Abstract
Lecanemab, a novel amyloid-sequestering agent, recently received accelerated Food and Drug Administration approval for the treatment of mild dementia due to Alzheimer disease (AD) and mild cognitive impairment (MCI). Approval was based on a large phase 3 trial, Clarity, which demonstrated reductions in amyloid plaque burden and cognitive decline with lecanemab. Three major concerns should give us pause before adopting this medication: Its beneficial effects are small, its harms are substantial, and its potential costs are unprecedented. Although lecanemab has a clear and statistically significant effect on cognition, its effect size is small and may not be clinically significant. The magnitude of lecanemab's cognitive effect is smaller than independent estimates of the minimally important clinical difference, implying that the effect may be imperceptible to a majority of patients and caregivers. Lecanemab's cognitive effects were numerically smaller than the effect of cholinesterase inhibitors and may be much smaller. The main argument in lecanemab's favor is that it may lead to greater cognitive benefit over time. Although plausible, there is a lack of evidence to support this conclusion. Lecanemab's harms are substantial. In Clarity, it caused symptomatic brain edema in 11% and symptomatic intracranial bleeding in 0.5% of participants. These estimates likely significantly underestimate these risks in general practice for 3 reasons: (1) Lecanemab likely interacts with other medications that increase bleeding, an effect minimized in Clarity. (2) The Clarity population is much younger than the real-world population with mild AD dementia and MCI (age 71 years vs 85 years) and bleeding risk increases with age. (3) Bleeding rates in trials are typically much lower than in clinical practice. Lecanemab's costs are unprecedented. Its proposed price of $26,500 is based on cost-effectiveness analyses with tenuous assumptions. However, even if cost-effective, it is likely to result in higher expenditures than any other medication. If its entire target population were treated, the aggregate medication expenditures would be $120 billion US dollars per year—more than is currently spent on all medications in Medicare Part D. Before adopting lecanemab, we need to know that lecanemab is not less effective, vastly more harmful, and 100× more costly than donepezil.
Dementia due to Alzheimer disease (AD) generates enormous burdens for patients, families, and society. For over a generation, the scientific community has sought effective AD treatments with uniformly disappointing results. The recent Clarity AD trial demonstrated statistically significant differences in cognitive decline among study participants with mild cognitive impairment (MCI) and mild AD dementia treated with the novel amyloid-sequestering agent lecanemab.1 Lecanemab substantially reduced brain amyloid plaque burden. Based on these data, the US Food and Drug Administration granted accelerated approval for lecanemab with an indication targeting MCI and mild AD dementia.2,3 While lecanemab has been hailed, particularly in the popular press, as a potential breakthrough, we must look carefully before we leap to adopting lecanemab for 3 reasons: Its beneficial effects are small, its harms are substantial, and its potential costs are unprecedented.
Lecanemab's Beneficial Effects Are Small
Numerous immunomodulatory amyloid-lowering agents were trialed previously. Before lecanemab, none demonstrated a clinically meaningful reduction in cognitive decline. Collectively, previous data identified a correlation between the magnitude of reduction in amyloid plaque burden and favorable cognitive effects. This effect, however, is minimal. In 1 analysis, for every 10% reduction in amyloid plaque burden, Mini-Mental State Examination scores fell by 0.09 points (30 point scale) less than in untreated patients.4,5 While lecanemab lowers amyloid burden more than previous trialed medications,6 generalizing from prior experience, a medication that completely eliminates amyloid is predicted to produce only small cognitive improvements.
This prediction is consistent with Clarity results—lecanemab's beneficial cognitive effect is statistically significant but clinically modest. Statistical significance means that sufficient statistical evidence exists to ensure that the difference between treatment and control groups is not due to random error (e.g., p < 0.05) and primarily reflects 2 factors—the magnitude of the clinical effect and the trial size. Clinical significance, instead, is a clinical judgment based on whether the magnitude of a given effect is meaningful to patients. As such, a statistically significant trial result does not necessarily imply a clinically meaningful effect. A simple exaggerated thought experiment illustrates this point. Imagine a new weight loss medication that was trialed in 2 million patients and 2 million controls and resulted in a 1 ounce of weight loss, on average. The result would be statistically significant (i.e., p < 0.05), but it is unlikely that patients would line up for this new medication. A commonly used metric to address the question of “is a given effect clinically meaningful?” is a benchmark called minimal clinically important difference (MCID). MCIDs are defined as the magnitude of the change in a potential trial outcome that correlates with a different quantity commonly considered meaningful, such as patient perception of benefit.
Clarity's primary outcome was a cognitive measure—change in the 18-point Clinical Dementia Rating-Sum of Boxes (CDR-SB) score. Lecanemab-treated patients had a mean 0.45 point smaller decline in CDR-SB scores over 18 months than the placebo control group, implying a 3-month to 4-month equivalent slowing of cognitive decline. Although this outcome exceeds the prespecified MCID used by the Clarity trial authors, it is substantially less than the MCID (0.98 for MCI and 1.63 for mild AD dementia at 1 year) that has been defined using real-world data and clinician-independent judgment about cognitive status.7-9 This implies that many, possibly most, patients and caregivers would not notice lecanemab's cognitive effects.
To contextualize lecanemab's effect, the observed difference on CDR-SB in Clarity is smaller than the effects of widely used cholinesterase inhibitors (e.g., donepezil), generally perceived to have small benefits for AD.10 In the subset of donepezil trials reporting CDR-SB, donepezil treatment resulted in a numerically larger effect on CDR-SB than lecanemab (0.53 vs 0.45). On other widely used cognitive measures, donepezil substantially outperformed lecanemab. For example, donepezil caused a 2.37-point slowing in Alzheimer Disease Assessment Scale-Cognitive subscale (ADAS-Cog) score decline at 6-month treatment intervals, whereas lecanemab reduced ADAS-Cog scores by 1.44 points at 18 months (with a smaller effect at 6 months).11
The long-term effects of lecanemab on cognition are unknown, and it is possible that lecanemab effects may increase over time beyond what was observed in Clarity. To the extent that amyloid deposits are important elements on the casual pathway of AD, lecanemab may prove to be a true disease-modifying medication, as it has a large effect on reducing brain amyloid in addition to its effect on other AD biomarkers. By contrast, cholinesterase inhibitors are commonly understood to improve cognition by altering neuronal transmission, not by effecting neurodegeneration per se.
Yet, even if lecanemab acts on the pathways giving rise to AD, this does guarantee that lecanemab will have a clinically meaningful effect. Numerous previous attempts at disease modification with antiamyloid therapies failed, many despite successfully and substantially reducing brain amyloid burden. These results imply that a medication substantially altering the biological pathways driving AD may not result in a clinically meaningful effect. A disease-modifying medication with a clinically meaningful effect should reduce the proportion of treated patients developing AD and slow transitions between AD stages. Although Clarity was a well-conducted study, it did not find clear evidence of such disease modification—lecamenab was not statistically significantly associated with a reduction in progression to later stages of AD. Even if lecanemab is eventually shown to have increasing cognitive benefits over time and even if these effects are shown to be due to true disease modification, lecanemab's effects would have to accumulate over a sustained interval before the average effect will be larger than the average cholinesterase inhibitor effect. While it is debatable whether lecanemab meets the threshold of clinical significance, it is hard to look at a medication with smaller cognitive effects than a cholinesterase inhibitor and conclude that it is a significant breakthrough.
Lecanemab's Harms Are Substantial and Likely Underestimated in Clarity
The small benefits of lecanemab must be weighed against potential harms. Lecanemab, like other amyloid-lowering agents, causes amyloid-related imaging abnormalities (ARIAs). Although ARIA rates may be lower with lecanemab than other amyloid-lowering antibodies,12 they are not insignificant. ARIAs with brain edema occurred in approximately 11% of Clarity participants and were symptomatic in approximately 3%. ARIAs with hemorrhage occurred in approximately 8% of lecanemab patients, and while most events were microhemorrhages or superficial siderosis, lecanemab caused symptomatic hemorrhage in 0.5% of treated patients. Even if we assume that Clarity outcomes accurately depict the real-world effects of lecanemab, does it have an acceptable risk/benefit profile? Would a 1:33 risk of symptomatic brain edema and 1:200 risk of stroke justify more than 50 IV infusion sessions to gain a cognitive effect imperceptible to many patients?
It is likely that the real-world harms of lecanemab treatment will be considerably greater than observed in Clarity. Real-world treatment will likely extend beyond 18 months for many patients, increasing risk exposure. In addition, the controlled trial context and highly selected trial population likely mitigated some of the complexities that will emerge with real-world use of this medication. The effects of lecanemab in combination with other treatments that increase bleeding risk are unknown, but may be substantial. This concern was illustrated recently by severe multifocal hemorrhage in a lecanemab-treated patient who received thrombolysis for acute ischemic stroke.13 Managing lecanemab-treated patients developing high-yield indications for anticoagulation (e.g., pulmonary embolus, high-risk atrial fibrillation) will likely result in either increases in symptomatic hemorrhages or delays to beneficial treatments.
Estimates of bleeding risks in trials are often considerably lower than real-world risks. Bleeding risks are 2–4 times higher in real-world studies of anticoagulants for atrial fibrillation than in trials.14,15 This concern is particularly relevant for lecanemab because Clarity is poorly representative of the target population and almost certainly enrolled participants at disproportionately lower bleeding risk. The median Clarity enrollee was aged 71 years, but the median patient with mild AD dementia or MCI is approximately 85 years.16 Age is strongly linked to bleeding risk in a variety of contexts, including atrial fibrillation17 and stroke thrombolysis.18 In real-world populations, it is likely that bleeding risk will be higher than observed in Clarity, possibly much higher.
Lecanemab's Price Is High, Cost-Effectiveness Is Uncertain, and Potential Total Expenditures Are Unprecedented
WNL-2023-000610In addition to concerns about efficacy and safety, lecanemab raises substantial and novel cost concerns. Lecanemab's price is currently set at $26,500 per year on the basis of a cost-effectiveness analysis concluding that lecenemab would deliver a fair societal value at this price.19 This cost-effectiveness analysis, however, was based on 2 tenuous premises.20 First, the median age in the cost-effectiveness analysis is 71 years (vs 85 years in the real-world population with MCI and mild AD), substantially biasing the estimate toward greater gains in health. Second, this analysis makes highly optimistic assumptions about the long-term effects of lecanemab by extrapolating increasing effects over time. This analysis assumes that the absolute benefits of lecanemab will increase over a 10-year time horizon compared with standard of care and implies a marked reduction of disease progression due to lecanemab, although Clarity did not establish such an effect. Even if benefits truly increase over time, it is a major extrapolation to assume the effect continues for 8+ years. Although CDR-SB changed by 0.45 at 18 months in Clarity, this analysis assumes a change of approximately 1.0 at 24 months and greater than 2.0 at 60 months. This optimistic long-term extrapolation amplifies the effect of selecting a young baseline population. If an older baseline population were selected, decade-long survival would be less common, and fewer individuals would live long enough to receive the most substantial benefits of treatment.
Even if lecancemab were clearly cost-effective, as conventionally defined, its high cost and the massive target population size should give us pause. Approximately 4.5 million American individuals have MCI or mild dementia. It is impossible to know how many American individuals would ultimately be treated with this medication at this cost. Recent data for other high-priced neurologic drugs found that only a fraction of the target population (e.g., 10%–20%) receive new treatments shortly after coming to market.21 There are, however, reasons to think this proportion could be higher for lecanemab. For most of the other conditions studied, alternative medications were already on the market, and no other new medication will have received the level of public attention as lecanemab. Off-label prescribing is ubiquitous in the United States,22,23 and the potential for indication creep is substantial with lecanemab because more than 1.5 million American individuals have moderate-to-severe AD, and tens of millions have brain amyloid without cognitive impairment, raising the possibility that many patients outside the target population could be treated. If the entire target population were treated with lecanemab (which should be our goal with any new treatment believed to have meaningful effectiveness), annual drug costs alone would be staggering—almost $120 billion dollars per year. Even if only 20% of the target population were treated, lecanemab expenditures would be higher than any other drug currently on the market.24
`Regardless of direct medication costs, the total societal costs will be considerably higher. Wide lecanemab implementation will require new infusion and drug administration infrastructure, a coordinated primary prevention screening program, a vast number of amyloid PET scans, broad genetic testing for APOE genotype given the higher rates of ARIAs seen in APOE4 carriers, and regular surveillance MRI scans in treated patients. In the United States, we typically ignore societal treatment costs in clinical regulatory decisions, but there must be a point at which opportunity costs become too great to ignore. A total of $120 billion would translate into 3% of all US health care expenditures and 0.6% of our gross domestic product. In this scenario, for every $33 we would spend on health care, $1 would go to lecanemab. For every $166 we spent on rent, the grocery store or on gas, $1 would go to lecanemab. At $120 billion, the cost of wide lecanemab dissemination would equal the amount spent on all medications in Medicare Part D.25 For $120 billion per year, we could more than triple the NIH budget, finance 4 times the debt forgiveness of the recent Biden debt relief proposal, or more than double green energy production.26 Even if lecanemab had unequivocal evidence of net effectiveness, we must grapple with the question of whether its benefits justify societal expenditures of this magnitude. This is not simply a question for individual physicians and patients to decide nor a question that should default to opaque regulatory rule-making. As it is possible that dissemination of this medication is equivalent to taxing every American hundreds of dollars per year, we need a democratic process to determine whether such expenditures, and their tradeoffs, are warranted.
Conclusion
Even if it was inexpensive, the best available evidence does not establish that lecanemab will lead to meaningful net patient benefits in real-world populations—its established benefits are small, and its potential harms are nontrivial. The single phase 3 trial supporting its use likely underestimates its real-world harms. To justify wide use, we need additional randomized data. We need to know whether lecanemab's cognitive effects truly increase over time and whether it slows progression of MCI to AD dementia and/or slows progression of AD. In short, we need to know whether lecanemab is truly a disease-modifying therapy with a clinically meaningful effect. Longer-term follow-up of Clarity participants may clarify aspects of these questions, but given the importance of knowing these effects with precision, independent replication might reasonably be expected before wide implementation. We also need to know what its risks look like in a population with an age and risk distribution that more closely mirrors the real-world population. This likely requires additional trials, or at a minimum, rigorous outcome measurement in a large and unselected sample of treated patients. If lecanemab does prove to be a truly disease-modifying therapy, it may have meaningful net societal benefit, and, therefore, be worth the individual level risks. On the other hand, if it only results in small or short-term changes in cognition without meaningfully slowing disease progression, it is very likely to lead to net harms.27 The only way to resolve these questions is to accumulate more randomized evidence.
Before we end up potentially paying more for lecanemab than any other medication, do not we need sufficient data to be confident that it is not less effective, vastly more harmful, and 100 times more costly than donepezil?
Glossary
- AD
Alzheimer disease
- ADAS-Cog
Alzheimer Disease Assessment Scale-Cognitive subscale
- ARIA
amyloid-related imaging abnormalities
- CDR-SB
Clinical Dementia Rating-Sum of Boxes
- MCI
mild cognitive impairment
- MCID
minimal clinically important difference
Appendix. Authors
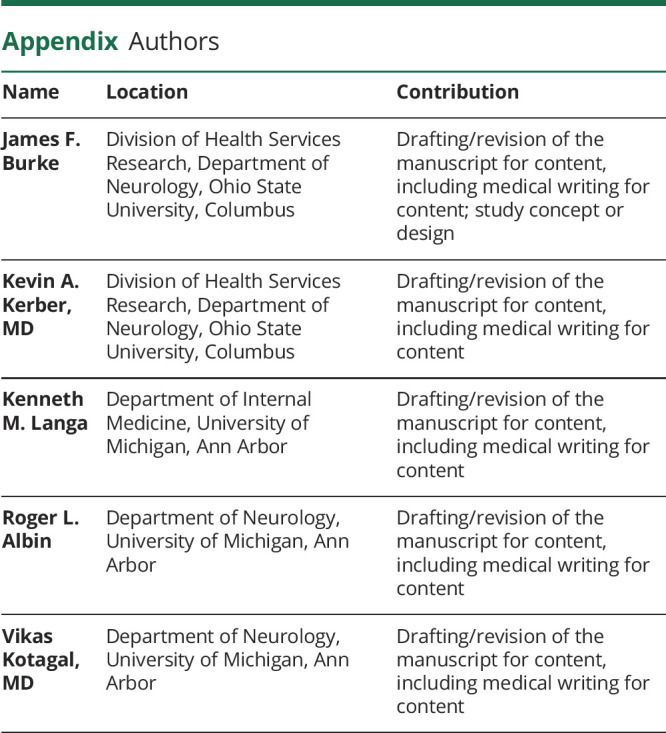
| Name | Location | Contribution |
| James F. Burke | Division of Health Services Research, Department of Neurology, Ohio State University, Columbus | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design |
| Kevin A. Kerber, MD | Division of Health Services Research, Department of Neurology, Ohio State University, Columbus | Drafting/revision of the manuscript for content, including medical writing for content |
| Kenneth M. Langa | Department of Internal Medicine, University of Michigan, Ann Arbor | Drafting/revision of the manuscript for content, including medical writing for content |
| Roger L. Albin | Department of Neurology, University of Michigan, Ann Arbor | Drafting/revision of the manuscript for content, including medical writing for content |
| Vikas Kotagal, MD | Department of Neurology, University of Michigan, Ann Arbor | Drafting/revision of the manuscript for content, including medical writing for content |
Study Funding
No targeted funding reported.
Disclosure
The authors report no relevant disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in early Alzheimer's disease. N Engl J Med. 2022;388(1):9-21. doi: 10.1056/nejmoa2212948 [DOI] [PubMed] [Google Scholar]
- 2.FDA News Release. FDA Grants Accelerated Approval for Alzheimer's Disease Treatment. Accessed February 24, 2023. fda.gov/news-events/press-announcements/fda-grants-accelerated-approval-alzheimers-disease-treatment. [Google Scholar]
- 3.Larkin HD. Lecanemab gains FDA approval for early Alzheimer disease. JAMA. 2023;329(5):363. doi: 10.1001/jama.2022.24490 [DOI] [PubMed] [Google Scholar]
- 4.Ackley SF, Zimmerman SC, Brenowitz WD, et al. Effect of reductions in amyloid levels on cognitive change in randomized trials: instrumental variable meta-analysis. BMJ. 2021;372:n156. doi: 10.1136/bmj.n156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Effect of reductions in amyloid levels on cognitive change in randomized trials: instrumental variable meta-analysis. BMJ. 2022;378:o2094. doi: 10.1136/bmj.o2094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Avgerinos KI, Ferrucci L, Kapogiannis D. Effects of monoclonal antibodies against amyloid-β on clinical and biomarker outcomes and adverse event risks: a systematic review and meta-analysis of phase III RCTs in Alzheimer's disease. Ageing Res Rev. 2021;68:101339. doi: 10.1016/j.arr.2021.101339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andrews JS, Desai U, Kirson NY, Zichlin ML, Ball DE, Matthews BR. Disease severity and minimal clinically important differences in clinical outcome assessments for Alzheimer's disease clinical trials. Alzheimers Dement (NY). 2019;5(1):354-363. doi: 10.1016/j.trci.2019.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu KY, Schneider LS, Howard R. The need to show minimum clinically important differences in Alzheimer's disease trials. Lancet Psychiatry. 2021;8(11):1013-1016. doi: 10.1016/s2215-0366(21)00197-8 [DOI] [PubMed] [Google Scholar]
- 9.Lancet T. Lecanemab for Alzheimer's disease: tempering hype and hope. Lancet. 2022;400(10367):1899. doi: 10.1016/s0140-6736(22)02480-1 [DOI] [PubMed] [Google Scholar]
- 10.Shega JW, Ellner L, Lau DT, Maxwell TL. Cholinesterase inhibitor and n-methyl-d-aspartic acid receptor antagonist use in older adults with end-stage dementia: a survey of hospice medical directors. J Palliat Med. 2009;12(9):779-783. doi: 10.1089/jpm.2009.0059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Birks JS. Cholinesterase inhibitors for Alzheimer's disease. Cochrane Database Syst Rev. 2006;2016(1):CD005593. doi: 10.1002/14651858.cd005593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Withington CG, Turner RS. Amyloid-related imaging abnormalities with anti-amyloid antibodies for the treatment of dementia due to Alzheimer's disease. Front Neurol. 2022;13:862369. doi: 10.3389/fneur.2022.862369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reish NJ, Jamshidi P, Stamm B, et al. Multiple cerebral hemorrhages in a patient receiving lecanemab and treated with t-PA for stroke. N Engl J Med. 2023;388(5):478-479. doi: 10.1056/nejmc2215148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee KH, Chen YF, Yeh WY, et al. Optimal stroke preventive strategy for patients aged 80 years or older with atrial fibrillation: a systematic review with traditional and network meta-analysis. Age Ageing. 2022;51(12):afac292. doi: 10.1093/ageing/afac292 [DOI] [PubMed] [Google Scholar]
- 15.Lip GYH, Keshishian A, Kamble S, et al. Real-world comparison of major bleeding risk among non-valvular atrial fibrillation patients initiated on apixaban, dabigatran, rivaroxaban, or warfarin. Thromb Haemost. 2016;116(05):975-986. doi: 10.1160/th16-05-0403 [DOI] [PubMed] [Google Scholar]
- 16.Brookmeyer R, Abdalla N, Kawas CH, Corrada MM. Forecasting the prevalence of preclinical and clinical Alzheimer's disease in the United States. Alzheimers Dement. 2018;14(2):121-129. doi: 10.1016/j.jalz.2017.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hijazi Z, Oldgren J, Lindbäck J, et al. The novel biomarker-based ABC (age, biomarkers, clinical history)-bleeding risk score for patients with atrial fibrillation: a derivation and validation study. Lancet. 2016;387(10035):2302-2311. doi: 10.1016/s0140-6736(16)00741-8 [DOI] [PubMed] [Google Scholar]
- 18.Ntaios G, Papavasileiou V, Michel P, Tatlisumak T, Strbian D. Predicting functional outcome and symptomatic intracranial hemorrhage in patients with acute ischemic stroke. Stroke. 2018;46(3):899-908. doi: 10.1161/strokeaha.114.003665 [DOI] [PubMed] [Google Scholar]
- 19.Global Eisai. Eisai's Approach to U.S. Pricing for Leqembi (Lecanemab), a Treatment for Early Alzheimer's Disease, Sets Forth Our Concept of “Societal Value of Medicine” in Relation to “Price of Medicine.” Accessed February 24, 2023. eisai.com/news/2023/news202302.html.
- 20.Monfared AAT, Tafazzoli A, Chavan A, Ye W, Zhang Q. The potential economic value of lecanemab in patients with early Alzheimer's disease using simulation modeling. Neurol Ther. 2022;11(3):1285-1307. doi: 10.1007/s40120-022-00373-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reynolds EL, Gallagher G, Hill CE, et al. Costs and utilization of new-to-market neurologic medications. Neurology. 2023;100(9):e884-e898. doi: 10.1212/wnl.0000000000201627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong J, Motulsky A, Abrahamowicz M, Eguale T, Buckeridge DL, Tamblyn R. Off-label indications for antidepressants in primary care: descriptive study of prescriptions from an indication based electronic prescribing system. BMJ. 2017;356:j603. doi: 10.1136/bmj.j603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johansen ME. Gabapentinoid use in the United States 2002 through 2015. JAMA Intern Med. 2018;178(2):292. doi: 10.1001/jamainternmed.2017.7856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tichy EM, Hoffman JM, Suda KJ, et al. National trends in prescription drug expenditures and projections for 2022. Am J Health Syst Pharm. 2022;79(14):1158-1172. doi: 10.1093/ajhp/zxac102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaiser Family Foundation. An Overview of the Medicare Part D Prescription Drug Benefit. Accessed February 24, 2023. kff.org/medicare/fact-sheet/an-overview-of-the-medicare-part-d-prescription-drug-benefit/. [Google Scholar]
- 26.IRENA. Renewable Power Generation Costs in 2021. Accessed February 24, 2023. irena.org/-/media/Files/IRENA/Agency/Publication/2022/Jul/IRENA_Power_Generation_Costs_2021.pdf?rev=34c22a4b244d434da0accde7de7c73d8. [Google Scholar]
- 27.Burke JF, Valdes-Sosa PA, Langa KM, Hayward RA, Albin RL. Modeling test and treatment strategies for presymptomatic Alzheimer disease. PLoS One. 2014;9(12):e114339. doi: 10.1371/journal.pone.0114339 [DOI] [PMC free article] [PubMed] [Google Scholar]


