ABSTRACT
Context:
Cervical disc arthroplasty (CDA) was developed for the treatment of cervical disc disease with the potential advantages of preservation of physiological motion at a discal level, thereby potentially reducing adjacent level stresses and degeneration, which were a known complication of anterior cervical arthrodesis. The objective of this study was the assessment of long-term functional and radiological outcomes overtime in all the patients who underwent CDA from 2011 to 2019 at our institute.
Materials and Methods:
Forty-eight patients who underwent CDA (2011–2019) with a minimum 2-year follow-up were retrospectively evaluated. The functional outcome included the Visual Analog Score (VAS) and Neck Disability Index (NDI). Radiographs were assessed for range of motion (ROM) at the index surgical level, presence of heterotopic ossification (HO), and adjacent segment degeneration.
Results:
The mean follow-up was 5.79 ± 2.96 (2.16–11.75) years. Significant improvement (P < 0.05) was observed in the VAS (8.91 ± 2.52 [preoperative] to 0.89 ± 1.27 [follow-up]) and NDI (65.5% ±23.06% [preoperative] to 4.79 ± 3.87 [follow-up]) score. Motion at index level increased significantly from 5.53° preoperatively to 7.47°, and 92% of the implanted segments were still mobile (referring to the threshold of ROM > 3°). HOs are responsible for the fusion of 4/50 (8%) levels at the last follow-up. Distal and proximal adjacent disc degeneration occurred in 36% and 28% of patients, respectively. No migration of the implant was observed on the radiograph.
Conclusion:
Our study showed favorable clinical outcome of CDA with preservation of ROM at the index surgical level. CDA can be a promising alternative to anterior cervical arthrodesis when properly indicated.
Keywords: Cervical disc replacement, cervical spine, disc arthroplasty, disc degeneration, functional outcomes, heterotopic ossification
INTRODUCTION
Degenerative cervical disc disorders leading to cervical myelopathy and radiculopathy can present with typical symptoms of radicular pain, numbness, and weakness of the shoulders and arms, with some patients may present with weakness of the legs and torso and imbalance while walking.[1] After the failure of conservative treatment in patients with cervical degenerative disc disease, anterior cervical discectomy and fusion (ACDF) has been the traditional standard surgical procedure.[2,3] ACDF relieves symptoms significantly, but the elimination of motion at the index level accelerated adjacent level degeneration and pseudoarthrosis at the surgical site remains procedure-specific complication.[4,5] Long-term follow-up has showed up to 38% of patients re-present with significant adjacent segment disease (ASD) within 10 years of the primary ACDF procedure.[6]
Cervical disc arthroplasty (CDA) was developed as a potential alternative treatment for degenerative cervical disc pathology with the advantage of motion preservation at the index level and reducing the incidence of adjacent level degeneration both in vitro and in clinical settings.[7,8] In addition, CDA avoids complications associated with fusion surgeries, including the requirement of bone graft, graft site morbidities, and pain and risk of pseudarthrosis after surgery.[5,9] However, implant migration, subsidence, and incidence of heterotopic ossification are reported disadvantages in the literature relating to CDA.[10,11,12] Literature has established that CDA provides pain relief with improvement in functional scores superior to ACDF and a lower rate of symptomatic adjacent segment degeneration in short-term to midterm follow-up.
To the best of our knowledge, there is no literature regarding the long-term follow-up of CDA both clinically and radiologically in the Indian population. The goal of this study is to study and is to assess the long-term outcome (minimum 2-year follow-up) of both functional and radiological of CDA for cervical discopathy.
MATERIALS AND METHODS
A retrospective review of patients who underwent CDA in our institute from January 2011 to December 2019 was carried out with approval of the local Ethical Committee of Stavya Spine Hospital and Research Institute and was registered in Clinical Trials Registry – India (CTRI/2022/09/04500).
Inclusion and exclusion criteria
The inclusion criteria were: (1) symptomatic cervical discopathy at 1 or 2 vertebral levels between C3 and C7 confirmed by imaging (magnetic resonance imaging, computed tomography, or myelogram) showing herniated nucleus pulposus and spondylosis; (2) age between 20 and 60 years; and (3) failure of at least 6 weeks of conservative therapy. The exclusion criteria were: (1) cervical fusion adjacent to the level to be operated; (2) cervical instability (translation >3 mm and/or >11 rotational difference to that or either adjacent level); (3) facet joint degeneration; (4) presence of ossification of posterior longitudinal ligament (PLL); (5) revision surgery; (6) severe spondylosis (bridging osteophytes and disc height loss >50%); (7) active local/systemic infection; and (8) autoimmune spondyloarthropathies (i.e., rheumatoid arthritis).
In accordance with the above inclusion criteria, 48 patients underwent CDA from January 2011 to December 2019 at the author’s institute.
Surgical technique
CDA is performed under general anesthesia. The patient is placed on the operating table in the supine position with the neck in the neutral position. Endotracheal intubation should be done with care to avoid manipulation of the neck, especially in cases of severe cord compression. Fiber-optic intubation can be used in these cases. The endotracheal tube should be tapped to the opposite side of the surgical approach.
The head is secured on the head ring with tapping across the chin in the neutral position, and the shoulders are secured down with tape to allow for proper visualization with fluoroscopy. The end plates of the index surgical level on lateral fluoroscopy to should be in a parallel position.
A standard anterior Smith–Robinson approach is used at the level of surgery. The skin is incised, and the platysma is divided in line of skin incisions using electrocautery Bovie. The superficial layer of the cervical fascia is opened and using blunt dissection; the avascular plane is developed between the sternocleidomastoid and carotid bundle laterally and strap muscle of neck and trachea–esophagus medial. The omohyoid muscle is sectioned for better retraction and exposure. Finger dissection and swabs on sticks are used to reach up to the prevertebral fascia. Finger palpation is used to confirm the disc space (hills of the discs and valleys of the anterior vertebrae bone), and radiographs should be taken to ensure the correct level.
The longus colli muscle over the vertebra is erased from midline to 1.5 cm lateral at the surgical level. Self-retaining retractor (TrimLine, Medtronic, USA) is placed below the longus colli muscle. Distraction pins are placed in the midline in anteroposterior (AP) radiograph at above and below the vertebral of surgical level and distracted. The annulus is incised with a sharp knife and discectomy is performed using curettes. The uncovertebral joints should be identified bilaterally. Once reached to PLL, the posterior disc spaced is opened with the help of lamina spreader, and PLL is resected till the ventral dura is visible. Uncinate osteophytes removal and foraminal decompression are done. The adequacy of decompression is checked with the help of tactile feedback with a nerve hook.
The traction on the distractor pin is released. Centering of prosthesis in the midline and adequate sizing are crucial steps of successful CDA. The end plates are prepared with the help of curette and rasps. The use of burr should be avoided to increase the incidence of heterotopic ossification (HO). Care should be taken to avoid violation of the end plates. Trials are used to determine proper implant size in all dimensions (height, width, and depth) and ensure proper alignment with the guidance of fluoroscopic imaging. Rail is prepared with the help of a rail guide and cutter. The prosthesis (PRESTIGE® LP, Medtronic, USA) is tamped into the proper position under fluoroscopic imaging. Hemostasis is achieved, copious irrigation is done, and wound is closed in a layer over a negative suction drain.
Outcomes assessment
All patients were followed up in the outpatient clinic to assess the patient-reported outcome measures and radiological parameters at 6 weeks, 6 months, 12 months, and subsequently at yearly follow-up after 12 months.
Functional assessment was evaluated on basis of the Visual Analog Scale (VAS) of neck and arm pain, and the Neck Disability Index (NDI) score in preoperative phase and at the final follow-up.
Radiological evaluation on dynamic (flexion/extension) and neutral lateral X-rays and AP radiographs, preoperatively and at final follow-up was done. Range of motion (ROM) has been measured at the index level (≥3° in flexion–extension radiograph was considered mobile). The extent of heterotopic ossifications (HO) was graded according to Mehran–McAfee classification,[13] which was Grade 0: absence of HO; Grade 1: presence of HO in front of vertebral body but not in the anatomic disc space; Grade 2: presence of HO in the disc space, possibly affecting the prosthesis’s function; Grade 3: bridging HO with prosthesis’s motion still preserved; and Grade 4: complete fusion of the segment with absence of motion in flexion/extension.
Evaluation of the occurrence of degeneration of initially healthy adjacent disc and evolution of altered disc in preoperative period was noted. Adjacent segment degeneration was evaluated according to Kellgren–Lawrence grading system[14] (Grades 0–4) in which Grade 0, 1: no or minimal anterior osteophytosis. Grade 2: definite anterior osteophytosis with possible narrowing of disc space and some sclerosis of vertebral plates; Grades 3: multiple osteophytes, definite narrowing of joint space, and some sclerosis and deformity of bone ends; and Grade 4: large osteophytes marked narrowing of joint space, severe sclerosis, and definite deformity of bone ends. Change of ≥1 grade in the initially healthy disc and ≥2 in the previously alternated disc was considered significant.
Complication in intraoperative and postoperative period and return to routine activity and patient satisfaction was noted in follow-up.
Statistical analysis
Data analysis was performed using SPSS statistical software version 25 (IBM Corp, Chicago, IL, USA). VAS score, NDI scores, and ROM were analyzed, and results were expressed as mean with standard deviations. Paired t-test was employed to compare preoperative and postoperative continuous variable data. McNemar’s test was used for the comparison of categorical data, and categorical variables are presented as proportions. The statistical significance level was set at P < 0.05.
RESULTS
Forty-eight patients underwent cervical disc CDA from January 2011 to December 2019. The mean age of the enrolled patients is 38.6 ± 6.69 (24–54) years. Thirty-eight (79.1%) patients were male and 10 (20.9%) were female. The most common diagnoses for which patients underwent CDA in our study were cervical disc herniation with radiculopathy (n = 36) followed by cervical spondylotic myelopathy without instability (n = 12). Forty-six patients underwent single-level procedure; two patients underwent double-level surgery. Total 50 prosthesis are implanted with distribution as follows; C5–C6 (n = 33), C5–C6 (n = 9), C6–C7 (n = 4), C4–C5/C5–C6 (n = 1), and C5–C6/C6–C7 (n = 1). The mean operative duration was 74.52 ± 11.61 min (50–110 min). Postoperative period was uneventful in all the patients. Demographic data and surgical records are tabulated in Table 1.
Table 1.
Patients demographics and surgical data of the cohort
| Variable | Number |
|---|---|
| Number of patients | 48 |
| Male:female | 38:10 |
| Age (years) | 38.6±6.69 (24–54) |
| Presentation | |
| Radiculopathy | 36 |
| Myelopathy/myeloradiculopathy | 12 |
| Level of procedure | |
| Single | 46 |
| Double | 2 |
| Level | |
| C5–C6 | 33 |
| C5–C6 | 9 |
| C6–C7 | 4 |
| C4–C5/C5–C6 | 1 |
| C5–C6/C6–C7 | 1 |
| Operative duration (min) | 74.52±11.61 (50–110) |
| Average follow-up (years) | 5.79±2.96 (2.16–11.75) |
The mean follow-up period was 5.79 ± 2.96 (2.16–11.75) years, and the mean NDI score was reduced significantly at the final follow-up compared to preoperative condition. The preoperative NDI score was 65.5% ±23.06%, which improved to 4.79% ±3.87% at the time of the last follow-up (P = 0.0352). The absolute improvement (NDI postoperative – NDI preoperative) was an average of 30.3 pts. The mean VAS score in patients decreased statistically significantly from 8.91 ± 2.52 preoperatively to 0.89 ± 1.27 at the last follow-up (P = 0.0118). The improvement in average VAS and NDI scores was 90.01% and 92.68%, respectively [Table 2].
Table 2.
Functional outcome measure after cervical disc arthroplasty
| Preoperative | Final follow-up | P | |
|---|---|---|---|
| VAS | 8.91±2.52 | 0.89±1.27 | 0.0118 |
| NDI (%) | 65.5±23.06 | 4.79±3.87 | 0.0252 |
VAS - Visual analog scale; NDI - Neck Disability Index
The index surgical level in the preoperative period had a mean ROM of 5.53° ±1.69°, which increased to 7.47° ±2.36° in the last follow-up and 92% (46/50) of implanted prostheses had mobility (ROM >3°), and of these, 46 implanted prostheses 86.95% (40/46) had ROM >5° [Figures 1 and 2]. The incidence and severity of HO at the last recorded follow-up were as follows: Grade 1 in 12% (n = 6), Grade 2 in 16% (n = 8), Grade 3 in 6% (n = 3) of cases, and Grade 4 (with solid fusion of the index segment) in 8% (n = 4) of cases [Figure 3]. The overall incidence of HO was 42% and responsible for the fusion of 4/50 levels at the last follow-up [Table 3]. Radiologically distal and proximal adjacent disc degeneration occurred in 36% and 28% of patients, respectively. There was no migration/expulsion of prosthesis, and no reoperation required in postoperative follow-up.
Figure 1.
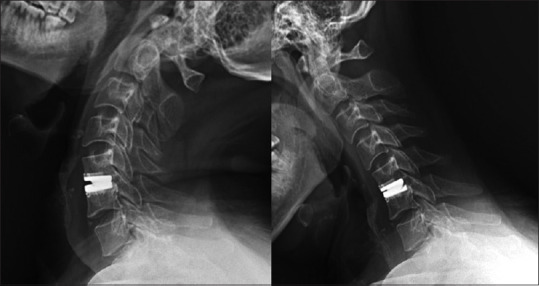
Lateral dynamic radiographs showing 7 years follow-up of C4–5 cervical disc arthroplasty with intact range of motion at index level
Figure 2.

Lateral dynamic radiographs showing 6 years follow-up of double level artificial cervical disc implantation at C5–6, C6–7 level showing intact range of motion in flexion-extension
Figure 3.

Presence of Grade 4 heterotropic ossification causing complete bridging fusion at index surgical level
Table 3.
Incidence and grading of HO as per Mehran–McAfee classification
| Grade of HO | Patient (%) |
|---|---|
| Grade 1 | 6 (12) |
| Grade 2 | 8 (8) |
| Grade 3 | 3 (6) |
| Grade 4 (solid fusion of the index segment) | 4 (8) |
HO - Heterotopic ossification
Return to routine activity, same as preoperative level, was seen in 93.75% (n = 45) of patients, and 89.58% (n = 43) of patients were able to return to the same job as earlier. 93.75% of the patients were satisfied with CDA procedure with 45/48 patients would consider to undergo CDA if needed in the future.
DISCUSSION
ACDF has been a time tested, treatment of choice in degenerative disc disorder (DDD) with excellent alleviation in clinical symptoms described in various literature.[9,15] Fusion of the intervertebral segment leads to increase intradiscal pressure in the adjacent segment, eventually accelerating the ongoing degenerative process secondarily to aging.[5]
In the last two decades, with significant evolution in the conservation of mobility at the index level and reemergence of disc replacement prosthesis due to development in tribology, CDA has gained popularity among surgeons as an alternative to fusion surgery for DDD.[16] The potential advantage of motion preservation and reducing the stress at the adjacent levels reduces the chances of ASD, thus increasing the longevity of the procedure before requiring any procedure for secondary. Degeneration has made CDA a practical and viable option for the treatment of DDD.[17,18]
In a meta-analysis by Findlay et al., CDA was found to have superior outcomes in improvement in NDI, 36-Item Short-Form Health Survey-36 physical component scores and satisfaction, index compared to ACDF at 5–7 years of follow-up.[19] Our study showed the comparable significant result in improvement of functional score in postoperative follow-up compared to preoperative period as reported in literature.
ROM at index surgical level was intact in 92% of prosthesis at average 5.79 years of follow-up and overall ROM improved by 1.87°, which was not statistically significant but intact and improved. This intact motion at the index level can dissipate the stress concentration at the adjacent level, thus slowing down the degenerative process. Our radiological ROM findings were concurrent with multiple investigational device exemption studies on given in the literature.[20,21]
It is still debatable whether the incidence of adjacent segment degeneration is related to natural degeneration or biomechanical stress as result of adjacent fusion.[22,23] Hilibrand et al. reported that after anterior cervical fusion surgery, the rate of ASD increases by 2.9%/year with yearly follow-up.[24] The literature has reported the success in reducing the ASD rate with CDA compared to ACDF in multiple meta-analysis and randomized control trials.[19,25,26] In an aforementioned meta-analysis by Findlay et al. showed a lower rate of ASD at 4–7 year follow-up in CDA compared to fusion surgery.[19] Adjacent segment degeneration and ASD are two different entities with the latter being the symptomatic manifestation which requires a medical or surgical management. A meta-analysis comparing randomized controlled trial by Dong et al. showed the rate of adjacent segment re-operation was reduced by 70% compared to ACDF (odds ratio = 0.30, 95% confidence interval [0.20, 0.44] [P < 0.001]) and advantage of the lower rate of adjacent segment reoperation in CDA compared with ACDF increased with the increasing length of follow-up.[17] Our study showed ASD in the proximal and distal segments being 36% and 28%, respectively, with no patient requiring the reoperation in follow-up tends to support the finding of a lower rate of symptomatic ASD with CDA.
Occurrence of HO after CDA is considered as a potential complication and a major obstacle in development in non-fusion surgical modality in the cervical spine. Even though literature has reported a high rate of HO post-CDA up to 35%, the causative factor and clinical impact of HO is yet to be fully understood.[13] Predisposing factors such as intervertebral height change and inadequate coverage at prosthesis are described as risk factors of HO development.[27] Shen et al. concluded the risk of HO significantly increased when the prosthesis coverage in the sagittal section is <93.8% or the change of intervertebral disc height after surgery was large than 1.80 mm.[28] Mcaffee Grades 3 and 4 are considered motion-restricting grades of HO and decrease ROM at the surgical level, but it does not alter the functional outcome or increase the disability.[29,30] Our study showed a cumulative 14% of the occurrence of Grades 3, 4 HO and 3 patients had a complete fusion of at the surgical site, but the patient did not complain of any functional disability at follow-up. Release of distraction by Casper pin at the discal level before sizing the prosthesis and choosing a size with maximal coverage in AP plane is critical factor for decreasing HO after CDA.[29]
We acknowledge the retrospective nature of this study and nonrandomization makes this study liable to potential selection bias. The lack of control group partially impacts the result, particularly in the assessment of ASD, which can be less relevant without a comparative group. In spite of these limitations, this study provides a long-term follow-up of CDA up to 11 years with good functional outcomes.
CONCLUSION
Our study assessed the functional and radiological outcome of CDA, which showed statistically significant improvement in functional outcomes and preservation of movement at index level. CDA continues to be a promising form of surgical treatment for degenerative cervical disc disease in patients with myelopathy and radiculopathy when properly indicated.
Informed consent statement
Patient consent was waived due to the retrospective nature of the study and the use of anonymized data.
Compliance with ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Stavya spine hospital’s ethics Committee and the national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The author thanks Stavya Research team for assistance with manuscript preparation.
REFERENCES
- 1.Amenta PS, Ghobrial GM, Krespan K, Nguyen P, Ali M, Harrop JS. Cervical spondylotic myelopathy in the young adult:A review of the literature and clinical diagnostic criteria in an uncommon demographic. Clin Neurol Neurosurg. 2014;120:68–72. doi: 10.1016/j.clineuro.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 2.Xie L, Liu M, Ding F, Li P, Ma D. Cervical disc arthroplasty (CDA) versus anterior cervical discectomy and fusion (ACDF) in symptomatic cervical degenerative disc diseases (CDDDs):An updated meta-analysis of prospective randomized controlled trials (RCTs) Springerplus. 2016;5:1188. doi: 10.1186/s40064-016-2851-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nanda A, Sharma M, Sonig A, Ambekar S, Bollam P. Surgical complications of anterior cervical diskectomy and fusion for cervical degenerative disk disease:A single surgeon's experience of 1,576 patients. World Neurosurg. 2014;82:1380–7. doi: 10.1016/j.wneu.2013.09.022. [DOI] [PubMed] [Google Scholar]
- 4.Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine (Phila Pa 1976) 1993;18:2167–73. doi: 10.1097/00007632-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002;27:2431–4. doi: 10.1097/00007632-200211150-00003. [DOI] [PubMed] [Google Scholar]
- 6.Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating:A 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976) 2005;30:2138–44. doi: 10.1097/01.brs.0000180479.63092.17. [DOI] [PubMed] [Google Scholar]
- 7.Hisey MS, Zigler JE, Jackson R, Nunley PD, Bae HW, Kim KD, et al. Prospective, randomized comparison of one-level mobi-C cervical total disc replacement versus anterior cervical discectomy and fusion:Results at 5-year follow-up. Int J Spine Surg. 2016;10:10. doi: 10.14444/3010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burkus JK, Haid RW, Traynelis VC, Mummaneni PV. Long-term clinical and radiographic outcomes of cervical disc replacement with the prestige disc:Results from a prospective randomized controlled clinical trial. J Neurosurg Spine. 2010;13:308–18. doi: 10.3171/2010.3.SPINE09513. [DOI] [PubMed] [Google Scholar]
- 9.Goldberg G, Albert TJ, Vaccaro AR, Hilibrand AS, Anderson DG, Wharton N. Short-term comparison of cervical fusion with static and dynamic plating using computerized motion analysis. Spine (Phila Pa 1976) 2007;32:E371–5. doi: 10.1097/BRS.0b013e318060cca9. [DOI] [PubMed] [Google Scholar]
- 10.Duggal N, Pickett GE, Mitsis DK, Keller JL. Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus. 2004;17:E9. doi: 10.3171/foc.2004.17.3.9. [DOI] [PubMed] [Google Scholar]
- 11.Chen J, Wang X, Bai W, Shen X, Yuan W. Prevalence of heterotopic ossification after cervical total disc arthroplasty:A meta-analysis. Eur Spine J. 2012;21:674–80. doi: 10.1007/s00586-011-2094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dufour T, Beaurain J, Huppert J, Dam-Hieu P, Bernard P, Steib JP. Clinical and radiological evaluation of cervical disc arthroplasty with 5-year follow-up:A prospective study of 384 patients. Eur Spine J. 2019;28:2371–9. doi: 10.1007/s00586-019-06069-z. [DOI] [PubMed] [Google Scholar]
- 13.Mehren C, Suchomel P, Grochulla F, Barsa P, Sourkova P, Hradil J, et al. Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976) 2006;31:2802–6. doi: 10.1097/01.brs.0000245852.70594.d5. [DOI] [PubMed] [Google Scholar]
- 14.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75:1298–307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Chin-See-Chong TC, Gadjradj PS, Boelen RJ, Harhangi BS. Current practice of cervical disc arthroplasty:A survey among 383 AOSpine international members. Neurosurg Focus. 2017;42:E8. doi: 10.3171/2016.11.FOCUS16338. [DOI] [PubMed] [Google Scholar]
- 17.Dong L, Xu Z, Chen X, Wang D, Li D, Liu T, et al. The change of adjacent segment after cervical disc arthroplasty compared with anterior cervical discectomy and fusion:A meta-analysis of randomized controlled trials. Spine J. 2017;17:1549–58. doi: 10.1016/j.spinee.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 18.Sasso WR, Smucker JD, Sasso MP, Sasso RC. Long-term clinical outcomes of cervical disc arthroplasty:A prospective, randomized, controlled trial. Spine (Phila Pa 1976) 2017;42:209–16. doi: 10.1097/BRS.0000000000001746. [DOI] [PubMed] [Google Scholar]
- 19.Findlay C, Ayis S, Demetriades AK. Total disc replacement versus anterior cervical discectomy and fusion:A systematic review with meta-analysis of data from a total of 3160 patients across 14 randomized controlled trials with both short- and medium- to long-term outcomes. Bone Joint J. 2018;100-B:991–1001. doi: 10.1302/0301-620X.100B8.BJJ-2018-0120.R1. [DOI] [PubMed] [Google Scholar]
- 20.Radcliff K, Coric D, Albert T. Five-year clinical results of cervical total disc replacement compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease:A prospective, randomized, controlled, multicenter investigational device exemption clinical trial. J Neurosurg Spine. 2016;25:213–24. doi: 10.3171/2015.12.SPINE15824. [DOI] [PubMed] [Google Scholar]
- 21.Vaccaro A, Beutler W, Peppelman W, Marzluff JM, Highsmith J, Mugglin A, et al. Clinical outcomes with selectively constrained SECURE-C cervical disc arthroplasty:Two-year results from a prospective, randomized, controlled, multicenter investigational device exemption study. Spine (Phila Pa 1976) 2013;38:2227–39. doi: 10.1097/BRS.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 22.Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y, et al. Anterior cervical decompression and fusion accelerates adjacent segment degeneration:Comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 2010;35:36–43. doi: 10.1097/BRS.0b013e3181b8a80d. [DOI] [PubMed] [Google Scholar]
- 23.Helgeson MD, Bevevino AJ, Hilibrand AS. Update on the evidence for adjacent segment degeneration and disease. Spine J. 2013;13:342–51. doi: 10.1016/j.spinee.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 24.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81:519–28. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Yang B, Li H, Zhang T, He X, Xu S. The incidence of adjacent segment degeneration after cervical disc arthroplasty (CDA):A meta analysis of randomized controlled trials. PLoS One. 2012;7:e35032. doi: 10.1371/journal.pone.0035032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verma K, Gandhi SD, Maltenfort M, Albert TJ, Hilibrand AS, Vaccaro AR, et al. Rate of adjacent segment disease in cervical disc arthroplasty versus single-level fusion:Meta-analysis of prospective studies. Spine (Phila Pa 1976) 2013;38:2253–7. doi: 10.1097/BRS.0000000000000052. [DOI] [PubMed] [Google Scholar]
- 27.Hui N, Phan K, Kerferd J, Lee M, Mobbs RJ. Cervical total disc replacement and heterotopic ossification:A review of literature outcomes and biomechanics. Asian Spine J. 2021;15:127–37. doi: 10.31616/asj.2019.0234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shen YW, Yang Y, Liu H, Rong X, Ding C, Meng Y, et al. Effects of endplate coverage and intervertebral height change on heterotopic ossification following cervical disc replacement. J Orthop Surg Res. 2021;16:693. doi: 10.1186/s13018-021-02840-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li G, Wang Q, Liu H, Yang Y. Postoperative heterotopic ossification after cervical disc replacement is likely a reflection of the degeneration process. World Neurosurg. 2019;125:e1063–8. doi: 10.1016/j.wneu.2019.01.244. [DOI] [PubMed] [Google Scholar]
- 30.Zhou HH, Qu Y, Dong RP, Kang MY, Zhao JW. Does heterotopic ossification affect the outcomes of cervical total disc replacement?A meta-analysis. Spine (Phila Pa 1976) 2015;40:E332–40. doi: 10.1097/BRS.0000000000000776. [DOI] [PubMed] [Google Scholar]


