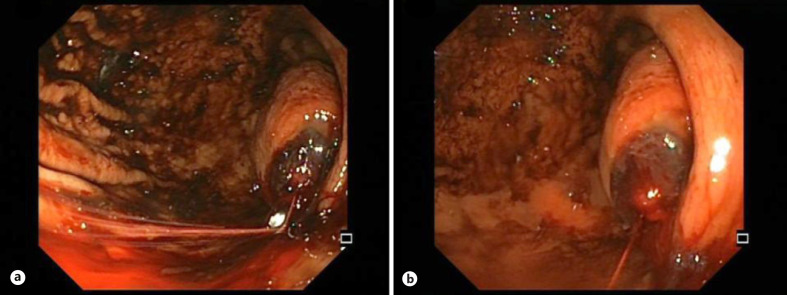
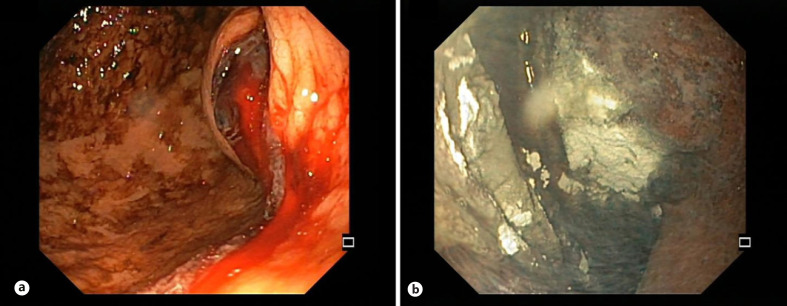
A 61-year-old man presented to the emergency department with hematemesis. The patient referred epigastric pain, anorexia, and vomits for the past 3 days. He had a medical history of dyslipidemia and chronic venous insufficiency under treatment with bioflavonoids and a statin. Physical examination was unremarkable. Laboratorial analysis revealed a serum hemoglobin of 9.6 g/dL (normal range 13–18 g/dL). Fluids and a bolus of esomeprazole were administered, and the patient was submitted to an esophagogastroscopy (Fig. 1). Esophagogastroscopy revealed a 5-cm spheric subepithelial lesion with central ulceration and pulsatile bleeding in the posterior wall of the gastric corpus (Fig. 1). Endoscopic treatment was performed with adrenalin injection in the ulcer margins and application of 4 clips on the vessel, which controlled the bleeding. Bite-on-bite biopsies of the ulcer borders were performed due to the suggestive features of a ruptured gastrointestinal stromal tumor (GIST) [1]. Due to the impossibility of complete closure of the ulcer and doubts if the bleeding completely stopped, hemospray® was applied over the lesion (Fig. 2). The biopsy samples were insufficient for histological characterization. A CT scan revealed a 5-cm nodular lesion with heterogeneous contrast enhancement in the posterior wall of the stomach without evidence of invasion of adjacent structures or metastatic disease. The differential diagnosis should be made with other potentially malignant subepithelial lesions of the stomach, namely, leiomyoma, glomus tumor, or neuroendocrine tumor. Nevertheless, the alternative diagnoses were less likely due to the ulceration, the location of the lesion, and the heterogeneous contrast enhancement in the CT scan [1, 2, 3].
Fig. 1.
a, b Endoscopic view of the gastric corpus before endoscopic treatment.
Fig. 2.
Endoscopic view of the gastric corpus after adrenalin injection in the bleeding lesion (a) and at the end of the endoscopic treatment (b).
The patient was submitted to an elective partial gastrectomy. The histological exam confirmed the diagnosis of a GIST with positive immunohistochemical staining for CD34, CD117, and DOG1 with preserved SDHB expression (stage pT2 G1 N0 R0) [4, 5]. One year after the diagnosis, the patient has no evidence of disease. This endoscopic snapshot illustrates a typical presentation of a large gastric GIST with massive luminal bleeding [5]. Endoscopic treatment was performed with success as a bridge to surgery [5].
Statement of Ethics
Written informed consent was obtained from the patient for publication of the details of their medical case and any accompanying images.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors have no funding to declare.
Author Contributions
S.S.M. performed the endoscopy and drafted the manuscript; R.G. and A.C.C. provided critical revision and completed the manuscript.
Data Availability Statement
The data that support the findings of this study are not publicly available due to their containing information that could compromise the privacy of research participants but are available from the corresponding author (S.S.M.) upon reasonable request.
Funding Statement
The authors have no funding to declare.
References
- 1.Faulx AL, Kothari S, Acosta RD, Agrawal D, Bruining DH, Chandrasekhara V, et al. The role of endoscopy in subepithelial lesions of the GI tract. Gastrointest Endosc. 2017;85((6)):1117–32. doi: 10.1016/j.gie.2017.02.022. [DOI] [PubMed] [Google Scholar]
- 2.Okanoue S, Iwamuro M, Tanaka T, Satomi T, Hamada K, Sakae H, et al. Scoring systems for differentiating gastrointestinal stromal tumors and schwannomas from leiomyomas in the stomach. Medicine. 2021;100((40)):e27520. doi: 10.1097/MD.0000000000027520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu M, Liu L, Jin E. Gastric sub-epithelial tumors: identification of gastrointestinal stromal tumors using CT with a practical scoring method. Gastric Cancer. 2019;22((4)):769–77. doi: 10.1007/s10120-018-00908-6. [DOI] [PubMed] [Google Scholar]
- 4.WHO Classification of Tumours Editorial Board . 5th ed. Vol. 3. Lyon, France: IARC; 2020. Soft tissue and bone tumours. ISBN–13 978–92–832–4502–5. [Google Scholar]
- 5.Casali PG, Blay JY, Abecassis N, Bajpai J, Bauer S, Biagini R, et al. Gastrointestinal stromal tumours: ESMO-EURACAN-GENTURIS Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2022;33((1)):20–33. doi: 10.1016/j.annonc.2021.09.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are not publicly available due to their containing information that could compromise the privacy of research participants but are available from the corresponding author (S.S.M.) upon reasonable request.