Abstract
Background
To enable successful inclusion of electroencephalography (EEG) outcome measures in Alzheimer’s disease (AD) clinical trials, we retrospectively mapped the progression of resting-state EEG measures over time in amyloid-positive patients with mild cognitive impairment (MCI) or dementia due to AD.
Methods
Resting-state 21-channel EEG was recorded in 148 amyloid-positive AD patients (MCI, n = 88; dementia due to AD, n = 60). Two or more EEG recordings were available for all subjects. We computed whole-brain and regional relative power (i.e., theta (4-8 Hz), alpha1 (8-10 Hz), alpha2 (10-13 Hz), beta (13-30 Hz)), peak frequency, signal variability (i.e., theta permutation entropy), and functional connectivity values (i.e., alpha and beta corrected amplitude envelope correlation, theta phase lag index, weighted symbolic mutual information, inverted joint permutation entropy). Whole-group linear mixed effects models were used to model the development of EEG measures over time. Group-wise analysis was performed to investigate potential differences in change trajectories between the MCI and dementia subgroups. Finally, we estimated the minimum sample size required to detect different treatment effects (i.e., 50% less deterioration, stabilization, or 50% improvement) on the development of EEG measures over time, in hypothetical clinical trials of 1- or 2-year duration.
Results
Whole-group analysis revealed significant regional and global oscillatory slowing over time (i.e., increased relative theta power, decreased beta power), with strongest effects for temporal and parieto-occipital regions. Disease severity at baseline influenced the EEG measures’ rates of change, with fastest deterioration reported in MCI patients. Only AD dementia patients displayed a significant decrease of the parieto-occipital peak frequency and theta signal variability over time. We estimate that 2-year trials, focusing on amyloid-positive MCI patients, require 36 subjects per arm (2 arms, 1:1 randomization, 80% power) to detect a stabilizing treatment effect on temporal relative theta power.
Conclusions
Resting-state EEG measures could facilitate early detection of treatment effects on neuronal function in AD patients. Their sensitivity depends on the region-of-interest and disease severity of the study population. Conventional spectral measures, particularly recorded from temporal regions, present sensitive AD treatment monitoring markers.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13195-023-01327-1.
Keywords: Longitudinal, Resting state, Electroencephalography, Alzheimer’s disease, Clinical trial design, Functional endpoint, Sample size
Background
Alzheimer’s disease (AD) is diagnosed in vivo by abnormalities on core biomarkers, including amyloid-beta (Aβ) deposition, pathologic tau, and neurodegeneration. The disease is a continuum, spanning preclinical, mild cognitive impairment (MCI), and dementia stages [1]. The worldwide population of AD dementia patients is anticipated to exceed 150 million by 2050, unless means of delay, prevention, or treatment are found [2]. Current experimental treatments of AD revolve around reversing existing pathology, primarily focusing on Aβ removal. Aducanumab (ADUHELM™) and lecanemab (Leqembi™) were recently approved for treatment of AD in the US, with evidence of cognitive efficacy to be confirmed in post-marketing trials. Other promising anti-amyloid antibodies are currently awaiting FDA approval (donanemab) or are under phase 3 investigation (gantenerumab). The advent of these agents is accompanied by that of non-pharmacological interventions, such as magnetic stimulation of the precuneus [3].
A critical step in designing valid and useful AD clinical trials is selecting appropriate outcome measures. Clinical efficacy of an intervention is typically evaluated by an assessment of cognition and everyday functioning, with growing interest for cognitive and functional composite scores [4, 5]. Identifying a successful therapy using these measures is difficult in preclinical stages of AD, in which the target population has not yet demonstrated cognitive decline and may not do so in the near future. Biomarkers provide a way to evaluate pathologic processes, or biological responses to a therapeutic intervention, prior to their clinical presentation. Trials that use biomarkers to establish a drug-placebo difference are generally much shorter and smaller than trials that require demonstration of clinical benefit, due to the low sensitivity of cognitive measures [6]. While established in vivo fluid and neuroimaging AD biomarkers mirror molecular and structural brain changes associated with the disease [7], high costs and/or invasiveness make them less suited for serial measurements. Electroencephalography (EEG) biomarkers have been proposed as alternative measures to demonstrate the efficacy of novel therapeutics [8, 9]. The non-invasive, low-cost neurophysiological technique provides a relatively direct measure of neuronal activity and synaptic function. The temporal resolution of EEG allows for investigation of cortical rhythms during a resting-state condition, as well as of quick positive and negative voltage peaks in response to cognitive-motor events (i.e., event-related potentials). Resting-state EEG has the practical advantage that it does not require any response by a patient. This allows more severely impaired patients, who may not be able to perform tasks accurately, to be studied.
Different types of resting-state EEG measures have been used to quantify neurophysiological dysfunction in AD patients. These can roughly be divided into (i) spectral, (ii) functional connectivity, and (iii) entropy measures, according to the analytical methodology that is employed for computation. Increased relative theta power has been reported as early as the preclinical stage of AD [10, 11]. Enhanced relative delta power, as well as posterior relative alpha and beta power reduction, have repeatedly been reported in later stages of the disease [12–14]. Disrupted communication between brain regions is another well-established finding in AD. MCI and AD dementia patients show large-scale disruptions in functional connections (e.g., a loss of connectivity in alpha and beta frequency bands, increased theta band connectivity [15–17]) and selective vulnerability of cortical hub regions (i.e., highly connected nodes with a central position in the overall organization of a network [16, 18–21]). Growing evidence furthermore suggests a significant, progressive loss of entropy of neural activity over the course of the disease [22–25].
The degree of EEG abnormalities has been shown to correlate strongly with cognitive impairment in AD patients, in both cross-sectional [26] and longitudinal studies [27]. Several measures, including relative power [11, 28], the spectral power ratio (delta/theta + alpha/beta power) [29], spectral coherence [30], and complexity [31], have shown significant associations with neuropsychological measures. EEG measures have also been shown to be predictive of clinical progression, predicting conversion from the preclinical to MCI, or from the MCI to dementia stage of AD [10, 11, 32]. This association with cognitive and clinical assessments is part of what makes EEG measures an interesting target for treatment monitoring.
In the relatively short time span of a clinical trial, EEG measures are hypothesized to be more sensitive to change than biomarkers obtained from cerebrospinal fluid (CSF), positron emission tomography (PET), and magnetic resonance imaging (MRI). Using them as markers of target engagement could therefore potentially reduce the size, duration, and costs of clinical trials. Furthermore, as the availability of clinically efficacious medication grows, investigation of its impact on brain function will become of increasing interest. EEG measures provide an opportunity to study the neurophysiological mechanisms underlying therapeutic outcomes. At present, the main clinical goal of AD clinical trials is a slowing or halting of cognitive decline. Assessment of (stabilizing) treatment effects using EEG measures depends on deterioration of electrophysiological measures in the placebo group. Sample size estimates and power analyses are generally based on information from previous research. Available longitudinal EEG studies in AD patients however often lack statistical power due to the use of small cohorts [33, 34], do not make use of (recently) established diagnostic guidelines (e.g., include amyloid-negative patients) [32, 33, 35–38], or only report on a limited number of EEG measures [39]. A solid understanding of the natural course of the EEG in amyloid-positive patients along the AD continuum is needed to help improve clinical trial design and facilitate selection of the most suitable neurophysiological markers for trial implementation.
We modeled the development of a variety of resting-state EEG measures over time in a large, amyloid-positive AD cohort, including patients with MCI or dementia (N = 148). Faster rates of change were expected for regional (i.e., temporal and parieto-occipital) than whole-brain measures, considering that disruption of local neuronal activity precedes the emergence of whole-brain abnormalities. Spectral measures, particularly relative theta power, were expected to be most sensitive to change. The development of EEG measures over time was compared between groups stratified based on baseline disease stage (MCI or dementia) to investigate the effect of clinical disease severity on the measures’ rates of change. Fastest deterioration was expected in non-demented patients, as the presence of extensive structural brain changes in AD dementia patients may cause the rate of functional decline to slow down or plateau. We computed yearly and two-yearly effect sizes for a subset of EEG measures that showed significant deterioration over time. These values were used to estimate the minimum sample size required to detect different treatment effects (i.e., 50% less deterioration, stabilization, or 50% improvement) on the development of EEG measures over time, in hypothetical clinical trials of 1- or 2-year duration.
Methods
Study design and participants
We retrospectively included patients who had been evaluated and followed up in the memory clinic of the Amsterdam UMC Alzheimer center, or who participated in a multicenter AD clinical trial with central EEG analysis at the Amsterdam UMC EEGlab, between October 15, 2003, and January 1, 2019. All participants provided written informed consent for the use of their data for research purposes. Although AD represents a seamless disease continuum, patients can be assigned to progressive phases based on physical, cognitive, and functional assessments [1]. We differentiated between patients with MCI and dementia due to AD based on established clinical guidelines [40]. For a detailed description of all investigations that were performed as part of our routine diagnostic screening, see Van der Flier et al. [41]. Two or more EEG recordings were available for all participants. Recordings that were heavily contaminated with artifacts were excluded from analysis. Follow-up durations shorter than 3 months or longer than 3 years are not commonly employed in AD clinical trials. We therefore only evaluated follow-up recordings that were obtained within this time-frame. All participants were positive for Aβ deposition, as assessed using CSF Aβ42 (cut-off < 813 pg/ml, Tijms et al. (2018)) [42] or [11C] PiB amyloid PET investigation (the routine PET protocol has been described elsewhere [43, 44]). Tau pathology and neurodegeneration were characterized at baseline using CSF p-tau (cut-off > 52 pg/ml) and t-tau levels (cut-off > 375 pg/ml) [45]. Tau and neurodegeneration positive and negative patients (T +/- , N +/-) were included in this study. Medial temporal lobe atrophy (MTA), ranging from 0 (no atrophy) to 4 (severe atrophy), was rated on coronal T1-weighted MRI images. To evaluate the potential effect of pharmacological agents (i.e., cholinesterase inhibitors, anti-depressants, anti-epileptic drugs, anti-psychotics, benzodiazepines) on our findings, medication use was evaluated and scored.
EEG acquisition and pre-processing
Twenty minutes eyes-closed resting-state EEG data was recorded on digital EEG systems from 21 electrodes at the positions of the 10–20 system: Fp2, Fp1, F8, F7, F4, F3, A2, A1, T4, T3, C4, C3, T6, T5, P4, P3, O2, O1, Fz, Cz, Pz. A common or average reference (including all electrodes except Fp2/1 and A2/1) was used. Electrode impedance was kept below 5 kΩ. Sample frequency (200, 250, 256, 500, or 512 Hz) and online filter settings (high-pass 0.16 or 0.5, low-pass 70 Hz) varied between clinical- and trial-related recording protocols. During acquisition, patients and their recordings were monitored by an EEG technician, in order to minimize artifacts and prevent drowsiness. Ten 4096-sample (sample frequency of 500 or 512 Hz) or 2048-sample (sample frequency of 200, 250, or 256 Hz) epochs of eyes-closed artifact-free data (containing no eye blinks, muscle artifact, slow eye movements, or EKG-artifacts) were selected from each EEG recording based on visual inspection of the data by one of the authors (E.S.).
Analysis and outcome measures
Different types of measures were computed from the EEG waveforms, using open access Brainwave software (version 0.9.163.26, developed by Professor C.J. Stam, http://home.kpn.nl/stam7883/brainwave.html).
Spectral measures
For each of the 21 electrodes, the relative contribution (i.e., power) of different frequency bands (i.e., theta (4–8 Hz), alpha1 (8–10 Hz), alpha2 (10–13 Hz), and beta (13–30 Hz)) to the broadband EEG signal (0.5–48 Hz) were calculated using a fast Fourier transform. Delta (0.5–4 Hz) and gamma (30–48 Hz) frequencies were excluded from analysis because of their respective sensitivity to ocular [46] and electromyogenic artifacts [47, 48]. In addition, the peak frequency of the power spectrum was identified for each electrode as the median frequency between 4 and 13 Hz.
Functional connectivity measures
Functional connectivity refers to the statistical dependence, or ‘inter-relatedness’, between time series of electrophysiological activity in distinct regions of the brain. We estimated connectivity strength using different techniques:
The amplitude envelope correlation (AEC) [49–51] is a measure of amplitude-based connectivity between two time series. The linear correlation coefficient between the power envelopes of two time series was computed and normalized between 0 and 1, with 0.5 indicating no functional connectivity. To correct for the effects of volume conduction, we made use of pairwise orthogonalization in two directions (i.e., X to Y and Y to X) prior to AEC estimation [15, 49]. The AEC values (i.e., the correlation between the orthogonalized envelopes) for both directions were averaged, resulting in corrected AEC (AEC-c) values.
The phase lag index (PLI) [52] provides an estimate of phase-based connectivity between two time series. If no phase synchronization exists between two time series, the distribution of their phase differences is expected to be flat. Any deviation from this flat distribution indicates phase synchronization. The PLI is an asymmetry index for this distribution. Its values range between 0 and 1, with 0 indicating no connectivity and 1 referring to perfect phase locking. The measure is invariant against the presence of common sources (i.e., volume conduction), as it discards phase differences that center around 0 mod π.
A single AEC-c and PLI value was obtained for each of the 21 electrodes, by averaging over its 20 pair-wise connectivity values. This value indicates the average connectivity strength between that electrode and the rest of the brain. This corresponds to the notion of “weighted degree” or “node strength” in graph theory.
Entropy measures
Single channel
Variability of each EEG time series was quantified using the permutation entropy (PE) [53]. The continuous EEG signal recorded from each electrode was transformed into a sequence of discrete symbols. Next, the Shannon’s information entropy of the symbol probability distribution was computed. High entropy values indicate a flat or uniform symbol probability distribution (i.e., high signal variability), whereas low entropy values indicate a more bell-shaped curve (i.e., low signal variability).
Functional connectivity
The weighted symbolic mutual information (wSMI) [54] evaluates the extent to which two time series present nonrandom joint fluctuations. To quantify the information shared between two time series, the continuous signals are first transformed into sequences of discrete symbols (as is done to compute the PE). The joint probability of each pair of symbols gives the SMI, with high values indicating strong coupling. To correct for potential common-source artifacts, the weights of pairs of identical or opposite-sign symbols in the joint probability matrix are set to zero.
The joint permutation entropy (JPE) [55] integrates information on local signal variability (as reflected by the PE) and interregional coupling (as reflected by the wSMI). Again, the continuous signals are transformed into sequences of discrete symbols. This time, connectivity is defined as the Shannon’s information entropy of the joint probability matrix. To facilitate comparison to more conventional connectivity measures, we report inverted JPE (JPEinv) values, so that higher values correspond to stronger coupling. Note that measures based on a symbolic representation of the EEG time series (i.e., PE, wSMI and JPEinv) require the choice of parameter settings, such as symbol size n and time-delay τ. In the present study, we made use of n = 4 and τ = 1. For more information on the role of these parameters in entropy computations and validation of the selected settings, see Scheijbeler et al. [55].
The investigated EEG outcome measures are presented in Table 1. We computed global (i.e., whole-brain) and regional averages (i.e., temporal—A2, A2, T4, T3, T6, T5 and parieto-occipital – P4, P3, O2, O1, Pz) for relative power, PE, AEC-c, PLI, wSMI, and JPEinv. The peak frequency of the power spectrum was computed over parieto-occipital sensors only. The AEC-c was computed in the alpha and beta band and the PLI in the theta band because of the reproducibility of these metrics infinding differences between AD dementia patients and cognitively healthy controls [15, 56]. The PE, wSMI, and JPEinv were computed in the theta band [55], resulting in 31 measures of interest.
Table 1.
EEG measures of interest
| Region | Measure | Frequency band |
|---|---|---|
| Global, parieto-occipital, temporal | Relative power | Theta |
| Alpha1 | ||
| Alpha2 | ||
| Beta | ||
| AEC-c | Alpha | |
| Beta | ||
| PLI | Theta | |
| PE | Theta | |
| wSMI | Theta | |
| JPEinv | Theta | |
| Parieto-occipital | Peak frequency | - |
PE Permutation entropy, AEC-c Corrected amplitude envelope correlation, PLI Phase lag index, wSMI Weighted symbolic mutual information, JPEinv Inverted joint permutation entropy
Statistical analysis
Group differences of demographic variables
Group differences for each demographic variable at baseline were assessed between the MCI and AD dementia subgroups using χ2 tests for categorical variables and Kruskal–Wallis tests for continuous variables.
Development of EEG measures over time
Development over time was analyzed using linear mixed models (LMMs). A LMM adjusts for the dependency of the repeated observations within a subject by modelling variability among individuals and including both fixed and random effects. The simplest form of a LMM only allows the intercepts to vary across subjects. In addition to a random intercept, it is possible that development over time varies across individuals, as reflected by a random slope. Model fit of “random intercept” and “random intercept and slope” models was compared using likelihood ratio tests. The best, or, in the case of similar fit, the simplest model, was used to analyze the development over time for the outcome variables of interest.
We first modeled the linear development of EEG measures over time within the whole cohort. Time, our covariate of interest, was included as a continuous variable in months. Its values reflect follow-up time between EEG recordings and were therefore unequally spaced in time. A separate LMM was built for each EEG outcome measure (Table 1, n = 31).
Table 2.
Baseline demographic and clinical characteristics
| MCI | AD dementia | Total | |
|---|---|---|---|
| N | 88 | 60 | 148 |
| Age, years (mean, SD) | 70.7 (7.2)** | 66.9 (8.2) | 69.2 (7.8) |
| Sex (male/female) | 46/42 | 31/29 | 77/71 |
| MMSE (median, IQR) | 27 (3)*** | 24 (5) | 26 (4) |
| MTA score (median, IQR) | |||
| Left hemisphere | 2 (2) | 1 (2) | 2 (2) |
| Right hemisphere | 2 (1) | 2 (2) | 2 (2) |
| Aβ + (nn, CSF Aβ42/ [11C] PiB-PET) | 88/0 | 57/3 | 145/3 |
| Phosphorylated tau (n, CSF p-tau +/-) | 46/4 | 33/8 | 79/12 |
| Total tau (n, CSF t-tau +/-) | 44/6 | 33/8 | 77/14 |
| Medication use (n/%) | |||
| Anticholinergics | 4 (5%) | 6 (10%) | 10 (7%) |
| Antidepressants | 9 (10%) | 5 (8%) | 14 (9%) |
| AEDs | 1 (1%) | 3 (5%) | 4 (3%) |
| Antipsychotics | 1 (1%) | 1 (2%) | 2 (1%) |
| Benzodiazepines | 3 (3%) | 5 (8%) | 8 (5%) |
SD Standard deviation, MMSE Mini mental state examination, IQR Inter-quartile range, MTA Medial temporal lobe atrophy, Aβ + Amyloid beta positive, as measured by cerebrospinal fluid Aβ42 concentration or [15] C-labeled Pittsburgh Compound-B positron emission topography examination, AEDs Anti-epileptic drugs
**p < .01, *** p < .001
To analyze the differences in development over time between subgroups, we stratified subjects based on baseline disease stage (i.e., MCI, AD dementia). To mimic real-life conditions in the context of clinical trial design, we modeled the course of EEG measures without including knowledge on future clinical progression. We modeled and compared the development of the EEG outcome measures over time between groups by adding Time, Group, and Time*Group interaction variables to the model. Again, a separate LMM was built for each measure of interest. To investigate whether sex, age, or medication use influenced the (difference between the) development of the groups over time, we performed both crude and covariate adjusted analysis. We report regression coefficients with 95% confidence intervals. A p-value < 0.05 was considered statistically significant. Due to the exploratory nature of the study, adjustment for multiple comparisons was not performed. Details of the LMM analyses are included in Additional file 1.
Effect- and sample size calculation
Effect sizes (measured as d) of the strongest whole-group and group-wise LMM results were computed per month using the formula below [57]. Yearly and two-yearly effect sizes were linearly estimated.
*Varslope was set to zero for models that only included a random intercept on subject level.
In the context of a clinical trial, different treatment effects on EEG outcome measures are imaginable. In a stabilizing scenario (1), a treatment effectively halts the progression of EEG abnormalities over time. Treatment effectiveness in this scenario corresponds to d, as computed from the LMM results. A treatment can also slow down the rate of deterioration of EEG outcome measures, which we will refer to as a “less deterioration” scenario (2). This second scenario results in a smaller treatment effect size than the stabilizing scenario. Finally, deterioration of EEG outcome measures (e.g., oscillatory slowing) may be reversed by a treatment. Improvement of the EEG measures in the active group results in a larger treatment effect size than would be observed in a stabilizing scenario (3).
We estimated minimum sample sizes required to detect different treatment effects (i.e., 50% less deterioration, stabilization, or 50% improvement) on EEG outcome measures in hypothetical clinical trials of 1- or 2-year duration, with EEG measurements taken at baseline and end-of-treatment. This was done using G*Power software [58] at 0.05 to 99% power, for a one-sided two-sample t-test, with a type I error (α) of p < 0.05. A balanced design was assumed.
Results
Baseline characteristics
Eighty-eight amyloid-positive MCI and 60 AD dementia subjects were included in this study. Table 2 summarizes the baseline demographic and clinical characteristics of the study population. The mean age of subjects with MCI was 70.7 years (SD 7.2). This was significantly higher than the mean age of AD dementia subjects (66.9 years, SD 8.2) (p < 0.01). We report significantly higher median MMSE scores (available for 143 subjects at baseline) for the MCI (27, IQR 3) than the AD dementia group (24, IQR 5) (p < 0.001). For a more comprehensive overview of neuropsychological test scores of the participants at baseline, see Table S1 & S2 in Additional file 2. Sex ratio and MTA scores (n = 84) did not differ significantly between groups at baseline. CSF p-tau and t-tau levels were available for 91 patients.
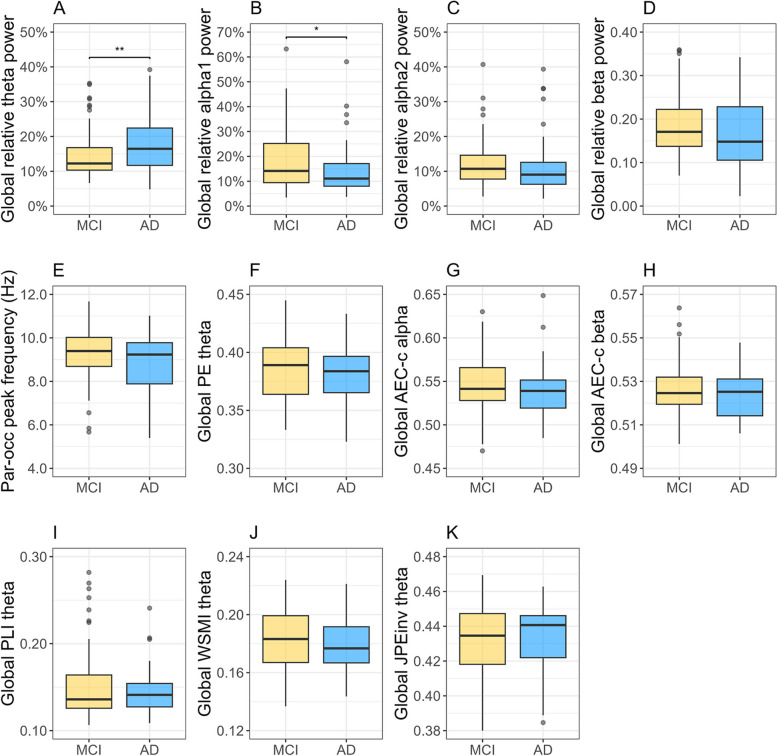
Baseline comparisons of global EEG measures and the parieto-occipital peak frequency between the MCI and AD dementia subgroups are displayed in Fig. 1. The MCI group had significantly lower global relative theta power (p < 0.01) and higher relative alpha1 power values (p < 0.05) compared to the AD dementia group (Fig. 1A, B). The groups did not differ significantly with respect to the remaining measures. Mean (SD) values for all measures are reported in Additional file 2 (Table S3).
Fig. 1.
A-K Baseline comparisons of global EEG measures and the parieto-occipital peak frequency between Aβ + MCI and AD dementia patients. A-D Global relative theta, alpha1, alpha2, and beta power. E Parieto-occipital peak frequency in Hz. F Global permutation entropy (PE) theta. G-H Corrected amplitude envelope correlation (AEC-c) alpha and beta. I Phase lag index (PLI) theta. J Weighted symbolic mutual information (wSMI) theta. K Inverted joint permutation entropy (JPEinv) theta. * p < .05, **p < .01
Follow-up characteristics
Participants underwent 2 to 4 EEG recordings within a follow-up period of 2.6 to 35.5 months (Table 3). Reasons for follow-up included clinical (re-)evaluation, screening for potential inclusion in a clinical trial, or participation in a clinical trial (as control subject). The MCI group had a longer median follow-up time (11.0 months (range 2.6 – 34.8)) than the AD dementia group (5.9 months (range 2.8 – 35.5)). This difference was however not statistically significant.
Table 3.
Follow-up characteristics
| MCI | AD dementia | Total | |
|---|---|---|---|
| Reason for follow-up (n) | |||
| Clinical follow-up | 46 | 18 | 64 |
| Clinical trial – screening phase | 5 | 24 | 29 |
| Clinical trial – control condition | 37 | 18 | 55 |
| Number of EEG recordings (median, range) | 2 (2–4) | 2 (2–3) | 2 (2–4) |
| Total follow-up time, months (median, range) | 11.0 (2.6 – 34.8) | 5.9 (2.8 – 35.5) | 7.2 (2.6 – 35.5) |
EEG measures’ development over time
Whole-group LMM
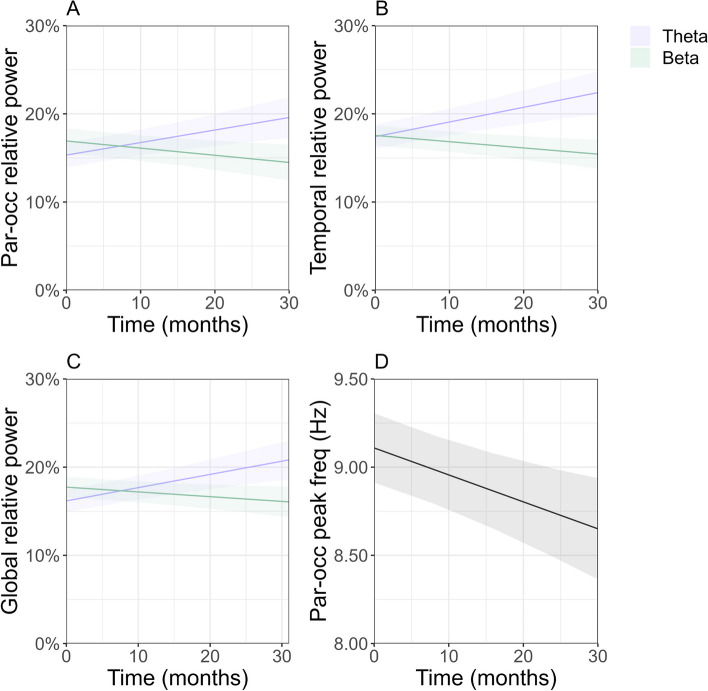
The whole-group LMM analysis revealed significant regional and global oscillatory slowing over time in our Aβ + AD cohort (N = 148), with strongest effects for regional measures. We found a significant increase in parieto-occipital, temporal, and global relative theta power, as well as a significant decrease in parieto-occipital, temporal and global relative beta power (Fig. 2A-C) and parieto-occipital peak frequency (Fig. 2D) over time. Although we report no significant longitudinal changes in functional connectivity strength and signal variability on whole-group level, estimates of regression coefficient β indicate a downward trend in parieto-occipital, temporal, and global AEC-c alpha and beta and JPEinv theta connectivity, as well as PE theta. PLI theta and wSMI theta connectivity exhibit a consistent positive trend across all regions. Regression coefficients and 95% confidence intervals are reported in Table 4. Regression coefficient β reflects the change in outcome measure per month. For visualization purposes, only significant estimates are plotted in Fig. 2.
Fig. 2.
A-D Estimated trajectories and 95% confidence intervals for EEG measures in Aβ + AD patients (MCI and AD dementia). Significant whole-group estimates are visualized (p < .05). A-C Parieto-occipital, temporal, and global relative theta and beta power. D Parieto-occipital peak frequency in Hz
Table 4.
Results of the whole-group LMM analysis performed to evaluate change in EEG measures over time (in months) in Aβ + AD patients (MCI and AD dementia). Regression coefficients (β) and 95% confidence intervals (CI) are reported
| Region | Measure | Frequency band | β | 95% CI | p-value | |
|---|---|---|---|---|---|---|
| Parieto-occipital | Relative power | Thetab | 1.4E-03 | 7.3E-04 | 2.2E-03 | < .001*** |
| Alpha1a | -2.9E-04 | -1.4E-03 | 8.5E-04 | 0.61 | ||
| Alpha2a | -2.6E-04 | -1.3E-03 | 7.8E-04 | 0.62 | ||
| Betaa | -8.1E-04 | -1.4E-03 | -2.3E-04 | < .01** | ||
| Peak frequency | -a | -1.5E-02 | -2.4E-02 | -6.8E-03 | < .001** | |
| AEC-c | Alphaa | -7.5E-05 | -4.2E-04 | 2.7E-04 | 0.67 | |
| Betaa | -9.3E-05 | -2.2E-04 | 3.7E-05 | 0.16 | ||
| PLI | Thetaa | 2.0E-04 | -2.0E-04 | 6.0E-04 | 0.33 | |
| PE | Thetaa | -9.7E-05 | -2.7E-04 | 7.4E-05 | 0.27 | |
| wSMI | Thetaa | 5.0E-05 | -7.8E-05 | 1.8E-04 | 0.44 | |
| JPEinv | Thetaa | -5.3E-05 | -1.6E-04 | 5.3E-05 | 0.32 | |
| Temporal | Relative power | Thetaa | 1.7E-03 | 9.2E-04 | 2.4E-03 | < .001*** |
| Alpha1a | -4.5E-04 | -1.1E-03 | 2.5E-04 | 0.21 | ||
| Alpha2a | -3.8E-04 | -8.3E-04 | 6.5E-05 | 0.09 | ||
| Betaa | -7.1E-04 | -1.2E-03 | -2.4E-04 | < .01** | ||
| AEC-c | Alphaa | -9.8E-05 | -4.2E-04 | 2.2E-04 | 0.55 | |
| Betaa | -3.6E-05 | -1.6E-04 | 9.0E-05 | 0.57 | ||
| PLI | Thetaa | 1.3E-04 | -2.3E-04 | 4.9E-04 | 0.49 | |
| PE | Thetaa | -1.6E-04 | -3.2E-04 | -3.6E-08 | 0.05 | |
| wSMI | Thetaa | 7.4E-05 | -4.5E-05 | 1.9E-04 | 0.22 | |
| JPEinv | Thetaa | -8.4E-05 | -1.7E-04 | 5.3E-06 | 0.07 | |
| Global | Relative power | Thetab | 1.5E-03 | 8.6E-04 | 2.2E-03 | < .001*** |
| Alpha1a | -4.6E-04 | -1.3E-02 | 3.4E-04 | 0.26 | ||
| Alpha2a | -3.1E-04 | -9.2E-04 | 3.0E-04 | 0.32 | ||
| Betaa | -5.4E-04 | -1.0E-03 | -4.6E-05 | < .05* | ||
| AEC-c | Alphaa | -9.2E-05 | -4.1E-04 | 2.3E-04 | 0.57 | |
| Betaa | -5.8E-05 | -1.8E-04 | 6.2E-05 | 0.34 | ||
| PLI | Thetaa | 1.5E-04 | -1.9E-04 | 5.0E-04 | 0.38 | |
| PE | Thetaa | -1.3E-04 | -2.8E-04 | 2.8E-05 | 0.11 | |
| wSMI | Thetaa | 6.5E-05 | -5.4E-05 | 1.8E-04 | 0.28 | |
| JPEinv | Thetaa | -5.5E-05 | -1.6E-04 | 4.7E-05 | 0.29 | |
AEC-c Corrected amplitude envelope correlation, PLI Phase lag index, PE Permutation entropy, wSMI Weighted symbolic mutual information, JPEinv Inverted joint permutation entropy
*p<.05, **p<.01, ***p<.001
aRandom intercept on subject level
bRandom intercept and random slope on subject level
Group-wise LMM
Group-wise LMM analysis was performed to investigate potential differences in the development of EEG measures over time between patients in different stages of AD. Tables 5, 6 and 7 present the regression coefficients and 95% confidence intervals of the Time effects for each group (i.e., MCI and AD dementia). None of the EEG measures showed significant Time*Group interactions. Note that regression coefficient β of the interaction effects indicates the difference in Time effect between the MCI and AD dementia subgroups. We report a negligible effect on the rates of change of the investigated EEG measures by the addition of sex, age, and medication use covariates to the LMMs (see Additional file 2, Table S4-6), and therefore make use of the uncorrected results in the remainder of the paper.
Table 5.
Results of the group-wise LMM analysis performed to evaluate change in parieto-occipital EEG measures over time (in months) in Aβ + MCI or AD dementia patients. Regression coefficients (β) and 95% confidence intervals (CI) of the Time effects are reported. Estimates for the Group*Time interaction effects, as well as estimates adjusted for age, sex and medication use are presented in Additional file 2 (Table S4)
| Region | Measure | Frequency band | Disease stage | β | 95% CI | p-value | |
|---|---|---|---|---|---|---|---|
| Parieto-occipital | Relative power | Theta | MCIb | 1.6E-03 | 8.3E-04 | 2.3E-03 | < .001*** |
| AD dementiab | 8.7E-04 | -2.0E-04 | 1.9E-03 | 0.12 | |||
| Alpha1 | MCIa | 3.8E-04 | -1.1E-03 | 1.9E-03 | 0.62 | ||
| AD dementiaa | -1.2E-03 | -3.0E-03 | 5.2E-04 | 0.17 | |||
| Alpha2 | MCIa | -1.3E-04 | -1.5E-03 | 1.2E-03 | 0.86 | ||
| AD dementiaa | -4.5E-04 | -2.0E-03 | 1.1E-03 | 0.58 | |||
| Beta | MCIa | -1.0E-03 | -1.8E-03 | -2.7E-04 | < .01** | ||
| AD dementiaa | -5.0E-04 | -1.4E-03 | 3.9E-04 | 0.27 | |||
| Peak frequency | - | MCIa | -1.0E-02 | -2.1E-02 | 1.2E-03 | 0.08 | |
| AD dementiaa | -2.3E-02 | -3.6E-02 | -9.6E-03 | < .001*** | |||
| AEC-c | Alpha | MCIa | -1.5E-04 | -6.1E-04 | 3.1E-04 | 0.53 | |
| AD dementiaa | 2.1E-05 | -5.1E-04 | 5.5E-04 | 0.94 | |||
| Beta | MCIa | -7.1E-05 | -2.4E-04 | 9.9E-05 | 0.41 | ||
| AD dementiaa | -1.2E-04 | -3.2E-04 | 7.5E-05 | 0.22 | |||
| PLI | Theta | MCIa | 1.9E-04 | -3.4E-04 | 7.2E-04 | 0.48 | |
| AD dementiaa | 2.1E-04 | -4.1E-04 | 8.3E-04 | 0.50 | |||
| PE | Theta | MCIa | -2.4E-05 | -2.5E-04 | 2.0E-04 | 0.84 | |
| AD dementiaa | -2.0E-04 | -4.6E-04 | 6.4E-05 | 0.14 | |||
| wSMI | Theta | MCIa | -1.8E-05 | -1.9E-04 | 1.5E-04 | 0.83 | |
| AD dementiaa | 1.4E-04 | -5.2E-05 | 3.4E-04 | 0.15 | |||
| JPEinv | Theta | MCIa | 7.6E-07 | -1.4E-04 | 1.4E-04 | 0.99 | |
| AD dementiaa | -1.3E-04 | -2.9E-04 | 3.6E-05 | 0.13 | |||
AEC-c Corrected amplitude envelope correlation, PLI Phase lag index, PE Permutation entropy, wSMI Weighted symbolic mutual information, JPEinv Inverted joint permutation entropy
*p<.05, **p<.01, ***p<.001
aRandom intercept on subject level
bRandom intercept and random slope on subject level
Table 6.
Results of the group-wise LMM analysis performed to evaluate change in temporal EEG measures over time (in months) in Aβ + MCI or AD dementia patients. Regression coefficients (β) and 95% confidence intervals (CI) of the Time effects are reported. Estimates for the Group*Time interaction effects, as well as estimates adjusted for age, sex, and medication use are presented in Additional file 2 (Table S5)
| Region | Measure | Frequency band | Disease stage | β | 95% CI | p-value | |
|---|---|---|---|---|---|---|---|
| Temporal | Relative power | Theta | MCIb | 2.2E-03 | 1.2E-03 | 3.1E-03 | < .001*** |
| AD dementiab | 8.2E-04 | -3.1E-04 | 2.0E-03 | 0.16 | |||
| Alpha1 | MCIb | -3.7E-04 | -1.3E-03 | 5.6E-04 | 0.44 | ||
| AD dementiab | -6.0E-04 | -1.7E-03 | 5.0E-04 | 0.30 | |||
| Alpha2 | MCIa | -2.5E-04 | -8.4E-04 | 3.4E-04 | 0.41 | ||
| AD dementiaa | -5.7E-04 | -1.3E-03 | 1.1E-04 | 0.10 | |||
| Beta | MCIa | -8.0E-04 | -1.4E-03 | -1.8E-04 | < .05* | ||
| AD dementiaa | -5.8E-04 | -1.3E-03 | 1.5E-04 | 0.12 | |||
| AEC-c | Alpha | MCIa | -1.6E-04 | -5.8E-04 | 2.7E-04 | 0.47 | |
| AD dementiaa | -2.2E-05 | -5.1E-04 | 4.7E-04 | 0.93 | |||
| Beta | MCIa | -2.5E-05 | -1.9E-04 | 1.4E-04 | 0.77 | ||
| AD dementiaa | -5.2E-05 | -2.5E-04 | 1.4E-04 | 0.60 | |||
| PLI | Theta | MCIa | 1.1E-04 | -3.7E-04 | 5.8E-04 | 0.66 | |
| AD dementiaa | 1.5E-04 | -4.0E-04 | 7.1E-04 | 0.59 | |||
| PE | Theta | MCIa | -9.2E-05 | -3.0E-04 | 1.2E-04 | 0.39 | |
| AD dementiaa | -2.5E-04 | -4.9E-04 | -7.6E-06 | < .05* | |||
| wSMI | Theta | MCIa | 1.5E-05 | -1.4E-04 | 1.7E-04 | 0.85 | |
| AD dementiaa | 1.5E-04 | -2.8E-05 | 3.4E-04 | 0.10 | |||
| JPEinv | Theta | MCIa | -5.0E-05 | -1.7E-04 | 6.7E-05 | 0.40 | |
| AD dementiaa | -1.3E-04 | -2.7E-04 | 6.9E-06 | 0.06 | |||
AEC-c Corrected amplitude envelope correlation, PLI Phase lag index, PE Permutation entropy, wSMI Weighted symbolic mutual information, JPEinv Inverted joint permutation entropy
*p<.05, **p<.01, ***p<.001
aRandom intercept on subject level
bRandom intercept and random slope on subject level
Table 7.
Results of the group-wise LMM analysis performed to evaluate change in global EEG measures over time (in months) in Aβ + MCI or AD dementia patients. Regression coefficients (β) and 95% confidence intervals (CI) of the Time effects are reported. Estimates for the Group*Time interaction effects, as well as estimates adjusted for age, sex and medication use are presented in Additional file 2 (Table S6)
| Region | Measure | Frequency band | Disease stage | β | 95% CI | p-value | |
|---|---|---|---|---|---|---|---|
| Global | Relative power | Theta | MCIb | 1.8E-03 | 1.1E-03 | 2.6E-03 | < .001*** |
| AD dementiab | 9.3E-04 | -4.6E-05 | 1.9E-03 | 0.07 | |||
| Alpha1 | MCIb | -2.4E-04 | -1.3E-03 | 7.8E-04 | 0.64 | ||
| AD dementiab | -9.9E-04 | -2.2E-03 | 1.8E-04 | 0.10 | |||
| Alpha2 | MCIa | -1.9E-04 | 1.0E-03 | 6.2E-04 | 0.64 | ||
| AD dementiaa | -4.8E-04 | -1.4E-03 | 4.6E-04 | 0.32 | |||
| Beta | MCIa | -7.0E-04 | -1.3E-03 | -5.1E-05 | < .05* | ||
| AD dementiaa | -3.2E-04 | -1.1E-03 | 4.3E-04 | 0.40 | |||
| AEC-c | Alpha | MCIa | -1.7E-04 | -5.9E-04 | 2.5E-04 | 0.42 | |
| AD dementiaa | 1.3E-05 | -4.7E-04 | 5.0E-04 | 0.96 | |||
| Beta | MCIa | -3.4E-05 | -1.9E-04 | 1.2E-04 | 0.67 | ||
| AD dementiaa | -9.1E-05 | -2.7E-04 | 9.3E-05 | 0.33 | |||
| PLI | Theta | MCIa | 1.3E-04 | -3.2E-04 | 5.8E-04 | 0.58 | |
| AD dementiaa | 1.8E-04 | -3.5E-04 | 7.0E-04 | 0.50 | |||
| PE | Theta | MCIa | -5.5E-05 | -2.6E-04 | 1.5E-04 | 0.60 | |
| AD dementiaa | -2.3E-04 | -4.6E-04 | 1.2E-05 | 0.06 | |||
| wSMI | Theta | MCIa | 2.9E-06 | -1.5E-04 | 1.6E-04 | 0.97 | |
| AD dementiaa | 1.5E-04 | -3.3E-05 | 3.3E-04 | 0.11 | |||
| JPEinv | Theta | MCIa | -5.6E-06 | -1.4E-04 | 1.3E-04 | 0.93 | |
| AD dementiaa | -1.2E-04 | -2.8E-04 | 3.4E-05 | 0.12 | |||
AEC-c Corrected amplitude envelope correlation, PLI Phase lag index, PE Permutation entropy, wSMI Weighted symbolic mutual information, JPEinv Inverted joint permutation entropy
*p<.05, **p<.01, ***p<.001
aRandom intercept on subject level
bRandom intercept and random slope on subject level
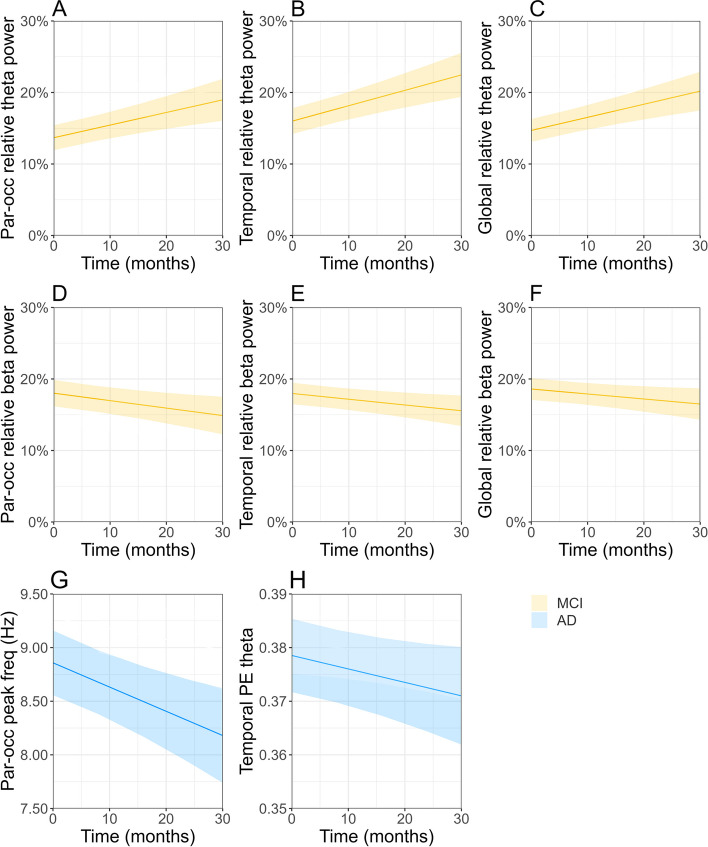
Electrophysiological deterioration was most prominent in MCI subjects, reflected by significant development of 6 EEG measures over time (Fig. 3A-F). Similar to the whole-group analysis, strongest effects were reported for regional measures (Tables 5 and 6). We found a significant increase in parieto-occipital, temporal, and global relative theta power (Fig. 3A-C), while a significant decrease was demonstrated for parieto-occipital, temporal, and global relative beta power (Fig. 3D-F). The AD dementia group showed a significant decrease of the parieto-occipital peak frequency and temporal PE theta over time. The direction of reported effects for the remaining measures was largely similar across groups (Tables 5, 6 and 7). We report a downward trend (although not significant) in parieto-occipital, temporal, and global AEC-c beta, relative alpha2 power and PE theta, as well as a positive trend in PLI theta connectivity. Global and temporal alpha1 power and JPEinv connectivity decreased in both groups, whereas wSMI theta connectivity increased over time.
Fig. 3.
A-F Estimated trajectories and 95% confidence intervals for EEG measures in Aβ + MCI or AD dementia patients. Significant group-wise estimates are visualized (p < .05). A-C Parieto-occipital, temporal, and global relative theta power, MCI (yellow). D-F Parieto-occipital, temporal, and global relative relative beta power, MCI. G Parieto-occipital peak frequency (in Hz), AD dementia (blue). H Temporal permutation entropy (PE) theta, AD dementia
EEG measures sensitive to change
Table 8 displays the subset of EEG measures that was included in the second part of the study. The EEG measures most sensitive to change in the whole-group LMM analysis included temporal relative theta and beta power and the parieto-occipital peak frequency. For the group-wise LMM analysis, this included temporal relative theta power and parieto-occipital relative beta power for MCI patients and the parieto-occipital peak frequency and temporal PE theta for AD dementia patients.
Table 8.
Subset of EEG measures most sensitive to change
| Analyzed subjects | Region | Measure | Frequency band |
|---|---|---|---|
| Whole-group | Temporal | Relative power | Theta, beta |
| Parieto-occipital | Peak frequency | - | |
| MCI | Temporal | Relative power | Theta |
| Parieto-occipital | Relative power | Beta | |
| AD dementia | Parieto-occipital | Peak frequency | - |
| Temporal | Permutation entropy | Theta |
Longitudinal effect sizes
To effectively compare the relative sensitivity to change of the EEG measures, yearly and two-yearly whole-group and group-wise effect sizes were computed from the LMM results. The largest longitudinal effect size was reported for temporal relative theta power (1 year: d = 0.23, 2 years: d = 0.45), followed by the parieto-occipital peak frequency (1 year: d = 0.15, 2 years: d = 0.30) and temporal relative beta power (1 year: d = 0.12, 2 years: d = 0.24). Larger effect sizes were reported for the individual MCI (1 year: temporal relative theta power d = 0.30, parieto-occipital beta power d = 0.14, 2 years: temporal relative theta power d = 0.60, parieto-occipital beta power d = 0.28) and AD dementia subgroups (1 year: parieto-occipital peak frequency d = 0.23, temporal PE theta d = 0.11, 2 years: parieto-occipital peak frequency d = 0.45, temporal PE theta d = 0.22). Effect sizes for different treatment scenarios (i.e., 50% less deterioration and 50% improvement) are displayed in Table S7 & S8 in Additional file 2.
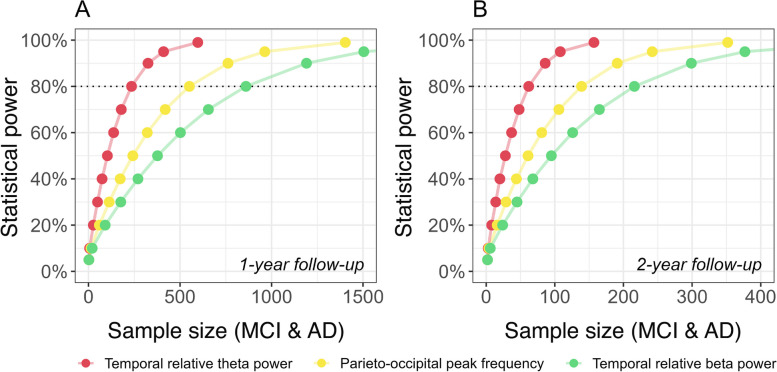
Sample size calculations
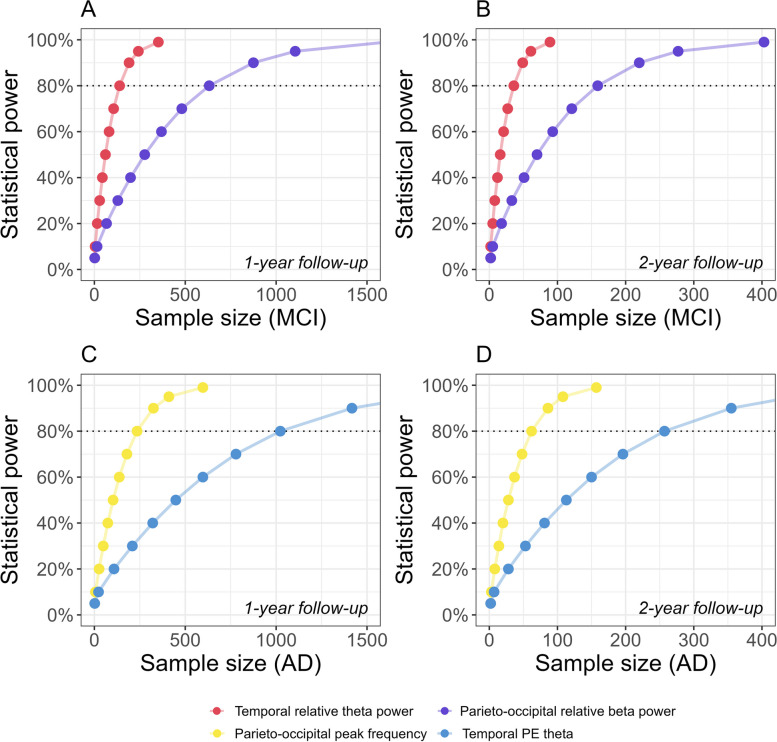
We estimated the number of participants required to demonstrate different treatment effects on the development of EEG outcome measures over time in hypothetical clinical trials of 1- or 2-year duration. For a 1-year trial, including both MCI and AD dementia patients, the minimum sample size per arm required to detect a stabilizing effect on progression of temporal relative theta, the parieto-occipital peak frequency, and temporal relative beta power at 80% power was 235, 551, and 860, respectively. For trials with a duration of 2 years, these estimates decreased by a factor of four to 62, 139, and 216 (Fig. 4, Table 9).
Fig. 4.
A-B Statistical power as a function of sample size (Aβ + MCI and AD dementia). The minimum required sample size per arm was estimated at 0.05 to 99% power for 1-year (A) and 2-year (B) trial duration. Effect sizes for EEG outcome measures were computed based on significant whole-group LMM results (Table S7, Additional file 2)
Table 9.
Required sample sizes (per arm) to detect different treatment effects on EEG outcome measures in Aβ + AD patients (MCI and AD dementia) in a hypothetical trial of 1- or 2-year duration, at 80% power
| Subjects | Region | Frequency band | Measure | Sample size (50% less deterioration) | Sample size (stabilization) | Sample size (50% improvement) | |||
|---|---|---|---|---|---|---|---|---|---|
| 1 year | 2 years | 1 year | 2 years | 1 year | 2 years | ||||
| Whole-group (MCI and AD dementia) | Temporal | Theta | Relative power | 1023 | 235 | 235 | 62 | 108 | 28 |
| Parieto-occipital | - | Peak frequency | 2525 | 551 | 551 | 139 | 257 | 62 | |
| Temporal | Beta | Relative power | 3436 | 860 | 860 | 216 | 383 | 102 | |
Stratification based on disease severity at baseline revealed differences in the development of EEG measures over time between MCI and AD dementia patients (Fig. 3, Tables 5, 6 and 7). Not all EEG measures showed significant change over time in each group. Figure 5 and Table 10 display sample size estimates for hypothetical trials that would specifically target MCI (Fig. 5A, B) or AD dementia patients (Fig. 5C, D). Minimum required sample sizes are substantially lower for trials focusing on a single disease stage. To reliably assess a stabilizing treatment effect in MCI patients in a 2-year trial, the minimum required sample size per arm would be 36 or 159 for temporal relative theta power and parieto-occipital relative beta power, respectively. The parieto-occipital peak frequency and temporal PE theta are most sensitive to change in AD dementia patients. Two-year AD dementia trials should include a minimum of 62 or 257 patients per arm to detect a stabilizing treatment effect on the respective measures. As expected, required sample sizes are substantially larger for treatments that slow down (rather than stabilize) the rate of deterioration of EEG, whereas required sample sizes are smaller for treatments that reverse deterioration (Tables 9 and 10).
Fig. 5.
A-D Statistical power as a function of sample size (Aβ + MCI or AD dementia patients). The minimum required sample size per arm was estimated at 0.05 to 99% power for 1-year (A, C) and 2-year (B, D) trial duration. Effect sizes for EEG outcome measures were computed based on significant group-wise LMM results (Table S8, Additional file 2)
Table 10.
Required sample sizes (per arm) to detect different treatment effects on EEG outcome measures in Aβ + MCI or AD dementia patients, in a hypothetical trial of 1- or 2-year duration, at 80% power
| Subjects | Region | Frequency band | Measure | Sample size (50% less deterioration) | Sample size (stabilization) | Sample size (50% improvement) | |||
|---|---|---|---|---|---|---|---|---|---|
| 1 year | 2 years | 1 year | 2 years | 1 year | 2 years | ||||
| MCI | Temporal | Theta | Relative power | 551 | 139 | 139 | 36 | 62 | 17 |
| Parieto-occipital | Beta | Relative power | 2525 | 632 | 632 | 159 | 282 | 71 | |
| AD dementia | Parieto-occipital | - | Peak frequency | 1023 | 235 | 235 | 62 | 108 | 28 |
| Temporal | Theta | PE | 3436 | 1023 | 1023 | 257 | 429 | 115 | |
Discussion
This retrospective longitudinal EEG study demonstrates significant deterioration of global, parieto-occipital, and temporal resting-state EEG measures over time (including relative theta, beta power, theta band signal variability, and peak frequency) in Aβ + patients with MCI or dementia due to AD. Effects were measurable after a period as short as 1 month. We provide support for the inclusion of EEG outcome measures in AD clinical trials, as their fast rate of deterioration may facilitate early detection of treatment effects on neuronal function. EEG measures’ sensitivity to change depended on the region-of-interest and the disease severity of subjects. The effect of baseline age, gender, and medication use on the development of the EEG measures over time was deemed negligible based on covariate adjusted analysis. When designing a trial with 1-year follow-up, the estimated sample size per arm (with two arms and 1:1 randomization, at 80% power) required to detect a stabilizing treatment effect on temporal relative theta power and parieto-occipital relative beta power in MCI patients was 139 or 632, respectively. For a 2-year follow-up period, these numbers were reduced to 36 or 159 MCI patients per arm. When a treatment is expected to slow down (rather than stabilize) the deterioration of EEG measures, it is advisable to set up a more conservative trial with larger sample sizes. Conversely, if a treatment is hypothesized to reverse deterioration of EEG measures, smaller sample sizes can be considered.
Our results are in line with previous studies reporting spectral EEG measures as most consistent for monitoring AD progression [59] and response to interventions in AD clinical trials [60, 61]. In agreement with our hypothesis, most prominent effects were localized in temporal regions, with highest sensitivity for relative theta power. This is consistent with earlier findings [13, 14, 35, 62].
Disease severity at baseline influenced EEG measures’ rates of change, with fastest deterioration reported in MCI subjects. The MCI group showed significant development over time for 6 EEG measures, including parieto-occipital, temporal, and global relative theta and beta power. AD dementia patients showed a significant decrease of the parieto-occipital peak frequency and temporal PE theta. We do not report significant Time x Group effects (Additional file 2, Table S4-6), indicating that the development of EEG measures over time did not differ significantly between groups.
Underlying mechanisms
A growing body of evidence suggests that large-scale circuit and network function are affected by a neuronal excitation/inhibition (E/I) imbalance in AD (for a recent review, see [63]). Neuronal hyperactivity has been demonstrated in early stages of AD, both in animal models (using in vivo calcium imaging, [64, 65] and human EEG data (using spike detection, [66]). There is substantial evidence that soluble Aβ is crucial for this increase in neuronal activity [67, 68]. Soluble tau has on the other hand been associated with the silencing of neuronal activity. The presence of neurofibrillary tangles has been linked to changes in the number and morphology of dendritic spines in pyramidal cells of AD patients. Considering that dendritic spines are fundamental structures in memory, learning, and cognition, this is thought to be a key event in AD pathogenesis [69]. Abnormal spectral power and functional connectivity within the alpha and delta-theta frequency ranges have previously been shown to be differentially associated with Aβ and tau accumulations in patients with AD [70, 71]. Microscale hyperactivity has moreover been linked to the large-scale oscillatory slowing of M/EEG signals that is observed in AD patients, using a whole-brain computational network model [72]. The increase of relative theta power and decrease of relative beta power that we report in this study may be indirect measures of (Aβ-mediated) hyperactivity of pyramidal cells and/or interneuron dysfunction. This raises the question whether measures that quantify the E/I ratio of neuronal oscillations more directly could be more sensitive to change than conventional spectral measures. The validity of available EEG E/I ratio measures (e.g., functional E/I balance [73], fitting oscillations and one over f (“FOOOF”) [74]) however remains to be evaluated in further studies. The density of Aβ deposits and neurofibrillary tangles is known to vary across cortical regions and disease stages [75–77]. Studies correlating EEG measures with PET maps of Aβ and tau accumulation may provide an explanation for the regional- and group-differences demonstrated in this study.
Sample size considerations
On whole-group level, largest effect sizes were reported for temporal relative theta and beta power and the parieto-occipital peak frequency. Temporal relative theta and parieto-occipital relative beta power exhibited largest effect sizes in MCI patients. AD dementia subjects displayed largest effect sizes for the parieto-occipital peak frequency and temporal PE theta. Corresponding sample sizes estimates were substantially lower for hypothetical trials focusing on a single disease stage than for trials including MCI and AD dementia patients. Clinical trials of phases 2 and 3 typically include 100 to 300 and 300 to 3000 patients in each patient group [78]. Our results suggest that EEG outcome measures are appropriate for trials of this size, particularly when outcome measures are tailored to the patient group under investigation (MCI or AD dementia). If these findings are replicated, they might even lower the minimum number of required trial participants. We did not differentiate between converters and non-converters in the MCI group. During the design stage of a clinical trial, information on future clinical progression of its participants is unknown. We therefore provided sample size estimates for groups categorized based on baseline diagnosis only.
The role of EEG outcome measures in AD clinical trials
Finding tools with sufficient sensitivity to detect drug-placebo differences in pre-dementia stages of AD is challenging. EEG measures however appear to be sensitive to change in early stages of disease. They could play an important role in early stages of drug development, for instance by demonstrating target engagement. In drug development programs, a proof-of-concept (POC) Phase 2a study is typically performed to help a drug developer make a “Go/NoGo” decision based on the efficacy performance of a medical agent. POC can be based on a clinical response, a biomarker response or a combination of both types of outcome measures. So far, no biomarker has been granted surrogate status in AD drug development [6]. This means that proof of target engagement (i.e., biomarker changes induced by a therapy) does not guarantee clinical benefit at a later stage. Nevertheless, biomarker outcomes are important to understand the biological impact of an agent. EEG outcome measures could provide insight into (rescued or restored) circuit-level function. Moreover, a candidate treatment and its Phase 3 program can be de-risked by acquiring a set of biomarkers and clinical measures that support its potential effectiveness. Target engagement markers that are currently employed in AD clinical trials (i.e., fluid, imaging) are obtained using invasive and/or expensive techniques. EEG outcome measures could be a cost-effective, non-invasive alternative to demonstrate target engagement.
Strengths
This study presents one of the largest and most comprehensive longitudinal EEG analyses in amyloid-positive AD patients to date. We provide recommendations for the design of future AD trials in which EEG measures will be used as secondary endpoints. In contrast to earlier longitudinal EEG studies [32, 33, 35–38], diagnoses were based on recent diagnostic guidelines and extensive diagnostic screening. We employed linear mixed effects models to model the development of a large variety of global and regional EEG measures over time. LMMs are known for their ability to handle missing data points and variable measurement schedules between individuals and are therefore highly valuable when analyzing a clinical dataset [79]. Our findings also emerged after controlling for baseline age, sex, and medication use, adding to their validity.
Limitations
As discussed in the "Underlying mechanisms" section, the presence of AD pathology is associated with changes in neuronal activity, which consequently affect EEG measures. All AD patients included in this study were positive for amyloid deposition. The extent of tau pathology and neurodegeneration (as assessed using cerebrospinal fluid p-tau and t-tau levels) however varied between patients (see Table 1) and was not characterized for the full cohort. This likely contributed to increased variability in the development of EEG measures over time among patients. Our results are not consistent with studies reporting changes in functional connectivity strength over time in AD patients [15, 32]. This includes a decrease in alpha and beta band AEC-c in temporal and parietal regions [80] and increased theta band PLI [81]. We also do not report significant differences in global alpha 2 and beta power, PE theta, AEC-c alpha and beta, PLI theta, wSMI theta and JPEinv theta between MCI and AD dementia patients at baseline, as was previously reported in cross-sectional studies [14, 15, 54, 55]. These discrepancies may be explained by a potential selection bias in the clinical part of our dataset. While EEG recording is part of the standardized diagnostic work-up of our center [41], it is not a routine examination during follow-up visits. Clinicians may request an additional EEG recording in situations where there is uncertainty about a patients’ diagnosis, or when aberrant symptoms or progression profiles are observed. As a result, our clinical cohort may be somewhat atypical compared to the general Alzheimer population, also reflected by the high age of MCI compared to AD dementia subjects at baseline. When LMM analysis was performed for the subset of patients that participated in a clinical trial (n = 55) (see Additional file 2, Table S9), reported effect sizes were considerably larger. This suggests that the well-controlled patient inclusion process of clinical trials may further reduce the minimum sample size required to detect a treatment effect on EEG outcome measures. In the future, we aim to (re)perform longitudinal EEG analysis within the context of AD clinical trials. Including a larger number of subjects with structured follow-up visits will improve longitudinal estimates and will allow for a better comparison of the development of EEG measures between patients in different disease stages. Analyzing data from more than two time-points for each subject would also allow potential non-linear aspects of change to be captured. Moreover, we wish to evaluate the potential value of combined (e.g., Hub Disruption Index [82], Pathological Oscillatory Slowing Index [83]), and less conventional EEG outcome measures for longitudinal effect monitoring in AD clinical trials.
Conclusion
The presented findings indicate that EEG measures, particularly spectral power, are promising secondary endpoints for AD interventions. They are sensitive to change over a short time period and have complementary value to neuroimaging biomarkers, by providing a more direct measurement of neurotransmission and synaptic activity. The selection of EEG outcome measures should be guided by the targeted disease stage (i.e., MCI or AD dementia). Based on our sample size estimations, EEG measures have potential to reduce the size, duration, and therefore costs of clinical trials, particularly for those aimed at slowing disease progression in MCI due to AD. Our study contributes to improved trial design, by enabling informed decision-making regarding the appropriate sample size for interpreting EEG results. Additional longitudinal studies are needed to validate these findings and to relate EEG measures more extensively to clinical and cognitive outcomes, ideally within the context of a clinical trial.
Supplementary Information
Additional file 1. Supplementary methods. Details of the linear mixed effect model analyses.
Additional file 2: Table S1. Neuropsychological test results for memory clinic patients at baseline. Table S2. Neuropsychological test results for trial participants at baseline. Table S3. Comparison of baseline EEG measures between diagnostic groups. Table S4. Results of the group-wise LMM analysis performed to evaluate change in parieto-occipital EEG measures over time (in months) in Aβ+ MCI or AD dementia patients. Table S5. Results of the group-wise LMM analysis performed to evaluate change in temporal EEG measures over time (in months) in Aβ+ MCI or AD dementia patients. Table S6. Results of the group-wise LMM analysis performed to evaluate change in global EEG measures over time (in months) in Aβ+ MCI or AD dementia patients. Table S7. Longitudinal effect sizes of whole-group LMM results. Table S8. Longitudinal effect sizes of group-wise LMM results. Table S9. Three-month effect sizes (measured as Cohen’s d) for EEG measures that demonstrated a significant change over time in the trial-, clinical- and total dataset [84].
Acknowledgements
The authors would like to thank the participants of the Amsterdam Dementia Cohort for their contribution. Research of Amsterdam Alzheimer Center is part of the Neurodegeneration program of Amsterdam Neuroscience. The Amsterdam Alzheimer Center is supported by Alzheimer Nederland and Stichting VUmc Fonds. The authors thank technicians P.J. Ris, C.H. Plugge, N. Sijsma, N.C. Akemann, N. Zwagerman, and M.C. Alting Siberg for the acquisition of the EEG data. The authors thank the technician in training J.E. Leistra for assisting in epoch selection based on visual inspection.
Abbreviations
- Aβ( +)
Amyloid beta (positive)
- AD
Alzheimer’s disease
- AEC-c
Corrected amplitude envelope correlation
- AED
Antiepileptic drugs
- CSF
Cerebrospinal fluid
- EEG
Electroencephalography
- JPEinv
Inverted joint permutation entropy
- LMM
Linear mixed model
- MCI
Mild cognitive impairment
- MMSE
Mini mental state examination
- MRI
Magnetic resonance imaging
- MTA
Medial temporal lobe atrophy
- PE
Permutation entropy
- PET
Positron emission tomography
- PLI
Phase lag index
- POC
Proof of concept
- SCD
Subjective cognitive decline
- wSMI
Weighted symbolic mutual information
Authors’ contributions
E.S. - Conceptualization; Data curation; Formal analysis; Visualization; Writing - original draft. W.H., C.S., A.G. - Conceptualization; Supervision; Writing - review and editing. J.T. - Supervision; Writing – review and editing.
Funding
W.H. and A.G. are founders of the EEGlab at Amsterdam UMC, location VUmc, The Netherlands. E.S. is part of the EEGlab research team at Amsterdam UMC, location VUmc. The EEGlab performs central EEG analysis for clinical trials funded by Vivoryon, EIP-Pharma, Fujifilm Toyoma, Immunobrain, and Treeway. This funding does not involve personal support. C.S. and J.T. did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The data which support the findings of this study are not freely available, but may be provided upon reasonable request. Due to the clinical nature of the data, a formal data sharing agreement is needed before any data can be shared.
Declarations
Ethics approval and consent to participate
The local Medical Ethics Committee (Amsterdam UMC, location VUmc) has approved a general protocol for biobanking and use of the clinical data for research purposes (2016.061; 2017.315). All subjects gave written informed consent for the use of their data for research purposes.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jack CR, Jr, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA research framework: toward a biological definition of Alzheimer's disease. Alzheimers Dement. 2018;14(4):535–562. doi: 10.1016/j.jalz.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nichols E, Steinmetz JD, Vollset SE, Fukutaki K, Chalek J, Abd-Allah F, et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2022;7(2):e105–e125. doi: 10.1016/S2468-2667(21)00249-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koch G, Casula EP, Bonnì S, Borghi I, Assogna M, Minei M, et al. Precuneus magnetic stimulation for Alzheimer’s disease: a randomized, sham-controlled trial. Brain. 2022;145(11):3776–3786. doi: 10.1093/brain/awac285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jutten RJ, Papp KV, Hendrix S, Ellison N, Langbaum JB, Donohue MC, et al. Why a clinical trial is as good as its outcome measure: a framework for the selection and use of cognitive outcome measures for clinical trials of Alzheimer's disease. Alzheimers Dement. 2023;19(2):708–720. doi: 10.1002/alz.12773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schneider LS, Goldberg TE. Composite cognitive and functional measures for early stage Alzheimer's disease trials. Alzheimers Dement. 2020;12(1):e12017. doi: 10.1002/dad2.12017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cummings J, Feldman HH, Scheltens P. The "rights" of precision drug development for Alzheimer's disease. Alzheimers Res Ther. 2019;11(1):76. [DOI] [PMC free article] [PubMed]
- 7.Scheltens P, De Strooper B, Kivipelto M, Holstege H, Chételat G, Teunissen CE, et al. Alzheimer's disease. The Lancet. 2021;397(10284):1577–1590. doi: 10.1016/S0140-6736(20)32205-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Babiloni C, Arakaki X, Azami H, Bennys K, Blinowska K, Bonanni L, et al. Measures of resting state EEG rhythms for clinical trials in Alzheimer's disease: recommendations of an expert panel. Alzheimers Dementia. 2021;17(9):1528–1553. doi: 10.1002/alz.12311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Straaten EC, Scheltens P, Gouw AA, Stam CJ. Eyes-closed task-free electroencephalography in clinical trials for Alzheimer’s disease: an emerging method based upon brain dynamics. Alzheimers Res Ther. 2014;6(9):1–10. doi: 10.1186/s13195-014-0086-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gouw AA, Alsema AM, Tijms BM, Borta A, Scheltens P, Stam CJ, et al. EEG spectral analysis as a putative early prognostic biomarker in nondemented, amyloid positive subjects. Neurobiol Aging. 2017;57:133–142. doi: 10.1016/j.neurobiolaging.2017.05.017. [DOI] [PubMed] [Google Scholar]
- 11.Musaeus CS, Engedal K, Høgh P, Jelic V, Mørup M, Naik M, et al. EEG theta power is an early marker of cognitive decline in dementia due to Alzheimer's disease. J Alzheimers Dis. 2018;64(4):1359–1371. doi: 10.3233/JAD-180300. [DOI] [PubMed] [Google Scholar]
- 12.Babiloni C, Binetti G, Cassetta E, Cerboneschi D, Dal Forno G, Del Percio C, et al. Mapping distributed sources of cortical rhythms in mild Alzheimer's disease. A multicentric EEG study. Neuroimage. 2004;22(1):57–67. doi: 10.1016/j.neuroimage.2003.09.028. [DOI] [PubMed] [Google Scholar]
- 13.Huang C, Wahlund L, Dierks T, Julin P, Winblad B, Jelic V. Discrimination of Alzheimer's disease and mild cognitive impairment by equivalent EEG sources: a cross-sectional and longitudinal study. Clin Neurophysiol. 2000;111(11):1961–1967. doi: 10.1016/s1388-2457(00)00454-5. [DOI] [PubMed] [Google Scholar]
- 14.Jeong J. EEG dynamics in patients with Alzheimer's disease. Clin Neurophysiol. 2004;115(7):1490–1505. doi: 10.1016/j.clinph.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Briels CT, Stam CJ, Scheltens P, Bruins S, Lues I, Gouw AA. In pursuit of a sensitive EEG functional connectivity outcome measure for clinical trials in Alzheimer’s disease. Clin Neurophysiol. 2020;131(1):88–95. doi: 10.1016/j.clinph.2019.09.014. [DOI] [PubMed] [Google Scholar]
- 16.Stam C, De Haan W, Daffertshofer A, Jones B, Manshanden I, van Cappellen van Walsum A-M, et al. Graph theoretical analysis of magnetoencephalographic functional connectivity in Alzheimer's disease. Brain. 2009;132(1):213–224. doi: 10.1093/brain/awn262. [DOI] [PubMed] [Google Scholar]
- 17.Stam CJ, Jones B, Manshanden I, Van Walsum AvC, Montez T, Verbunt JP, et al. Magnetoencephalographic evaluation of resting-state functional connectivity in Alzheimer's disease. Neuroimage. 2006;32(3):1335–1344. doi: 10.1016/j.neuroimage.2006.05.033. [DOI] [PubMed] [Google Scholar]
- 18.Crossley NA, Mechelli A, Scott J, Carletti F, Fox PT, McGuire P, et al. The hubs of the human connectome are generally implicated in the anatomy of brain disorders. Brain. 2014;137(8):2382–2395. doi: 10.1093/brain/awu132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Haan W, Mott K, Van Straaten EC, Scheltens P, Stam CJ. Activity dependent degeneration explains hub vulnerability in Alzheimer's disease. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van den Heuvel MP, Sporns O. Network hubs in the human brain. Trends Cogn Sci. 2013;17(12):683–696. doi: 10.1016/j.tics.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 21.Yu M, Engels MMA, Hillebrand A, van Straaten ECW, Gouw AA, Teunissen C, et al. Selective impairment of hippocampus and posterior hub areas in Alzheimer’s disease: an MEG-based multiplex network study. Brain. 2017;140(5):1466–1485. doi: 10.1093/brain/awx050. [DOI] [PubMed] [Google Scholar]
- 22.Ando M, Nobukawa S, Kikuchi M, Takahashi T. Identification of Electroencephalogram Signals in Alzheimer's Disease by Multifractal and Multiscale Entropy Analysis. Front Neurosci. 2021;15:667614. [DOI] [PMC free article] [PubMed]
- 23.Echegoyen I, López-Sanz D, Martínez JH, Maestú F, Buldú JM. Permutation entropy and statistical complexity in mild cognitive impairment and Alzheimer’s disease: an analysis based on frequency bands. Entropy. 2020;22(1):116. doi: 10.3390/e22010116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maturana-Candelas A, Gómez C, Poza J, Pinto N, Hornero R. EEG characterization of the Alzheimer’s disease continuum by means of multiscale entropies. Entropy. 2019;21(6):544. doi: 10.3390/e21060544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shumbayawonda E, López-Sanz D, Bruña R, Serrano N, Fernández A, Maestú F, et al. Complexity changes in preclinical Alzheimer’s disease: an MEG study of subjective cognitive decline and mild cognitive impairment. Clin Neurophysiol. 2020;131(2):437–445. doi: 10.1016/j.clinph.2019.11.023. [DOI] [PubMed] [Google Scholar]
- 26.Kowalski JW, Gawel M, Pfeffer A, Barcikowska M. The diagnostic value of EEG in Alzheimer disease: correlation with the severity of mental impairment. J Clin Neurophysiol. 2001;18(6):570–575. doi: 10.1097/00004691-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Briels CT, Stam CJ, Scheltens P, Gouw AA. The predictive value of normal EEGs in dementia due to Alzheimer’s disease. Ann Clin Transl Neurol. 2021;8(5):1038–1048. doi: 10.1002/acn3.51339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gianotti LR, Künig G, Lehmann D, Faber PL, Pascual-Marqui RD, Kochi K, et al. Correlation between disease severity and brain electric LORETA tomography in Alzheimer's disease. Clin Neurophysiol. 2007;118(1):186–196. doi: 10.1016/j.clinph.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 29.Benwell CSY, Davila-Pérez P, Fried PJ, Jones RN, Travison TG, Santarnecchi E, et al. EEG spectral power abnormalities and their relationship with cognitive dysfunction in patients with Alzheimer's disease and type 2 diabetes. Neurobiol Aging. 2020;85:83–95. doi: 10.1016/j.neurobiolaging.2019.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fonseca LC, Tedrus GM, Prandi LR, Almeida AM, Furlanetto DS. Alzheimer's disease: relationship between cognitive aspects and power and coherence EEG measures. Arq Neuropsiquiatr. 2011;69(6):875–881. doi: 10.1590/s0004-282x2011000700005. [DOI] [PubMed] [Google Scholar]
- 31.Yang AC, Wang SJ, Lai KL, Tsai CF, Yang CH, Hwang JP, et al. Cognitive and neuropsychiatric correlates of EEG dynamic complexity in patients with Alzheimer's disease. Prog Neuropsychopharmacol Biol Psychiatry. 2013;47:52–61. doi: 10.1016/j.pnpbp.2013.07.022. [DOI] [PubMed] [Google Scholar]
- 32.Rossini PM, Del Percio C, Pasqualetti P, Cassetta E, Binetti G, Dal Forno G, et al. Conversion from mild cognitive impairment to Alzheimer's disease is predicted by sources and coherence of brain electroencephalography rhythms. Neuroscience. 2006;143(3):793–803. doi: 10.1016/j.neuroscience.2006.08.049. [DOI] [PubMed] [Google Scholar]
- 33.Dattola S, La Foresta F. An eLORETA longitudinal analysis of resting state EEG rhythms in Alzheimer’s disease. Appl Sci. 2020;10(16):5666. [Google Scholar]
- 34.Morabito FC, Campolo M, Labate D, Morabito G, Bonanno L, Bramanti A, et al. A longitudinal EEG study of Alzheimer's disease progression based on a complex network approach. Int J Neural Syst. 2015;25(2):1550005. doi: 10.1142/S0129065715500057. [DOI] [PubMed] [Google Scholar]
- 35.Jelic V, Johansson S, Almkvist O, Shigeta M, Julin P, Nordberg A, et al. Quantitative electroencephalography in mild cognitive impairment: longitudinal changes and possible prediction of Alzheimer’s disease. Neurobiol Aging. 2000;21(4):533–540. doi: 10.1016/s0197-4580(00)00153-6. [DOI] [PubMed] [Google Scholar]
- 36.Lehtovirta M, Partanen J, Könönen M, Hiltunen J, Helisalmi S, Hartikainen P, et al. A longitudinal quantitative EEG study of Alzheimer's disease: relation to apolipoprotein E polymorphism. Dement Geriatr Cogn Disord. 2000;11(1):29–35. doi: 10.1159/000017210. [DOI] [PubMed] [Google Scholar]
- 37.Meghdadi AH, Stevanović Karić M, McConnell M, Rupp G, Richard C, Hamilton J, et al. Resting state EEG biomarkers of cognitive decline associated with Alzheimer’s disease and mild cognitive impairment. PLoS ONE. 2021;16(2):e0244180. doi: 10.1371/journal.pone.0244180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Soininen H, Partanen J, Laulumaa V, Pääkkönen A, Helkala EL, Riekkinen PJ. Serial EEG in Alzheimer's disease: 3 year follow-up and clinical outcome. Electroencephalogr Clin Neurophysiol. 1991;79(5):342–348. doi: 10.1016/0013-4694(91)90198-d. [DOI] [PubMed] [Google Scholar]
- 39.Dubois B, Epelbaum S, Nyasse F, Bakardjian H, Gagliardi G, Uspenskaya O, et al. Cognitive and neuroimaging features and brain β-amyloidosis in individuals at risk of Alzheimer's disease (INSIGHT-preAD): a longitudinal observational study. Lancet Neurol. 2018;17(4):335–346. doi: 10.1016/S1474-4422(18)30029-2. [DOI] [PubMed] [Google Scholar]
- 40.McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimer's Dementia. 2011;7(3):263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Van der Flier WM, Scheltens P. Amsterdam dementia cohort: performing research to optimize care. J Alzheimers Dis. 2018;62(3):1091–1111. doi: 10.3233/JAD-170850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tijms BM, Willemse EAJ, Zwan MD, Mulder SD, Visser PJ, van Berckel BNM, et al. Unbiased Approach to Counteract Upward Drift in Cerebrospinal Fluid Amyloid-β 1-42 Analysis Results. Clin Chem. 2018;64(3):576–85. [DOI] [PubMed]
- 43.Leuzy A, Carter SF, Chiotis K, Almkvist O, Wall A, Nordberg A. Concordance and diagnostic accuracy of [11C]PIB PET and cerebrospinal fluid biomarkers in a sample of patients with mild cognitive impairment and Alzheimer’s disease. J Alzheimers Dis. 2015;45:1077–1088. doi: 10.3233/JAD-142952. [DOI] [PubMed] [Google Scholar]
- 44.Ossenkoppele R, Tolboom N, Foster-Dingley JC, et al. Longitudinal imaging of Alzheimer pathology using [11C] PIB, [18F]FDDNP and [18F]FDG PET. Eur J Nucl Med Mol Imaging. 2012;39:990–1000. doi: 10.1007/s00259-012-2102-3. [DOI] [PubMed] [Google Scholar]
- 45.Mulder C, Verwey NA, van der Flier WM, Bouwman FH, Kok A, van Elk EJ, et al. Amyloid-beta(1–42), total tau, and phosphorylated tau as cerebrospinal fluid biomarkers for the diagnosis of Alzheimer disease. Clin Chem. 2010;56(2):248–253. doi: 10.1373/clinchem.2009.130518. [DOI] [PubMed] [Google Scholar]
- 46.Hagemann D, Naumann E. The effects of ocular artifacts on (lateralized) broadband power in the EEG. Clin Neurophysiol. 2001;112(2):215–231. doi: 10.1016/s1388-2457(00)00541-1. [DOI] [PubMed] [Google Scholar]
- 47.Pope KJ, Fitzgibbon SP, Lewis TW, Whitham EM, Willoughby JO. Relation of gamma oscillations in scalp recordings to muscular activity. Brain Topogr. 2009;22(1):13–17. doi: 10.1007/s10548-009-0081-x. [DOI] [PubMed] [Google Scholar]
- 48.Whitham EM, Pope KJ, Fitzgibbon SP, Lewis T, Clark CR, Loveless S, et al. Scalp electrical recording during paralysis: quantitative evidence that EEG frequencies above 20 Hz are contaminated by EMG. Clin Neurophysiol. 2007;118(8):1877–1888. doi: 10.1016/j.clinph.2007.04.027. [DOI] [PubMed] [Google Scholar]
- 49.Brookes MJ, Woolrich MW, Barnes GR. Measuring functional connectivity in MEG: a multivariate approach insensitive to linear source leakage. Neuroimage. 2012;63(2):910–920. doi: 10.1016/j.neuroimage.2012.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bruns A, Eckhorn R, Jokeit H, Ebner A. Amplitude envelope correlation detects coupling among incoherent brain signals. NeuroReport. 2000;11(7):1509–1514. [PubMed] [Google Scholar]
- 51.Hipp JF, Hawellek DJ, Corbetta M, Siegel M, Engel AK. Large-scale cortical correlation structure of spontaneous oscillatory activity. Nat Neurosci. 2012;15(6):884–890. doi: 10.1038/nn.3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stam CJ, Nolte G, Daffertshofer A. Phase lag index: assessment of functional connectivity from multi channel EEG and MEG with diminished bias from common sources. Hum Brain Mapp. 2007;28(11):1178–1193. doi: 10.1002/hbm.20346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bandt C, Pompe B. Permutation entropy: a natural complexity measure for time series. Phys Rev Lett. 2002;88(17):174102. doi: 10.1103/PhysRevLett.88.174102. [DOI] [PubMed] [Google Scholar]
- 54.King J-R, Sitt JD, Faugeras F, Rohaut B, El Karoui I, Cohen L, et al. Information sharing in the brain indexes consciousness in noncommunicative patients. Curr Biol. 2013;23(19):1914–1919. doi: 10.1016/j.cub.2013.07.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Scheijbeler EP, van Nifterick AM, Stam CJ, Hillebrand A, Gouw AA, de Haan W. Network-level permutation entropy of resting-state MEG recordings: a novel biomarker for early-stage Alzheimer’s disease? Netw NeuroscI. 2022;6(2):382–400. doi: 10.1162/netn_a_00224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schoonhoven DN, Briels CT, Hillebrand A, Scheltens P, Stam CJ, Gouw AA. Sensitive and reproducible MEG resting-state metrics of functional connectivity in Alzheimer's disease. Alzheimers Res Ther. 2022;14(1):38. doi: 10.1186/s13195-022-00970-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Westfall J, Kenny DA, Judd CM. Statistical power and optimal design in experiments in which samples of participants respond to samples of stimuli. J Exp Psychol Gen. 2014;143(5):2020. [DOI] [PubMed]
- 58.Faul F, Erdfelder E, Lang A-G, Buchner A. G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 59.Jovicich J, Babiloni C, Ferrari C, Marizzoni M, Moretti DV, Del Percio C, et al. Two-year longitudinal monitoring of amnestic mild cognitive impairment patients with prodromal Alzheimer's disease using topographical biomarkers derived from functional magnetic resonance imaging and electroencephalographic activity. J Alzheimer's Dis. 2019;69(1):15–35. doi: 10.3233/JAD-180158. [DOI] [PubMed] [Google Scholar]
- 60.Scheltens P, Hallikainen M, Grimmer T, Duning T, Gouw AA, Teunissen CE, et al. Safety, tolerability and efficacy of the glutaminyl cyclase inhibitor PQ912 in Alzheimer’s disease: results of a randomized, double-blind, placebo-controlled phase 2a study. Alzheimers Res Ther. 2018;10(1):1–14. doi: 10.1186/s13195-018-0431-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jelic V, Dierks T, Amberla K, Almkvist O, Winblad B, Nordberg A. Longitudinal changes in quantitative EEG during long-term tacrine treatment of patients with Alzheimer's disease. Neurosci Lett. 1998;254(2):85–8. [DOI] [PubMed]
- 62.Babiloni C, Binetti G, Cassetta E, Dal Forno G, Del Percio C, Ferreri F, et al. Sources of cortical rhythms change as a function of cognitive impairment in pathological aging: a multicenter study. Clin Neurophysiol. 2006;117(2):252–268. doi: 10.1016/j.clinph.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 63.Maestú F, de Haan W, Busche MA, DeFelipe J. Neuronal excitation/inhibition imbalance: core element of a translational perspective on Alzheimer pathophysiology. Ageing Res Rev. 2021;69:101372. doi: 10.1016/j.arr.2021.101372. [DOI] [PubMed] [Google Scholar]
- 64.Busche MA, Chen X, Henning HA, Reichwald J, Staufenbiel M, Sakmann B, et al. Critical role of soluble amyloid-β for early hippocampal hyperactivity in a mouse model of Alzheimer’s disease. Proc Natl Acad Sci. 2012;109(22):8740–8745. doi: 10.1073/pnas.1206171109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Busche MA, Eichhoff G, Adelsberger H, Abramowski D, Wiederhold K-H, Haass C, et al. Clusters of hyperactive neurons near amyloid plaques in a mouse model of Alzheimer's disease. Science. 2008;321(5896):1686–1689. doi: 10.1126/science.1162844. [DOI] [PubMed] [Google Scholar]
- 66.Minkeviciene R, Rheims S, Dobszay MB, Zilberter M, Hartikainen J, Fülöp L, et al. Amyloid beta-induced neuronal hyperexcitability triggers progressive epilepsy. J Neurosci. 2009;29(11):3453–3462. doi: 10.1523/JNEUROSCI.5215-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Keskin AD, Kekuš M, Adelsberger H, Neumann U, Shimshek DR, Song B, et al. BACE inhibition-dependent repair of Alzheimer’s pathophysiology. Proc Natl Acad Sci. 2017;114(32):8631–8636. doi: 10.1073/pnas.1708106114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zott B, Simon MM, Hong W, Unger F, Chen-Engerer H-J, Frosch MP, et al. A vicious cycle of β amyloid–dependent neuronal hyperactivation. Science. 2019;365(6453):559–565. doi: 10.1126/science.aay0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.DeFelipe J. The dendritic spine story: an intriguing process of discovery. Front Neuroanat. 2015;9:14. doi: 10.3389/fnana.2015.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ranasinghe KG, Cha J, Iaccarino L, Hinkley LB, Beagle AJ, Pham J, et al. Neurophysiological signatures in Alzheimer's disease are distinctly associated with TAU, amyloid-β accumulation, and cognitive decline. Sci Transl Med. 2020;12(534):eaaz4069. doi: 10.1126/scitranslmed.aaz4069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ranasinghe KG, Verma P, Cai C, Xie X, Kudo K, Gao X, et al. Altered excitatory and inhibitory neuronal subpopulation parameters are distinctly associated with tau and amyloid in Alzheimer's disease. Elife. 2022;11:e77850. doi: 10.7554/eLife.77850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.van Nifterick AM, Gouw AA, van Kesteren RE, Scheltens P, Stam CJ, de Haan W. A multiscale brain network model links Alzheimer's disease-mediated neuronal hyperactivity to large-scale oscillatory slowing. Alzheimers Res Ther. 2022;14(1):101. doi: 10.1186/s13195-022-01041-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bruining H, Hardstone R, Juarez-Martinez EL, Sprengers J, Avramiea A-E, Simpraga S, et al. Measurement of excitation-inhibition ratio in autism spectrum disorder using critical brain dynamics. Sci Rep. 2020;10(1):9195. doi: 10.1038/s41598-020-65500-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Donoghue T, Haller M, Peterson EJ, Varma P, Sebastian P, Gao R, et al. Parameterizing neural power spectra into periodic and aperiodic components. Nat Neurosci. 2020;23(12):1655–1665. doi: 10.1038/s41593-020-00744-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Braak H, Braak E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 1991;82(4):239–259. doi: 10.1007/BF00308809. [DOI] [PubMed] [Google Scholar]
- 76.Braak H, Del Tredici K. The preclinical phase of the pathological process underlying sporadic Alzheimer’s disease. Brain. 2015;138(10):2814–2833. doi: 10.1093/brain/awv236. [DOI] [PubMed] [Google Scholar]
- 77.Thal DR, Rüb U, Orantes M, Braak H. Phases of Aβ-deposition in the human brain and its relevance for the development of AD. Neurology. 2002;58(12):1791–1800. doi: 10.1212/wnl.58.12.1791. [DOI] [PubMed] [Google Scholar]
- 78.Friedman LM, Furberg CD, DeMets DL, Reboussin DM, Granger CB. Fundamentals of clinical trials. New York: Springer; 2015.
- 79.Twisk JW. Applied longitudinal data analysis for epidemiology: a practical guide. Cambridge: Cambridge University press; 2013.
- 80.Koelewijn L, Bompas A, Tales A, Brookes MJ, Muthukumaraswamy SD, Bayer A, et al. Alzheimer's disease disrupts alpha and beta-band resting-state oscillatory network connectivity. Clin Neurophysiol. 2017;128(11):2347–2357. doi: 10.1016/j.clinph.2017.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ruiz-Gómez SJ, Hornero R, Poza J, Maturana-Candelas A, Pinto N, Gómez C. Computational modeling of the effects of EEG volume conduction on functional connectivity metrics. Application to Alzheimer’s disease continuum. J Neural Eng. 2019;16(6):066019. doi: 10.1088/1741-2552/ab4024. [DOI] [PubMed] [Google Scholar]
- 82.Achard S, Delon-Martin C, Vértes PE, Renard F, Schenck M, Schneider F, et al. Hubs of brain functional networks are radically reorganized in comatose patients. Proc Natl Acad Sci. 2012;109(50):20608–20613. doi: 10.1073/pnas.1208933109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wiesman AI, Murman DL, Losh RA, Schantell M, Christopher-Hayes NJ, Johnson HJ, et al. Spatially resolved neural slowing predicts impairment and amyloid burden in Alzheimer’s disease. Brain. 2022;145(6):2177–2189. doi: 10.1093/brain/awab430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Maruff P, Lim YY, Darby D, Ellis KA, Pietrzak RH, Snyder PJ, et al. Clinical utility of the cogstate brief battery in identifying cognitive impairment in mild cognitive impairment and Alzheimer’s disease. BMC psychology. 2013;1(1):1–11. doi: 10.1186/2050-7283-1-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplementary methods. Details of the linear mixed effect model analyses.
Additional file 2: Table S1. Neuropsychological test results for memory clinic patients at baseline. Table S2. Neuropsychological test results for trial participants at baseline. Table S3. Comparison of baseline EEG measures between diagnostic groups. Table S4. Results of the group-wise LMM analysis performed to evaluate change in parieto-occipital EEG measures over time (in months) in Aβ+ MCI or AD dementia patients. Table S5. Results of the group-wise LMM analysis performed to evaluate change in temporal EEG measures over time (in months) in Aβ+ MCI or AD dementia patients. Table S6. Results of the group-wise LMM analysis performed to evaluate change in global EEG measures over time (in months) in Aβ+ MCI or AD dementia patients. Table S7. Longitudinal effect sizes of whole-group LMM results. Table S8. Longitudinal effect sizes of group-wise LMM results. Table S9. Three-month effect sizes (measured as Cohen’s d) for EEG measures that demonstrated a significant change over time in the trial-, clinical- and total dataset [84].
Data Availability Statement
The data which support the findings of this study are not freely available, but may be provided upon reasonable request. Due to the clinical nature of the data, a formal data sharing agreement is needed before any data can be shared.