Abstract
Gangliosides are sialylated glycolipids, mainly present at the cell surface membrane, involved in a variety of cellular signaling events. During malignant transformation, the composition of these glycosphingolipids is altered, leading to structural and functional changes, which are often negatively correlated to patient survival. Cancer cells have the ability to shed gangliosides into the tumor microenvironment, where they have a strong impact on anti-tumor immunity and promote tumor progression. Since most ganglioside species show prominent immunosuppressive activities, they might be considered checkpoint molecules released to counteract ongoing immunosurveillance. In this review, we highlight the current state-of-the-art on the ganglioside-mediated immunomodulation, specified for the different immune cells and individual gangliosides. In addition, we address the dual role that certain gangliosides play in the tumor microenvironment. Even though some ganglioside species have been more extensively studied than others, they are proven to contribute to the defense mechanisms of the tumor and should be regarded as promising therapeutic targets for inclusion in future immunotherapy regimens.
Keywords: Gangliosides, Shedding, Tumor immunity, Glycosylation
Introduction
Glycosylation is the most abundant covalent modification that proteins and lipids undergo in living organisms [1]. Glycosylation occurs post-translationally in case of proteins, and post-synthesis for lipids and is highly diverse, in terms of glycan structures, and also varies with cell type, cellular activation, and during disease. Also, malignant transformation leads to an aberrant glycosylation profile [2]. One of the most frequently observed glycosylation changes in cancer is an increased expression of sialic acids, which negatively correlates to disease outcome and patient survival [3]. Sialic acids are terminal nine-carbon sugar residues present on mammalian glycoproteins and glycolipids. Sialylated glycosphingolipids, or gangliosides, are expressed throughout the entire human body, but are most abundant in the brain and nervous system. Due to their location in the outer leaflet of the plasma membrane, gangliosides participate in cell-cell and cell-matrix interactions and are able to modulate signal transduction of receptor tyrosine kinases (RTKs) through their association with lipid rafts. For example, tyrosine phosphorylation of epidermal growth factor receptor is inhibited by a variety of gangliosides [4]. In addition, certain pathogens, including malaria parasite Plasmodium falciparum, employ gangliosides to gain entry into the host cell and initiate infection [5, 6]. Gangliosides are likewise crucial in the protection of host structures against the autologous immune system by protecting host cells and tissues from complement attack and autoimmune responses [5, 7]. Even under healthy conditions, gangliosides are released and taken up by neighboring cells, possibly to coordinate signaling responses across cells and tissues [8].
Altered ganglioside expression has been linked to several pathological processes and is known to promote tumor initiation and progression [9]. Gangliosides are abundantly present in the tumor microenvironment (TME), as they are secreted by tumor cells in the form of micelles, monomers, and membrane vesicles [10]. Their glycan profiles are frequently disturbed during cancer progression and can therefore be used as tumor biomarkers [11]. Already in the 1980s, the shedding of tumor gangliosides was evident, showing a clear immunosuppressive activity in vitro and in vivo [12]. Tumor gangliosides are considered to have tumor-promoting properties and to stimulate tumor progression in vivo [13] by promoting cell motility, angiogenesis, and metastasis [11, 14]. Moreover, gangliosides are key modulators of signaling through tyrosine kinases and suppressors of immune surveillance against the tumor [15]. Therefore, the shedding of gangliosides by tumor cells has been strongly correlated to disease progression and lower survival rates [16]. Nevertheless, some gangliosides show anti-tumorigenic properties and differences in ganglioside function appear to vary between different tumor types [17]. In this review, we summarize the current state-of-the-art on ganglioside-mediated immune modulation in the tumor microenvironment, focusing on the expression and shedding of gangliosides by tumors, as well as their interactions with different immune cell subsets.
Healthy synthesis of gangliosides
Glycosphingolipids are formed through the stepwise addition of sugars by glycosyltransferases, first to ceramide and subsequently to the growing glycan structures, thereby generating a wide range of glycolipids. Gangliosides are a specific class of glycosphingolipids characterized by the addition of one or more sialic acids. Their synthesis starts in the endoplasmic reticulum and the further elongation occurs in the Golgi [18]. Gangliosides are classified into groups according to the number of sialic acid residues attached (mono, di, tri) and the order of migration of the gangliosides on thin layer chromatograms (GM3 > GM2 > GM1). The addition of one sialic acid to the precursor of most gangliosides, lactosylceramide (LacCer), generates GM3 and after addition of other sialic acids also GD3 and GT3. Each of these gangliosides then becomes an acceptor for another N-acetylgalactosamine (GalNAc) residue, generating the GM2, GD2, and GT2 lipids. Once the GalNAc is added, further addition or removal of sialic acid residues no longer occurs, thus committing the gangliosides to the “a-series” (one sialic acid), “b-series” (two sialic acids), or “c-series” (three sialic acids) (Fig. 1) [14]. After completion, the gangliosides are transferred to the outer leaflet of the plasma membrane, via vesicular delivery, where they are positioned facing the extracellular environment. Gangliosides are present in all cells; however, the exact ganglioside expression patterns differ per cell type and are dependent on the expression and intracellular distribution of the specific glycosyltransferases required for their biosynthesis [20].
Fig. 1.
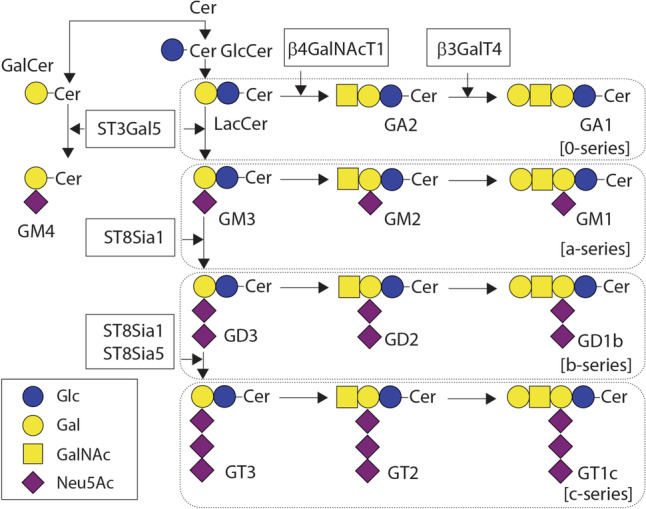
Schematic overview of the ganglioside structure and biosynthesis. Gangliosides are generated from the precursor LacCer or GalCer after addition of sialic acids by different sialyltransferases. Cer, ceramide; Lac, lactosyl; Gal, galactose; Glc, glucose; GalNAc, N-acetylgalactosamine; Neu5Ac, N-acetylneuraminic acid (sialic acid); ST3Gal5, ST3 βgalactoside α-2,3-sialyltransferase 5 (GM3 synthase); ST8Sia1, ST8 α-N-acetyl-neuraminide α-2,8-sialyltransferase 1 (GD3 synthase); ST8Sia5, ST8 α-N-acetyl-neuraminide α-2,8-sialyltransferase 5 (GT3 synthase); β4GalNAcT1, β-1,4-N-acetylgalactosaminyltransferase 1 (GM2/GD2 synthase); β3GalT4, β-1,3-galactosyltransferase 4 (GM1/GA1/GD1 synthase). Adapted from Inokuchi et al. [19]
Shedding and expression of gangliosides in cancer
An altered ganglioside metabolism contributes to pathological conditions, such as cancer, autoimmune disease, and inflammatory disorders, especially if these diseases originate in the neurological system. For example, mutations in GM3 synthase have been identified as the cause of an autosomal recessive infantile-onset epilepsy syndrome [21]. The formation of anti-ganglioside antibodies has been related to Alzheimer’s disease, Parkinson’s disease, and Guillain-Barré syndrome [22–24].
During malignant transformation, the ganglioside repertoire is distinctly changed, due to alterations in the expression levels of glycosyltransferases involved in ganglioside synthesis [11]. These alterations vary from overexpression of certain gangliosides, loss of expression for others, truncated structures, accumulation of precursors, and, very rarely, the appearance of novel structures [14]. Very few gangliosides are truly tumor-specific, as many of these altered gangliosides are also found in healthy cells, albeit at a different expression level [25]. Ganglioside expression in tumor cells even seems to vary according to the tumor stage, as metastatic tumors tend to have a different ganglioside profile compared to primary tumors [26, 27]. Besides that, gangliosides are also shed into the TME in much larger quantities than under healthy conditions (an overview is given in Table 1). Gangliosides can even be detected in the blood circulation of cancer patients, as first detected in the plasma of neuroblastoma patients [28, 29], potentially providing a clinically useful biomarker for diagnosis and/or prognosis of tumor recurrence and progression [30].
Table 1.
Overview of gangliosides expressed and shed by different tumor types
| Cancer type | Gangliosides | Refs |
|---|---|---|
| Tumors of the central nervous system (glioblastoma, neuroblastoma, medulloblastoma, retinoblastoma) | GM3, GM2, GM1, GD3, GD2, GD1a | [9, 25, 30–40] |
| Melanoma | GM3, GD3, GD2, GM1 | [9, 41–44] |
| Breast cancer | GM3, GD3, GD2, GD1a, GD1b, GT1b, GQ1b | [9, 45–47] |
| Lung cancer | GM3, GD3, GM2, GD2, (fucosyl-)GM1 | [16, 48–51] |
| Ovarian cancer | GD3, GD1a | [52, 53] |
| Renal carcinoma | GM3, GM2 | [54, 55] |
| Colorectal cancer | GM3, GM1, GD1a | [56, 57] |
| Leukemias | GM3, GD3 | [58, 59] |
| Pancreatic cancer | GM2 | [60] |
| Hepatocellular carcinoma | GM3, GM2, GD3 | [61–63] |
The expression level of gangliosides in different tissues and tumor types mainly depends on the level of expression of glycosyltransferases involved in their biosynthesis, such as the ST3 β-galactoside α2-3 sialyltransferase 5 (ST3Gal5) which is the enzyme generating monosialylated gangliosides (Fig. 1). ST3Gal5, also named GM3 synthase, is differentially expressed in multiple tumor types compared to adjacent healthy tissue, and associated with beneficial or poor prognosis, depending on the type of tumor. [64–68]. Also, ST8Sia I, which synthesizes disialylated ganglioside species, plays a role in proliferation, invasion and survival of tumor cells in vitro [69–71]. ST8Sia1 is highly expressed in melanoma and breast cancer, and is correlated with increased biosynthesis of the downstream gangliosides and poor clinical outcome [72–74]. Inhibition of GD3 synthase (ST8Sia1) in vivo suppressed tumor growth and angiogenesis by downregulating vascular endothelial growth factor (VEGF) [75]. For additional information on the synthesis and degradation of tumor-associated gangliosides in tumors, we refer the reader to Groux-Degroote et al. [16].
The role that gangliosides play in the tumor context is quite diverse as several gangliosides promote tumor cell growth, whereas others stimulate angiogenesis and metastasis [66, 76]. These effects may be for a large part due to the ability of gangliosides to modulate RTK signaling [77]. RTKs often bind growth factors, which upon engagement of the receptor stimulate cell survival, proliferation, differentiation, and migration. Gangliosides can directly engage RTKs within glycolipid-enriched microdomains in the plasma membrane [78]. An aberrant ganglioside profile will thus alter the structure of the glycolipid-containing microdomains and the interaction with RTKs, often resulting in receptor dysregulation, favoring tumor progression. In addition, the shed gangliosides have been shown to influence anti-tumor immunity [79]. In the next sections, we will highlight the immune modulatory effects of gangliosides in the TME.
Immunomodulatory properties of gangliosides in the tumor microenvironment
The shedding of gangliosides by tumor cells is mainly suppressive to allow tumor cells to escape immune recognition, although the opposite effect has been observed as well, depending on the type and concentration of individual gangliosides [80]. To date, our knowledge regarding immune modulatory properties of the gangliosides shed by cancer cells is still mainly based on in vitro studies. The impact of gangliosides on individual immune cell subsets will be further specified below. Of note, in most studies, “soluble” gangliosides are added to the cells; therefore, the observed effects are mainly representative of gangliosides shed by tumor cells, likely forming micelles or vesicles, and does not necessarily reflect how tumor-associated gangliosides modulate anti-tumor immunity.
T cells
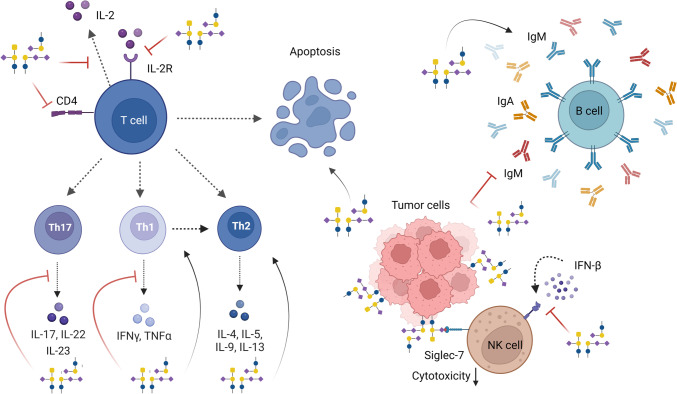
CD8+ cytotoxic T lymphocytes (CTLs) are crucial cells in the anti-tumor immune response, because of their direct cytotoxic action on cancer cells. However, CD4 T helper cells are gaining attention for their direct anti-tumor action as well as their ability to license and sustain CTLs for killing [81]. How gangliosides affect T cell immunity is described below and summarized in Table 2 and Fig. 2.
Table 2.
Ganglioside effects on the immune system
| Ganglioside | Tumorigenic effect | Impact on immune cell/response | References |
|---|---|---|---|
| T cells | |||
| GM3 | Pro-tumor |
Inhibition of T cell proliferation by blocking the interaction of IL-2 with IL-2R Generation of a Th2 bias through induction of IL-10, limiting a Th1 response Down-regulation of CD4 expression on T cells |
[82–84] |
| GM2 | Pro-tumor |
Stimulation of T cell proliferation by enhancing the IL-2 response Generation of a Th2 bias by inhibiting Th1 cytokine production and by inducing IL-4 secretion Induction of T cell apoptosis |
[54, 83, 85, 86] |
| GM1 | Pro-tumor |
Inhibition of T cell proliferation by blocking the interaction of IL-2 with IL-2R Generation of a Th2 bias through induction of IL-10, limiting a Th1 response Induction of T cell apoptosis by inhibiting NF-kB Down-regulation of CD4 expression on T cells |
[83, 86–88] |
| GD3 | Pro-tumor |
Inhibition of T cell proliferation by neutralizing IL-2 Inhibition of T cell activation through TCR arrest Generation of a Th2 bias by inhibiting Th1 cytokine production Suppression of Th17 activity and IL-17A production Induction of (activated) T cell apoptosis by inhibiting NF-kB, stimulating ROS production, and through induction of caspase-3 and -9 |
[82, 86, 89–92] |
| GD2 |
Anti-/pro- tumor (tumor type dependent) |
Stimulation of T cell proliferation by enhancing the IL-2 response Generation of a Th2 bias by inhibiting Th1 cytokine production |
[82, 86] |
| GD1a | Pro-tumor |
Inhibition of T cell proliferation by depleting IL-2 Generation of a Th2 bias by inhibiting Th1 cytokines, through induction of IL-10, and by increasing apoptosis of Th1 cytokine-producing cells Induction of T cell apoptosis by inhibiting NF-kB |
[83–85, 87, 93] |
| GD1b | Anti-/pro-tumor (tumor type dependent) |
Inhibition of T cell proliferation by depleting IL-2 Generation of a Th1 response by stimulating Th1 cytokine secretion and reducing Th2 cytokines |
[83, 93–96] |
| GT1b | Anti-/pro-tumor (tumor type dependent) |
Inhibition of T cell proliferation by binding and blocking IL-2, and interfering with IL-4 Generation of a Th1 response by stimulating Th1 cytokine secretion and reducing Th2 cytokines |
[94–97] |
| B cells | |||
| GM2 | Pro-tumor | Inhibition of Ig production by inhibiting IL-10 and TNF-α production | [98] |
| GD1a | Anti-tumor | Enhancement of Ig production through increased IL-6 and IL-10 production | [99] |
| GD1b | Pro-tumor | Inhibition of Ig production through reduced IL-6 and IL-10 production | [100] |
| GT1b | Pro-tumor | Inhibition of Ig production through reduced IL-6 and IL-10 production | [101] |
| NK/NKT cells | |||
| GM3 | Pro-tumor/ anti-tumor |
Inhibition of NK cell cytotoxicity (in serum) Cell-associated gangliosides may activate NK cells |
[102, 103] |
| GM2 | Pro-tumor | Inhibition of NK cell cytotoxicity | [102] |
| GM1 | Pro-tumor | Inhibition of interferon responsiveness | [104] |
| GD3 | Pro-tumor/ anti-tumor |
Reduction of NK cell cytotoxicity (in serum) in a Siglec-7 dependent manner Cell-associated gangliosides may activate NK cells Induction of NK cell immunosuppression Prevention of NKT cell activation |
[52, 103, 105–108] |
| Dendritic cells | |||
| GM3 | Pro-tumor |
Diminished expression of costimulatory molecules Reduced production of pro-inflammatory cytokines upon LPS stimulation Impaired ability to stimulate allogenic T cell responses Blunted maturation and migration of LC Increased DC and LC apoptosis |
[41, 109–111] |
| GM2 | Pro-tumor |
Impaired moDC differentiation from monocytes Reduced endocytic capacity Impaired ability to stimulate allogenic T cell responses |
[112] |
| GM1 | Pro-tumor |
Inhibition of TLR signaling Reduced production of pro-inflammatory cytokines Impaired ability to induce (murine) Th1 responses |
[93, 113] |
| GD3 | Pro-tumor |
Diminished expression of costimulatory molecules Reduced production of pro-inflammatory cytokines upon LPS stimulation Impaired ability to stimulate allogenic T cell responses Blunted maturation and migration of LC Increased DC and LC apoptosis |
[41, 109, 111] |
| GD2 | Pro-tumor |
Compromised DC differentiation form murine bone marrow precursor or human CD34+ cells Impaired ability to stimulate allogenic T cell responses |
[114] |
| GD1a | Pro-tumor |
Inhibition of TLR signaling Diminished expression of costimulatory molecules Reduced production of pro-inflammatory cytokines upon LPS stimulation Impaired ability to induce (murine) Th1 responses Impaired ability to stimulate allogenic and TT-specific T cell responses |
[93, 113, 115, 116] |
| Macrophages | |||
| GM3 | Pro-tumor |
Inhibition of Fc receptor expression to reduce phagocytosis of tumor cells Suppression of RNI and NO production Inhibition of IL-1β, IL-6, and TNF-α production stimulating tumor growth |
[117–120] |
| GM2 | Pro-tumor |
Inhibition of Fc receptor expression to reduce phagocytosis of tumor cells Inhibition of TNF-α production stimulating tumor growth |
[117, 120] |
| GM1 | Pro-tumor |
Inhibition of IL-1β production to counteract cytotoxicity to tumor cells Inhibition of TNF-α production stimulating tumor growth Stimulation of an M2 macrophage bias to support angiogenesis and anti-inflammatory conditions |
[117, 120, 121] |
| GD3 | Pro-tumor |
Inhibition of IL-1β production to counteract cytotoxicity to tumor cells Inhibition of TNF-α production stimulating tumor growth |
[117, 120] |
| GD1a | Pro-tumor |
Suppression of RNI and NO production Suppression of pro-inflammatory cytokine production, including TNFα, IL-1α and IL-1β |
[120, 122] |
| Monocytes | |||
| GM3 | Pro-tumor | Inhibition of Fc receptor expression | [117, 123] |
| GM2 | Pro-tumor | Inhibition of Fc receptor expression | [117] |
| GM1 | Pro-tumor |
Decreased TLR signaling Suppression of IL-1 production |
[93, 117] |
| GD3 | Pro-tumor | Suppression of IL-1 production | [117] |
| GD1a | Pro-tumor |
Downregulation of CD80 and CD40 Impaired production of IL-12 and TNFα Decreased TLR signaling |
[93, 124] |
Abbreviations: Th1 T helper cell 1, Th2 T helper cell 2, Th17 T helper cell 17, DC dendritic cell, LC Langerhans cell, IL interleukin, TNF tumor-necrosis factor, NF-kB Nuclear Factor kappa B, ROS reactive oxygen species, NO nitric oxide, RNI reactive nitrogen intermediates, Ig immunoglobulin, IFNγ interferon γ, TLR toll-like receptor, LPS lipopolysaccharide, TT tetanus toxoid
Fig. 2.
Immunomodulatory effects of gangliosides on lymphoid cells. Gangliosides modify T cell function by different pathways, promoting T cell apoptosis and skewing to a Th2 phenotype. They can also suppress the cytotoxicity of NK cells via Siglec-7 binding and by blocking the interaction between IFN-β and its receptor. In the case of B cells, gangliosides can either stimulate or inhibit the secretion of IgA, IgM, and IgG, depending on the type of ganglioside. General ganglioside structures are depicted in the figure. Please refer to the main text and tables for the action of individual gangliosides. Created with Biorender.com
Inhibition of T cell proliferation
Gangliosides can inhibit T cell function in multiple ways to promote tumor progression [79]. Most studies demonstrate that gangliosides can interfere with lymphocyte proliferation by depleting IL-2 in a dose-dependent manner, preventing it from binding to the IL-2 receptor (IL-2R) on the surface of activated T cells [82, 83, 125, 126]. However, there is also evidence that gangliosides can bind to IL-2 directly, thus neutralizing free IL-2 without blocking the interaction between IL-2 and the IL-2R [127]. Nevertheless, the presence and position of the sialic acids on the gangliosides seem to be relevant, as GM3 and GD3 have an inhibitory effect on IL-2, while GM2 and GD2 stimulate T cell proliferation by enhancing the response to IL-2 [82]. Moreover, the ability of gangliosides to induce immunosuppression via the IL-2/IL-2R axis appears to be most effective in low protein conditions, since they are known to interact with various serum components like albumin. Therefore, gangliosides will be more immunosuppressive in the local TME where the overall protein concentration is lower than in an in vitro setting [126]. In addition, GD1b, and to a lesser extent GM2 and GD3, also inhibit T cell proliferation by interfering with IL-4 signaling even though this effect is much weaker compared to IL-2 [94].
Induction of T cell apoptosis
Several studies have demonstrated that depriving proliferating T cells from IL-2 results in T cell apoptosis [128, 129]. In consequence, if gangliosides are able to deplete IL-2, they might indirectly induce T cell death. Moreover, IL-4 is able to trigger apoptosis in an IL-2 dependent manner; thus, a Th2 bias could also result in increased T cell apoptosis [130]. Yet gangliosides are also capable of inducing T cell apoptosis directly.
Even at relatively low concentrations, GM2 is able to induce apoptosis in human T cells in vitro. This T cell death was partially blocked by anti-GM2 antibodies, suggesting that GM2 may not be the only ganglioside or the factor involved [54]. Indeed, glioblastoma cell lines expressing both CD70 as well as elevated levels of both GM2 and GD1a are especially prone promotors of T cell apoptosis [85]. The renal cell carcinoma-derived gangliosides and GD3 can enhance apoptosis of human activated T cells in vitro through inhibition of the NF-kB pathway, resulting in reduced expression of anti-apoptotic genes, but also through an increase in mitochondrial permeability, accumulation of ROS and cytochrome c release [55, 87, 89, 90]. GD3-containing exosomes, isolated from human ovarian tumor ascites, mediated arrest of T cell activation after a short exposure to the ganglioside, but did not result in T cell apoptosis, suggesting that a prolonged exposure to gangliosides is needed to induce T cell death. Also, this GD3-mediated arrest appeared to be dependent on the sialic acid groups, as their enzymatic removal reversed the inhibitory effect [91].
Downregulation of CD4 expression
Another mechanism through which gangliosides modulate T cell functionality is by downregulating the surface expression of CD4. Gangliosides GM3 and GM1 inhibit the expression of CD4 in murine and human T lymphocytes, especially in naive T cells, by changing the molecular orientation of CD4 within the cell membrane, which renders CD4 epitopes inaccessible [88, 131, 132]. After this redistribution, CD4 molecules are endocytosed and degraded, resulting in a persistent low level of CD4 expression on the cell surface [133]. Nevertheless, the internalization of CD4 seems to be reversible, since its expression is restored after removal of gangliosides [131]. CD4 modulation appears to be a general characteristic of gangliosides as both the lipid and the sialylated moieties are key in regulating this change in CD4 redistribution [88]. Nevertheless, downregulation of CD4 in the TME could be a long-lasting effect induced by tumor cells to promote tumor progression.
Switch from Th1 to Th2
While generally Th1-type responses are favorable in anti-tumor immunity, gangliosides shed by tumors strongly induce Th2 skewing through several mechanisms. They can downregulate Th1 responses by initiating apoptosis of IFNγ-producing cells and thereby inducing a type 2 bias [128]. Furthermore, the presence of gangliosides during T cell activation blocks IL-2 and IFNγ gene transcription without inhibiting the production of Th2-associated cytokines in a human and murine setting [86, 134]. This is possible due to the ability of gangliosides to interfere with NF-κB activation, a transcription factor for pro-inflammatory cytokines, such as IFNγ and IL-2 [134]. Interestingly, the ganglioside-mediated enhancement of IL-4 production in vivo was independent of IFNγ, suggesting multiple mechanisms disturbing Th1/Th2 skewing [86]. However, Rayman et al. report that GD1a inhibits IFNγ secretion without affecting secretion of type 2 cytokines after human T cell stimulation in vitro [128]. Besides, gangliosides GD1a and GM3 strongly induce IL-10 secretion in human T cells, which in turn suppress the production of Th1 cytokines [84].
Even though the majority of gangliosides appears responsible for creating a Th2 bias, some gangliosides seem to induce the opposite. Kanda et al. demonstrated that GD1b, and other gangliosides containing even more sialic acids, enhanced the production of IL-2 and IFNγ, while reducing the production of IL-4 and IL-5 in human T cells [95]. This suggests that the ganglioside composition, and specially the sialic acid content, determines whether T cell skewing is towards a Th1 or Th2 type immune response.
Th17 interference
The role of Th17 cells in cancer still remains controversial since they exhibit both pro- and anti-tumorigenic activities. Not much is known about how gangliosides modulate Th17 responses in cancer, but GD3 has been shown to suppress the Th17 activity of benign T cells in cutaneous T cell lymphoma [92].
B cells
Even though T cells are considered to be the most effective immune cells mediating the anti-tumor immune response, there is increasing evidence that B cells play an important role in tumor control. Besides producing antibodies, tumor-infiltrating B cells can present antigens to T cells and secrete a variety of cytokines [135]. However, tumor-infiltrating B cells are also able to promote angiogenesis or secrete immunoregulatory cytokines, including TGFβ and IL-10, that suppress the anti-tumor immune response and its effector cells [136].
Immunoglobulin production
Gangliosides have been shown to modulate immunoglobulin (Ig) secretion of B cells (Table 2; Fig. 2). For example, GM2 can inhibit the production of IgM, IgA and IgG in human B cell lines. This effect was counteracted by the addition of both IL-10 and TNFα, suggesting that GM2 inhibits Ig production through the inhibition of IL-10 and TNF-α secretion [98]. Similarly, GD1b and GT1b also suppress IgM, IgG, and IgA production from human PBMCs by reducing IL-6 and IL-10 release of CD4+ T cells and monocytes, respectively [100, 101]. In contrast, the ganglioside GD1a enhances IgG, IgM, and IgA production of human PBMCs by increasing IL-6 and IL-10 secretion of monocytes [99]. In all these in vitro studies, the effect of gangliosides on Ig production was reversible and did not affect the proliferation nor the viability of the B cells [98–101]. So, gangliosides may be involved in regulating humoral responses, but how they modulate B cells in the TME remains unclear.
NK and NKT cells
Natural killer (NK) cells are important players in the overall immune responses against tumors. Their functions are similar to that of cytotoxic T cells, considering they induce anti-viral and anti-tumor immunity by producing IFNγ, granzyme B, and perforin, resulting in cell lysis. They are able to recognize and eliminate MHC-I deficient cells (missing-self) or through engagement of tumor-specific antibodies with their CD16 Fc receptor, triggering antibody-dependent cell-mediated cytotoxicity (ADCC) [137]. Gangliosides can actively suppress NK cell function, decreasing their cytotoxic response and cytokine production (Table 2; Fig. 2).
Inhibition of NK cell cytotoxicity
GM3 and GM2 gangliosides isolated from human brain tissue were able to inhibit NK cell activity in vitro, in contrast to other gangliosides containing more sialic acids. GM3 and GM2 are present in high concentrations in neuroblastoma and gliomas, supporting the hypothesis that shedding of these gangliosides promotes tumor progression [102]. Also, tumor cells containing GD3 decreased the cytotoxic ability of NK cells in an in vitro model [105]. Interestingly, incubation of lymphoma cells with gangliosides prior to NK cell co-culture, resulted in increased NK cell activity towards tumor cells. This suggests that tumor-bound gangliosides function as target structures recognized by NK cells, while shed gangliosides actually contribute to NK cell inhibition during tumor development [103]. One possible explanation might be the insertion of gangliosides into the plasma lipid bilayer of tumor cells, leading to new binding sites for NK cells, thereby increasing their capacity to kill tumor cells.
One of the mechanisms used by gangliosides to modulate NK cell cytotoxicity could be via the binding of sialic-acid binding immunoglobulin-like lectins (Siglecs). Siglecs are a family of sialic acids receptors expressed on immune cells, most of them containing an immunoreceptor tyrosine-based inhibitory motif (ITIM). Nicoll et al. demonstrated that GD3-expressing cells strongly bind to Siglec-7 on NK cells, thereby downregulating NK cell cytotoxicity [106] (Fig. 2). In another study, blocking Siglec-7 binding with an anti-GD2 antibody also sensitized tumor cells to macrophage-mediated phagocytosis resulting in tumor eradication in vivo [138].
Inhibition of interferon production
Several interferons, including IFN-β, have been shown to enhance the cytotoxic activity of NK cells, and are therefore important in anti-tumor immune responses. The gangliosides GM1, GD1b, and GT1b all inhibit the stimulatory effect of IFN-β on murine NK cells in vitro, by competing with NK cells for their interaction with IFN-β. Likely, the direct binding of gangliosides is responsible for the IFN-β-mediated suppression of NK cell activation [104]. The suppression of IFNs is thus a direct mechanism of action of gangliosides to stimulate tumor progression and enhance immune evasion.
Immunosuppression due to senescence
A recent study revealed that senescent cells modify their glycosphingolipid composition towards a higher ganglioside level, characterized by the overexpression of GD3. This is due to a transcriptional upregulation during senescence of the gene encoding the enzyme ST8Sia1, which is responsible for GD3 synthesis. Increased levels of GD3 lead to an immunosuppressive effect on NK cells in vitro and in vivo by binding to Siglec-7 receptor on NK cells [107].
NKT cells
The effect of gangliosides on NKT cells is poorly studied. However, Wu et al. demonstrated that mice immunized with GD3+ human melanoma cells developed a CD1d-restricted NKT cell response against GD3. The observed response was typical of Th2-like cells (secretion of IL-4, IL-10), although the cells also produced some transient IFNγ [108]. Similarly, GD3 isolated from ovarian cancer-associated ascites also prevented activation and IFNγ production by NKT cells; however, in this study, also, IL-4 secretion was inhibited [52].
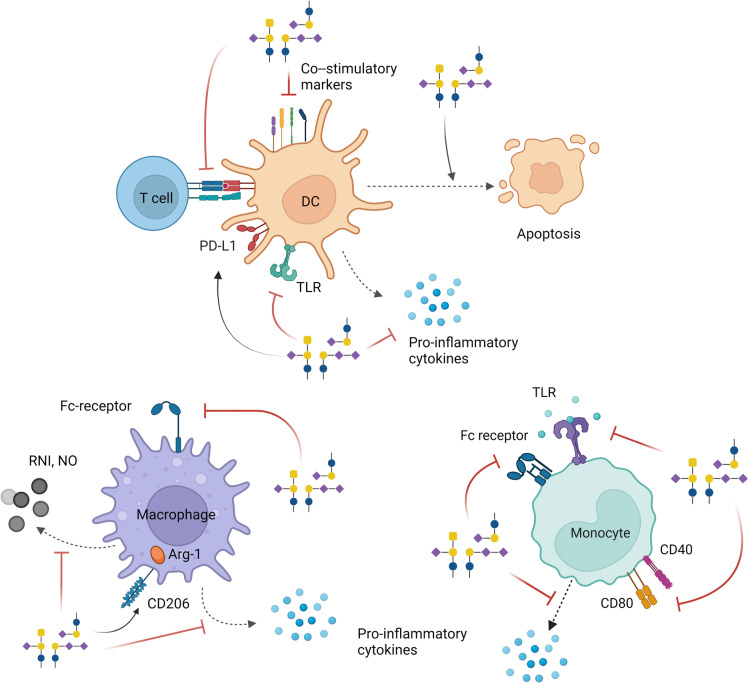
Dendritic cells
Dendritic cells (DCs) are professional antigen-presenting cells, capable of initiating adaptive T cell responses towards pathogens and malignant cells. In addition, DCs play a crucial role in maintaining immunological tolerance, through the selection and depletion of self-reactive T cells. Gangliosides seem to disrupt the whole DC life cycle, ranging from DC development to DC maturation, thus promoting a tolerogenic TME (Table 2; Fig. 3).
Fig. 3.
Immunomodulatory effects of gangliosides on myeloid cells. Gangliosides downregulate the differentiation and maturation of DCs through several mechanisms. They reduce the capacity of DCs to activate T cells and induce DC apoptosis. Gangliosides inhibit the production of pro-inflammatory cytokines by DCs, macrophages, and monocytes. Besides, they can block Fc receptors, TLRs, and co-stimulatory molecules on different myeloid populations. Some gangliosides stimulate the M2-polarization of macrophages by increasing the levels of Arg-1 through CD206, and suppress the production of RNI and NO. General ganglioside structures are depicted in the figure. Please refer to the main text and tables for the action of individual gangliosides. Created with Biorender.com
Impaired DC differentiation
In vivo DCs develop from dedicated precursors; however, under inflammatory conditions, monocytes can also differentiate into so-called monocyte-derived DCs (moDCs). The impact of ganglioside on DC differentiation has not been widely studied; however, early reports indicate that neuroblastoma-derived GD2 impairs DC development from mouse bone marrow and human CD34+ progenitors [114], while GM2, GD3, and GM3 dampen monocyte to DC differentiation, resulting in a DC population with altered morphology, reduced endocytic capacity, as well as a reduced expression of the DC markers CD1a, HLA-DR, and CD80 [41, 112].
Inhibition of TLR activation
Interestingly, in non-small cell lung cancer, a high expression of the ganglioside N-glycolyl-GM3 was associated with a decreased density of mature CD83+ DCs, indicating that gangliosides may blunt DC maturation [48]. Indeed, in several in vitro studies, DC maturation was inhibited in the presence of gangliosides. DC maturation is generally triggered by the engagement and subsequent signaling through pattern recognition receptors, such as the toll-like receptors (TLRs). The gangliosides GM1, GD1a, and GD1b are able to inhibit the activation of multiple TLRs in vitro through the upregulation of the TLR signaling pathway inhibitor, IL-1 receptor–associated kinase M (IRAK-M) [93]. GD1a also reduces TLR-dependent phosphorylation of p38, the key downstream kinase in TLR4 signaling [115], and the subsequent nuclear translocation of NF-κB [116, 124]. This inhibition of TLR activation occurs in a dose-dependent manner and seems to be reversible, with complete recovery of TLR signaling, as assessed by the regained production of pro-inflammatory cytokines, after removal of gangliosides [93]. Interestingly, GD3 is furthermore able to block CD40L-induced maturation [41].
Interference with DC maturation
Gangliosides appear to have the ability to inhibit the LPS-driven and IFNγ boosted DC maturation and cytokine production, and therefore downregulate the pro-inflammatory response triggered against tumor cells.
Gangliosides GM3 and GD3 are modest inhibitors of human DC maturation marker expression in vitro, influencing costimulatory molecules CD40, CD80, CD86, and MHC-II [109]. While GM3 only impaired IL-10 and IL-12 production, GD3 also reduced IL-6 and TNFα secretion after LPS triggering [109]. A similar GM3-mediated downregulation of CD40 and IL-12 was observed in vivo in neuroblastoma bearing mice [110]. In these mice, IL-12 secretion was abrogated in a CD40-dependent manner. GD1a and to a lesser extent GM1 also inhibit the TLR-induced expression of co-stimulatory molecules, such as CD40, CD80, CD83, and CD86 on murine and human DC in vitro [113, 116, 124]. Moreover, GD1a is a potent inhibitor of IL-6, IL-10, IL-12, and TNFα secretion in vitro [113, 116, 124]. Strong pro-inflammatory conditions might counteract the tumor ganglioside-induced phenotype. Yet, IFNγ further amplified the GD1a effects and augmented both IDO1 and PD-L1 expression on the DCs, indicating that IFNγ and GD1a may act in concert to further amplify the tumor immunosuppressive loop [115].
Inability to activate T cells
Exposure of DCs to a wide variety of gangliosides not only impairs TLR-mediated maturation, costimulatory marker expression, and cytokine production, but it also impairs their ability to activate T cells. Treatment of both murine and human DCs with a plethora of gangliosides, including GM3, GD3, GM2, GD2, and GD1a, reduces the DC stimulatory capacity in vitro, resulting in a diminished T cell proliferative response in an allogeneic mixed lymphocyte reaction (MLR) assay [41, 109, 112, 114, 116]. GD1a-preincubated DCs show a similar deficiency in stimulating tetanus toxoid antigen-specific CD4+ T cell responses [124].
In addition, and expected from the aberrant cytokine secretion profiles, gangliosides can derail DC-mediated induction of T helper differentiation. Both GD1a and GM1 compromise Th1 and Th2 differentiation and instead favor the instruction of functional Tregs [113]. Interestingly, this altered Th1 skewing could not be rescued by exogenous IL-12, suggesting that other factors, besides IL-12, contribute to the tapered Th1 differentiation.
Impaired maturation and migration of LC
Langerhans cells (LC) are a type of dendritic cells present in the epidermal layer of the human skin where they act as an immune barrier. Melanoma-derived GM3 and GD3 impair the maturation and migration of human epidermal LCs, which might explain the marked decrease in activated LCs in the lymph nodes close to the tumor [111]. GM3 and GD3 both significantly downregulate expression of costimulatory and maturation markers, which correlated to an impaired ability of the LCs to mount allogeneic T cell proliferation. Also, expression of CCR7 was downregulated, reducing the migration towards CCL19, a chemokine crucial for LC migration to the lymph node.
Induction of DC and LC apoptosis
The gangliosides GM3 and GD3 are also able to induce early apoptosis of DCs and LCs (Fig. 3) [111, 139], which may be attributed to a dysregulated and early DC differentiation and maturation [41]. Interestingly, the GM3- and GD3-induced apoptosis was independent of ganglioside catabolism [139], but did involve activation of caspase-3. Whereas GD3 exposure let to a loss of mitochondrial membrane potential and production of ROS, GM3 exposure did not [139]. Clearly, the mechanisms through which GM3 and GD3 induce caspase-3 activation and apoptosis are different and still not fully elucidated.
Overall, gangliosides seem to foster the development of an immunosuppressive tumor microenvironment, low in fully matured DCs and elevated in Treg numbers.
Macrophages
Macrophages are important players of the innate immune system. They are not a single-cell population with a defined phenotype and function, but depending on the tissue context rather a collection of cell types with a wide range of functional roles in homeostatic and pathological conditions [140]. In the context of cancer, myeloid cells are often seen as double-edged swords, since on the one hand, they have the potential to kill tumor cells, mediate ADCC, and activate lymphoid cells. In contrast, tumor-associated macrophages (TAMs) contribute to cancer progression and angiogenesis as well as to an immunosuppressive TME [141]. The effects of specific gangliosides on macrophages can be found in Table 2 and Fig. 3.
Inhibition of Fc receptor expression
The Fc receptor on macrophages is an important contributor to the immune functions of macrophages [140, 142]. It can bind specifically to antibody-opsonized malignant cells, thereby resulting in phagocytosis of tumor cells [143]. Treatment of human macrophages with GM3 and GM2 gangliosides in vitro inhibited their Fc receptor expression, while other gangliosides did not have this capacity [117].
Suppression of cytokine release
IL-1β is produced by infiltrating myeloid cells, including macrophages, and can promote tumor progression, metastasis, and the generation of an immunosuppressive TME [144]. GM1 and GD3 melanoma-derived gangliosides inhibit IL-1β production by macrophages in vitro [117]. Similarly, GM3 suppresses the secretion of IL-1β and IL-6 in murine RAW 264.7 macrophages [145]. The production of IL-1α and IL-1β was also inhibited by GD1a in LPS-stimulated macrophages [122]. Even though gangliosides might thus be involved in dampening IL-1β release, the underlying mechanisms are still unclear.
TNFα is a pro-inflammatory cytokine that mainly has anti-tumorigenic effects; however, at low levels, this cytokine may also sustain tumor development [146]. Several gangliosides, including GM3 and GD1a, were all effective in reducing TNFα production by murine macrophages in vitro [118, 122]. These gangliosides appear to act at an early step of the signaling transduction cascade as they inhibit MAPK upstream of NF-kB, a key transcription factor for TNFα [118].
Inhibition of RNI production
Reactive nitrogen intermediates (RNI), including nitric oxide (NO), are produced by TAMs and can cause DNA damage and genomic instability, resulting in tumor progression [141]. In contrast, RNI produced by macrophages may also be involved in tumor killing [147]. GM3 and GD1a, amongst other gangliosides shed by tumor cells, appear to inhibit the production of RNI and NO by macrophages in vitro [119, 122, 145]. The mechanism behind this inhibition is still unresolved, but likely involves a direct action of the gangliosides on macrophage function.
Stimulation of M2 macrophage polarization
Macrophages can adopt different functional phenotypes, classically referred to as the pro-inflammatory M1-like macrophages and the anti-inflammatory M2-macrophages, which share similarities with TAMs in the TME. GM1 seems to be a potent stimulator of the polarization towards M2-like macrophages in vitro for both human as well as murine macrophages. It does so by increasing the expression of arginase-1 (Arg-1), a M2-macrophage marker, through the mannose receptor (CD206) and common gamma chain (γc)-mediated activation of JAK3 and STAT6 [121]. In addition, GM1-stimulated macrophages secrete monocyte chemoattractant protein-1 (MCP-1/CCL2) promoting tumor growth and angiogenesis [121].
Monocytes
Monocytes are well known as a precursors of macrophages and moDCs, but they can also act as APCs that are able to prime CD8+ and CD4+ T cells [148]. Similar to other immune cell subsets, gangliosides modulate the proliferation and function of monocytes [149]. For instance, exposing LPS-stimulated monocytes to GD1a downregulates CD40 and CD80, as well as hampers the release of IL-12 and TNFα [120, 124]. Moreover, incubation of monocytes with specific gangliosides impairs Fc receptor expression (GM3 and GM2), reduces IL-1 production (GM1 and GD3), and decreases TLR signaling [93, 117]. Additionally, GM3 suppresses monocyte adhesion to endothelial cells by inhibiting ICAM-1 and VCAM-1 expression on endothelial cells through activation of NF-κB [123] (Table 2; Fig. 3).
Myeloid-derived suppressor cells (MDSCs)
Tumor-infiltrating MDSCs are a heterogeneous population of myeloid cells known to have many immunosuppressive properties, including recruitment of Tregs and inhibition of CD8+ T cell infiltration. To study the role of gangliosides shed by tumor cells, Wondimu et al. used a novel tumor cell created by oncogenic transformation of murine embryonic fibroblasts in which the GM3 and GM2 synthase were knocked-out [150]. This KO rendered the tumor cells completely devoid of gangliosides and resulted in decreased tumor growth in vivo and less infiltration of MDSCs in the TME. The exact mechanism on how gangliosides enhance MDSC remains unclear; however, it might be due to altered chemokine release. In addition, gangliosides can induce the production of iNOS and Arg-1, which are crucial factors for the MDSC-induced immunosuppression [150].
Discussion and outlook
Gangliosides play crucial roles in the context of tumor immunity. During malignancy, changes occur in the glycosphingolipid composition present on the surface of tumor cells, which aid in tumor progression through inhibition of the immune system [11]. Cancer cells have the ability to shed gangliosides into the surrounding environment or to present them as tumor-associated antigens influencing a wide range of immune cells, including T lymphocytes, B cells, NK cells, DCs, macrophages, and monocytes. Gangliosides can suppress the activation, proliferation, and cytotoxicity of these immune cells to inhibit the anti-tumor immune response. However, certain gangliosides also have the capacity to activate specific immune cells. This ganglioside-mediated immunomodulatory effect depends on the type of ganglioside, the amount of sialylation, and on the specific tumor type.
Many aspects of ganglioside-mediated immunomodulation are still unclear, especially regarding individual gangliosides and their specific roles during the anti-tumor immune response. Multiple studies have focused on T cells, dendritic cells, and macrophages and demonstrated that most gangliosides have potent inhibitory effects on the activation, proliferation and functionality of these immune cells. Overall, the shedding of gangliosides by cancer cells and their suppressive actions appear to be great weapons to counteract anti-tumor immunity. Interestingly, the impact of these glycosphingolipids on B cells, NK cells, monocytes, and even neutrophils has hardly been investigated. Moreover, most of the studies related to the immunomodulatory properties of gangliosides have been performed in vitro with isolated gangliosides in co-cultures with one specific immune cell subset. More elaborate functional assays and in vivo studies are needed to gain more insight in the shedding of gangliosides and their immunomodulation in a dynamic and complex environment like the TME.
The gangliosides described in this review can be categorized into gangliosides that exhibit pro-tumorigenic and anti-inflammatory properties stimulating tumor growth, and gangliosides that exhibit anti-tumorigenic and pro-inflammatory properties. Almost all gangliosides, including GM3, GM2 and GM1, are considered immunosuppressive, whereas GD2, GD1b, and GT1b show a dual response depending on the tumor type and the interacting immune cell. Remarkably, gangliosides containing one or two sialic acid moieties appear to be good immune cell inhibitors, thereby promoting tumor progression. On the contrary, the more complex gangliosides, carrying more than two sialic acid residues, also possess anti-tumorigenic features, stimulating T cell proliferation and production of pro-inflammatory cytokines. The mechanism behind this phenomenon is unknown, but could be related to the fact that simple gangliosides predominate in most peripheral tissues [5]. Clearly, the molecular composition of gangliosides is of great importance in cancer immunosurveillance. It is also relevant to mention that sialylated glycosphingolipids are ligands for inhibitory Siglec receptors on immune cells (reviewed in [151]). Siglec-1, for example, interacts with several gangliosides, including GM3, GD1a, GD1b, and GT1b resulting in phagocytosis, degradation, and antigen presentation. Siglec-7 and Siglec-9, amongst other Siglecs, also engage endogenous gangliosides to inhibit immune signaling, such as NK cell cytotoxicity. The ganglioside-Siglec axis could be one of the mechanisms by which lipid sialoglycans modulate immune responses. However, more research is needed to draw strong conclusions about the exact role of ganglioside-Siglec interactions in the TME.
Since many tumors upregulate and shed gangliosides, they are prime candidates for antibody therapy. Gangliosides present in the bloodstream are a perfect diagnostic marker for several tumors and provide targets for antibody therapies directed against tumor-associated gangliosides [16, 152]. Many of these antibodies are now being investigated in pre-clinical and clinical studies [9, 14, 25]. For example, anti-GD2 is currently being administered to neuroblastoma patients in a phase III trial (trial NCT01704716). Additionally, a GD3 antibody-drug conjugate has been administered to melanoma patients in a phase I trial (NCT03159117). However, so far, these therapies were only partially successful. Synthetic antigens mimicking the carbohydrate moiety of GD2 and GD3 gangliosides as vaccines have been tested in an in vivo pre-clinical setting. Interestingly, mice vaccinated with these synthetic gangliosides had an initial γδ T cell response followed by a cascade of CD8+ T cells that infiltrated tumors [153]. Since these proof-of-concept synthetic gangliosides induce both a cellular and humoral response, these glycomimetic vaccines might be expanded to target other tumor gangliosides expressed in several malignancies [153]. In combination with other treatments or as an adjuvant therapy, this approach could be a promising new lead to combat cancer cells. Nevertheless, exploiting tumor-associated gangliosides has been challenging, because glycolipids are poor immunogens, as the carbohydrates may not be efficiently processed nor presented in the context of MHC-I/II [154]. An alternative could be the development of chimeric antigen receptor (CAR) T- and NKT cells directed against tumor-associated gangliosides. Because of its highly tumor-specific expression pattern, GD2-specific CAR-T- and NKT cells have already been used in neuroblastoma or glioma with promising results [155–157]. The development of GD3 CAR-T cells is in a pre-clinical phase, but showed promising results in several murine tumor models [158].
In conclusion, this review highlights gangliosides and their importance in the complex and dynamic process of tumor development and anti-tumor immunity. The importance of shed- or tumor-associated gangliosides in modulating the anti-tumor immune response is evident and multi-disciplinary in nature. We postulate that future research should focus more on complex sialylated glycosphingolipids and on the Siglec-ganglioside interactions to better understand their physiological role and to expand the horizon for targeting gangliosides as an immunomodulatory strategy to cure cancer.
Funding
This work was funded by the KWF Dutch Cancer Society, project grant number 12420, and COST Action CA18103: INNOGLY: INNOvation with GLYcans: new frontiers from synthesis to new biological targets.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Reily C, Stewart TJ, Renfrow MB, Novak J. Glycosylation in health and disease. Nature Reviews Nephrology. 2019;15(6):346–366. doi: 10.1038/s41581-019-0129-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vajaria BN, Patel PS. Glycosylation: a hallmark of cancer? Glycoconjugate Journal. 2017;34(2):147–156. doi: 10.1007/s10719-016-9755-2. [DOI] [PubMed] [Google Scholar]
- 3.Pearce OMT, Läubli H. Sialic acids in cancer biology and immunity. Glycobiology. 2016;26(2):111–128. doi: 10.1093/glycob/cwv097. [DOI] [PubMed] [Google Scholar]
- 4.Daniotti JL, Crespo PM, Yamashita T. In vivo modulation of epidermal growth factor receptor phosphorylation in mice expressing different gangliosides. Journal of Cellular Biochemistry. 2006;99(5):1442–1451. doi: 10.1002/jcb.21034. [DOI] [PubMed] [Google Scholar]
- 5.Cutillo G, Saariaho A-H, Meri S. Physiology of gangliosides and the role of antiganglioside antibodies in human diseases. Cellular & Molecular Immunology. 2020;17(4):313–322. doi: 10.1038/s41423-020-0388-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen L, McCord KA, Bui DT, Bouwman KM, Kitova EN, Elaish M, Kumawat D, Daskhan GC, Tomris I, Han L, Chopra P, Yang TJ, Willows SD, Mason AL, Mahal LK, Lowary TL, West LJ, Hsu SD, Hobman T, Klassen JS. Sialic acid-containing glycolipids mediate binding and viral entry of SARS-CoV-2. Nature Chemical Biology. 2022;18(1):81–90. doi: 10.1038/s41589-021-00924-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blaum BS, Hannan JP, Herbert AP, Kavanagh D, Uhrin D, Stehle T. Structural basis for sialic acid-mediated self-recognition by complement factor H. Nature Chemical Biology. 2015;11(1):77–82. doi: 10.1038/nchembio.1696. [DOI] [PubMed] [Google Scholar]
- 8.Lauc G, Heffer-Lauc M. Shedding and uptake of gangliosides and glycosylphosphatidylinositol-anchored proteins. Biochimica et Biophysica Acta. 2006;1760(4):584–602. doi: 10.1016/j.bbagen.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 9.Cavdarli S, Delannoy P, Groux-Degroote S. O-acetylated gangliosides as targets for cancer immunotherapy. Cells. 2020;9(3):741. doi: 10.3390/cells9030741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kong Y, Li R, Ladisch S. Natural forms of shed tumor gangliosides. Biochimica et Biophysica Acta. 1998;1394(1):43–56. doi: 10.1016/s0005-2760(98)00096-4. [DOI] [PubMed] [Google Scholar]
- 11.Birklé S, Zeng G, Gao L, Yu RK, Aubry J. Role of tumor-associated gangliosides in cancer progression. Biochimie. 2003;85(3):455–463. doi: 10.1016/S0300-9084(03)00006-3. [DOI] [PubMed] [Google Scholar]
- 12.Ladisch S, Gillard B, Wong C, Ulsh L. Shedding and immunoregulatory activity of YAC-1 lymphoma cell gangliosides. Cancer Res. 1983;43(8):3808–3813. [PubMed] [Google Scholar]
- 13.Ladisch S, Kitada S, Hays EF. Gangliosides shed by tumor cells enhance tumor formation in mice. The Journal of Clinical Investigation. 1987;79(6):1879–1882. doi: 10.1172/JCI113031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Groux-Degroote S, Guérardel Y, Delannoy P. Gangliosides: Structures, biosynthesis, analysis, and roles in cancer. ChemBioChem. 2017;18(13):1146–1154. doi: 10.1002/cbic.201600705. [DOI] [PubMed] [Google Scholar]
- 15.Zhang T, de Waard AA, Wuhrer M, Spaapen RM. The role of glycosphingolipids in immune cell functions. Frontiers in Immunology. 2019;10:90. doi: 10.3389/fimmu.2019.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Groux-Degroote S, Delannoy P. Cancer-associated glycosphingolipids as tumor markers and targets for cancer immunotherapy. International Journal of Molecular Sciences. 2021;22(11):6145. doi: 10.3390/ijms22116145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Potapenko, M., Shurin, G. V., & de León, J. (2007). Gangliosides as immunomodulators. Advances in Experimental Medicine and Biology. [DOI] [PubMed]
- 18.Schnaar, R. L., Sandhoff, R., Tiemeyer, M., & Kinoshita, T. (2022). Glycosphingolipids. In th, A. Varki, R. D. Cummings, J. D. Esko, P. Stanley, G. W. Hart, M. Aebi, D. Mohnen, T. Kinoshita, N. H. Packer, J. H. Prestegard, R. L. Schnaar, & P. H. Seeberger (Eds.), Essentials of Glycobiology (pp. 129-140). 10.1101/glycobiology.4e.11
- 19.Inokuchi, J.-i., & Uemura, S. (2014). ST3 Beta-Galactoside Alpha-2,3-Sialyltransferase 5 (ST3GAL5). In N. Taniguchi, K. Honke, M. Fukuda, H. Narimatsu, Y. Yamaguchi, & T. Angata (Eds.), Handbook of glycosyltransferases and related genes (pp. 675-686)Springer . 10.1007/978-4-431-54240-7_61
- 20.Varki A, Cummings R, Esko J. Essentials of glycobiology. 2. Cold Spring Harbor Laboratory Press; 2009. [PubMed] [Google Scholar]
- 21.Simpson MA, Cross H, Proukakis C, Priestman DA, Neville DCA, Reinkensmeier G, Wang H, Wiznitzer M, Gurtz K, Verganelaki A, Pryde A, Patton MA, Dwek RA, Butters TD, Platt FM, Crosby AH. Infantile-onset symptomatic epilepsy syndrome caused by a homozygous loss-of-function mutation of GM3 synthase. Nature Genetics. 2004;36(11):1225–1229. doi: 10.1038/ng1460. [DOI] [PubMed] [Google Scholar]
- 22.Willison HJ, Jacobs BC, van Doorn PA. Guillain-Barré syndrome. The Lancet. 2016;388(10045):717–727. doi: 10.1016/S0140-6736(16)00339-1. [DOI] [PubMed] [Google Scholar]
- 23.Chapman J, Sela B-A, Wertman E, Michaelson DM. Antibodies to ganglioside GM1 in patients with Alzheimer's disease. Neuroscience Letters. 1988;86(2):235–240. doi: 10.1016/0304-3940(88)90577-0. [DOI] [PubMed] [Google Scholar]
- 24.Zappia M, Crescibene L, Bosco D, Arabia G, Nicoletti G, Bagalà A, Bastone L, Napoli ID, Caracciolo M, Bonavita S, Di Costanzo A, Gambardella A, Quattrone A. Anti-GM1 ganglioside antibodies in Parkinson’s disease. Acta Neurologica Scandinavica. 2002;106(1):54–57. doi: 10.1034/j.1600-0404.2002.01240.x. [DOI] [PubMed] [Google Scholar]
- 25.Krengel, U., & Bousquet, P. A. (2014). Molecular recognition of gangliosides and their potential for cancer immunotherapies. Frontiers in Immunology, 5, 325. 10.3389/fimmu.2014.00325 [DOI] [PMC free article] [PubMed]
- 26.Ruggieri S, Mugnai G, Mannini A, Calorini L, Fallani A, Barletta E, Mannori G, Cecconi O. Lipid characteristics in metastatic cells. Clinical & Experimental Metastasis. 1999;17(4):271–276. doi: 10.1023/A:1006662811948. [DOI] [PubMed] [Google Scholar]
- 27.Saito S, Nojiri H, Satoh M, Ito A, Ohyama C, Orikasa S. Inverse relationship of expression between GM3 and globo-series ganglioside in human renal cell carcinoma. The Tohoku Journal of Experimental Medicine. 2000;190(4):271–278. doi: 10.1620/tjem.190.271. [DOI] [PubMed] [Google Scholar]
- 28.Balis FM, Busch CM, Desai AV, Hibbitts E, Naranjo A, Bagatell R, Irwin M, Fox E. The ganglioside GD2 as a circulating tumor biomarker for neuroblastoma. Pediatric Blood & Cancer. 2020;67(1):e28031. doi: 10.1002/pbc.28031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ladisch S, Wu ZL. Detection of a tumour-associated ganglioside in plasma of patients with neuroblastoma. Lancet. 1985;1(8421):136–138. doi: 10.1016/s0140-6736(85)91906-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Valentino L, Moss T, Olson E, Wang H, Elashoff R, Ladisch S. Shed tumor gangliosides and progression of human neuroblastoma. Blood. 1990;75(7):1564–1567. doi: 10.1182/blood.V75.7.1564.1564. [DOI] [PubMed] [Google Scholar]
- 31.Chang F, Li R, Ladisch S. Shedding of gangliosides by human medulloblastoma cells. Experimental Cell Research. 1997;234(2):341–346. doi: 10.1006/excr.1997.3619. [DOI] [PubMed] [Google Scholar]
- 32.Seyfried TN, Mukherjee P. Ganglioside GM3 is antiangiogenic in malignant brain cancer. Journal of Oncology. 2010;2010:e961243. doi: 10.1155/2010/961243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mirkin BL, Clark SH, Zhang C. Inhibition of human neuroblastoma cell proliferation and EGF receptor phosphorylation by gangliosides GM1, GM3, GD1A and GT1B. Cell Proliferation. 2002;35(2):105–115. doi: 10.1046/j.1365-2184.2002.00228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li R, Ladisch S. Shedding of human neuroblastoma gangliosides. Biochimica et Biophysica Acta (BBA) - Lipids and Lipid Metabolism. 1991;1083(1):57–64. doi: 10.1016/0005-2760(91)90124-Z. [DOI] [PubMed] [Google Scholar]
- 35.Zeng G, Li DD, Gao L, Birklé S, Bieberich E, Tokuda A, Yu RK. Alteration of ganglioside composition by stable transfection with antisense vectors against GD3-synthase gene expression. Biochemistry. 1999;38(27):8762–8769. doi: 10.1021/bi9906726. [DOI] [PubMed] [Google Scholar]
- 36.Hettmer S, Ladisch S, Kaucic K. Low complex ganglioside expression characterizes human neuroblastoma cell lines. Cancer Letters. 2005;225(1):141–149. doi: 10.1016/j.canlet.2004.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ladisch S, Wu ZL, Feig S, Ulsh L, Schwartz E, Floutsis G, Wiley F, Lenarsky C, Seeger R. Shedding of GD2 ganglioside by human neuroblastoma. International Journal of Cancer. 1987;39(1):73–76. doi: 10.1002/ijc.2910390113. [DOI] [PubMed] [Google Scholar]
- 38.Nakamura O, Iwamori M, Matsutani M, Takakura K. Ganglioside GD3 shedding by human gliomas. Acta Neurochirurgica(Wien) 1991;109(1-2):34–36. doi: 10.1007/BF01405694. [DOI] [PubMed] [Google Scholar]
- 39.Schengrund CL, Repman MA, Shochat SJ. Ganglioside composition of human neuroblastomas. Correlation with prognosis. A Pediatric Oncology Group Study. Cancer. 1985;56(11):2640–2646. doi: 10.1002/1097-0142(19851201)56:11<2640::aid-cncr2820561118>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 40.Chiricozzi E, Biase ED, Maggioni M, Lunghi G, Fazzari M, Pomè DY, Casellato R, Loberto N, Mauri L, Sonnino S. GM1 promotes TrkA-mediated neuroblastoma cell differentiation by occupying a plasma membrane domain different from TrkA. Journal of Neurochemistry. 2019;149(2):231–241. doi: 10.1111/jnc.14685. [DOI] [PubMed] [Google Scholar]
- 41.Péguet-Navarro J, Sportouch M, Popa I, Berthier O, Schmitt D, Portoukalian J. Gangliosides from human melanoma tumors impair dendritic cell differentiation from monocytes and induce their apoptosis. The Journal of Immunology. 2003;170(7):3488–3494. doi: 10.4049/jimmunol.170.7.3488. [DOI] [PubMed] [Google Scholar]
- 42.Gabri MR, Otero LL, Gomez DE, Alonso DF. Exogenous incorporation of neugc-rich mucin augments n-glycolyl sialic acid content and promotes malignant phenotype in mouse tumor cell lines. Journal of Experimental & Clinical Cancer Research. 2009;28(1):146. doi: 10.1186/1756-9966-28-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bernhard H, Zum Büschenfelde K-HM, Dippold WG. Ganglioside GD3 shedding by human malignant melanoma cells. International Journal of Cancer. 1989;44(1):155–160. doi: 10.1002/ijc.2910440127. [DOI] [PubMed] [Google Scholar]
- 44.Dong Y, Ikeda K, Hamamura K, Zhang Q, Kondo Y, Matsumoto Y, Ohmi Y, Yamauchi Y, Furukawa K, Taguchi R, Furukawa K. GM1/GD1b / GA1 synthase expression results in the reduced cancer phenotypes with modulation of composition and raft-localization of gangliosides in a melanoma cell line. Cancer Science. 2010;101(9):2039–2047. doi: 10.1111/j.1349-7006.2010.01613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Marquina G, Waki H, Fernandez LE, Kon K, Carr A, Valiente O, Perez R, Ando S. Gangliosides expressed in human breast cancer. Cancer Research. 1996;56(22):5165–5171. [PubMed] [Google Scholar]
- 46.Wiesner DA, Sweeley CC. Circulating gangliosides of breast-cancer patients. International Journal of Cancer. 1995;60(3):294–299. doi: 10.1002/ijc.2910600303. [DOI] [PubMed] [Google Scholar]
- 47.Battula VL, Shi Y, Evans KW, Wang RY, Spaeth EL, Jacamo RO, Guerra R, Sahin AA, Marini FC, Hortobagyi G, Mani SA, Andreeff M. Ganglioside GD2 identifies breast cancer stem cells and promotes tumorigenesis. Journal of Clinical Investigation. 2012;122(6):2066–2078. doi: 10.1172/JCI59735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Cruijsen H, Ruiz MG, van der Valk P, de Gruijl TD, Giaccone G. Tissue micro array analysis of ganglioside N-glycolyl GM3 expression and signal transducer and activator of transcription (STAT)-3 activation in relation to dendritic cell infiltration and microvessel density in non-small cell lung cancer. BMC Cancer. 2009;9:180. doi: 10.1186/1471-2407-9-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gu Y, Zhang J, Mi W, Yang J, Han F, Lu X, Yu W. Silencing of GM3 synthase suppresses lung metastasis of murine breast cancer cells. Breast Cancer Research. 2008;10(1):R1. doi: 10.1186/bcr1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hayashi N, Chiba H, Kuronuma K, Go S, Hasegawa Y, Takahashi M, Gasa S, Watanabe A, Hasegawa T, Kuroki Y, Inokuchi J, Takahashi H. Detection of N-glycolyated gangliosides in non-small-cell lung cancer using GMR8 monoclonal antibody. Cancer Science. 2013;104(1):43–47. doi: 10.1111/cas.12027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yoshida S, Fukumoto S, Kawaguchi H, Sato S, Ueda R, Furukawa K. Ganglioside GD2 in small cell lung cancer cell lines: Enhancement of cell proliferation and mediation of apoptosis. Cancer Research. 2001;61(10):4244–4252. [PubMed] [Google Scholar]
- 52.Webb TJ, Li X, Giuntoli RL, 2nd, Lopez PH, Heuser C, Schnaar RL, Tsuji M, Kurts C, Oelke M, Schneck JP. Molecular identification of GD3 as a suppressor of the innate immune response in ovarian cancer. Cancer Research. 2012;72(15):3744–3752. doi: 10.1158/0008-5472.Can-11-2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ravindranath MH, Muthugounder S, Presser N, Santin AD, Selvan SR, Morton DL. Ganglioside GD1a, present in ovarian cancer cells, ascites and sera of patients elicits endogenous IgM response. Cancer Research. 2005;65(9):1216–1216. [Google Scholar]
- 54.Biswas K, Richmond A, Rayman P, Biswas S, Thornton M, Sa G, Das T, Zhang R, Chahlavi A, Tannenbaum CS, Novick A, Bukowski R, Finke JH. GM2 expression in renal cell carcinoma: Potential role in tumor-induced T-cell dysfunction. Cancer Research. 2006;66(13):6816–6825. doi: 10.1158/0008-5472.CAN-06-0250. [DOI] [PubMed] [Google Scholar]
- 55.Kudo D, Rayman P, Horton C, Cathcart MK, Bukowski RM, Thornton M, Tannenbaum C, Finke JH. Gangliosides expressed by the renal cell carcinoma cell line SK-RC-45 are involved in tumor-induced apoptosis of T cells. Cancer Research. 2003;63(7):1676–1683. [PubMed] [Google Scholar]
- 56.Chung TW, Choi HJ, Kim SJ, Kwak CH, Song KH, Jin UH, Chang YC, Chang HW, Lee YC, Ha KT, Kim CH. The ganglioside GM3 is associated with cisplatin-induced apoptosis in human colon cancer cells. PLoS One. 2014;9(5):e92786. doi: 10.1371/journal.pone.0092786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kwak DH, Ryu JS, Kim CH, Ko K, Ma JY, Hwang KA, Choo YK. Relationship between ganglioside expression and anti-cancer effects of the monoclonal antibody against epithelial cell adhesion molecule in colon cancer. Experimental & Molecular Medicine. 2011;43(12):693–701. doi: 10.3858/emm.2011.43.12.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Westrick MA, Lee WM, Goff B, Macher BA. Gangliosides of human acute leukemia cells. Biochimica et Biophysica Acta. 1983;750(1):141–148. doi: 10.1016/0005-2760(83)90213-8. [DOI] [PubMed] [Google Scholar]
- 59.De Maria R, Lenti L, Malisan F, d'Agostino F, Tomassini B, Zeuner A, Rippo MR, Testi R. Requirement for GD3 ganglioside in CD95- and ceramide-induced apoptosis. Science. 1997;277(5332):1652–1655. doi: 10.1126/science.277.5332.1652. [DOI] [PubMed] [Google Scholar]
- 60.Sasaki N, Hirabayashi K, Michishita M, Takahashi K, Hasegawa F, Gomi F, Itakura Y, Nakamura N, Toyoda M, Ishiwata T. Ganglioside GM2, highly expressed in the MIA PaCa-2 pancreatic ductal adenocarcinoma cell line, is correlated with growth, invasion, and advanced stage. Scientific Reports. 2019;9(1):19369. doi: 10.1038/s41598-019-55867-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Paris R, Morales A, Coll O, Sánchez-Reyes A, García-Ruiz C, Fernández-Checa JC. Ganglioside GD3 sensitizes human hepatoma cells to cancer therapy. Journal of Biological Chemistry. 2002;277(51):49870–49876. doi: 10.1074/jbc.M208303200. [DOI] [PubMed] [Google Scholar]
- 62.Li Y, Huang X, Zhong W, Zhang J, Ma K. Ganglioside GM3 promotes HGF-stimulated motility of murine hepatoma cell through enhanced phosphorylation of cMet at specific tyrosine sites and PI3K/Akt-mediated migration signaling. Molecular and Cellular Biochemistry. 2013;382(1-2):83–92. doi: 10.1007/s11010-013-1720-9. [DOI] [PubMed] [Google Scholar]
- 63.Huang X, Li Y, Zhang J, Xu Y, Tian Y, Ma K. Ganglioside GM3 inhibits hepatoma cell motility via down-regulating activity of EGFR and PI3K/AKT signaling pathway. Journal of Cellular Biochemistry. 2013;114(7):1616–1624. doi: 10.1002/jcb.24503. [DOI] [PubMed] [Google Scholar]
- 64.Ouyang S, Liu JH, Ni Z, Ding GF, Wang QZ. Downregulation of ST3GAL5 is associated with muscle invasion, high grade and a poor prognosis in patients with bladder cancer. Oncology Letters. 2020;20(1):828–840. doi: 10.3892/ol.2020.11597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang J, van der Zon G, Ma J, Mei H, Cabukusta B, Agaser CC, Madunić K, Wuhrer M, Zhang T, Ten Dijke P. ST3GAL5-catalyzed gangliosides inhibit TGF-β-induced epithelial-mesenchymal transition via TβRI degradation. The EMBO Journal. 2023;42(2):e110553. doi: 10.15252/embj.2021110553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Suzuki M, Nagane M, Kato K, Yamauchi A, Shimizu T, Yamashita H, Aihara N, Kamiie J, Kawashima N, Naito S, Yamashita T. Endothelial ganglioside GM3 regulates angiogenesis in solid tumors. Biochemical and Biophysical Research Communications. 2021;569:10–16. doi: 10.1016/j.bbrc.2021.06.063. [DOI] [PubMed] [Google Scholar]
- 67.Cai H, Zhou H, Miao Y, Li N, Zhao L, Jia L. MiRNA expression profiles reveal the involvement of miR-26a, miR-548l and miR-34a in hepatocellular carcinoma progression through regulation of ST3GAL5. Laboratory Investigation. 2017;97(5):530–542. doi: 10.1038/labinvest.2017.12. [DOI] [PubMed] [Google Scholar]
- 68.Liu J, Li M, Wu J, Qi Q, Li Y, Wang S, Liang S, Zhang Y, Zhu Z, Huang R, Yan J, Zhu R. Identification of ST3GAL5 as a prognostic biomarker correlating with CD8(+) T cell exhaustion in clear cell renal cell carcinoma. Frontiers in Immunology. 2022;13:979605. doi: 10.3389/fimmu.2022.979605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cazet A, Lefebvre J, Adriaenssens E, Julien S, Bobowski M, Grigoriadis A, Tutt A, Tulasne D, Le Bourhis X, Delannoy P. GD3 synthase expression enhances proliferation and tumor growth of MDA-MB-231 breast cancer cells through c-Met activation. Molecular Cancer Research. 2010;8(11):1526–1535. doi: 10.1158/1541-7786.Mcr-10-0302. [DOI] [PubMed] [Google Scholar]
- 70.Lluis JM, Llacuna L, von Montfort C, Bárcena C, Enrich C, Morales A, Fernandez-Checa JC. GD3 synthase overexpression sensitizes hepatocarcinoma cells to hypoxia and reduces tumor growth by suppressing the cSrc/NF-κB survival pathway. PLoS One. 2009;4(11):e8059. doi: 10.1371/journal.pone.0008059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kasprowicz, A., Sophie, G. D., Lagadec, C., & Delannoy, P. (2022). Role of GD3 synthase ST8Sia I in cancers. Cancers (Basel), 14(5). 10.3390/cancers14051299 [DOI] [PMC free article] [PubMed]
- 72.Ruan S, Lloyd KO. Glycosylation pathways in the biosynthesis of gangliosides in melanoma and neuroblastoma cells: Relative glycosyltransferase levels determine ganglioside patterns. Cancer Research. 1992;52(20):5725–5731. [PubMed] [Google Scholar]
- 73.Thampoe IJ, Furukawa K, Vellvé E, Lloyd KO. Sialyltransferase levels and ganglioside expression in melanoma and other cultured human cancer cells. Cancer Research. 1989;49(22):6258–6264. [PubMed] [Google Scholar]
- 74.Ruckhäberle E, Karn T, Rody A, Hanker L, Gätje R, Metzler D, Holtrich U, Kaufmann M. Gene expression of ceramide kinase, galactosyl ceramide synthase and ganglioside GD3 synthase is associated with prognosis in breast cancer. Journal of Cancer Research and Clinical Oncology. 2009;135(8):1005–1013. doi: 10.1007/s00432-008-0536-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zeng G, Gao L, Birklé S, p., & Yu, R. K. Suppression of ganglioside GD3 expression in a Rat F-11 tumor cell line reduces tumor growth, angiogenesis, and vascular endothelial growth factor production. Cancer Research. 2000;60(23):6670–6676. [PubMed] [Google Scholar]
- 76.Ladisch S. Biological significance of tumor gangliosides: Shedding, transfer, and immunosuppression. In: Vanderhoek JY, editor. Frontiers in bioactive lipids. Springer; 1996. pp. 215–221. [Google Scholar]
- 77.Russo D, Parashuraman S, D’Angelo G. Glycosphingolipid–protein interaction in signal transduction. International Journal of Molecular Sciences. 2016;17(10):1732. doi: 10.3390/ijms17101732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Julien S, Bobowski M, Steenackers A, Le Bourhis X, Delannoy P. How do gangliosides regulate RTKs signaling? Cells. 2013;2(4):751–767. doi: 10.3390/cells2040751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hossain DM, Mohanty S, Ray P, Das T, Sa G. Tumor gangliosides and T cells: A deadly encounter. Frontiers in Bioscience (Schol Ed) 2012;4(2):502–519. doi: 10.2741/281. [DOI] [PubMed] [Google Scholar]
- 80.Bergelson LD. Serum gangliosides as endogenous immunomodulators. Immunology Today. 1995;16(10):483–486. doi: 10.1016/0167-5699(95)80032-8. [DOI] [PubMed] [Google Scholar]
- 81.Tay RE, Richardson EK, Toh HC. Revisiting the role of CD4(+) T cells in cancer immunotherapy-new insights into old paradigms. Cancer Gene Therapy. 2021;28(1-2):5–17. doi: 10.1038/s41417-020-0183-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hoon DSB, Irie RF, Cochran AJ. Gangliosides from human melanoma immunomodulate response of T cells to interleukin-2. Cellular Immunology. 1988;111(2):410–419. doi: 10.1016/0008-8749(88)90104-9. [DOI] [PubMed] [Google Scholar]
- 83.Chu JW, Sharom FJ. Gangliosides inhibit T-lymphocyte proliferation by preventing the interaction of interleukin-2 with its cell surface receptors. Immunology. 1993;79(1):10–17. [PMC free article] [PubMed] [Google Scholar]
- 84.Kanda N. Gangliosides GD1a and GM3 induce interleukin-10 production by human T cells. Biochemical and Biophysical Research Communications. 1999;256(1):41–44. doi: 10.1006/bbrc.1999.0281. [DOI] [PubMed] [Google Scholar]
- 85.Chahlavi A, Rayman P, Richmond AL, Biswas K, Zhang R, Vogelbaum M, Tannenbaum C, Barnett G, Finke JH. Glioblastomas induce T-lymphocyte death by two distinct pathways involving gangliosides and CD70. Cancer Research. 2005;65(12):5428–5438. doi: 10.1158/0008-5472.CAN-04-4395. [DOI] [PubMed] [Google Scholar]
- 86.Crespo FA, Sun X, Cripps JG, Fernandez-Botran R. The immunoregulatory effects of gangliosides involve immune deviation favoring type-2 T cell responses. Journal of Leukocyte Biology. 2006;79(3):586–595. doi: 10.1189/jlb.0705395. [DOI] [PubMed] [Google Scholar]
- 87.Finke JH, Rayman P, George R, Tannenbaum CS, Kolenko V, Uzzo R, Novick AC, Bukowski RM. Tumor-induced sensitivity to apoptosis in T cells from patients with renal cell carcinoma: Role of nuclear factor-κB suppression. Clinical Cancer Research. 2001;7(3):940s–946s. [PubMed] [Google Scholar]
- 88.Offner H, Thieme T, Vandenbark AA. Gangliosides induce selective modulation of CD4 from helper T lymphocytes. The Journal of Immunology. 1987;139(10):3295–3305. doi: 10.4049/jimmunol.139.10.3295. [DOI] [PubMed] [Google Scholar]
- 89.Colell A, García-Ruiz C, Roman J, Ballesta A, FernándezCheca JC. Ganglioside GD3 enhances apoptosis by suppressing the nuclear factor-κB-dependent survival pathway. The FASEB Journal. 2001;15(6):1068–1070. doi: 10.1096/fsb2fj000574fje. [DOI] [PubMed] [Google Scholar]
- 90.Sa G, Das T, Moon C, Hilston CM, Rayman PA, Rini BI, Tannenbaum CS, Finke JH. GD3, an overexpressed tumor-derived ganglioside, mediates the apoptosis of activated but not resting T cells. Cancer Research. 2009;69(7):3095–3104. doi: 10.1158/0008-5472.CAN-08-3776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Shenoy GN, Loyall J, Berenson CS, Kelleher RJ, Iyer V, Balu-Iyer SV, Odunsi K, Bankert RB. Sialic acid–dependent inhibition of T cells by exosomal ganglioside GD3 in ovarian tumor microenvironments. The Journal of Immunology. 2018;201(12):3750–3758. doi: 10.4049/jimmunol.1801041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kume, M., Kiyohara, E., Matsumura, Y., Koguchi-Yoshioka, H., Tanemura, A., Hanaoka, Y., Taminato, M., Tashima, H., Tomita, K., Kubo, T., Watanabe, R., & Fujimoto, M. (2021). Ganglioside GD3 may suppress the functional activities of benign skin T cells in cutaneous T-cell lymphoma. Frontiers in Immunology, 12, 651048. 10.3389/fimmu.2021.651048 [DOI] [PMC free article] [PubMed]
- 93.Shen W, Stone K, Jales A, Leitenberg D, Ladisch S. Inhibition of TLR activation and up-regulation of IL-1R-associated kinase-M expression by exogenous gangliosides. The Journal of Immunology. 2008;180(7):4425–4432. doi: 10.4049/jimmunol.180.7.4425. [DOI] [PubMed] [Google Scholar]
- 94.Morioka N, Furue M, Tsuchida T, Ishibashi Y. Gangliosides inhibit the proliferation of human T cells stimulated with interleukin-4 or interleukin-2. The Journal of Dermatology. 1991;18(8):447–453. doi: 10.1111/j.1346-8138.1991.tb03114.x. [DOI] [PubMed] [Google Scholar]
- 95.Kanda N, Watanabe S. Gangliosides GD1b, GT1b, and GQ1b enhance IL-2 and IFN-γ production and suppress IL-4 and IL-5 production in phytohemagglutinin-stimulated human T cells. The Journal of Immunology. 2001;166(1):72–80. doi: 10.4049/jimmunol.166.1.72. [DOI] [PubMed] [Google Scholar]
- 96.Kanda N, Nakai K, Watanabe S. Gangliosides GD1b, GT1b, and GQ1b suppress the growth of human melanoma by inhibiting interleukin-8 production: the inhibition of adenylate cyclase. The Journal of Investigative Dermatology. 2001;117(2):284–293. doi: 10.1046/j.0022-202x.2001.01423.x. [DOI] [PubMed] [Google Scholar]
- 97.Pique C, Mahé Y, Scamps C, Tétaud C, Tursz T, Wiels J. Analysis of phenotypic and functional changes during ganglioside-induced inhibition of human T cell proliferation. Molecular Immunology. 1991;28(11):1163–1170. doi: 10.1016/0161-5890(91)90002-2. [DOI] [PubMed] [Google Scholar]
- 98.Kimata H, Yoshida A. Inhibition of spontaneous immunoglobulin production by ganglioside GM2 in human B cells. Clinical Immunology and Immunopathology. 1996;79(2):197–202. doi: 10.1006/clin.1996.0068. [DOI] [PubMed] [Google Scholar]
- 99.Kanda N, Watanabe S. Ganglioside GD1a enhances immunoglobulin production by human peripheral blood mononuclear cells. Experimental Hematology. 2000;28(6):672–679. doi: 10.1016/S0301-472X(00)00167-3. [DOI] [PubMed] [Google Scholar]
- 100.Kanda N, Tamaki K. Ganglioside GD1b suppresses immunoglobulin production by human peripheral blood mononuclear cells. Experimental Hematology. 1999;27(10):1487–1493. doi: 10.1016/S0301-472X(99)00093-4. [DOI] [PubMed] [Google Scholar]
- 101.Kanda N, Tamaki K. Ganglioside GT1b suppresses immunoglobulin production by human peripheral blood mononuclear cells. Immunology. 1999;96(4):628–633. doi: 10.1046/j.1365-2567.1999.00734.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Grayson G, Ladisch S. Immunosuppression by human gangliosides. II. Carbohydrate structure and inhibition of human NK activity. Cellular Immunology. 1992;139(1):18–29. doi: 10.1016/0008-8749(92)90096-8. [DOI] [PubMed] [Google Scholar]
- 103.Bergelson LD, Dyatlovitskaya EV, Klyuchareva TE, Kryukova EV, Lemenovskaya AF, Matveeva VA, Sinitsyna EV. The role of glycosphingolipids in natural immunity. gangliosides modulate the cytotoxicity of natural killer cells. European Journal of Immunology. 1989;19(11):1979–1983. doi: 10.1002/eji.1830191102. [DOI] [PubMed] [Google Scholar]
- 104.Ankel CKH. Inhibition of beta-interferon augmentation of murine natural killer cytoxicity by gangliosides. Journal of Interferon Research. 2009;2(2):245–251. doi: 10.1089/jir.1982.2.245. [DOI] [PubMed] [Google Scholar]
- 105.Lee WC, Lee WL, Shyong WY, Yang LW, Ko MC, Yeh CC, Hsieh SL, Wang PH. Altered ganglioside GD3 in HeLa cells might influence the cytotoxic abilities of NK cells. Taiwanese Journal of Obstetrics and Gynecology. 2012;51(2):199–205. doi: 10.1016/j.tjog.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 106.Nicoll G, Avril T, Lock K, Furukawa K, Bovin N, Crocker PR. Ganglioside GD3 expression on target cells can modulate NK cell cytotoxicity via siglec-7-dependent and -independent mechanisms. European Journal of Immunology. 2003;33(6):1642–1648. doi: 10.1002/eji.200323693. [DOI] [PubMed] [Google Scholar]
- 107.Iltis, C., Seguin, L., Cervera, L., Duret, L., Hamidouche, T., Kunz, S., Croce, O., Delannoy, C., Gueŕardel, Y., Allain, F., Moudombi, L., Hofman, P., Cosson, E., Guglielmi, J., Pourcher, T., Braud, V. M., Shkreli, M., Michallet, M.-C., Feral, C. C., Cherfils-Vicini, J. (2021). A ganglioside-based senescence-associated immune checkpoint. bioRxiv, 2021.2004.2023.440408. 10.1101/2021.04.23.440408
- 108.Wu DY, Segal NH, Sidobre S, Kronenberg M, Chapman PB. Cross-presentation of disialoganglioside GD3 to natural killer T cells. Journal of Experimental Medicine. 2003;198(1):173–181. doi: 10.1084/jem.20030446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Brønnum H, Seested T, Hellgren LI, Brix S, Frøkiær H. Milk-derived GM3 and GD3 differentially inhibit dendritic cell maturation and effector functionalities. Scandinavian Journal of Immunology. 2005;61(6):551–557. doi: 10.1111/j.1365-3083.2005.01566.x. [DOI] [PubMed] [Google Scholar]
- 110.Walker SR, Redlinger RE, Jr, Barksdale EM., Jr Neuroblastoma-induced inhibition of dendritic cell IL-12 production via abrogation of CD40 expression. Journal of Pediatric Surgery. 2005;40(1):244. doi: 10.1016/j.jpedsurg.2004.09.050. [DOI] [PubMed] [Google Scholar]
- 111.Bennaceur K, Popa I, Portoukalian J, Berthier-Vergnes O, Peguet-Navarro J. Melanoma-derived gangliosides impair migratory and antigen-presenting function of human epidermal Langerhans cells and induce their apoptosis. International Immunology. 2006;18(6):879–886. doi: 10.1093/intimm/dxl024. [DOI] [PubMed] [Google Scholar]
- 112.WöLFL M, Batten WY, Posovszky C, Bernhard H, Berthold F. Gangliosides inhibit the development from monocytes to dendritic cells. Clinical & Experimental Immunology. 2002;130(3):441–448. doi: 10.1046/j.1365-2249.2002.02006.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Jales A, Falahati R, Mari E, Stemmy EJ, Shen W, Southammakosane C, Herzog D, Ladisch S, Leitenberg D. Ganglioside-exposed dendritic cells inhibit T-cell effector function by promoting regulatory cell activity. Immunology. 2011;132(1):134–143. doi: 10.1111/j.1365-2567.2010.03348.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Shurin GV, Shurin MR, Bykovskaia S, Shogan J, Lotze MT, Barksdale EM. Neuroblastoma-derived gangliosides inhibit dendritic cell generation and function. Cancer Research. 2001;61(1):363–369. [PubMed] [Google Scholar]
- 115.Dillinger B, Ahmadi-Erber S, Lau M, Hoelzl MA, Erhart F, Juergens B, Fuchs D, Heitger A, Ladisch S, Dohnal AM. IFN-γ and tumor gangliosides: Implications for the tumor microenvironment. Cellular Immunology. 2018;325:33–40. doi: 10.1016/j.cellimm.2018.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Shen W, Ladisch S. Ganglioside GD1a impedes lipopolysaccharide-induced maturation of human dendritic cells. Cellular Immunology. 2002;220(2):125–133. doi: 10.1016/s0008-8749(03)00004-2. [DOI] [PubMed] [Google Scholar]
- 117.Hoon DSB, Jung T, Naungayan J, Cochran AJ, Morton DL, McBride WH. Modulation of human macrophage functions by gangliosides. Immunology Letters. 1989;20(4):269–275. doi: 10.1016/0165-2478(89)90034-5. [DOI] [PubMed] [Google Scholar]
- 118.Park J, Kwak CH, Ha SH, Kwon KM, Abekura F, Cho SH, Chang YC, Lee YC, Ha KT, Chung TW, Kim CH. Ganglioside GM3 suppresses lipopolysaccharide-induced inflammatory responses in rAW 264.7 macrophage cells through NF-kappaB, AP-1, and MAPKs signaling. Journal of Cellular Biochemistry. 2018;119(1):1173–1182. doi: 10.1002/jcb.26287. [DOI] [PubMed] [Google Scholar]
- 119.Kumar A, Parajuli P, Singh SM. Gangliosides produced by a T cell lymphoma inhibit the production of reactive nitrogen intermediates by murine peritoneal macrophages. Journal of Clinical Biochemistry and Nutrition. 1996;21(3):171–182. doi: 10.3164/jcbn.21.171. [DOI] [Google Scholar]
- 120.Ziegler-Heitbrock HW, Käfferlein E, Haas JG, Meyer N, Ströbel M, Weber C, Flieger D. Gangliosides suppress tumor necrosis factor production in human monocytes. The Journal of Immunology. 1992;148(6):1753–1758. doi: 10.4049/jimmunol.148.6.1753. [DOI] [PubMed] [Google Scholar]
- 121.Chung T-W, Choi H-J, Park M-J, Choi H-J, Lee S-O, Kim K-J, Kim C-H, Hong C, Kim K-H, Joo M, Ha K-T. The function of cancer-shed gangliosides in macrophage phenotype: involvement with angiogenesis. Oncotarget. 2016;8(3):4436–4448. doi: 10.18632/oncotarget.13878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wang Y, Cui Y, Cao F, Qin Y, Li W, Zhang J. Ganglioside GD1a suppresses LPS-induced pro-inflammatory cytokines in RAW264.7 macrophages by reducing MAPKs and NF-κB signaling pathways through TLR4. International Immunopharmacology. 2015;28(1):136–145. doi: 10.1016/j.intimp.2015.05.044. [DOI] [PubMed] [Google Scholar]
- 123.Kim S-J, Chung T-W, Choi H-J, Jin U-H, Ha K-T, Lee Y-C, Kim C-H. Monosialic ganglioside GM3 specifically suppresses the monocyte adhesion to endothelial cells for inflammation. The International Journal of Biochemistry & Cell Biology. 2014;46:32–38. doi: 10.1016/j.biocel.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 124.Caldwell S, Heitger A, Shen W, Liu Y, Taylor B, Ladisch S. Mechanisms of ganglioside inhibition of APC function. Journal of Immunology. 2003;171(4):1676–1683. doi: 10.4049/jimmunol.171.4.1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Chu JWK, Sharom FJ. Effect of micellar and bilayer gangliosides on proliferation of interleukin-2-dependent lymphocytes. Cellular Immunology. 1991;132(2):319–338. doi: 10.1016/0008-8749(91)90031-6. [DOI] [PubMed] [Google Scholar]
- 126.Lu P, Sharom FJ. Gangliosides are potent immunosuppressors of IL-2-mediated T-cell proliferation in a low protein environment. Immunology. 1995;86(3):356–363. [PMC free article] [PubMed] [Google Scholar]
- 127.Parker, J., Caldini, G., Krishnamurti, C., Ahrens, P., & Ankel, H. (1984). Binding of interleukin 2 to gangliosides. FEBS Letters. 10.1016/0014-5793(84)81351-4 [DOI] [PubMed]
- 128.Rayman P, Wesa AK, Richmond AL, Das T, Biswas K, Raval G, Storkus WJ, Tannenbaum C, Novick A, Bukowski R, Finke J. Effect of renal cell carcinomas on the development of type 1 T-cell responses. Clinical Cancer Research. 2004;10(18):6360S–6366S. doi: 10.1158/1078-0432.Ccr-050011. [DOI] [PubMed] [Google Scholar]
- 129.Röpke C, Gladstone P, Nielsen M, Borregaard N, Ledbetter JA, Svejgaard A, Odum N. Apoptosis following interleukin-2 withdrawal from T cells: Evidence for a regulatory role of CD18 (beta 2-integrin) molecules. Tissue Antigens. 1996;48(2):127–135. doi: 10.1111/j.1399-0039.1996.tb02617.x. [DOI] [PubMed] [Google Scholar]
- 130.Zhang J, Bárdos T, Shao Q, Tschopp J, Mikecz K, Glant TT, Finnegan A. IL-4 potentiates activated T cell apoptosis via an IL-2-dependent mechanism. The Journal of Immunology. 2003;170(7):3495–3503. doi: 10.4049/jimmunol.170.7.3495. [DOI] [PubMed] [Google Scholar]
- 131.Leòn J, Fernández A, Mesa C, Clavel M, Fernandez LE. Role of tumour-associated N-glycolylated variant of GM3 ganglioside in cancer progression: Effect over CD4 expression on T cells. Cancer Immunology, Immunotherapy. 2006;55(4):443–450. doi: 10.1007/s00262-005-0041-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sorice M, Pavan A, Misasi R, Sansolini T, Garofalo T, Lenti L, Pontieri GM, Frati L, Torrisi MR. Monosialoganglioside GM3 induces CD4 internalization in human peripheral blood T lymphocytes. Scandinavian Journal of Immunology. 1995;41(2):148–156. doi: 10.1111/j.1365-3083.1995.tb03547.x. [DOI] [PubMed] [Google Scholar]
- 133.Garofalo T, Sorice M, Misasi R, Cinque B, Giammatteo M. A novel mechanism of CD4 down-modulation induced by monosialoganglioside GM3. Journal of Biological Chemistry. 1998;273:35153–35160. doi: 10.1074/jbc.273.52.35153. [DOI] [PubMed] [Google Scholar]
- 134.Irani DN, Lin KI, Griffin DE. Brain-derived gangliosides regulate the cytokine production and proliferation of activated T cells. Journal of Immunology (Baltimore, Md.: 1950) 1996;157(10):4333–4340. doi: 10.4049/jimmunol.157.10.4333. [DOI] [PubMed] [Google Scholar]
- 135.Laumont CM, Banville AC, Gilardi M, Hollern DP, Nelson BH. Tumour-infiltrating B cells: immunological mechanisms, clinical impact and therapeutic opportunities. Nature Reviews Cancer. 2022;22(7):414–430. doi: 10.1038/s41568-022-00466-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Yuen GJ, Demissie E, Pillai S. B lymphocytes and cancer: A love-hate relationship. Trends in Cancer. 2016;2(12):747–757. doi: 10.1016/j.trecan.2016.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Morvan MG, Lanier LL. NK cells and cancer: you can teach innate cells new tricks. Nature Reviews Cancer. 2016;16(1):7–19. doi: 10.1038/nrc.2015.5. [DOI] [PubMed] [Google Scholar]
- 138.Theruvath J, Menard M, Smith BAH, Linde MH, Coles GL, Dalton GN, Wu W, Kiru L, Delaidelli A, Sotillo E, Silberstein JL, Geraghty AC, Banuelos A, Radosevich MT, Dhingra S, Heitzeneder S, Tousley A, Lattin J, Xu P, Majzner RG. Anti-GD2 synergizes with CD47 blockade to mediate tumor eradication. Nature Medicine. 2022;28(2):333–344. doi: 10.1038/s41591-021-01625-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bennaceur K, Popa I, Chapman JA, Migdal C, Péguet-Navarro J, Touraine J-L, Portoukalian J. Different mechanisms are involved in apoptosis induced by melanoma gangliosides on human monocyte-derived dendritic cells. Glycobiology. 2009;19(6):576–582. doi: 10.1093/glycob/cwp015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.DeNardo DG, Ruffell B. Macrophages as regulators of tumour immunity and immunotherapy. Nature Reviews Immunology. 2019;19(6):369–382. doi: 10.1038/s41577-019-0127-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mantovani, A., Allavena, P., Marchesi, F., & Garlanda, C. (2022). Macrophages as tools and targets in cancer therapy. Nature Reviews Drug Discovery. 10.1038/s41573-022-00520-5 [DOI] [PMC free article] [PubMed]
- 142.Ben Mkaddem, S., Benhamou, M., & Monteiro, R. C. (2019). Understanding Fc receptor involvement in inflammatory diseases: from mechanisms to new therapeutic tools. Frontiers in Immunology, 10, 811.10.3389/fimmu.2019.00811 [DOI] [PMC free article] [PubMed]
- 143.Weiskopf K, Weissman IL. Macrophages are critical effectors of antibody therapies for cancer. MAbs. 2015;7(2):303–310. doi: 10.1080/19420862.2015.1011450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Gelfo V, Romaniello D, Mazzeschi M, Sgarzi M, Grilli G, Morselli A, Manzan B, Rihawi K, Lauriola M. Roles of IL-1 in cancer: From tumor progression to resistance to targeted therapies. International Journal of Molecular Sciences. 2020;21(17):6009. doi: 10.3390/ijms21176009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Park J, Kwak C-H, Ha S-H, Kwon K-M, Abekura F, Cho S-H, Chang Y-C, Lee Y-C, Ha K-T, Chung T-W, Kim C-H. Ganglioside GM3 suppresses lipopolysaccharide-induced inflammatory responses in rAW 264.7 macrophage cells through NF-κB, AP-1, and MAPKs signaling. Journal of Cellular Biochemistry. 2018;119(1):1173–1182. doi: 10.1002/jcb.26287. [DOI] [PubMed] [Google Scholar]
- 146.Montfort A, Colacios C, Levade T, Andrieu-Abadie N, Meyer N, Segui B. The TNF paradox in cancer progression and immunotherapy. Frontiers in Immunology. 2019;10:1818. doi: 10.3389/fimmu.2019.01818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kashfi, K., Kannikal, J., & Nath, N. (2021). Macrophage reprogramming and cancer therapeutics: Role of iNOS-derived NO. Cells, 10(11). 10.3390/cells10113194 [DOI] [PMC free article] [PubMed]
- 148.Jakubzick CV, Randolph GJ, Henson PM. Monocyte differentiation and antigen-presenting functions. Nature Reviews Immunology. 2017;17(6):349–362. doi: 10.1038/nri.2017.28. [DOI] [PubMed] [Google Scholar]
- 149.Ladisch S, Ulsh L, Gillard B, Wong C. Modulation of the immune response by gangliosides. Inhibition of adherent monocyte accessory function in vitro. Journal of Clinical Investigation. 1984;74(6):2074–2081. doi: 10.1172/jci111631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wondimu A, Liu Y, Su Y, Bobb D, Ma JS, Chakrabarti L, Radoja S, Ladisch S. Gangliosides drive the tumor infiltration and function of myeloid-derived suppressor cells. Cancer Res. 2014;74(19):5449–5457. doi: 10.1158/0008-5472.CAN-14-0927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Schnaar, R. L. (2023). Gangliosides as Siglec ligands. Glycoconjugate Journal. 10.1007/s10719-023-10101-2 [DOI] [PMC free article] [PubMed]
- 152.Li Q, Sun M, Yu M, Fu Q, Jiang H, Yu G, Li G. Gangliosides profiling in serum of breast cancer patient: GM3 as a potential diagnostic biomarker. Glycoconjugate Journal. 2019;36(5):419–428. doi: 10.1007/s10719-019-09885-z. [DOI] [PubMed] [Google Scholar]
- 153.Tong, W., Maira, M., Roychoudhury, R., Galan, A., Brahimi, F., Gilbert, M., Cunningham, A. M., Josephy, S., Pirvulescu, I., Moffett, S., & Saragovi, H. U. (2019). Vaccination with tumor-ganglioside glycomimetics activates a selective immunity that affords cancer therapy. Cell Chemical Biology, 26(7), 1013-1026 e1014. 10.1016/j.chembiol.2019.03.018 [DOI] [PubMed]
- 154.Sun L, Middleton DR, Wantuch PL, Ozdilek A, Avci FY. Carbohydrates as T-cell antigens with implications in health and disease. Glycobiology. 2016;26(10):1029–1040. doi: 10.1093/glycob/cww062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Prapa M, Caldrer S, Spano C, Bestagno M, Golinelli G, Grisendi G, Petrachi T, Conte P, Horwitz EM, Campana D, Paolucci P, Dominici M. A novel anti-GD2/4-1BB chimeric antigen receptor triggers neuroblastoma cell killing. Oncotarget. 2015;6(28):24884–24894. doi: 10.18632/oncotarget.4670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Heczey A, Courtney AN, Montalbano A, Robinson S, Liu K, Li M, Ghatwai N, Dakhova O, Liu B, Raveh-Sadka T, Chauvin-Fleurence CN, Xu X, Ngai H, Di Pierro EJ, Savoldo B, Dotti G, Metelitsa LS. Anti-GD2 CAR-NKT cells in patients with relapsed or refractory neuroblastoma: An interim analysis. Nature Medicine. 2020;26(11):1686–1690. doi: 10.1038/s41591-020-1074-2. [DOI] [PubMed] [Google Scholar]
- 157.Majzner RG, Ramakrishna S, Yeom KW, Patel S, Chinnasamy H, Schultz LM, Richards RM, Jiang L, Barsan V, Mancusi R, Geraghty AC, Good Z, Mochizuki AY, Gillespie SM, Toland AMS, Mahdi J, Reschke A, Nie EH, Chau IJ, Monje M. GD2-CAR T cell therapy for H3K27M-mutated diffuse midline gliomas. Nature. 2022;603(7903):934–941. doi: 10.1038/s41586-022-04489-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Thomas, A., Sumughan, S., Dellacecca, E. R., Shivde, R. S., Lancki, N., Mukhatayev, Z., Vaca, C. C., Han, F., Barse, L., Henning, S. W., Zamora-Pineda, J., Akhtar, S., Gupta, N., Zahid, J. O., Zack, S. R., Ramesh, P., Jaishankar, D., Lo, A. S., Moss, J., & Le Poole, I. C. (2021). Benign tumors in TSC are amenable to treatment by GD3 CAR T cells in mice. JCI. Insight, 6(22). 10.1172/jci.insight.152014 [DOI] [PMC free article] [PubMed]