Abstract
Aims:
To investigate expectations and experiences of internet-based therapy (IBT) in adolescents with temporomandibular disorder (TMD) pain.
Methods:
Seven adolescents were strategically selected for this study. All patients had received IBT for their TMD pain in a previous randomized controlled trial. One-on-one interviews were conducted in a nonclinical setting. The interviews were semi-structured, following an interview guide with six domains. The recorded interviews were transcribed, and a qualitative inductive content analysis was then performed.
Results:
Content analysis indicated that the expectations of the adolescents and their experiences of IBT as a treatment for TMD pain can be understood in light of three main categories: (1) To become better; (2) An ambivalent experience; and (3) A personal challenge. The adolescents expressed expectations of less TMD pain after treatment, but also of improvement in general well-being and everyday life. Although their experiences of IBT varied, adolescents described having mixed feelings about treatment and feeling that it was personally challenging.
Conclusion:
Gained understanding of expectations and experiences is a necessary basis for revising the IBT program to meet the demands of adolescents and to improve treatment adherence. Furthermore, the content of the three categories clarifies the values of adolescents, and this understanding can in turn contribute to the development of new patient-centered treatment programs. J Oral Facial Pain Headache 2022;36:237–252. doi: 10.11607/ofph.3042
Adolescents today face high demands and expectations. Their environment requires that they continually follow new trends in technology, seek social acceptance, and maintain a high level of performance at school, as well as in their work life and spare time. Recent reports of adolescent health issues, including mental health, are alarming.1,2 Several studies have documented increases in the prevalence of depression, anxiety, and stress over the years,1,3,4 with stress contributing substantially to the development of a wide range of health issues, including several pain conditions.5,6
Chronic pain is a common and significant health issue involving consequences at the physical, psychologic, and social levels. It has been estimated that 20% of the adult population suffers from chronic pain.7,8 The most common chronic orofacial pain with a nonodontogenic origin is temporomandibular disorder (TMD) pain. TMD pain has a reported prevalence in adolescents of 2% to 6%, with prevalence rates increasing with age.9 Current research reports gender differences in this condition.10 One study9 found a TMD pain prevalence of 8% to 9% among 17- to 19-year-old girls, but only 3% to 4% among boys of the same age. Other sources have also reported higher incidences of TMD pain among girls than boys.11
The impact of TMD pain in adolescents can cause negative consequences, with depressive symptom scores and somatic complaints being higher than in nonaffected adolescents.12 One study on adolescents with TMD pain described how their physical problems and daily demands developed into a vicious circle that caused them to oscillate between hope and despair.13 Other studies found that every fifth adolescent was absent from school due to TMD pain and its consequences.10,12
Although several studies have assessed TMD risk factors,14 the etiology of TMD pain is still not fully understood. Predictors include multiple pain conditions elsewhere in the body, severe depression, and female gender.15 Further, evidence suggests that these factors are associated with the maintenance of TMD pain in adults.16,17 For example, Grossi et al found that depression predicted poor treatment outcome.16 Evidence on etiologic factors of TMD pain is derived mainly from adult populations. LeResche et al14 have published one of the few large prospective studies on the onset of TMD pain in adolescents. Their study confirmed that many of the risk factors for onset of clinically significant TMD pain are similar in adolescents and adults. Moreover, pain reports in early adolescence have been found to be associated with pain in early adulthood,18,19 which indicates the importance of early diagnostics and treatment of perceived pain. Nevertheless, studies have found that TMD pain is severely underdiagnosed and undertreated.9 According to List et al,10 the majority of adolescents with TMD pain who reported pain once a week or more had a perceived treatment need. A more recent Swedish study reported similar findings.12
The debilitating consequences of TMD pain for both the patient and for society have brought increasing attention to the condition as a serious health issue, with numerous therapies being explored and developed. Aside from individualized information about the condition, occlusal appliance therapy is commonly used in the treatment of TMD pain and has proved to be effective.20 Other treatments include behavioral treatments such as relaxation training and cognitive behavioral therapy (CBT). Although these have been proven successful in the treatment of TMD pain among adults,21 Wahlund et al22,23 found them to be less effective in adolescents with TMD pain compared to occlusal appliance therapy.
Occlusal appliance therapy focuses on the symptoms of TMD and is thus considered a symptomatic treatment. Despite results indicating its effectiveness, it does not treat the causal factors behind TMD. In contrast, behavioral treatments emphasize individual causative factors and require active engagement of patients during treatment. These causal treatments have the potential to deliver a more long-lasting treatment effect. Cooperation, however, is key for any treatment to be effective, and behavioral therapies have difficulties achieving sufficient levels of patient cooperation, most likely due to the time and effort required to reach improvement.
A more recent behavioral treatment option offered at the Department of Orofacial Pain and Jaw Function in Malmö, Sweden, is an internet-based therapy (IBT) program for adolescents with TMD pain. The seven-part program is based on CBT. Each section has an estimated treatment period of 1 week. The program is designed to help patients identify the personal causative and maintaining factors of their TMD and uses video and text to provide patients with information, recommendations, and training programs. At the beginning of treatment, patients receive a paper workbook that supplements the online treatment program. In the workbook, participants write down their responses as they work through each section online. The layout of the workbook and the treatment program are the same. Treatment time is approximately 7 to 8 weeks and includes weekly contact with a treating dentist.
Use of modern technology to treat chronic pain is promising, and technology makes it possible to reach many patients at a relatively low cost. IBTs have already been developed for the treatment of headache, juvenile idiopathic arthritis, and chronic general pain in adolescents. Studies evaluating the effectiveness of these treatments report favorable results.24–26 To the authors’ knowledge, no published studies have examined the effect of IBT on TMD pain and jaw dysfunction in adolescents, and the IBT described herein is the first internet-based intervention designed for TMD pain in this age group. Adherence to and the effectiveness of IBT were evaluated in a multicenter RCT (Bijelic et al, unpublished) in which IBT was compared to occlusal appliance therapy. The study group comprised Swedish adolescents and showed comparable effectiveness for IBT vs occlusal appliance therapy after a 3-month follow-up; however, the adherence to IBT was considerably lower.
Care providers must account for the particular preferences, concerns, and expectations of each patient in clinical praxis if treatment is to be effective. To identify these values and thereby contribute to further knowledge of patient values as part of evidence-based medicine, the study design must be based on qualitative research methodology. Qualitative research methods incorporate various analytical methods for data interpretation that allow us to deepen the understanding of a phenomenon. Previous studies have used qualitative methodology to investigate experiences of TMD pain13 in adolescents and TMD pain treatment with jaw exercises in adults.27 However, no study has shed light on the expectations and experiences of IBT for TMD pain among adolescents.
Behavioral therapies have been proven to be effective in the treatment of pain, but adherence has been rather difficult to achieve.28,29 Understanding why is important; thus, the present study used qualitative methodology aiming to explore the expectations and experiences of IBT among adolescents with TMD pain in order to increase understanding of the low adherence observed in the previous RCT.
Materials and Methods
As behavioral therapy has been shown to reduce pain and improve activity interference related to pain,30 the present study employed a qualitative design to evaluate patient expectations of and experiences with an internet-based behavioral approach to treating TMD pain in adolescents. Data were collected through one-on-one interviews with seven adolescents. Qualitative content analysis as described by Burnard31 and Elo and Kyngäs32 was used to analyze the transcribed texts. One of the authors, a dentist and researcher (T.B.), conducted the semi-structured interviews.
All participants in the present study received detailed verbal and written information about the study that repeatedly emphasized the voluntary nature of participation. Before treatment began, each patient (or guardian if the patient was younger than 18 years) signed an informed consent form. The Ethics Board at the University of Lund in Lund, Sweden, approved the study (Daybook no. [DNR] 2015/70).
Participants and Recruitment
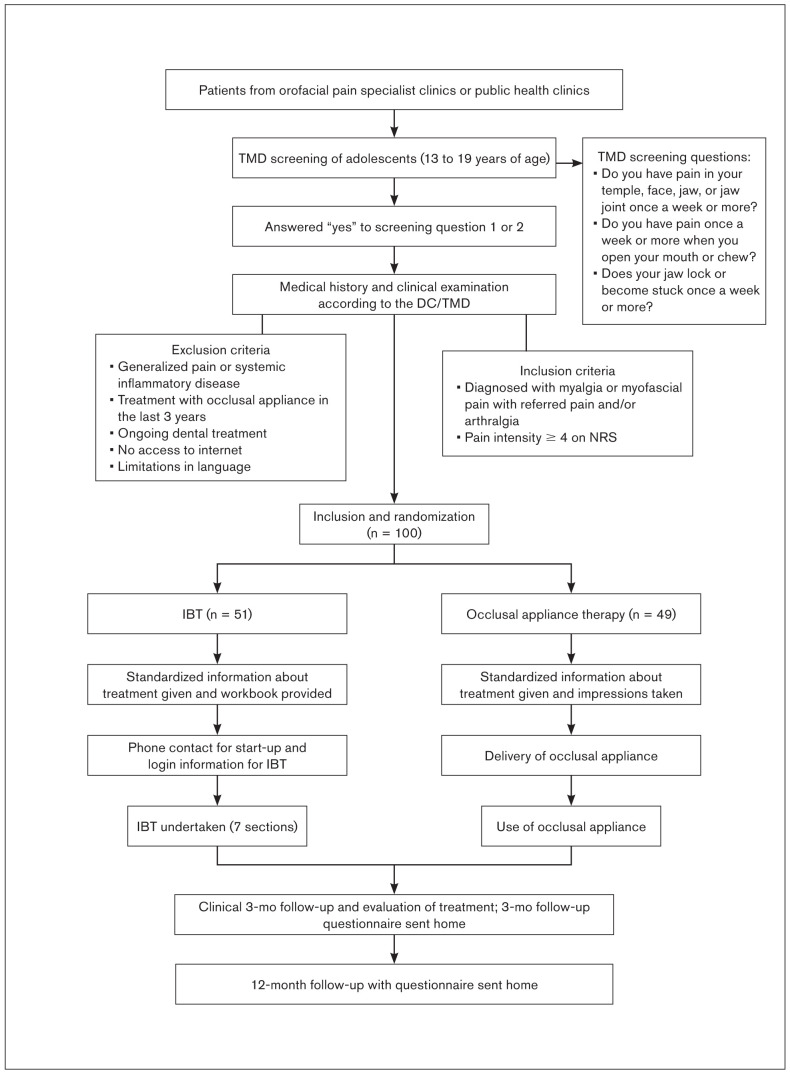
All patients in the present study had participated in a previous RCT (Bijelic et al, unpublished), a study of 100 Swedish adolescents with TMD pain that compared the adherence and effectiveness of occlusal appliance therapy to IBT after 3 and 12 months (Fig 1). Patients were examined according to the Diagnostic Criteria for TMD (DC/TMD)33 and then randomly selected to receive treatment with an occlusal appliance or with IBT. A detailed description of the IBT program is provided in Table 1. Inclusion criteria in the present study were:
Fig 1.
Flowchart of the randomized controlled trial.
Table 1.
Description of the IBT Program for Chronic TMD Pain in Adolescents
| Section | Content | ||
|---|---|---|---|
| Educational information | Pedagogical method | Patient assignment | |
| 1. Introduction | Introduction to IBT, treatment purpose, goal-setting, and obstacles | Text, descriptive pictures | Reflect on previous strategies of managing TMD pain, assess treatment expectations, reflect on goals and obstacles. |
| 2. What is face and jaw pain? | Etiology and epidemiology of TMD pain, anatomy of the masticatory system | Text, descriptive pictures, video (jaw anatomy and function, etiology of pain) | Make a pain drawing and identify jaw functions limited by pain. |
| 3. What affects/contributes to my face and jaw pain? | Causal factors of TMD pain, pain physiology, acute and chronic pain, consequences of pain | Text, descriptive and symbolic pictures, video (pain physiology) | One-week pain diary: Score pain intensity and identify activities and/or situations that trigger pain. |
| 4. How can I relieve my pain? | Treatment alternatives: analgesics, relaxation and jaw exercises, and occlusal splints | Text, descriptive and symbolic pictures, multiple videos (relaxation and jaw exercises shown by dentist) | Identify patterns of pain from pain diary, practice relaxation and jaw exercises. |
| 5. What is the relationship between pain and stress? | What stress is, stress symptoms and responses, the relationship between stress and pain, what a situational analysis is and how it is to be done | Text, descriptive and symbolic pictures, video (situational analysis) | A questionnaire to assess the degree of stress and physical and psychologic symptoms of stress, situational analyses, state desired ways to increase recovery, continue relaxation and jaw exercises. |
| 6. How can I reduce my stress and pain? | Stress and pain management, breathing exercise, the importance of sleep, training, and good dietary habits, time management, acceptance, setting boundaries | Text, symbolic pictures, videos (the relationship between stress and pain, breathing exercise, the impact of sleep, training, and diet on stress experience, time management) | One-week diary of sleep, training, and dietary habits, activity planning to make desired changes regarding these, continue relaxation and jaw exercises. |
| 7. Summary and plan for the future | Different potential effects of IBT, summary of IBT, setbacks, and maintenance plan | Text, symbolic pictures | Describe performed changes in life, new reflection on goals and obstacles, reflect on treatment effect, develop a maintenance plan and plan for setbacks. |
Aged 13 to 19 years
A diagnosis of myalgia/myofascial pain with referred pain and/or arthralgia according to the DC/TMD
A self-reported pain intensity of ≥ 4 on a 1 to 10 numeric rating scale (NRS)
Randomization to IBT, which they had completed or discontinued, in the previous RCT
The objective was to select a strategic sample of participants with variations in age, gender, and geography in the study group. The selection of participants also had the purpose of including subjects who could express themselves, and thereby their various expectations and experiences of IBT, in Swedish in order to illustrate the phenomenon being examined. Experiences from previous studies contributed to the choice of this selection strategy.13,34 The ability of the participants to express themselves was assessed during phone follow-ups as part of the IBT.
The number of participants was not determined beforehand. An offer of participation in the study was made by phone or personal contact (during follow-up visits to the specialist clinic in orofacial pain at Malmö University) with potential participants. To include the full range of IBT experiences, potential participants were contacted a second time by mail and phone. A total of seven adolescents, six girls and one boy, were enrolled; six had completed the IBT. The age of the study population ranged between 15 and 20 years (one 19-year-old participant had turned 20). The group resided in the southern and central regions of Sweden.
Data Collection
The semi-structured interview had two focuses: (1) expectations and (2) experiences of IBT. The interview guide had six domains that covered these two focuses (Table 2). The six domains were identified and defined after discussion in the author group, which included two specialists/researchers in orofacial pain, one expert in qualitative methodology, and one general dentist. The domains were thus defined based on the author groups’ different experiences of interviews and adolescent patients. The interview questions were open-ended to encourage participants to freely reflect and express themselves. The interviewer started by asking all participants the same question: Can you tell me about your expectations of IBT? As the interviews progressed following the layout of the domains, probing questions such as “Can you tell me more about …?” and “Can you elaborate a little more on that?” were used to encourage the participants to elaborate further.
Table 2.
Interview Guide
| Domain | Topic/theme |
|---|---|
| 1 | Expectations of treatment |
| 2 | Perceived need of treatment |
| 3 | Experience of treatment |
| 4 | Advantages and disadvantages of IBT treatment |
| 5 | Perceived effect of treatment |
| 6 | Experience of treatment support |
Interviews were conducted between December 2017 and May 2018. They took place in a nonclinical setting and were recorded on a voice recorder. Thereafter, the recording was transcribed verbatim by a medical secretary and saved as a coded file. The first author listened to all interviews while reading the transcripts in order to confirm the correctness of the transcriptions. Only minor corrections were made. The interviews lasted 20 to 43 minutes, and the collected data totaled 125 double-spaced pages.
Data Analysis
Content analysis according to Burnard31 was used to analyze the transcribed texts. This method is not linear; rather, it is an inductive process with several steps.
First, all authors read the transcriptions several times in order to form an overall impression of the material. One author (T.B.) identified sentences or paragraphs in the transcriptions (“meaning units”) that addressed the study aim. Thereafter, all authors reviewed the meaning units. Each meaning unit was condensed in a two-step process that removed unnecessary words and left the essence. Three authors (T.B., EC.E., and I.M.N.) then grouped the condensed meaning units with similar meaning into “codes.” Codes were labeled in a way that represented all aspects of the content in the related meaning units. The fourth author (A.W.) reviewed the codes and their associated condensed meaning units, which led to minor revisions of the groups. All authors then made a final review of the codes. After discussion and further adjustments, a consensus was reached, and the codes were grouped into “categories.” All data fitted, and no data were left over. Table 3 illustrates how a meaning unit was gradually condensed and assigned to a code and then a category.
Table 3.
Example of Steps from Meaning Unit (MU) to IBT Category
| Transcribed MU | First condensation of MU | Second condensation of MU | Code | Category |
|---|---|---|---|---|
| Mm, it’s probably that you’ve had problems for so long, that you’re so tired of. So when the help comes, you think it will be like “now it will be good right away and nice.” (laughs) But that is not always the case, it takes time. | My problems would disappear immediately because I’ve had problems for a long time that I’m tired of, so when you’re about to get help for them you think it will be good right away. | My problems would disappear immediately because I’ve had them for a long time and was getting help for them. | Receive help: The pain would disappear | To become better |
Results
Content analysis indicated that three main categories (“To become better”; “An ambivalent experience”; and “A personal challenge”) and their supporting codes described the expectations and experiences of adolescents with TMD pain who had been enrolled in the CBT-inspired IBT program (Table 4). Quotations from the interviews illustrate the categories and their respective codes. Letters A to G identify the participants.
Table 4.
The Three IBT Categories and Their Supporting Codes
| Category | Expectations | Experiences | |
|---|---|---|---|
| To become better | An ambivalent experience | A personal challenge | |
| Codes | Receive help: The pain would disappear | Confusion and skepticism: Treatment doubtfulness | Demands of performance: Own and others |
| Acquire knowledge and tools: To become better | IBT makes demands: Gives rise to anxiety and stress | Structure and discipline: Need for control and confirmation | |
| Need for support: An ambivalent experience | A new way of thinking: Gave understanding | ||
| Treatment exercises: A double-faced experience | Difficulties describing personal issues: Personal life is private | ||
| Benefits of IBT: A mixed experience | Concerns about remaining problems: Future consequences | ||
| IBT shows patterns: Gives new knowledge | |||
Category 1: To Become Better
This category describes the expectations of the participants before the start of IBT. Some expectations focus directly on pain relief to some degree, while others are more general and focus on an overall improvement in well-being. Common for all expectations is an expectation of being better after finishing IBT. The following two codes describe this category.
Receive help: The pain would disappear.
The content of this code describes expectations of being free of TMD pain after IBT. Sometimes, the participants stated reasons why the pain would disappear; for example:
It [my problems] would be solved because now someone is taking me seriously. —G
My problems would disappear immediately because I’ve had them for a long time and was getting help for them. —F
In general, the expressions in this code reveal expectations of pain elimination and describe how this ought to be achievable. Nonetheless, one interviewee narrated expectations beyond becoming pain-free:
Treatment would immediately solve all problems and everything would become perfect. —F
Overall, participants expected their pain and problems to disappear due to an awareness that they were receiving help and being taken seriously.
Acquire knowledge and tools: To become better.
The content of this code describes milder expectations. For instance, although the adolescents did not expect to become pain-free, they did expect to become better and feel less pain:
[I expected to] . . . become better because I am treating it, which I have not done before. —D
I expected the pain not to be there as much. —A
Pain alleviation was considered to be not only a welcome lessening of pain but also related to an improvement in general well-being:
[I expected to] . . . live with fewer worries in life and to have fewer things wrong with me. —A
However, complete freedom of pain was considered less likely, as one participant expressed it:
I did not expect the pain to disappear, those expectations are too high. —E
The reasons for expectations of persistent pain varied. One adolescent explained that expectations of persistent pain were related to a deviant jaw function:
I did not expect to be completely pain-free because sometimes my jaw locks. —B
Further, adolescents also expected to gain knowledge about their pain and acquire tools for reducing and coping with it. Similar to the “Receive help: The pain would disappear” code, this code describes the expectations for pain alleviation but to a more moderate extent. Additionally, their expectations included improved general well-being and the acquisition of knowledge and tools for dealing with the pain.
Category 2: An Ambivalent Experience
This category, the first of two describing participant experiences, highlights the ambivalence and variation in IBT responses, which ranged from feelings of confusion and stress to satisfaction with the gained knowledge and improvement in TMD symptoms. This wide range of experiences is discernible throughout the category, occurring in each code. Although the adolescents performed identical tasks in the treatment program, their perceptions differed and they reported varying experiences. Not only did the reports of experience differ from one participant to another, but the same participant would sometimes make contradictory statements about an experience. This inconsistency in experiences within a participant was labeled “ambivalence.” Codes corresponding to this category are presented below in chronologic order of the treatment program.
Confusion and skepticism: Treatment doubtfulness.
In this code, views reflected the confusion of the adolescents and their skepticism regarding IBT. Expressions of two participants clearly illustrate their uncertainty toward treatment:
In the beginning, I felt very messed up and completely confused [that this was CBT] . . . [I thought] is this really right? —A
I believe more in physical treatment methods. —F
Another adolescent explained the reason for skepticism toward treatment as:
I did not understand how it would help . . . my problems are physical and IBT can only help in a psychological sense. —C
Another participant described skepticism as being related to thoughts expressed by their family, which affected their attitude to treatment:
My partner urged me to try, but my family was skeptical . . . [asking] “Why are you doing it?” . . . I myself thought “I hope it works,” but I did not know if it would. —G
Participants shared the view that they were confused, hesitant, questioning, and skeptical. In general, the uncertainty and confusion regarding IBT was something that occurred within the individual, while skepticism was directed toward the treatment.
IBT makes demands: Gives rise to anxiety and stress.
Participant statements made it clear that the adolescents felt anxious, worried, and stressed during IBT, which are experiences related to their perception of demands made by the treatment. One participant expressed feeling:
Anxious for forgetting to answer something [in the workbook]. —A
Another adolescent expressed feelings of guilt:
I felt guilty because I hadn’t done the exercises [in the workbook], so I did not want to have a follow-up by telephone. That was mostly the reason why it got postponed so much...I had much anxiety about not finishing treatment. —F
The adolescents reported recurring experiences of stress during the interviews. Stress was related to various things throughout treatment; overall, adolescents experienced difficulties incorporating new routines and activities into their everyday lives, which was a common cause of stress:
It was a bit stressful . . . just one more thing to do. So now I have a job and school and another thing [IBT] on top of that, it’s tough. When I have my day planned out, it becomes stressful to add another thing to do and find time to do it. —G
Aside from the demands that the adolescents felt IBT imposed, a combination of difficulties establishing routines, completing tasks, and personal demands resulted in experiences of anxiety and stress among the adolescents.
Need of support: An ambivalent experience.
In this code, the ambivalence previously described becomes clearly discernible. Although participants said they felt no need for support during treatment, they could also feel otherwise at some point, as one participant expressed:
Did not need any support from my family
. . . [but sometimes I] got the feeling of being left out . . . It meant a lot to be able to talk to her [the IBT caregiver]. —C
The overall content of this code seems to reveal that adolescents differ on the importance of support from family, partners, and friends vs support from the health care provider. While the first is considered less critical for some participants, they attach great importance to support from the caregiver during and after treatment, for example:
[During follow-ups by telephone] I could ask questions if I needed to, I thought that was good . . . Good that the follow-ups by telephone were quite often. —E
I would have liked a follow-up with a dentist during treatment . . . to get a confirmation that you are heading in the right direction. —G
This, in turn, seems to indicate a potentially low level of empowerment among participants.
Treatment exercises: A double-faced experience.
When interviewees were asked to reflect on the jaw exercises in IBT, the shared view was mainly one of satisfaction. They seemed to feel the exercises were helpful, as one participant described:
The exercises help one to relax [the jaw]. —B
One participant emphasized the benefits of trying different types of exercises, and another thought that it was:
Good with individualized exercises, it then felt as if they were the right kind of exercises. —A
However, not all adolescents experienced positive effects. Some reported that they did not like the exercises since they provoked more pain:
From time to time, it only got worse in my jaws . . . Some exercises made the pain much worse. —E
Thus, these statements highlight the double-faced experience that adolescents described regarding jaw exercises in IBT.
Benefits of IBT: A mixed experience.
The adolescents described varying benefits of their IBT experiences. Responses concerning treatment effect on TMD pain ranged from IBT helping very much to not at all. Quotations from one participant illustrate the mixed experiences that several had of IBT:
It [IBT] had a good design, but I couldn’t relate to all the questions in the treatment . . . I can’t say that it made me feel better, but I got more knowledge and it made me think in another way . . . I don’t regret doing the treatment, I thought it was good because I gained more understanding. —D
The inability to relate to certain parts of treatment was approached by another participant, who further elaborated on the consequences of this by expressing a personal sense of alienation:
It felt as if it [IBT] was designed with younger persons in mind . . . it included many questions about school . . . I couldn’t relate to some sections because they concerned a younger age group, so I just felt like, what about me? —G
Among benefits with IBT, one participant mentioned:
While I was undergoing treatment, I found that I felt less stressed. I became more balanced. —C
But not all participants were clear on the benefits of IBT. A quotation from one participant reveals uncertainty about the treatment effect:
I thought that you should have some kind of follow-up after half the treatment . . . like some confirmation that you are on the right track, because I was a bit unsure during the whole time, “Is it better now? Because it doesn’t feel better, but it might be better”. —G
Overall, the participants described a mixed experience, with both benefits of and drawbacks to treatment.
IBT shows patterns: Gives new knowledge.
This code demonstrated that interviewees reflected on what they learned about pain and stress from IBT. The potential to see a pattern was recurrently brought up and related to their gain of new knowledge, for example:
I could see that when I have a lot to do at school or at work, I feel more pain . . . I learned about triggers of pain and the consequences. —D
It also appears that adolescents had reached an understanding of stress and how it relates to their TMD pain. One participant stated that:
About triggers [of pain], when I was going to have a test in school, I noticed that I became very stressed . . . training helped reduce stress. —D
By considering their pain from a new perspective learned in IBT, the adolescents began to understand the reasons for and how to cope with TMD pain:
I learned that my pain can be stress-related . . . and how to manage the pain in the future. —B
One participant summarized the content of this code by describing how IBT had affected their way of thinking:
It is more about how I think of the psychological part. When you have pain, it is possible to get stressed by the fact that you have pain since it affects your everyday life and school, relationships and such. So, it might have made me less stressed about my pain. —C
Category 3: A Personal Challenge
This category reflects some thoughts and views of the adolescents on IBT. They express how they had difficulty answering questions about themselves, how they felt about the demands they and others had placed on them regarding their performance during treatment, and the need for structure and control. Participants were also concerned that their TMD symptoms would be misunderstood by the caregiver and that symptoms would persist with their related consequences.
Further, the participants reflected on the new way of thinking, stating that it was positive and allowed an understanding of the perceived symptoms, but also that it was demanding and a personal challenge. The codes of this category are presented in descending order of the amount of data in each code.
Demands of performance: Own and others.
The condensed meaning units in this code reflect how participants felt pressured to perform during treatment. Some felt the need to perform for the sake of the study, and others to meet their own demands on themselves:
I felt pressured to perform . . . It is me as a person who says, “Ok, now I have to do it [IBT] to be able to answer your questions,” so that you get the answers you need [for the study]. —A
I like to support things, although it can be too much sometimes . . . I agreed to participate for your [university’s] sake, so that it would be a good study. —F
The adolescents gave the impression of being highly performing in general, causing them to feel obligated to perform well during IBT and thus experiencing demands. For example, one interviewee reflected:
I am stressed and I feel bad if I can’t perform well. —D
The existence of personal demands can be repeatedly observed during the interviews. Apart from demands of performance experienced when enrolling in IBT, personal demands were also experienced during treatment:
I did it anyway, I tried and did as good as I could . . . even though the exercises did not work. —E
One part of the treatment program that seemed to have been particularly stressful for the adolescents was the follow-up by telephone:
I feel very . . . I almost get claustrophobic. I feel weighed down when I must make a telephone call, I don’t know why. —F
Although feeling stressed to perform, interviewees expressed satisfaction with their performance, with the time allowed for each section, and with the number of tasks. They also felt that they were able to balance IBT with everyday life.
Structure and discipline: Need for control and confirmation.
Analysis of the meaning units in this code shows how adolescents value having control during treatment. Control was related to knowing what the next section would cover so that they were able to mentally prepare themselves, having constant access to the workbook, and feeling that treatment is a “complete treatment.” Further, being in control was described as being able to ask questions and influence follow-up content and as having scheduled times, durations, and frequency of the follow-ups by phone.
Adolescents repeatedly expressed need for control by highlighting the importance of a well-organized treatment program through expressions such as:
I like when there is structure . . . it makes me calm . . . I have control needs. —E
Something that further reflected their need for control was expression of a demand for confirmation; for example:
It was nice to know that the exercises were being done in the right way. —C
Although the participants previously claimed that phone support was stressful and demanding, the content of this code indicates that this structured follow-up method met their demands for control and confirmation.
A new way of thinking: Gave understanding.
The content of this code shows how adolescents reflected on a new way of thinking regarding their pain, which gave them the potential to see a pattern from a new perspective; for example:
It looks like a pattern . . . I try to avoid chewing gum and hard and tough food. [I could see that] It makes it worse, so I have tried to avoid it. —D
They felt that reflecting on their problems in order to deal with them was valuable and gave them greater understanding of perceived TMD symptoms. With this perspective on perceived TMD pain, adolescents gained insight into their problems, which among other things could make them realize that:
I’m a person who stresses about things . . . I get tense when I’m nervous or have a lot to do. That’s one reason why I have pain. —D
Generally, the new way of thinking and reflecting on their issues appears to have been appreciated among the participants:
I have benefited from the treatment, I think in another way now. —G
Difficulties describing personal issues: Personal life is private.
The adolescents reported difficulties answering questions about their pain and personal life during treatment. One participant who was concerned with how this might affect the ability to receive future treatment expressed:
I find it difficult to describe my thoughts in words. I don’t want my problems to be exaggerated, but neither do I want to downplay the pain and discomfort. So I got a little anxious about it. —F
Another informant clearly described what a number of informants appeared to have experienced during treatment:
I think it’s difficult to answer questions about myself, how much pain I have and how I feel, and to describe it. —D
One participant also questioned the reason for answering these personal questions:
I usually don’t like answering questions about my well-being and personal life . . . I thought, “How can you relate this to my pain?” —F
Thus, the content of this code clearly shows that participants found questions about their personal life difficult to deal with and that they created both stress and worry.
Concerns about remaining problems: Future consequences.
This code describes how the informants worried that their health problems and TMD symptoms would persist. For example, they felt:
Anxious that it won’t get better. —E
That I will have to live with the problems with my jaw for the rest of my life. —A
Worry was also related to the uncertainty of what persistent problems would lead to, and, for some, increased their stress experience:
I was very stressed about that. So I thought, “Will this go away? Will it not go away? In that case, what will it lead to?” —C
Another participant reflected on what would be needed for future improvement, stating that:
A miracle is needed for the jaws to get better . . . it’s stuck so hard that it feels like it could not get better that easy. —E
Overall, the expressions in this code demonstrate a reflection on and presence of concern related to the thoughts of the adolescents on future consequences if their perceived symptoms persist.
Discussion
The present study explored and described the expectations and experiences of IBT among adolescents with TMD pain, performed through one-on-one interviews that encouraged adolescents to describe and reflect on IBT in order to achieve an understanding of their individual values. More interview data were collected for IBT experiences than for IBT expectations.
IBT Category 2: An Ambivalent Experience
In general, adolescence is a stressful time of life, with increasing social, physical, and cognitive demands. Experiencing pain makes these demands more challenging,13 emphasizing the importance of treatment to reduce pain. Treatment of TMD pain with IBT was seemingly an ambivalent and demanding experience, feelings that prevailed both between participants and within the same participant.
Ambivalence during IBT could be observed in several parts of the treatment; for example, the treatment exercises. While sharing an overall view of satisfaction with the exercises, some adolescents also expressed dissatisfaction when their pain worsened. This description of jaw exercises is consistent with findings in previous studies in an adult population.27
Further, adolescents narrated being confused and feeling doubtful toward treatment, especially those with the perception that IBT is a “psychologic” treatment. For others, doubtfulness was related to uncertainty about whether IBT was the appropriate treatment, with stronger beliefs in “physical” methods for the treatment of perceived symptoms. These findings are consistent with previous findings in adolescents with chronic pain.35 The origin of these preconceived ideas among the adolescents in the present study is unclear, but it is known that these ideas impact the way they engage in treatment, the way they interact with their caregiver, and their success and satisfaction with treatment. Studies show that better treatment outcomes often are achieved if patients believe they are going to have a positive outcome and thus engage more constructively in treatment.36
Concerning these findings, it is of interest to highlight potential factors that could influence the thoughts and beliefs of adolescents about their pain and hence their experiences of treatment for their pain. In the interviews, the participants expressed that their families were skeptical of IBT. Crushell et al37 found that children of parents who acknowledged a psychologic aspect and not a purely physical cause of their child’s pain were significantly more likely to have recovered after treatment. At the same time, Guite et al38 did not manage to find significant agreement between adolescents and parents regarding their degree of endorsement of a biopsychosocial perspective of pain. In a study with a qualitative design,34 adolescents with TMD pain presented self-constructed explanations of their pain, with some adopting a physical explanatory model while others related their pain to psychologic factors. Consequently, experiences of doubtfulness and confusion during IBT can be related to preconceived ideas of pain by the patient, as well as beliefs and thoughts about pain among family members.
On the topic of need for treatment support, ambivalence among the participants became apparent. While partly sharing a view of no need for support from family and friends, they later reflected on the importance of treatment support from their caregiver, primarily in search of confirmation. This forces a discussion on the level of self-efficacy and empowerment of the adolescents. Overall, it can be interpreted that participants in the present study had a low belief in their own ability to evaluate their treatment efforts and the outcome of such efforts.
In recent years, a stronger focus on patient empowerment has emerged as an outgrowth of contemporary health care ambitions to be patient-centered. Also, e-health services are rapidly evolving, and patient activity and engagement are essential for the success of these services. Patient empowerment is considered to facilitate patient independence, self-management, and self-efficacy.
A 2017 review on patient empowerment in the e-health context39 revealed that e-health interventions improve self-reported levels of engagement and knowledge and are positively correlated with better health outcomes in various study populations. In line with these findings, the participants in this study reported enhanced knowledge and an ability to distinguish patterns of perceived pain.
Although sharing a mixed experience concerning the benefits of IBT, the adolescents notably appreciated their gain in knowledge and the associated understanding of factors related to their TMD pain. Yet, for some, this enhanced knowledge was not related to improved well-being, underlining an ambivalence regarding perceived benefits of IBT. In this case, readiness to adopt a self-management approach and thus engage in behavioral change can be questioned. Greater readiness to adopt a self-management approach has been associated with better treatment outcomes in adolescents with chronic pain in terms of reduction in functional disability, depressive symptoms, and fear of pain.40 Consequently, it is important to consider the readiness of adolescents to self-manage before they begin care in order to support their willingness for behavioral change and optimize conditions for treatment effect.
IBT Category 3: A Personal Challenge
A general overview of the data in this category presents an image of IBT as a personal challenge. Throughout the interviews, participants recurrently delineated their experiences between personal demands and demands from their surroundings. These in turn gave rise to feelings of stress and pressure to perform during treatment, enhancing the experience of IBT as a challenge and revealing their need for control and confirmation. The need for control during e-health interventions is not unique to these participants. Lenhard et al found that adolescents undergoing internet-delivered treatment for obsessive compulsive disorder had a positive experience of working independently with the treatment program and thus having control over the therapy process.41 This agrees with the results of the present study, where adolescents reacted positively to being able to communicate questions or problems and to choose when to work with the treatment.
Adolescents stressed difficulties during treatment, including struggles incorporating IBT into their daily life and answering questions during treatment. Previous studies have reported similar findings of difficulties with integrating self-management interventions into everyday life.27,42 Interestingly, clear understanding of the purpose of interventions has been found to be an important factor for adolescents wishing to incorporate challenging interventions in everyday life.42 This may explain why the adolescents in the present study reported such difficulties. Because self-management interventions for pain, such as IBT, commonly comprise elements that require patients to describe their symptoms and analyze these in relation to their general well-being and private life, exploring the reasons for these difficulties is highly relevant.
Pronounced difficulties in describing personal issues may be related to a limited experience of autonomy, which has been identified as an important experiential dimension of internet-delivered therapy.41,43 The findings of this study contrast with those of other studies reporting positive feedback from adolescents on this issue; in comparison with face-to-face contact, they felt that internet-based interventions better facilitated communication about personal problems in everyday life.41 Regarding the design of the IBT in the present study, the authors believe there is good potential for promoting the autonomy of the patient. This includes the flexibility of working at a self-chosen time and place and the possibilities of asking questions during treatment, deciding when to have a follow-up by phone, and to some extent, extending the treatment time if needed. However, the adolescents still found it difficult to express and describe their own symptoms and related personal problems. Reflecting on a statement from one participant stressing “difficulties turning thoughts into words” raises questions about language skills, vocabulary, and cognitive control among the participating adolescents and suggests a need to consider cognitive factors in order for adolescents to successfully engage in treatment.
Although the treatment was demanding, the participants described having achieved an understanding of their pain. Despite this, they expressed concern about the future and questioned whether they would ever be pain-free. This phenomenon was also found in another study on adolescents with TMD pain.13
Overall, participants implied that the IBT program was challenging in many ways. For most of the included adolescents, IBT meant more demands in an everyday life that was already demanding and stressful. For some, it also fostered a need to control and thoughts of future consequences. However, despite the challenges of IBT, participants gained a new perspective, and, as they expressed it, learned to view their issues in a way that allowed them to move on.
Expectations
The results of the present study revealed that the adolescents had diverse expectations of IBT; however, they all expected an improvement in well-being. Expectations expressed in the code “Receive help: The pain would disappear” mainly concerned thoughts of becoming pain free and could be interpreted as excessive when compared to expectations expressed in the code "Acquire knowledge and tools: To become better,” where adolescents expressed expectations of a reduction in TMD pain in a less pronounced way.
Expectations commonly viewed as excessive or unrealistic are usually thought to be detrimental to patients. Consequently, it seems natural to assume that the expectations among the present participants of becoming pain-free may have played a crucial role in their adherence to IBT and could thereby explain why adherence was found to be less successful in the authors’ previous RCT (unpublished). However, one study demonstrated that excessive expectations were related to superior treatment outcomes in patients with chronic pain.44 These findings contradict other studies45,46 suggesting that moderate expectations are associated with better outcomes, and, to some extent, also contradict the explanation of a lower adherence to IBT.
Nonetheless, it can be speculated as to whether the expectations of the adolescents in the present study may have influenced this outcome in other ways. One reason for dropping out of IBT could be that adolescents are unfamiliar with internet-based treatments in general, and, more specifically, internet-based interventions in dentistry. For that reason, they might not know what to expect from such a treatment, which could create expectations that are out of alignment with the purpose of the treatment or that are unreasonable for the treatment to achieve. Moreover, IBT might be the first time they have ever received treatment for their TMD pain, and they are thus unaware of what to expect.
Surprisingly, adolescents expected to acquire knowledge and tools. This raises questions regarding previous experiences of CBT. During interviews, it was recurrently mentioned that IBT was a psychologic treatment, and, in some cases, this was described as the reason for not expecting to become pain-free. Another question is whether the expectations of the caregiver influenced the treatment expectations of the adolescents. Because general practicing dentists were involved in the recruitment of the participants, their lack of experience in e-health interventions and interventions for chronic pain may have influenced the expectations of IBT among the adolescents. E-health interventions are not yet an established form of treatment in general dental care in Sweden; thus, general dentists have little experience with these treatments and therefore cannot yet provide accurate and informed guidance. There is evidence that interactions between the clinician and the patient enhance patient expectations47 and that the quality of the patient-clinician relationship, as well as the amount of information provided, can alter how patients view their condition and their response to treatment.48,49 Further, by communicating expectations of treatment success as a care provider, it is possible to contribute to improved functioning and decreased pain in patients through a placebo mechanism.50,51 The present findings indicate that treatment expectations are important to account for and that creating reasonable expectations among patients will improve treatment adherence and success.
Study Limitations
Qualitative content analysis, as conducted in the present study, is a common and validated qualitative method. It is purely descriptive, which constitutes a limitation since this method only allows for description of what is there and may not reveal underlying motives, which would be possible with other methods of analysis. However, the amount and depth of the data in the present study were insufficient to allow use of other methods of analysis. The limited ability of several adolescents to express themselves in depth despite further exploratory questions by the interviewer to stimulate reflection contributed to this limitation. It became evident that they lacked the language skills needed to express themselves and that they were not used to analyzing themselves. Moreover, the interviewer had limited experience in interview techniques and qualitative research methodology, which may have also affected the amount and depth of collected data.
Today, qualitative research methodology is being increasingly applied in dental contexts, and the value of this methodology is widely acknowledged. Quantitative research relies on group observations, which blinds the clinical caregiver to patient-level variations in preferences, concerns, and expectations. Qualitative research methodology is thus a necessary method of contributing to further knowledge of patient values as part of evidence-based medicine. The results and conclusions of a qualitatively designed study, however, might not be generalizable at the population level. Polit and Beck52 have tried to bring clarity to this issue and concluded that both quantitative and qualitative research have inherent difficulties that prevent an ideal generalization according to accepted models.53 Transferability is one of the proposed models of generalization, which requires collaboration between researcher and reader and is sometimes referred to as reader generalizability.54 To enable generalization through transferability, researchers need to provide “thick descriptions” to allow readers to extrapolate the findings of a study. Thick descriptions refer to rich descriptive information about the research setting, study participants, demographic information, processes, study context, and the phenomenon itself.55 In the present study, a strategic sample of participants was chosen, resulting in the inclusion of six girls and one boy; this sample was considered to be representative of the study population. Among the study participants, only one participant had discontinued IBT. Interviews with a total of seven informants was assessed as enough to meet the aim of the study and reach the principle of redundancy, which is a criterion for limiting sample size.55,56
In qualitative research, credibility is one of the quality criteria used to determine the trustworthiness of the results.57 Credibility is a measure of the plausibility or the truth of the results.55 The rigorous inductive analysis and inclusion of an adolescent who had discontinued IBT (a negative case) strengthened the credibility of the present study.58 Moreover, the use of multiple analysts to review the findings in an attempt to achieve analyst triangulation also strengthened the credibility. All authors in the present study were engaged in the inductive analysis and interpretation of the data, and results from the analytical process were repeatedly checked through reconciliation. This process reduced potential bias related to data collection by a single author and allowed for the interview data to be validated.
The authors of the current study have varying degrees of experience in qualitative research methodology, with the first author (interviewer) having the least amount. As described earlier, the first author had first met the participants as a caregiver during IBT. Credibility of the researcher (in this case, a dentist with a particular interest in the field of TMD pain among adolescents) concerns prior involvement in and knowledge of the research topic that may affect data collection, analysis, and interpretation.58 Prior knowledge of TMD pain, however, applies to two of the other study authors as well. One author (A.W.) does lack experience and knowledge in this field, but has the most comprehensive experience in qualitative research of the group. With the intention of improving credibility, the interviewer strove to restrain personal expectations and pre-understanding in order to reduce the risk of affecting the interviews and process of analysis. Pre-understanding is therefore not considered to have conflicted with the research process.
The age of the first author (25 years at the time of the interviews) and being trained in the interview technique are positive aspects of researcher credibility. The present authors believe that, despite their limitations in vocabulary, the study participants felt more at ease being interviewed by a researcher nearer their age. They most likely felt comfortable expressing their expectations and experiences in relaxed, adolescent language and did not feel the need to be concerned about more formal language. This could be compared to previous findings of difficulties experienced by adolescents with TMD pain in talking openly due to feelings of uncertainty and shyness, possibly related to the age difference between the interviewer and the adolescent and the status of the interviewer as a dentist.13 Thus, considering age and language skills when interviewing adolescents can contribute to greater depth in data and greater understanding of the investigated phenomenon.
Conclusions
Adolescents with TMD pain described their expectations and experiences of IBT, which provided greater understanding of their values, characteristics, motivation, restraints, and possible causes of the low adherence to treatment. IBT, from an adolescent perspective, can be summarized as a treatment that: aims to relieve or eliminate TMD pain; aims to improve general well-being and to provide knowledge and tools to deal with the pain; can be an ambivalent experience; and is a personal challenge.
Clinical Implications
This study explored the expectations and experiences of IBT among adolescents with TMD pain and thus contributed to one pillar of evidence-based medicine.
The study findings suggest that expectations of IBT, patient empowerment, and willingness to engage in behavioral change among adolescents need to be addressed before they enter care to promote treatment adherence and to optimize conditions for the treatment effect.
Adolescents described IBT as a personal challenge, stressing the importance of caregivers being clear about the aim of treatment and what is expected of the patients. This also implies the need to consider cognitive factors and to promote patient autonomy.
This study is a further step in developing an internet-based behavioral therapy for adolescents with TMD pain that better meets their treatment demands.
These findings can also be used in the development of other treatment programs from which adolescents may benefit.
Acknowledgments
The authors are grateful to the Regional Board of Dental Public Health in Skåne, Sweden, and to the Public Dental Service of Östergötland, Sweden (Dnr 3-17-22), for funding this study.
The authors declare no conflicts of interest. Author contributions: T.B.: acquisition of data, substantial contributions to the analysis and interpretation of data, drafting and revising the manuscript, final approval of the version to be published; EC.E.: substantial contributions to the analysis and interpretation of data, revising the manuscript, final approval of version to be published, and received grant from the Regional Board of Dental Public Health in Skåne; A.W.: substantial contributions to the design of the study, analysis and interpretation of data, revising the manuscript, and final approval of version to be published; I-M.N.: substantial contributions to the design of the study, analysis and interpretation of data, revising the manuscript, final approval of version to be published, and received grant from the Public Dental Service of Östergötland.
Funding Statement
The authors are grateful to the Regional Board of Dental Public Health in Skåne, Sweden, and to the Public Dental Service of Östergötland, Sweden (Dnr 3-17-22), for funding this study.
References
- Bor W, Dean AJ, Najman J, Hayatbakhsh R. Are child and adolescent mental health problems increasing in the 21st century? A systematic review. Aust N Z J Psychiatry. 2014;48:606–616. doi: 10.1177/0004867414533834. [DOI] [PubMed] [Google Scholar]
- Sweden Public Health Agency. Health Behaviour in School-aged Children (HBSC) WHO: 2018. Report No.: 18065. [Google Scholar]
- Sweden Public Health Agency. Why have multiple health complaints increased among children and adolescents in Sweden? Development between 1985 and 2014. WHO: 2018. Report No.: 18023–1. [Google Scholar]
- Durbeej N, Sörman K, Norén Selinus E, et al. Trends in childhood and adolescent internalizing symptoms: Results from Swedish population based twin cohorts. BMC Psychol. 2019;7:50. doi: 10.1186/s40359-019-0326-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Østerås B, Sigmundsson H, Haga M. Pain is prevalent among adolescents and equally related to stress across genders. Scand J Pain. 2016;12:100–107. doi: 10.1016/j.sjpain.2016.05.038. [DOI] [PubMed] [Google Scholar]
- Alfven G, Grillner S, Andersson E. Review of childhood pain highlights the role of negative stress. Acta Paediatr. 2019;108:2148–2156. doi: 10.1111/apa.14884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287–333. doi: 10.1016/j.ejpain.2005.06.009. [DOI] [PubMed] [Google Scholar]
- Brattberg G, Thorslund M, Wikman A. The prevalence of pain in a general population. The results of a postal survey in a county of Sweden. Pain. 1989;37:215–222. doi: 10.1016/0304-3959(89)90133-4. [DOI] [PubMed] [Google Scholar]
- Nilsson IM, List T, Drangsholt M. Prevalence of temporomandibular pain and subsequent dental treatment in Swedish adolescents. J Orofac Pain. 2005;19:144–150. [PubMed] [Google Scholar]
- List T, Wahlund K, Wenneberg B, Dworkin SF. TMD in children and adolescents: Prevalence of pain, gender differences, and perceived treatment need. J Orofac Pain. 1999;13:9–20. [PubMed] [Google Scholar]
- Nilsson IM, List T, Drangsholt M. Incidence and temporal patterns of temporomandibular disorder pain among Swedish adolescents. J Orofac Pain. 2007;21:127–132. [PubMed] [Google Scholar]
- Nilsson IM, Drangsholt M, List T. Impact of temporomandibular disorder pain in adolescents: Differences by age and gender. J Orofac Pain. 2009;23:115–122. [PubMed] [Google Scholar]
- Nilsson IM, List T, Willman A. Adolescents with temporomandibular disorder pain—The living with TMD pain phenomenon. J Orofac Pain. 2011;25:107–116. [PubMed] [Google Scholar]
- LeResche L, Mancl LA, Drangsholt MT, Huang G, Von Korff M. Predictors of onset of facial pain and temporomandibular disorders in early adolescence. Pain. 2007;129:269–278. doi: 10.1016/j.pain.2006.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Korff M, Resche LL, Dworkin SF. First onset of common pain symptoms: A prospective study of depression as a risk factor. Pain. 1993;55:251–258. doi: 10.1016/0304-3959(93)90154-H. [DOI] [PubMed] [Google Scholar]
- Grossi ML, Goldberg MB, Locker D, Tenenbaum HC. Reduced neuropsychologic measures as predictors of treatment outcome in patients with temporomandibular disorders. J Orofac Pain. 2001;15:329–339. [PubMed] [Google Scholar]
- John MT, Miglioretti DL, LeResche L, Von Korff M, Critchlow CW. Widespread pain as a risk factor for dysfunctional temporomandibular disorder pain. Pain. 2003;102:257–263. doi: 10.1016/S0304-3959(02)00404-9. [DOI] [PubMed] [Google Scholar]
- Brattberg G. Do pain problems in young school children persist into early adulthood? A 13-year follow-up. Eur J Pain. 2004;8:187–199. doi: 10.1016/j.ejpain.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Nilsson IM, List T. Does adolescent self-reported TMD pain persist into early adulthood? A longitudinal study. Acta Odontol Scand. 2020;78:377–383. doi: 10.1080/00016357.2020.1730000. [DOI] [PubMed] [Google Scholar]
- Wahlund K, List T, Larsson B. Treatment of temporomandibular disorders among adolescents: A comparison between occlusal appliance, relaxation training, and brief information. Acta Odontol Scand. 2003;61:203–211. doi: 10.1080/00016350310003891. [DOI] [PubMed] [Google Scholar]
- Litt MD, Shafer DM, Kreutzer DL. Brief cognitive-behavioral treatment for TMD pain: Long-term outcomes and moderators of treatment. Pain. 2010;151:110–116. doi: 10.1016/j.pain.2010.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlund K, Nilsson IM, Larsson B. Treating temporomandibular disorders in adolescents: A randomized, controlled, sequential comparison of relaxation training and occlusal appliance therapy. J Oral Facial Pain Headache. 2015;29:41–50. doi: 10.11607/ofph.1285. [DOI] [PubMed] [Google Scholar]
- Wahlund K, Larsson B. Long-term treatment outcome for adolescents with temporomandibular pain. Acta Odontol Scand. 2018;76:153–160. doi: 10.1080/00016357.2017.1394490. [DOI] [PubMed] [Google Scholar]
- Trautmann E, Kröner-Herwig B. A randomized controlled trial of Internet-based self-help training for recurrent headache in childhood and adolescence. Behav Res Ther. 2010;48:28–37. doi: 10.1016/j.brat.2009.09.004. [DOI] [PubMed] [Google Scholar]
- Stinson JN, Luca NJ, Jibb LA. Assessment and management of pain in juvenile idiopathic arthritis. Pain Res Manag. 2012;17:391–396. doi: 10.1155/2012/237258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo TM, Law EF, Fales J, Bromberg MH, Jessen-Fiddick T, Tai G. Internet-delivered cognitive-behavioral treatment for adolescents with chronic pain and their parents: A randomized controlled multicenter trial. Pain. 2016;157:174–185. doi: 10.1097/j.pain.0000000000000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindfors E, Hedman E, Magnusson T, Ernberg M, Gabre P. Patient experiences of therapeutic jaw exercises in the treatment of masticatory myofascial pain: A qualitative study. J Oral Facial Pain Headache. 2017;31:46–54. doi: 10.11607/ofph.1623. [DOI] [PubMed] [Google Scholar]
- Nicholas MK, Asghari A, Sharpe L, et al. Cognitive exposure versus avoidance in patients with chronic pain: Adherence matters. Eur J Pain. 2014;18:424–437. doi: 10.1002/j.1532-2149.2013.00383.x. [DOI] [PubMed] [Google Scholar]
- Voerman JS, Remerie S, Westendorp T, et al. Effects of a guided Internet-delivered self-help intervention for adolescents with chronic pain. J Pain. 2015;16:1115–1126. doi: 10.1016/j.jpain.2015.07.011. [DOI] [PubMed] [Google Scholar]
- Aggarwal VR, Fu Y, Main CJ, Wu J. The effectiveness of self-management interventions in adults with chronic orofacial pain: A systematic review, meta-analysis and meta-regression. Eur J Pain. 2019;23:849–865. doi: 10.1002/ejp.1358. [DOI] [PubMed] [Google Scholar]
- Burnard P. A method of analysing interview transcripts in qualitative research. Nurse Educ Today. 1991;11:461–466. doi: 10.1016/0260-6917(91)90009-y. [DOI] [PubMed] [Google Scholar]
- Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62:107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the international RDC/TMD consortium network* and orofacial pain special interest group. J Oral Facial Pain Headache. 2014;28:6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson IM, Willman A. Treatment seeking and self-constructed explanations of pain and pain management strategies among adolescents with temporomandibular disorder pain. J Oral Facial Pain Headache. 2016;30:127–133. doi: 10.11607/ofph.1450. [DOI] [PubMed] [Google Scholar]
- Stinson JN, Lalloo C, Harris L, et al. iCanCope with pain: User-centred design of a web- and mobile-based self-management program for youth with chronic pain based on identified health care needs. Pain Res Manag. 2014;19:257–265. doi: 10.1155/2014/935278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino MJ, Arnkoff DB, Glass CR, Ametrano RM, Smith JZ. Expectations. J Clin Psychol. 2011;67:184–192. doi: 10.1002/jclp.20754. [DOI] [PubMed] [Google Scholar]
- Crushell E, Rowland M, Doherty M, et al. Importance of parental conceptual model of illness in severe recurrent abdominal pain. Pediatrics. 2003;112:1368–1372. doi: 10.1542/peds.112.6.1368. [DOI] [PubMed] [Google Scholar]
- Guite JW, Kim S, Chen CP, et al. Pain beliefs and readiness to change among adolescents with chronic musculoskeletal pain and their parents before an initial pain clinic evaluation. Clin J Pain. 2014;30:27–35. doi: 10.1097/AJP.0b013e31828518e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risling T, Martinez J, Young J, Thorp-Froslie N. Evaluating patient empowerment in association with ehealth technology: Scoping review. J Med Internet Res. 2017;19:e329. doi: 10.2196/jmir.7809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan DE, Conroy C, Sieberg CB, Simons LE. Changes in willingness to self-manage pain among children and adolescents and their parents enrolled in an intensive interdisciplinary pediatric pain treatment program. Pain. 2012;153:1863–1870. doi: 10.1016/j.pain.2012.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenhard F, Vigerland S, Engberg H, Hallberg A, Thermaenius H, Serlachius E. “On my own, but not alone”—Adolescents’ experiences of internet-delivered cognitive behavior therapy for obsessive-compulsive disorder. PLoS One. 2016;11:e0164311. doi: 10.1371/journal.pone.0164311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanstrup M, Jordan A, Kemani MK. Adolescent and parent experiences of acceptance and commitment therapy for pediatric chronic pain: An interpretative phenomenological analysis. Children (Basel) 2019;6:101. doi: 10.3390/children6090101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhelmsen M, Lillevoll K, Risør MB, et al. Motivation to persist with internet-based cognitive behavioural treatment using blended care: A qualitative study. BMC Psychiatry. 2013;13:296. doi: 10.1186/1471-244X-13-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cormier S, Lavigne GL, Choinière M, Rainville P. Expectations predict chronic pain treatment outcomes. Pain. 2016;157:329–338. doi: 10.1097/j.pain.0000000000000379. [DOI] [PubMed] [Google Scholar]
- Goldstein AP. Patient’s expectancies and non-specific therapy as a basis for (un) spontaneous remission. J Clin Psychol. 1960;16:399–403. doi: 10.1002/1097-4679(196010)16:4<399::aid-jclp2270160416>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Noble LM, Douglas BC, Newman SP. What do patients expect of psychiatric services? A systematic and critical review of empirical studies. Soc Sci Med. 2001;52:985–998. doi: 10.1016/s0277-9536(00)00210-0. [DOI] [PubMed] [Google Scholar]
- Di Blasi Z, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: A systematic review. Lancet. 2001;357:757–762. doi: 10.1016/s0140-6736(00)04169-6. [DOI] [PubMed] [Google Scholar]
- Goossens ME, Vlaeyen JW, Hidding A, Kole-Snijders A, Evers SM. Treatment expectancy affects the outcome of cognitive-behavioral interventions in chronic pain. Clin J Pain. 2005;21:18–26. doi: 10.1097/00002508-200501000-00003. [DOI] [PubMed] [Google Scholar]
- Horvath P. Treatment expectancy as a function of the amount of information presented in therapeutic rationales. J Clin Psychol. 1990;46:636–642. doi: 10.1002/1097-4679(199009)46:5<636::aid-jclp2270460516>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Bensing JM, Verheul W. The silent healer: The role of communication in placebo effects. Patient Educ Couns. 2010;80:293–299. doi: 10.1016/j.pec.2010.05.033. [DOI] [PubMed] [Google Scholar]
- Finniss DG, Benedetti F. Mechanisms of the placebo response and their impact on clinical trials and clinical practice. Pain. 2005;114:3–6. doi: 10.1016/j.pain.2004.12.012. [DOI] [PubMed] [Google Scholar]
- Polit DF, Beck CT. Generalization in quantitative and qualitative research: Myths and strategies. Int J Nurs Stud. 2010;47:1451–1458. doi: 10.1016/j.ijnurstu.2010.06.004. [DOI] [PubMed] [Google Scholar]
- Firestone WA. Alternative arguments for generalizing from data as applied to qualitative research. Educ Res. 1993;22:16–23. [Google Scholar]
- Misco T. The frustrations of reader generalizability and grounded theory: Alternative considerations for transferability. J Res Pract. 2007;3:1–11. [Google Scholar]
- Lincoln YS, Guba EG. Naturalistic Inquiry. ed 1. Beverly Hills, California: Sage; 1985. [Google Scholar]
- Patton MQ. Qualitative Research and Evaluation Methods. ed 3. Thousand Oaks, California: Sage; 2001. [Google Scholar]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Serv Res. 1999;34:1189–1208. [PMC free article] [PubMed] [Google Scholar]