Abstract
This study analyzes the COVID-19 homelessness response in King County, Washington, in which people were moved out of high-density emergency shelters into hotel rooms. This intervention was part of a regional effort to de-intensify the shelter system and limit the transmission of the virus to protect vulnerable individuals experiencing homelessness. This study used quantitative and qualitative methods to describe the experiences of and outcomes on individuals who were moved from shelters to noncongregate hotel settings. The study highlights a new approach to shelter delivery that not only responded to the public health imperatives of COVID-19, but also indicated positive health and social outcomes compared to traditional congregate settings. The findings establish an evidence base to help inform future strategic responses to homelessness as well as to contribute to the broader policy conversations on our nation’s response to homelessness.
Keywords: Homelessness, shelter, COVID-19, policy, evaluation
The most common homelessness intervention in the United States is the use of emergency shelters, which can be a lifesaving intervention for unhoused individuals and families who need a place to sleep. The risk of mortality for people experiencing unsheltered homelessness (i.e., those living on the street or other unsheltered locations) is 10 times that of the general population and 3 times that of the adult sheltered homeless population (Roncarati et al., 2018). The health consequences of unsheltered homelessness are also significant, including higher reports of mental health issues, substance abuse, and serious medical issues (Levitt et al., 2009). These consequences as well as right-to-shelter laws in many jurisdictions provide the justification and motivation for the broad use of emergency shelters as a response to unsheltered homelessness.
A broader perspective notes that shelter is just one of many types of housing or housing support that can be provided to precariously housed families and individuals, and these various forms of housing are not all created equal. Even though emergency shelter may provide some benefits over unsheltered homelessness, the shelter system is not an effective, permanent response to homelessness. Importantly, emergency shelter is not housing—either in a conceptual sense or in terms of legal definitions. According to the U.S. Department of Housing and Urban Development (HUD)’s official definition of homelessness, those residing in the emergency shelter system are still considered homeless. The literature highlights a range of negative outcomes for those who temporarily reside in congregate shelters (Daiski, 2007), which underscores the shortcomings of this common response to homelessness. Providing a shelter experience that more closely resembles permanent housing has the potential to lessen or mitigate these shortcomings.
In general, most emergency shelters are congregate settings—large numbers of people are housed in relatively small spaces. The reason for the dense living conditions is clear: shelters attempt to serve as many people as possible. The existing literature highlights numerous shortcomings of traditional congregate emergency shelter models. Crowding people—many of whom are experiencing intersecting crises—in dense, congregate settings has a host of negative consequences. Those staying in shelters often experience stress, violence, and poor physical and mental health (Daiski, 2007) as well as high rates of mortality (Barrow et al., 1999). Although shelters temporarily get people off the street, these settings generally do not promote the improved stability and health that are needed for people to end their homelessness crisis. Although these shortcomings of shelter systems are known, there has been little support and few resources devoted to meaningfully restructuring emergency shelters to promote the health and well-being of their residents. The arrival of COVID-19 provided the impetus and resources to modify the traditional, congregate shelter model—an unplanned innovation.
In April 2020, in response to the outbreak of COVID-19, King County, Washington, took the unprecedented step to move more than 700 people out of high-density congregate emergency shelters and into hotel rooms. Between April and December, these hotels served nearly 600 additional individuals. (We use the term group hotel to describe this intervention). This intervention was part of a regional effort to limit the transmission of the virus within homeless shelters and protect vulnerable individuals experiencing homelessness. Beyond the use of group hotels, King County, the City of Seattle, and service provider agencies took additional measures, including opening new shelters to provide more space in congregate settings to accommodate social distancing and decrease density in existing shelters. These efforts were all part of a regional effort known as shelter de-intensification. In all locations, King County and its partners supported providers to meet U.S. Centers for Disease Control and Prevention (CDC) and local public health guidance for social distancing as well as infection prevention and control.
Shortly after beginning to operate the group hotel locations, service providers and government staff began receiving positive feedback from clients and frontline workers—feedback that was unrelated to COVID-19 disease transmission. Based on a desire to systematically investigate the experiences and outcomes of this innovation, King County evaluation staff reached out to university researchers to initiate a research partnership. When the research partnership first formed, King County had secured federal funding to support the group hotels only through June 30, 2020. Given the interest in this intervention in local policy discussions and the anticipated challenges of locating homeless individuals after their exit from these hotels, the research team prioritized conducting the research as quickly as possible. As we finalized the research design in May 2020, King County announced an extension of the group hotels until August 31, 2020. Over the course of our study, we operated under the assumption that we had a limited window in which to conduct this research and learn about the intervention and its outcomes. Toward the end of our research, the county announced an extension of the intervention until the end of 2020. (Following the completion of our research, the group hotel shelter locations were subsequently funded through all of 2021). This sense of urgency simultaneously created study limitations while enabling the study’s policy impact. These trade-offs are further explored in the discussion section.
Drawing from this context, the study addresses the following research questions: First, was the group hotel intervention successful in its primary goal of limiting the spread of COVID-19 among individuals experiencing homelessness? Following the anecdotal evidence indicating spillover benefits unrelated to COVID-19, the study also pursued more exploratory questions about the group hotel experience: What, if any, other outcomes were associated with this intervention? To the extent that there are additional benefits, what specific attributes of the intervention most contributed to these benefits?
Although this study provides evidence related to this intervention and its outcomes, there are important policy-relevant questions that remain unanswered with this research. For example, was this a cost-effective intervention? As we shared our initial report with the public, we were clear in highlighting that we presented these outcomes and conclusions independent of the cost of the intervention. That is, due to data and time limitations, we did not quantify the costs of the program and compare these costs to the benefits we identify. The cost effectiveness of new models of shelter provision is critically important to assess and deserves research attention. Our study helps to identify the outcomes of the intervention (some of which may be quantifiable, and others of which may not).
Drawing from analyses of administrative and interview data, the study findings indicate that this intervention was successful in its primary goal of limiting the spread of COVID-19 among individuals experiencing homelessness. Beyond reducing their risk of contracting the virus, the findings also revealed a host of benefits related to health and well-being experienced by individuals staying in the group hotel settings. This study expands our understanding of the potential for new or enhanced emergency shelter models to better support beneficial health and life outcomes for those they serve. Our findings underscore the important role that physical structure plays in the delivery of shelter services—different shelter settings have the potential to produce different results. We proceed in this paper by providing a summary of the relevant literature, describing the empirical context for the study, summarizing our data and methods, describing our key research findings, and concluding with a discussion of study limitations as well as how this study might inform future efforts to respond to the crisis of homelessness.
Literature Review
The existing literature highlights the important link between housing and health/well-being (Bonnefoy, 2007; Braubach, 2011; Jacobs et al., 2009; Sharpe et al., 2018). A lack of housing, or inferior housing conditions such as overcrowding and mold, is associated with a range of negative health outcomes (Bashir, 2002; Shenassa et al., 2007), including greater prevalence of infectious diseases (Fazel et al., 2014), poor mental health (Bashir, 2002; Bentley et al., 2012), and higher mortality (Fazel et al., 2014). Research also demonstrates that the negative health effects of inadequate housing persist in adulthood among those who were unstably housed as children (Marsh et al., 2000). These negative outcomes are partly due to the fact that unhoused people tend to receive less medical care and face higher barriers to receiving medical care (Kushel et al., 2001). However, the relationship between health and housing is more complex. Research demonstrates a bidirectional causal relationship, in which housing conditions affect health outcomes and health conditions affect housing outcomes (Bentley et al., 2012; Libman et al., 2012). Understandably, much of this literature focuses on poor housing and health outcomes, but extensions of this research also demonstrate that health outcomes improve as housing conditions do (Fitzpatrick-Lewis et al., 2011; Thomson et al., 2009).
Given the robust link between housing and health, the COVID-19 pandemic represented a particularly acute risk for unhoused populations. Qualitative research conducted prior to the pandemic confirmed that conventional, congregate shelter conditions were not conducive to good health; shelter residents believed that congregate shelter conditions promoted disease spread, violence, and emotional distress (Daiski, 2007). Studies conducted early in the pandemic demonstrated the disproportionate risk of COVID-19 for residents of homeless shelters (Baggett et al., 2020; Karb et al., 2020; Rogers et al., 2021). Researchers also noted that efforts to promote social distancing and residential stability reduce the risk of infection among people living in homeless shelters (Karb et al., 2020; O’Shea et al., 2021). The link between housing and health provides the empirical backdrop for our study.
Although using hotels to house the homeless was lauded as a new and novel response to homelessness, hotels have been used in the past to provide shelter for those without housing. Decades ago, single-room occupancy (SRO) hotels were a significant source of housing for people experiencing homelessness, especially in New York City (Sullivan & Burke, 2014). Over time, forces of gentrification largely eliminated SROs as a housing option for people who were precariously housed (Kasinitz, 1986), but the resurgence of the use of hotels to house the homeless during the pandemic represents the return of a housing type that has been dormant for decades (Doughtery, 2021). Even after SROs largely disappeared from the housing landscape, commercial hotels have been used as overflow housing for people experiencing homelessness, particularly in cities with right-to-shelter laws. Because these jurisdictions are required to provide a place to stay for people when congregate shelters are fully occupied, additional capacity is created by housing people temporarily in hotels. This use of hotels has been found to be very expensive and isolating for residents given that they are not treated as a traditional hotel guest would be; they are prohibited from mingling with paying customers and are not allowed to use any of the hotel facilities that are reserved for paying customers (Bhattacharyya, 2016). For this reason, the temporary use of hotels as overflow capacity has not been well received by policymakers or residents. This long history of using hotels to house the homeless suggests that context and implementation matter in determining the success or failure of this approach.
Empirical Context
The empirical site for our study is the King County shelter network. King County is a county located in Western Washington in the United States and includes the city of Seattle. The Seattle/King County Continuum of Care (CoC)1 has a large network of emergency shelters intended to reduce the region’s rate of unsheltered homelessness while also connecting individuals to housing and support services. According to the 2020 Point-In-Time (PIT) count, an estimated 11,751 individuals were experiencing homelessness in King County on the morning of January 24, 2020, and approximately 47% of those individuals were living unsheltered. The King County CoC has the third largest total homeless population among all CoCs in the country. According to the 2020 Housing Inventory Count (HIC), 40 provider agencies across the county reported a total inventory of 5,060 emergency shelter beds designated for adult households without children, youth and young adults, or families with children. The majority of the shelter capacity (57%) is concentrated in the five largest emergency shelter providers in King County—three of which participated in the qualitative portion of this study. On the night of the HIC, 4,291 of the 5,060 beds were filled—an overall utilization rate of 85%. According to data from the local Homeless Management Information System (HMIS), between April 1, 2019, and March 1, 2020, the King County emergency shelter system served over 25,600 households.
King County has a robust infrastructure to respond to the local crisis of homelessness. Nationwide, the Seattle–King County CoC has the third highest number of year-round beds in its homeless response system and the fifth highest number of year-round emergency shelter beds. A notable difference between King County and many other CoCs in the country is the relatively high percentage of the total homeless population that is unsheltered. A primary driver of this variation is that King County (and many other west coast cities) do not have right-to-shelter laws, whereas cities on the east coast, such as Boston (Massachusetts), New York, and Washington, DC, do. This legal difference helps to explain the higher percentage of the total homeless population that is sheltered in eastern cities.
Prior to the COVID-19 pandemic, King County’s emergency shelter programs offered a range of services with varying levels of support: from basic services of providing a place to sleep overnight (often mats on the floor or bunkbeds) and a check-in/check-out process to additional services that include 24/7 access to services and facilities, meals, bathrooms, medical care, case management, and mental health support.
King County Hotel Program
King County experienced the first U.S. outbreak of COVID-19 in February 2020. Local and statewide orders to prohibit large gatherings to reduce the spread of the virus followed, and large employers such as King County, the City of Seattle, Microsoft Corporation, and Amazon all mandated remote work for many of their employees. Public health officials identified that populations at the highest risk of infection and death from COVID-19 included older people, those with underlying health conditions, and those without the means or facilities to follow guidance on hygiene, social distancing, and self-isolation or quarantine. This meant that high-density congregate shelters and those using their services were particularly susceptible to outbreaks of COVID-19. A regional and cross-governmental partnership, including King County Department of Community and Human Services, the City of Seattle Human Services Department, Public Health—Seattle & King County, King County Facilities Management Division, the Healthcare for the Homelessness Network, King County METRO, and a network of community partners provided the infrastructure to de-intensify (or reduce density within) the shelter system in an effort to reduce the spread of COVID-19 among individuals experiencing homelessness in King County. These steps allowed existing shelters and new shelter locations (such as hotels) to adhere to social distancing requirements. Because entire shelters—and those residing in those shelters—moved from congregate settings to group hotels, the process for identifying the shelters to move locations was based on the population of people in those shelters (with a focus on those locations serving the most vulnerable) and the willingness of shelter operators to participate.
The county pursued a range of initiatives to implement the shelter de-intensification strategy. The opening of group hotels in particular was fundamental to facilitating the de-intensification of shelters while still maintaining services typically provided in shelters. The county used two strategies to de-intensify congregate shelters using hotels. First, the county leased six group hotels in their entirety (group hotels in Table 1). With this strategy, certain existing congregate shelters were closed, and all current shelter stayers, staff, and services (at the time of closure) moved to a new hotel location. In other words, these group hotels maintained pre-pandemic shelter communities but transitioned the clients and staff from congregate to group hotel settings. The six group hotels provide 24 hour / 7 days a week access and provided case management, security measures, meals, and secure storage for personal belongings. Shelter programs were selected for transition to group hotels based on a combination of the assessed COVID-19 risk within the shelter population (e.g., primarily based on density and age of population) and the willingness and capacity of nonprofit providers to collaborate on a rapid move to hotels. Because of the way the program was structured, there was no individual selection into the group hotels.
Table 1.
Primary de-intensification interventions.
| Item | Group hotels | De-intensified congregate shelter sites | Individual hoteling |
|---|---|---|---|
| Unique individuals served through 12/31/20 | 937 | 1,612 | 351 |
| Description | 6 leased hotels with provider staff on site 24/7, case management, and access to other services | Continue/expand emergency overnight services while meeting public health social distancing guidance through transitions to 7 new “de-intensified” sites | Used to move high-risk individuals from congregate settings into scattered hotel locations |
| Enhanced or basic services | Enhanced | Enhanced or basic | Basic |
| Included in study | Yes | Yes | No |
Note. Data in Table 1 are reported as of 2/1/2021 from the Seattle/King County Homeless Management Information System.
Second, the county provided funding to agencies to move a smaller number of individuals to hotel rooms scattered across the region, but without on-site shelter services and staff. In these situations, the hotels were not solely used for sheltering people experiencing homelessness and may have hosted other guests (individual hoteling category in Table 1). Both the group hotel and individual hoteling strategies offered shelter stayers private rooms (single or double occupancy) and bathrooms. Finally, beyond the use of hotels, the county also reorganized existing and new shelter locations to provide for greater social distancing within traditional, congregate shelter settings (the de-intensified congregate shelter sites in Table 1). Table 1 summarizes the primary de-intensification interventions used in King County.
Data and Methods
This study used a combination of quantitative and qualitative data to investigate the experiences and outcomes of people who stayed in the group hotels. This approach allowed us to rely on both administrative and interview data to generate a deeper understanding of the group hotel intervention and its outcomes. Our quantitative analysis is largely descriptive and compares the outcomes of people residing in group hotels and those staying in de-intensified congregate shelter sites.2 The qualitative component of the study included semistructured interviews with individuals who resided in group hotels during the pandemic after having previously stayed in traditional congregate shelters prior to COVID-19. The qualitative component also incorporates the perspectives of public and nonprofit staff involved with decision-making about and implementation of these interventions.
Quantitative Component
Using administrative data from multiple sources, we assess whether the group hotels limited the spread of COVID-19 (Research Question 1) and also explore the experiences of those who moved to group hotels (Research Questions 2 and 3). Analyses use cohort comparisons as well as program-level descriptive comparisons.
Sample Selection for Cohort Comparisons
The sample for the cohort comparisons was drawn from individuals within the Seattle/King County HMIS. This database captures information about all individuals who receive shelter services at a King County shelter that participates in HMIS, either because it is required to (i.e., receives HUD funding) or voluntarily. To construct a sample that includes individuals within all shelter types during the study period, the study team identified individuals who stayed at an emergency shelter serving adults without children—the population primarily impacted by this intervention—on February 26, 2020. This date marks the first confirmed case of COVID-19 in King County. Among adults receiving services in shelters on this date, we excluded individuals who exited the emergency shelter system before April 1, 2020 (the date when major COVID emergency response de-intensification efforts were in place) and did not return by August 31, 2020. These individuals were omitted because they did not experience the de-intensified condition in any location.
For the remaining individuals, we identified three cohorts (as outlined in Table 2) based on the type of shelter service received: group hotel (Cohort 1), enhanced shelter (Cohort 2), and shelter with basic services (Cohort 3). Both the enhanced shelter and shelter with basic services conditions constitute the de-intensified congregate shelter sites as outlined in Table 1. Because service intensity varied by enhanced versus basic services within the congregate sites, we created two cohorts to reflect these differences. In general, enhanced shelter sites provide unrestricted access and on-site case management, whereas shelter with basic services sites are more likely to have restricted times when clients can access the site and do not offer on-site case management.
Table 2.
Study population service details and demographics, by cohort.
| Item | Cohort 1: Group hotel | Cohort 2: Enhanced shelter | Cohort 3: Shelter with basic services | Total Study population |
|---|---|---|---|---|
| Study population and cohort sizes | ||||
| Size (n) | 383 | 926 | 326 | 1,635 |
| Size (% of total study population) | 23 | 57 | 20 | 100 |
| Service details | ||||
| De-intensified facility | Yes | Yes | Yes | |
| Room | Private | Shared | Shared | |
| Bathroom | Private | Shared | Shared | |
| Hours of access | 24/7 | Variable | Variable | |
| On-site case management | Yes | Yes | No | |
| Gender (% in cohort) | ||||
| Female | 31 | 24** | 39** | 29 |
| Male | 67 | 75*** | 60** | 70 |
| Other or unknown | 2 | 1 | 1 | 1 |
| Race and ethnicity (% in cohort) | ||||
| American Indian or Alaska Native | 1 | 3*** | 3*** | 3 |
| Asian | 4 | 3 | 6 | 4 |
| Black or African American | 28 | 29 | 19*** | 27 |
| Hispanic/Latino | 11 | 12 | 16* | 12 |
| Multiracial | 3 | 5 | 5 | 4 |
| Native Hawaiian or other Pacific Islander | 2 | 1 | 1 | 1 |
| White | 49 | 44 | 42* | 45 |
| Unknown | 4 | 2 | 9** | 4 |
| Age group (% in cohort) | ||||
| 18–24 | – | – | – | – |
| 25–54 | 52 | 58** | 63*** | 58 |
| 55 and older | 48 | 41** | 36*** | 41 |
| Chronic homeless status (%) | ||||
| Not Chronically homeless | 68 | 61*** | 83*** | 67 |
| Chronically homeless | 32 | 39*** | 18*** | 33 |
| Veteran status (%) | ||||
| Veteran Nonveteran | 7 | 12*** | 6 | 10 |
| Veteran Nonveteran | 93 | 88*** | 94 | 90 |
Note. Data in Table 2 are reported as of 9/1/2020 from the Seattle/King County Homeless Management Information System.
represent a statistically significant difference between Cohort 1 and Cohort 2, and between Cohort 1 and Cohort 3, at p ≤ .10, p ≤ .05 and p ≤ .01, respectively.
Sample Description
The study sample for the cohort analyses includes 1,635 total individuals. Table 2 summarizes the suite of services and cohort demographics of the three quantitative study cohorts. The sample is mostly male (70%), nearly half are White (45%), a third are Black or African American (27%), a little under half are 55 or older (41%), and a third are chronically homeless (U.S. Department of Housing and Urban Development, 2016).
When compared to the total study population, the people who moved to group hotel locations were slightly more likely to be female (31% vs. 29%). The group hotel population was slightly more White (49% vs. 45%), and American Indian and Alaska Native ethnicities were underrepresented (1% vs. 3%). Other racial categories in group hotels were similar in proportion to the overall study population, and those moved to group hotels were older than the study population (48% were 55 years old or older, compared to 41% for the overall study population). Shares of chronic homeless status between those placed in group hotels and the overall study population were very similar (68% vs. 67%), but veteran status was underrepresented (7% vs. 10%). As noted earlier, shelter programs were selected for group hotels based in part on the risk assessment at that time related to COVID-19 vulnerability. Given that age was the first risk factor identified by public health officials, shelters with older populations were more likely to be targeted for the group hotel intervention. In spite of cohort differences by age, other demographic comparisons do not indicate that the group hotel cohort was more advantaged or less vulnerable than those who were placed in Cohorts 2 and 3.
The six shelters that moved to group hotels were selected based on COVID-19 risk within their shelter population and providers’ willingness to move locations. In each of these cases, shelters moved all of their program participants at the time from the original locations to group hotel sites (Cohort 1 in Table 2). Thus, bias due to individual selection into the group hotel intervention is not an analytical concern. For congregate shelters moving some of their participants to new congregate settings as part of the efforts to spread out, or de-intensify, their populations, providers navigated the specific decisions about individuals’ moves based on immediate space needs, public health conditions in facilities, public health guidance on COVID-19 risk factors (age, health conditions), and each program participant’s willingness and ability to move locations (Cohort 2 and Cohort 3 in Table 2). Whether these participants moved to a new congregate setting or stayed in their original location, they were in congregate shelters in both time periods.
Data Sources and Outcome Variables
To compare the experiences and outcomes across the three groups, the cohort analyses drew outcome data from two administrative sources during the time frame of April 1, 2020, to August 31, 2020:
The Washington Disease Reporting System (WDRS), which measured the spread of COVID-19; and
HMIS, which indicated enrollment activity in housing services.
The binary outcome variable associated with the WDRS data is whether an individual received a positive COVID-19 test result during the study period. The binary outcome variables associated with HMIS enrollment activity are exits from shelter programs and completed assessment for permanent housing services.
In addition to the cohort analyses, the quantitative component leverages site-based data from two sources:
Publicly available emergency dispatch data from the Seattle Fire Department (they provided data about 911 calls at key shelter locations in Seattle); and
One nonprofit service provider’s proprietary administrative data (consisting of internally tracked 911 calls made to emergency personnel).
The key outcome variable for both sources is a standardized measure of incidents relative to shelter capacity, calculated by taking the count of corresponding incidents and dividing it by the bed-night capacity by location. “Bed-nights” is the total number of beds available to program participants during a given reporting period. For both data sets, the time frame is May 1 to October 20 in 2019 and 2020. This time frame was selected due to data availability on the part of the nonprofit provider, and subsequent alignment with public 911 data.
Quantitative Analysis
Data were cleaned and analyzed using R software. T-tests were used to compare mean outcomes on a range of demographic characteristics and program outcomes between the different cohorts. To identify HMIS clients in WDRS data, deterministic and probabilistic matching was based on full name and date of birth using the “fuzzyjoin” R package (Robinson, 2020). Three researchers reviewed and verified the accuracy of the code.
Qualitative Component
The study’s qualitative data were gathered via semistructured interviews in August and September 2020. Researchers conducted interviews with individuals representing two types of participants in the intervention: clients and staff. Purposive sampling for both groups prioritized representation from the different organizations and hotels as well as demographic variation among the client participants. Researchers also made numerous attempts to schedule interviews with individuals staying in de-intensified congregate shelters; however, this component of the research had to be cancelled because of logistical challenges and COVID-19 outbreaks.
Sample and Recruitment
Sampling and recruitment procedures varied in accordance with the two participant types.
Client Sample.
Researchers worked collaboratively with three service providers to identify and recruit a sample of individuals from four group hotel locations to participate in the qualitative portion of the study. Prior to recruitment, provider staff attended a training session that articulated the recruitment process, recruitment goals (i.e., recruitment of individuals across the different sites who represented diverse genders, age groups, races and ethnicities, and chronic homelessness status), and interview logistics. Following the completion of training, King County research team members ran a query of administrative records for each group hotel location based on the following eligibility criteria: experience in congregate emergency shelters within Seattle–King County prior to moving to a group hotel site and an active enrollment with the group hotel shelter at the time of the query.
To facilitate recruitment, provider staff referred to the list of eligible clients for each group hotel site. Although not used to determine eligibility, the lists also provided information on several demographic characteristics: gender identity, race/ethnicity, and chronic homelessness status. Provider staff were also given a recommendation for the number of participants to recruit stratified by the different identities (e.g., “one to two female or trans-female people of color; one chronically homeless male or trans-male of any race”). This information assisted the provider staff in achieving the recruitment goal of diverse representation across client interviewees. Researchers also equipped provider staff with informational materials to share with potential participants. Following successful recruitment, provider staff followed up with researchers to schedule interviews. A total of 22 clients staying at four group hotel locations operated by three nonprofit service providers participated in interviews.
Staff Sample.
Researchers recruited staff participants from among the nonprofit service providers and local government staff most involved with decision-making and oversight of the group hotel program, particularly during the initial implementation of the intervention. King County research team members identified the key staff at their agency. Other staff were identified based on leadership of the provider agencies involved, supplemented by word of mouth. Researchers reached out to potential staff participants via an email invitation that included basic study information. A total of nine staff participated representing the City of Seattle, King County, the three nonprofit service providers with clients who participated in the interviews, and a fourth service provider that managed one of the de-intensified congregate locations.
Data Collection and Procedure
Study participants from both the client and the staff sample participated in semistructured interviews led by university-affiliated members of the research team. Client interviews were conducted individually; three of the staff interviews included two staff from the same agency, totaling six interviews. The interview protocol for clients included the following topics: present experiences in the group hotel setting, past experiences in traditional congregate shelters (prior to the COVID-19 pandemic), the experience of transitioning from the congregate shelter to group hotel setting, and perspectives on the future. In the client interviews participants were also asked to share their race, gender, and age. Table 3 describes the group hotel interview participant demographics.
Table 3.
Hotel interview participant demographics.
| Demographic characteristic | n | % (of total) |
|---|---|---|
| Race | ||
| Black or African American | 7 | 31.8 |
| Multiracial/other | 4 | 18.2 |
| White | 6 | 27.3 |
| Unreported | 5 | 22.3 |
| Total | 22 | |
| Gender | 50.0 | |
| Male | 11 | |
| Female | 7 | 31.2 |
| Unreported | 5 | 22.3 |
| Total | 22 | |
| Age | ||
| Range: 33–60 | 51 (mean) |
The interview protocol for staff prompted general comments on the intervention and its implementation, the impacts and outcomes of the intervention (including for service recipients, staff, the agency, and the larger shelter system), and an overall assessment of the intervention, including next steps for the agency. Demographic data were not collected for the staff sample in order to protect confidentiality, given the smaller pool of participants.
All interviews were conducted via Zoom due to safety concerns related to COVID-19. Researchers provided iPads and detailed instructions to staff members at each hotel location in advance of the client interviews. Provider staff assisted with client interview scheduling and day-of logistics, but no providers were present during interviews with those staying in group hotels. Interview participants staying at the hotels received a $25 Visa gift card as an incentive for their participation. Staff participants did not receive an incentive but were interviewed during the workday. Interviews lasted between 10 and 65 minutes, with an average of 31 minutes.
Qualitative Analysis
All interviews were audio recorded and professionally transcribed. The research team used a six-phase approach to thematic analysis, based on Braun and Clarke (2012). Two members of the research team began the process by reviewing each of the interview transcripts (Phase 1), generating initial codes (Phase 2), and clustering codes and quotes for the purpose of identifying preliminary themes (Phase 3). Following this, two different members of the research team reviewed the preliminary themes (Phase 4) and further developed these themes in relation to the research questions (Phase 5). Finally, all research team members contributed to writing and revising the themes as qualitative findings (Phase 6).
Results
We present our results as responses to our three primary research questions. First, we highlight the effects of the hotel intervention on the spread of COVID-19 in the shelter system. Second, we highlight the additional outcomes of the intervention beyond preventing COVID-19 outbreaks. Last, we summarize the features of the hotel settings that were, according to participant interviews, most responsible for producing the favorable results that were identified.
Limiting the Spread of COVID-19
The primary purpose and motivation for the use of hotels and the de-intensification of congregate shelters was to prevent widespread COVID-19 outbreaks. Data derived both from the administrative data and the qualitative interviews confirmed that moving individuals from congregate shelter settings to group hotels successfully limited the spread of COVID-19. Figure 1 demonstrates the dramatic drop in positive COVID-19 cases following the move of individuals to group hotel locations in April 2020.
Figure 1.

COVID-19 positive cases among the study population, by cohort.
Note. Data in Figure 1 represent laboratory COVID-19 test results as reported to the Washington State Department of Health in the Washington Disease Reporting System (WDRS) between March 3, 2020, and September 8, 2020, as of September 25, 2020. Data reflect individuals’ associations with the study groups, not the locations individuals were infected or tested for COVID-19. Among the 1,635 individuals included in the study population, 54% (n = 884) had any test result. The research team was unable to determine the testing status for 17% of the study population (n = 284) as they did not consent to share identifying information in the Seattle/King County Homelessness Management Information System to link to the WDRS database. Those in Cohort 3—Congregate shelters with basic services accounted for 40% of this total, and their results may thus be disproportionately underrepresented in the figure. In addition, there may be individuals who were tested but could not be linked due to other data quality issues, such as the accuracy of names and other identifying information.
Throughout the study period, outbreaks among those experiencing homelessness mirrored the trends in the general population—an initial wave of COVID-19 outbreaks in the spring of 2020, followed by a decline in cases, and a second wave in the summer (see Figure 1). Among the sheltered homeless population in King County, an initial wave occurred at the traditional, congregate shelter sites that were ultimately shifted to group hotels; more than 3% of Cohort 1—the group that was moved to group hotels—tested positive in the weeks before de-intensification. After the implementation of shelter de-intensification, there was a decline in cases. A second wave did occur over the summer; however, it appeared only at congregate shelter sites—where more than 2% of Cohort 2 tested positive—not the group hotel locations. Among the quantitative study population, the small number of cases that occurred in group hotel (Cohort 1) locations constituted isolated, individual cases and did not result in outbreaks. Over the summer, the only outbreaks occurred in shelters offering enhanced services (Cohort 2) versus those with basic services (Cohort 3). One possible explanation for this difference is that compared to enhanced shelter sites, individuals at shelters with basic services may have less frequent personal interactions due to the lower level of services. Alternatively, the WDRS data may not have attributed some COVID-19 cases to individuals in the shelter sites with basic services given that these shelters have high rates of nonconsent to share personal data in HMIS, which is a condition for accurate data matching (see the note to Figure 1). We note that it would be inappropriate to compare the COVID-19 positivity rate among shelter stayers to that of the general public in the same time period, as Public Health—Seattle & King County implemented a comprehensive testing strategy for this at-risk population.3
In addition to the administrative data demonstrating the efficacy of the group hotels to limit the spread of COVID-19, we also heard about this success in our qualitative data. When discussing the effects of the pandemic on their experiences in the shelter system, interview participants confirmed that COVID-19 was a source of stress and concern. Some of the interviewees had contracted the virus while staying in congregate shelters and had recovered while staying in the hotels. For these individuals, COVID-19 added to the trauma of homelessness: “I was still weak. I’m so much better now, of course, but it affects me. I can’t explain how bad it was.”
Others moved from locations where an outbreak had occurred. One participant commented on how she “freaked out” in congregate shelter because “we have a numerous amount of people clamored together in one building and no escape … I felt really unsafe, very unsafe.” A staff member noted, “we’ve seen more COVID in those [congregate] settings, just flatly. When we’ve seen COVID it’s been harder to stop the potential spread.” At all locations in the shelter system (including hotels) staff implemented health protocols to reduce the likelihood of infection. Even in the group hotels, participants highlighted common challenges of living in a pandemic: “People have come up, and they’re not wearin’ a mask and wanna talk or whatever. I’m like, ‘Just stay and keep your distance.’” Even with the reduced risk of infection in hotel locations over congregate shelters, individuals continued to take precautions. One participant noted, “That virus definitely scares the heck out of me, and I’m doing everything I can to keep from getting it.”
Non-COVID Effects of the Hotel Intervention
Although limiting the spread of COVID-19 was the catalyst for shelter de-intensification, qualitative analysis of interviews and analysis of administrative data from HMIS and the emergency dispatch system suggest that the move to group hotels provided an improved living environment as compared to traditional congregate shelters. Statements such as “It’s better than shelter” and “It’s just better” emerged in nearly every interview with individuals staying in group hotels. One participant elaborated:
The sleeping area at the shelter, I mean, you was like two or three inches away from the next person. You roll over, they blow in your face, your ear. Now, you don’t have to worry ‘bout that. You got your own bed, your own space, your own room, and everything. To explain it, this is a whole lot better than the shelter.
These responses were not surprising to staff, who noted that “even before COVID, [we knew] that noncongregate is the best way to go.” As one staff member described, the challenging conditions found in congregate shelters could exacerbate problems that individuals experiencing homelessness were facing rather than to help resolve them:
I don’t think it can be overstated how stressful it is for people to experience homelessness. To be going through that and have the physical environment you’re in be a place that is unpleasant and crowded and filled with people who are tense and angry and acting strangely only further intensifies the experience that somebody has. It is debilitating. It stops people from taking action to deal with their own situations.
Staff did identify a tension between emergency and longer-term solutions, because “every dollar we’re taking to invest in shelter is a dollar that we’re not putting towards housing.” Yet, from the perspective of staff, the hotels offer a better response to the crisis of homelessness than traditional congregate shelters do. Staff also noted that a change in the shelter system is long overdue:
We would have never considered this new model in hotels. We had been advocating for many years in many of these programs that they were undersourced, that people were not getting the wraparound care that they needed … . What we had during COVID is money to make significant changes. That cannot be discounted, right?
In addition to the consensus that the group hotels represented a marked improvement over congregate settings, specific benefits emerged from the analysis. The following sections describe individual benefits of the hotel intervention related to stability, program engagement, health and well-being, feelings of safety, interpersonal conflict, and ability to focus on and plan for the future. Although we present these effects as independent findings, they intersect and overlap and contribute to our understanding of the health and social benefits of this particular intervention.
Residential Stability and Feelings of Home
Both the interviews and the administrative analysis indicated that the group hotels engendered a greater sense of stability than traditional congregate shelters do. HMIS data from the study population demonstrate that after moving into hotels, individuals had far more residential stability than they typically did in a traditional congregate shelter setting pre-COVID (see Table 4). During the study period, individuals in Cohort 1 (group hotels) were less likely to end their services and exit from the homeless response system (11%) compared to those in enhanced and basic congregate settings (32% and 28%, respectively). Studying exits from shelter is a complicated endeavor. Residential stability (a worthy goal) may conflict with a desire to have people exit the shelter system. Given the unique context of sheltering people during a pandemic, greater residential stability was positive given that an exit from the system might create a greater risk of COVID-19 infection for an individual. Greater stability in Cohort 1 is also consistent with the meaningful upgrade in living conditions (privacy, a real bed, and a private bathroom) compared to congregate settings.
Table 4.
Exits from the homeless response system among the study population, by cohort.
| Study cohort | Number of individuals | Total exited | Exited (%) |
|---|---|---|---|
| Cohort 1: Group hotel | 383 | 43 | 11 |
| Cohort 2: Enhanced congregate shelter | 926 | 295 | 32*** |
| Cohort 3: Congregate shelter with basic services | 326 | 92 | 28*** |
| Total | 1,635 | 430 | 26 |
Note. Data in Table 4 represent exits from the homeless response system between April 1, 2020, and August 31, 2020, as reported in the Seattle/King County Homeless Management Information System as of 9/1/2020.
represent a statistically significant difference between Cohort 1 and Cohort 2, and between Cohort 1 and Cohort 3, at p ≤ .10, p ≤ .05 and p ≤ .01, respectively.
When analyzing exits from shelter, it is important to underscore that not all exits are created equal. An exit back to an unsheltered situation is not a positive outcome. Therefore, for individuals in our study sample who exited the shelter system during the study period, we quantify how many of those exits were positive, meaning an exit to a permanent housing situation (as compared to an unknown location). Table 5 highlights that exits by individuals in Cohort 1 (group hotel) and Cohort 2 (enhanced congregate shelters) were far more likely to be to permanent settings than were those in Cohort 3 (congregate shelter with basic services). We attributed these statistically significant differences to varying levels of service provision and support that may help to facilitate positive exits from the shelter system.
Table 5.
Exits from the homeless response system among the study population, by cohort and exit destination (%).
| Study cohort | Permanent housing | Unknown location | Other location | Unsheltered |
|---|---|---|---|---|
| Cohort 1: Group hotel (N = 43) | 60 | 28 | 12 | 0 |
| Cohort 2: Enhanced congregate shelter (N = 295) | 53 | 29 | 10 | 5*** |
| Cohort 3: Congregate shelter with basic services (N = 92) | 13*** | 82*** | 5 | 0 |
| Total | 45 | 39 | 13 | 3 |
Note. Data in Table 5 represent exits from the homeless response system between April 1, 2020, and August 31, 2020, as reported in the Seattle/King County Homeless Management Information System as of 9/1/2020.
represent a statistically significant difference between Cohort 1 and Cohort 2, and between Cohort 1 and Cohort 3, at p ≤ .10, p ≤ .05 and p ≤ .01, respectively.
Data from the qualitative interviews also underscored the feelings of stability that were associated with staying in the group hotels: “It’s a little bit of stability. It’s something to build on, a foundation that’s not sand or quicksand.” Respondents drew a clear connection between the stability provided by the hotels and broader measures of well-being. One interviewee highlighted the profound contrast between the hotel location and congregate shelter settings: “It has helped to re-establish my self-esteem and dignity … . It feels more like home. I have space to create things, not just exist. I have the capacity to live.” We did not hear any evidence from the interview respondents that there was a desire to return to congregate shelter or unsheltered settings.
Greater Engagement With Staff
Both staff interviews and administrative data highlighted the increased opportunities for high-quality engagement with staff in a hotel setting. According to interviews with residents and staff, more frequent and better interactions with service staff contributed to improvements in service uptake and overall well-being. One resident commented on the greater engagement with staff in hotel settings compared to pre-pandemic congregate shelters: “Oh, yeah, I’d say it was different. It’s different, yep. Yeah, I think they see you more … the communication with them would probably be better and stronger and all that.” When asked why the hotel setting seemed to foster better relationships between staff and residents, one staff person offered this analogy:
When you’re at the airport and your flight’s delayed and you’re there all day, are you your best self? No. Right? Now imagine somebody trying to ask you about the hardest parts of your life and help you plan forward. You would not want to engage with that person. You would not want to be in that conversation. You would be brushing them off or irritable. That is what we’ve asked of folks all these years in these intense congregate settings, right?
Now flip that to, you give [the] person the lounge experience at the airport, right? They got the comfy chair. You gave them some water, right? It’s a better conversation, obviously. I don’t want to go back to the waiting game with the four-hour delay. It is not unusual that we’re seeing more of people, better of people, people opening up. They’re under less stress in that sense.
HMIS data substantiate that engagement with staff was higher among those who moved to group hotels as well as those who resided in enhanced shelters with on-site case management. In King County, completing an assessment through Coordinated Entry for All (CEA) is required to access homeless housing (i.e., rapid rehousing, permanent supportive housing, transitional housing and other permanent housing). Because assessments are voluntary and time intensive, and cover sensitive topics, assessment rates serve as a proxy for of engagement with shelter staff. Because of the burdens associated with the assessment process, rates of assessment are low among those in the shelter system.
Approximately 58% of the study population that we analyzed using administrative data had not previously been assessed at the beginning of the intervention. Table 6 shows that although assessment completion rates after shelter de-intensification for those who were not previously assessed are relatively low across all groups, they are higher for those who moved to group hotels and enhanced shelters (7% and 5%, respectively) compared to individuals who resided in basic shelters (1%). The greater interaction and engagement with staff may help to explain the statistical differences between groups.
Table 6.
Coordinated entry for all assessments among the study population, by cohort.
| Cohort | Number of individuals | Not previously assessed | Not previously assessed (%) | Newly assessed | Newly assessed (%, among not previously assessed) |
|---|---|---|---|---|---|
| Cohort 1 – T1: Group hotel | 383 | 205 | 54 | 14 | 7 |
| Cohort 2 – C1: Enhanced congregate shelter | 926 | 482 | 52 | 24 | 5 |
| Cohort 3 – C2: Congregate shelter with basic services | 326 | 266 | 82*** | 2 | 1*** |
| Total | 1,635 | 953 | 58 | 40 | 4 |
Note. Data in Table 6 represent Coordinated Entry for All assessments completed between April 1, 2020, and August 31, 2020, as reported in the Seattle/King County Homeless Management Information System as of 9/1/2020.
represent a statistically significant difference between Cohort 1 and Cohort 2, and between Cohort 1 and Cohort 3, at p ≤ .10, p ≤ .05 and p ≤ .01, respectively.
Health, Well-Being, and Feelings of Safety
Interviews with both residents and staff highlighted notable improvements in health and well-being for individuals living in group hotel locations. Respondents identified a direct relationship between clean and private rooms with bathroom facilities and improved sleep, hygiene, mental health, and overall well-being. The stability provided by a hotel room—as well as greater engagement with staff—increased the ability of residents to schedule and attend appointments with healthcare professionals. Both residents and staff drew a link between higher levels of healthcare utilization and overall well-being.
Responses from residents provided clear evidence of these benefits. One participant simply stated, “I can think and sleep,” whereas another stated, “You’re at peace. You’re more at peace with yourself … . It just feels good. It feels really good.” Several participants drew connections between lowered stress levels and healthier behavior:
I would drink a lot. Now that I’m here, I don’t drink. You would drink because of the boredom of the day being on the street. That’s one thing that I can say this helps with is I don’t even care to drink no more. Now I can sit and be in here and not have to be around all the wildness. It doesn’t stress me out to where I wanna drink or smoke pot or anything.
The additional time and stability provided by the intervention allowed some participants to pursue hobbies and leisure activities that were not possible when staying in shelter. The activities ranged from the mundane—watching TV in their room—to the adventurous—hiking and fishing. Individuals also noted that they participated in activities that improved their health, such as exercise and meditation. Additional activities highlighted by respondents included reading, listening to music, volunteering, participating in professional and personal development trainings, and following professional sports. For staff and participants, the pursuit of hobby and leisure served as a positive indicator of overall well-being.
Reduced Interpersonal Conflict
A major theme that emerged in qualitative interviews was the dramatic drop in interpersonal conflict in the group hotel settings. As one individual staying in a hotel described, “It’s [conflict] nonexistent here. There’s no conflict here. Yeah, this is nice.” Another resident noted how privacy and space lowered the level of anxiety and the associated conflict dropped:
In the shelter, we were in a big dorm with a lotta—I guess 100 different men. There was a lotta stress. It was also bein’ around the same—with the arguing all the time. In the room, we’re more isolated. We’re more alone. It’s quieter. It’s less stressful.
Another resident summarized the dynamic: “we’re much more tolerant.” Although the hotel stay is temporary, private rooms provide peace: “It’s like I get to go home, and I can lay in a bed and can watch what I want to on TV. I [don’t] have to listen to people screamin’, yellin’, and fightin’ in the bathroom over dope.”
We corroborate the qualitative findings with analyses of administrative data about public safety. In the first analysis, we use data drawn from Seattle Fire Department 911 dispatches. Figure 2 illustrates the drop in 911 dispatch activity to shelters managed by Provider A after de-intensification and the move to a group hotel location. Comparing emergency dispatches over the same months, the number of calls per bed-night in 2020 were about one third of the amount in 2019.
Figure 2.
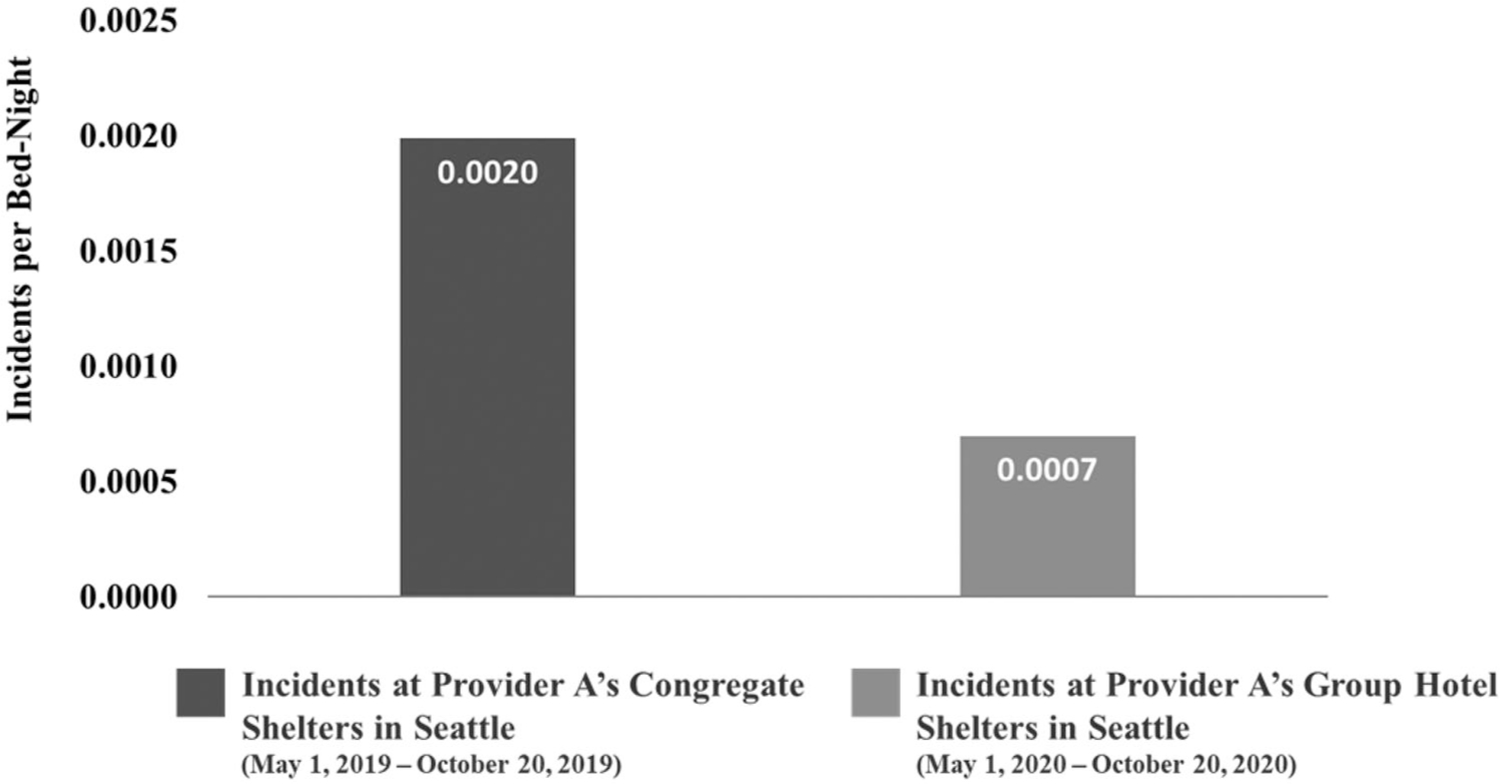
Seattle Fire 911 emergency dispatches to key locations associated with Provider A’s moves to a group hotel shelter.
Note. Data in Figure 2 represent the number of 911 dispatches to Provider A’s congregate shelters in Seattle, Washington, between May 1, 2019, and October 20, 2019, divided by the congregate shelters’ bed-night capacity (on the left) and to the group hotel shelter in Seattle between May 1, 2020, and October 20, 2020, divided by the hotel shelter’s bed-night capacity. Data are from the Seattle Fire Department 911 Emergency Dispatch database as of December 30, 2021. Individuals from two of Provider A’s congregate shelters were moved to the group hotel at the end of April 2020.
To supplement the analysis from the Seattle Police Department, we also analyze police and fire dispatch data from Provider B’s internal database. This large provider follows and logs these data in the ordinary course of their operation of shelter locations. The data from this source are consistent with the trends highlighted in the analysis of Seattle Fire Department data. Individuals from this agency’s main, urban congregate shelter were moved to a suburban group hotel setting at the beginning of April 2020. Figure 3 compares the number of emergency responses from the Seattle police and fire departments initiated from calls at the congregate shelter between May 1, 2019, and October 20, 2019, with the number of responses from the corresponding local police and fire departments initiated from calls at the hotel site in the same time period in 2020 (between May 1, 2020, and October 20, 2020). The results demonstrate that call volumes per bed-night fell by over 75% in 2020 compared to 2019.
Figure 3.

Incidents requiring emergency response to Provider B’s congregate shelter in Seattle, Washington, and group hotel shelter in Renton, WA.
Note. AMR = American Medical Response, a local ambulance provider. Data in Figure 3 represent the number of incidents requiring emergency 911 calls from Provider B’s congregate shelter in Seattle between May 1, 2019, and October 20, 2019, divided by the congregate shelter’s bed-night capacity and from the group hotel in Renton between May 1, 2020, and October 20, 2020, divided by the hotel shelter’s bed-night capacity as reported in Provider B’s internal client records. Seattle Fire Department (SFD) policy requires that all calls to SFD result in a subsequent call to the Seattle Police Department for assistance. These extra calls are not included in the police department totals.
The difference measured here is the number of incidents prompting responses from the corresponding local police and fire departments in the shelter or hotel location. Pre-pandemic, this measures the number of incident responses from the congregate shelter setting in downtown Seattle. This does not measure calls from the vicinity of the shelter, but rather responses to events occurring within this specific location. Following de-intensification, all people from this downtown location were moved to a suburban location. The same service provider continued to track incident responses at the new hotel location in suburban Seattle. The comparison here is between two locations housing a similar population of people in similar circumstances. There was a dramatic fall in incidents per bed-night and responses from police and fire departments in these two locations (one based on the pre-pandemic period and the other occurring during the COVID-19 intervention). Although there may be many explanations for this fall, descriptive data demonstrate a dramatic fall in police/fire response volume between the two settings. Interviews with staff from this shelter provider corroborate the analysis of administrative data. Staff noticed a significant reduction in personal conflict and stress—frequent drivers of calls to police and fire—after the move to the suburban hotel location. The ability of residents to de-escalate situations by retreating to their own room was highlighted by staff members as a key reason for the reduction. This concept was evident in resident responses as well,
I feel safe. I have a door that locks. I have people around me that also have doors that lock, so striking out at your neighbor is not as common as it is when you are struggling over square inches of a concrete floor. There’s a big difference in how humans treat each other in the two situations.
The decline in calls throughout the system highlights a significant potential benefit of the de-intensification strategy. Certainly there are many factors that might help to explain this fall, but these descriptive data combined with qualitative data from interviews suggest a relationship between shelter de-intensification and interpersonal conflict. This association is consistent with intuition: the ability to retreat to one’s own room and lock the door dramatically decreases the risk of conflict as compared to a congregate setting where shelter residents live and sleep in close proximity.
Greater Focus on Future Goals
The final theme relates to the increased future orientation of those who stayed in group hotels. During interviews, participants discussed their desire to secure permanent housing, find a job, or pursue additional education. As one resident describes, “one can retreat into their own space. Like with any home, it gives you shelter. It gives you time to contemplate, to plan, and to execute. These things are important when you’re trying to put your life back together.” Another participant described the link between the group hotel intervention and this focus on the future:
I’m starting to get my dreams back. You get to the point when you’re homeless you don’t even care. You don’t think about even why I’m going to get a place. You’re gonna say, “I’m out here, that’s that.” Now that I’ve been in here, I’m like, “Yeah, I wanna get my own place again.”
Interviewees perceived that the COVID-19 pandemic would likely complicate their ambitions to secure housing and employment because “the work’s just not out there right now.” Participants were also aware of the precarity of the intervention given its connection to the pandemic. One participant lamented that a sudden end to the intervention could result in backward steps, noting, “I’m just hoping that I’m good here for about another two or three months until I can save enough money off my Social Security to get myself an apartment.” Many of the participants hoped to transition “from here to [their] own place,” either through connections with subsidized housing or by saving enough for a private rental.
Features of the Hotel Intervention That Drove Improved Outcomes
The final component of the analysis identified the specific attributes of the group hotel intervention that contributed to the beneficial non-COVID outcomes identified in the prior section. This set of findings decouples the concept of “hotel” from its attributes in order to highlight opportunities for the homeless response system, regardless of hotel use and/or availability. These findings are important because the “hotel” intervention may not be a permanent component of the homelessness response system, but the learning from this intervention may inform future homelessness programming and responses.
Designated Personal Space
Interviewees consistently praised having one’s own bed and bathroom. This finding is intuitive and unsurprising, but it was a dominant theme. One participant clearly articulated the benefit: “It’s nice. It’s nice to have your privacy and a TV and a toilet where you ain’t gotta deal with other people.” A staff member emphasized the contrast between hotel rooms and traditional shelters:
These are literally rooms designed for people to sleep in, and that’s what people are doing in them. Coming with the privacy and the access to your own bathroom that those things are seemingly simple, but knowing the alternative and what we came from, they’re massive.
In addition to these obvious benefits of private living, numerous respondents commented on the independent value of privacy, where one can “get my alone time, get-myself-together time.” Interviewees repeatedly identified personal space as a source of peace and restoration:
One can retreat into their own space. Like with any home, it gives you shelter. It gives you time to contemplate, to plan, and to execute. These things are important when you’re trying to put your life back together.
Personal Safety
The concepts of personal safety and security emerged throughout the interviews. Physical attributes of certain hotel sites contributed to feelings of greater security, such as the presence of a security guard, a perimeter fence, and locks on hotel room doors. Many of the respondents appreciated these security features; as one participant commented, “You don’t have to worry ‘bout somebody steppin’ over you or robbin’ unless they come to your door and knock. If you choose not to open your door, then you’re all right.” Another stated, “Safety is no issue here. It’s a hell of a lot safer here than it is at the shelter.”
Secure Storage for Personal Belongings
Hotel rooms provided individuals experiencing homelessness with a place to store their belongings. In contrast, participants in shelters have to leave their belongings unattended during routine trips to the bathroom, which provokes fears about theft. Even while sleeping in a congregate shelter, participants expressed frustration regarding how concerns about the potential loss of personal belongings can disrupt or prevent quality sleep. Beyond securing personal items, one participant highlighted broader benefits of safe, longer-term storage in the hotel:
It’s been really nice to keep my stuff there and be able to leave and come back, and it’s all still there. I don’t have to pack it around, which has been really nice to feel normal again … . When you drag a backpack and luggage around and stuff, people tend to judge you right off the bat, homeless or whatever. When you don’t have to carry that stuff around, people, they don’t judge you as being homeless or whatever. They look at you differently. It’s been nice to not be judged like that.
Unrestricted Access
In contrast to many traditional congregate shelters, which have strict time constraints, the group hotels allowed participants access to and from their rooms on their own schedules. This unlimited access gave individuals more free time and greater control over their lives. Repeatedly, the notion of autonomy emerged in interviews with the individuals staying in hotels:
I get to move at my own speed now. Do things the way I need to do ‘em versus when you’re on the street, and you gotta worry about being back to get into the night shelter. Now you can do things at your own pace.
Predictable Access to Food
Each of the group hotels provided three meals a day for individuals staying in their rooms. Many hotel participants contrasted this experience with prior struggles to procure adequate food on a daily basis. For these individuals, regular food provision was noteworthy: “When we wake up in the morning, we eat. We have breakfast, ready meals, so we eat.” Multiple respondents also emphasized that removing the need to “try to hustle up [food] every day” reduced the level of stress in life and freed up time for other endeavors.
Discussion and Conclusion
The COVID-19 pandemic initiated a broad transformation of emergency shelter systems (National Alliance to End Homelessness, 2021; Wu & Karabanow, 2020). This study examined one such intervention in King County, Washington, that moved individuals from traditional congregate shelters to group hotels shortly after the local onset of the pandemic. The study findings indicate that the intervention was successful in reducing the risk of contracting COVID-19 for those in the group hotel settings. Furthermore, the results highlight myriad nonpandemic-related benefits for participants in group hotels. Finally, the study specifies the attributes of the hotel intervention that contributed to the positive participant experiences.
The study, as described earlier, is limited in its scope and does not address the cost effectiveness of the intervention. Understanding the long-term costs and benefits of this type of intervention is critical and is an essential area of emphasis for future research. Comments from public officials in King County have acknowledged that the group hotel intervention is a more expensive option than traditional congregate shelter and, as a result, cost will be an important factor as they consider ongoing changes to the emergency shelter system (Kroman, 2021).
Although the pandemic created this intervention opportunity, this unique context may also limit the generalizability of some of the findings outside of a pandemic context. For example, interviewees had little to say about the impact of moving neighborhoods or, in some cases, from an urban core to a suburban city. This likely relates to the complete disruption of typical activities and settings. Some of the public spaces commonly used by those experiencing homelessness, such as public libraries, were closed to the public during the entire study period. Drop-in social services and non-COVID medical services abruptly restricted access. The impact of changing geographies may be more salient in a nonpandemic context.
It is also important to note that there were other hotel interventions happening concurrently in the Seattle region during the pandemic; this study focuses on one such program. A related initiative moved people off of the streets and out of encampments and placed them in hotel rooms. The program, called JustCARE, produced positive results, but the evaluators highlighted that its success stemmed from a “multifaceted and integrated approach that distinguishes itself from other approaches” (Beckett et al., 2021, p. 3). These approaches included a response that addressed housing needs, mental and physical health, substance use, and criminal legal system involvement. These various supports demonstrate that all hotel interventions are not created equal, and the level of services must scale to meet the depth of needs of the population the program serves.
In King County, the positive impacts associated with this intervention have prompted county leadership to acquire hotels to permanently house people experiencing homelessness (as opposed to using hotels as emergency shelter). By the end of 2021, through its Health Through Housing Initiative, the county had acquired eight hotels for an aggregate purchase price in excess of $200 million. The justification for these purchases was the success of the hotel interventions during COVID-19 and the relative cost-effectiveness and timeliness of hotel purchases compared to new construction. The county expects to provide over 1,600 units to people experiencing homelessness via hotel purchases by the end of 2022. According to county data, the acquisition price per unit is roughly $270,000, compared to the cost of new development which is much higher (King County, Washington, 2022). Not surprisingly, these efforts have been met with some community resistance. Local cities have requested greater input before a hotel is converted to provide housing for the homeless, and certain cities have opted out of the funding mechanism that has been used to fund hotel acquisition and have chosen to redirect their funds to other housing-related activities. But despite this opposition, the county has dramatically increased its stock of housing units for the homeless through its hotel acquisition strategy.
Although the motivation for and context of this hotel intervention were novel, study findings are consistent with broader concepts of a sense of place and the benefits of a safe, stable environment. As noted in the literature review, there are strong connections between health and housing (Bonnefoy, 2007; Braubach, 2011; Jacobs et al., 2009; Sharpe et al., 2018) and those relationships were affirmed in this study. Prior research also indicates the efficacy of interventions that offer dignity and autonomy to those experiencing homelessness, such as through a Housing First approach (i.e., providing permanent housing without requiring treatment or other program participation). Although an entirely different intervention—Housing First is permanent housing, whereas the hotel intervention is not—the results of the study reinforce the link between interventions that provide autonomy for basic human functions (e.g., when to sleep, unlimited access to a private bathroom) and improved physical, mental, and emotional health.
The results of this study can provide policymakers with evidence to help inform future homeless response decision-making. For example, the beneficial attributes of hotels (privacy, storage, safety and security, and meals) need not be limited only to hotel settings. These attributes could, in part, be provided in congregate settings. In addition, we identified positive aspects of enhanced, de-intensified shelter locations that could also serve as a roadmap for communities that are unable or unwilling to convert to a more expensive hotel strategy.
The singularity of the pandemic emerged as a theme in both staff interviews and ad hoc discussions with government and provider staff. The pandemic provided a unique opportunity to implement substantial changes in the way that shelter services are delivered in a very different physical setting. It was an experiment that service providers had long hoped for, but the opportunity to carry it out never presented itself—until the arrival of COVID-19. Therefore, in the midst of the tragedy and hardship of a global pandemic, new and promising avenues emerged in society’s response to homelessness. The rapid response also highlighted the efficient and effective collaboration between governmental agencies and the nonprofit sector, which was essential to the success of this intervention.
In sum, the findings we observe in this isolated case are consistent with other recently released research on similar interventions that have occurred elsewhere in the United States (Hsu et al., 2021; O’Shea et al., 2021; Padgett et al., 2022). This evaluation, and many others, will provide, in part, the empirical support for potential changes in the structure of the emergency response to homelessness (Beckett et al., 2021; National Alliance to End Homelessness, 2021). In King County, Washington, the County Executive, Dow Constantine, referenced this study when announcing the county’s permanent commitment toward the use of hotels as a temporary or permanent alternative to congregate shelters (King County, Washington, 2021). The use of hotels, initially as an alternative to congregate shelter, and the subsequent acquisition of hotels to be used as permanent housing also occurred in California, with the state’s Project Roomkey (shelter) and subsequent Project Homekey (permanent housing) (National Alliance to End Homelessness, 2021). Whether hotels continue to be used as alternatives to congregate shelter in a post-pandemic world remains to be seen, but growing evidence suggests that this unique moment has altered—in permanent ways—how communities can and will respond to the crisis of homelessness (Aitken, 2021).
Acknowledgments
This work was supported by a University of Washington Population Health Initiative COVID-19 Economic Recovery Research Grant, the Bill & Melinda Gates Foundation, and Urban@UW.
Footnotes
A CoC covers a specific geography and manages and coordinates housing and services for individuals and families experiencing homelessness.
A true counterfactual would be those who remained in standard, congregate shelter settings. Due to public health directives, the pre-pandemic congregate settings no longer existed for comparative purposes.
In the initial public health response period from March to July 2020, testing for COVID-19 was targeted to facilities in response to either a confirmed COVID-19 case or COVID-like illness based on symptoms. The goals around this testing strategy were to rapidly detect COVID-19 cases, isolate those who needed it, and support people and facilities to help contain outbreaks. In the time since this period, Public Health has had a proactive testing strategy for surveillance and prevention purposes in settings where no known cases of COVID-19 or COVID-like illness are present.
Disclosure Statement
No potential conflict of interest was reported by the authors.
References
- Aitken E (2021). Covid-19: Opportunity to improve crisis responses to homelessness? The Journal of the Royal College of Physicians of Edinburgh, 51(S1), S53–S62. 10.4997/JRCPE.2021.242 [DOI] [PubMed] [Google Scholar]
- Baggett TP, Keyes H, Sporn N, & Gaeta JM (2020). Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. Jama, 323(21), 2191–2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrow SM, Herman DB, Cordova P, & Struening EL (1999). Mortality among homeless shelter residents in New York City. American Journal of Public Health, 89(4), 529–534. 10.2105/ajph.89.4.529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir SA (2002). Home is where the harm is: Inadequate housing as a public health crisis. American Journal of Public Health, 92(5), 733–738. 10.2105/ajph.92.5.733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckett K, Brydolf-Horwitz M, Collins D, Goldberg A, Knaphus-Soran E, & Turner A (2021). The development and impact of a multi-faceted collective impact model. University of Washington https://coleadteam.org/wp-content/uploads/2021/07/JustCARE_Report-ExecutiveSummary_7.12.21.pdf
- Bentley R, Baker E, & Mason K (2012). Cumulative exposure to poor housing affordability and its association with mental health in men and women. Journal of Epidemiology and Community Health, 66(9), 761–766. [DOI] [PubMed] [Google Scholar]
- Bhattacharyya S (2016). Homeless Hotels in New York: Who Benefits from the Industry’s Side Business. Craig Newmark Graduate School of Journalism, City University of New York https://academicworks.cuny.edu/cgi/viewcontent.cgi?article=1150&context=gj_etds
- Bonnefoy X (2007). Inadequate housing and health: An overview. International Journal of Environment and Pollution, 30(3/4), 411–429. 10.1504/IJEP.2007.014819 [DOI] [Google Scholar]
- Braubach M (2011). Key challenges of housing and health from WHO perspective. International Journal of Public Health, 56(6), 579–580. 10.1007/s00038-011-0296-y [DOI] [PubMed] [Google Scholar]
- Braun V, & Clarke V (2012). Thematic analysis. In Cooper H, Camic PM, Long DL, Panter AT, Rindskopf D, & Sher KJ (Eds.), APA handbook of research methods in psychology, Vol. 2. Research designs: Quantitative, qualitative, neuropsychological, and biological (pp. 57–71). American Psychological Association. [Google Scholar]
- Daiski I (2007). Perspectives of homeless people on their health and health needs priorities. Journal of Advanced Nursing, 58(3), 273–281. 10.1111/j.1365-2648.2007.04234.x [DOI] [PubMed] [Google Scholar]
- Doughtery C (2021, April 17). One way to get people off the streets: Buy hotels. The New York Times
- Fazel S, Geddes JR, & Kushel M (2014). The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. The Lancet, 384(9953), 1529–1540. 10.1016/S0140-6736(14)61132-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick-Lewis D, Ganann R, Krishnaratne S, Ciliska D, Kouyoumdjian F, & Hwang SW (2011). Effectiveness of interventions to improve the health and housing status of homeless people: A rapid systematic review. BMC Public Health, 11(1), 1–14. 10.1186/1471-2458-11-638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu YT, Lan FY, Wei CF, Suharlim C, Lowery N, Ramirez A, Panerio-Langer J, Kawachi I, & Yang J (2021). Comparison of COVID-19 mitigation and decompression strategies among homeless shelters: A prospective cohort study. Annals of Epidemiology, 64, 96–101. 10.1016/j.annepidem.2021.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs DE, Wilson J, Dixon SL, Smith J, & Evens A (2009). The relationship of housing and population health: A 30-year retrospective analysis. Environmental Health Perspectives, 117(4), 597–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karb R, Samuels E, Vanjani R, Trimbur C, & Napoli A (2020). Homeless shelter characteristics and prevalence of SARS-CoV-2. Western Journal of Emergency Medicine, 21(5), 1048–1053. 10.5811/westjem.2020.7.48725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasinitz P (1986). Gentrification and homelessness: The single room occupant and the Inner City Revival. In Erickson J & Wilhelm C (Eds.), Housing the homeless (pp. 241–252). Center for Urban Policy Research. [Google Scholar]
- King County, Washington. (2021). Executive Constantine’s state of the county: “We are making transformational changes for our shared future” https://kingcounty.gov/elected/executive/constantine/news/release/2021/May/11-state-of-the-county.aspx [Google Scholar]
- King County, Washington. (2022). Health through housing: A regional approach to address chronic homelessness https://kingcounty.gov/depts/community-human-services/initiatives/health-through-housing.aspx [Google Scholar]
- Kroman D (2021). Can King County keep using empty hotels to fight homelessness? Crosscut Retrieved February 18, 2021 from https://crosscut.com/news/2021/02/can-king-county-keep-using-empty-hotels-fight-homelessness
- Kushel MB, Vittinghoff E, & Haas JS (2001). Factors associated with the health care utilization of homeless persons. JAMA, 285(2), 200–206. [DOI] [PubMed] [Google Scholar]
- Levitt AJ, Culhane DP, DeGenova J, O’Quinn P, & Bainbridge J (2009). Health and social characteristics of homeless adults in Manhattan who were chronically or not chronically unsheltered. Psychiatric Services, 60(7), 978–981. 10.1176/ps.2009.60.7.978 [DOI] [PubMed] [Google Scholar]
- Libman K, Fields D, & Saegert S (2012). Housing and health: A social ecological perspective on the us foreclosure crisis. Housing, Theory and Society, 29(1), 1–24. 10.1080/14036096.2012.624881 [DOI] [Google Scholar]
- Marsh A, Gordon D, Heslop P, & Pantazis C (2000). Housing deprivation and health: A longitudinal analysis. Housing Studies, 15(3), 411–428. 10.1080/02673030050009258 [DOI] [Google Scholar]
- National Alliance to End Homelessness. (2021, July 20). Hotels to housing case studies. NAEH
- National Alliance to End Homelessness. (2021). Homekey: California’s statewide hotels-to-housing initiative https://endhomelessness.org/wp-content/uploads/2021/07/CA-H2H-Case-Study_7-19-21.pdf
- O’Shea T, Bodkin C, Mokashi V, Beal K, Wiwcharuk J, Lennox R, Guenter D, Smieja M, Bulir D, & Chong S (2021). Pandemic planning in homeless shelters: A pilot study of a Coronavirus Disease 2019 (COVID-19) testing and support program to mitigate the risk of COVID-19 outbreaks in congregate settings. Clinical Infectious Diseases, 72(9), 1639–1641. 10.1093/cid/ciaa743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padgett DK, Bond L, & Wusinich C (2022). From the streets to a hotel: A qualitative study of the experiences of homeless persons in the pandemic era. Journal of Social Distress and Homelessness, 2022, 1–7. 10.1080/10530789.2021.2021362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson D (2020). Fuzzyjoin: Join tables together on inexact matching https://cats.informa.com/PTS/proof/launchProofTool.do?proofId=3702793&nopopup=true&manuscriptId=2075027&t=MANUSCRIPT
- Rogers JH, Link AC, McCulloch D, Brandstetter E, Newman KL, Jackson ML, Hughes JP, Englund JA, Boeckh M, Sugg N, Ilcisin M, Sibley TR, Fay K, Lee J, Han P, Truong M, Richardson M, Nickerson DA, Starita LM, Bedford T, & Chu HY (2021). Characteristics of COVID-19 in homeless Shelters: A community-based surveillance study. Annals of Internal Medicine, 174(1), 42–49. 10.7326/M20-3799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncarati JS, Baggett TP, O’Connell JJ, Hwang SW, Cook EF, Krieger N, & Sorensen G (2018). Mortality among unsheltered homeless adults in Boston, Massachusetts, 2000–2009. JAMA Internal Medicine, 178(9), 1242–1248. 10.1001/jamainternmed.2018.2924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpe RA, Taylor T, Fleming LE, Morrissey K, Morris G, & Wigglesworth R (2018). Making the case for “whole system” approaches: Integrating public health and housing. International Journal of Environmental Research and Public Health, 15(11), 2345–2313. 10.3390/ijerph15112345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shenassa ED, Daskalakis C, Liebhaber A, Braubach M, & Brown MJ (2007). Dampness and mold in the home and depression: An examination of mold-related illness and perceived control of one’s home as possible depression pathways. American Journal of Public Health, 97(10), 1893–1899. 10.2105/AJPH.2006.093773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan BJ, & Burke J (2014). Single-room occupancy housing in New York City: The origins and dimensions of a crisis. CUNY Law Review, 113, 113–143. [Google Scholar]
- Thomson H, Thomas S, Sellstrom E, & Petticrew M (2009). The health impacts of housing improvement: A systematic review of intervention studies from 1887 to 2007. American Journal of Public Health, 99(S3), S681–S692. 10.2105/AJPH.2008.143909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Housing and Urban Development. (2016). Flowchart of HUD’s definition of chronic homelessness https://files.hudexchange.info/resources/documents/Flowchart-of-HUDs-Definition-of-Chronic-Homelessness.pdf
- Wu H, & Karabanow J (2020). COVID-19 and beyond: Social work interventions for supporting homeless populations. International Social Work, 63(6), 790–794. 10.1177/0020872820949625 [DOI] [Google Scholar]


