Abstract
Giulia Muraca and colleagues argue that Canada’s high rates of maternal and neonatal trauma following operative vaginal delivery warrant urgent recognition, transparency, and action
Operative vaginal deliveries—forceps and vacuum assisted deliveries—are recommended as safe, acceptable alternatives to caesarean delivery for women in the second stage of labour when descent of the fetal head is arrested, there is imminent risk to the baby, or there are conditions that contraindicate pushing (expulsive) efforts.1 2 3 Although available data on maternal and neonatal mortality and morbidity show no clear advantage of operative vaginal delivery over caesarean delivery, such comparisons often fail to recognise the impact of maternal trauma, the most common injury associated with operative vaginal delivery.3 This is particularly pertinent in Canada, which has the highest rate of maternal trauma after operative vaginal deliveries among high income countries (fig 1).4
Fig 1.
Rate of obstetric anal sphincter injury from operative vaginal deliveries (forceps and vacuum assisted combined) in 24 Organisation for Economic Cooperation and Development (OECD) countries, 20194 *OECD=average among the 24 OECD countries
Each year, more than 35 000 singleton infants are born after attempted operative vaginal delivery in Canada. One in four (25.3%) attempted forceps deliveries and one in eight (13.2%) attempted vacuum deliveries result in maternal (obstetric) trauma, most commonly obstetric anal sphincter injury.5 Additionally, severe neonatal trauma occurs in one in 105 (9.6/1000) infants following attempted forceps or vacuum birth, with brachial plexus injury the most common trauma and neonatal death the most serious adverse outcome.5 6
Initiatives to decrease caesarean deliveries in North America that include scaling up training and use of operative vaginal deliveries need to acknowledge the serious safety concerns related to operative vaginal deliveries and ensure that women are informed of the risks of forceps, vacuum, and second stage caesarean delivery. The obstetric community should focus on reducing the high rates of trauma in Canada and shift the narrative around mode of delivery away from aiming to reduce caesarean delivery rates and towards transparent, evidence based, patient centred care and safe, positive birth experiences.
Reasons behind Canada’s statistics
The rates of obstetric anal sphincter injury in Canada are almost three times higher than in the UK, which has rates close to the average for countries in the Organisation for Economic Cooperation and Development (fig 1).4 Although differences in coding practices and data reporting between countries may have affected these comparisons, with under-reporting of obstetric trauma likely in some countries, estimates of maternal trauma rates in Canada have been repeatedly shown to be accurate.7 8 9 Differing practice with regard to use of forceps and episiotomy (figs 2 and 3), training, and safety initiatives are all likely to have a role (box 1).
Fig 2.

Rate of operative vaginal delivery by instrument among nulliparous women5 10 11 12 13 14 15
Fig 3.
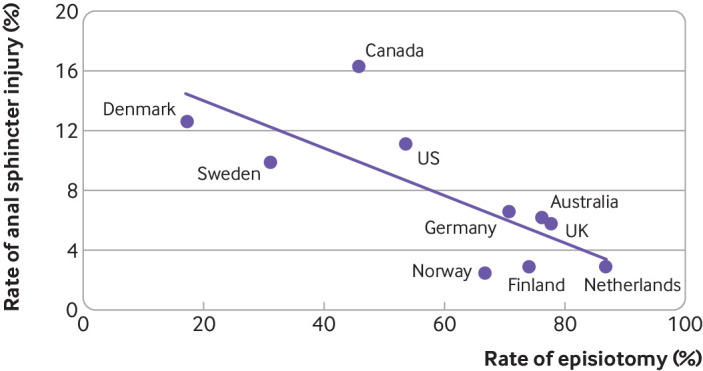
Correlation between rates of episiotomy and obstetric anal sphincter injury among operative vaginal deliveries in OECD countries5 10 11 12 13 14 15 (Pearson’s correlation coefficient=0.76; P=0.01). Data on episiotomy rate among operative vaginal deliveries in Ireland were not available
Box 1. Factors contributing to Canada’s high rate of obstetric anal sphincter injury .
Relatively high rates of forceps delivery—Rates of obstetric anal sphincter injury are higher with forceps delivery than with vacuum delivery,16 17 and Canada uses forceps more often than many other countries5 (5.1% v 2.5% in Norway among nulliparous women). Some European countries have abandoned forceps altogether,12 and only Australia, Ireland, and the UK have higher rates of use (fig 2).
Relatively low rates of episiotomy—Accumulating evidence supports the routine use of mediolateral episiotomy (with an incision angle of 60°) in operative vaginal delivery to reduce the risk of obstetric anal sphincter injury, particularly with forceps and among nulliparous women.18 However, no adequately powered randomised trial has examined this, and recommendations surrounding mediolateral episiotomy in operative vaginal delivery vary.2 14 19 20 21 For example, European and Australian guidelines recommend mediolateral episiotomy for operative vaginal delivery in women having their first vaginal birth,19 20 whereas Canadian guidelines recommend restricted use of mediolateral episiotomy.2 Large differences in episiotomy rates between countries parallel these diverse recommendations22 23; in 2020, reported rates of episiotomy were 90% with forceps and 50-60% with vacuum in the UK,14 compared with 65% and 38%, respectively, in Canada in 2018 (fig 3).24
Decline in training opportunities—Diminishing expertise in operative vaginal delivery may be contributing to the high injury rates. Canadian studies show that maternal and neonatal trauma have increased as use of operative vaginal delivery has declined.25 However, studies that attempt to assess practitioner skill using proxy measures, such as procedure volume or years in practice, have not shown an association with maternal or neonatal trauma.26 27 28 29 A detailed report6 on the safety of operative vaginal delivery during 2013-19 showed that several hospitals offering the highest level of obstetric care in Canada had high rates of maternal and severe neonatal trauma, even after adjustment for differences in case mix and irrespective of how many forceps or vacuum deliveries were performed each year3; however, practitioner level information was not available.
Lack of efforts to reduce injury—Unlike many other countries, Canada has had no national initiative aimed at reducing maternal injury.30 31 32 For example, in the UK the Royal College of Obstetricians and Gynaecologists and Royal College of Midwives introduced a “care bundle” to reduce injury, comprising antenatal discussion about obstetric anal sphincter injury, manual perineal protection, mediolateral episiotomy, and systematic examination of the perineum.30 A similar campaign was launched by Women’s Healthcare Australasia.31
Does evidence support increased use of operative vaginal deliveries?
Although no randomised trials have compared outcomes from operative vaginal deliveries and second stage caesarean deliveries,33 population based, observational studies in Canada and the United States have shown that caesarean delivery in the second stage of labour is associated with higher rates of neonatal respiratory morbidity and maternal infection than operative vaginal delivery.34 35 36 37 Composite severe maternal morbidity and mortality rates (which do not include maternal trauma) vary by instrument, with lower rates among women having vacuum deliveries and similar rates among women with forceps or caesarean deliveries. Rates of severe perinatal morbidity and mortality in Canada are higher after operative vaginal delivery than caesarean delivery performed for arrest in labour but not for fetal distress.34 Although several demographic and clinical factors were controlled for in the adjusted estimates, important clinical features were not captured (eg, fetal head flexion, asynclitism, moulding, and caput). In addition, indicators of patient preference and practitioner skill, important factors in deciding the delivery method, were not available.
Evidence on trauma is clearer. Operative vaginal deliveries are associated with high rates of severe maternal and neonatal trauma, most notably obstetric anal sphincter injury in mothers, and subaponeurotic haemorrhage and brachial plexus injury in neonates.5 36 38 39 40 The rate of obstetric anal sphincter injury in Canadian women is 2.8% for spontaneous vaginal deliveries,5 18-25% for forceps deliveries, and 11-16% for vacuum delivery, depending on indication and pelvic station.34 Adjusted rates of severe neonatal trauma are fourfold higher for operative vaginal deliveries than for caesarean deliveries. Although the absolute rates of severe neonatal trauma are low (0.96% with forceps and vacuum, 0.2% with second stage caesarean delivery),5 34 rates of maternal and severe neonatal trauma with operative vaginal delivery are increasing in Canada, especially with forceps delivery.25 40
The long term effects of each delivery option also need to be considered. A primary caesarean delivery carries a 0.7-1.5% risk of developing placenta previa, a 0.3% risk of placenta accreta, and 0.3% risk of uterine rupture in a subsequent pregnancy, and these risks increase with increasing numbers of previous caesarean deliveries (table 1).41 Morbidity associated with placenta accreta can be severe, with high rates of haemorrhage, hysterectomy, and intensive care unit admission.41
Table 1.
| No of previous caesarean deliveries | Placenta previa | Placenta accreta | Uterine rupture | Hysterectomy | Wound infection | Wound dehiscence | Postpartum haemorrhage | Placental abruption | Surgical injury |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 0.7-1.5 | 0.3 | 0.3 | 0.1-0.7 | 0.9-1.5 | 0.1 | 0 | 1.0-1.4 | 0.1 |
| 2 | 1.1-2.0 | 0.6 | 0.6 | 0.1-0.9 | 0.4-1.5 | 0.2-0.3 | 0.1 | 1.0-1.3 | 0.3 |
| 3 | 1.0-2.3 | 2.1 | 0.8 | 0.4-2.4 | 1.3-1.6 | 0.2-0.8 | 1.9 | 1.1-1.5 | 1.2 |
| 4 | 2.3-4.2 | 2.3 | 0.6 | 1.4-3.5 | 3.5 | 0-1.4 | 1.4 | — | 1.9 |
| ≥5 | 3.4 | 6.7 | 0.8 | 9.0 | 3.4 | 1.2 | — | — | 4.5 |
The long term consequences of operative vaginal deliveries are also considerable, albeit qualitatively different and less visible from the obstetric perspective. Obstetric anal sphincter injury is associated with an increased risk of dyspareunia, pelvic floor disorders, pelvic pain, and sexual dysfunction.17 44 45 46 Faecal and anal incontinence are direct complications of these injuries and can have devastating effects on social, psychological, and physical wellbeing.17 45 46 47 48 Reported rates of anal incontinence following repair of obstetric anal sphincter injury are 15-61% (mean 39%),17 and these increase from 31% at 3-6 months to 69% at 20 years after delivery.46 47 A prospective cohort study of 6760 Swedish women with two vaginal deliveries found the rate of faecal incontinence 20 years after delivery was 23.7% among women with one obstetric anal sphincter injury and 36.1% among those with two.47
A study of women’s future pregnancy and mode of delivery experience after an operative vaginal delivery or second stage caesarean delivery found women in both groups commonly avoided further pregnancy because of fear of childbirth (51% operative vaginal delivery, 42% caesarean delivery). Women with a previous operative vaginal delivery were two to three times more likely to have a vaginal delivery than women who had a caesarean delivery.49 However, the study did not identify caesarean deliveries that resulted from a failed operative vaginal delivery attempt and combined forceps and vacuum delivery into one category, making interpretation challenging. Studies evaluating the association between second stage caesarean delivery and preterm birth in a subsequent pregnancy have the same methodological flaws.50 51 52 Reassuringly, neurodevelopmental and cognitive outcomes in children and young adults seem to be similar for operative vaginal and second stage caesarean delivery.53 54 55 56 57
Supporting patient centred, evidence informed choice
The most recent Canadian clinical practice guideline on operative vaginal delivery2 asserts that “Overall, in carefully selected circumstances, both vacuum and forceps are associated with relatively low rates of serious morbidity and mortality in both mother and baby.”2 The high incidence of maternal trauma associated with such deliveries is obscured by aggregating spontaneous and operative vaginal deliveries: the guideline mentions an incidence of obstetric anal sphincter injury “between 4% and 6.6% of all vaginal births, including those by [operative delivery].”2 The failure to acknowledge the high rate of injury associated with operative vaginal deliveries (eg, 25.3% rate of maternal trauma following forceps delivery) signals a disregard for transparency and could limit the ability of patients to make evidence informed decisions about childbirth.
Evidence from Canadian hospitals shows that informed consent practices related to operative vaginal deliveries reflect this tendency to under-report the associated risks.58 59 A study examining consenting practices documented in medical records of women who had operative vaginal deliveries at two tertiary care centres in Ontario, Canada, in 2019, showed that neonatal and maternal risks were not mentioned for 68% of forceps deliveries and 92% of vacuum deliveries.58 A Canadian survey of patient satisfaction with the informed consent procedure during labour also found that women with operative vaginal delivery had more than fourfold lower satisfaction rates compared with those who had had a caesarean delivery.59
The benefits and risks associated with all delivery alternatives need to be carefully communicated to pregnant women, ideally in the antenatal period,60 with current, empirically derived measures that reflect the risks women encounter in routine obstetric practice. The UK Royal College of Obstetricians and Gynaecologists provides advice for clinicians on obtaining consent for operative vaginal delivery that can be easily tailored to reflect local contexts.61 Evidence based decision aids regarding delivery options developed in consultation with patients can help to facilitate informed decisions that reflect patient values.62
Strategies to reduce rates of obstetric trauma
Preventing operative intervention in second stage of labour
Efforts should be directed towards safely avoiding all operative delivery (whether vaginal or caesarean) among women who choose to attempt a vaginal delivery. Strategies shown to reduce the need for operative delivery include providing continuous support for women during labour63 and encouraging women to adopt specific positions in the second stage of labour (upright or lateral for women not using epidural64 and recumbent in women using epidural).65 66 Evidence is conflicting on other strategies, including delayed pushing,67 68 higher thresholds of prolonged labour,69 70 manual rotation of the fetal occiput for malposition,71 and intrapartum ultrasonography.72 73 74
National quality improvement initiatives
National quality improvement campaigns in high income settings have been shown to reduce obstetric anal sphincter injuries.30 32The campaigns use multiple approaches or “care bundles,” including antenatal discussion about risk of obstetric anal sphincter injury and personal risk factors, manual perineal protection during childbirth (with consent), mediolateral episiotomy (when indicated and with consent), and systematic examination for perineal trauma by an experienced clinician following vaginal births.
These protective measures should be implemented for all vaginal deliveries. Although the incidence of obstetric anal sphincter injury after spontaneous vaginal deliveries is lower than after operative delivery (2.8% in Canada, 2013-19), spontaneous deliveries account for most (89%) vaginal deliveries and more than half of obstetric anal sphincter injuries in Canada.5 Care bundles have been shown to reduce anal injury rates among women having spontaneous vaginal deliveries by 25%.30
Improve training in forceps and vacuum delivery
Before initiating programmes to increase training in forceps and vacuum delivery, it is necessary to identify skilled practitioners (ie, those with documented low rates of trauma with operative vaginal delivery on chart review) to act as instructors. Competency should be demonstrated before unsupervised operative vaginal deliveries can be performed, and maternity care providers should be required to audit their performance regularly.75
High fidelity simulation training could provide a safe method of gaining experience. A systematic review76 investigating the effect of simulated operative vaginal delivery training concluded that it improved physician knowledge, comfort, and skill as well as patient outcomes. However, only two of the eight studies included in the review assessed patient outcomes. One of these studies found very high, albeit reduced, rates of obstetric anal sphincter injury with forceps (32% for deliveries by residents and 28% for attending physicians),26 while the other combined outcomes from vacuum and forceps deliveries, making it difficult to interpret.77 Further study on the effect of simulation training on patient outcomes is warranted before larger scale investment in this approach.
Doing better
The characterisation of operative vaginal deliveries as safe procedures given the consistently high rates of trauma in Canada is misleading. Efforts to reduce the rates of caesarean delivery and associated risks must be balanced against all the potential harms of alternative interventions. Lower rates of caesarean delivery are not synonymous with better care. Although maternity care services in Canada generally conform to the highest standards, there is an urgent need for recognition, transparency, and action regarding maternal and neonatal trauma associated with operative vaginal delivery. Maternal trauma can no longer be regarded as a minor, acceptable, or unavoidable outcome of childbirth; this belief contributes to the stigma experienced by women with these injuries and disregards the patient perspective on what constitutes morbidity.
Key messages.
Maternal and neonatal trauma rates from operative vaginal delivery are substantially higher in Canada than in other high income countries
Despite high rates, maternal trauma is not properly accounted for in data on safety of operative delivery methods
Counselling about delivery options should take place antenatally and be informed by guidelines that use balanced, up-to-date evidence and support patient autonomy
Efforts to reduce rates of trauma should be accompanied by the promotion of informed, respectful care to support safe and positive birth experiences
Acknowledgments
SL is supported by a scholar award from the Michael Smith Foundation for Health Research. KSJ is supported by an investigator award from the British Columbia Children’s Hospital Research Institute.
Contributors and sources: GMM, SL, and KSJ are perinatal epidemiologists who have investigated the safety of forceps and vacuum deliveries for over a decade. RD and RG are obstetrician/gynaecologists specialising in maternal-fetal medicine and urogynaecology, respectively; LER is a patient and advocate for issues related to maternal trauma; and PC is the executive director of Birth Trauma Canada, an organisation supporting people affected by all forms of trauma resulting from childbirth. All authors contributed to the conceptualisation of the article. GMM wrote the first draft and all other authors offered critical comments. All authors contributed extensively to further refining, editing, and proofing, and have approved the final version of the article. GMM is the guarantor.
Patient and public involvement: Two of the authors are members of patient groups that are the focus of this article. One experienced maternal trauma following a forceps delivery in 2016. The other is the executive director of Birth Trauma Canada, which represents the voices of numerous women, many of whom seek support anonymously because of the isolating and stigmatising nature of their injuries.
Competing interests: We have read and understood the BMJ policy on declaration of interests and have no interests to declare.
References
- 1. Murphy DJ. Operative vaginal delivery. Best Pract Res Clin Obstet Gynaecol 2019;56:1-2. 10.1016/j.bpobgyn.2019.02.003 [DOI] [PubMed] [Google Scholar]
- 2. Hobson S, Cassell K, Windrim R, Cargill Y. No 381. Assisted vaginal birth. J Obstet Gynaecol Can 2019;41:870-82. 10.1016/j.jogc.2018.10.020 [DOI] [PubMed] [Google Scholar]
- 3. Caughey AB, Cahill AG, Guise JM, Rouse DJ, American College of Obstetricians and Gynecologists (College) Society for Maternal-Fetal Medicine . Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol 2014;210:179-93. 10.1016/j.ajog.2014.01.026 [DOI] [PubMed] [Google Scholar]
- 4. Organization for Economic Cooperation and Development (OECD) . Obstetric trauma, vaginal delivery with and without instrument, 2019 (or nearest year) and 2020. Health at a Glance 2021. OECD Publishing, 2021. https://www.oecd-ilibrary.org/social-issues-migration-health/obstetric-trauma-vaginal-delivery-with-and-without-instrument-2019-or-nearest-year-and-2020_28659be4-en [Google Scholar]
- 5. Muraca GM, Boutin A, Razaz N, et al. Maternal and neonatal trauma following operative vaginal delivery. CMAJ 2022;194:E1-12. 10.1503/cmaj.210841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muraca GM, Boutin A, Cherian AM, et al. Attempted forceps and attempted vacuum delivery: maternal and neonatal trauma rates by province/territories, tier of obstetric service and hospital, Canada, April 2013 to March 2019. Report of the CIHR Team for Improving Perinatal Health Care Regionalization. University of British Columbia, 2021, https://med-fom-phsr-obgyn.sites.olt.ubc.ca/files/2022/01/OVDReportFINAL2021.pdf [Google Scholar]
- 7. Joseph KS, Fahey J, Canadian Perinatal Surveillance System . Validation of perinatal data in the Discharge Abstract Database of the Canadian Institute for Health Information. Chronic Dis Can 2009;29:96-100. 10.24095/hpcdp.29.3.01 [DOI] [PubMed] [Google Scholar]
- 8. Frosst G, Hutcheon J, Joseph KS, Kinniburgh B, Johnson C, Lee L. Validating the British Columbia Perinatal Data Registry: a chart re-abstraction study. BMC Pregnancy Childbirth 2015;15:123. 10.1186/s12884-015-0563-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dunn S, Lanes A, Sprague AE, et al. Data accuracy in the Ontario birth Registry: a chart re-abstraction study. BMC Health Serv Res 2019;19:1001. 10.1186/s12913-019-4825-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Friedman AM, Ananth CV, Prendergast E, D’Alton ME, Wright JD. Evaluation of third-degree and fourth-degree laceration rates as quality indicators. Obstet Gynecol 2015;125:927-37. 10.1097/AOG.0000000000000720 [DOI] [PubMed] [Google Scholar]
- 11. Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2017. Natl Vital Stat Rep 2018;67:1-50. [PubMed] [Google Scholar]
- 12. Seijmonsbergen-Schermers AE, van den Akker T, Rydahl E, et al. Variations in use of childbirth interventions in 13 high-income countries: a multinational cross-sectional study. PLoS Med 2020;17:e1003103. 10.1371/journal.pmed.1003103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Blondel B, Alexander S, Bjarnadóttir RI, et al. Euro-Peristat Scientific Committee . Variations in rates of severe perineal tears and episiotomies in 20 European countries: a study based on routine national data in Euro-Peristat Project. Acta Obstet Gynecol Scand 2016;95:746-54. 10.1111/aogs.12894 [DOI] [PubMed] [Google Scholar]
- 14. Murphy DJ, Strachan BK, Bahl R, Royal College of Obstetricians and Gynaecologists . Assisted vaginal birth: Green-top guideline No. 26. BJOG 2020;127:e70-112. 10.1111/1471-0528.16336 [DOI] [PubMed] [Google Scholar]
- 15.Australian Institute of Health and Welfare. Perineal status: Australia's mothers and babies Australia. 2023. https://www.aihw.gov.au/reports/mothers-babies/australias-mothers-babies/contents/labour-and-birth/perineal-status
- 16. Verma GL, Spalding JJ, Wilkinson MD, Hofmeyr GJ, Vannevel V, O’Mahony F. Instruments for assisted vaginal birth. Cochrane Database Syst Rev 2021;9:CD005455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harvey MA, Pierce M, Alter JE, et al. Society of Obstetricians and Gynaecologists of Canada . Obstetrical anal sphincter injuries (OASIS): prevention, recognition, and repair. J Obstet Gynaecol Can 2015;37:1131-48. 10.1016/S1701-2163(16)30081-0 [DOI] [PubMed] [Google Scholar]
- 18. Okeahialam NA, Wong KW, Jha S, Sultan AH, Thakar R. Mediolateral/lateral episiotomy with operative vaginal delivery and the risk reduction of obstetric anal sphincter injury (OASI): a systematic review and meta-analysis. Int Urogynecol J 2022;33:1393-405. 10.1007/s00192-022-05145-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Laine K, Yli BM, Cole V, et al. European guidelines on perinatal care- peripartum care episiotomy. J Matern Fetal Neonatal Med 2022;35:8797-802. 10.1080/14767058.2021.2005022 [DOI] [PubMed] [Google Scholar]
- 20.Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Instrumental vaginal birth Victoria, Australia. 2020. https://ranzcog.edu.au/wp-content/uploads/2022/05/Instrumental-vaginal-birth.pdf
- 21.Kessler J, Frostad KIJ, Sivertsen H. Operativ vaginal forløsning. Norwegian Gynecological Association, 2023. https://www.legeforeningen.no/foreningsledd/fagmed/norsk-gynekologisk-forening/veiledere/veileder-i-fodselshjelp/operativ-vaginal-forlosning/
- 22. Ray CL, Audibert F, Cabrol D, Goffinet F. [Perineal consequences according to obstetric practices: A comparative study here and elsewhere, Canada and France]. J Obstet Gynaecol Can 2009;31:1035. 10.1016/S1701-2163(16)34348-1 [DOI] [PubMed] [Google Scholar]
- 23. Goldberg J, Hyslop T, Tolosa JE, Sultana C. Racial differences in severe perineal lacerations after vaginal delivery. Am J Obstet Gynecol 2003;188:1063-7. 10.1067/mob.2003.251 [DOI] [PubMed] [Google Scholar]
- 24. Muraca GM, Liu S, Sabr Y, et al. Episiotomy use among vaginal deliveries and the association with anal sphincter injury: a population-based retrospective cohort study. CMAJ 2019;191:E1149-58. 10.1503/cmaj.190366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Muraca GM, Lisonkova S, Skoll A, et al. Ecological association between operative vaginal delivery and obstetric and birth trauma. CMAJ 2018;190:E734-41. 10.1503/cmaj.171076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gossett DR, Gilchrist-Scott D, Wayne DB, Gerber SE. Simulation training for forceps-assisted vaginal delivery and rates of maternal perineal trauma. Obstet Gynecol 2016;128:429-35. 10.1097/AOG.0000000000001533 [DOI] [PubMed] [Google Scholar]
- 27. Crosby DA, Sarangapani A, Simpson A, Windrim R, Satkunaratnam A, Higgins MF. An international assessment of trainee experience, confidence, and comfort in operative vaginal delivery. Ir J Med Sci 2017;186:715-21. 10.1007/s11845-017-1593-0 [DOI] [PubMed] [Google Scholar]
- 28. Powell J, Gilo N, Foote M, Gil K, Lavin JP. Vacuum and forceps training in residency: experience and self-reported competency. J Perinatol 2007;27:343-6. 10.1038/sj.jp.7211734 [DOI] [PubMed] [Google Scholar]
- 29. Miller ES, Barber EL, McDonald KD, Gossett DR. Association between obstetrician forceps volume and maternal and neonatal outcomes. Obstet Gynecol 2014;123:248-54. 10.1097/AOG.0000000000000096 [DOI] [PubMed] [Google Scholar]
- 30. Gurol-Urganci I, Bidwell P, Sevdalis N, et al. Impact of a quality improvement project to reduce the rate of obstetric anal sphincter injury: a multicentre study with a stepped-wedge design. BJOG 2021;128:584-92. 10.1111/1471-0528.16396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Women’s Healthcare Australasia. The how to guide: WHA CEC perineal protection bundle. 2019. https://women.wcha.asn.au/wp-content/uploads/sites/3/2022/04/wha_national_collaborative_how_to_guide_21.1.20.pdf
- 32. Hals E, Øian P, Pirhonen T, et al. A multicenter interventional program to reduce the incidence of anal sphincter tears. Obstet Gynecol 2010;116:901-8. 10.1097/AOG.0b013e3181eda77a [DOI] [PubMed] [Google Scholar]
- 33. Murphy DJ. Operative vaginal delivery. Best Pract Res Clin Obstet Gynaecol 2019;56:1-2. 10.1016/j.bpobgyn.2019.02.003 [DOI] [PubMed] [Google Scholar]
- 34. Muraca GM, Sabr Y, Lisonkova S, et al. Morbidity and mortality associated with forceps and vacuum delivery at outlet, low, and midpelvic station. J Obstet Gynaecol Can 2019;41:327-37. 10.1016/j.jogc.2018.06.018 [DOI] [PubMed] [Google Scholar]
- 35. Halscott TL, Reddy UM, Landy HJ, et al. Maternal and neonatal outcomes by attempted mode of operative delivery from a low station in the second stage of labor. Obstet Gynecol 2015;126:1265-72. 10.1097/AOG.0000000000001156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bailit JL, Grobman WA, Rice MM, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network . Evaluation of delivery options for second-stage events. Am J Obstet Gynecol 2016;214:638.e1-10. 10.1016/j.ajog.2015.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Muraca GM, Skoll A, Lisonkova S, et al. Perinatal and maternal morbidity and mortality among term singletons following midcavity operative vaginal delivery versus caesarean delivery. BJOG 2018;125:693-702. 10.1111/1471-0528.14820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Panelli DM, Leonard SA, Joudi N, et al. Severe maternal and neonatal morbidity after attempted operative vaginal delivery. Am J Obstet Gynecol MFM 2021;3:100339. 10.1016/j.ajogmf.2021.100339 [DOI] [PubMed] [Google Scholar]
- 39. Frenette P, Crawford S, Schulz J, Ospina MB. Impact of episiotomy during operative vaginal delivery on obstetrical anal sphincter injuries. J Obstet Gynaecol Can 2019;41:1734-41. 10.1016/j.jogc.2019.02.016 [DOI] [PubMed] [Google Scholar]
- 40. Gyhagen M, Ellström Engh M, Husslein H, et al. Temporal trends in obstetric anal sphincter injury from the first vaginal delivery in Austria, Canada, Norway, and Sweden. Acta Obstet Gynecol Scand 2021;100:1969-76. 10.1111/aogs.14244 [DOI] [PubMed] [Google Scholar]
- 41. Marshall NE, Fu R, Guise JM. Impact of multiple cesarean deliveries on maternal morbidity: a systematic review. Am J Obstet Gynecol 2011;205:262.e1-8. 10.1016/j.ajog.2011.06.035 [DOI] [PubMed] [Google Scholar]
- 42. Guise JM, Eden K, Emeis C, et al. Vaginal birth after cesarean: new insights. Evid Rep Technol Assess (Full Rep) 2010;•••:1-397. [PMC free article] [PubMed] [Google Scholar]
- 43. Silver RM, Landon MB, Rouse DJ, et al. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network . Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol 2006;107:1226-32. 10.1097/01.AOG.0000219750.79480.84 [DOI] [PubMed] [Google Scholar]
- 44. Sultan AH. Obstetrical perineal injury and anal incontinence. Clin Risk 1999;5:193-6 10.1177/135626229900500601. [DOI] [Google Scholar]
- 45. Handa VL, Danielsen BH, Gilbert WM. Obstetric anal sphincter lacerations. Obstet Gynecol 2001;98:225-30. [DOI] [PubMed] [Google Scholar]
- 46. Wegnelius G, Hammarström M. Complete rupture of anal sphincter in primiparas: long-term effects and subsequent delivery. Acta Obstet Gynecol Scand 2011;90:258-63. 10.1111/j.1600-0412.2010.01037.x [DOI] [PubMed] [Google Scholar]
- 47. Nilsson IEK, Åkervall S, Molin M, Milsom I, Gyhagen M. Symptoms of fecal incontinence two decades after no, one, or two obstetrical anal sphincter injuries. Am J Obstet Gynecol 2021;224:276.e1-23. 10.1016/j.ajog.2020.08.051 [DOI] [PubMed] [Google Scholar]
- 48. Nilsson IE, Åkervall S, Molin M, et al. Severity and impact of accidental bowel leakage two decades after no, one, or two sphincter injuries. Am J Obstet Gynecol 2022. [DOI] [PubMed] [Google Scholar]
- 49. Bahl R, Strachan B, Murphy DJ. Outcome of subsequent pregnancy three years after previous operative delivery in the second stage of labour: cohort study. BMJ 2004;328:311. 10.1136/bmj.37942.546076.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wang M, Kirby A, Gibbs E, Gidaszewski B, Khajehei M, Chua SC. Risk of preterm birth in the subsequent pregnancy following caesarean section at full cervical dilatation compared with mid-cavity instrumental delivery. Aust N Z J Obstet Gynaecol 2020;60:382-8. 10.1111/ajo.13058 [DOI] [PubMed] [Google Scholar]
- 51. Williams C, Fong R, Murray SM, Stock SJ. Caesarean birth and risk of subsequent preterm birth: a retrospective cohort study. BJOG 2021;128:1020-8. 10.1111/1471-0528.16566 [DOI] [PubMed] [Google Scholar]
- 52. Van Winsen KD, Savvidou MD, Steer PJ. The effect of mode of delivery and duration of labour on subsequent pregnancy outcomes: a retrospective cohort study. BJOG 2021;128:2132-9. 10.1111/1471-0528.16864 [DOI] [PubMed] [Google Scholar]
- 53. Bahl R, Patel RR, Swingler R, Ellis M, Murphy DJ. Neurodevelopmental outcome at 5 years after operative delivery in the second stage of labor: a cohort study. Am J Obstet Gynecol 2007;197:147.e1-6. 10.1016/j.ajog.2007.03.034 [DOI] [PubMed] [Google Scholar]
- 54. Hsieh DC, Smithers LG, Black M, et al. Implications of vaginal instrumental delivery for children’s school achievement: A population-based linked administrative data study. Aust N Z J Obstet Gynaecol 2019;59:677-83. 10.1111/ajo.12952 [DOI] [PubMed] [Google Scholar]
- 55. Ayala NK, Schlichting LE, Kole MB, et al. Operative vaginal delivery and third grade educational outcomes. Am J Obstet Gynecol MFM 2020;2:100221. 10.1016/j.ajogmf.2020.100221 [DOI] [PubMed] [Google Scholar]
- 56. Ngan HY, Miu P, Ko L, Ma HK. Long-term neurological sequelae following vacuum extractor delivery. Aust N Z J Obstet Gynaecol 1990;30:111-4. 10.1111/j.1479-828X.1990.tb03237.x [DOI] [PubMed] [Google Scholar]
- 57. Ahlberg M, Ekéus C, Hjern A. Birth by vacuum extraction delivery and school performance at 16 years of age. Am J Obstet Gynecol 2014;210:361.e1-8. 10.1016/j.ajog.2013.11.015 [DOI] [PubMed] [Google Scholar]
- 58. Sheinis M, Zhu J, Hobson S, et al. Consent practices for assisted vaginal births (AVB) at two tertiary care hospitals: a retrospective review of physician documentation. J Obstet Gynaecol Can 2023;45:496-502. 10.1016/j.jogc.2023.04.021 [DOI] [PubMed] [Google Scholar]
- 59. Levy KS, Smith MK, Lacroix M, Yudin MH. Patient satisfaction with informed consent for cesarean and operative vaginal delivery. J Obstet Gynaecol Can 2022;44:785-90. 10.1016/j.jogc.2022.03.010 [DOI] [PubMed] [Google Scholar]
- 60. Smith MK, Levy KS, Yudin MH. Informed consent during labour: patient and physician perspectives. J Obstet Gynaecol Can 2018;40:614-7. 10.1016/j.jogc.2017.12.013 [DOI] [PubMed] [Google Scholar]
- 61.Royal College of Obstetricians and Gynaecologists. Operative vaginal delivery (consent advice No 11) 2010. https://www.rcog.org.uk/media/wpbhtluu/ca11-15072010.pdf
- 62. Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2017;4:CD001431. 10.1002/14651858.CD001431.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev 2017;7:CD003766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gupta JK, Hofmeyr GJ, Shehmar M. Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database Syst Rev 2012;(5):CD002006. [DOI] [PubMed] [Google Scholar]
- 65. Epidural and Position Trial Collaborative Group . Upright versus lying down position in second stage of labour in nulliparous women with low dose epidural: BUMPES randomised controlled trial. BMJ 2017;359:j4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Walker KF, Kibuka M, Thornton JG, Jones NW. Maternal position in the second stage of labour for women with epidural anaesthesia. Cochrane Database Syst Rev 2018;11:CD008070. 10.1002/14651858.CD008070.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Roberts CL, Torvaldsen S, Cameron CA, Olive E. Delayed versus early pushing in women with epidural analgesia: a systematic review and meta-analysis. BJOG 2004;111:1333-40. 10.1111/j.1471-0528.2004.00282.x [DOI] [PubMed] [Google Scholar]
- 68. Tuuli MG, Frey HA, Odibo AO, Macones GA, Cahill AG. Immediate compared with delayed pushing in the second stage of labor: a systematic review and meta-analysis. Obstet Gynecol 2012;120:660-8. 10.1097/AOG.0b013e3182639fae [DOI] [PubMed] [Google Scholar]
- 69. Wood S, Skiffington J, Brant R, et al. REDUCED Trial Team . The REDUCED trial: a cluster randomized trial for REDucing the utilization of CEsarean delivery for dystocia. Am J Obstet Gynecol 2023;228(5S):S1095-103. 10.1016/j.ajog.2022.10.038 [DOI] [PubMed] [Google Scholar]
- 70. Main EK, Chang SC, Cape V, Sakowski C, Smith H, Vasher J. Safety assessment of a large-scale improvement collaborative to reduce nulliparous cesarean delivery rates. Obstet Gynecol 2019;133:613-23. 10.1097/AOG.0000000000003109 [DOI] [PubMed] [Google Scholar]
- 71. Bertholdt C, Morel O, Zuily S, Ambroise-Grandjean G. Manual rotation of occiput posterior or transverse positions: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol 2022;226:781-93. 10.1016/j.ajog.2021.11.033 [DOI] [PubMed] [Google Scholar]
- 72. Ramphul M, Ooi PV, Burke G, et al. Instrumental delivery and ultrasound : a multicentre randomised controlled trial of ultrasound assessment of the fetal head position versus standard care as an approach to prevent morbidity at instrumental delivery. BJOG 2014;121:1029-38. 10.1111/1471-0528.12810 [DOI] [PubMed] [Google Scholar]
- 73. Popowski T, Porcher R, Fort J, Javoise S, Rozenberg P. Influence of ultrasound determination of fetal head position on mode of delivery: a pragmatic randomized trial. Ultrasound Obstet Gynecol 2015;46:520-5. 10.1002/uog.14785 [DOI] [PubMed] [Google Scholar]
- 74. Nassr AA, Hessami K, Berghella V, et al. Angle of progression measured using transperineal ultrasound for prediction of uncomplicated operative vaginal delivery: systematic review and meta-analysis. Ultrasound Obstet Gynecol 2022;60:338-45. 10.1002/uog.24886 [DOI] [PubMed] [Google Scholar]
- 75. Lane S, Weeks A, Scholefield H, Alfirevic Z. Monitoring obstetricians’ performance with statistical process control charts. BJOG 2007;114:614-8. 10.1111/j.1471-0528.2007.01270.x [DOI] [PubMed] [Google Scholar]
- 76. Bligard KH, Lipsey KL, Young OM. Simulation training for operative vaginal delivery among obstetrics and gynecology residents: a systematic review. Obstet Gynecol 2019;134(Suppl 1):16S-21S. 10.1097/AOG.0000000000003431 [DOI] [PubMed] [Google Scholar]
- 77. Cheong YC, Abdullahi H, Lashen H, Fairlie FM. Can formal education and training improve the outcome of instrumental delivery? Eur J Obstet Gynecol Reprod Biol 2004;113:139-44. 10.1016/S0301-2115(03)00340-3 [DOI] [PubMed] [Google Scholar]



