Abstract
Aims:
To assess differences in catastrophizing and kinesiophobia in relation to areas of pain and somatic symptoms among participants with temporomandibular disorders (TMDs) and controls.
Methods:
In total, 401 participants (333 women, 68 men, mean age: 45.8 years) in the TMJ Impact Project were examined in accordance with the Diagnostic Criteria for TMD, including clinical examination (Axis I) and psychosocial assessment (Axis II) augmented with imaging of the temporomandibular joint (TMJ). Of these, 218 participants had a painful TMD pain diagnosis, 63 had a nonpainful TMD diagnosis, and 111 had no TMD. Nine participants had missing data. Participants completed the Pain Catastrophizing Scale, Tampa Scale for Kinesiophobia, Areas of Pain figure, and the Patient Health Questionnaire-15 for assessing somatic symptoms.
Results:
Compared to controls, participants with TMD pain showed higher levels of catastrophizing (P = .017), kinesiophobia (P < .001), areas of pain (P < .001), and somatic symptoms (P < .001). Participants with nonpainful TMD showed a higher level of kinesiophobia (P < .001) than controls. There was a positive correlation between catastrophizing and kinesiophobia for participants with TMD pain (r = 0.33, P < .001) and nonpainful TMD (r = 0.42, P < .001).
Discussion:
The results suggest more fear of movement, as well as an association between catastrophizing and fear of movement, in participants with TMD pain and in participants with nonpainful TMD compared to controls. Assessment and management of fear of movement as well as catastrophizing may be useful as part of individualized treatment strategies for patients with TMD. J Oral Facial Pain Headache 2022;36:59–66. doi: 10.11607/ofph.3060
Keywords: catastrophization, facial pain, kinesiophobia, somatic symptoms, temporomandibular joint disorders
“Temporomandibular disorders” (TMD) is an umbrella term for pain and dysfunction involving the masticatory muscles, the temporomandibular joint (TMJ), and associated structures.1 TMDs are the most common cause of chronic pain in the orofacial region,2 with a prevalence of 10% to 15% in the adult population, and is twice as common in women as in men.3–5 TMD affects quality of life in the individual and incurs substantial economic burden on society.2 Various biopsychosocial factors have been shown to be associated with both the development and chronification of TMD, and the Diagnostic Criteria for TMD (DC/TMD) assessment protocol is advocated as part of a comprehensive approach in the assessment of patients with TMD.6
The multifactorial etiology of TMD includes a range of psychosocial factors. One such factor is catastrophizing, an exaggerated cognitive response to an actual or anticipated painful event that can affect the overall painful experience.7 It has been suggested that catastrophizing affects the prognostics of chronification of pain,8 predominantly occurs in patients who suffer from chronic pain, and is also related to inadequate pain relief.9 Negative thoughts about pain may incur a catastrophizing response in which the patient imagines the worst possible outcome, which in turn may lead to fear and avoidance, which strengthens the original negative outlook. This vicious cycle that can reinforce negative thinking and predispose to fear of movement is described in the fear-avoidance model.10
Fear of movement, or “kinesiophobia,” refers to an irrational and restrictive fear of movement as a result of vulnerability related to painful events in the past.10 Individuals who suffer from kinesiophobia have developed a particular anxiousness and concern toward reliving painful experiences and thereby avoid everything that might provoke it. Kinesiophobia has been highlighted as an important component in chronic pain11,12 and is potentially of significant clinical value also in the evaluation and treatment of patients with TMDs.13 In fact, kinesiophobia together with catastrophizing and pain intensity have been suggested to be the main predictors for pain-related disability.14,15 In patients with TMD, this relationship between pain catastrophizing and kinesiophobia may affect an individual’s ability to carry out daily tasks such as eating, chewing, and verbally communicating.
Levels of pain catastrophizing have also been shown to be related to pain comorbidity, with higher levels of catastrophizing in individuals with pain in multiple regions.16 Pain comorbidity is often assessed by using the number of painful body sites as a measure of the general spread of pain and as an indication of possible central sensitization. In addition to pain comorbidity, which is often reported by patients with chronic pain conditions, comorbidity with somatic symptoms is also common.17,18 Such somatic symptoms include not only pain in other body regions, but also nonpainful symptoms—for example, shortness of breath and dizziness. Somatic symptoms, even if not painful, may still cause distress and affect daily activities, and they have been proposed to be related to the development of chronic pain conditions.19
The aim of the present study was to investigate the possible interplay between psychologic factors and pain comorbidity by assessing differences in catastrophizing and kinesiophobia in relation to areas of pain and somatic symptoms among participants with TMDs and controls.
Materials and Methods
Study Setting and Study Population
The TMJ Impact Project20 is a follow-up study of a cohort of 724 subjects enrolled 8 years previously in the Validation Project.6 Both projects were conducted at the University of Minnesota, University of Washington, and University at Buffalo. The Validation Project included participants with the full spectrum of TMD symptoms recruited through advertisements or referral, with a final sample size of 614 participants with TMD and 91 controls aged 18 to 70 years. For the TMJ Impact Project, 620 participants had the potential to be recalled, but, due to financial restrictions, only 401 could be examined. Criteria for inclusion were participation in the Validation Project, previous consent to be recalled for the follow-up study, and no contraindication for imaging. In total, 333 women and 68 men (mean age: 45.8 years) were evaluated 5.8 to 10 years (mean: 7.9 years) after participating in the Validation Project. The included participants were considered representative of the original study cohort based on comparisons of the initial examinations of the participants (n = 401) with those who were not recalled (n = 323).20 Ethical approval was obtained from the Institutional Review Board at each of the three study sites, and all participants provided informed consent.
Clinical and Radiologic Examinations
Participants were examined clinically by a calibrated examiner, and any pain-related TMD diagnoses were algorithmically derived in accordance with the Axis I DC/TMD protocol.6 In addition, TMJ imaging was carried out to establish the presence or absence of TMJ intra-articular disorders, as assessed by three calibrated radiologists according to a consensus protocol. Normal/indeterminant disc position, disc displacement with reduction (DDwR), and disc displacement without reduction (DDw/oR) were established with MRI, and normal/indeterminant hard tissue and degenerative joint disease (DJD) were established with CBCT. Details of the procedures for the radiologic assessment have been described previously.20
Based on the clinical and radiologic examinations, the participants were allocated into three groups: (1) TMD pain (myalgia and/or arthralgia); (2) nonpainful TMD (TMJ intra-articular diagnosis but no pain diagnoses), and controls (without any TMD).
Questionnaires
In addition to the clinical and radiologic examinations described above, inclusion in the present secondary data analysis required data from the questionnaires described below.
The Pain Catastrophizing Scale (PCS) is a reliable and valid instrument consisting of 13 statements about thoughts or feelings associated with pain. Each statement is ranked on an ordinal scale (0–4), where 0 means “not at all” and 4 “all the time.”21,22 An additional item, “I feel my life isn’t worth living,” was included in the present study, making a total of 14 items and resulting in a total score of 0–56 points.23
The Tampa Scale for Kinesiophobia (TSK-TMD) is a reliable and valid instrument initially designed to evaluate the degree of fear of movement in chronic back pain conditions.10 It has been adapted for TMD13 and consists of 18 questions that concern fear of injury and relapse related to jaw movement, with a maximum of 4 points per question and a total of 18 to 72 points.
The areas of pain (AOP) figure, as used in Rhon et al, illustrates 11 body areas where participants mark the areas where pain is present, resulting in a score between 0 (no pain) and 11 (pain in all areas).24
The Patient Health Questionnaire-15 Somatic Symptom Severity Scale (PHQ-15) is a reliable and valid instrument consisting of 15 questions regarding somatic symptoms or symptom clusters that comprise 90% of the most common physical complaints, with three possible answers: “not bothered at all,” which equals 0 points; “bothered a little,” which equals 1 point; or “bothered a lot,” which equals 2 points, resulting in a total of 0 to 30 points.25
Statistical Analyses
Descriptive statistics were used to characterize the study population. Kruskal-Wallis and Mann-Whitney U tests were used for comparisons among the three groups (painful TMD, nonpainful TMD, and controls), together with chi-square (χ2) test for evaluating differences in sex distribution among the groups. Associations between catastrophizing (PCS), kinesiophobia (TSK-TMD), areas of pain (AOP figure), and physical symptoms (PHQ-15) were evaluated with Spearman correlation, with the following cut-offs: 0.00–0.19 = very weak; 0.20–0.39 = weak; 0.40–0.59 = moderate; 0.60–0.79 = strong; and 0.80–1.0 = very strong.26 Statistical analyses were conducted in SPSS statistics for Windows version 24.0 (IBM) and Prism version 9.0.0 (GraphPad). P < .05 was regarded as statistically significant.
Results
Based on the clinical and radiologic assessments, 218 participants had painful TMD (pain-related TMD diagnosis), 63 had nonpainful TMD (TMD intra-articular disorder without pain), and 111 were non-TMD controls. Data were missing for 9 participants. Demographic data are provided in Table 1.
Table 1.
Demographic Data of the Final Study Sample (n = 392)
| TMD pain (n = 218) |
Nonpainful TMD (n = 63) |
Controls (n = 111) |
P value | |
|---|---|---|---|---|
| Mean (SD) age, y | 46.7 (12.9) | 44.6 (12.3) | 44.9 (12.9) | .287 |
| Women, n (%) | 195 (89.4) | 54 (85.7) | 75 (67.6) | < .001 |
| Men, n (%) | 23 (10.6) | 9 (14.3) | 32 (32.4) |
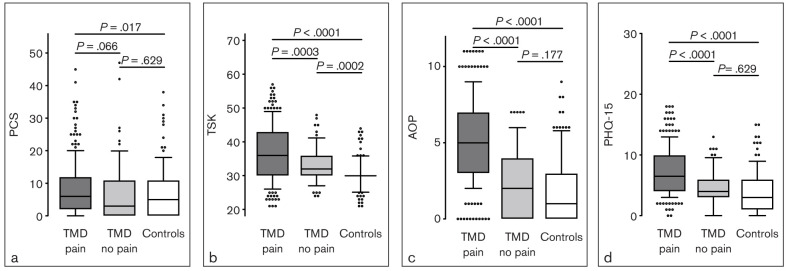
Compared to participants with nonpainful TMD, participants with TMD pain showed more kinesiophobia (P < .001), areas of pain (P < .001), and somatic symptoms (P < .001), but no significant difference in catastrophizing. Compared to controls, participants with TMD pain showed more catastrophizing (P = .017), kinesiophobia (P < .001), areas of pain (P < .001), and somatic symptoms (P < .001). Participants with nonpainful TMD showed a higher level of kinesiophobia (P < .001) than controls, but no difference for the other three variables (Fig 1).
Fig 1.
Comparison of (a) levels of catastrophizing (Pain Catastrophizing Scale [PCS]), (b) fear of movement (Tampa Scale for Kinesiophobia [TSK]), (c) number of painful body areas (areas of pain [AOP]), and (d) physical symptoms (Patient Health Questionnaire 15 [PHQ-15]) mean scores for the three groups: TMD pain (n = 218), nonpainful TMD (n = 63), and control (n = 111).
Participants with TMD Pain
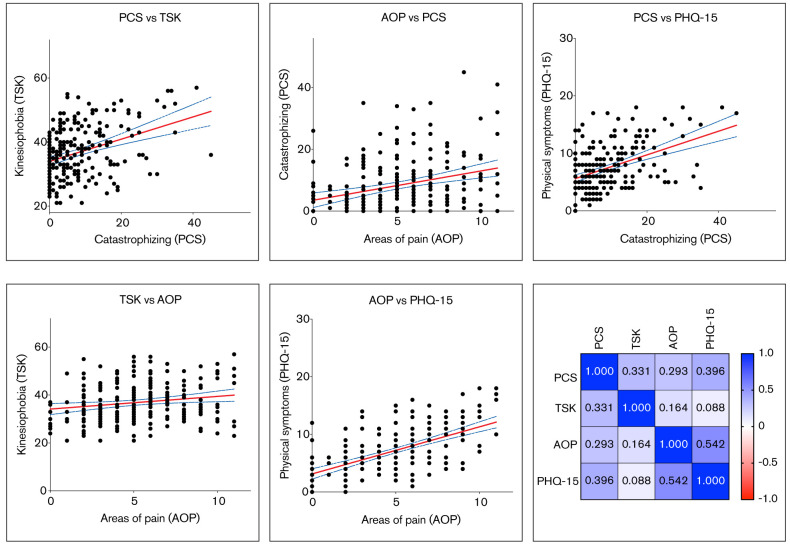
In TMD pain participants, there were statistically significant weak to moderate correlations between catastrophizing and kinesiophobia, areas of pain, and physical symptoms (r = 0.29–0.40, all P < .001). There was also a significant but very weak correlation between kinesiophobia and areas of pain (r = 0.16, P = .015), together with a significant moderate correlation between areas of pain and physical symptoms (r = 0.54, P < .001). There was no significant correlation (r = 0.09, P = .195) between kinesiophobia and physical symptoms (Fig 2).
Fig 2.
Correlations among catastrophizing, kinesiophobia, number of painful body areas, and physical symptoms for the TMD pain group (n = 218) displayed as scatter plots for significant correlations, together with a heat map for all variables.
Participants with Nonpainful TMD
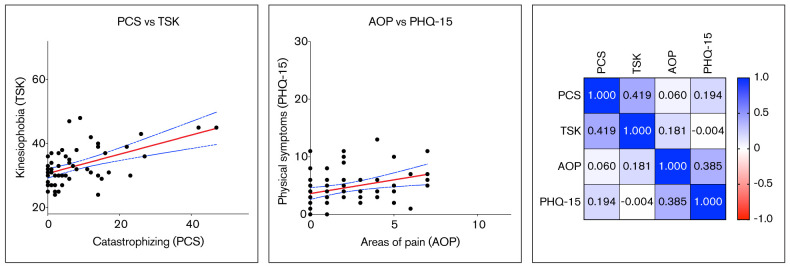
There was a significant moderate correlation (r = 0.42, P < .001) between catastrophizing and kinesiophobia, together with a significant but weak correlation between areas of pain and physical symptoms (r = 0.39, P = .002), in participants with nonpainful TMD. There were no other significant correlations (r = 0.00–0.19, all P > 0.1; Fig 3).
Fig 3.
Correlations among kinesiophobia, number of painful body areas, and physical symptoms for the nonpainful TMD pain group (n = 63) displayed as scatter plots for significant correlations, together with a heat map for all variables.
Controls
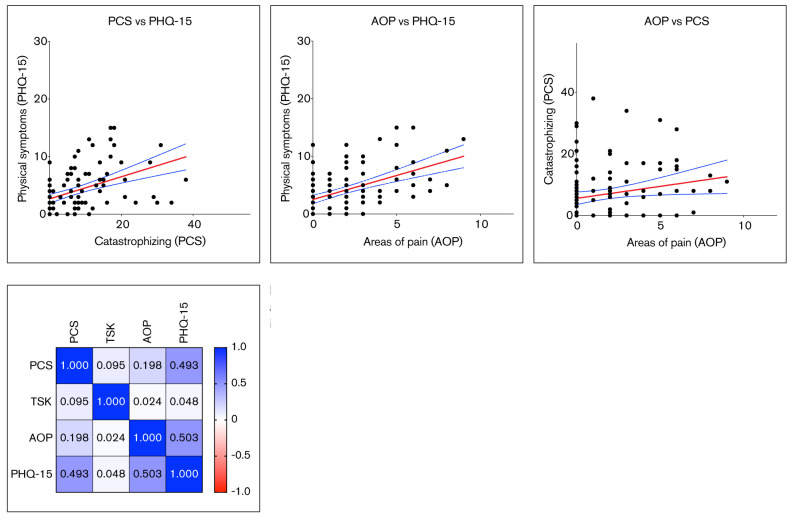
There was a significant but very weak correlation (r = 0.20, P = .037) between catastrophizing and areas of pain in control participants. There were significant moderate correlations between catastrophizing and physical symptoms (r = 0.49, P < .001) and between areas of pain and physical symptoms (r = 0.50, P < .001). There were no other significant correlations (r = 0.02 – 0.09, all P > 0.1; Fig 4).
Fig 4.
Correlations among catastrophizing, kinesiophobia, number of painful body areas, and physical symptoms for the control group (n = 111) displayed as scatter plots for significant correlations, together with a heat map for all variables.
Discussion
To the authors’ knowledge, this is the first study to assess pain catastrophizing and kinesiophobia in relation to somatic symptoms and areas of pain in participants with TMD. Higher levels of kinesiophobia were found in the painful TMD compared to the nonpainful TMD group, and both of the TMD groups reported higher levels compared to controls. Participants with painful TMD also reported higher levels of catastrophizing compared to controls, as well as more pain comorbidities and somatic symptoms compared to both controls and to participants with nonpainful TMD. The findings that even participants with nonpainful TMD (ie, a TMJ intra-articular diagnosis without any pain-related diagnoses) had higher levels of kinesiophobia compared to controls, together with the finding that the correlation between catastrophizing and kinesiophobia was weak for the TMD pain group and moderate for the nonpainful TMD group, suggest an association between catastrophizing and fear of movement in participants with TMD regardless of presence of pain.
The higher proportion of women in the painful TMD and nonpainful TMD groups reflects recruitment in the baseline Validation Project population, and also the fact that women are overrepresented in TMD conditions in the general population.3–6 The baseline population was recruited in line with the STARD (Standards for Reporting Diagnostic Accuracy) guidelines.27 Based on a recent meta-analysis of 220 primary studies, it was concluded that catastrophizing was mainly related to the type of pain condition, with higher levels in generalized pain, but was not related to age or gender.16 This suggests that the difference in catastrophizing between the TMD pain and control groups in the present study can be attributed to the presence of TMD pain and pain morbidities, and not to gender differences between the groups. Differences in levels of catastrophizing between TMD pain patients and participants without TMD were confirmed in a recent systematic review based on a meta-analysis of nine studies that included both TMD groups and controls.28 In common with catastrophizing, kinesiophobia has been proposed to be more strongly related to the type of pain condition than to gender.29 In fact, fear of movement is slightly more common in men compared to women, meaning that the finding in the present study of higher levels of kinesiophobia in the TMD groups is, if anything, an underestimation.
The finding that participants with TMD pain also reported more pain comorbidities, as assessed by areas of pain and somatic symptoms, compared to participants with nonpainful TMD and controls is in line with previous studies.18,30 For both of these variables, the possible effect from gender differences should be considered with regard to comparisons between the control group and both of the TMD groups, as both the painful TMD group and the nonpainful TMD group had a higher proportion of women. Apart from back pain, it has been established in a range of studies that women are overrepresented not only in orofacial pain but in chronic pain conditions in general,31 and also that women generally report more widespread pain32 as well as somatic symptoms.17,25 This proposed relationship between chronic pain conditions and general somatic symptoms is in accordance with the results of the present study. It should however be emphasized that the positive correlation between areas of pain and somatic symptoms, present in both TMD groups as well as in the control group, is not surprising given that the instrument used for assessing somatic symptoms, the PHQ-15, includes six pain-related items and will therefore be correlated to some degree to the number of areas of pain.
The levels of catastrophizing reported by the controls in the present study were in accordance with previous reports, whereas levels reported by the TMD pain group are relatively low compared to many other studies in TMD populations.28 This may be related to the fact that the baseline population in the Validation Project was recruited both by referral and by advertising6 and is thus not directly comparable with TMD samples from orofacial pain clinics. In fact, the study sample in the present sample is more comparable to a recent study with a community-based sample.33 Such differences between community and specialist clinic samples are in congruence with the association between levels of catastrophizing and severity of TMD28 and with catastrophizing as a strong predictor for seeking of care.34
Both TMD groups in the present study reported higher levels of kinesiophobia compared to controls. The levels of kinesiophobia are comparable to a recent study using the 18-item version of the TSK-TMD35; that study, however, did not have a control group without TMD. Although the painful TMD group in the present study had significantly higher levels compared to the nonpainful TMD group, a positive correlation between catastrophizing and kinesiophobia was seen for both TMD groups; it is noteworthy that the correlation between catastrophizing and kinesiophobia was weak for the former and moderate for the latter. These findings suggest an association between catastrophizing and fear of movement in individuals with TMD regardless of the presence of pain.
The relationship between catastrophizing and fear of movement in the TMD pain group is in agreement with previous studies13 and with the fear-avoidance model.10 The positive correlation between catastrophizing and kinesiophobia in the nonpainful TMD group is in accordance with the results from Visscher et al, which were based on multiple regression analysis and factor analysis.13 Thus, it is not always the painful component in TMD that evokes fear of movement; other symptoms, such as nonpainful sounds from the TMJ, acute jaw dislocation (luxation), or catching/locking of the jaw may initiate or increase kinesiophobia. It may be that patients avoid such movements because they are perceived as worrisome even if they are nonpainful, or that loud noises or catching/locking of the jaw are embarrassing in a social context.13 Taken together, these results suggest that TMJ sounds such as clicking and crepitus, together with catching of the jaw, may contribute to higher levels of kinesiophobia, especially so in individuals with higher levels of catastrophizing.
It was only possible to include cross-sectional data from the follow-up examinations in the present study, as the baseline Validation Project did not include data on kinesiophobia. This is due to the fact that the first study on kinesiophobia in relation to TMD13 was published after the baseline data had been collected. The strength of the present study is the use of a comprehensive examination protocol by a calibrated examiner in accordance with the DC/TMD.6 The clinical examination was augmented with TMJ imaging, both MRI and CBCT, to establish the presence or absence of TMJ intra-articular disorders, as assessed by three calibrated radiologists according to a consensus protocol.20
In addition to a strict standardized examination protocol, the DC/TMD also includes a comprehensive set of instruments for carrying out a psychosocial assessment. This set of instruments includes an area of pain drawing for assessing pain comorbidity and the PHQ-15 for assessing somatic symptoms. The findings in the present study suggest that the relationship between catastrophizing and kinesiophobia, as described in the fear-avoidance model,10 also applies to patients with TMD.13 Whether assessment of catastrophizing and kinesiophobia should be considered as an additional measure in patients with TMD who do not respond to initial treatment therefore warrants further research.
It has been suggested that patients who do not suffer from catastrophizing, subsequently avoiding fear-evoking thoughts, stand a higher chance of confronting their problems and have a more solution-oriented cognitive pattern and behavior.8 Furthermore, poorer treatment outcomes have been reported in relation to high levels of catastrophizing for patients with TMD, but it has also been reported that outcomes can be improved by cognitive behavioral therapy.28 The clinical implication from these findings is that the evident association and interplay between catastrophizing and kinesiophobia in TMD, regardless of presence of pain, suggests that advice and self-management for these patients could benefit from incorporation of strategies including cognitive behavioral therapy. As a first line of treatment, this can involve patient education in the setting of the dental practice, with emphasis on explaining the benign nature of functional TMJ disorders. This approach may be sufficient for a majority of patients, but if further management is deemed necessary, especially for patients presenting with high levels of catastrophizing, this could involve sessions with a professional suitably trained in cognitive behavioral therapy, either in-house or through referral. Improving self-efficacy and reducing catastrophic thinking and fear of movement could thereby play a valuable role in comprehensive individualized treatment programs for different subgroups of patients with TMD.
Conclusions
Individuals with TMD pain reported more kinesiophobia than individuals with nonpainful TMD, and both painful and nonpainful TMDs are related to higher levels. TMD pain is also related to higher levels of catastrophizing, pain comorbidity, and physical symptoms. Pain comorbidity and somatic symptoms were mainly related to each other and to pain catastrophizing. The results suggest more fear of movement, as well as an association between catastrophizing and fear of movement, in participants with TMD regardless of the presence of pain. The overall findings suggest that assessment and management of fear of movement and catastrophizing may be useful as part of individualized treatment strategies for patients with TMD.
Clinical Implications
TMD pain is related to higher levels of catastrophizing, pain comorbidity, and physical symptoms.
Both painful and nonpainful TMD are related to higher levels of fear of movement.
The results suggest more fear of movement, as well as an association between catastrophizing and fear of movement, in patients with TMD, regardless of presence of pain.
Assessment and management of fear of movement and catastrophizing may be useful as part of individualized treatment strategies for patients with TMD.
Acknowledgments
This study was supported by the National Institute of Dental and Craniofacial Research of the National Institutes of Health (award U01DE019784). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
Preliminary results from this paper were presented as an abstract and poster at the virtual International Association for Dental Research meeting on 21 July 2021.
N.J., X.M.A., T.L., E.S., and B.H.H.: original concept; N.J., X.M.A., and B.H.H.: data analysis; B.H.H.: first draft. Interpretation of data was done by all authors, and all authors revised the manuscript for intellectual content and approved the final version of the manuscript.
Funding Statement
This study was supported by the National Institute of Dental and Craniofacial Research of the National Institutes of Health (award U01DE019784). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Dworkin S, LeResche L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- National Institute of Dental and Craniofacial Research. Facial pain. Updated July 2018. https://www.nidcr.nih.gov/research/data-statistics/facial-pain . Accessed 10 January 2022. [Google Scholar]
- Lövgren A, Häggman-Henrikson B, Visscher CM, Lobbezoo F, Marklund S, Wänman A. Temporomandibular pain and jaw dysfunction at different ages covering the lifespan – a population based study. Eur J Pain. 2016;20:532–540. doi: 10.1002/ejp.755. [DOI] [PubMed] [Google Scholar]
- National Institute of Dental and Craniofacial Research. Prevalence of TMJD and its signs and symptoms. Updated July 2018. https://www.nidcr.nih.gov/research/data-statistics/facial-pain/prevalence . Accessed 10 January 2022. [Google Scholar]
- Häggman-Henrikson B, Liv P, Ilgunas A, et al. Increasing gender differences in the prevalence and chronification of orofacial pain in the population. Pain. 2020;161:1768–1775. doi: 10.1097/j.pain.0000000000001872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014;28:6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan MJL, Lynch ME, Clark AJ. Dimensions of catastrophic thinking associated with pain experience and disability in patients with neuropathic pain conditions. Pain. 2005;113:310–315. doi: 10.1016/j.pain.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Wertli MM, Eugster R, Held U, Steurer J, Kofmehl R, Weiser S. Catastrophizing-a prognostic factor for outcome in patients with low back pain: A systematic review. Spine J. 2014;14:2639–2657. doi: 10.1016/j.spinee.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Pavlin DJ, Sullivan MJ, Freund PR, Roesen K. Catastrophizing: A risk factor for postsurgical pain. Clin J Pain. 2005;21:83–90. doi: 10.1097/00002508-200501000-00010. [DOI] [PubMed] [Google Scholar]
- Vlaeyen JWS, Kole-Snijders AMJ, Boeren RGB, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62:363–372. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- Vlaeyen JWS, Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain. 2012;153:1144–1147. doi: 10.1016/j.pain.2011.12.009. [DOI] [PubMed] [Google Scholar]
- Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain. 2000;85:317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- Visscher CM, Ohrbach R, van Wijk AJ, Wilkosz M, Naeije M. The Tampa Scale for Kinesiophobia for Temporomandibular Disorders (TSK-TMD) Pain. 2010;150:492–500. doi: 10.1016/j.pain.2010.06.002. [DOI] [PubMed] [Google Scholar]
- Gil-Martínez A, Grande-Alonso M, La Touche R, Lara-Lara M, López-López A, Fernández-Carnero J. Psychosocial and somatosensory factors in women with chronic migraine and painful temporomandibular disorders. Pain Res Manag. 2016;2016:3945673. doi: 10.1155/2016/3945673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velly AM, Look JO, Carlson C, et al. The effect of catastrophizing and depression on chronic pain–a prospective cohort study of temporomandibular muscle and joint pain disorders. Pain. 2011;152:2377–2383. doi: 10.1016/j.pain.2011.07.004. [DOI] [PubMed] [Google Scholar]
- Wheeler CHB, Williams ACC, Morley SJ. Meta-analysis of the psychometric properties of the Pain Catastrophizing Scale and associations with participant characteristics. Pain. 2019;160:1946–1953. doi: 10.1097/j.pain.0000000000001494. [DOI] [PubMed] [Google Scholar]
- Barsky AJ, Peekna HM, Borus JF. Somatic symptom reporting in women and men. J Gen Intern Med. 2001;16:266–275. doi: 10.1046/j.1525-1497.2001.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velly A, List T, Lobbezoo F. Comorbid pain and psychological conditions in patients with orofacial pain. In: Sessle BJ, editor. Orofacial Pain: Recent Advances in Assessment, Management, and Understanding of Mechanisms. Washington, DC: IASP; 2014. pp. 53–73. [Google Scholar]
- Fillingim RB, Ohrbach R, Greenspan JD, et al. Psychological factors associated with development of TMD: The OPPERA prospective cohort study. J Pain. 2013;14(suppl 12):T75–T90. doi: 10.1016/j.jpain.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiffman EL, Ahmad M, Hollender L, et al. Longitudinal stability of common TMJ structural disorders. J Dent Res. 2017;96:270–276. doi: 10.1177/0022034516679396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychol Assess. 1995;7:524–532. [Google Scholar]
- Osman A, Barrios FX, Kopper BA, Hauptmann W, Jones J, O’Neill E. Factor structure, reliability, and validity of the Pain Catastrophizing Scale. J Behav Med. 1997;20:589–605. doi: 10.1023/a:1025570508954. [DOI] [PubMed] [Google Scholar]
- Darnall BD, Sturgeon JA, Cook KF, et al. Development and validation of a daily pain catastrophizing scale. J Pain. 2017;18:1139–1149. doi: 10.1016/j.jpain.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhon DI, Lentz TA, George SZ. Unique contributions of body diagram scores and psychosocial factors to pain intensity and disability in patients with musculoskeletal pain. J Orthop Sports Phys Ther. 2017;47:88–96. doi: 10.2519/jospt.2017.6778. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- Campbell MJ, Swinscow TDV. Statistics at Square One. ed 11. London: Wiley-Blackwell; 2009. [Google Scholar]
- Bossuyt PM, Reitsma JB, Bruns DE, et al. The STARD statement for reporting studies of diagnostic accuracy: Explanation and elaboration. Ann Intern Med. 2003;138:W1–W12. doi: 10.7326/0003-4819-138-1-200301070-00012-w1. [DOI] [PubMed] [Google Scholar]
- Häggman-Henrikson B, Bechara C, Pishdari B, Visscher CM, Ekberg E. Impact of catastrophizing in patients with temporomandibular disorders-a systematic review. J Oral Facial Pain Headache. 2020;34:379–397. doi: 10.11607/ofph.2637. [DOI] [PubMed] [Google Scholar]
- Roelofs J, van Breukelen G, Sluiter J, et al. Norming of the Tampa Scale for Kinesiophobia across pain diagnoses and various countries. Pain. 2011;152:1090–1095. doi: 10.1016/j.pain.2011.01.028. [DOI] [PubMed] [Google Scholar]
- Plesh O, Adams SH, Gansky SA. Temporomandibular joint and muscle disorder-type pain and comorbid pains in a national US sample. J Orofac Pain. 2011;25:190–198. [PMC free article] [PubMed] [Google Scholar]
- Von Korff M, Dworkin SF, Le Resche L, Kruger A. An epidemiologic comparison of pain complaints. Pain. 1988;32:173–183. doi: 10.1016/0304-3959(88)90066-8. [DOI] [PubMed] [Google Scholar]
- Macfarlane GJ. The epidemiology of chronic pain. Pain. 2016;157:2158–2159. doi: 10.1097/j.pain.0000000000000676. [DOI] [PubMed] [Google Scholar]
- Häggman-Henrikson B, Visscher C, Wänman A, Ljótsson B, Peck C, Lövgren A. Even mild catastrophic thinking is related to pain intensity in individuals with painful temporomandibular disorders. J Oral Rehabil. 2021;48:1193–1200. doi: 10.1111/joor.13251. [DOI] [PubMed] [Google Scholar]
- Rollman A, Visscher CM, Gorter RC, Naeije M. Care seeking for orofacial pain. J Orofacial Pain. 2012;26:206–214. [PubMed] [Google Scholar]
- Poluha RL, De la Torre Canales G, Bonjardim LR, Conti PCR. Clinical variables associated with the presence of articular pain in patients with temporomandibular joint clicking. Clin Oral Investig. 2021;25:3633–3640. doi: 10.1007/s00784-020-03685-8. [DOI] [PubMed] [Google Scholar]