Supplemental Digital Content is Available in the Text.
Reviewing historic articles offers important learning points for current practice in chronic pain management and veterans' health, which is still a significant issue for military rehabilitation.
Keywords: Chronic pain, Postamputation pain, Phantom limb pain, Residual limb pain, British army, Rehabilitation, Military medicine, First World War, Afghanistan, Veterans, Blast injury, Applied history, Systematic review, History
Abstract
Limb trauma remains the most prevalent survivable major combat injury. In the First World War, more than 700,000 British soldiers received limb wounds and more than 41,000 underwent an amputation, creating one of the largest amputee cohorts in history. Postamputation pain affects up to 85% of military amputees, suggesting that up to 33,000 British First World War veterans potentially reported postamputation pain. This qualitative systematic review explores the professional medical conversation around clinical management of chronic postamputation pain in this patient cohort, its development over the 20th century, and how this information was disseminated among medical professionals. We searched The Lancet and British Medical Journal archives (1914–1985) for reports referring to postamputation pain, its prevalence, mechanisms, descriptors, or clinical management. Participants were First World War veterans with a limb amputation, excluding civilians and veterans of all other conflicts. The search identified 9809 potentially relevant texts, of which 101 met the inclusion criteria. Reports emerged as early as 1914 and the discussion continued over the next 4 decades. Unexpected findings included early advocacy of multidisciplinary pain management, concerns over addiction, and the effect of chronic pain on mental health emerging decades earlier than previously thought. Chronic postamputation pain is still a significant issue for military rehabilitation. Similarities between injury patterns in the First World War and recent Iraq and Afghanistan conflicts mean that these historical aspects remain relevant to today's military personnel, clinicians, researchers, and policymakers.
1. Introduction
Limb trauma represents the most prevalent survivable major combat injury. Collectively, for all belligerent nations, the First World War yielded the largest military amputee cohort in history. In excess of 700,000 British soldiers received limb wounds during the conflict, resulting in an estimated total of more than 41,000 surviving young male amputees in the United Kingdom alone.5 The pattern and scale of limb wounds sustained during the First World War was unlike anything seen in prior conflicts. The combination of penetrating injuries from high-velocity projectiles, consequential major tissue disruption, and a high risk of infection in contaminated wounds (particularly by anaerobic microbes in the preantibiotic era) predicated a low threshold for the consideration of early life-saving amputation. Without effective vaccinations or antibiotics, debridement and early surgical intervention were often the most appropriate surgical tactics. Early amputation was further utilised due to the need to process unprecedented numbers of casualties through the evacuation pathway and avoid the time consuming and often ultimately futile job of limb reconstruction. Of all injuries amongst British soldiers in the First World War that were not immediately fatal, an overall proportion of 13% resulted in amputation.20 These numbers are unequalled by any subsequent conflict. For comparison, the Second World War led to approximately 12,000 British amputee veterans and the most recent Afghanistan conflict resulted in 302 UK service personnel undergoing one or more traumatic or surgical amputations between 2001 and 2020 (a total of 0.2% of the 150,610 British personnel who served in Afghanistan).50,51
Significant residual limb pain affects up to 85% of today's military amputees, and phantom limb is reported by at least 59% of all military amputees.1,26,37 If the same were true for the First World War cohort, then 35,000 British amputee veterans may have experienced chronic pain as a result of their amputation. Chronic pain has significant negative effect on the quality of life.53 Yet there has been no detailed analysis reporting the effect of conflict-related chronic postamputation pain on veterans' long-term health and quality of life, on resulting years lost to disability, in the evolution of medical attitudes, the clinical assessment, or the management for postamputation pain.68
This systematic review is part of a wider programme examining this topic, including conventional historiography and analysis of archival material, notably First World War veterans' pension files, and a prospective long-term follow-up of British injured veterans from recent conflicts.2,3,24 Although articles from medical journals of this period are often cited by historians, the cited sources are usually selected without a systematic approach, with the inherent risk of bias that such an approach risks.
It has been suggested that pain is often absent in published medical accounts due to a professional reluctance to discuss a condition that could not be surgically resolved. Edwards et al. considered that “because there was not potential for surgical resolution and it did not affect tissue viability for prosthetics, it [pain] was marginalised in medical discussion of amputation during World War One and in the period of reflection afterwards.”26 Establishing the extent to which this knowledge and interest was disseminated amongst medical professionals was one of the key objectives of this review. The goals of this systematic review were therefore to explore, using a systematic search of professional medical journals:
(1) the professional medical conversation on the aetiology (in terms of mechanistic descriptor), contemporary treatment, clinical presentation, and assessment of chronic postamputation pain in veterans injured on active service during the First World War;
(2) the extent to which these developed over the lifetimes of these veterans.
Secondary aims were to identify when chronic postamputation pain (including phantom and residual limb, as defined in Table 1) became recognised as a potential disability either in its own right or as a contributing factor, when concepts of interdisciplinary or multidisciplinary treatment for chronic postamputation pain emerged, and the extent to which emergent medical specialties (eg, neurology, anaesthetics, psychiatry, orthopaedics, pain medicine) started to contribute to pain management.
Table 1.
Definitions of postamputation pain as outlined by Edwards et al. and the International Association for the Study of Pain.25,33,34
| Residual limb pain | Spontaneous (continuous or paroxysmal) or evoked pain perceived as originating in the residual limb including the stump; pain unrelated to amputation, eg, other injuries, such as damage of the nerves above the level of amputation |
| Stump pain | Spontaneous (continuous or paroxysmal) or evoked pain in the amputation stump, includes neuroma, muscle, and bone stump as pain sources |
| Phantom limb pain | Spontaneous (continuous or paroxysmal) or evoked pain perceived as arising in the missing limb |
| Phantom limb sensation | Any sensation of the missing limb including pain |
| Neuropathic pain | Pain caused by a lesion of disease of the somatosensory nervous system |
2. Methods
The review protocol was prospectively registered with the Open Science Framework on May 4, 2020 at osf.io/cr5ab (DOI: 10.17605/OSF.IO/CR5AB).
2.1. Search criteria
A search of the 2 major professional medical journals of the 20th century in the United Kingdom, The Lancet and the British Medical Journal, for the full years 1914 to 1985 was undertaken. This time window is in line with the medical pension files for the First World War veterans held by the UK's National Archives at Kew catalogued in the file series and referred to as “PIN 26.”24 The search was intended to retrieve all articles that described the prevalence, assessment, or pathophysiological pain mechanisms of postamputation pain sustained by veterans of the First World War, as well as clinical descriptions, case histories, and treatments. The search was not limited to specific types of text, with all original research studies, reviews, editorials, conference reports, and correspondence included. As not all past issues of the journals were available on standard medical databases (eg, PubMed), The Lancet was searched through its own archives with texts retrieved through ScienceDirect, whereas JSTOR was used to search and retrieve texts from the British Medical Journal. Searches were conducted on June 3 to 4, 2020 (see Appendix, available online at http://links.lww.com/PR9/A204).
2.2. Selection criteria
Included reports covered participants who were military veterans identified as having sustained a limb injury whilst on active service during the First World War (Table 2). In line with the British government's definition, “veterans” were all those who served one day or more in the armed forces.51 In the registered protocol, we had intended to include veterans with chronic pain due to amputation and peripheral nerve injury. However, due to the nature and number of retrieved texts, a protocol amendment decision was made by the first and senior author to focus on postamputation pain only. Texts on peripheral nerve injury were thus excluded during full-text screening.
Table 2.
Inclusion criteria for text screening.
| Population | First World War veterans with limb injury and amputation sustained on active service |
| Intervention | Any treatments intended to alleviate postamputation pain |
| Comparison | A range of methods were employed but no randomised control trials. Therefore, there are often no comparisons. However, comparisons were extracted where the author has described them |
| Outcome | Often no recorded outcomes or imprecise descriptions. Therefore, anything reported by the author as an outcome was extracted |
Reports regarding veterans from all subsequent conflicts and civilians were excluded. The participant's injury and date range were the only specific inclusion criteria for the study because it was intended to explore the professional medical “conversation” around these conditions, their aetiologies, and their treatments as broadly and inclusively as possible. Limiting the search with specific inclusion and exclusion criteria based on particular interventions or study designs would have been overly restrictive and could create selection bias. Due to the age of the texts, it was not possible to seek a greater level of detail through contacting authors or searching unpublished sources.
2.3. Study selection and data extraction
Screening was performed by one author (S.D.S.) with inclusion conflicts and uncertainties resolved by conversation with the senior author (A.S.C.R.). Data extraction was performed by one author (S.D.S.).
Deduplication, title, and full-text screening were performed using Covidence (Veritas Health Innovation, Melbourne, Australia). It had been intended to screen studies by title and abstract before a full-text screening. However, due to the age of the texts, the method of digitisation and the wide range of article types identified in the search, none of the retrieved texts included an abstract, so initial screening had to be performed based on title alone. As the search covered almost a century of publication, there was no standardisation of format or terminology within the text, and data were extracted only in a qualitative manner. Extracted data were recorded in Microsoft Excel 365 and included details on patients, wounds sustained, treatment, and assumed mechanistic descriptors of pain. Results were exported into the qualitative analysis software, NVivo 12 (QSR International, Doncaster, Australia).
This study was conducted using archival material and was intended to explore the professional medical conversation across the 20th century, with a particular focus on the dynamics of how clinicians discussed and shared these ideas. Hence, a meta-analysis or a risk of bias assessment would have been inappropriate and was not conducted. Therefore, the output is in the form of a descriptive synthesis, structured around the aetiology and mechanistic descriptors of chronic postamputation pain and treatments strategies applied.
2.4. Terminology
We attempted to employ a classification of pain in our findings, using the terminology of the texts' authors. Doing so on a consistent and widely agreed basis proved problematic as definitions and criteria for diagnoses changed over the period, and attempts to formalise classification of pain are a recent phenomenon, which postdate our search period. Chapters in the classification of chronic pain were only included for the first time in the 11th iteration of the International Classification of Diseases (ICD-11) in 2019.68
As a result, postamputation pain was defined with the definitions in Table 1, taken from Edwards et al.26 Neuropathic pain was defined, as far as possible given the historic nature of the text, in broad alignment with current era definition published by the International Association for the Study of Pain, which is consistent with the recently published inaugural pain chapters in ICD-11.33–35,60 The historical and diverse nature of the reports resulted in a necessary degree of diagnostic imprecision, with reviewers exercising a degree of pragmatism. We based our classification largely on the history of nerve injury (inherently a feature of limb amputation), symptom descriptors, and the authors' use of contemporary terms such as “neuritis,” “neuralgia,” and “causalgia.” This would be broadly consistent with the “possible” level of diagnostic certainty in modern algorithms, the use of which we have previously reported in a historical context.29,57
3. Results
3.1. Article types
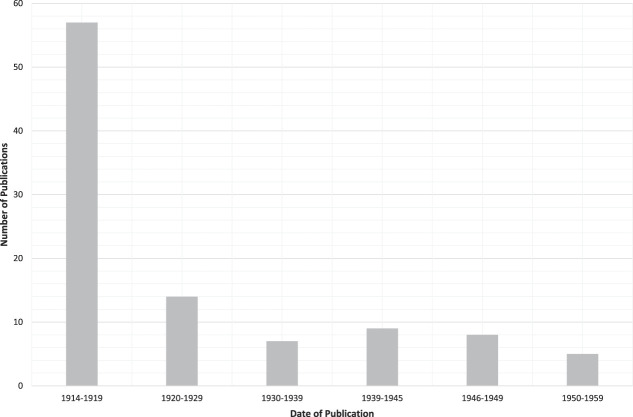
After deduplication, 8981 reports were assessed for inclusion. Screening by title excluded 4600 texts, and full-text screening removed a further 4280. One hundred one texts were thus included in the final data set (Fig. 1). Although the search covered the years 1914 to 1985, the most recent relevant text to be included in the final data set was published in 1956. That no relevant texts were retrieved from subsequent decades probably reflects the decreasing number of living veterans of First World War. Seventy-one of the texts were retrieved from the British Medical Journal and 30 from The Lancet. As anticipated, the discussion around conflict-related chronic pain peaked during the First World War, and the number of texts declined rapidly after 1919, with only a small increase around the Second World War (Fig. 2).
Figure 1.
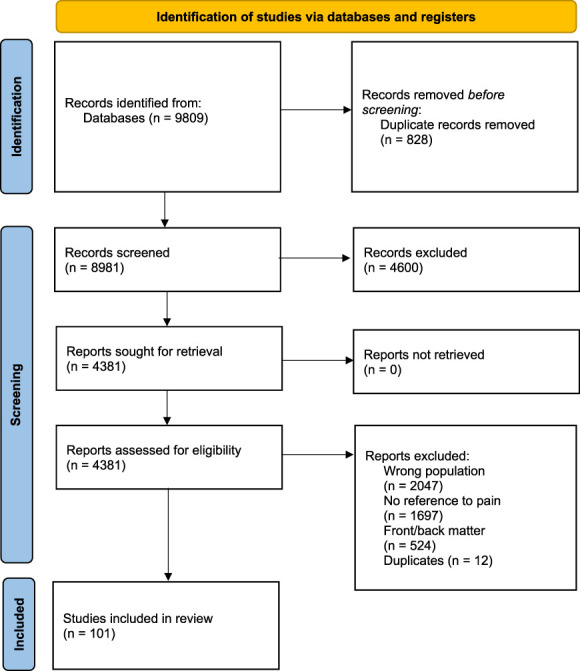
Retrieved texts for The Lancet and The British Medical Journal, with reasons for exclusion.
Figure 2.
Total retrieved publications by decade for The Lancet and the British Medical Journal.
Retrieved texts categorised by article type are shown in Table 3. Conference summaries accounted for the largest type at 22 (22%). Narrative reviews and articles reflecting on previous cases, categorised as “in my experience,” each totalled 19 (19%). The remainder were 18 case reports (18%), 13 book reviews (13%), and 6 “other” (6%), the majority of which was correspondence. No randomised controlled trials testing an intervention were identified.
Table 3.
Categories of texts retrieved.
| Category | Total | 1914–19 | 1920–29 | 1930–39 | 1940–45 | 1946–49 | 1950–59 |
|---|---|---|---|---|---|---|---|
| Book review | 13 | 8 | 1 | 2 | 1 | 1 | — |
| Case report series | 16 | 6 | 5 | 1 | — | 2 | 2 |
| Conference summary | 22 | 15 | 3 | 2 | 2 | — | — |
| “In my experience” | 19 | 10 | 2 | 1 | 1 | 4 | 1 |
| Narrative review | 19 | 13 | 2 | — | 4 | — | — |
| Other | 6 | 5 | — | — | 1 | — | — |
| Question and answer | 2 | — | — | 1 | — | — | 1 |
| Single case report | 2 | — | 1 | — | — | 1 | — |
In total, 50 articles referenced other texts with a total of 170 references: 26 (15%) of which were in another issue of the same journal, suggesting a response to an article or correspondence, and 53 (31%) were in another professional medical journal. A further 39 (23%) were originally published in an European journal, most commonly in French, German, or Italian, indicating that these ideas were being discussed and shared internationally.
3.2. Types of pain
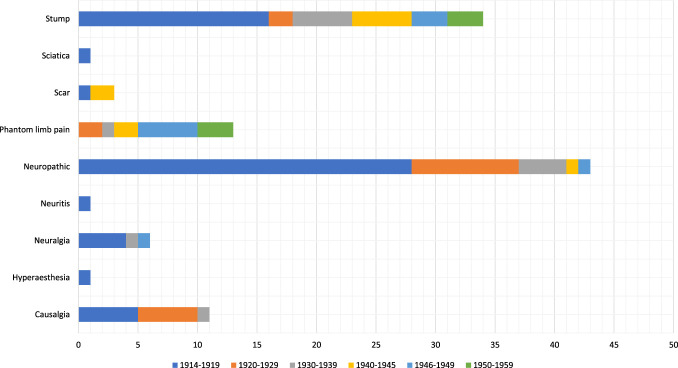
The retrieved files contained 131 direct references to pain, categorised during data extraction into 9 types, with 18 articles (14%) referencing more than one type of pain (Table 4). The most frequently reported pain categories were neuropathic and stump pain (as defined in Table 1), with 43 (33%) and 34 (26%) references, respectively. Stump pain was the only category to feature in every decade from the 1910s to the 1950s. Neuropathic pain was most commonly recorded during 1914 to 1918. Common terms for neuropathic pain (“neuralgia,” “neuritis,” and “causalgia”) were directly employed by the primary authors in 18 of articles (14%). Despite modern estimates that phantom limb sensation (as defined in Table 1) can affect up to 70% of amputees, no specific references to this condition were retrieved.1 Thirteen studies (13%) investigated causes and treatment of phantom limb pain, reaching a peak in the period 1946 to 1949.
Table 4.
Types of pain reported in retrieved texts.
| Pain type | Total | 1914–19 | 1920–29 | 1930–39 | 1940–45 | 1946–49 | 1950–59 |
|---|---|---|---|---|---|---|---|
| Causalgia | 11 | 5 | 5 | 1 | — | — | — |
| Hyperaesthesia | 1 | 1 | — | — | — | — | — |
| Neuralgia | 6 | 4 | — | 1 | — | 1 | — |
| Neuritis | 1 | 1 | — | — | — | — | — |
| Neuropathic | 43 | 28 | 9 | 4 | 1 | 1 | — |
| Phantom limb pain | 13 | — | 2 | 1 | 2 | 5 | 3 |
| Scar | 3 | 1 | — | — | 2 | — | — |
| Sciatica | 1 | 1 | — | — | — | — | — |
| Stump | 34 | 16 | 2 | 5 | 5 | 3 | 3 |
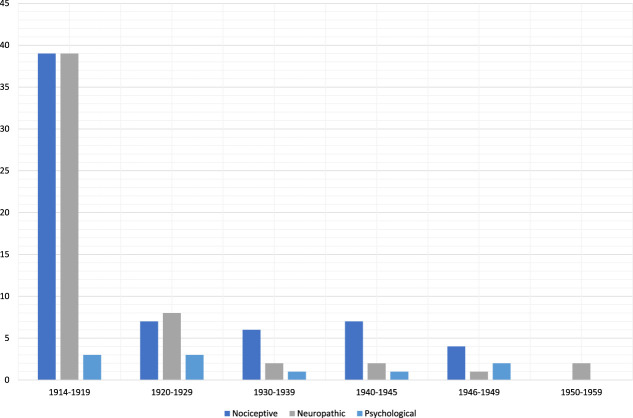
Theories into potential causes of chronic postamputation pain were recorded and classified under 3 themes: “nociceptive,” “neuropathic,” or “psychological,” in accordance with the usage and concepts pertaining at the time of publication (Table 5). Although these 3 categories are not terms necessarily widely used by clinicians of the period, these descriptive terms were felt to be most appropriate by the authors. The most commonly reported theories were based around pain caused by a physiological mechanism often relating to treatment and rehabilitation. These included a poorly fitting prosthesis, amputation technique causing physical issues with the stump, scarring, or necrosed bone. Together, these accounted for 64 (50%) of all mechanistic descriptors. The second category, pain with a neuropathic origin, accounted for 54 references (42%) and also peaked during the First World War. The third category, “pain of a psychological origin,” accounted for 10 references (8%), and whilst this is an outdated concept for today's medicine, it was considered important to include due to the stigma that still surrounds chronic pain and the potential effect of untreated pain on a patient's mental health.
Table 5.
Mechanistic descriptors of postamputation pain in retrieved texts.
| Mechanistic descriptors | Total | 1914–19 | 1920–29 | 1930–39 | 1940–45 | 1946–49 | 1950–59 |
|---|---|---|---|---|---|---|---|
| Nociceptive | 64 | 39 | 7 | 6 | 7 | 4 | 1 |
| Abscesses | 3 | 1 | — | 1 | — | 1 | — |
| Prosthetic limb fit | 3 | 1 | 1 | — | — | 1 | — |
| Amputation technique | 11 | 5 | — | 2 | 3 | — | 1 |
| Treatment | 7 | 3 | 1 | 1 | 2 | — | — |
| Bone spurs | 2 | 2 | — | — | — | — | — |
| Calluses | 2 | 1 | — | — | — | 1 | — |
| Foreign bodies | 6 | 6 | — | — | — | — | — |
| Jactitation | 2 | — | — | 1 | — | 1 | — |
| Necrosis | 2 | 2 | — | — | — | — | — |
| New bone formation | 1 | 1 | — | — | — | — | — |
| Osteitis | 3 | 2 | — | — | 1 | — | — |
| Scar tissue | 16 | 12 | 2 | 1 | 1 | — | — |
| Sepsis | 2 | — | 2 | — | — | — | — |
| Sequestrum | 2 | 2 | — | — | — | — | — |
| Vascular | 2 | 1 | 1 | — | — | — | — |
| Neuropathic | 54 | 39 | 8 | 2 | 2 | 1 | 2 |
| Damage to nerve fibres | 2 | 2 | — | — | — | — | — |
| Infective inflammation | 13 | 11 | 1 | 1 | — | — | — |
| Lesions of nerve trunks | 10 | 8 | 2 | — | — | — | — |
| Nerve concussion | 3 | 3 | — | — | — | — | — |
| Nerve regeneration | 9 | 4 | 4 | — | — | — | 1 |
| Nerves | 2 | 1 | — | 1 | — | — | — |
| Neuroma | 15 | 10 | 1 | — | 2 | 1 | 1 |
| Psychological | 10 | 3 | 3 | 1 | 1 | 2 | — |
| Psychical | 9 | 3 | 3 | 1 | 1 | 1 | — |
| Personality type | 1 | — | — | — | — | 1 | — |
The total number of participants described in the included reports was 9,326. Eleven studies included at least 100 participants; the largest reported 2000 patients. The mechanism of injury was specifically noted for only 168 patients. The most common cause reported was a gunshot wound, a term used during the First World War as inclusive of both projectile and blast injuries and which varied from a rifle bullet to shrapnel and fragments from artillery shells.
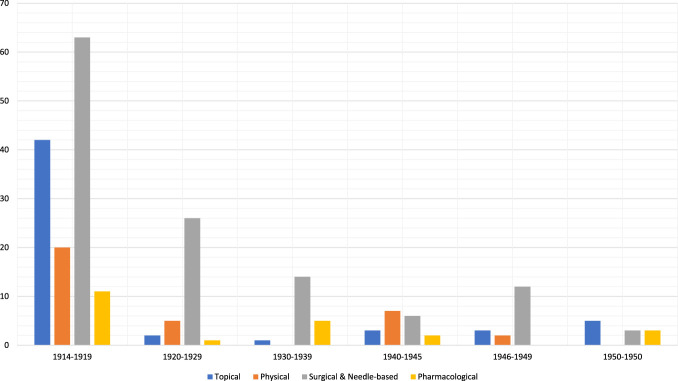
3.3. Interventions
Forty-three pain management interventions were described by authors (Table 6). The most frequently reported interventions were surgical or percutaneous needle-based therapies. Sixty-seven reports (66%) were made from a surgical perspective. Outcomes for interventions were reported in any manner in only 28 texts (28%). The most successful treatment reported was neuroma percussion, a “refreshingly simple method” based on the theory that repeated targeted pressure with a small mallet or bar on traumatised nerve endings would cause them to degenerate into fibrous tissue and render them into a painless state of “chronic concussion.”12 Articles referring to this treatment reported 2 positive and zero negative outcomes. Eight separate treatments reported a single negative outcome, although no treatments reported more than one.
Table 6.
Treatments for postamputation pain in retrieved texts.
| Treatment | Total | 1914–19 | 1920–29 | 1930–39 | 1940–45 | 1946–49 | 1950–59 |
|---|---|---|---|---|---|---|---|
| Topical | 56 | 42 | 2 | 1 | 3 | 3 | 5 |
| Bath (unspecified) | 2 | 2 | — | — | — | — | — |
| Air bath | 2 | 2 | — | — | — | — | — |
| Wax bath | 1 | — | — | 1 | — | — | — |
| Whirlpool bath | 4 | 4 | — | — | — | — | — |
| Compression | 4 | 1 | — | — | 1 | 2 | — |
| Counter irritation | 1 | 1 | — | — | — | — | — |
| Electrical | 14 | 13 | — | — | 1 | — | — |
| Electrodes | 1 | 1 | — | — | — | — | — |
| Faradism | 4 | 4 | — | — | — | — | — |
| Galvanism | 5 | 4 | — | — | 1 | — | — |
| Sinusoidal | 1 | 1 | — | — | — | — | — |
| Heat | 4 | 3 | 1 | — | — | — | — |
| Diathermy | 1 | 1 | — | — | — | — | — |
| Radiant heat | 1 | 1 | — | — | — | — | — |
| Irradiation | 1 | 1 | — | — | — | — | — |
| Percussion | 4 | — | — | — | — | 1 | 3 |
| Radium | 2 | 1 | 1 | — | — | — | — |
| Vibration | 4 | 2 | — | — | — | — | 2 |
| Physical | 34 | 20 | 5 | - | 7 | 2 | - |
| Distraction | 2 | — | — | — | 2 | — | — |
| Massage | 16 | 12 | 2 | — | 2 | — | — |
| Physiotherapy | 9 | 5 | 2 | — | 1 | 1 | — |
| Prosthetic limb | 4 | — | 1 | — | 2 | 1 | — |
| Rest | 1 | 1 | — | — | — | — | — |
| Splinting | 2 | 2 | — | — | — | — | — |
| Surgical and needle based | 124 | 63 | 26 | 14 | 6 | 12 | 3 |
| Surgery (unspecified) | 28 | 21 | 5 | — | — | 2 | — |
| Chordotomy | 1 | — | — | — | — | 1 | — |
| Excision | 14 | 7 | 3 | 2 | 1 | 1 | — |
| Injections | 7 | 2 | 1 | 1 | — | 3 | — |
| Alcohol injections | 13 | 5 | 3 | 3 | 2 | — | — |
| Local anaesthesia injections | 5 | 1 | — | 2 | — | — | 2 |
| Minimal disturbance | 5 | 1 | 1 | 1 | 2 | — | — |
| Nerve block | 2 | — | 1 | — | — | 1 | — |
| Nerve division | 5 | 2 | 1 | — | — | 2 | — |
| Nerve graft | 4 | 2 | 2 | — | — | — | — |
| Nerve shortening | 12 | 8 | 1 | 2 | 1 | — | — |
| Nerve suture | 20 | 14 | 6 | — | — | — | — |
| Rhizotomy | 2 | — | 2 | — | — | — | — |
| Re-amputation | 3 | — | — | 2 | — | 1 | — |
| Sympathectomy | 3 | — | — | 1 | — | 1 | 1 |
| Pharmacological | 22 | 11 | 1 | 5 | 2 | - | 3 |
| Drugs (unspecified) | 3 | 1 | 1 | — | 1 | — | — |
| Aprobarbital (Allonal) | 1 | — | — | 1 | — | — | — |
| Benzocaine | 1 | — | — | — | — | — | 1 |
| Bromides | 2 | 2 | — | — | — | — | — |
| Fibrolysin | 1 | 1 | — | — | — | — | — |
| Luminal | 1 | — | — | 1 | — | — | — |
| Morphine | 2 | 1 | — | 1 | — | — | — |
| Nerve sedatives | 1 | — | — | — | 1 | — | — |
| Novocain | 1 | 1 | — | — | — | — | — |
| Omnopon | 1 | — | — | 1 | — | — | — |
| Opiates (unspecified) | 1 | 1 | — | — | — | — | — |
| Phenacetin | 2 | 2 | — | — | — | — | — |
| Procaine | 1 | — | — | — | — | — | 1 |
| Aminophenazone (Pyramidon) | 2 | 2 | — | — | — | — | — |
| Sedobrol | 1 | — | — | 1 | — | — | — |
| Tolazoline | 1 | — | — | — | — | — | 1 |
4. Discussion
The aim of this qualitative systematic review was to describe the evolution of professional recognition and clinical management of postamputation pain in First World War veterans between 1914 and 1985. We systematically searched the archives of The Lancet and the British Medical Journal to investigate the professional medical conversation regarding the mechanistic descriptors, assessment, and treatment of chronic postamputation pain in this cohort across the first 70 post–(First World) war years.
The results demonstrate that clinicians were aware of, and discussed, the possibility of long-term pain after conflict-related amputations from at least the beginning of the 20th century. It also reveals sparse consensus regarding the pathophysiology or clinical management of this condition and how it should be assessed, a situation which persists to the current era. The final article to be retrieved by the search (although excluded during the screening process), published in 1982, acknowledged that through a “lack of understanding, lack of treatment, and even perhaps the wrong treatment … many pain syndromes are virtually untreatable,” echoing sentiments expressed in 1918, when “it became evident that there was much to be learnt … prognosis … was little more than sanguine guesswork.”18,45 Apart from the Official History of the First World War and recommendations published at the start of the Second World War, we are unable to identify any major organised or prospective effort to research this cohort from this archive.48,53 This represents a missed research opportunity to improve the lives of military personnel who sustained such injuries, and which perhaps gives some way to explaining the lack of advance that was seen in this area across the 20th century.26 The prospective and longitudinal Armed Services Trauma Rehabilitation Outcome Study (ADVANCE) examining injured British veterans from recent conflicts represents the grasping of an important opportunity to rectify this historical omission.2,3
Throughout the 101 articles included in this review, 4 discussion themes emerged and were selected for further discussion: mechanistic descriptors of pain, treatment of chronic postamputation pain, assessment of pain and treatments, and cycles of learning.
4.1. Mechanistic descriptors of pain
Only recently have mechanistic descriptors of pain been formalised into the 11th Revision of the International Classification of Diseases, which perhaps reflects our still incomplete understanding of chronic pain.33,68 The lack of such a universally agreed classification in the 20th century presented challenges for this review. Nevertheless, we were able to identify 3 broad descriptive themes relating to chronic postamputation pain in the retrieved texts. This interpretation was predominately by the primary author (S.D.S.) with assistance from the senior author (A.S.C.R.) based on the original terms used in the retrieved texts. These can be broadly categorised as follows: “pain of a nociceptive origin” (sometimes also described as “physiological pain”), “pain of a neuropathic origin” from nerve lesions (which includes an infective neuritis theory that was prevalent at certain times), and the concept of “pain of a psychological origin,” which is largely an outmoded idea today (Table 5). In data extraction, the terms “physical” or “physiological mechanisms” were used to include all pain described by the original authors to have been associated with the amputation, with the subsequent medical treatment of the stump, such as poorly fitting prostheses, inadequate rehabilitation, or with issues physiologically concomitant with the amputation, such as bone spurs, sequestrum, new bone formation, or heterotopic ossification. Pain of a neuropathic origin often related to lesions to nerve trunks, neuromata, and the involvement of nerve fibres in scarring, whilst “psychological” has been used to refer to all mechanisms of pain that were believed to include a psychological or emotional component, in addition to “malingering,” “neurasthenia,” and “innate personality types.”
The peaks in these usages reflect wider trends within medical practice across the 20th century, including the rise of new specialities: for example, reports of a nociceptive mechanism peaked during the First World War as discussion focused on the evaluation and adaptation of techniques for amputation and integrated rehabilitation, and reports of psychological mechanisms peaked in the 1940s when it was becoming clear that physical or pharmaceutical treatments were unlikely to succeed in treating this cohort's chronic pain (Fig. 3). Patient files from The National Archives demonstrate that some veterans moved across these pain categories throughout their lives, roughly following the trends in mechanistic descriptors seen in this review. One veteran who suffered chronic postamputation pain for 6 decades was serially recorded by his doctors as having pain originating from a “bad stump,” which was unsuccessfully treated with surgery, then “nerve irritation,” again unsuccessfully treated with sedatives and bromides (antiseizure medication), and finally when it became clear that no treatment had any substantial effect on his pain, doctors theorised that his pain was of psychological origin: he was simply an innately “weak personality” and unlikely to ever recover.5,24,52
Figure 3.
Mechanistic descriptors of pain in retrieved texts by decade.
Recently published literature on this topic has asserted that discussion of postamputation pain was “exclusively within the framework of residual stump pain and the barriers it posed to successful fitting and use of a prosthesis” and that “there was little discussion of the other major form of postamputation pain, namely, phantom limb pain, although phantom limb pain had been identified and described at least 50 years previously.”26 This wider review of both The Lancet and the British Medical Journal reveals that this was in fact not the case and, whilst stump pain was the most commonly referenced type of postamputation pain within this cohort, phantom limb pain was also regularly discussed, accounting for 12 (12%) of all references to pain and appearing in every decade from the 1920s until the 1950s (Fig. 4). Two of these texts note the incidence of phantom limb pain was likely higher but “patients are often so afraid of their sanity being doubted if they talk of their phantom pain that they frequently only complain of a tender stump” or as “one very intelligent subject remarked, “I did not report sick because I did not expect the doctor to treat a ghost.””4,25
Figure 4.
Total references to categorised pain types in retrieved texts by decade.
Given the prevalence of both patient and professional concerns over the stigma of chronic pain and the tendency within military hospitals to encourage stoic acceptance of pain, one unexpected finding of this review was that the potential for untreated chronic pain to affect a patient's mental health was recognised and discussed amongst clinicians from the beginning of this period: neuropathic pain was noted to be “particularly intolerable and apt to undermine the mental stability in a remarkable way.”13,20 The psychological aspects of chronic pain were acknowledged from the beginning of the period and throughout, with surgeons warning “against too readily ascribing to hysteria the terrible sufferings of many cases of nerve injury” as “prolonged pain from any cause can lead to the development of psychic changes and increased susceptibility to all painful stimuli: resistance is diminished by suffering.”14,16
The importance of the patient's state of mind during treatment and of a good doctor/patient relationship was noted by multiple authors across both journals. Based on his experience as a consulting surgeon at England's major limb-fitting centre, Queen Mary's Hospital, Edred M Corner believed that long-term pain was caused by 3 factors, in a theory similar to today's biopsychosocial concept of chronic pain: infective inflammation, the presence of foreign bodies, and psychological factors: “the patient will have stored up memories of past operations, pains and phantoms. With such a combination any hope of immediate cure is futile.”21 From 1920, the role of the patient in their recovery was emphasised in professional lectures with the radical idea that “the surgeon is not all important, the patient must assist,” as “whether pain recurred depended on the patient's power to combat [it] …. The degree of mental deterioration had a good deal with do with the amount of success attained.”40,42 This phase within the professional conversation also highlighted the importance of a good doctor/patient relationship in which patients were not afraid to share their symptoms and would not be stigmatised for doing so. In a series of correspondence in 1948, JAW Bingham and Donaldson Craig refer to the possibility that phantom limb pain was likely far more common than the medical literature would suggest but that
It is not very uncommon for a patient with a tender stump to mention that he also feels pain in the absent hand or foot only after he has been under one’s care for a considerable time and after he has learnt that his complaints will not be scoffed at4
Although brief, this text by Donaldson Craig demonstrates the relationship between doctor and patient, the potential stigma for chronic pain patients, particularly those with phantom limb pain, and raises the possibility that although there may be no apparent physical aetiological explanation for a patient's chronic pain, this does not mean that it is any less “real” or distressing to the patient:
The persistent symptoms experienced by such patients are very real indeed, despite the frequent paucity of demonstrable abnormality in the stump, and they may lead to complete breakdown of physical and emotional stability, as in one unfortunate case in my experience25
In his 1921 report on the value of “war knowledge” in teaching and clinical practice, Consulting Surgeon to Roehampton, EM Corner, noted this connection between poor mental health and the presence of untreated chronic pain, and the importance of valuing patient testimony. He wrote of a case with severe neuropathic pain caused by neuroma, improved to a certain degree by excision, although he recovered “slowly because of his convictions that he would not get better. He did not become well enough to work; his nervous system has never recovered. He is useless and miserable.”22 Despite a seemingly judgemental tone in this account, Corner appears to have been sympathetic to these patients, noting:
Over such people there must be no differences of opinion. Almost all are neurasthenic, but at the bottom of the neurasthenia is a real cause, however much it may be exaggerated by the patient. It is the duty of those in charge to find that cause, to advise the Ministry of Pensions of it, and not to follow the easy path of regarding all complaints as due to the action of the central or psychological factor22
As with many lessons from the Roehampton surgeons, it is difficult to analyse the extent to which this advice was adopted into clinical practice.
4.2. Treatment
In scrutinising the reports of interventions and their efficacy, it must be borne in mind that much of the search predates the introduction of controlled clinical trials and modern standards of clinical evidence. In terms of the therapeutic interventions reported, surgical interventions were the most frequently reported treatment for postamputation pain both during the war and in every subsequent decade until 1960, demonstrating the dominance of surgeons in rehabilitation at this point, despite government advice warning against surgical intervention (Fig. 5).53 During the years 1914 to 1918, trends in treatment mirrored the conversation around nociceptive aetiology for chronic postamputation pain with excision and nerve shortening the most commonly reported treatments for stump pain. Surgeons were advised to “freely excise” any nerve damage or neuroma, particularly in patients who were to be fitted with a prosthesis because “painful nerve-ends are not always evident to the patient until pain, which may be intolerable, is elicited by the pressure on the bucket” and thus “they should be sought for by the surgeon and removed before the artificial limb is fitted.”7
Figure 5.
Interventions for postamputation pain in retrieved texts by decade.
The results reveal that as growing numbers of amputee veterans presented with chronic pain in the following decades, increasingly invasive surgical interventions for chronic postamputation pain were reported, with once “last-resort” treatments advocated in journals as potential procedures for standard practice (Table 6).48 From 1920, neurosurgical procedures, including rhizotomy, cordotomy, and sympathectomy, were described as potential treatments for stump and phantom limb pain, all of which appear to be advocated by individuals, rather than more widely by professional journals or associations.4,62,67 None of these descriptions of more aggressive invasive techniques were reported as successful or had replicable outcomes. Reasons for failure were given as inadequate technique (“if sympathectomy did not relieve causalgia it was because the operation had not been adequate”), or even the patients themselves, as was the case for Thorburn's rhizotomy, which had a 33% failure rate and a 6% mortality rate, which he believed to be due to the patients as “the results of the operation are much confused by the highly neurotic condition of the patient … many of these are accustomed to large doses of morphine, of alcohol and of other drugs, and when in hospital they feel acutely the absence of such drugs.”41,67 There are very few references to veterans self-medicating with drugs or alcohol within both the reports of this review and the National Archives' medical pension files, suggesting that perhaps, this was not as widespread an issue as Thorburn implied.24
In contrast to the invasive and potentially harmful surgical procedures, the literature also shows the emergence of physical therapies for stump and phantom limb pain and those that could be applied to the surface of the skin, referred to in this review as “topical.” These include short-lived treatments such as counterirritation or diathermy and those which may be recognisable to today's clinicians including wax baths.8,32,47 These noninvasive methods were often combined, and 4 articles reported patients being treated by a combination of heat, electricity, and physical therapy for the years 1915 to 1921 alone.9,11,22,23,36 Physical therapy also offered the additional benefit as an employment opportunity for other wounded veterans: in 1916, the first graduates of the St Dunstan's hospital for blinded veterans joined the Massage Corps and were able to treat 20 wounded veterans daily.50
The review revealed that concepts of multidisciplinary or interdisciplinary treatment for pain developed earlier than initially believed. Previous research in this project suggested that interdisciplinary treatment for chronic postamputation pain was first reported at the Queen Mary's Hospital at Roehampton, the United Kingdom's leading limb-fitting centre.54 By 1918, more than 26,000 patients had been treated at the Queen Mary's (two-thirds of all amputee veterans), and the hospital remained responsible for the majority of these patients, with almost 11,000 veterans still receiving treatment or prosthetic limbs in the years 1938 to 1939, and the hospital itself becoming dominant in the field of rehabilitation.19,69 In the 1950s, Queen Mary's introduced “Stump Panels,” where clinicians from varying disciplines met to review complex cases: one of the convoluted treatment pathways recommended by these panels is evident in the archive files from 1956, in which a veteran with chronic stump and phantom pain was recommended various pharmaceuticals, percussion therapy, psychiatric treatment, a prostatectomy, and neurosurgery in just a two-week inpatient stay.6,24,54 These panels were believed to be one of the first examples of multidisciplinary collaboration for the treatment and rehabilitation of amputees. However, articles retrieved by this search demonstrate the importance of organised cooperation between specialities in 1918 during the First World War as a British Medical Journal article noted:
Teamwork at the front means work by associated individuals whose exact functions are so practised and defined as to accomplish a maximum of efficient work in a minimum time … there is urgent need for the closest cooperation between the physiologist, the neurologist, the psychologist, the pathologist, the surgeon, the directors of the physical, electrical and massage departments, and for nursing at its most intelligent level18
Reports of pharmacological interventions were sparse. There were just 4 reports of pharmacological interventions reporting positive outcomes across the entire period covered by the review. Morphine was the most common drug to be referenced specifically, whilst opioids as a whole had the greatest patient total. However, neither appeared to be successful in treating chronic postamputation pain: there were no positive outcomes associated with either.10,14,66 Before 1950, one study in which a First World War veteran received pharmacological analgesia for chronic pain was retrieved by the search terms: this gunshot wound patient complained of regular attacks of stump pain and jactitation (“jerking of the amputation stump … coinciding with lancinating neuralgic stump pains”28) lasting several hours and was treated with hypodermic morphine, Omnopon (a combination of morphine, papaverine, codeine, and noscapine), aprobarbital (Allonal), a bromide (Sedobrol), and phenobarbital (Luminal).66 Although hypodermic injection of morphine and Omnopon did relieve pain, the side effects were thought too severe for the patient and Allonal, Sedobrol, and Luminal were reported to have no effect.
Concerns over addiction and the suitability of opioids for treating intractable or long-term pain are far from new issues and were discussed in the medical press from the late 1940s. In 1946 The Lancet reported that no form of analgesia was ideal for chronic pain: whilst general and local anaesthetics “dispel all non-specifically by abolishing all forms of sensation,” newer drugs such as pethidine (Demerol) could be more targeted, although “they carry the grave risk of addiction”.44 The increasing interest in finding a pharmaceutical solution for the treatment of chronic pain can be seen by the fact that the second plenary session of the British Medical Association's Annual Meeting in 1952 was dedicated to “the relief of pain” and attended by “some 500 members.”15 In a speech that could equally have been written 60 years later, the plenary highlighted,
The ideal means of relieving chronic pain has not yet been achieved. A drug that will supress pain without affecting consciousness or muscular power and without producing the euphoria that leads to addiction awaits discovery39
4.3. Assessment of treatment outcomes
One of the initial aims of this project had been to document the terminology used across the reporting period to describe and measure the effect of postamputation pain. However, it is difficult to interpret how successful treatments in the retrieved texts were in reducing or abolishing chronic postamputation pain or the original authors' criteria for a “successful” treatment. Although 35 (35%) of the retrieved texts reported treatment outcomes, there was no consistency across reports with little standardised language and none of the standard reporting structures used in medical journals today. Negative outcomes were considered by the authors to be all those reporting an increase or no change in pain levels after an intervention.
Although there was no standardised measure for success across all texts, the most common approach appears to have been measuring changes in pain levels against the complete abolishment of pain or the full return of function and sensation; anything less than this result was considered to be a negative outcome. There appears to be no equivalent for cases with positive results, and measurable outcomes are replaced with empty rhetoric: positive results were reported with descriptions such as “marked improvement,” “appreciable results,” “completely cured,” or to have delivered “advantages hardly to be exaggerated.”30,31,58 Just one article included patient-reported outcomes with a direct quote from the patient, and only 14 (14%) included an explanation of treatment aetiology in relation to the mechanistic descriptors of pain.
This makes it difficult to interpret how successful treatments were in reducing or abolishing chronic postamputation pain or to know the authors' criteria for a “successful” treatment. Where clear statistics regarding improvement in function are included within the retrieved texts, they relate to return to active service and the savings to the state in disability pensions and medical treatment. One study reported that 51% of their cases were “completely cured,” with 452 men returned to active service in a single month, saving the state £80,000 in pensions.30 Once again, when treatment was considered to have been unsuccessful, the blame was often placed on the patient: one study reported that 20% of cases were discharged as permanently unfit, “many of these were untreatable from the first.”49 What is clear is the importance of and need for clear aims, standardised measurement, and reporting of pain intensity and impact in published studies if this information is to be of use in future reviews.
4.4. Cycles of learning
The retrieved articles demonstrate an awareness of the need to learn from past conflicts and of consolidating and utilising experiences of the First World War when shaping clinical policy for the Second World War, in which the consulting surgeons of Queen Mary's took a principal role. The results of the review show that several of the hospital's limb-fitting surgeons lectured on lessons learned from their war experience at meetings of professional organisations such as the Royal Society of Medicine and the British Medical Association throughout the 1930s as long-term issues associated with amputation were becoming more evident. Of the 100 speakers directly named in the published conference summaries, 66% appear in the years 1914 to 1919, with 7 individual clinicians who appeared in the texts more than once. Forty-three (43%) of these were consulting surgeons at Queen Mary's.
The lessons that were learnt from war experiences at Roehampton and shared amongst the medical professionals can be seen most clearly in the discussion around nerve-shortening surgery. At the end of the war, the literature advised that nerves should be cut short at the primary amputation, with 1 to 2 inches pulled down and removed, preferably with scissors.58 However, by 1930, the British Medical Journal published recommendations that cutting nerves led to greater postoperative pain, and, to treat stump pain and prevent neuroma, nerves should instead be injected with absolute alcohol and crushed. This was despite findings that this procedure was rarely successful and “the pain recurs above the old level of interruption.”47 From 1938, the Roehampton surgeons were actively advocating against these procedures in both The Lancet and the British Medical Journal, with warnings that nerves should not be cut short “as we once did,” they may then be subject to pressure from the artificial limb's socket, whereas they would have been “unhurt” if left long in the stump.66 It appears that despite the influence of the surgeons and the circulation of the 2 journals, their warnings went unheeded because this idea was repeated throughout the next decade.53
The cyclical nature of recommendations is not unique to nerve shortening. A process, whereby a treatment or test is introduced, discussed, and recommended within the medical literature, discovered to have unexpected consequences or potentially cause harm to patients is discarded and forgotten, and then, rediscovered after a period of around 20 years; this pattern can be seen repeatedly in the results of this review. Similar patterns can be seen across treatment and diagnostics, including recommendations for sympathectomies, cordotomies, and the “period of signs … many of them eponymously named, by which one could infallibly diagnose any nerve injury.”43 Articles within both journals show an awareness of these cycles, although no solutions, with The Lancet noting that newly qualified surgeons were forced to “unlearn” their anatomy textbooks “when the symptoms do not agree with his preconceived notions of the necessary motor and sensory loss … we passed through that phase during the last war …. We have seen the same phase during this war but its duration seems to have been mercifully shorter.”43
4.5. Future work
Results of this review will be used in conjunction with other archive sources as part of a wider patient-centred research project to investigate chronic postamputation pain and subsequent physical health conditions in First World War veterans and the possible benefits of this data set to the amputee veterans of the recent Iraq and Afghanistan conflicts. A study of the prevalence and clinical management of chronic postamputation pain in the First World War cohort and the likelihood of these veterans developing subsequent physical health conditions has recently been published by this project team in the Journal of Veteran, Military and Family Health.24 To date, it has centred on the medical pension records held within the British archives but has the potential for expansion into similar national archives held in Canada, Australia, New Zealand, and Germany.
Although systematic reviews are rarely used with historical material and are not a standard research method within the history as a discipline, it was felt by all authors that this was the most effective approach to search and analyse a large collection of texts over 7 decades of publications. Presenting the results of this research as a narrative based on a systematic search has allowed us to bridge historical and clinical approaches to research and incorporate data from individual studies with a strategic overview across almost a century, permitting the investigation of both the “what” and the “how” of professional medical conversation over this period. Combining these approaches demonstrates one of the advantages of true interdisciplinary work in that it has allowed a more in-depth analysis than would be possible alone and illustrates the potential value of systematic searches and reviews within the humanities and the discipline of history in particular.
4.6. Limitations
One limitation of this study is that the screening and extraction were performed by one author (S.D.S.). Ideally, this would have been performed by 2 authors, but any errors were minimised as the Covidence platform ensured that both title and full-text screening were performed to the same publications twice, and any uncertainties or conflicts between rounds of screening were referred to the senior author (A.S.C.R.).
One of the original aims of the review was to investigate the assessment of disability caused by pain by medical professionals and, if possible, establish the point at which chronic pain was recognised as a potential contributor to disability. However, the review included just 6 reports in which disability was discussed, usually in the context of calculations to the cost to the state of injured veterans and the savings that could be achieved through suitable treatment and rehabilitation. Other approaches were being used to investigate this issue, including analyses of the Ministry of Pensions' administration files.24
A further and the potentially most significant limitation is the lack of standardised language, taxonomy, agreed definitions, and disease classification across the retrieved texts. The population for this review was a clearly defined and large cohort undergoing medical treatment across a multitude of specialties for almost a century, a research opportunity that is unlikely to occur again. A lack of consistent measurement or presentation of results within these studies increases the difficulty in combining the results of multiple small studies to a coherent overview, thus reducing their potential value to future research and squandering a unique opportunity.
5. Conclusion and implications for current practice
The aims of this review were to investigate the evolution of the professional medical conversation around chronic postamputation pain in First World War veterans. The search strategy retrieved 101 relevant texts for the period 1914 to 1985, which described 43 separate types of treatment. The use of multidisciplinary treatment as early as 1916 was an unexpected finding because the previous literature had suggested that this was not standard practice until the 1950s. Further unexpected findings were that contemporary topics of discussion such as concerns over the addictive nature of pain medication and the effect of untreated chronic pain on patients' mental health have been published in medical journals since the early 20th century.
This review offers important learning points for current practice and highlights some areas of research that have changed little over the past century: in particular, the importance of fully utilising research opportunities to conduct organised studies, with clearly recorded objectives and results, consistent reporting and outcome measures, and agreed definitions of both conditions studied and criteria for success. Opportunities to learn from past conflicts are often overlooked, potentially harming patients, and treatments still occur in roughly twenty-year cycle: for example, the recent discussion around nerve shortening in amputations by military surgeons.54 If current studies are to be of use to future reviews, authors must ensure that clearly established aims, reporting methods, and standardised language are included within their published work. The articles in this review demonstrate that consistent terminology is not self-generating over time, even after several decades, and will not occur without a concerted effort and agreement from both authors and publications.
Perhaps, the most important lesson to take from this review is that institutional memory is short, opportunities to learn from experience are lost, and the importance of skill sharing and retention amongst military and civilian staff in postconflict and interconflict practice is often undervalued. Although multiple texts discussed the importance of learning from prior conflicts and the experience of the Queen Mary Hospital surgeons dominated the conversation from the late 1930s onwards, it appears that this information was not adapted into practice by the wider medical profession: treatments and aetiologies continued to appear in twenty-year cycles with little improvement in outcomes or even mortality rates. The results of this review also demonstrate the physical, mental, and financial cost to both the patient and the state of poor postoperative treatment of amputees and poorly integrated rehabilitation, all of which is preventable with specialist pain management, good clinician–patient relationship, and well-planned multidisciplinary care. These may be especially useful lessons now, almost a decade after the end of Op HERRICK (the codename for British operations in Afghanistan [2002–2014]) when long-term care for these veterans is estimated to cost £288 million over the next 40 years, and the point at which both interest in and funding for this area of work has begun to decrease.2,27
Although the number of military personnel undergoing limb amputation as a consequence of combat trauma has never subsequently reached that of the First World War, chronic postamputation pain is still a significant issue for the military in the rehabilitation of conflict wounds.3 Similarities in injury patterns of the First World War and the most recent Iraq and Afghanistan conflicts mean that this project is potentially of relevance to today's clinicians, researchers, and policy makers as the long-term effect of the conflict wounds sustained by the United Kingdom's military personnel becomes more evident.
Disclosures
The authors have no conflict of interest to declare.
Appendix A. Supplemental digital content
A supplemental appendix is available at http://links.lww.com/PR9/A204.
Supplementary Material
Acknowledgements
The study was funded by The Royal British Legion through the Centre for Blast Injury Studies at the Imperial College London.65 The authors gratefully acknowledge the expert advice of Dr Emily Mayhew.
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painrpts.com).
References
- [1].Aldington D, Small C, Edwards D, Ralph J, Woods P, Jagdish S, Moore RA. A survey of post-amputation pain in serving military personnel. J R Army Med Corps 2014;160:39–41. [DOI] [PubMed] [Google Scholar]
- [2].Armed Services Trauma Rehabilitation Outcome Study. Available at: https://www.advancestudydmrc.org.uk. Accessed June 31, 2020.
- [3].Bennett AN, Dyball DM, Boos J, Fear NT, Schofield S, Bull AMJ, Cullinan P. Study protocol for a prospective, longitudinal cohort study investigating the medical and psychosocial outcomes of UK combat casualties from the Afghanistan war: the ADVANCE Study 2020. BMJ Open 2020;10:e037850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bingham JAW. Pain in phantom limbs. Br Med J 1948;2:51–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Bourke J. Dismembering the male: men's bodies, Britain and the great war. London: Reaktion Books, 1996. [Google Scholar]
- [6].Bourke J. Phantom Suffering: amputees, stump pain and phantom sensations in modern Britain. In: Boddice R, editor. Pain and emotion in modern history. London: Palgrave Macmillan, 2014. p. 66–89. [Google Scholar]
- [7].British Medical Journal. Amputations and amputation stumps. Br Med J 1916;1:534–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].British Medical Journal. An epitome of current medical literature: electrical treatment of nerve injuries. Br Med J 1915;2:33–6. [Google Scholar]
- [9].British Medical Journal. An epitome of current medical literature: local treatment of nerve lesions. Br Med J 1916;2:1–4.20768190 [Google Scholar]
- [10].British Medical Journal. An epitome of current medical literature: operation for neuralgia of the third cervical nerve from gunshot injury. Br Med J 1917;1:5–8. [Google Scholar]
- [11].British Medical Journal. Lesions of peripheral nerves resulting from war injuries: pathology and treatment. Br Med J 1918;1:379–82.20768987 [Google Scholar]
- [12].British Medical Journal. Pain in phantom limbs. Br Med J 1949;1:1132. [Google Scholar]
- [13].British Medical Journal. Reports of societies: discussion on gunshot wounds on peripheral nerves. Br Med J 1915;2:643–4. [Google Scholar]
- [14].British Medical Journal. Reports of societies: nerve injuries. Br Med J 1918;1:287–8. [Google Scholar]
- [15].British Medical Journal. Second plenary session: the relief of pain. Br Med J 1952;2:146–8. [Google Scholar]
- [16].British Medical Journal. The management of intractable pain. Br Med J 1949;2:430.20787628 [Google Scholar]
- [17].British Medical Journal. The phantom limb. Br Med J 1948;2:262. [Google Scholar]
- [18].British Medical Journal. War injuries of peripheral nerves. Br Med J 1918;2:551–2. [Google Scholar]
- [19].Buxton JD. Roehampton 1915-1965. Br Med J 1965;2:1238–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Carden-Coyne A. The politics of wounds: military patients and medical power in the First World War. Oxford: Oxford University Press, 2012. [Google Scholar]
- [21].Corner EM. Abstract of the Harbeian lecture on nerves in amputation stumps. Br Med J 1919;1:638. [Google Scholar]
- [22].Corner EM. Amputations: the effect of war knowledge on teaching, practice and after-care. Lancet 1921;197:114–5. [Google Scholar]
- [23].Corner EM. War scars and their pains: with special reference to painful amputation stumps. Br Med J 1918;1:665–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Dixon Smith S, Henson D, Hay G, Rice ASC. Chronic post-amputation pain and blast injury: an analysis of British First World War veterans' pensions records. J Mil Veteran Fam Health 2021;7:64–73. [Google Scholar]
- [25].Donaldson Craig J. Pain in phantom limbs. Br Med J 1948;1:904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Edwards DS, Mayhew E, Rice ASC. “Doomed to go in company with miserable pain”: surgical recognition and treatment of amputation-related pain on the Western Front during World War One. Lancet 2014;384:1715–7. [DOI] [PubMed] [Google Scholar]
- [27].Edwards DS, Phillip RD, Bosanquet N, Bull AM, Clasper JC. What is the magnitude and long-term economic cost of care of the British Military Afghanistan amputee cohort? Clin Orthop Relat Res 2015;9:2848–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Fahn S, Jankovic J, Hallett M, Jenner P. ‘Restless legs syndrome and peripheral movement disorders’ in principles and practice of movement disorders. London: Churchill Livingstone, 2007. [Google Scholar]
- [29].Finnerup NB, Haroutounian S, Kamerman P, Baron R, Bennett DLH, Bouhassira D, Cruccu G, Freeman R, Hansson P, Nurmikko T, Raja SN, Rice ASC, Serra J, Smith BH, Treede R-D, Jensen TS. Neuropathic pain: an updated grading system for research and clinical practice. PAIN 2016;157:1599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Fox F, Campbell JM. A new combined physical treatment for wounded and disabled soldiers (heat, massage, electricity, movements). Lancet 1916;187:311–2. [Google Scholar]
- [31].Grace JJ. A note on the electrical treatment of disabilities due to wounds. Br Med J 1915;2:812–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Hill L. An economical design of the melted paraffin wax bath. Br Med J 1934;2:171. [Google Scholar]
- [33].International Association for the Study of Pain. Available at: https://www.iasp-pain.org. Accessed December 21, 2021.
- [34].International Association for the Study of Pain. Terminology, 2017. Available at: https://www.iasp-pain.org/resources/terminology/#neuropathic-pain. Accessed December 21, 2021. [Google Scholar]
- [35].Jensen TS, Baron R, Haanpää M, Kalso E, Loeser JD, Rice ASC, Treede R-D. A new definition of neuropathic pain. PAIN 2011;152:2204–5. [DOI] [PubMed] [Google Scholar]
- [36].Jocelyn Swan RH. Gunshot injuries to peripheral nerves. Lancet 1915;186:1081–3. [Google Scholar]
- [37].Ketz A. The experience of phantom limb pain in patients with combat-related traumatic amputations. Arch Phys Med Rehabil 2008;89:1127–32. [DOI] [PubMed] [Google Scholar]
- [38].Kooijman CM, Dijkstra PU, Geertzen JHB, Elzinga A, van der Schans CP. Phantom pain and phantom sensations in upper limb amputees: an epidemiological study. PAIN 2000;87:33–41. [DOI] [PubMed] [Google Scholar]
- [39].Lancet. British medical association: plenary sessions: the relief of pain. Lancet 1952;260:129. [Google Scholar]
- [40].Lancet. How to tackle nerve injuries. Lancet 1920;196:512. [Google Scholar]
- [41].Lancet. Joint meeting of orthopaedic associations: sympathectomy for causalgia. Lancet 1952;260:80–6. [PubMed] [Google Scholar]
- [42].Lancet. Medical society of London: re-education of the amputated. Lancet 1920;195:768–70. [Google Scholar]
- [43].Lancet. Quick diagnosis of peripheral nerve injuries. Lancet 1944;244:83. [Google Scholar]
- [44].Lancet. Surgical treatment of pain. Lancet 1946;248:16. [Google Scholar]
- [45].Lancet. The work of a pain clinic. Lancet 1982;319:486–7. [PubMed] [Google Scholar]
- [46].Latham PW. On causalgia and allied changes in the joints. Lancet 1918;191:780–1. [Google Scholar]
- [47].Learmonth JR. The surgeon and pain. Br Med J 1935;1:47–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Macpherson WG, Bowlby AA, Wallace C, English C. Medical services of the war. Vol. 2. London: His Majesty’s Stationery Office, 1922. [Google Scholar]
- [49].McKenzie T. The treatment of convalescent soldiers by physical means. Br Med J 1916;2:215–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Ministry of Defence. Official statistics Afghanistan and Iraq amputation statistics: 1 April 2015 to 31 March 2020. London: Ministry of Defence, 2020. Available at: https://www.gov.uk/government/statistics/uk-service-personnel-amputations-financial-year-20192020/afghanistan-and-iraq-amputation-statistics-1-april-2015-to-31-march-2020. Accessed December 21, 2021. [Google Scholar]
- [51].Ministry of Defence. Veterans: key facts. London: Ministry of Defence, 2017. Available at: https://www.armedforcescovenant.gov.uk/wp-content/uploads/2016/02/Veterans-Key-Facts.pdf. Accessed December 21, 2021. [Google Scholar]
- [52].Ministry of pensions and successors: selected First World War pensions award files, Lt Francis Hopkinson. PIN 26/21799. The National Archives Kew, United Kingdom. [Google Scholar]
- [53].Ministry of Pensions. Artificial limbs and their relation to amputations. London: His Majesty’s Stationery Office, 1939. [Google Scholar]
- [54].Noblet T, Lineham B, Wiper J, Harwood P. Amputation in trauma—how to achieve a good result from lower extremity amputation irrespective of the level. Curr Trauma Rep 2019;5:69–78. [Google Scholar]
- [55].Penn-Barwell JG, Roberts SAG, Midwinter MJ, Bishop JRB. Improved survival in UK combat casualties from Iraq and Afghanistan: 2003-2012. J Acute Trauma Care Surg 2015;78:1014–20. [DOI] [PubMed] [Google Scholar]
- [56].Roocroft NT, Mayhew E, Parkes M, Frankland AW, Gill GV, Bouhassira D, Rice ASC. Flight Lieutenant peach's observations on burning feet syndrome in far Eastern prisoners of war 1942-45. QJM 2017;110:131–9. [DOI] [PubMed] [Google Scholar]
- [57].Scholz J, Finnerup NB, Attal N, Aziz Q, Baron R, Bennett MI, Benoliel R, Choen M, Cruccu G, Davis KD, Evers S, First M, GiamberardinoHansson MAP, Kaasa S, Korwidi B, Kosek E, Lavand’homme P, Nicholas M, Nurmikko T, Perrot S, Raja SJ, Rice ASC, Rowbotham MC, Schug S, Simpson DM, Smith BH, Svensson P, Vlaeyen JWS, Wang SJ, Barke A, Rief W, Treede R-D; Classification Committee of the Neuropathic Pain Special Interest Group (NeuPSIG). The IASP classification of chronic pain for ICD-11: chronic neuropathic pain. PAIN 2019;160:53–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Sheild MA. Treatment of the main nerves in amputation. Lancet 1916;188:342–3. [Google Scholar]
- [59].Sliosberg A. Pain in phantom limbs. Br Med J 1948;1:1108–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Smith BH, Torrance N, Bennett MI, Lee AJ. Health and quality of life associated with chronic pain of predominately neuropathic origin in the community. Clin J Pain 2007;23:143–9. [DOI] [PubMed] [Google Scholar]
- [61].Stewart CPU, Jain AS. An epidemiological study of war amputees and the cost to society. J Int Soc Prosthetics Orthotics 1999;23:102–6. [DOI] [PubMed] [Google Scholar]
- [62].The Royal British Legion Centre for blast injury studies, Imperial College London. Available at: https://www.imperial.ac.uk/blast-injury. Accessed June 30, 2020. [Google Scholar]
- [63].Thomson ROC. Queries and answers: muscular spasms in stump after amputation. Br Med J 1930;1:1031. [Google Scholar]
- [64].Thorburn W. Remarks on posterior rhizotomy for the relief of pain. Br Med J 1921;1:629–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, Giamberardino MA, Kaasa S, Korwisi B, Kosek E, Lavand’homme P, Nicholas M, Perrot S, Scholz J, Chug S, Smith BH, Svensson P, Vlaeyen JWS, Wang S-J. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International Classification of Diseases: (ICD-11). PAIN 2019;160:19–27. [DOI] [PubMed] [Google Scholar]
- [66].Verrall PJ. Adapting the limb to the stump. Lancet 1938;232:1489. [Google Scholar]
- [67].Weedon B, Alper H. A history of Queen Mary's University Hospital Roehampton. London: Richmond, Twickenham, and Roehampton Healthcare NHS Trust, 1996. [Google Scholar]
- [68].World Health Organisation. International statistical classification of diseases and related health problems (ICD-11). Available at: https://www.who.int/standards/classifications/classification-of-diseases/. Accessed July 2, 2020. [Google Scholar]
- [69].World Health Organisation. Metrics: disability-adjusted life year (DALY). Available at: https://www.who.int/healthinfo/global_burden_disease/letrics_daly/en/. Accessed July 1, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A supplemental appendix is available at http://links.lww.com/PR9/A204.