Abstract
The L2 reference strain of Chlamydia trachomatis was exposed to subinhibitory concentrations of ofloxacin (0.5 μg/ml) and sparfloxacin (0.015 μg/ml) to select fluoroquinolone-resistant mutants. In this study, two resistant strains were isolated after four rounds of selection. The C. trachomatis mutants presented with high-level resistance to various fluoroquinolones, particularly to sparfloxacin, for which a 1,000-fold increase in the MICs for the mutant strains compared to the MIC for the susceptible strain was found. The MICs of unrelated antibiotics (doxycycline and erythromycin) for the mutant strains were identical to those for the reference strain. The gyrase (gyrA, gyrB) and topoisomerase IV (parC, parE) genes of the susceptible and resistant strains of C. trachomatis were partially sequenced. A point mutation was found in the gyrA quinolone-resistance-determining region (QRDR) of both resistant strains, leading to a Ser83→Ile substitution (Escherichia coli numbering) in the corresponding protein. The gyrB, parC, and parE QRDRs of the resistant strains were identical to those of the reference strain. These results suggest that in C. trachomatis, DNA gyrase is the primary target of ofloxacin and sparfloxacin.
Chlamydia trachomatis, an obligate intracellular bacterium, causes a wide spectrum of human diseases and is one of the most common sexually transmitted pathogens in the world (49). The antibiotic of choice for the treatment of chlamydial infection is doxycycline, but erythromycin and azithromycin are used as alternative therapies (41). Some fluoroquinolones also have good antichlamydial activity, and ofloxacin has been administered for the treatment of C. trachomatis urethritis and cervicitis and is proposed for use in the treatment of pelvic inflammatory diseases (41). Recent studies of the in vitro and in vivo activities of sparfloxacin against C. trachomatis have reported that it may provide a promising therapy for genital chlamydial infections (36, 38). The relative resistance of C. trachomatis isolates to tetracyclines and erythromycin has been reported previously (21, 30). Although fluoroquinolone resistance in C. trachomatis has never been described, the emergence of resistant isolates posttherapy could occur and could have dramatic clinical implications.
The principal targets of the quinolones are DNA gyrase and topoisomerase IV (Topo IV). DNA gyrase is composed of two pairs of subunits A and B encoded by the gyrA and gyrB genes, respectively. Gyrase catalyzes ATP-dependent negative supercoiling of DNA and is involved in DNA replication, recombination, and transcription (40, 51). Topo IV, recently described in Escherichia coli (22), is a tetramer consisting of two pairs of ParC (GrlA) and ParE (GrlB) subunits, which are homologous to the GyrA and GyrB subunits of DNA gyrase, respectively, and is involved in the partitioning of the replicated chromosome (1, 22). Fluoroquinolone resistance has been related to single point mutations which occur in the quinolone-resistance-determining region (QRDR) of DNA gyrase and Topo IV subunit genes. The GyrA QRDR is located between amino acid residues equivalent to Ala-67 through Gln-106 in E. coli (54), and the most frequent mutations associated with quinolone resistance are located at Ser-83 and relatively fewer mutations associated with quinolone resistance are located at Asp-87 (5, 15, 34, 54). Recent studies have identified in the analogous QRDR of ParC similar point mutations that result in fluoroquinolone resistance (2, 24, 32). Furthermore, substitutions of the amino acids corresponding to residues 426, 447, and 463 in GyrB (E. coli numbering) (11, 20, 55) and residues 420, 445, and 458 in ParE (3, 9, 37) have also been determined to confer quinolone resistance.
Other mechanisms of resistance associated with a reduction of the level of intracellular accumulation of fluoroquinolones and involving active efflux systems or decreased permeability of the outer membrane in gram-negative bacteria have also been identified (39).
In this study, the sequences of the putative gyrA and parC QRDRs and of most of the gyrB and parE genes of the C. trachomatis L2/434/Bu (L2) reference strain are reported. In addition, two quinolone-resistant mutants of C. trachomatis were selected with ofloxacin and sparfloxacin by using a stepwise procedure and were characterized for gyrase (gyrA, gyrB) and Topo IV (parC, parE) QRDRs. A point mutation located in the gyrA QRDRs of these strains was associated with fluoroquinolone resistance.
MATERIALS AND METHODS
Bacterial strains and cells.
The reference strain C. trachomatis L2 was used for the selection of quinolone-resistant mutants. Competent E. coli JM 109, which was used in the cloning experiments, was obtained from Promega (Charbonnières, France).
McCoy cells, which were used for chlamydial culture, were grown in minimal essential medium supplemented with 5% fetal bovine serum and 2 mM l-glutamine and were incubated at 37°C in 5% CO2.
Antibiotics.
The antimicrobial agents tested were sparfloxacin and pefloxacin (purchased from Rhône-Poulenc-Rorer, Vitry-sur-Seine, France), ciprofloxacin (Bayer-Pharma, Puteaux, France), ofloxacin and erythromycin (Roussel-Uclaf, Paris, France), norfloxacin (Marion-Merrell-Dow, Levallois-Perret, France), and doxycycline (Pfizer, Orsay, France).
MIC determinations.
The antibiotic susceptibilities of the L2 reference strain of C. trachomatis and in vitro-selected quinolone-resistant mutants were determined by the standard method. Briefly, McCoy cells that had been seeded into 24-well plastic plates with glass coverslips and incubated for 24 h at 37°C in 5% CO2 were inoculated with 103 inclusion-forming units of the L2 strain per ml. The plates were centrifuged at 1,200 × g at 37°C for 1 h and were incubated for 2 h at 37°C in 5% CO2. Then, the cell monolayers were washed with 0.5 ml of culture medium and were incubated with twofold dilution series of antibiotics in complete medium containing culture medium supplemented with 0.5% (wt/vol) glucose and 1 μg of cycloheximide per ml. The drug concentrations tested ranged from 0.25 to 256 μg/ml for ciprofloxacin, pefloxacin, and ofloxacin, from 3 to 384 μg/ml for norfloxacin, from 0.008 to 64 μg/ml for sparfloxacin, from 0.05 to 1.6 μg/ml for erythromycin, and from 0.0125 to 0.4 μg/ml for doxycycline. Moreover, the titer of C. trachomatis was verified in each MIC determination experiment with McCoy cells inoculated with 10-fold dilutions of the chlamydial strain and incubated in antibiotic-free complete medium. The plates were incubated for 48 h at 37°C in 5% CO2. Then, the MICs and strain titers were determined by fluorescence microscopy. Cell monolayers were fixed in methanol, stained for chlamydial inclusions with an anti-Chlamydia major outer membrane protein fluorescein-conjugated monoclonal antibody (Syva Microtrak; Behring-Syva, Rueil-Malmaison, France), and observed at ×400 magnification. The MIC was defined as the lowest antibiotic concentration at which no inclusion was observed.
Selection of ofloxacin- and sparfloxacin-resistant mutants.
The quinolone-resistant mutants of the L2 strain of C. trachomatis were selected by successive passages in the presence of subinhibitory concentrations of ofloxacin and sparfloxacin. The protocol used for the stepwise selection of resistant mutants of C. trachomatis was derived from those previously described by Tipples and McClarty (50) and Wang et al. (52). First, confluent McCoy cell monolayers in 75-cm2 flasks were inoculated with approximately 108 inclusion-forming units of C. trachomatis L2, and complete medium supplemented with 0.5 and 0.015 μg of ofloxacin and sparfloxacin per ml, respectively, was immediately added. The infected cells were incubated at 37°C in 5% CO2 for 48 h. Then, the supernatant was removed and a freeze-thaw cycle at −80°C was performed to disrupt the cells and liberate the intracellular bacteria. After thawing, sterile glass beads and 5 ml of complete medium plus 0.5 and 0.015 μg of ofloxacin and sparfloxacin per ml, respectively, were added. The cellular suspension (i.e., elementary bodies [EBs] and cell debris) was centrifuged at 400 × g for 5 min. Then, 4 ml of the supernatant, which contained EBs, was used to inoculate fresh confluent McCoy cell monolayers in the presence of subinhibitory concentrations of ofloxacin and sparfloxacin (0.5 and 0.015 μg/ml, respectively). The flasks were incubated for 48 h at 37°C in 5% CO2, and the presence of inclusions was observed by inverted light microscopy. The passages were repeated with the same fluoroquinolone concentrations until a highly infectious inoculum was obtained, and the MICs for these selected strains were determined. An aliquot (1 ml) from each passage was stored at −80°C. To attempt to increase the level of resistance of the mutants selected with subinhibitory concentrations of ofloxacin and sparfloxacin, several passages were performed with these fluoroquinolones at 16, 32, and 64 μg/ml.
DNA isolation.
Genomic DNA was extracted from three chlamydial strains, the L2 reference strain and the in vitro-selected ofloxacin- and sparfloxacin-resistant strains L2-OFXR and L2-SPXR, respectively. Each strain was grown on confluent McCoy cell monolayers in three flasks (75 cm2) with antibiotic-free complete medium for the reference strain or in the presence of 8 μg of ofloxacin per ml or 4 μg of sparfloxacin per ml for the resistant strains L2-OFXR and L2-SPXR, respectively, to maintain selection pressure. EBs were purified by using a previously described protocol (42, 46) that included a DNase I treatment to digest the eukaryotic DNA. Then, the EBs, which were resuspended in phosphate-buffered saline (pH 7.2), were mixed with a lysis buffer (10 mM Tris HCl [pH 8.3], 50 mM KCl, 4.5 mM MgCl2, 0.45% Nonidet P-40, 0.45% Tween 20) and were treated with 200 μg of proteinase K per ml. They were heated at 56°C for 90 min and at 95°C for 15 min. Then, the DNA was purified by phenol-chloroform-isoamyl alcohol extractions and ethanol precipitation as described previously (44, 46). Control DNA, isolated from uninfected McCoy cells, was extracted by the same protocol. Moreover, a simplified procedure consisting of direct lysis after culture (i.e., without EB purification and DNA extraction and precipitation) was also used for some PCR experiments. Lysates were prepared from the three chlamydial strains and from uninfected control McCoy cells.
Amplification of the QRDRs of the gyrA and gyrB genes.
PCR amplification of the gyrA QRDR of C. trachomatis L2 was carried out with the degenerate primers CTA1 and CTA2 (Table 1), whose nucleotide sequences were deduced from highly conserved motifs of the Chlamydia psittaci (19), Helicobacter pylori (28), and Campylobacter jejuni (53) GyrA proteins. From the sequence of the CTA1-CTA2 fragment, two specific primers, primers CTA3 plus CTA4 (Table 1; see Fig. 1), were chosen to amplify a 362-bp DNA fragment from the resistant mutant strains of C. trachomatis.
TABLE 1.
Nucleotide sequences of the primers used for PCR
| Gene | Primer | Nucleotide sequence (5′→3′) |
|---|---|---|
| gyrA | CTA1 | GA(T,C)GG(T,C)TT(G,A)AA(G,A)CC(T,C)GT(G,T)CAT |
| CTA2 | (G,C)GCCAT(G,C)CC(T,C)AC(G,A)GCGAT(A,C)CC | |
| CTA3 | TTAAAACCTTCTCAGCGACG | |
| CTA4 | GAAGGAAAAACTACAGGTTC | |
| CTA5 | TCCTTCATTTCCTCTTCAAG | |
| gyrB | CTB1 | CC(T,C)GG(T,C)AA(G,A)TT(G,A)GC(G,C)GA(T,C)TG(T,C) |
| CTB2 | (G,A)TC(A,C)AC(G,A)TC(G,C)GC(G,A)TC(G,A)GTCAT | |
| CTB3 | AGGAATCCCTATTCAGATTC | |
| CTB4 | AACACCTTGTCTACAATCGTT | |
| CTB5 | TAAGTTAATTGACTGCTTGG | |
| CTB6 | ACGTTTATAACGCAATTTGC | |
| CTB7 | TGGATGGCTATTTGCTGAAC | |
| parC | CTC1 | GA(T,C)GG(T,C)CT(G,A)AA(G,A)CC(T,C)GT(G,T)CA(G,A) |
| CTC2 | (A,C)GT(T,C)AG(T,C)GG(G,A)TT(G,T)CC(G,A)AA(G,A)TT | |
| CTC3 | GATGGCCTCAAGCCTGTTCA | |
| CTC4 | CAGTGGATTGCCAAAGTTCCC | |
| CTC5 | CATTTTACCATCATCCATAC | |
| parE | CTE1 | AA(T,C)GC(A,G)AT(A,T)GA(T,C)GA(A,G)TT(T,C)GT |
| CTE2 | AAGGCATTCTCTTACACACA | |
| CTE3 | ACAACTGATGGCGGAACCCAT | |
| CTE4 | GCTGTGCTCTCTTCTTTGAA | |
| CTE5 | TCAACATCCGCATCTGTTGC | |
| CTE6 | CACAGACAATTCTCTGTATG |
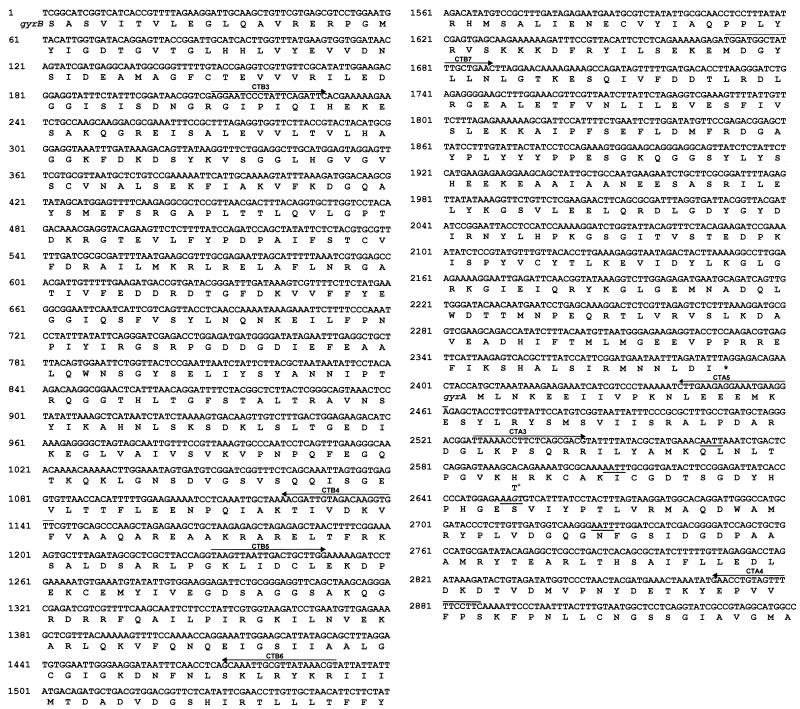
FIG. 1.
Nucleotide and amino acid sequences of a 2,942-bp fragment which contains most of the gyrB gene and the 5′ end of the gyrA gene of the C. trachomatis L2 reference strain. Specific primers are indicated by arrows. +, nucleotide mutation (G→T) in the gyrA gene leading to the Ser→Ile substitution in the GyrA protein. Tsp509I restriction sites (AATT) are underlined; the site indicated in italics corresponds to the site created by the mutation (G→T).
The nucleotide sequences of the degenerate primers CTB1 and CTB2 (Table 1) were deduced from the sequence of the two conserved motifs PGKLADC (residues 404 to 410 by the E. coli GyrB numbering) and MTDADVD (residues 496 to 502) flanking the GyrB QRDRs of various bacteria (26). An unexpected 1,521-bp PCR product was amplified and was completely sequenced with two internal primers, primers CTB3 and CTB4 (Table 1; see Fig. 1). From the sequence of this large fragment, two specific primers, primers CTB5 and CTB6 (Table 1; see Fig. 1), were chosen to amplify a 262-bp gyrB fragment including the QRDRs from the resistant strains of C. trachomatis.
The gyrB and gyrA genes were recently described to be contiguous in Chlamydia (19), and so a PCR amplification was performed with the specific primers CTB5 (gyrB) and CTA4 (gyrA). The amplified fragment was directly sequenced with the internal primers CTB7 and CTA5 (Table 1; see Fig. 1), whose sequences were chosen from the sequences of the gyrB and gyrA genes, respectively.
All PCRs were performed in a final volume of 50 μl containing each primer at a concentration of 1 μM, 200 μM deoxynucleoside triphosphates, 1.5 mM MgCl2, 1× Taq buffer, 2 U of Taq polymerase (Perkin-Elmer Applied Biosystems, Roissy, France), and 100 ng of purified strain L2 DNA. After a denaturation step of 10 min at 95°C, amplification with the degenerate primers was performed over 40 cycles of 1 min at 95°C, 1 min at 55°C, and 2 min at 72°C. With the pairs of specific primers CTA3 plus CTA4, CTB5 plus CTB6, and CTB5 plus CTA4, PCR conditions differed from those described above only by the annealing temperature (60°C). Two negative controls containing DNA extracted from uninfected McCoy cells or water were included in each PCR experiment.
Amplification of the QRDRs of the parC and parE genes.
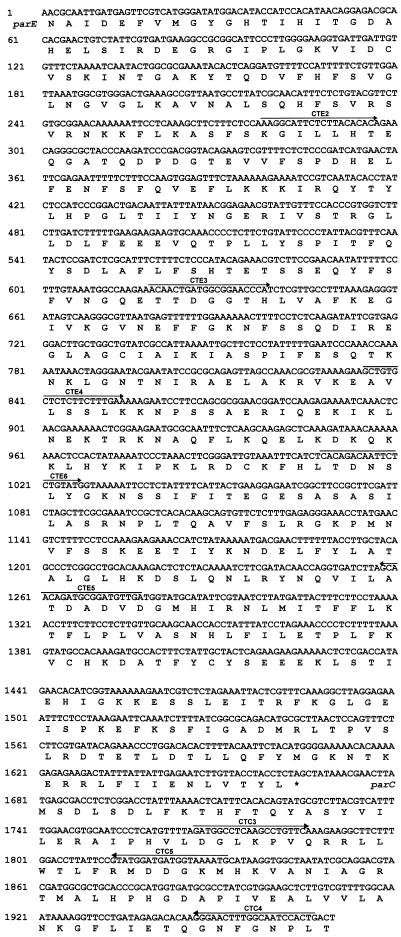
PCR amplification of the parC QRDR of the C. trachomatis L2 reference strain was carried out with the degenerate primers CTC1 and CTC2 (Table 1), whose sequences were deduced from the amino acid sequence of the C. psittaci ParC protein (19). From the nucleotide sequence of the CTC1-CTC2 product, two specific primers, primers CTC3 and CTC4 (Table 1; see Fig. 2), were selected to amplify a 201-bp fragment, including the QRDRs from the resistant strains of C. trachomatis, under the conditions described above for CTA3-CTA4 amplification.
FIG. 2.
Nucleotide and amino acid sequences of a 1,970-bp fragment which contains most of the parE gene and the 5′ end of the parC gene of the C. trachomatis L2 reference strain. Specific primers are indicated by arrows.
The degenerate primer CTE1 (Table 1), whose sequence was deduced from one of the two GyrB-like partial sequences of C. trachomatis published by Huang (18), was chosen to amplify the parE gene of this organism. The parE and parC genes were recently found to be contiguous in Chlamydia (19), and so primer CTE1 was associated with the specific primer CTC4 (parC) for PCR amplification. The amplified product was directly sequenced with four internal primers, primers CTE2, CTE3, CTE6 (in the parE gene), and CTC5 (in the parC gene) (Table 1; see Fig. 2). Then, from the nucleotide sequence of the parE gene of C. trachomatis, two specific primers, primers CTE4 and CTE5 (Table 1; see Fig. 2), were selected to amplify the QRDRs from the fluoroquinolone-resistant strains as described above.
DNA sequencing and sequence analysis.
The amplification products of C. trachomatis L2 and quinolone-resistant strains were purified with the Wizard PCR Preps DNA Purification System (Promega). The PCR products of C. trachomatis L2 were cloned in E. coli by using the pGEM-T Easy Vector System II (Promega) and were then sequenced, whereas those of the quinolone-resistant strains were directly sequenced. Sequencing was carried out with an AmpliTaq DNA polymerase FS Dye Terminator Cycle Sequencing Ready Reaction kit and an ABI-Prism 377 sequencer (Applied Biosystems Division, Perkin-Elmer) according to the manufacturer’s instructions.
Nucleotide sequence accession numbers.
The nucleotide sequence data reported here will appear in the GenBank nucleotide sequence databases with the following accession numbers: AF044267 for the gyrB and gyrA sequences and AF044268 for the parE and parC sequences.
RESULTS
In vitro selection of ofloxacin- and sparfloxacin-resistant mutants of C. trachomatis.
Two fluoroquinolone-resistant mutants of C. trachomatis were isolated by repeated exposures of the L2 reference strain to subinhibitory concentrations of ofloxacin and sparfloxacin. Spontaneous mutants L2-OFXR and L2-SPXR were obtained after four passages of the reference strain in the presence of 0.5 μg of ofloxacin per ml and 0.015 μg of sparfloxacin per ml, respectively. After the first passage with subinhibitory concentrations of ofloxacin and sparfloxacin, a few small inclusions could be seen. The inclusion size and number increased during the subsequent steps with the same antibiotic concentration until about 80 to 100% of the McCoy cells were infected after four passages. These fluoroquinolone-resistant mutants were expanded, and their gyrA, gyrB, parC, and parE QRDR sequences were analyzed. Passages in the presence of higher concentrations (16, 32, and 64 μg/ml) of ofloxacin and sparfloxacin were unsuccessful in generating higher levels of resistance.
The patterns of susceptibility to fluoroquinolones and unrelated antibiotics of the L2 reference strain and its two derivative mutants, L2-OFXR and L2-SPXR, are shown in Table 2. The MICs of the five fluoroquinolones tested increased for both mutants compared with those for the reference strain, particularly the MICs of sparfloxacin, for which a 1,000-fold increase in the MIC was obtained (MIC, 32 μg/ml). Both mutants showed high-level resistance to ofloxacin, pefloxacin, and ciprofloxacin, and the increase in the MICs for the mutants varied from 16- to 64-fold compared with the MIC for the susceptible reference strain. Eight- and fourfold increases in the MICs of norfloxacin were found for strains L2-OFXR and L2-SPXR, respectively. The MICs of ofloxacin, ciprofloxacin, and norfloxacin were slightly lower for strain L2-SPXR, selected on sparfloxacin, than for the ofloxacin-selected L2-OFXR mutant, with at most a difference of 1 dilution. This difference is probably due to the imprecision of the MIC reading method, and it is not significant. Interestingly, the MICs of unrelated antibiotics, such as doxycycline and erythromycin, were identical for the reference strain and its derivative mutants (Table 2).
TABLE 2.
Antibiotic susceptibilities of the reference strain and fluoroquinolone-resistant mutants of C. trachomatis L2
| Strain | Selecting agents | MIC (μg/ml)a
|
||||||
|---|---|---|---|---|---|---|---|---|
| OFX | SPX | PFX | CFX | NFX | ERY | DOX | ||
| Reference | None | 1 | 0.03 | 2 | 1 | 12 | 0.4 | 0.05 |
| L2-OFXR | Ofloxacin | 64 | 32 | 32 | 32 | 96 | 0.4 | 0.05 |
| L2-SPXR | Sparfloxacin | 32 | 32 | 32 | 16 | 48 | 0.4 | 0.05 |
OFX, ofloxacin; SPX, sparfloxacin; PFX, pefloxacin; CFX, ciprofloxacin; NFX, norfloxacin; ERY, erythromycin; DOX, doxycycline.
Amplification and sequence analysis of the gyrA QRDR and most of the gyrB gene of C. trachomatis.
The degenerate primer pairs CTA1-CTA2 and CTB1-CTB2 were chosen to amplify the gyrA and gyrB QRDRs of C. trachomatis L2, respectively. As expected, a 441-bp DNA fragment was obtained with primer pair CTA1-CTA2, whereas an unexpected large product of 1,521 bp was amplified with primers CTB1 and CTB2. Analysis of the sequences of these two fragments revealed the presence of highly conserved motifs in the bacterial GyrA- and GyrB-like proteins, respectively. With the specific primers CTA4 (gyrA) and CTB5 (gyrB), a 1,657-bp DNA fragment was amplified, confirming that the gyrB and gyrA genes of C. trachomatis are contiguous, with the gyrB gene being located upstream of the gyrA gene (19). The nucleotide and amino acid sequences of most of the gyrB gene and the 5′ end of the gyrA gene of C. trachomatis are presented in Fig. 1. The sequences of the chlamydial GyrA and GyrB proteins were compared to the sequences of other bacterial GyrA-like (Table 3) and GyrB-like (Table 4) proteins, respectively. The amino acid sequence of the GyrA fragment of C. trachomatis was closely related to that of C. psittaci (19), with 91% identity. When compared to other GyrA QRDRs, the C. trachomatis GyrA QRDR sequence was more related to those of E. coli (47) and Staphylococcus aureus (17). The GyrA QRDR of C. trachomatis showed a higher percentage of identity with the GyrA sequences than with the ParC sequences of other bacteria, particularly for Borrelia burgdorferi (19) (Table 3). The sequence of the N-terminal region of the chlamydial GyrB protein was identical to one of the two GyrB-like partial sequences of C. trachomatis (sequence CT1) published by Huang (18) (data not shown). The GyrB protein of C. trachomatis shared 42, 46, 48, and 48.5% identities with those of B. burgdorferi (45), S. aureus (17), Bacillus subtilis (29), and E. coli (4), respectively (Table 4), and appeared to be more closely related to the GyrB proteins than to the ParE proteins of these bacteria (Table 4).
TABLE 3.
Identities between the amino acid sequences of the GyrA and ParC QRDRs from various speciesa
| C. trachomatis sequence compared | % Sequence identity
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Ec GyrA | Sa GyrA | Bs GyrA | Bb GyrA | Ec ParC | Sa GrlA | BsGrlA | BbParC | Ct ParC | |
| GyrA | 63 | 63 | 60.5 | 57 | 54 | 58 | 59.5 | 41.5 | 38 |
| ParC | 33 | 42 | 35.5 | 39.5 | 37 | 37 | 37 | 68.5 | 100 |
Portions of GyrA from E. coli (Ec) (47), S. aureus (Sa) (17), B. subtilis (Bs) (29), B. burgdorferi (Bb) (19), and C. trachomatis and of ParC from E. coli (Ec) (22), S. aureus (Sa) (6), B. subtilis (Bs) (43), B. burgdorferi (Bb) (19), and C. trachomatis (Ct) were compared. All sequences compared corresponded to amino acids 39 to 179 and 36 to 111 of E. coli GyrA and ParC, respectively.
TABLE 4.
Identities between the amino acid sequences of most of the GyrB and ParE proteins from various speciesa
| C. trachomatis sequence compared | % Sequence identity
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Ec GyrB | Sa GyrB | Bs GyrB | Bb GyrB | Ec ParE | Sa GrlB | Bs GrlB | Bb ParE | Ct ParE | |
| GyrB | 48.5 | 46 | 48 | 42 | 33 | 38.5 | 39.5 | 23.5 | 22 |
| ParE | 21 | 27 | 27 | 27 | 28 | 25 | 26.5 | 50 | 100 |
Portions of GyrB from E. coli (Ec) (4), S. aureus (Sa) (17), B. subtilis (Bs) (29), B. burgdorferi (Bb) (45), and C. trachomatis and of ParE from E. coli (Ec) (22), S. aureus (Sa) (6), B. subtilis (Bs) (43), B. burgdorferi (Bb) (10), and C. trachomatis (Ct) were compared. All the sequences compared corresponded to amino acids 6 to 804 and 42 to 555 of E. coli GyrB and ParE, respectively.
Furthermore, no terminator-like structure was found between the gyrB and gyrA genes (Fig. 1).
From these data, we concluded that the fragments amplified with the primers pairs CTA1-CTA2 and CTB1-CTB2 belonged to the gyrA and gyrB genes of C. trachomatis, respectively.
Amplification and sequence analysis of the parC QRDR and most of the parE gene of C. trachomatis.
With the degenerate primers CTC1 and CTC2, whose sequences were deduced from the regions flanking the QRDR of the C. psittaci ParC protein (19), an expected 204-bp DNA fragment was amplified from C. trachomatis. When the specific primer CTC4 (parC) was associated with the degenerate primer CTE1, whose sequence was deduced from the partial GyrB-like sequence CT2 of C. trachomatis described by Huang (18), a 1,967-bp DNA fragment was amplified. This result suggested that the parE and parC genes are contiguous in C. trachomatis, as described recently (19), with the parE gene being located upstream of the parC gene on the chlamydial chromosome. The nucleotide and deduced amino acid sequences of most of the parE gene and the 5′ end of the parC gene of C. trachomatis are presented in Fig. 2. Partial sequences of the ParC and ParE proteins of C. trachomatis were compared to those other bacterial GyrA-like (Table 3) and GyrB-like (Table 4) protein sequences. The amino acid sequence of the CTC1-CTC2 fragment amplified from C. trachomatis shared 93.5% identity with the ParC QRDR of C. psittaci (19). When compared to the ParC sequences of unrelated bacterial species, the ParC QRDR of C. trachomatis was more closely related to that of B. burgdorferi (19), with 68.5% identity. The ParC QRDR of C. trachomatis showed higher percentages of identity with the ParC sequences than with the GyrA sequences of other bacteria such as B. burgdorferi (19), E. coli (22, 47), and B. subtilis (29, 43) but, surprisingly, not with that of S. aureus (Table 3). Furthermore, the GyrA and ParC QRDR sequences of C. trachomatis shared 38% identity.
When compared to other ParE sequences, the chlamydial ParE protein appeared to be quite distant from the other known bacterial ParE sequences except that of B. burgdorferi (10) (50% identity) (Table 4). The ParE protein of C. trachomatis showed a significantly higher percentage of identity with the ParE sequences than with the GyrB sequences of B. burgdorferi (10, 45) and E. coli (4, 22). The GyrB and ParE sequences of C. trachomatis shared only 22% identity and presented a difference in size of about 150 amino acids in the C-terminal region, with ParE being smaller than GyrB.
Furthermore, no terminator-like structure was detected between the parE and parC genes.
Characterization of ofloxacin- and sparfloxacin-resistant strains of C. trachomatis.
The gyrA, gyrB, parC, and parE QRDRs of the L2-OFXR and L2-SPXR strains were amplified by PCR and were directly sequenced. The sequences of the specific primers CTA3 and CTA4 were chosen from the nucleotide sequence of the 441-bp DNA fragment of C. trachomatis containing the gyrA QRDR. These primers amplified an expected 362-bp fragment of the C. trachomatis gyrA gene. A single base change (G→T) was detected in the sequence of the gyrA QRDR of resistant strains L2-OFXR and L2-SPXR compared to the sequence of the L2 strain. This mutation resulted in a Ser (AGT)-to-Ile (ATT) substitution at the position corresponding to amino acid 83 in the E. coli GyrA protein (Fig. 1). Interestingly, the G→T mutation led to the creation of a Tsp509I restriction site (AATT). After digestion with Tsp509I, the 362-bp PCR product of C. trachomatis L2 yielded four fragments of 161, 118, 43, and 40 bp, suggesting the presence of three Tsp509I sites. In contrast, the digested CTA3-CTA4 PCR product of resistant strains L2-OFXR and L2-SPXR produced five fragments of 161, 76, 43, 42, and 40 bp, indicating the presence of one additional Tsp509I site (data not shown).
The specific primer pairs CTB5-CTB6, CTC3-CTC4, and CTE4-CTE5, corresponding to the gyrB, parC, and parE QRDR of C. trachomatis, respectively, amplified 262-, 201-, and 443-bp fragments, respectively. No mutation was detected in the QRDRs of the resistant strains L2-OFXR and L2-SPXR.
Furthermore, similar results were obtained when purified DNA and lysates were used as DNA templates for PCR amplifications. Thus, lysates, the preparation of which is easier than that of extracted DNA, could be used as the DNA template for PCR amplification for the characterization of a large number of C. trachomatis strains.
To summarize, the Ser83→Ile substitution was found in the GyrA QRDRs of both mutants of C. trachomatis selected on ofloxacin and sparfloxacin, whereas no base change was found in the ParC, GyrB, and ParE QRDRs of these mutants compared to those of the L2 reference strain.
DISCUSSION
The sequences of the gyrA and parC QRDRs and of most of the gyrB and parE genes of C. trachomatis L2 are reported here. By using primers corresponding to highly conserved regions in each of the topoisomerase II subunits, these sequences were amplified and characterized. Sequence analysis of the CTA1-CTA2 PCR product amplified from C. trachomatis showed that it shares higher percentages of identity with the GyrA QRDRs than with the ParC sequences of other bacteria, and it was assigned as a GyrA fragment of this organism.
The sequence of most of the GyrB protein of C. trachomatis was compared to those of other bacterial GyrB-like proteins, and it shared higher homology scores with the GyrB proteins than with the ParE proteins of other bacteria. Comparison of the protein sequence of the C. trachomatis GyrB with those of some gram-negative and gram-positive bacteria revealed that the chlamydial protein falls in the same class as the proteobacterial GyrB proteins, which are about 800 amino acids in length (19). Moreover, it is noteworthy that all known ParE proteins are about 650 amino acids in length; this seems to confirm that the sequence assigned as the GyrB of C. trachomatis belonged to DNA gyrase subunit B. Moreover, the gyrB and gyrA genes of C. trachomatis were found to be contiguous, as described recently (19). In Chlamydia (19), gram-positive bacteria such as S. aureus (27) and B. subtilis (29), mycoplasmas (except Mycoplasma hominis), and spirochetes (19), the gyrB and gyrA genes are contiguous, whereas in gram-negative proteobacteria such as E. coli or Haemophilus influenzae, the gyrA and gyrB genes have different chromosomal locations (19). Furthermore, since no terminator-like structure was found between the gyrB and gyrA genes of C. trachomatis, it is likely that the DNA gyrase genes are transcribed as a single message.
Partial sequences of the Topo IV genes of C. trachomatis were also determined. When compared to the ParC proteins of other bacterial genera, the ParC sequence of C. trachomatis was more related to that of B. burgdorferi, confirming the recent observations of Huang (19).
The sequence of the ParE protein of C. trachomatis, which shares a low degree of homology with those of the ParE proteins of gram-negative and gram-positive bacteria, is closely related to the B. burgdorferi ParE sequence and shares some common motifs with it; this is in agreement with a recent comparative study of the bacterial type II topoisomerase subunit genes (19). Moreover, as found for the other bacterial ParE sequences that are known, the C-terminal region of the chlamydial ParE protein is about 150 amino acids shorter than those of the proteobacterial and chlamydial GyrB proteins. Like the DNA gyrase genes, the parC and parE genes of C. trachomatis were found to be contiguous, as has been found in gram-positive bacteria such as S. aureus (6) and B. subtilis (43). Furthermore, as found for the gyrase genes, no terminator-like structure was detected between the parE and parC genes of C. trachomatis, suggesting that the Topo IV genes are also cotranscribed.
In summary, this study revealed that in C. trachomatis, the genes encoding the two subunits of the DNA gyrase, on the one hand, and Topo IV, on the other hand, are contiguous, as is found in gram-positive bacteria and spirochetes. The GyrB protein of C. trachomatis is similar in length to that of the gram-negative bacteria, and the chlamydial Topo IV proteins appeared to be more closely related to that of the spirochete B. burgdorferi. The sequences reported here for the L2 strain of C. trachomatis are very similar to those for the serovar D strain, whose complete genome sequence is available at http://chlamydia-www.berkeley.edu:4231/. The sequences of both the gyrA and the gyrB genes identified in that sequence correspond to the gyrA-like (gyrA and parC) and gyrB-like (gyrB and parE) sequences, respectively, described here.
Here the isolation and characterization of in vitro-selected strains of C. trachomatis highly resistant to fluoroquinolones are reported. These mutants were selected from reference strain C. trachomatis L2 by stepwise selection with ofloxacin and sparfloxacin. The resistant chlamydial strains L2-OFXR and L2-SPXR showed high levels of resistance to all the fluoroquinolones tested and were susceptible to unrelated antibiotics (i.e., doxycycline and erythromycin).
Sequencing of the gyrA QRDRs of both resistant strains of C. trachomatis revealed only one point mutation (G→T) leading to the Ser83→Ile substitution. This single mutation was still present in the L2-OFXR and L2-SPXR strains cultivated without antibiotic for four passages, suggesting that the mutation is stable (data not shown). The amino acid at position 83 in the E. coli GyrA protein is the one most commonly associated with quinolone resistance (54). The Ser→Ile change is not the most prevalent substitution, but it has been described in clinical isolates of Enterococcus faecalis (23, 48) and Aeromonas salmonicida (33). A Thr83→Ile substitution in GyrA has also been described in clinical isolates of C. jejuni and Pseudomonas aeruginosa, which had high-level resistance to nalidixic acid and ciprofloxacin, respectively (25, 53). The Ser83→Ile change found in C. trachomatis is similar to the Ser83→Leu or Trp mutations in E. coli GyrA, leading to the replacement of a small polar amino acid by a nonpolar residue (5, 34). Interestingly, in resistant C. trachomatis strains, the G→T mutation in the gyrA QRDR led to the creation of a restriction site for the Tsp509I endonuclease and can be detected by restriction fragment length polymorphism analysis of the amplified fragment. The presence of the additional restriction site for Tsp509I could be used to identify the gyrA mutation in clinical isolates of C. trachomatis whose antibiotic susceptibilities are not systematically studied. Commonly, gyrA mutations at Ser83 led to the loss of the HinfI restriction enzyme site in resistant strains (8).
Recently, the first isolation of fluoroquinolone-resistant mutant from an intracellular bacterium, Coxiella burnetii, has been described (31). Sequence analysis of the gyrA QRDR of this strain with high-level resistance revealed a point mutation at position 87 (E. coli numbering). The selective agent was ciprofloxacin, whereas in our study, mutants were selected with ofloxacin and sparfloxacin.
The high level of resistance of the C. trachomatis mutants might not be explained by only one point mutation in their gyrA genes. Mutations in the gyrB (20, 55), parC (24, 32), and parE (3, 9, 37) genes which confer fluoroquinolone resistance in bacteria have been described. However, sequencing of the parC, gyrB, and parE QRDRs of the resistant strains C. trachomatis L2-OFXR and L2-SPXR revealed no mutations in their sequences compared with the sequence of the susceptible reference strain. The present results suggest that gyrase may be the primary target of fluoroquinolones in C. trachomatis, a gram-negative bacterium, which is in agreement with previous studies. Indeed, gyrA mutations have been described to occur primarily in gram-negative bacteria after exposure to fluoroquinolones, with parC-mediated resistance being detectable only in gyrA mutants (2, 16). In contrast, in the gram-positive bacterium S. aureus, mutations in the parC QRDR have been detected in strains with low-level quinolone resistance and precede those in gyrA (6, 7, 32), suggesting that in this species Topo IV is the primary target of quinolones, with the gyrase being altered secondarily. In Streptococcus pneumoniae, another gram-positive bacterium, the primary targets of ciprofloxacin and sparfloxacin are Topo IV and gyrase, respectively (35). Thus, in S. pneumoniae, the nature of the primary target of quinolones seems to be dependent on the drug structure. In C. trachomatis, ofloxacin and sparfloxacin primarily target the same enzyme, DNA gyrase.
As found in C. psittaci (19), the ParC protein of C. trachomatis harbors an alanine residue at position 80 (E. coli numbering), a nonpolar amino acid. A comparative study of the intrinsic susceptibility to ofloxacin of reference strains of nine Mycobacterium species revealed that those harboring an Ala-83 in GyrA were 4- to 64-fold less susceptible than species harboring a serine residue at the same position (13). Moreover, an Ser→Ala substitution at position 83 in E. coli and S. aureus GyrA has been shown to confer relatively low-level resistance to quinolones (12, 14). Thus, the presence of an alanine at position 80 in ParC of Chlamydia may be responsible for the lower affinity of the ParC than the GyrA subunit for fluoroquinolones in this genus.
The possibility that other mechanisms of resistance involving drug permeation and/or drug efflux modifications may contribute to the high-level resistance to fluoroquinolones in C. trachomatis cannot be excluded. However, alteration of permeability or efflux mechanisms are usually responsible for low-level resistance and are associated with cross-resistance with different families of antibiotics. In summary, the present results suggest that high-level resistance to fluoroquinolones in C. trachomatis is associated with a Ser83→Ile substitution in the GyrA QRDR, whereas the other topoisomerase QRDRs were not found to be altered at this step of selection with ofloxacin and sparfloxacin. It will be interesting to continue stepwise selection with the same antibiotics to investigate the occurrence of parC mutations and to use other fluoroquinolones as selective agents to determine whether GyrA is the primary target of all quinolones in C. trachomatis. Selection of quinolone-resistant strains of C. trachomatis by repeated exposures of a susceptible strain to ofloxacin and sparfloxacin suggests that acquired resistance may occur in vivo during quinolone therapy, and therefore, surveillance of this situation will be necessary.
ACKNOWLEDGMENT
This work was supported by a grant from Conseil Régional d’Aquitaine.
REFERENCES
- 1.Adams D E, Shekhtmann E M, Zechiedrich E L, Schmid M B, Cozzarelli N R. The role of topoisomerase IV in partitioning bacterial replicons and the structure of catenated intermediates in DNA replication. Cell. 1992;71:277–288. doi: 10.1016/0092-8674(92)90356-h. [DOI] [PubMed] [Google Scholar]
- 2.Belland R J, Morrison S G, Ison C, Huang W H. Neisseria gonorrhoeae acquires mutations in analogous regions of gyrA and parC in fluoroquinolone-resistant isolates. Mol Microbiol. 1994;14:371–380. doi: 10.1111/j.1365-2958.1994.tb01297.x. [DOI] [PubMed] [Google Scholar]
- 3.Breines D M, Ouadbesselam S, Ng E Y, Tankovic J, Shah S, Soussy C J, Hooper D C. Quinolone resistance locus nfxD of Escherichia coli is a mutant allele of the parE gene encoding a subunit of topoisomerase IV. Antimicrob Agents Chemother. 1997;41:175–179. doi: 10.1128/aac.41.1.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burland V, Plunkett III G, Daniels D L, Blattner F R. DNA sequence and analysis of 136 kilobases of the Escherichia coli genome: organizational symmetry around the origin of replication. Genomics. 1993;16:551–561. doi: 10.1006/geno.1993.1230. [DOI] [PubMed] [Google Scholar]
- 5.Cullen M E, Wyke A W, Kuroda R, Fisher L M. Cloning and characterization of a DNA gyrase A gene from Escherichia coli that confers clinical resistance to 4-quinolones. Antimicrob Agents Chemother. 1989;33:886–894. doi: 10.1128/aac.33.6.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferrero L, Cameron B, Manse B, Lagneaux D, Crouzet J, Framechon A, Blanche F. Cloning a primary structure of Staphylococcus aureus DNA topoisomerase IV: a primary target of fluoroquinolones. Mol Microbiol. 1994;13:641–653. doi: 10.1111/j.1365-2958.1994.tb00458.x. [DOI] [PubMed] [Google Scholar]
- 7.Ferrero L, Cameron B, Crouzet J. Analysis of gyrA and grlA mutations in stepwise-selected ciprofloxacin-resistant mutants of Staphylococcus aureus. Antimicrob Agents Chemother. 1995;39:1554–1558. doi: 10.1128/aac.39.7.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher, L. M., J. M. Lawrence, I. C. Josty, R. Hopewell, and E. E. C. Margerrison. 1989. Ciprofloxacin and the fluoroquinolones—new concepts on the mechanism of action and resistance. Am. J. Med. 87(Suppl. 5A):2S–8S. [DOI] [PubMed]
- 9.Fournier B, Hooper D C. Mutations in topoisomerase IV and DNA gyrase of Staphylococcus aureus: novel pleiotropic effects on quinolone and coumarin activity. Antimicrob Agents Chemother. 1998;42:121–128. doi: 10.1128/aac.42.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fraser C M, Casjens S, Huang W M, Sutton G G, Clayton R A, Lathigra R, White O, Ketchum K A, Dodson R, Hickey E K, Gwinn M, Dougherty B, Tomb J-F, Fleischmann R D, Richardson D, Peterson J, Kerlavage A R, Quackenbush J, Salzberg S, Hanson M, van-Vugt R, Palmer N, Adams M D, Gocayne J D, Weidman J, Utterback T, Watthey L, McDonald L, Artiach P, Bowman C, Garland S, Fujii C, Cotton M D, Horst K, Roberts K, Hatch B, Smith H O, Venter J C. Genomic sequence of a Lyme disease spirochete, Borrelia burgdorferi. Nature. 1997;390:580–586. doi: 10.1038/37551. [DOI] [PubMed] [Google Scholar]
- 11.Gensberg K, Jin Y F, Piddock L J V. A novel gyrB mutation in a fluoroquinolone-resistant clinical isolate of Salmonella typhimurium. FEMS Microbiol Lett. 1995;132:57–60. doi: 10.1111/j.1574-6968.1995.tb07810.x. [DOI] [PubMed] [Google Scholar]
- 12.Goswitz J J, Willard K E, Fashing C E, Peterson L R. Detection of gyrA gene mutations associated with ciprofloxacin resistance in methicillin-resistant Staphylococcus aureus: analysis by polymerase chain reaction and automated direct DNA sequencing. Antimicrob Agents Chemother. 1992;36:1166–1169. doi: 10.1128/aac.36.5.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guillemin I, Cambau E, Jarlier V. Sequences of conserved region in the A subunit of DNA gyrase from nine species of the genus Mycobacterium: phylogenetic analysis and implication for intrinsic susceptibility to quinolones. Antimicrob Agents Chemother. 1995;39:2145–2149. doi: 10.1128/aac.39.9.2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hallett P, Maxwell A. Novel quinolone resistance mutations of the Escherichia coli DNA gyrase A protein: enzymatic analysis of the mutant proteins. Antimicrob Agents Chemother. 1991;35:335–340. doi: 10.1128/aac.35.2.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heisig P, Schedletzky H, Falkenstein-Paul H. Mutations in the gyrA gene of a highly fluoroquinolone-resistant clinical isolate of Escherichia coli. Antimicrob Agents Chemother. 1993;37:696–701. doi: 10.1128/aac.37.4.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heisig P. Genetic evidence for a role of parC mutations in development of high-level fluoroquinolone resistance in Escherichia coli. Antimicrob Agents Chemother. 1996;40:879–885. doi: 10.1128/aac.40.4.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hopewell R, Oram M, Briesewitz R, Fisher L M. DNA cloning and organization of the Staphylococcus aureus gyrA and gyrB genes: close homology among gyrase proteins and implications for 4-quinolone action and resistance. J Bacteriol. 1990;172:3481–3484. doi: 10.1128/jb.172.6.3481-3484.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang W M. Multiple DNA gyrase-like in eubacteria. In: Andoh T, Ikeda H, Oguro M, editors. Molecular biology of DNA topoisomerases and its application to chemotherapy. London, United Kingdom: CRC Press; 1992. pp. 39–48. [Google Scholar]
- 19.Huang W M. Bacterial diversity based on type II DNA topoisomerase genes. Annu Rev Genet. 1996;30:79–107. doi: 10.1146/annurev.genet.30.1.79. [DOI] [PubMed] [Google Scholar]
- 20.Ito H, Yoshida H, Bogaki-Shonai M, Niga T, Hattori H, Nakamura S. Quinolone resistance mutations in the DNA gyrase gyrA and gyrB genes of Staphylococcus aureus. Antimicrob Agents Chemother. 1994;38:2014–2023. doi: 10.1128/aac.38.9.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones R B, Van Der Pol B, Martin D H, Shepard M K. Partial characterization of Chlamydia trachomatis isolates resistant to multiple antibiotics. J Infect Dis. 1990;162:1309–1315. doi: 10.1093/infdis/162.6.1309. [DOI] [PubMed] [Google Scholar]
- 22.Kato J, Nishimura Y, Imamura R, Niki H, Hiraga S, Suzuki H. New topoisomerase essential for chromosome segregation in Escherichia coli. Cell. 1990;63:393–404. doi: 10.1016/0092-8674(90)90172-b. [DOI] [PubMed] [Google Scholar]
- 23.Korten V, Huang W M, Murray B E. Analysis by PCR and direct DNA sequencing of gyrA mutations associated with fluoroquinolone resistance in Enterococcus faecalis. Antimicrob Agents Chemother. 1994;38:2091–2094. doi: 10.1128/aac.38.9.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kumagai Y, Kato J I, Hoshino K, Akasaka T, Sato K, Ikeda H. Quinolone-resistant mutants of Escherichia coli DNA topoisomerase IV parC gene. Antimicrob Agents Chemother. 1996;40:710–714. doi: 10.1128/aac.40.3.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kureishi A, Diver J M, Beckthold B, Schollaardt T, Bryan L E. Cloning and nucleotide sequence of Pseudomonas aeruginosa DNA gyrase gyrA gene from strain PAO1 and quinolone-resistant clinical isolates. Antimicrob Agents Chemother. 1994;38:1944–1952. doi: 10.1128/aac.38.9.1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ladefoged S A, Christiansen G. Sequencing analysis reveals a unique gene organisation in the gyrB region of Mycoplasma hominis. J Bacteriol. 1994;176:5835–5842. doi: 10.1128/jb.176.18.5835-5842.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Margerrison E E C, Hopewell R, Fisher L M. Nucleotide sequence of the Staphylococcus aureus gyrB-gyrA locus encoding the DNA gyrase A and B proteins. J Bacteriol. 1992;174:1596–1603. doi: 10.1128/jb.174.5.1596-1603.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moore R A, Beckthold B, Wong S, Kureishi A, Bryan L E. Nucleotide sequence of the gyrA gene and characterization of ciprofloxacin-resistant mutants of Helicobacter pylori. Antimicrob Agents Chemother. 1995;39:107–111. doi: 10.1128/aac.39.1.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moriya S, Ogasawara N, Yoshikawa H. Structure and function of the region of the replication origin of the Bacillus subtilis chromosome. III. Nucleotide sequence of some 10000 base pairs in the origin region. Nucleic Acids Res. 1985;13:2251–2265. doi: 10.1093/nar/13.7.2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mourad A, Sweet R L, Sugg N, Schachter J. Relative resistance to erythromycin in Chlamydia trachomatis. Antimicrob Agents Chemother. 1980;18:696–698. doi: 10.1128/aac.18.5.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Musso D, Drancourt M, Osscini S, Raoult D. Sequence of quinolone resistance-determining region of gyrA gene for clinical isolates and for an in vitro-selected quinolone-resistant strain of Coxiella burnetii. Antimicrob Agents Chemother. 1996;40:870–873. doi: 10.1128/aac.40.4.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ng E Y, Trucksis M, Hooper D C. Quinolone resistance mutations in topoisomerase IV: relationship to the flqA locus and genetic evidence that topoisomerase IV is the primary target and DNA gyrase is the secondary target of fluoroquinolones in Staphylococcus aureus. Antimicrob Agents Chemother. 1996;40:1881–1888. doi: 10.1128/aac.40.8.1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oppegaard H, Sorum H. gyrA mutations in quinolone-resistant isolates of the fish pathogen Aeromonas salmonicida. Antimicrob Agents Chemother. 1994;38:2460–2464. doi: 10.1128/aac.38.10.2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oram M, Fisher L M. 4-Quinolone resistance mutations in the DNA gyrase of Escherichia coli clinical isolates identified by using the polymerase chain reaction. Antimicrob Agents Chemother. 1991;35:387–389. doi: 10.1128/aac.35.2.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pan X-S, Fisher L M. Targeting of DNA gyrase in Streptococcus pneumoniae by sparfloxacin: selective targeting of gyrase or topoisomerase IV by quinolones. Antimicrob Agents Chemother. 1997;41:471–474. doi: 10.1128/aac.41.2.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perea E J, Aznar J, Garcia-Iglesias M C, Pascual A. Comparative in vitro activity of sparfloxacin against genital pathogens. J Antimicrob Chemother. 1996;37:19–25. doi: 10.1093/jac/37.suppl_a.19. [DOI] [PubMed] [Google Scholar]
- 37.Perichon B, Tankovic J, Courvalin P. Characterization of a mutation in the parE gene that confers fluoroquinolone resistance in Streptococcus pneumoniae. Antimicrob Agents Chemother. 1997;41:1166–1167. doi: 10.1128/aac.41.5.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Phillips I, Dimian C, Barlow D, Moi H, Stolz E, Weidner W, Perea E. A comparative study of two different regimens of sparfloxacin versus doxycycline in the treatment of non-gonococcal urethritis in men. J Antimicrob Chemother. 1996;37:123–134. doi: 10.1093/jac/37.suppl_a.123. [DOI] [PubMed] [Google Scholar]
- 39.Piddock L J V. Mechanisms of resistance to fluoroquinolones: state-of-the-art 1992–1994. Drugs. 1995;49:29–35. doi: 10.2165/00003495-199500492-00006. [DOI] [PubMed] [Google Scholar]
- 40.Reece R, Maxwell A. DNA gyrase: structure and function. Crit Rev Biochem Mol Biol. 1991;26:335–375. doi: 10.3109/10409239109114072. [DOI] [PubMed] [Google Scholar]
- 41.Ridgway G L. Treatment of chlamydial genital infection. J Antimicrob Chemother. 1997;40:311–314. doi: 10.1093/jac/40.3.311. [DOI] [PubMed] [Google Scholar]
- 42.Rodriguez P, Allardet-Servent A, de Barbeyrac B, Ramuz M, Bébéar C. Genetic variability among Chlamydia trachomatis reference and clinical strains analyzed by pulsed-field gel electrophoresis. J Clin Microbiol. 1994;32:2921–2928. doi: 10.1128/jcm.32.12.2921-2928.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rose M, Entian K D. New genes in the 170 degrees region of the Bacillus subtilis genome encode DNA gyrase subunits, a thioredoxin, a xylanase and an amino acid transporter. Microbiology. 1996;142:3097–3101. doi: 10.1099/13500872-142-11-3097. [DOI] [PubMed] [Google Scholar]
- 44.Sambrook J, Fritsch E F, Maniatis T. Molecular cloning: a laboratory manual. 2nd ed. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory Press; 1989. [Google Scholar]
- 45.Samuels D S, Marconi R T, Huang W M, Garon C F. gyrB mutations in coumermycin A1-resistant Borrelia burgdorferi. J Bacteriol. 1994;176:3072–3075. doi: 10.1128/jb.176.10.3072-3075.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Scieux C, Grimont F, Regnault B, Grimont P A D. DNA fingerprinting of Chlamydia trachomatis by use of ribosomal RNA, oligonucleotide and randomly cloned probes. Res Microbiol. 1992;143:755–765. doi: 10.1016/0923-2508(92)90103-u. [DOI] [PubMed] [Google Scholar]
- 47.Swanberg S L, Wang J C. Cloning and sequencing of the Escherichia coli gyrA gene coding for the A subunit of DNA gyrase. J Mol Biol. 1987;197:729–736. doi: 10.1016/0022-2836(87)90479-7. [DOI] [PubMed] [Google Scholar]
- 48.Tankovic J, Mahjoubi F, Courvalin P, Duval J, Leclercq R. Development of fluoroquinolone resistance in Enterococcus faecalis and role of mutations in the DNA gyrase A gene. Antimicrob Agents Chemother. 1996;40:2558–2561. doi: 10.1128/aac.40.11.2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Taylor-Robinson D. Genital chlamydial infections: clinical aspects, diagnosis, treatment and prevention. In: Harris J R W, Foster S M, editors. Recent advances in sexually transmitted diseases and AIDS. London, United Kingdom: Churchill Livingstone; 1991. pp. 219–262. [Google Scholar]
- 50.Tipples G, McClarty G. Isolation and initial characterization of a series of Chlamydia trachomatis isolates selected for hydroxyurea resistance by a stepwise procedure. J Bacteriol. 1991;173:4932–4940. doi: 10.1128/jb.173.16.4932-4940.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang J C. DNA topoisomerases. Annu Rev Biochem. 1996;65:635–692. doi: 10.1146/annurev.bi.65.070196.003223. [DOI] [PubMed] [Google Scholar]
- 52.Wang L L, Henson E, McClarty G. Characterization of trimethoprim- and sulphisoxazole-resistant Chlamydia trachomatis. Mol Microbiol. 1994;14:271–281. doi: 10.1111/j.1365-2958.1994.tb01288.x. [DOI] [PubMed] [Google Scholar]
- 53.Wang Y, Huang W-M, Taylor D E. Cloning and nucleotide sequence of Campylobacter jejuni gyrA gene and characterization of quinolone resistance mutations. Antimicrob Agents Chemother. 1993;37:457–463. doi: 10.1128/aac.37.3.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yoshida H, Bogaki M, Nakamura M, Nakamura S. Quinolone resistance-determining region in the DNA gyrase gyrA gene of Escherichia coli. Antimicrob Agents Chemother. 1990;34:1271–1272. doi: 10.1128/aac.34.6.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yoshida H, Bogaki M, Nakamura M, Yamanaka L M, Nakamura S. Quinolone resistance-determining region in the DNA gyrase gyrB gene of Escherichia coli. Antimicrob Agents Chemother. 1991;35:1647–1650. doi: 10.1128/aac.35.8.1647. [DOI] [PMC free article] [PubMed] [Google Scholar]