Abstract
Background:
The Simple Ankle Value (SAV) is a patient-reported outcome measure (PROM) in which patients grade their ankle function as a percentage of that of their contralateral uninjured ankle.
Purpose/Hypothesis:
The primary aims of this study were to validate the SAV and evaluate its correlation with other PROMs. It was hypothesized that the SAV would be seen as a valid score that provides results comparable with those of the Foot and Ankle Ability Measure (FAAM) and the European Foot & Ankle Society (EFAS) score.
Study Design:
Cohort study (Diagnosis); Level of evidence, 2.
Methods:
Patients seen for an ankle or hindfoot tissue were divided into those treated operatively and nonoperatively. A control group of patients treated for issues outside of the foot and ankle was also created. All patients completed the SAV followed by the FAAM and the EFAS scores. Patients treated operatively completed the questionnaires before surgery and 3 months after surgery. Patients treated nonoperatively completed the questionnaires twice 15 days apart. The correlation between the SAV score, the FAAM score, and the EFAS score was estimated with the Spearman correlation coefficient.
Results:
A total of 209 patients (79 in the operative group, 103 in the nonoperative group, and 27 in the control group) were asked to complete the questionnaire, and all were included. The test-retest reliability of the SAV was excellent (intraclass correlation coefficient, 0.92; 95% CI, 0.88-0.94). No ceiling or floor effect was reported. Strong correlation was found between the SAV and the FAAM and EFAS scores. The SAV was able to discriminate patients from controls (54.18 ± 21.22 and 93.52 ± 9.589; P < .0001); however, SAV was not able to detect change from preoperative to 3 months postoperative (from 54.18 ± 21.22 to 62.53 ± 20.83; P = .44).
Conclusion:
Our study suggests that the SAV is correlated with existing accepted ankle PROMs. Further work with this PROM is needed to validate the questionnaire.
Keywords: PROMs, SANE, SAV, ankle evaluation, FAAM
Functional assessment provides objective follow-up of a patient’s condition, in particular of treatment efficacy, especially after surgery. In the era of evidence-based medicine, the use of functional scores has become a clinical necessity, 5 but their use remains difficult in daily practice. One study in the United States in 2016 4 found that orthopaedic surgeons spend a mean of 11.3 h/wk processing external quality measures, including following quality measure specifications, developing and implementing data collection processes, entering information into the medical record, and collecting and transmitting data, at an annual cost of US$15.6 billion. A study on surgical practices 31 showed that 17% of surgeons did not use patient-reported outcome measures (PROMs), 34% used them for the clinical follow-up of their patients, and 72% used them for research purposes. PROMs are standardized and validated questionnaires that are filled out by the patient to measure one’s perception of his or her own functional status. 6
The increase in the number of functional scores, by joint, pathology, and type of patient, has made their use more complex, in particular in the foot and ankle,20,23,31 and sometimes makes the choice difficult. 11 Their construction and validation is not always optimized for the specific pathology that is being evaluated. 12 For example, the complexity of certain questionnaires with several dozen questions that may be considered redundant and pointless by the patient may be counterproductive. 21 Thus, Hutchings et al 14 clearly showed the difficulty of obtaining a high level of participation, especially in elderly, vulnerable patients with severe impairments. Zwiers et al 31 reported that the main criteria for the use of PROMs were rapidity and ease of use for 71% of the experts, followed by their routine use in the literature (68%) and scientific validation (60%). These criteria were similar whether the PROMs were used for scientific research or for clinical follow-up.
To simplify data collection, Williams et al29,30 proposed a single method of numeric evaluation, the Single Assessment Numeric Evaluation (SANE), which asks patients how they evaluate their articular function on the day of the test, as a percentage of their uninjured contralateral joint. The SANE has been evaluated and validated in the shoulder 8 and more recently in the knee, 16 it is extensively used in both its joints. It has never been proposed in the ankle and it has never been compared with the more routine and validated scores 12 used for all ankle disorders, such as the Foot and Ankle Ability Measure (FAAM)1,3,9,17,27 or the European Foot & Ankle Society (EFAS) score. 19
The main objective of this study was to validate the Simple Ankle Value (SAV), which is a SANE-style evaluation that can be applied to all disorders of the ankle and hindfoot. For this, the degree of correlation of the SAV with the FAAM and the EFAS score was studied. The secondary objectives were to determine its reliability and sensitivity to change, as well as its discriminatory value. Our hypothesis was that the SAV would be a valid score that provides results comparable with those of the FAAM and EFAS functional scores.
Methods
This prospective multicenter cohort study received ethics committee approval, and all of the included patients provided informed consent. All the patients who attended a consultation or who underwent surgery for ankle or hindfoot disorders at the Atlantique health clinic in Saint Herblain and the Paris sports clinic between September 2021 and March 2022 were considered for the study. Patients were categorized into 3 groups. Included in the operative group were patients who underwent ankle or hindfoot surgery. Patients who attended a consultation for ankle impairment without undergoing surgery were included in the nonoperative group, without considering whether the impairment was of a surgical character. These nonoperative impairments were chronic pathologies with no prospect of improvement or worsening in the short term. In addition, no treatment was instituted during the study period. Patients who came for pathologies other than those of the foot and ankle and who had agreed to complete the study questionnaires were included in the control group. Patients were excluded from any of the groups if they were incapable of filling out the questionnaire, <18 years old, had psychiatric disorders, and/or refused to participate. No patient was excluded from the study.
Overall, 209 patients were included: 79 patients in the operative group, 103 patients in the nonoperative group, and 27 patients in the control group. The demographic characteristics of the different study groups are summarized in Table 1.
Table 1.
Patient Characteristics of Different Groups a
| Nonoperative Group (n = 103) | Operative Group (n = 79) | Control Group (n = 27) | |
|---|---|---|---|
| Men/women, n | 63/40 | 43/36 | 15/12 |
| Age, y, mean ± SD | 42.03 ± 15.85 | 41.91 ± 16.57 | 41.44 ± 15.73 |
| Diagnosis, % | • Hindfoot osteoarthritis: 20.3 • Chronic painful instability: 17.4 • Ankle instability: 15.5 • Ankle impingement: 12.6 • Tendinopathy (Achilles or peroneal): 9.7 • Chronic ankle pain with no organic cause: 9.7 • Osteochondral talar dome lesion: 8.7 • Syndesmosis injury: 2.9 |
• Ligament reconstruction ± associated procedure: 43 • Arthrodesis (subtalar ankle/twist): 25.3 • Osteochondral graft: 5.8 • Debridement ankle impingement: 5 • Tear or speed bridge Achilles tendon: 5 • Regularization peroneal tendon: 5 • Treatment pseudarthrosis (external malleolus or other): 3.8 • Ablation of osteosynthesis equipment in the ankle: 2.5 • Calcaneonavicular coalition: 1.2 • Calcaneal osteotomy: 1.2 |
— |
| Postoperative follow-up, % | 2.9 | — | — |
Dashes indicate areas not applicable.
Study Questionnaire
The SAV consisted of the following question: “How normal do you consider your ankle function to be today, as a percentage?” Responses were reported on a scale from 0% to 100%, with 100% being completely normal. The SAV was included within a questionnaire that also included the FAAM 17 and the EFAS score. 19 Both the 29-item FAAM and the 10-item EFAS consist of a daily life and a sports activities subsection, with a possible score from 0% to 100%.
These 3 scores were distributed blindly, and patients were unaware that they were filling out 3 different outcome measures. Simultaneous collection of these 3 scores allowed us to evaluate the validity of the SAV. All the patients included in the study filled out the questionnaire without assistance. The time required to complete the questionnaire was not assessed.
During the inclusion period, patients in the operative group completed the questionnaire preoperatively and 3 months after surgery to evaluate the sensitivity of the SAV to change. Patients in the nonoperative group filled out the questionnaire during the first consultation (test) then 15 days after the consultation (retest) to evaluate the reliability of the SAV. The SAV was filled out once by the control group to evaluate its discriminatory value.
Statistical Analysis
An a priori power analysis indicated that a sample size of 30 patients would produce a 2-sided 95% CI with a width smaller than 0.09 when the estimate of Spearman rank correlation was above 0.750.
Continuous variables were reported as means and standard deviations when they were normally distributed (verified with Shapiro test) and by their medians and range when they were not normally distributed. Binary variables were presented as the number of events and their percentage. The correlation between the SAV score, the FAAM score, 17 and the EFAS score 19 was estimated with the Spearman correlation coefficient, in which correlations were considered to be strong (rS > 0.5), moderate (0.5 < rS < 0.3), or weak (0.3 < rS < 0.1).
Discriminant validity was tested between the SAV scores in the operated and in the control patients by the Mann-Whitney test. The score’s sensitivity to change was tested by comparing the patients’ preoperative and postoperative SAV score.
Reliability was evaluated with the intraclass correlation coefficient (ICC; 2-way model based on individual data). Reliability was considered to be excellent (ICC > 0.75), good (0.75 < ICC < 0.40) or weak (ICC < 0.40). To identify any threshold or ceiling effect(s), we determined the number of patients who had a score <10% (threshold effect) and those with a score >90% (ceiling effect). A rate >15% corresponded to the presence of a ceiling or threshold effect. 25 A P value <.05 was considered significant for a power of 80%. The RStudio software (Version 1.0.153; RStudio Inc) was used for all statistical analyses.
Results
Scores on the SAV, FAAM, and EFAS are shown in Table 2. There was a strong correlation between the SAV and the other pre- and postoperative scores. The different correlations in the operative group are presented in Table 2.
Table 2.
Outcome Scores and Correlations Between the SAV and Other Scores in the Operative Group a
| SAV, % | FAAM, % | EFAS, % | |||
|---|---|---|---|---|---|
| Daily Activities | Sports | Daily Activities | Sports | ||
| Score, mean ± SD | |||||
| Preoperative | 54.18 ± 21.22 | 62.76 ± 20.35 | 38.39 ± 25.92 | 35.58 ± 22.5 | 25.66 ± 27.65 |
| Postoperative | 62.53 ± 20.83 | 69.49 ± 20.91 | 37.57 ± 31.76 | 50.53 ± 23.2 | 24.28 ± 29.68 |
| r S (95% CI) | |||||
| Preoperative | 0.60 (0.41-0.75) P < .001 |
0.56 (0.37-0.71) P < .001 |
0.48 (0.26-0.67) P < .001 |
0.50 (0.29-0.65) P < .001 |
|
| Postoperative | 0.66 (0.48-0.79) P < .001 |
0.62 (0.43-0.76) P < .001 |
0.56 (0.36-0.72) P < .001 |
0.61 (0.43-0.76) P < .001 |
|
EFAS, European Foot & Ankle Society; FAAM, Foot and Ankle Ability Measure; SAV, Simple Ankle Value.
The mean preoperative SAV was 54.18 ± 21.22 in the operative group and 93.52 ± 9.589 in the control group (P < .0001); thus, the SAV was able to detect a significant difference between patients and controls. The reliability of the SAV was excellent, with an ICC of 0.92 (95% CI, 0.88-0.94) between the initial consultation and the retest at 15 days (with no change in clinical status). The results are presented in Figure 1.
Figure 1.
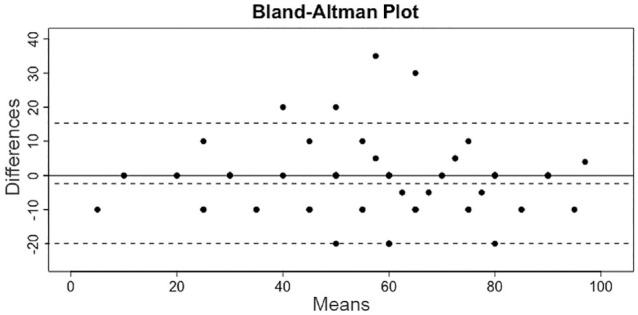
Intraclass correlation between test and retest. Top line, +1.96 SD; middle line, mean; bottom line, −1.96 SD.
Although there was a change in clinical status between the preoperative and the 3-month postoperative SAV score, the sensitivity to change was not significant (54.18 ± 21.22 [preoperatively] vs 62.53 ± 20.83 [3 months postoperatively]; P = .44) (Figure 2). Distribution of the SAV at different time intervals is presented in Figures 2 and 3. No threshold or ceiling effects were identified. No SAV scores <10% were identified, and only 2 of 79 patients had an SAV >90% (2.53%) in the operated group.
Figure 2.
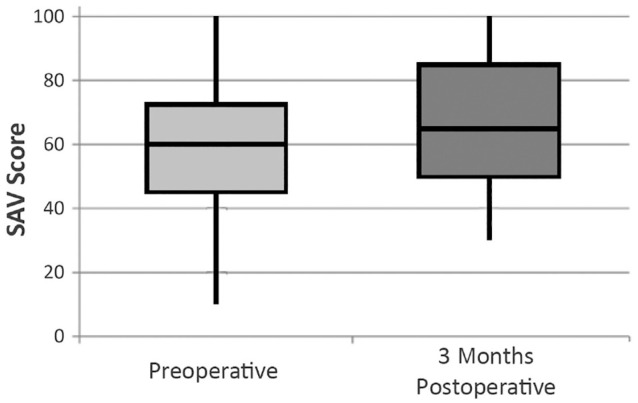
Distribution of the Simple Ankle Value (SAV) for preoperative and 3 months postoperative in the operated group. In operative group: Low mustache, minimum SAV score of the series; high mustache, maximum SAV score of the series; low box, 1st quartile value; high box, 3rd quartile value; horizontal line, median value.
Figure 3.
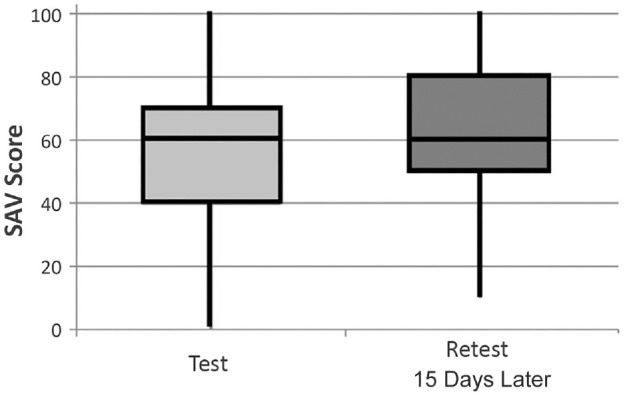
Distribution of the Simple Ankle Value (SAV) scores for the test and retest 15 days later in the nonoperative group. In nonoperative group: low mustache, minimum SAV score of the series; high mustache, maximum SAV score of the series; low box, 1st quartile value; high box, 3rd quartile value; horizontal line, median value.
Discussion
The most important result of our study was that there was a strong correlation between SAV, FAAM, and EFAS scores (rS between 0.48 [95% CI, 0.26-0.67], P < .001; and 0.66 [95% CI, 0.48-0.79], P < .001). These results validate the SAV score in the evaluation of ankle and hindfoot impairment. Our hypothesis was therefore validated. The reliability and the discriminatory value of the SAV were also validated. All SAV scores collected are distributed without any threshold or ceiling effect and report a discriminating score adapted to the study population.
Marot et al 16 validated a simplified score for the knee called the Simple Knee Value with results that were close to and strongly correlated with the Lysholm, International Knee Documentation Committee (IKDC), Knee injury and Osteoarthritis Outcome Score, and Western Ontario and McMaster Universities Osteoarthritis Index scores. Gilbart and Gerber 8 validated a SANE for the shoulder called the Subjective Shoulder Value and found results close to those of the Constant score with a correlation of between 0.4 and 0.69. Since its publication and mainly because it is simple and rapid to use, the Subjective Shoulder Value has become regularly used in routine practice by shoulder surgeons, rehabilitation specialists, and rheumatologists. 16 Different studies have reported the correlation between the SANE and certain knee scores for specific knee surgeries. Williams et al 29 reported a correlation of 0.87 between the SANE and the Lysholm score in patients who underwent anterior cruciate ligament reconstruction. Shelbourne et al 21 reported a correlation of 0.74 between the SANE and other scores such as the IKDC and the Cincinnati Knee Rating System in patients who underwent knee arthroscopy, and Sueyoshi et al 24 reported a correlation of 0.38 between the SANE and the Lysholm score in patients after total knee replacement.
Our results were similar to those in the literature for other joints, even if we could not compare our results with other studies in the ankle.
In orthopaedic surgery, most existing functional scores include the assessment of joint function for daily activities as well as during sports, pain perception, and patient quality of life. An ideal evaluation of the results should be reliable, reproducible, and sensitive to change and should precisely reflect the patient’s perception.
Numerous functional scores are available to foot and ankle specialists. A recent review of the literature identified 76 tools to assess the results in these joints. 20 A practical investigation by Zwiers et al 31 found that there was significant confusion about the understanding and use of these scores. Zwier’s study questioned 188 ankle experts from 53 countries about PROMs. To the question “Which PROMs are you familiar with?” the response of 78 of the surgeons (41.5%) was the American Orthopaedic Foot & Ankle Society (AOFAS). 15 Paradoxically, although it is the most frequently used score in the literature, 20 the AOFAS has numerous limitations—in particular, it is not a PROM because a physician is needed to measure range of motion.
The measurements for this complex score are a combination of ordinals and intervals, which can complicate statistical analyses; additionally, they lack precision. The AOFAS has not been validated in the ankle (in particular, in chronic ankle instability), and its sensitivity and reliability have not been confirmed, as mentioned by numerous authors.2,10,20,22,23,26,31
General scores such as the 36-Item Short Form Health Survey 28 provide a global, but not specific, estimation of the patient’s health. Thus, these scores were not included as references in this article.
As a result, we used the FAAM and EFAS scores to evaluate the SAV. In particular, the FAAM 17 seems to be the most appropriate existing score for use as a reference tool in the ankle (development and validation of contents, comparison with other tests). It includes 29 items with subgroups for daily activities (21 items) and athletic activities (8 items). The FAAM was validated in athletes with chronic ankle instability. 27 The EFAS score is one of the most recent tools in the literature. 19 It is not specific for particular pathologies. Thus, it is generic and can be applied in the analysis of numerous ankle disorders. It includes 10 items, with subgroup for daily activities (6 items) and athletic activities (4 items). It has the advantage of having been validated in 7 of the most widely spoken European languages. The EFAS score is easy to use, pertinent, valid, and sensitive in clinical practice.
The ideal functional score should include certain metrological qualities to provide a valid, reliable, reproducible score that is sensitive to change, with discriminative value in the specific organ. It must be able to be used for any type of pathology and should also precisely represent the patient’s perceived health at a moment time.2,7,10,11,13,18 The SAV seems to fulfill these criteria. Other advantages include its ease of understanding by the patient and rapid impression of the patient’s perception and expectations.
Limitations
The current study is not without limitation. The SAV does not reveal the most invalidating symptoms, which is possible with other, more in-depth scores. Moreover, the sensitivity of the SAV was not statistically confirmed. This was probably due to the short follow-up (3 months) of the postoperative SAV. The delay before the benefits of foot and ankle surgery are seen is both variable depending on the pathology and often long, especially due to a postoperative period without weightbearing.
Thus, the SAV is a complementary and simplified tool to evaluate function in patients with pathologies of the ankle or hindfoot.
Conclusion
Our study suggests the SAV is useful, having some value in our sample of patients, and correlates with existing accepted ankle PROMs. Further work with this PROM is needed to validate the questionnaire.
Footnotes
Final revision submitted April 10, 2023; accepted May 3, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: R.L. has received education payments, consulting fees, speaking fees, and royalties from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from GCS Ramsay Santé (No. COS-RGDS-2021-09-003-HARDY-A).
References
- 1. Borloz S, Crevoisier X, Deriaz O, Ballabeni P, Martin RL, Luthi F. Evidence for validity and reliability of a French version of the FAAM. BMC Musculoskelet Disord. 2011;12:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Button G, Pinney S. A meta-analysis of outcome rating scales in foot and ankle surgery: is there a valid, reliable, and responsive system? Foot Ankle Int. 2004;25:521-525. [DOI] [PubMed] [Google Scholar]
- 3. Carcia CR, Martin RL, Drouin JM. Validity of the Foot and Ankle Ability Measure in athletes with chronic ankle instability. J Athl Train. 2008;43:179-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Casalino LP, Gans D, Weber R, et al. US physician practices spend more than $15.4 billion annually to report quality measures. Health Aff (Millwood). 2016;35:401-406. [DOI] [PubMed] [Google Scholar]
- 5. Dawson J, Carr A. Outcomes evaluation in orthopaedics. J Bone Joint Surg Br. 2001;83:313-315. [DOI] [PubMed] [Google Scholar]
- 6. Dawson J, Doll H, Fitzpatrick R, Jenkinson C, Carr AJ. The routine use of patient reported outcome measures in healthcare settings. BMJ. 2010;340:C186. [DOI] [PubMed] [Google Scholar]
- 7. Eechaute C, Vaes P, Van Aerschot L, Asman S, Duquet W. The clinimetric qualities of patient-assessed instruments for measuring chronic ankle instability: a systematic review. BMC Musculoskelet Disord. 2007;8:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gilbart MK, Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg. 2007;16:717-721. [DOI] [PubMed] [Google Scholar]
- 9. Goulart Neto AM, Maffulli N, Migliorini F, de Menezes FS, Okubo R. Validation of Foot and Ankle Ability Measure (FAAM) and the Foot and Ankle Outcome Score (FAOS) in individuals with chronic ankle instability: a cross-sectional observational study. J Orthop Surg Res. 2022;17:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guyton GP. Theoretical limitations of the AOFAS scoring systems: an analysis using Monte Carlo modeling. Foot Ankle Int. 2001;22:779-787. [DOI] [PubMed] [Google Scholar]
- 11. Hansen CF, Jensen J, Siersma V, Brodersen J, Comins JD, Krogsgaard MR. A catalogue of PROMs in sports science: quality assessment of PROM development and validation. Scand J Med Sci Sports. 2021;31:991-998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hansen CF, Obionu KC, Comins JD, Krogsgaard MR. Patient reported outcome measures for ankle instability. An analysis of 17 existing questionnaires. Foot Ankle Surg. 2022;28:288-293. [DOI] [PubMed] [Google Scholar]
- 13. Hunt KJ, Hurwit D. Use of patient-reported outcome measures in foot and ankle research. J Bone Joint Surg Am. 2013;95:e118(111-119). [DOI] [PubMed] [Google Scholar]
- 14. Hutchings A, Grosse Frie K, Neuburger J, van der Meulen J, Black N. Late response to patient-reported outcome questionnaires after surgery was associated with worse outcome. J Clin Epidemiol. 2013;66:218-225. [DOI] [PubMed] [Google Scholar]
- 15. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-353. [DOI] [PubMed] [Google Scholar]
- 16. Marot V, Justo A, Alshanquiti A, et al. Simple Knee Value: a simple evaluation correlated to existing knee PROMs. Knee Surg Sports Traumatol Arthrosc. 2021;29:1952-1959. [DOI] [PubMed] [Google Scholar]
- 17. Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005;26:968-983. [DOI] [PubMed] [Google Scholar]
- 18. Pynsent PB. Choosing an outcome measure. J Bone Joint Surg Br. 2001;83:792-794. [DOI] [PubMed] [Google Scholar]
- 19. Richter M, Agren PH, Besse JL, et al. EFAS Score—multilingual development and validation of a patient-reported outcome measure (PROM) by the score committee of the European Foot and Ankle Society (EFAS). Foot Ankle Surg. 2018;24:185-204. [DOI] [PubMed] [Google Scholar]
- 20. Shazadeh Safavi P, Janney C, Jupiter D, Kunzler D, Bui R, Panchbhavi VK. A systematic review of the outcome evaluation tools for the foot and ankle. Foot Ankle Spec. 2019;12:461-470. [DOI] [PubMed] [Google Scholar]
- 21. Shelbourne KD, Barnes AF, Gray T. Correlation of a single assessment numeric evaluation (SANE) rating with modified Cincinnati Knee Rating System and IKDC subjective total scores for patients after ACL reconstruction or knee arthroscopy. Am J Sports Med. 2012;40:2487-2491. [DOI] [PubMed] [Google Scholar]
- 22. SooHoo NF, Shuler M, Fleming LL. Evaluation of the validity of the AOFAS Clinical Rating Systems by correlation to the SF-36. Foot Ankle Int. 2003;24:50-55. [DOI] [PubMed] [Google Scholar]
- 23. Spennacchio P, Meyer C, Karlsson J, Seil R, Mouton C, Senorski EH. Evaluation modalities for the anatomical repair of chronic ankle instability. Knee Surg Sports Traumatol Arthrosc. 2020;28:163-176. [DOI] [PubMed] [Google Scholar]
- 24. Sueyoshi T, Emoto G, Yato T. Correlation between Single Assessment Numerical Evaluation score and Lysholm score in primary total knee arthroplasty patients. Arthroplast Today. 2018;4:99-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34-42. [DOI] [PubMed] [Google Scholar]
- 26. Toolan BC, Wright Quinones VJ, Cunningham BJ, Brage ME. An evaluation of the use of retrospectively acquired preoperative AOFAS clinical rating scores to assess surgical outcome after elective foot and ankle surgery. Foot Ankle Int. 2001;22:775-778. [DOI] [PubMed] [Google Scholar]
- 27. Uimonen MM, Ponkilainen VT, Toom A, et al. Validity of five foot and ankle specific electronic patient-reported outcome (ePRO) instruments in patients undergoing elective orthopedic foot or ankle surgery. Foot Ankle Surg. 2021;27:52-59. [DOI] [PubMed] [Google Scholar]
- 28. Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473-483. [PubMed] [Google Scholar]
- 29. Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Am J Sports Med. 1999;27:214-221. [DOI] [PubMed] [Google Scholar]
- 30. Williams GN, Taylor DC, Gangel TJ, Uhorchak JM, Arciero RA. Comparison of the Single Assessment Numeric Evaluation method and the Lysholm score. Clin Orthop Relat Res. 2000;373:184-192. [DOI] [PubMed] [Google Scholar]
- 31. Zwiers R, Weel H, Mallee WH, Kerkhoffs G, van Dijk CN. Large variation in use of patient-reported outcome measures: a survey of 188 foot and ankle surgeons. Foot Ankle Surg. 2018;24:246-251. [DOI] [PubMed] [Google Scholar]


