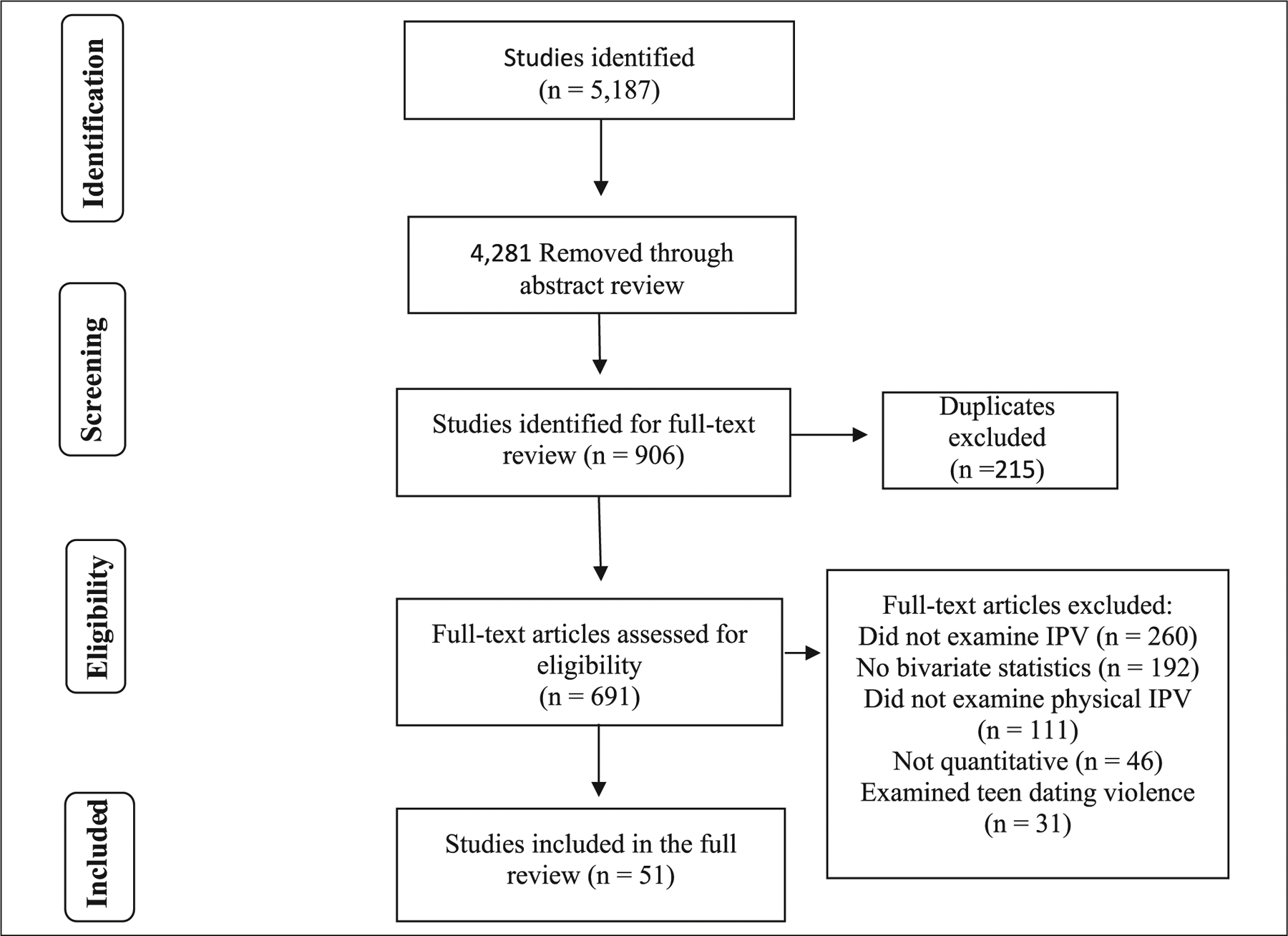
Flowchart of included studies.
Coding Procedures
Typical protocols were followed to code the articles included in the study (Card, 2012). A 37-item code sheet was developed to collect pertinent information from each article included in the analysis. Information collected from each article included study characteristics, such as the sample size, gender of participants, how the data were collected, study design (longitudinal or cross-sectional), and statistical information used to calculate effect sizes to be included in the analysis. All studies were coded together by two research team members. If the coding team members were unsure or disagreed about how to code something, they would discuss the question or discrepancy in understanding until coming to consensus or consult with the lead analyst to work together to come to an agreement. Discrepancies mostly concerned whether or how to report an outcome statistic.
Analysis Plan
Comprehensive Meta-Analysis 3.0 software (Borenstein et al., 2014) was used to run the meta-analyses. The meta-analysis followed an analysis plan outlined by Spencer et al. (2020). The study utilized a random-effects approach when analyzing the data to account for within- and between-study variance (Borenstein et al., 2010). A random effects approach takes into account population differences between unique studies (Borenstein et al., 2010). This allows for the results to be more generalizable compared to a fixed-effects approach. When risk markers were identified in at least three unique studies (Cumming, 2012), an aggregate effect size was calculated for that risk marker. Using each individual study as the unit of measurement, we calculated a Pearson’s r for each risk marker present in two or more studies and used Cohen’s (1992) criteria that states r < .10 is trivial, r = .10 to .29 is small, r = .30 to .49 is medium, and r > .50 is a large effect. When significant risk markers were found, we ran additional analysis to test for potential publication bias (Hunter & Schmidt, 2004). Publication bias refers to the term that insignificant results have a tendency to not be published compared to significant findings, leading to a potential publication bias. We calculated the classic fail-safe n (Rosenthal, 1979), which provides the number of insignificant studies that would need to be included for the current effect sizes to no longer be significant.
Results
See Table 1 for an overview of the studies included in the meta-analysis and Table 2 for risk marker outcomes. The strongest risk markers for male physical IPV perpetration were relational and included the male having also perpetrated emotional IPV against the victim (r = .57, p < .001; see Table 2), followed by the male partner also perpetrating sexual IPV (r = .40, p < .01), the male having witnessed parental IPV as a child (r = .37, p < .001), and the male having experienced child abuse victimization (r = .36, p < .001). Other relational significant risk markers for IPV perpetration were cohabitating but not being married (r = .31, p < .001) and controlling behaviors (r = .30, p < .001). Individual risk markers of drug (r = .28, p < .001) and alcohol use (r = .27, p < .001) were also significant. Employment status (individual, community), age, marital status (relational), and levels of education (individual, community) were not significantly related to physical IPV perpetration for men.
Table 1.
Characteristics of Studies Included in the Analysis.
| Authors | Article Type | Sample Size | Study Type | Sample Location |
|---|---|---|---|---|
| Abrahams and Jewkes (2005) | Peer Reviewed Article | 1,368 | Cross-Sectional | South Africa (Cape Town) |
| Abrahams et al. (2006) | Peer Reviewed Article | 1,368 | Cross-Sectional | South Africa |
| Adebowale (2018) | Peer Reviewed Article | 6,765 | Cross-Sectional | Nigeria |
| Adjah and Agbemafle (2016) | Peer Reviewed Article | 1,524 | Cross-Sectional | Ghana |
| Afe et al. (2016) | Peer Reviewed Article | 77 | Cross-Sectional | Nigeria |
| Balogun et al. (2013) | Peer Reviewed Article | 300 | Cross-Sectional | Nigeria |
| Barchi et al. (2018) | Peer Reviewed Article | 469 | Cross-Sectional | Kenya |
| Barchi et al. (2020) | Peer Reviewed Article | 684 | Cross-Sectional | Kenya |
| Bernards and Graham (2013) | Peer Reviewed Article | 37,320 | Cross-Sectional | Uganda |
| Choi and Ting (2008) | Peer Reviewed Article | 4,948 | Cross-Sectional | South Africa |
| Conroy (2014) | Peer Reviewed Article | 844 | Cross-Sectional | Malawi |
| Deribe et al. (2012) | Peer Reviewed Article | 844 | Cross-Sectional | Ethiopia |
| Deyessa et al. (2009) | Peer Reviewed Article | 1,994 | Cross-Sectional | Ethiopia |
| Dibaba (2008) | Peer Reviewed Article | 308 | Cross-Sectional | Ethiopia |
| Dim (2019) | Peer Reviewed Article | 26,403 | Cross-Sectional | Nigeria |
| Fawole et al. (2005) | Peer Reviewed Article | 431 | Cross-Sectional | Nigeria |
| Fesena et al. (2012) | Peer Reviewed Article | 422 | Cross-Sectional | Ethiopia |
| Fielding-Miller and Dunkle (2017) | Peer Reviewed Article | 401 | Cross-Sectional | Swaziland |
| Flake and Forste (2006) | Peer Reviewed Article | 588 | Cross-Sectional | Dominican Republic |
| Flegar et al. (2011) | Peer Reviewed Article | 40 | Cross-Sectional | South Africa |
| Fonck et al. (2005) | Peer Reviewed Article | 520 | Cross-Sectional | Kenya |
| Gage and Thomas (2017) | Peer Reviewed Article | 20,311 | Cross-Sectional | Nigeria |
| Gass (2011) | Peer Reviewed Article | 1,715 | Cross-Sectional | South Africa |
| Groves et al. (2015) | Peer Reviewed Article | 445 | Longitudinal | South Africa |
| Gupta et al. (2008) | Peer Reviewed Article | 834 | Cross-Sectional | South Africa |
| Gust et al. (2021) | Peer Reviewed Article | 8,003 | Cross-Sectional | Kenya |
| Issahanku (2012) | Dissertation | 443 | Cross-Sectional | Ghana |
| Jaoko (2005) | Dissertation | 208 | Cross-Sectional | Kenya |
| Jewkes et al. (2002) | Peer Reviewed Article | 1,279 | Cross-Sectional | South Africa |
| Karamagi et al. (2006) | Peer Reviewed Article | 457 | Cross-Sectional | Uganda |
| Kimuna, et al. (2018) | Peer Reviewed Article | 4,512 | Cross-Sectional | Kenya |
| Machisa et al. (2016) | Peer Reviewed Article | 416 | Cross-Sectional | South Africa |
| Malan et al. (2018) | Peer Reviewed Article | 150 | Cross-Sectional | South Africa |
| Mandal (2013) | Peer Reviewed Article | 8,385 | Cross-Sectional | Malawi |
| Meade et al. (2012) | Peer Reviewed Article | 3,328 | Cross-Sectional | South Africa |
| Moore (2008) | Peer Reviewed Article | 2,759 | Cross-Sectional | Togo |
| Mthembu et al. (2016) | Peer Reviewed Article | 975 | Cross-Sectional | South Africa |
| Owoaje and OlaOlorun (2012) | Peer Reviewed Article | 924 | Cross-Sectional | Nigeria |
| Peltzer et al. (2013) | Peer Reviewed Article | 268 | Cross-Sectional | South Africa |
| Peltzer (2013) | Peer Reviewed Article | 607 | Cross-Sectional | South Africa |
| Pengpid and Peltzer (2013) | Peer Reviewed Article | 268 | Cross-Sectional | South Africa |
| Prabhu et al. (2011) | Peer Reviewed Article | 2,436 | Cross-Sectional | Tanzania |
| Sa and Larsen (2007) | Peer Reviewed Article | 1,418 | Cross-Sectional | Tanzania |
| Stockl et al. (2010) | Peer Reviewed Article | 1,721 | Cross-Sectional | Tanzania |
| Sunmola et al. (2021) | Peer Reviewed Article | 20,101 | Cross-Sectional | Nigeria |
| Tlapek (2015) | Peer Reviewed Article | 1,821 | Cross-Sectional | Democratic Republic of Congo |
| Tumwesigye et al. (2012) | Peer Reviewed Article | 1,743 | Cross-Sectional | Uganda |
| Umubyei (2014) | Peer Reviewed Article | 917 | Cross-Sectional | Rwanda |
| van der Straten et al. (1998) | Peer Reviewed Article | 921 | Cross-Sectional | Rwanda |
| Wong et al. (2008) | Peer Reviewed Article | 395 | Cross-Sectional | South Africa (Cape Town) |
| Zacarias et al. (2012) | Peer Reviewed Article | 1,442 | Cross-Sectional | Mozambique |
Table 2.
Risk Markers for Perpetration and Victimization of Male-to-Female IPV From Studies in SSA.
| Risk Marker | k | r | 95% CI | Classic Fail-Safe N |
|---|---|---|---|---|
| Male Perpetration | ||||
| Emotional IPV PerpetrationR | 4 | .57*** | [0.44, 0.67] | 477 |
| Sexual IPV PerpetrationR | 5 | .40** | [0.11, 0.63] | 402 |
| Witness Parental IPVR | 6 | .37*** | [0.26, 0.47] | 398 |
| Abused as a ChildR | 5 | .36*** | [0.25, 0.46] | 195 |
| Cohabitating (Not Married)R | 3 | .31*** | [0.15, 0.45] | 41 |
| Controlling BehaviorsR | 5 | .30*** | [0.22, 0.39] | 2,344 |
| Drug UseI | 5 | .28*** | [0.12, 0.43] | 53 |
| Alcohol UseI | 21 | .27*** | [0.23, 0.30] | 8,947 |
| EmployedI,C | 7 | .01 | [−0.06, 0.08] | — |
| Age (Older)I | 4 | .00 | [−0.00, 0.00] | — |
| MarriedR | 3 | −.01 | [−0.20, 0.20] | — |
| Education (Higher)I,C | 5 | −.05 | [−0.11, 0.01] | — |
| Female Victimization | ||||
| Post-traumatic Stress SymptomsI | 5 | .45*** | [0.23, 0.62] | 181 |
| Depressive SymptomsI | 10 | .26*** | [0.14, 0.36] | 326 |
| Abused as a ChildR | 3 | .26*** | [0.12, 0.40] | 41 |
| Witness Parental IPVR | 9 | .22*** | [0.10, 0.34] | 240 |
| Drug UseI | 5 | .22** | [0.09, 0.34] | 23 |
| Alcohol UseI | 15 | .21*** | [0.16, 0.26] | 508 |
| Rural ResidenceC | 4 | .08*** | [0.04, 0.11] | 95 |
| Approval of ViolenceI,S | 4 | .08 | [−0.00, 0.17] | — |
| Length of RelationshipR | 3 | .05 | [−0.04, 0.14] | — |
| Number of ChildrenR | 12 | .04* | [0.02, 0.07] | 97 |
| Income (Higher)I,C | 7 | .03 | [−0.03, 0.08] | — |
| Education (Higher)I,C | 14 | .02 | [−0.03, 0.07] | — |
| EmployedI,C | 13 | .02 | [−0.03, 0.06] | — |
| Age (Older)I | 16 | −.00 | [−0.00, 0.00] | — |
| ReligiosityI | 4 | −.09 | [−0.23, 0.05] | — |
| MarriedR | 13 | −.14 | [−0.32, 0.05] | — |
Note. R = relational level; I = individual level; C = community level; S = societal level; k = effect sizes, r = Pearson’s r; CI = confidence interval.
p < .05.
p < .01.
p < .001.
The strongest risk markers for female physical IPV victimization were individual level risk markers of her experiencing PTSD (r = .45, p < .001) and depressive symptoms (r = .26, p < .001). Relational level risk markers of child abuse victimization (r = .26, p < .001) and witnessing parental IPV as a child (r = .22, p < .001) were likewise significant. Individual level risk markers related to drug (r = .22, p < .01) and alcohol use (r = .21, p < .001), living in a rural residence (r = .08, p < .001), and having more children (r = .04, p < .05) were all significant risk markers for physical IPV victimization for women. Approval of violence, length of relationship, higher income, education, being employed, older age, being married, and religiosity were not significant risk markers for IPV victimization.
Discussion
In the last two decades, global research has shown that some of the highest rates of physical IPV are present in SSA. Subsequent studies across SSA that identify IPV risk markers have proliferated, providing an unprecedented opportunity to design prevention and response interventions that more precisely target risk markers. This is one of the first meta-analyses to quantitatively synthesize IPV risk markers across the levels of the socioecological model in SSA. Main findings revealed that the most prominent risk markers for male physical IPV perpetration were relational, such as perpetrating other forms of IPV and men’s exposure to and witnessing of violence as a child in their family of origin. In contrast, the risk markers for female victimization were related to mental distress (individual level) and family of origin exposure to violence (relational level).
Relational Risk Markers for IPV Perpetration
The strongest associations for perpetration of IPV were risk markers situated at the relational level of the socioecological model, which included perpetration of other forms of IPV, cohabitating while not being married, and exhibiting controlling behaviors. These risk markers speak to the importance of integrating screening beyond physical IPV only and including screening for emotional or sexual IPV. Perhaps emotional IPV, which showed a large effect size, carries less stigma than physical or sexual IPV and could serve as a proxy screening domain for the more stigmatized forms of IPV. Given the relational context of these risk markers, it follows that programming should consider addressing IPV with a relationally based intervention. In high-income countries, state-mandated treatment for IPV perpetrators that involves gender-specific men-only treatment is generally ineffective (Crane et al., 2014; Dutton & Corvo, 2007; Eckhardt et al., 2014) but remains widespread due to concerns of victim advocates that couples-based treatment might provoke or exacerbate violence (Armenti & Babcock, 2016). However, in SSA countries such as Uganda (Horn et al., 2016), sociocultural factors have discouraged women’s separation from abusive male partners. Interventions, therefore, should aim to improve family relationships and reduce violence within families when women do not have options to leave or choose to remain in their relationships rather than rely only on interventions focusing on women leaving violent family spaces (Mootz et al., 2020).
Researchers (McCollum & Stith, 2008; Stith & McCollum, 2011; Stith et al., 2012) have demonstrated that conjoint treatment for IPV can be both safe and effective (Antunes-Alves & de Stefano, 2014; Stith & McCollum, 2011).With careful screening to ensure IPV is not severe, rigorous training of providers, and ongoing risk assessment and safety planning, couples can reduce IPV and improve their relationship through enhanced communication and problem-solving skills (Antunes-Alves & de Stefano, 2014; Armenti & Babcock, 2016; Hurless & Cottone, 2018). A meta-analysis of randomized controlled trials of conjoint therapies for IPV showed that conjoint interventions resulted in significantly greater reductions in IPV than did individual treatments and control conditions (Karakurt et al., 2016). However, these studies were all conducted in high-income settings. One notable couple-based intervention in Zambia found significant reductions in mild to moderate, but not severe, IPV, although the intervention focused on HIV prevention (Jones et al., 2014). More research on acceptability, feasibility, and efficacy of couple-based treatments to reduce IPV in SSA is needed.
Individual Risk Markers for IPV Victimization
Regarding IPV victimization, our meta-analysis confirmed that women’s mental health status at the individual level presented as risk markers with small to medium effect sizes in SSA. While the WHO has recommended first addressing psychosocial stressors such as IPV in mental health treatment, little is known about how to treat IPV experienced by women with common mental disorders in LMICs, such as those found in SSA. A recent review found that only two studies in LMICs had adapted interventions for common mental disorders in women to address IPV (with reduction in common mental disorder symptoms), concluding the need for future research on adapting feasible, acceptable, and effective evidence-based treatments for common mental disorders that address IPV in LMICs (Keynejad et al., 2020). Thus, this research gap constitutes a global mental health care priority (Chibber & Krishnan, 2011).
Witnessing or Experiencing Violence As a Child
Witnessing or experiencing violence as a child were relational risk markers for both male perpetration and female victimization for physical IPV. These family-of-origin relational risk markers have been recognized across settings. A meta-analysis of 46 studies with 56 effect sizes found that experiencing physical, sexual, and psychological abuse and neglect were all associated with IPV victimization (Li et al., 2019), although the effect sizes were small. Another meta-analysis examined the association of child maltreatment and IPV victimization and perpetration among men and found that effect sizes varied according to form of child maltreatment (Godbout et al., 2019). Witnessing IPV as a child has a well-established relationship with IPV. While a systematic review of 19 studies confirmed an association between witnessing IPV as a child and perpetrating IPV as an adult, the quality of these studies was low and measurement of child exposure to IPV varied considerably (Kimber et al., 2018). Having too much measurement variability has presented challenges for evaluating and understanding intergenerational research (Haselschwerdt et al., 2019).
While the strength of the effect sizes of family of origin exposure differed for perpetration (medium) and victimization (small), taken together, the associations suggest that interventions for IPV present an opportunity to interrupt the cycle of violence for future generations. To refine intervention and prevention efforts in SSA where resources may be scarce, more exploration of mediators and moderators for how exposure to family of origin violence relates to exposure to IPV is needed. Many refer to social learning theory to explain that exposure to violence when young normalizes violent behaviors and leads to an increased tolerance for violence in adult relationships (Sellers et al., 2005), yet there are other significant mediators. For example, both IPV perpetration and victimization carried risk markers of alcohol and drug use at the individual level. Substance use and mental health problems are associated both with adverse childhood experiences (Schiff et al., 2014) and adult IPV (Trevillion et al., 2012, 2015), and preventing these disorders from emerging could avert intergenerational transmission of violence.
Community and Societal Level Risk Markers for IPV Perpetration and Victimization
There were fewer risk markers at the community or societal level identified for inclusion in the meta-analysis. While measured at the individual level—employment, education, and income—could represent community level economic opportunities. The finding that community level variables were not significant risk markers for perpetration or victimization of IPV contrasts with other systematic reviews of research in high-income settings and Africa (Capaldi et al., 2012; Shamu et al., 2011). Others have found that the relation between education level and IPV subsides when more proximal variables (e.g., couple conflict) are considered (Capaldi et al., 2012). Income and employment, however, have had more robust associations with IPV even with inclusion of more proximal variables (Capaldi et al., 2012). Our findings could have resulted because we examined risk markers for physical IPV only whereas others (e.g., Muluneh et al., 2021) have looked at risk markers for gender-based violence or combined types of IPV. A cross-sectional study across eight southern African countries likewise found no association between income, education, or employment when examining physical IPV only (Andersson et al., 2007). Perhaps the lack of association points to the complexity of SES, as has been demonstrated in IPV economic intervention research in SSA that shows no effect on reduction of IPV (Glass et al., 2017; Gupta et al., 2013). Given that programmatic resources in SSA and other low-income settings often target economic development (especially for women) as a means of empowerment, these results warrant further consideration as to whether their relation can better be explained with other variables that could be more constructive intervention targets. Finally, measurement of societal level variables, often represented as attitudes toward IPV, lacked representation among studies included in this meta-analysis. Although an analysis of acceptance of physical IPV toward women with data from 39 LMICs found that women in Africa and South Asia were most likely to endorse acceptance (Tran et al., 2016), our analysis found no association between approval of violence and IPV victimization.
Limitations
One potential limitation of this study, which is a limitation of all meta-analyses, is that we may have missed studies to include in the analysis. Additionally, it is possible that studies were not included in the study because of the “file drawer” problem (Hunter & Schmidt, 2004), where insignificant studies go into the “file drawer” and are never published. In order to combat this potential limitation, we conducted publication bias tests for significant findings. In addition to missing studies that were not published, we were also unable to include studies that were not written in English. This could have led to missing key studies examining risk markers for physical IPV in SSA. Another limitation of the study is that we are looking at risk markers of physical IPV perpetration and we cannot determine the temporal ordering of the variables associated with physical IPV perpetration or victimization. For example, the strongest risk marker for female victimization was post-traumatic stress symptoms, which could be a consequence of IPV victimization, but we cannot determine this with the cross-sectional nature of the analysis. Another limitation of the study was the lack of societal-level factors that we were able to identify to be included in the analysis. A positive aspect of this study was the effort to be inclusive and to include all appropriate research focusing on risk markers for male-to-female physical IPV in SSA, which allows for generalization to a broad population of SSA. However, a limitation of this study, in “promoting diversity and inclusion in our research” (Tajima, 2021, p. 4976), is that we needed to rely on authors of manuscripts included in our meta-analysis to carefully support diversity and inclusion with respect to sampling and measurement (Tajima, 2021, p. 4976).
Critical Findings
This is the first meta-analysis to synthesize risk markers for male-to-female IPV in SSA.
This meta-analysis uniquely applied the socioecological model to interpret levels of risk factors and findings.
The strongest risk markers for male IPV perpetration were relational and included other forms of IPV and exposure to family of origin violence.
The strongest risk markers for female IPV victimization were individual and relational and included mental distress and exposure to family of origin violence.
There were fewer community or societal level variables included in this analysis.
Community level variables were not significant risk markers for perpetration or victimization of IPV.
Implications for Practice, Policy, and Research
Integrate screening for emotional or sexual IPV with a focus on emotional IPV given less stigma.
Consider addressing IPV with a relationally based intervention, especially given cultural values that highly stigmatize separation.
Develop research on acceptability, feasibility, and efficacy of couple-based treatments to reduce IPV in SSA to ensure relevance for context.
Adapt evidence-based treatments already in use in SSA for common mental disorders to address IPV.
Explore mediators and moderators for how exposure to family of origin violence relates to exposure to IPV.
Conduct more research on community and societal level variables’ association with IPV in SSA.
Conclusion
This meta-analysis of 51 studies from SSA examined 11 risk markers for perpetration and 16 risk markers for victimization of male-to-female physical IPV. The risk markers for male perpetration that had medium-to-large effect sizes were perpetration of other forms of IPV, exhibition of controlling behaviors, and experiencing abuse as a child, all of which are relational risk markers according to the socioecological model. Alcohol and drug use had small effect sizes for perpetration. Regarding female victimization, risk markers at the individual and relational levels were strongest. Endorsing PTSD symptoms had a medium effect size; and depressive symptoms, abuse as a child, witnessing parental IPV, and drug and alcohol use held small effect sizes for victimization. Demographic risk markers, such as income, employment, and education level were not significantly associated with perpetration or victimization of IPV. Findings highlight opportunities for screening and intervention at the couple level, the need to test and incorporate interventions for IPV in mental health treatment, and further research on sociodemographic risk markers and the interventions that target them.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by the National Institute of Mental Health funded #K23 MH122661.
Biographies
Jennifer Mootz, PhD, is an Assistant Professor of Clinical Medical Psychology (in Psychiatry) at Columbia University. Her research has focused on reducing the global mental health and substance use treatment gap in low-income and humanitarian settings internationally and in the US through digitized innovations and consideration of social determinants.
Chelsea M. Spencer, PhD,is a Research Assistant Professor in the Couple and Family Therapy program at Kansas State University. Her research primarily focuses on intimate partner violence, intimate partner homicide, and sexual violence. Dr. Spencer’s goal is to conduct research that can be utilized in violence prevention and intervention efforts.
Julia Ettelbrick, BA, is a Patient Navigator for The Undetectables Program at Sun River Health. As Patient Navigator, she works directly with individuals living with HIV to support them in maintaining a low viral load through incentivization of antiretroviral therapy adherence.
Bianca Kann, BA, is Project Manager at Columbia University’s Mailman School of Public Health and Research Assistant at the New York Psychiatric Institute. Her work focuses on implementation of evidence-based treatments for adults and adolescents. She is interested in researching the social determinants that shape mental health populations and ways to develop interventions that address barriers to care for diverse communities in low- and middle-income countries.
Palmira Fortunato dos Santos, PhD, is a licensed Clinical Psychologist and guest professor at Eduardo Mondlane University Faculty of Medicine in Mozambique. She is the Mental Health Research Service Coordinator and Mental Health Policies and Services Specialist at the Mozambique Ministry of Health. Her expertise is on task-shifting and integration of mental health into primary care in low-resource settings with a focus on adolescents and intimate partner violence prevention.
Megan Palmer, MS, is a doctoral student in the Couple and Family Therapy program at Kansas State University. Her research primarily focuses on intimate partner violence, trauma bonding, and familial transmission of violence. Megan’s goal is to conduct research to further develop an understanding of violent relationships to better intervene and prevent these outcomes.
Sandra Stith, PhD, is a University Distinguished Professor, emeritus in the Family Therapy program at Kansas State University. In 2011, APA published her book, “Couples Treatment for Domestic Violence: Finding Safe Solutions,” describing a treatment program developed with NIMH funding. Her ongoing research focuses on understanding risk markers for and treatment of partner violence.
Footnotes
Declarations of Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Agyepong IA, Sewankambo N, Binagwaho A, Coll-Seck AM, Corrah T, Ezeh A, Fekadu A, Kilonzo N, Lamptey P, Masiye F, Mayosi B, Mboup S, Muyembe JJ, Pate M, Sidibe M, Simons B, Tlou S, Gheorghe A, Legido-Quigley H, & Piot P (2017). The path to longer and healthier lives for all Africans by 2030: The Lancet Commission on the future of health in sub-Saharan Africa. The Lancet, 390(10114), 2803–2859. 10.1016/S0140-6736(17)31509-X [DOI] [PubMed] [Google Scholar]
- Andersson N, Ho-Foster A, Mitchell S, Scheepers E, & Goldstein S (2007). Risk factors for domestic physical violence: National cross-sectional household surveys in eight southern African countries. BMC Women’s Health, 7(11), 11. 10.1186/1472-6874-7-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antunes-Alves S, & de Stefano J (2014). Intimate partner violence: Making the case for joint couple treatment. The Family Journal, 22(1), 62–68. 10.1177/1066480713505056 [DOI] [Google Scholar]
- Armenti NA, & Babcock JC (2016). Conjoint treatment for intimate partner violence: A systematic review and implications. Couple and Family Psychology: Research and Practice, 5(2), 109–123. 10.1037/cfp0000060 [DOI] [Google Scholar]
- Bacchus LJ, Ranganathan M, Watts C, & Devries K (2018). Recent intimate partner violence against women and health: A systematic review and meta-analysis of cohort studies. BMJ Open, 8(7), e019995. 10.1136/bmjopen-2017-019995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bent-Goodley T (2021). Diversity in interpersonal violence research. Journal of Interpersonal Violence, 36(11–12), 4937–4952. 10.1177/08862605211013003 [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, & Rothstein HR (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods, 1(2), 97–111. 10.1002/JRSM.12 [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges L, Higgins J, & Rothstein H (2014). Comprehensive meta-analysis (No. 3). Biostat. [Google Scholar]
- Bronfenbrenner U (1977). Toward an experimental ecology of human development. American Psychologist, 32(7), 513–531. 10.1037//0003-066x.32.7.513 [DOI] [Google Scholar]
- Capaldi DM, Knoble NB, Shortt JW, & Kim HK (2012). A systematic review of risk factors for intimate partner violence. Partner Abuse, 3(2), 231–280. 10.1891/1946-6560.3.2.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card NA (2012). Applied meta-analysis for social science research. Guilford Press. [Google Scholar]
- Chibber KS, & Krishnan S (2011). Confronting intimate partner violence: A global health priority. Mount Sinai Journal of Medicine, 78(3), 449–457. 10.1002/msj.20259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1992). A power primer. Psychological Bulletin, 112(1), 155–159. 10.1037//0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Coll CVN, Ewerling F, García-Moreno C, Hellwig F, & Barros AJD (2020). Intimate partner violence in 46 low-income and middle-income countries: An appraisal of the most vulnerable groups of women using national health surveys. BMJ Global Health, 5(1), e002208. 10.1136/BMJGH-2019-002208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane CA, Oberleitner LMS, Devine S, & Easton CJ (2014). Substance use disorders and intimate partner violence perpetration among male and female offenders. Psychol Violence, 4(3), 322–333. 10.1037/a0034338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumming G (2012). Understanding the new statistics: Effect sizes, confidence intervals, and meta-analysis. Routledge. [Google Scholar]
- Devries KM, Child JC, Bacchus LJ, Mak J, Falder G, Graham K, Watts C, & Heise L (2014). Intimate partner violence victimization and alcohol consumption in women: A systematic review and meta-analysis. Addiction, 109(3), 379–391. 10.1111/add.12393 [DOI] [PubMed] [Google Scholar]
- Devries KM, Mak JY, Bacchus LJ, Child JC, Falder G, Petzold M, Astbury J, & Watts CH (2013). Intimate partner violence and incident depressive symptoms and suicide attempts: A systematic review of longitudinal studies. PLoS Medicine, 10(5), e1001439. 10.1371/journal.pmed.1001439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devries KM, Mak JYT, Garcia-Moreno C, Petzold M, Child JC, Falder G, Lim S, Bacchus LJ, Engell RE, Rosenfeld L, Pallitto C, Vos T, Abrahams N, & Watts CH (2013). The global prevalence of intimate partner violence against women. Science, 340(6140), 1527–1528. 10.1126/science.1240937 [DOI] [PubMed] [Google Scholar]
- Dutton DG, & Corvo K (2007). The Duluth model: A data-impervious paradigm and a failed strategy. Aggression and Violent Behavior, 12(6), 658–667. 10.1016/j.avb.2007.03.002 [DOI] [Google Scholar]
- Eckhardt C, Murphy C, & Sprunger J (2014). Interventions for perpetrators of intimate partner violence. Psychiatric Times. http://www.psychiatrictimes.com/special-reports/interventions-perpetrators-intimate-partner-violence [Google Scholar]
- Falchetta G, Hammad AT, & Shayegh S (2020). Planning universal accessibility to public health care in sub-Saharan Africa. Proceedings of the National Academy of Sciences, 117(50), 31760–31769. 10.1073/PNAS.2009172117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Moreno C, Jansen HAFM, Ellsberg M, Heise L, & Watts C (2006). Prevalence of intimate partner violence: Findings from the WHO multi-country study on women’s health and domestic violence. The Lancet, 368(9543), 1260–1269. 10.1016/S0140-6736(06)69523-8 [DOI] [PubMed] [Google Scholar]
- García-Moreno C, Pallitto C, Devries K, Stöckl H, Watts C, & Abrahams N (2013). Global and regional estimates of violence against women: Prevalence and health effects of intimate partner violence and non-partner sexual violence. World Health Organization. [Google Scholar]
- Glass N, Perrin NA, Kohli A, Campbell J, & Remy MM (2017). Randomised controlled trial of a livestock productive asset transfer programme to improve economic and health outcomes and reduce intimate partner violence in a postconflict setting. BMJ Global Health, 2(1), e000165. 10.1136/bmjgh-2016-000165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godbout N, Vaillancourt-Morel MP, Bigras N, Briere J, Hébert M, Runtz M, & Sabourin S (2019). Intimate partner violence in male survivors of child maltreatment: A meta-analysis. Trauma, Violence & Abuse, 20(1), 99–113. 10.1177/1524838017692382 [DOI] [PubMed] [Google Scholar]
- Gupta J, Falb KL, Lehmann H, Kpebo D, Xuan Z, Hossain M, Zimmerman C, Watts C, & Annan J (2013). Gender norms and economic empowerment intervention to reduce intimate partner violence against women in rural Côte d’Ivoire: A randomized controlled pilot study. BMC International Health and Human Rights, 13(1), 46. 10.1186/1472-698X-13-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haselschwerdt ML, Savasuk-Luxton R, & Hlavaty K (2019). A methodological review and critique of the “intergenerational transmission of violence” literature. Trauma, Violence, and Abuse, 20(2), 168–182. 10.1177/1524838017692385 [DOI] [PubMed] [Google Scholar]
- Heise LL (1998). Violence against women: An integrated, ecological framework. Violence Against Women, 4(3), 262–290. 10.1177/1077801298004003002 [DOI] [PubMed] [Google Scholar]
- Hindin MJ, Kishor S, & Ansara DL (2008). Intimate partner violence among couples in 10 DHS countries: Predictors and health outcomes. DHS Analytical Studies No 18. Macro International Inc. [Google Scholar]
- Hoque ME, Hoque M, & Kader SB (2009). Prevalence and experience of domestic violence among rural pregnant women in KwaZulu-Natal, South Africa. Southern African Journal of Epidemiology and Infection, 24(4), 34–37. 10.1080/10158782.2009.11441360 [DOI] [Google Scholar]
- Horn R, Puffer ES, Roesch E, & Lehmann H (2016). “I don’t need an eye for an eye”: Women’s responses to intimate partner violence in Sierra Leone and Liberia. Global Public Health, 11(1–2), 108–121. 10.1080/17441692.2015.1032320 [DOI] [PubMed] [Google Scholar]
- Hunter JE, & Schmidt FL (2004). Methods of meta-analysis: Correcting error and bias in research findings. Sage. [Google Scholar]
- Hurless N, & Cottone RR (2018). Considerations of conjoint couples therapy in cases of intimate partner violence. The Family Journal, 26(3), 324–329. 10.1177/1066480718795708 [DOI] [Google Scholar]
- Jewkes RK, Dunkle K, Nduna M, & Shai N (2010). Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: A cohort study. The Lancet, 376(9734), 41–48. 10.1016/S0140-6736(10)60548-X [DOI] [PubMed] [Google Scholar]
- Jones D, Weiss SM, Arheart K, Cook R, & Chitalu N (2014). Implementation of HIV prevention interventions in resource limited settings: The partner project. Journal of Community Health, 39(1), 151–158. 10.1007/s10900-013-9753-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karakurt G, Whiting K, van Esch C, Bolen SD, & Calabrese J (2016). Couple therapy for intimate partner violence: A systematic review and meta-analysis HHS public access. J Marital Fam Ther, 42(4), 567–583. 10.1111/jmft.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keynejad RC, Hanlon C, & Howard LM (2020). Psychological interventions for common mental disorders in women experiencing intimate partner violence in low-income and middle-income countries: A systematic review and meta-analysis. Lancet Psychiatry, 7(2), 173–190. 10.1016/S2215-0366(19)30510-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimber M, Adham S, Gill S, McTavish J, & MacMillan HL (2018). The association between child exposure to intimate partner violence (IPV) and perpetration of IPV in adulthood-A systematic review. Child Abuse & Neglect, 76, 273–286. 10.1016/J.CHIABU.2017.11.007 [DOI] [PubMed] [Google Scholar]
- Kouyoumdjian FG, Calzavara LM, Bondy SJ, O’Campo P, Serwadda D, Nalugoda F, Kagaayi J, Kigozi G, Wawer M, & Gray R (2013). Risk factors for intimate partner violence in women in the Rakai Community Cohort Study, Uganda, from 2000 to 2009. BMC Public Health, 13(1), 566. 10.1186/1471-2458-13-566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krauss HH (2006). A protoscientific master metaphor for framing violence. Annals of the New York Academy of Sciences, 1087(1), 22–34. 10.1196/annals.1385.021 [DOI] [PubMed] [Google Scholar]
- Krug EG, Mercy JA, Dahlberg LL, & Zwi AB (2002). The world report on violence and health. The Lancet, 360(9339), 1083–1088. 10.1016/S0140-6736(02)11133-0 [DOI] [PubMed] [Google Scholar]
- Li S, Zhao F, & Yu G (2019). Childhood maltreatment and intimate partner violence victimization: A meta-analysis. Child Abuse & Neglect, 88, 212–224. 10.1016/J.CHIABU.2018.11.012 [DOI] [PubMed] [Google Scholar]
- McCollum EE, & Stith SM (2008). Couples treatment for interpersonal violence: A review of outcome research literature and current clinical practices. Violence and Victims, 23(2), 187–201. 10.1891/0886-6708.23.2.187 [DOI] [PubMed] [Google Scholar]
- Miller E, & McCaw B (2019). Intimate partner violence. New England Journal of Medicine, 380(9), 850–857. 10.1056/NEJMra1807166 [DOI] [PubMed] [Google Scholar]
- Mootz JJ, Stabb SD, Carlson C, Helpman L, Mangen PO, & Wainberg ML (2020). Why place and space matter for intimate partner violence survivors’ mental wellbeing and communities in Northeastern Uganda. Women & Health, 60(9), 975–986. 10.1080/03630242.2020.1784366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muluneh MD, Francis L, Agho K, & Stulz V (2021). A systematic review and meta-analysis of associated factors of gender-based violence against women in sub-Saharan Africa. International Journal of Environmental Research and Public Health, 18(9), 4407. 10.3390/ijerph18094407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal R (1979). The file drawer problem and tolerance for null results. Psychological Bulletin, 86(3), 638–641. 10.1037/0033-2909.86.3.638 [DOI] [Google Scholar]
- Schiff M, Plotnikova M, Dingle K, Williams GM, Najman J, & Clavarino A (2014). Does adolescent’s exposure to parental intimate partner conflict and violence predict psychological distress and substance use in young adulthood? A longitudinal study. Child Abuse & Neglect, 38(12), 1945–1954. 10.1016/j.chiabu.2014.07.001 [DOI] [PubMed] [Google Scholar]
- Schoch M, & Lakner C (2020). African countries show mixed progress towards poverty reduction and half of them have an extreme poverty rate above 35%. World Bank Blogs. https://blogs.worldbank.org/opendata/african-countries-show-mixed-progress-towards-poverty-reduction-and-half-them-have-extreme [Google Scholar]
- Selassie AA, & Hakobyan S (2021). Six charts show the challenges faced by sub-Saharan Africa. IMF Country Focus. https://www.imf.org/en/News/Articles/2021/04/12/na041521-six-charts-show-the-challenges-faced-by-sub-saharan-africa [Google Scholar]
- Sellers CS, Cochran JK, & Branch KA (2005). Social learning theory and partner violence: A research note. Deviant Behavior, 26(4), 379–395. 10.1080/016396290931669 [DOI] [Google Scholar]
- Shamu S, Abrahams N, Temmerman M, Musekiwa A, & Zarowsky C (2011). A systematic review of African studies on intimate partner violence against pregnant women: Prevalence and risk factors. PLoS One, 6(3), e17591. 10.1371/journal.pone.0017591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer CM, & Stith SM (2020). Risk factors for male perpetration and female victimization of intimate partner homicide: A meta-analysis. Trauma Violence Abuse, 21(3), 527–540. 10.1177/1524838018781101 [DOI] [PubMed] [Google Scholar]
- Spencer CM, Stith SM, & Cafferky B (2019). Risk markers for physical intimate partner violence victimization: A meta-analysis. Aggression and Violent Behavior, 44, 8–17. 10.1016/j.avb.2018.10.009 [DOI] [Google Scholar]
- Stith SM, & McCollum EE (2011). Conjoint treatment of couples who have experienced intimate partner violence. Aggression and Violent Behavior, 16(4), 312–318. 10.1016/j.avb.2011.04.012 [DOI] [Google Scholar]
- Stith SM, McCollum EE, Amanor-Boadu Y, & Smith D (2012). Systemic perspectives on intimate partner violence treatment. Journal of Marital and Family Therapy, 38(1), 220–240. 10.1111/j.1752-0606.2011.00245.x [DOI] [PubMed] [Google Scholar]
- Tajima EA (2021). First, do no harm: From diversity and inclusion to equity and anti-racism in interpersonal violence research and scholarship. Journal of Interpersonal Violence, 36(11–12), 4953–4987. 10.1177/08862605211012999 [DOI] [PubMed] [Google Scholar]
- Tran TD, Nguyen H, & Fisher J (2016). Attitudes towards intimate partner violence against women among women and men in 39 low- and middle-income countries. PLoS One, 11(11), e0167438. 10.1371/JOURNAL.PONE.0167438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevillion K, Oram S, Feder G, & Howard LM (2012). Experiences of domestic violence and mental disorders: A systematic review and meta-analysis. PLoS One, 7(12), e51740. 10.1371/journal.pone.0051740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevillion K, Williamson E, Thandi G, Borschmann R, Oram S, & Howard LM (2015). A systematic review of mental disorders and perpetration of domestic violence among military populations. Soc Psychiatry Psychiatr Epidemiol, 50(9), 1329–1346. 10.1007/s00127-015-1084-4 [DOI] [PubMed] [Google Scholar]
- United Nations Development Programme. (2020). Tackling social norms: A game changer for gender inequalities. United Nations Development Programme. [Google Scholar]
- United Nations. (2020). UNSD – Geographic Regions. United Nations Statistics Division. https://unstats.un.org/unsd/methodology/m49/#geo-regions [Google Scholar]
- United Nations Development Programme. (2016). Gender Inequality Index (GII). http://hdr.undp.org/en/content/gender-inequality-index-gii
- World Health Organization. (2016). Violence against women. http://www.who.int/mediacentre/factsheets/fs239/en/
- World Health Organization. (2017). Violence Info – Intimate partner violence. https://apps.who.int/violence-info/intimate-partner-violence/
- Yllö KA (2006). Through a feminist lens: Gender, diversity, and violence: Extending the feminist framework. In Loseke DR Gelles RJ, & Cavanaugh MM (Eds.), Current Controversies on Family Violence (pp. 19–34). SAGE Publications, Inc. 10.4135/9781483328584.n2 [DOI] [Google Scholar]
- Zembe YZ, Townsend L, Thorson A, Silberschmidt M, & Ekstrom AM (2015). Intimate partner violence, relationship power inequity and the role of sexual and social risk factors in the production of violence among young women who have multiple sexual partners in a peri-urban setting in South Africa. PLoS One, 10(11), e0139430. 10.1371/journal.pone.0139430 [DOI] [PMC free article] [PubMed] [Google Scholar]


