Abstract
Lack of skilled human resources in primary care remains a major concern for policymakers in low- and middle-income countries. There is little evidence supporting the impact of residency training in family medicine in the quality of care, and it perpetuates misconceptions among policymakers that the provision of primary care can be easily done by any physician without special training. This article compares the risk of patients being hospitalized due to Ambulatory care sensitive conditions and the odds of having follow-up visits in primary care after hospital discharge, according to the type of their medical provider: (1) Generalists (reference), (2) Family physicians; and, (3) patients with no consultations prior to the event. Multilevel multivariate binomial regression models estimated the relative risks of a patient being hospitalized in a given month and the relative risks for the occurrence of a follow-up visit in primary care in a retrospective cohort of 636.640 patients between January 2013 and July 2018 in Rio de Janeiro. For all 14 conditions, there was a higher risk of hospitalization when patients had no consultation in primary care prior to the event. Except for Ear, Nose and Throat infections, patients seen by family physicians had a lower risk of being hospitalized, compared to patients seen by Generalists. Follow-up visits were more likely to happen among patients treated by family physicians for almost every condition analyzed. With two years of training in family medicine, Family physicians can reduce the risk of their patients being hospitalized and increase the likelihood of those patients having a follow-up consultation in primary care. Investments in residency training in family medicine should be made to fix the shortage of skilled physicians in primary care, reduce hospitalizations and improve quality and continuity of care.
Introduction
Hospital admissions have been used over the last 30 years as a valuable indicator of the effectiveness of Primary Health Care (PHC) [1]. Health conditions for which good quality, timely and effective primary care can prevent hospitalization are known as ambulatory-care sensitive conditions (ACSC). Good quality PHC services can change the course of these health conditions, making a hospital admission less likely to happen [2, 3]. High rates of hospitalizations due to ACSC would represent the provision of suboptimal PHC to the community.
This concept has been used worldwide to measure the impact of PHC initiatives, policies, and services [4–7], and in Brazil to show the impact of the Family Health Strategy [8] (FHS), a federal policy that organizes the public PHC system, providing the structure and financial resources for Family Health Teams (FHTs). The FHS today–with nearly 43 000 FHTs in place–is responsible for the provision of PHC for 64% of the Brazilian population [9, 10]. Over its 25 years of implementation, many achievements have been reported, such as the reduction of infant, neonatal [11–13], and cardiovascular deaths [14, 15], and for the reduction of hospital admissions due to ACSC [16], and among older adults [17, 18].
However, the lack of trained human resources in PHC remains a major concern for policymakers in low- and middle-income countries. Recent policies–the More Doctors and the Doctors for Brazil programs–have tried to promote provision and fixation of physicians in underserved areas [19, 20]. Nonetheless, the vast majority of doctors working at the FHS have no training in family medicine (FM) [21]. Despite the recent incentives to boost residency training in family medicine (RTFM) in the country, with less than 4% of the total number of vacancies for residency training dedicated to FM [22], this picture is far away from being changed. Unfortunately, there is little of evidence showing the impact of RTFM on the quality of care, and it perpetuates misconceptions among policymakers that the provision of primary care can be easily done by any physician without RTFM.
This study tests the hypothesis that RTFM can make doctors more capable of providing good quality primary care and prevent the occurrence of hospitalizations due to ACSC. The rationale behind this argument is that during two years of RTFM, physicians would develop the skills and competencies needed to better manage a wider set of conditions in primary care, thus preventing unnecessary hospital admissions. This article aims to (1) compare the risk of patients being hospitalized due to ACSC and (2) the odds of a patient having follow-up visits in primary care after hospital discharge, according to the type of training of their medical health care provider. Finally, it (3) estimates the population attributable fraction and the absolute change in hospital admissions per year in the sample that would happen if all medical consultations were performed by specialists in family medicine.
Methods
Ethics statement
Patients’ consent was not necessary since only anonymized information was used during the study and the Rio de Janeiro Municipal Health Department, the actual caretaker of this information, gave the consent to use this dataset for this research. The study was approved by the Rio de Janeiro Municipal Health Department research ethics board and it is registered under the number 03795118.0.0000.5279. It was conducted in accordance with the 466/12 resolution from the Brazilian National Health Council and the Declaration of Helsinki.
Study design and data source
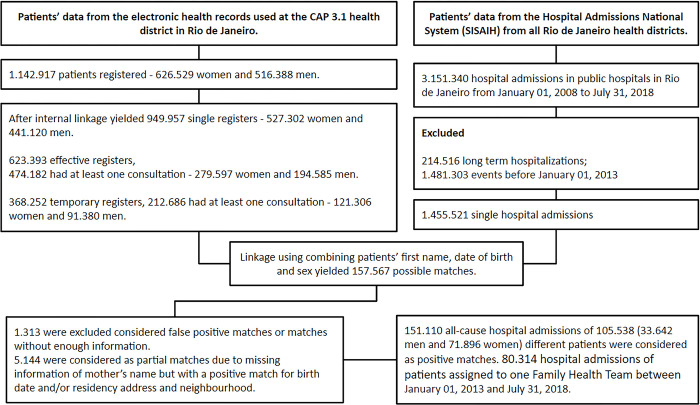
A retrospective longitudinal analysis of medical consultations in primary care and hospital admissions in the Rio de Janeiro municipality was performed using as data source patients’ information from electronic health records used in the municipal public primary care system and patients’ information from the National Hospital Admissions System. Deterministic linkage combining patient’s name, date of birth, mother’s name, gender and patient’s address was performed and false-positive matches between the datasets were excluded after manual review–Fig 1.
Fig 1. Flowchart describing data cleaning and data linkage process used in this study.
Setting
The Family Health Strategy (Estratégia de Saúde da Família–FHS) is the Brazilian federal policy for public PHC launched in 1994. It provides structural organization and financial support to the municipal Family Health Teams (FHTs) that are formed by one physician, one nurse, and four to six community health workers. They are responsible for providing comprehensive primary care for up to 4.000 patients in a given catchment area. In Rio de Janeiro, the number of FHTs expanded from 2008 to 2016, increasing coverage of the FHS from 3.5% to 70% of the population [23]. New community-based primary care clinics were created and strong investments to expand RTFM were made [24].
Exposure and independent variables
Physicians were categorized according to their type of formal training to work in PHC: (1) Generalists, i.e. doctors without RTFM, were considered as the reference category; and (2) Family physicians (FPs)–graduated FPs, FM preceptors and residents enrolled in the FM residency programs. Patients that were hospitalized but had no consultations in primary care prior to the event were categorized as (3) “No consultation prior”.
Residents and preceptors in FM share responsibilities for the same patients at the same FHT for two years of training and the decisions the residents make are usually supervised by their preceptor, hence they were both considered as FPs. Residents work 48 hours per week under the full supervision of FM preceptors in a community-based primary care clinic. They have learning sessions every week addressing topics of FM and PHC and clinical content about the most prevalent health conditions in primary care. All learning activities the residents must take during the course are designed in line with the National Committee for Medical Residencies and with the Brazilian Society of Family and Community Medicine (SBMFC) [25]. Information about other forms of post-graduate training or specialization was not available and were not taken into account, nor the number of years in practice for any doctor.
Patients’ data from electronic health records used to adjust the models were (1) age (continuous), (2) sex, and (3) the Charlson Comorbidity Index [26]. We considered each patient as “individual at risk for being hospitalized” only from the date of subscription at the clinic until the last day available at the dataset, or the day the patient was unsubscribed or the date of death. The Social Development Index (SDI) was used to bring information about the context where the patient lives. The SDI is a linear scale combining information about sanitation, schooling, income, and housing conditions from every household in the FHT catchment area, representing the grade of social development of a neighborhood. Hence, patients registered in the same FHT have the same SDI. It varies from 0 (least developed) to 1 (most developed).
All clinics and FHT in this sample have the same physical structure, offices equipped with computer, printer, medical equipment, room for small surgical procedures, the same arsenal of laboratory tests and medicines in the pharmacy, and the same type of human resources available: nurses, technicians, dentists, pharmacists, and managers. The distribution of doctors among different clinics and FHT didn’t follow any criteria that is known to interfere and generate confounding in the relationship between the medical categories, the population assisted, and the study outcomes.
Outcomes
Two outcomes were considered in this study: (1) The occurrence of hospital admissions, and (2) the occurrence of a follow-up visit in primary care in the following two, four, and six months after patient’s discharge from the hospital.
Fourteen health conditions from the Brazilian list of Ambulatory-care Sensitive Conditions (ICSAP-Brazil) were analyzed. ICD-10 codes and clinical criteria for each condition were used to identify both population-at-risk and the event, i.e. the hospital admissions–Table 1. Both hospital admissions and follow up visits were considered as binary events, i.e. being or not being hospitalized in a given month among those at risk and having or not having one medical consultation within 60 days, 120 days, or 180 days after being discharged from the hospital. For the follow-up visits, patients that were hospitalized and have not died during hospitalization were considered as the population-at-risk.
Table 1. List of health conditions according to their ICD10 codes and clinical criteria and respective population-at-risk used in the regression models.
| Domain/condition | ICD10 codes, clinical criteria or procedure | Population-at-risk |
|---|---|---|
| ICSAP-Brazil | ||
| Hypertension | I10, I11 | I10, I11, and at least one SBP > = 140 mmHg or DBP > = 90 mmHg |
| Diabetes mellitus | E10, E11, E12, E13, E14 | E10-E14, and at least one glycemia > 126 mg/dl or A1C hemoglobin > 6.5% |
| Stroke | I63, I64, I65, I66, I67, I69, G45, G46 | Patients with Diabetes, Hypertension, Ischemic heart disease, Stroke or Heart failure |
| Angina pectoris | I20 | Older than 40 years old |
| Heart failure | I50, J81 | Younger than 12 years old |
| Epilepsy | G40, G41, R56 | Older than 40 years old |
| Asthma | J45, J46 | Younger than 12 years old |
| Pregnancy related | O23, A50, P350 | Women during pregnancy or puerperium |
| Gastroenteritis | E86, A00, A01, A02, A03, A04, A05, A06, A07, A08, A09 | Younger than 12 years old |
| Pneumonias—children | J13, J14, J153, J154, J158, J159, J181 | Younger than 12 years old |
| Pneumonias—adults | J13, J14, J153, J154, J158, J159, J181 | Older than 40 years old |
| Skin infection | A46, L01, L02, L03, L04, L08 | Younger than 12 years old |
| Ear, nose & throat | H66, J00, J01, J02, J03, J06, J31 | Younger than 12 years old |
| Pelvic inflammatory disease | N70, N71, N72, N73, N75, N76 | Women (14–50 years old) |
By studying both phenomena here we aim to capture both sides of coordination of care between primary and secondary/tertiary care. If RTFM can make doctors more competent to work in primary care, it will make hospital admissions less likely to occur and, at the same time, for those patients that have been hospitalized, it will make a follow-up visit more likely to occur.
Statistical analyses
Multilevel multivariate binomial regression models estimated the relative risks (RR) of a patient being hospitalized in a given month and the RR for the occurrence of a follow-up visit, according to the type of doctor taking care of the patient, i.e. (1) Generalists (reference), (2) FPs, and, for those with no consultations prior to the event, (3) “No consultation prior”. Two and three levels hierarchical data structures were created clustering months within patients (two level) and months within patients within FHT (three levels). Multilevel regression models–also known as hierarchical linear models or mixed-effect models–can deal with data when observations within the same subject may be correlated and the outcomes are not independent within the same subject. Using multilevel analysis and this data structure allowed us to control for the variance in hospital admissions that happened in between each family health team and its population (third level) and to control for the variance in the risk of the same patient (second level) being hospitalized in subsequent months (first level). These models may give us a more precise measurement of the event of interest (residency training in FM) by controlling for factors that can affect the outcome but are not related to the type of training that the doctor in charge had. Since the results between the two and three level models were very similar, we decided to report only the results from the two level models in the article.
For follow-up visits in primary care, only patients that were hospitalized and did not die during hospitalization were considered as population-at-risk. Time effects were regarded using dummy variables for months and years. All models were adjusted for patient information (sex, age, and Charlson comorbidity index) and contextual information (SDI and time). For both acute and chronic conditions, patients were considered “at risk” during the whole period they were subscribed at the clinic. For Pregnancy related hospital-admissions, only pregnant women and women during the puerperium were considered as patients-at-risk.
Finally, Population Attributable Fraction (PAF) for each outcome was calculated using the RR from the regression models to estimate the absolute change in terms of number of hospital admissions per year in the sample that would happen if all medical consultations were performed by trained FPs. Data processing and statistical analysis were performed using R version 3.6.2 and lme4 package.
Results
From the original list of 636.640 patients (376.204 women and 261.432 men), 457.533 (184.505 men and 273.662 women) were subscribed in 195 FHTs and 30 different PHC clinics. From the patients assigned to one FHT, 406.271 patients were responsible for 2.433.924 medical consultations between January 2013 and December 2018, and for 80.314 hospital admissions between January 2013 and July 2018 that occurred among 59.106 different patients. The flowchart in Fig 1 describes data cleaning and data linkage process used in this study. Table 2 summarizes the number of doctors, number of medical consultations and patients’ characteristics according to each medical category in the study.
Table 2. Number of medical consultations and patients’ characteristics according to each medical category in the study sample.
Rio de Janeiro, Brazil, 2015–2018.
| Medical category | Number of doctors–N (%) | Consultations–N (%) | SDI -mean (SD) | Patients’ age (%) | Patients according to sex–N (%) | |||
|---|---|---|---|---|---|---|---|---|
| < 18 | > 18 & < 45 | > 45 | Women | men | ||||
| Generalists | 633 (75.6) | 1.629.235 (67.5) | 0.573 (0.03) | 21.3 | 31.8 | 46.9 | 1.067.212 (65.6) | 562.023 (34.4) |
| Family physicians | 204 (24.4) | 785.273 (32.5) | 0.585 (0.03) | 18.5 | 34.5 | 47.0 | 517.813 (65.9) | 267.460 (34.1) |
For all 14 domains studied and for both hierarchical models, there was a higher risk of hospitalization when patients had no consultation in primary care prior to the event. This effect was higher when the cause of hospitalization was due to Stroke, Gastroenteritis and Pelvic inflammatory disease, and had its smallest value in cases of Asthma and Epilepsy–Table 3.
Table 3. Relative risks for hospital admissions from January 2013 to July 2018 according to the proportion of consultations performed by Family physicians or Generalists in a Family Health Team in primary care.
Rio de Janeiro, Brazil. 2013–2018.
| Family physicians | No consultation prior | |
|---|---|---|
| Hypertension | 0.83 (0.61; 1.15) | 2.63 (2.04; 3.40) |
| Diabetes mellitus | 0.76 (0.56; 1.04) | 2.75 (2.11; 3.60) |
| Stroke | 0.74 (0.58; 0.95) | 5.47 (4.50; 6.65) |
| Angina pectoris | 0.62 (0.51; 0.75) | 2.58 (2.19; 3.03) |
| Heart failure | 0.52 (0.40; 0.67) | 2.78 (2.19; 3.53) |
| Epilepsy | 0.79 (0.57; 1.11) | 1.40 (1.07; 1.83) |
| Asthma | 0.35 (0.21; 0.57) | 1.46 (1.04; 2.05) |
| Pregnancy related | 0.78 (0.60; 1.01) | 2.89 (2.30; 3.63) |
| Gastroenteritis | 0.45 (0.25; 0.79) | 3.17 (2.19; 4.59) |
| Pneumonias—children | 0.57 (0.42; 0.77) | 2.19 (1.74; 2.76) |
| Pneumonias—adults | 0.36 (0.24; 0.56) | 2.90 (2.13; 3.95) |
| Skin infection | 0.82 (0.69; 0.97) | 2.61 (2.23; 3.00) |
| Ear, nose & throat | 1.06 (0.64; 1.77) | 1.78 (1.13; 2.83) |
| Pelvic inflammatory disease | 0.59 (0.38; 0.93) | 3.35 (2.34; 4.81) |
Multilevel multivariate binomial regression models adjusted for age, sex, time, and the Social development index of the area covered by the FHT.
Except for Ear, Nose and Throat infections, patients seen by FPs tended to have a lower risk of being hospitalized, compared to patients seen by Generalists. This effect was greater in hospital admissions due to Asthma, Pneumonias in adults, Gastroenteritis, Heart failure and Pneumonia in children–Table 3.
In absolute numbers, Heart failure, Angina pectoris, Pneumonias in adults would express the biggest decrease in the total number of hospital admissions, with 68, 61 and 59 fewer hospitalizations every year, if all doctors working in FHTs were trained in FM residency programs. In this scenario, there could be a 47% reduction in hospital admissions for Asthma, a 50% reduction in Pneumonia in adults and a 31% reduction in Pelvic inflammatory diseases–Table 4.
Table 4. Population attributable fraction and the absolute change in the number of hospital admissions in 12 months in a scenario where all Family Health Teams in the sample would have trained Family physicians as medical professionals.
Rio de Janeiro, Brazil, 2013–2018.
| Conditions | Population at risk | HA* per year | Population attributable fraction PAF (%) | Number of HA added or taken |
|---|---|---|---|---|
| Hypertension | 91958 | 128 | -3.5 (-25.1; 20.9) | -4 (-32; +27) |
| Diabetes mellitus | 38784 | 160 | -12.2 (-31.2; 9.7) | -17 (-43; +13) |
| Stroke | 4807 | 244 | -13 (-28.6; 4.7) | -32 (-70; +11) |
| Angina pectoris | 4277 | 271 | -22.6 (-10; -33.9) | -61 (-92; -27) |
| Heart failure | 2617 | 230 | -29.4 (-13; -43.4) | -68 (-100; -30) |
| Epilepsy | 449 | 86 | -15.3 (-33.9; 7.2) | -13 (-29; 6) |
| Asthma | 5514 | 54 | -47.4 (-67.1; 20.9) | -26 (-36; 11) |
| Pregnancy related | 45445 | 136 | -16.1 (-32.1; 1.4) | -22 (-44; 2) |
| Gastroenteritis | 5858 | 45 | -41.5 (-66; -7) | -19 (-30; -3) |
| Pneumonias—children | 2319 | 114 | -28.6 (-45.4; -9.2) | -33 (-52; -10) |
| Pneumonias—adults | 2777 | 116 | -50.5 (-67.1; -27.7) | -59 (-78; -32) |
| Skin infection | 33126 | 331 | -5.6 (-18.5; 7.2) | -19 (-61; 24) |
| Ear, nose & throat | 78059 | 28 | 0 (-39.9; 33.0) | 0 (-11; 9) |
| Pelvic inflammatory disease | 4044 | 41 | -31.2 (-52.6; -2.8) | -13 (-22; -1) |
* Hospital admissions
Population attributable fraction estimated using relative risks from two level multilevel multivariate binomial regression models, using a initial proportion of 30% of family physicians.
For follow-up visits (Table 5), patients that had no prior visit at the clinic before hospitalization were less likely than those seen by Generalists to have a follow-up consultation in primary care after hospital discharge. This effect is almost the same for consultations within two, four and six months. Oppositely, follow-up visits were more likely to happen among patients treated in FHTs with FPs for almost all conditions analyzed. Patients treated by FPs that were hospitalized for Heart failure and Angina pectoris had consistent higher odds of having follow-up consultations. The exceptions were hospital admissions due to Pregnancy-related and Gastroenteritis, where the odds of a follow-up consultation happening were the same for patients seen by Generalists and FPs.
Table 5. Relative risks for a patient having a follow-up consultation in primary care after one, three, and six months after hospital discharge according to the proportion of medical consultations performed by Family physicians or Generalists in a Family Health Team in the previous twelve months.
Rio de Janeiro, Brazil.
| 2 months | 4 months | 6 months | |
|---|---|---|---|
| Family physicians | |||
| Hypertension | 1.19 (0.55–2.55) | 1.11 (0.49–2.48) | 1.22 (0.5–2.93) |
| Diabetes mellitus | 1.30 (0.66–2.54) | 1.26 (0.58–2.72) | 1.54 (0.69–3.45) |
| Stroke | 1.43 (0.84–2.43) | 2.2 (1.21–3.99) | 1.8 (0.97–3.32) |
| Angina pectoris | 2.1 (1.33–3.31) | 1.78 (1.11–2.87) | 1.94 (1.15–3.28) |
| Heart failure | 3.09 (1.63; 5.88) | 3.50 (1.80; 6.82) | 3.33 (1.67; 6.62) |
| Epilepsy | 1.81 (0.74; 4.41) | 2.05 (0.83; 5.09) | 1.69 (0.68; 4.21) |
| Asthma | 1.07 (0.30; 3.81) | 1.30 (0.41; 4.10) | 0.95 (0.29; 3.12) |
| Pregnancy related | 1.17 (0.66; 2.07) | 0.90 (0.48; 1.70) | 0.87 (0.44; 1.72) |
| Gastroenteritis | 1.08 (0.24; 4.93) | 1.56 (0.37; 6.50) | 0.96 (0.23; 4.10) |
| Pneumonias—children | 1.84 (0.95; 3.56) | 2.92 (1.40; 6.07) | 3.18 (1.49; 6.78) |
| Pneumonias—adults | 3.93 (1.32; 11.68) | 2.60 (0.84; 8.01) | 2.08 (0.66; 6.57) |
| Skin infection | 1.62 (1.12; 2.36) | 1.39 (0.95; 2.02) | 1.30 (0.88; 1.93) |
| Ear, nose & throat | 1.72 (0.42; 7.02) | 2.24 (0.55; 9.15) | 1.28 (0.34; 4.79) |
| Pelvic inflammatory disease | 1.12 (0.36–3.51) | 2.10 (0.70–6.27) | 1.17 (0.38–3.57) |
| No consultation prior | |||
| Hypertension | 0.09 (0.04–0.22) | 0.09 (0.04–0.19) | 0.13 (0.06–0.29) |
| Diabetes mellitus | 0.27 (0.14–0.52) | 0.21 (0.11–0.43) | 0.22 (0.11–0.43) |
| Stroke | 0.23 (0.15–0.34) | 0.30 (0.20–0.44) | 0.27 (0.18–0.40) |
| Angina pectoris | 0.23 (0.16–0.34) | 0.17 (0.12–0.25) | 0.17 (0.12–0.24) |
| Heart failure | 0.18 (0.10; 0.33) | 0.28 (0.16; 0.47) | 0.27 (0.16; 0.46) |
| Epilepsy | 0.15 (0.06; 0.36) | 0.12 (0.05; 0.28) | 0.12 (0.05; 0.27) |
| Asthma | 0.21 (0.06; 0.71) | 0.26 (0.09; 0.75) | 0.20 (0.07; 0.57) |
| Pregnancy related | 0.39 (0.21; 0.75) | 0.32 (0.17; 0.60) | 0.39 (0.20; 0.78) |
| Gastroenteritis | 0.52 (0.17; 1.61) | 0.56 (0.21; 1.49) | 0.59 (0.23; 1.54) |
| Pneumonias—children | 0.51 (0.28; 0.92) | 0.44 (0.25; 0.79) | 0.54 (0.31; 0.95) |
| Pneumonias—adults | 0.45 (0.20; 1.04) | 0.17 (0.07; 0.39) | 0.22 (0.10; 0.48) |
| Skin infection | 0.50 (0.36; 0.70) | 0.45 (0.33; 0.62) | 0.39 (0.29; 0.53) |
| Ear, nose & throat | 0.14 (0.02; 0.80) | 0.39 (0.11; 1.42) | 0.33 (0.10; 1.08) |
| Pelvic inflammatory disease | 0.15 (0.05–0.49) | 0.11 (0.04–0.33) | 0.10 (0.04–0.27) |
All models were adjusted for age, sex, time, and the Social development index of the area covered by the FHT.
Discussion
By way of clarification, the comparisons made here between Generalists and FPs are not judgmental and we believe that all doctors in this sample were doing their best to help their patients. We aimed solely to test the hypothesis that the addition of two years of training in family medicine, on top of the current six years of medical school in Brazil, modifies the risk of patients being hospitalized.
First aim–impact of RTFM on the risk of hospital admissions due to ACSC
With two years of training in family medicine, Family physicians working in primary care can reduce the risk of their patients being hospitalized for all fourteen health conditions from the Brazilian list of Ambulatory-care Sensitive Conditions (ICSAP-Brazil), except for Ear, nose and throat infections. Moreover, patients subscribed to a FHT that had no consultations at the clinic were at a higher risk of been hospitalized for all conditions, compared to patients treated by Generalists or Family physicians. These findings add important information to the well-established notion that the increased coverage of FHS in Brazilian municipalities leads to lower hospital admissions [5, 16], lower mortality from heart and cerebrovascular diseases [14], and lower mortality from ameanable conditions [15]. These previous ecological studies, however, focused mainly on the number of FHTs available to the population, which translates to “the proportion of the population covered or not by a FHT in the municipality”. In other words, the higher the proportion of the population covered by the FHS in a municipality, the larger will be the impact on health outcomes. For the patients, being covered by a FHT–i.e., having one doctor, one nurse, one nurse-technician and community-health agents as a team of healthcare providers–makes the risk of a comprehensive list of events decrease, such as hospital admissions. What is new from our study is that the already known beneficial effect of being covered by a FHT increases if the doctor in charge is a Family physician. It also expands the evidence raised in previous studies showing that specialists in family medicine are more capable of detecting chronic health conditions, requesting fewer laboratory tests and fewer referrals to secondary care and providing more follow-up consultations to their patients in primary care [27, 28].
Exploring the specific causes–infectious diseases
Exploring the specific causes for hospital admissions, with the exception of Ear, nose & throat infections and–to a lesser extent–Skin infections, all infectious disesases had their risk decreased when a Family physician was present at the FHT. Pelvic inflammatory disease, Gastroenteritis, Pneumonia (children and adults) and Gastroenteritis were strongly affected by the presence of a FP at the FHT and in the case of Pneumonias in adults more than 50% of all cases could be avoided if all FHT in this samples had trained family physicians as their healthcare provider. In all these acute conditions, with the exception of Gastroenteritis, it is possible that the treatment will require the use of antibiotics, which is a matter of concern in a scenario where there is no shortage of these drugs and health professionals can freely prescribe them. The prescription of antibiotics in ambulatory care is the subject of campaigns aiming to protect patients from unnecessary treatments and procedures. Choosing wisely is one of them and the rational use of antibiotics is a key competence that residents in FM need to develop [29]. Future studies will need to explore the previous use of antibiotics for these patients-at-risk. Even if there is no difference in the risk of Hospital admission, like in Ear, nose & throat infections, if a lower prescription of antibiotics is found, it can represent a gain in terms of good practice.
Hospital admissions due to Gastroenteritis (diarrhea and dehydration) would also be influenced by RTFM, with a lower risk (RR 0.49–95%CI 0.26; 0.90) favoring patients treated by FPs. This lower risk is very unexpected, since this is an acute condition easily treated by a cheap and widely available intervention (oral rehydration salts). Moreover, Gastroenteritis is not a condition that challenges doctors to identify and treat, like heart failure, HIV, or dementia. Initiatives like the Integrated Management of Childhood Illness initiative–AIDIPI in Brazil–have been tackling this issue for many years by task shifting a simple procedure that, most of the time, does not require medical care. Nevertheless, biomedical content learned during RTFM cannot be entirely responsible for the lower risk of hospital admissions due to Gastroenteritis. Developing skills and attitudes that are beyond biomedical content represents a paradigm shift for medical education and a key element present in many competency-based curriculum in family medicine around the world [25, 30, 31].
One can speculate whether the development of relational, communication and time management skills could increase patients’ trust in their doctors and change the way parents seek medical care for their sick children. The lower risk of Hospital admissions due to Asthma and Epilepsy for Family physicians can maybe be the consequence of the combination of these skills–clinical skills and competencies of family physicians. If patients with Asthma or Epilepsy in the case of an acute event have access to a competent physician able to manage the acute situation, most of the time it will be solved in the primary care setting. Looking for an answer to this question would require studies designed to explore the interaction of these skills and competencies and their effect on healthcare. This is not a simple research question to be pursued but it could help to highlight the pathways in which RTFM makes this happen.
Exploring the specific causes–chronic conditions
Hypertension and Diabetes mellitus–Chronic cardiovascular conditions that play a major role as risk factors for cardiovascular outcomes–seemed to be less influenced by the presence of a FP in the FHT, when compared to Angina pectoris and Heart failure–outcomes that usually have Hypertension and Diabetes mellitus as their main causes. To a lesser degree, hospital admissions due to Stroke also seemed to be affected by the presence of FP in the FHT. There is a contradiction in these findings and it is reasonable to supose that treating Hypertension and Diabetes mellitus would decrease in a higher extent the risk for hospital admissions due to these conditions, and not so much the risk for their final consequences.
Lowering diabetic patients’ blood glucose reduces the risk of major cardiovascular events, especially for those patients with cardiovascular disease at baseline [32]. Reducing systolic blood pressure significantly reduces coronary heart disease, stroke, and heart failure, with the effect increasing in that order [33]. However, these measures would affect primarily Hypertension and Diabetes mellitus, and a larger effect in the reduction of hospital admissions should be expected. However, different population-at-risk were considered for each outcome. For Hypertension, all patients with blood pressure higher than 140/90 mmHg were included as patients-at-risk of being hospitalized–the same procedure was undertaken for every condition. Hence, the population-at-risk for Diabetes mellitus and Hypertension ended up including patients with different health statuses–from mild cases that require no more than lifestyle changes and one diuretic pill, to more severe cases with multimorbidity and polypharmacy involved, with an extensive list of medicines, insulin regimens, and a higher morbidity burden. On the other hand, all patients-at-risk for Angina pectoris, Stroke and Heart failure had been diagnosed (at the hospital or at the primary care clinic) for these conditions, making all of them high-risk patients. The differences in terms of their health status are smaller, hence the population-at-risk for these conditions are more homogenous than that for Hypertension and Diabetes mellitus.
Second aim–risk of patients having follow-up consultations in primary care after hospital discharge
Information on follow-ups also highlights an important aspect for the study of PHC and hospital admissions, which is continuity of care. Not only the risk of hospitalization was lower among patients treated by Family physicians but, for most conditions in our list, RTFM makes follow-up visits after hospital discharge more likely to happen. Since health care do not cease after hospital discharge, it seems that RTFM is also important in promoting continuity and coordination of care, making medical consultations more likely to happen after hospitalization. When compared to patients that had no consultation prior to the hospital admission (covered but not using the FHS), patients using their FHT as healthcare providers were more likely to have follow-up consultations. It is hard to tell what are the reasons for these patients to have fewer follow-up visits at the PHC clinic after hospital discharge. The same can be said about the reasons for these patients not to use their FHT before the hospital admission. Personal preferences for another healthcare service (private out-of-pocket or private health insurance), poor selfcare, and barriers to access the public primary care clinic are some possible reasons that should be explored in future studies.
Third aim–absolute reduction in hospital admissions
Reporting the Population attributable fraction (PAF) and the total number of hospital admissions avoided in a year can better translate the information reported as relative risks into meaningful information for policymakers and healthcare managers. Relative risks can show us only the relationship between the two categories of exposure. Its value represents the change in the odds of an outcome happening for patients in each of the two categories but do not show us the magnitude of this change in a given scenario when the proportion of the population exposed versus not exposed is affected. In our scenario, when we change the proportion of the population that have a FP as their medical health care provider. In that way, these two discrete variables–the total number of hospital admissions and the total number of FPs in charge of the FHTs in place–can be directly related. In other words, PAF helps us to see the change in the total number of hospital admissions that will happen by increasing the number of FPs taking care of a given population. In our context of interest, policymakers can than estimate the total number of hospital admissions that can be avoided in the future by training and/or hiring more trained FPs to each FHT.
In Table 4 the relative risks are expressed in terms of the absolute number of hospital admissions that would happen if all FHTs had a family medicine specialist as medical provider. In a scenario where 116 cases of pneumonia would be hospitalized every year, 59 (CI95% 32; 78) of the actual 116, would be avoided if all doctors working at the FHTs were trained family physicians. For Angina pectoris and Heart failure–conditions with 271 and 230 hospital admissions per year, respectively–would experience a large absolute reduction of events (61 and 68, respectively).
Some conditions would experience a big relative change with a small absolute reduction in the number of hospital admissions, due to the actual lower number of cases happening in this scenario. This is the case for Asthma and Pelvic inflammatory disease. Even with 47% and 31% fewer hospital admissions every year, the total number of events avoided would be only 26 and 13, respectively. However, every avoided hospitalization due to ambulatory care sensitive conditions represents healthcare resources that are saved to better use with patients in need.
Finally, health care conditions will be differently affected by RTFM (relative risks) but will also result in different number of events, with different costs and different time number of days in the hospital. This dimension of the impact that RTFM can make in patient care was not measured in our study but would be an interesting focus for future research exploring duration of stay, quality of life and outcomes related to the very hospital admission.
Methodological considerations and implications for future research
Exploring in detail the ways that Family physicians interact with their patients to change the life course of these conditions was not the aim of this study. Future research describing more precisely these populations-at-risk would be extremely valuable to explore the actions taken by family physicians and their patients during their health care trajectory that are responsible for lowering the risk for hospital admissions. Furthermore, each health condition in each patient might have a different time lapse to change under the effect of having a Family physician as his/her medical professional. Prenatal care issues and other acute conditions are more likely to be affected in a short term. A urinary tract infection in a pregnant woman develops over the period of one month (from the first symptoms to its resolution). On the contrary, chronic conditions resulting from years of exposure to risk factors will lead patients to a series of appointments, blood tests, follow-ups, changes in drug treatments.
In the case of Pregnancy related conditions, the lower risk of a women being hospitalized when a Family physician is responsible for her prenatal care is not followed by a change in the risk of having follow-up visits after hospital discharge. This information shows us that, in this sample, there were doctors available in the FHT to see these women after hospital discharge. Probably there was a doctor in that FHT before a hospital admission has occurred as well.
Hospital admissions avoided and follow-up visits after hospital discharge are only the tip of the iceberg. FPs can prevent these hospital admissions on top of changing a series of events that happen every day, such as the detection of health conditions, follow up consultations, procedures, prescriptions, and referrals to secondary care.
The ICSAP-Brazil creates a comprehensive list of conditions to explore and measure the effectiveness of PHC services, but it keeps out of its framework conditions that are widely prevalent in the community, such as Mental health conditions, HIV/AIDS, and Cancer. Those are some examples of prevalent conditions that might have the risk of hospitalization affected by strong PHC services and, moreover, by skilled Family physicians. Expanding the scope of health care conditions would be necessary to further explore in which extent RTFM affects the occurrence of hospital admissions.
Implications for healthcare
The World Health Organization in 2020 published the Operational Framework for Primary Health Care [34], describing the health care workforce as one of the 14 strategic levers to enable the development of PHC. Since the inauguration of the FHS in 1994 [8], some of the 14 levers were prioritized: an organized model of care was established for the whole country, strengthening governance and social participation, and creating policy frameworks organizing the way PHC should be funded, delivered and how resources should be allocated.
As mentioned before, the More Doctors and the Doctors for Brazil programs are good examples of policies that have tried to move the Healthcare workforce lever up, promoting provision and fixation of physicians in underserved areas. This is especially important when we look at the relative risks for Hospital admissions between patients with no consultation prior compared to those seen a Generalist. In a city with one of the highest density of doctors in the country [22], having a Family physician as a medical healthcare provider is beneficial to decrease the number of Hospital admissions but having consultations with a physician and using the FHT is crucial. For the rest of the country and especially in remotes areas, it is essential that the federal government fixes this inequality by providing physicians for places that can hardly get any.
Nevertheless, one more step must be taken by the federal government to leverage this lever, which is to fix the unequal distribution of vacancies for residency training in the country by increasing the number of seats for family medicine and redistributing these seats across the country. The political structure for these programs is already in place and the financial resources are available. In other words, the country already has the foundation to build a national program for provision, fixation and training of physicians in primary care aligned with the established family medicine residency programs.
Only with investments in RTFM it will be possible to fix the shortage of skilled physicians we see today in Brazilian PHC [21, 22]. To make it happen, we need to correct common misconceptions among policymakers that doctors do not need residency training to work in primary care.
Strengths and limitations
The main limitation of our study is the lack of information regarding the usage of emergency care services in the city to fully cover all paths between primary care and hospital care. These services play an important role in managing every domain at the ICSAP-Brazil list, especially acute conditions and exacerbations of chronic diseases. Certainly, these services can avoid hospitalizations by providing short term treatment, and discharging patients to complete their treatment at home. Another limitation is the lack of information about private health care services in the community. Having the complete information would help to clarify if patients were sent to the hospital by the public primary care clinic, by a private clinic or by the emergency service, providing better information to clarify if there was a lack of access to the FHTs.
As explained above, working in primary care is a common form of practice among recently graduated physicians in Brazil and, although we do not have information about other forms of training or about the number of years of practice in primary care, we assume that this missing information is more likely to be at random. Both FPs and generalists may have received some other form of training and may have accumulated years of practice. It is unlikely that the two types of doctors under analysis had a significant difference in the number of years of practice that would influence their ability to manage the clinical situations explored here. However, the willingness to pursue a career and to seek for improving their skills can be a common denominator across FPs, preceptors and residents in FM. Motivation to improve their practice could be the drive that influence a type of practice that presents the results found here in hospital admissions avoided.
Relative risks, most of the time, cannot reach a broad audience. By reporting the population attributable fraction, we tried to translate relative risks into absolute numbers to provide more palatable information for decision makers and politicians get better understanding of the impact of RTFM. The total number of hospital admissions that would be added or taken if all FHTs had trained Family physicians as their medical provider can more easily reach those responsible for deciding to implement an educational initiative for capacity building of human resources for primary care.
Finally, using real-world data to analyze an actual intervention in a middle-income country may reverberate better to other countries that are also trying to expand and improve their PHC systems.
Conclusion
The Brazilian Family Health Strategy has been responsible for an impressive impact on public health for the last 25 years, decreasing health inequalities by strengthening governance and providing structure and financial support for FHTs in the whole country. Only recently, capacity building of human resources for primary care–especially residency training in family medicine–has been considered as an important piece for the success of this national policy. In this study, we presented evidence that public investments in capacity building of human resources for primary care can prevent the occurrence of hospital admissions.
It will take a lot of effort from all stakeholders and political will to allocate financial resources today in educational initiatives that will take some years to pay back in health outcomes the investment made. In the case of the medical workforce for primary care–especially in LMIC–this will not be achieved without investments in residency training in family medicine.
Data Availability
All data used in this research represent patients, health care providers, medical consultations and hospital admissions information that are under the protection of the Rio de Janeiro Municipal Health Department. These data can be obtained from the Rio de Janeiro Superintendence of Primary Care (sapsmsrj@gmail.com) under the authorization of the Rio de Janeiro Municipal Health Department Research Ethics Committee (cepsmsrj@yahoo.com.br).
Funding Statement
The authors received no specific funding for this work.
References
- 1.Homar JC, Matutano CC. La evaluación de la atención primaria y las hospitalizaciones por ambulatory care sensitive conditions. Marco conceptual. Atención primaria. 2003;31: 61–65. doi: 10.1016/S0212-6567(03)70662-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Starfield B, Shi L, Macinko J. Contribution of Primary Care to Health Systems and Health. Milbank Q. 2005;83: 457–502. doi: 10.1111/j.1468-0009.2005.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact Of Socioeconomic Status On Hospital Use In New York City. Health Aff. 1993;12: 162–173. Available: https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.12.1.162 [DOI] [PubMed] [Google Scholar]
- 4.Niti M, Ng T. Avoidable hospitalisation rates in Singapore, 1991–1998: assessing trends and inequities of quality in primary care. Public Heal Policy Pract. 2003;57: 17–22. doi: 10.1136/jech.57.1.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dourado I, Oliveira VB, Aquino R, Bonolo P, Lima-Costa MF, Medina MG, et al. Trends in Primary Health Care-sensitive Conditions in Brazil. Med Care. 2011;49: 577–584. doi: 10.1097/MLR.0b013e31820fc39f [DOI] [PubMed] [Google Scholar]
- 6.Afonso MPD, Shimizu HE, Merchan-Hamann E, Ramalho WM, Afonso T. Association between hospitalisation for ambulatory care-sensitive conditions and primary health care physician specialisation: A cross-sectional ecological study in Curitiba (Brazil). BMJ Open. 2017. doi: 10.1136/bmjopen-2016-015322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gonçalves MR, Hauser L, Prestes IV, Schmidt MI, Duncan BB, Harzheim E. Primary health care quality and hospitalizations for ambulatory care sensitive conditions in the public health system in Porto Alegre, Brazil. Fam Pract. 2016;33: 238–242. doi: 10.1093/fampra/cmv051 [DOI] [PubMed] [Google Scholar]
- 8.Macinko J, Harris MJ. Brazil’s Family Health Strategy—Delivering Community-Based Primary Care in a Universal Health System. N Engl J Med. 2015;372: 2177–2181. doi: 10.1056/NEJMp1501140 [DOI] [PubMed] [Google Scholar]
- 9.Barreto ML, Rasella D, Machado DB, Aquino R, Lima D, Garcia LP, et al. Monitoring and Evaluating Progress towards Universal Health Coverage in Brazil. PLoS Med. 2014;11: 9–11. doi: 10.1371/journal.pmed.1001692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neves RG, Flores TR, Manjourany SSD, Nunes BP, Tomasi E. Time trend of Family Health Strategy coverage in Brazil, its Regions and Federative Units, 2006–2016. Epidemiol Serv Saude. 2016;27: 1–8. doi: 10.5123/S1679-49742018000300008 [DOI] [PubMed] [Google Scholar]
- 11.Rasella D, Aquino R, Barreto ML. Reducing Childhood Mortality From Diarrhea and Lower Respiratory Tract Infections in Brazil. Pediatrics. 2010;126. doi: 10.1542/peds.2009-3197 [DOI] [PubMed] [Google Scholar]
- 12.Aquino R, Oliveira NF De, Barreto ML. Impact of the Family Health Program on Infant Mortality in Brazilian Municipalities. Am J Public Health. 2009;99: 87–93. doi: 10.2105/AJPH.2007.127480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Venancio SI, Etsuko T, Teresa M, Sanches C. Effectiveness of Family Health Strategy on child´s health indicators in São Paulo State. Rev Bras Saúde Matern Infant. 2016;16: 271–281. 10.1590/1806-93042016000300004 [DOI] [Google Scholar]
- 14.Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: A nationwide analysis of longitudinal data. BMJ. 2014. doi: 10.1136/bmj.g4014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hone T, Rasella D, Barreto M, Atun R, Majeed A. Large Reductions In Amenable Mortality Associated With Brazil’s Primary Care Expansion And Strong Health Governance. Health Aff. 2017;36: 149–158. doi: 10.1377/hlthaff.2016.0966 [DOI] [PubMed] [Google Scholar]
- 16.Mendonça CS, Harzheim E, Duncan BB, Nunes LN, Leyh W. Trends in hospitalizations for primary care sensitive conditions following the implementation of Family Health Teams in Belo Horizonte, Brazil. Health Policy Plan. 2012;27: 348–355. doi: 10.1093/heapol/czr043 [DOI] [PubMed] [Google Scholar]
- 17.Marques AP, Elena D, Montilla R. Hospitalization of older adults due to ambulatory care sensitive conditions. Rev Saude Publica. 2014;48: 817–826. doi: 10.1590/s0034-8910.2014048005133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Macinko BJ, Dourado I, Aquino R, Bonolo PDF, Lima-costa MF, Medina MG, et al. Major Expansion Of Primary Care In Brazil Linked To Decline In Unnecessary Hospitalization. Health Aff. 2010;29: 2149–2160. Available: https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2010.0251 [DOI] [PubMed] [Google Scholar]
- 19.Ministério da Saúde. Programa Mais Médicos. 2017. doi: 10.1590/1807-57622016.0520 [DOI] [Google Scholar]
- 20.Wollmann L, D’Avila OP, Harzheim E. Programa Médicos pelo Brasil: mérito e equidade. Rev Bras Med Família e Comunidade. 2019;15: 1–6. [Google Scholar]
- 21.Augusto DK, David L, Oliveira DOPS de, Trindade TG da, Junior NL, Poli Neto P. Quantos médicos de família e comunidade temos no Brasil? Rev Bras Med Família e Comunidade. 2018;13: 1–4. 10.5712/rbmfc13(40)1695 [DOI] [Google Scholar]
- 22.Scheffer Mário. DEMOGRAFIA MÉDICA NO BRASIL 2018. São Paulo; 2018. [Google Scholar]
- 23.Soranz D, Pinto LF, Penna GO. Themes and Reform of Primary Health Care (RCAPS) in the city of Rio de Janeiro, Brazil article. Cien Saude Colet. 2016; 1327–1338. doi: 10.1590/1413-81232015215.01022016 [DOI] [PubMed] [Google Scholar]
- 24.Justino ALA, Oliver LL, Melo TP de. Implementation of the Residency Program in Family and Community Medicine of the Rio de Janeiro Municipal Health Department, Brazil article. 2016; 1471–1480. doi: 10.1590/1413-81232015215.04342016 [DOI] [PubMed] [Google Scholar]
- 25.SBMFC. Currículo Baseado em Competências para Medicina de Família e Comunidade. In: Currículo Baseado em Competências para Medicina de Família e Comunidade [Internet]. 2015. [cited 27 Feb 2020]. Available: http://www.sbmfc.org.br/wp-content/uploads/media/Curriculo Baseado em Competencias(1).pdf [Google Scholar]
- 26.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994. doi: 10.1016/0895-4356(94)90129-5 [DOI] [PubMed] [Google Scholar]
- 27.Jantsch AG, Burström B, Nilsson GH, Leon AP De. Residency training in family medicine and its impact on coordination and continuity of care: an analysis of referrals to secondary care in Rio de Janeiro. BMJ Open. 2022;12: 1–9. doi: 10.1136/bmjopen-2021-051515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jantsch AG, Burström B, Nilsson G, Leon AP De. Detection and follow-up of chronic health conditions in Rio de Janeiro–the impact of residency training in family medicine. BMC Fam Pract. 2021;22: 1–11. doi: 10.1186/s12875-021-01542-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Levinson W, Kallewaard M, Bhatia RS, Wolfson D, Shortt S, Kerr EA. ‘Choosing Wisely’: a growing international campaign. BMJ. 2014; 1–9. doi: 10.1136/bmjqs-2014-003821 [DOI] [PubMed] [Google Scholar]
- 30.Shaws E, Oandasan I, Fowler N. CanMEDS-FM 2017: A competency framework for family physicians across the continuum. In: The College of Family Physicians of Canada—Le Collège des Médecins de Famille du Canada [Internet]. Mississauga, ON; 2017. [cited 27 Feb 2020] p. 21. Available: https://www.cfpc.ca/uploadedFiles/Resources/Resource_Items/Health_Professionals/CanMEDS-Family-Medicine-2017-ENG.pdf [Google Scholar]
- 31.EURACT Council. THE EUROPEAN DEFINITION OF GENERAL PRACTICE/FAMILY MEDICINE. 2011. [cited 1 Jan 2020] p. 11. Available: https://www.woncaeurope.org/sites/default/files/documents/Definition EURACTshort version revised 2011.pdf [Google Scholar]
- 32.Giugliano D, Maiorino MI, Bellastella G, Chiodini P, Esposito K. Glycemic Control, Preexisting Cardiovascular Disease, and Risk of Major Cardiovascular Events in Patients with Type 2 Diabetes Mellitus: Systematic Review With Meta-Analysis of Cardiovascular Outcome Trials and Intensive Glucose Control Trials. J Am Heart Assoc. 2019;8. doi: 10.1161/JAHA.119.012356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387: 957–967. doi: 10.1016/S0140-6736(15)01225-8 [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization and the United Nations Children’s Fund (UNICEF). Operational Framework for Primary Health Care: Transforming Vision into Action. Geneva; 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used in this research represent patients, health care providers, medical consultations and hospital admissions information that are under the protection of the Rio de Janeiro Municipal Health Department. These data can be obtained from the Rio de Janeiro Superintendence of Primary Care (sapsmsrj@gmail.com) under the authorization of the Rio de Janeiro Municipal Health Department Research Ethics Committee (cepsmsrj@yahoo.com.br).