Abstract
Aims:
To perform a scoping review of the literature to elucidate the occurrence of nerve damage related to dental implant placement and the factors causing the sensory changes.
Methods:
An extensive electronic search was conducted using the Cochrane Library, Medline via Ovid, PubMed, Wiley Online, Science Direct, CINAHL, and the Google Scholar databases from the year 1950 to 2020.
Results:
The search resulted in 1,067 articles, out of which 76 were selected for this review. The articles were categorized as literature review articles, retrospective studies, prospective studies, and case series/case reports. Altogether, 2,526 subjects were assessed retrospectively, with 5.27% transient and 1.39% persistent sensory changes, and a cohort of 2,750 subjects were followed prospectively, with 6.22% transient and 1.31% persistent sensory changes. A total of 336 subjects were enrolled in various case reports and case series, with 5.95% transient sensory changes and 84.52% persistent neurosensory changes. The articles included were not of high quality and have variations in their study designs and reporting procedures, with limited sensory change data to include in this study.
Conclusion:
After surgical placement of dental implants in 5,612 patients, the incidence of transient sensory changes was 5.63%, and the incidence of persistent sensory changes was 6.33%. Factors affecting the incidence were: mandibular location of the implant, with the inferior alveolar nerve as the most commonly affected nerve. The common symptoms reported were paresthesia and dysesthesia. Age and gender were among other factors, for which data were not available in all the articles. J Oral Facial Pain Headache 2022;36:165–186. doi: 10.11607/ofph.3027
Keywords: dental implants, sensory changes, transient and permanent, trigeminal neuropathy
Dental implants have become a common mode of treatment for the replacement of missing dentition.1,2 Though the clinical restorative success rate is very good,3 the neurologic complications associated with dental implant placement have not been clearly described in the literature.4 Goodacre et al5 performed a systematic review analysis with 217 articles from 1981 to 2001. After collecting clinical data on the success and failure rates of dental implants and listing the associated complications, the review concluded that, among the most acute complications associated with the surgical placement of dental implants, neurosensory disturbances rated as high as 39% and as low as 0.6%, with a mean of 6.1% after one-stage implant surgery.6 Berglundh et al7 published a systematic review in 2002 including articles with a 5-year follow-up period and found that, in the studies included, the incidence of sensory disturbance was 41%. In 1% to 2% of cases, these disturbances persisted for more than a year after dental implant surgery. In 2008, Greenstein et al8 detailed the surgical complications while placing dental implants and recommended steps to avoid and manage them. Lamas Pelayo et al9 performed a Medline search in 2008 for intraoperative complications during dental implant placement and found that nerve damage was the second most common acute complication after hemorrhage, which can become persistent if left untreated. Most of the literature available previously does not delineate between painful and nonpainful transient and persistent sensory changes.10
There is a wide discrepancy and inconsistent data on the incidence and characterization of sensory changes and pain caused due to surgical placement of dental implants in the literature.4 During the surgical placement of dental implants, nerve injury can occur at any stage; ie, while administering the local anesthetic, during or after implant surgery, or during insertion of the implant. Neural damage can either occur due to direct mechanical injury to the nerve (ie, during the osteotomy or implant placement) or indirectly due to the inflammatory response in surrounding tissues following the surgery.11 Crush-type injuries can occur or compartment syndrome can affect the inferior alveolar nerve due to the nature of the nerve’s anatomy.12 Perineural inflammation along the nerve trunk with no frank axonal damage is sufficient to induce pain in an organ innervated by the affected nerves.13 Depending on the degree of nerve damage, altered sensations and/or pain can occur.12 These sensory changes can vary from being transient to permanent. Nonpainful sensory changes may present with signs such as paresthesia and/or anesthesia, whereas painful sensory changes may pre-sent with signs such as allodynia and hyperalgesia in addition to the signs of nonpainful sensory changes.11 The literature reports 4% to 8% incidence of residual long-term neurosensory disturbances, such as inferior alveolar nerve paresthesia.14,15 In many instances, there is a reduction in these symptoms as time progresses. According to a retrospective review by Goodacre et al,6 neurosensory impairments reduced from 7% to 1–2% after the elapse of the first year. However, a few other prospective studies16–18 provide a range from 0% to 13% for the incidence of long-term neurosensory alterations. This wide-ranged discrepancy may be due to numerous factors, including variability in surgical techniques, the type of surgery performed, the proximity to the nerve canal, the psychologic status of the patient, and most important, lack of documentation and skill in evaluating neurosensory function.19
This study aims to perform a scoping review of the literature to elucidate the incidence of and factors affecting the transient and persistent sensory changes after dental implant placement in order to map the research done in this area and to identify any existing gaps in knowledge, which will pave the way for future systematic reviews on this topic.20
Materials and Methods
The inclusion criteria were as follows: articles published from 1950 to 2020, with no language restrictions, only human studies, and any study design, including meta-analysis, systematic review, non/randomized clinical trial, cohort, case-control, prospective, retrospective, literature review, case report, and case series.
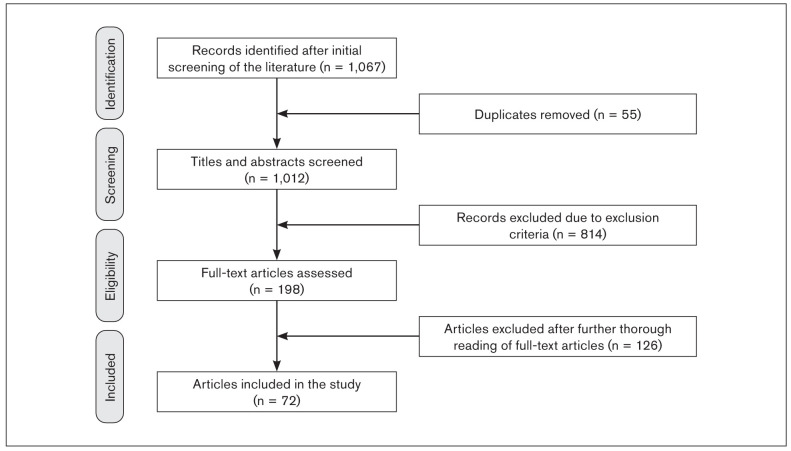
Although the present study is not a systematic review, the PRISMA-ScR methodology was followed (see checklist Fig 1) to conduct this scoping review.20,21 A scoping review is a newer approach for gathering evidence and is different from a systematic review. A scoping review is a useful tool to identify research gaps and summarize the qualitative findings of the available research.22–25 Assessment of risk of bias is required for a systematic review but is not mandatory for a scoping review. A scoping review is less rigorous and can be a prerequisite to doing a systematic review. A scoping review informs us what the gap in knowledge is and whether it is necessary to do a systematic review on the subject.
Fig 1.

PRISMA-Scr protocol.
The use of the present scoping review protocol was attempted in the Cochrane Library; however, its strict guidelines failed to identify any articles. Extensive electronic searches of the Cochrane Library, Medline, PubMed, and Science Direct, Springer link, Wiley online library, CINAHL (Cumulative Index to Nursing and Allied Health Literature), and Google Scholar databases were conducted with no language barrier from the years 1950 to 2020. The Boolean search method was used for the following keywords: dental implants; sensory changes; altered sensations; paresthesia; neurosensory disturbances; neuropathy; and trigeminal neuropathy.
Introduction
With the limited and conflicting data available, an attempt was made to perform a critical overview of available publications and research to reach valid conclusions on the incidence of transient (less than 3 months) and persistently altered (3 or more months) sensations following surgical placement of dental implants. This is the cutoff point used in the literature to demarcate the transition between acute and chronic pain,26 and the authors decided to use the same cutoff point for the demarcation between transient and persistent sensory changes, though a recent meta-analysis reported short-term sensory changes lasting up to 10 days following implant placement, intermediate altered sensations lasting from 3 to 6 months, and persistent sensory changes 1 year after implant placement.27
The exclusion criteria were as follows: animal studies, articles reporting neurosensory disturbances following any other invasive surgical procedures, and articles reporting sensory disturbances due to prostheses following dental implant placement. If information was available on chronic pain (3 or more months) after dental implant placement, it was included.
For the data collection process, the preliminary search included literature on any database or internet source with the key terms and without any language restrictions. Research articles, literature reviews, case reports, scientific posters, and published chapters in books, dissertations, and websites were reviewed.
The online searches resulted in: sensory changes with dental implants (29,100 results); dental implant neuropathy (19,900 results); paresthesia with dental implants (7,510 results); pain with dental implants (120,000 results); neurosensory disturbances after dental implant (10,700 results); and trigeminal neuropathy (51,100 results).
An overview of the entire search provided 1,067 articles. Around 55 duplicates were found, and the remaining 1,012 abstracts were screened. Of these, 814 articles were excluded, resulting in 198 articles with abstracts and full texts. After a further thorough reading of the full-text articles, 126 articles were excluded because of lack of exclusivity of transient or persistent sensory changes after dental implant placement in patients. Finally, 72 articles were included in this study. The PRISMA flow diagram was used to obtain the information through the different phases of this scoping review (Fig 2).
Fig 2.
Flowchart showing study inclusion process.
The literature review articles reveal that numerous reviews have been performed in the past; however, none provide an accurate report on the incidence of long-term sensory alterations after dental implant placement with predefined inclusion criteria. Therefore, out of the 72 articles included in this scoping review, further categorization was based on the study design: 30 literature reviews (Table 1); 7 retrospective studies (Table 2); 12 prospective studies (Table 3); and 23 case reports and case series (Table 4).
Table 1.
Literature Review Articles
| Author | Year | Journal | Methods, Results, and Conclusions |
|---|---|---|---|
| Padmanabhan et al37 | 2020 | Journal of Indian Prosthodontic Society |
|
| Carter et al42 | 2016 | British Dental Journal |
|
| Lin et al27 | 2016 | PLoS One |
|
| Al-Sabbagh et al19 | 2015 | Dental Clinics of North America |
|
| Jacobs et al43 | 2014 | Periodontology 2000 |
|
| Dannan44 | 2013 | The Internet Journal of Dental Science |
|
| Juodzbalys et al45 | 2013 | Clinical Oral Implants Research |
|
| Renton46 | 2013 | British Dental Journal |
|
| Tinastepe and Oral47 | 2013 | Ağri |
|
| Greenwood and Corbett48 | 2012 | Chapter in: Dental Emergencies |
|
| Palma-Carrió et al49 | 2011 | Medicina Oral, Patologia Oral, y Cirugia Bucal |
|
| Juodzbalys et al30 | 2011 | Journal of Oral & Maxillofacial Research |
|
| Siqueira and Siqueira50 | 2011 | Revista Dor |
|
| Sánchez Garcés et al51 | 2011 | Chapter in: Implant Dentistry. The Most Promising Discipline of Dentistry |
|
| Kim52 | 2011 | Chapter in: Implant Dentistry. A Rapidly Evolving Practice |
|
| Alhassani and AlGhamdi53 | 2010 | Journal of Oral Implantology |
|
| Moore and Haas54 | 2010 | Dental Clinics of North America |
|
| Renton55 | 2010 | Dental Update |
|
| Lamas Pelayo et al9 | 2008 | Medicina Oral, Patologia Oral, y Cirugia Bucal |
|
| Misch and Wang56 | 2008 | Implant Dentistry |
|
| Greenstein et al8 | 2008 | Journal of Periodontology |
|
| Peñarrocha et al57 | 2007 | Oral Diseases |
|
| Greenstein and Tarnow58 | 2006 | Journal of Periodontology |
|
| Hegedus and Diecidue59 | 2006 | International Journal of Oral & Maxillofacial Implants |
|
| Worthington60 | 2004 | International Journal of Oral Maxillofacial Implants |
|
| Goodacre et al5 | 2003 | Journal of Prosthetic Dentistry |
|
| Mraiwa et al61 | 2003 | Clinical Implant Dentistry & Related Research |
|
| Gregg14 | 2000 | Annals of the Royal Australasian College of Dental Surgeons |
|
| Dao and Mellor12 | 1998 | International Journal of Prosthodontics |
|
| Vallerand62 | 1992 | New York State Dental Journal |
|
Table 2.
Retrospective Research Articles
| Author | Year | Title | Journal | Study design | Enrolled subjects for dental implant surgeries |
Gender/age | Location | Subjects with altered sensation |
Tests performed | Symptoms | Duration of symptoms |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Vázquez-Delgado et al10 | 2018 | Prevalence of neuropathic pain and sensory alterations after dental implant placement in a university-based oral surgery department: A retrospective cohort study | Gerodontology | Retrospective cohort study; clinical files from patients submitted to dental implant placement between February 2004 and September 2014 in the Oral Surgery and Implantology Master degree program of the Faculty of Dentistry of the University of Barcelona (Spain) | 1,156 patients, of which 1,012 met the study inclusion criteria | 417 men (41.2%) and 595 women (58.8%) Mean age 60.7 y (16–90 y) |
Maxilla, mandible, and intermental implant placements | 3 patients were diagnosed as having PPTN, which corresponds to a prevalence of 0.3% (95% CI: 0%–0.6%). Additionally, 5 patients (0.5%; 95% CI: 0%–1.07%) presented TNWP. The combined prevalence of both disorders was 0.8% (95% CI: 0.02%–1.3%). | Sensory alterations were assessed according to the Guidelines of the International Taskforce on Somatosensory Testing of the IASP SIG-OFP (IASP): pinprick testing of the affected zone, thermal stimulation, von Frey filaments evaluation, directional discrimination, two-point discrimination, and finally subjective evaluation by the patient. | Patients with the diagnosis of painful PTTN according to diagnostic criteria of the ICHD-3 beta; paresthesias, hypoesthesia | Follow-up appointments lasted until the medical condition resolved or until it was considered stable in time (ie, permanent paraesthesia after a 12- to 14-month follow-up period). |
| Scarano et al63 | 2017 | Neurosensory disturbance of the inferior alveolar nerve after 3,025 implant placements | Implant Dentistry | Retrospective study; patients enrolled between February 2004 and July 2015. | 1,065 patients | No gender prevalence mentioned in the study; mean age 58.9 y | Patients with partial or complete mandibular edentulism were selected to receive dental implants for oral rehabilitation. | Only 23 (2.2%) of the 1,065 patients presented with sensitivity disturbances 1 month after implant placement, and only 2 (0.19%) after 6 months, though a complete recovery was observed in these patients within 13 months. | Sensitivity (thermal, tactile, pain) was evaluated on the first recall, and patients with IAN sensory disturbances were recalled at intervals of 1, 3, and 6 months after implant placement. | Sensitivity disturbances | 10 days after implant surgery and repeated at intervals of 1, 3, and 6 months up to 13 months |
| Deppe et al64 | 2015 | Trigeminal nerve injuries after mandibular oral surgery in a university outpatient setting—A retrospective analysis of 1,559 cases | Clinical Oral Investigation | Retrospective analysis from January 2000 to December 2009 | 48 patients had dental implant surgery | NA | Mandibular post-canine region | 2 patients (4.1%); alveolar nerve injuries | Clinical tests performed with 3 months of follow-up | Hypoesthesia Anesthesia | Not significant after a year |
| KÜtÜk et al65 | 2013 | Anterior mandibular zone safe for implants | Journal of Craniofacial Surgery | Retrospective clinical study 2007 to 2012 | 55 | 9 women, 1 man | Mandibular canine region | 1,019 dental implants were placed | Dental volumetric CT scans; mechano-receptive test to determine neurosensory changes | Tingling, burning in 8 patients (80%); throbbing in 2 patients (20%); continuous pain in all patients: unilateral (90%), bilateral (10%) | 1 mo in 50%; 6 mo in 10%; 24 mo in 10%; continued in 30% |
| Kwon et al66 | 2004 | The prevalence of sensory disturbance after implant surgery—Retrospective survey of implant practitioners | Journal of the Korean Association of Oral and Maxillofacial Surgeons | Retrospective | 47 | NA | N/A | Inferior alveolar nerve damage was seen in 45%; 21 cases (61%) were found with a sensory disturbance, which recovered in 6 months, except for 2 cases where sensory disturbance persisted | NA | Dysesthesia Anesthesia Hyperesthesia Hypoesthesia | Sensory disturbance recovered in 6 mo, except for 2 cases where sensory disturbance persisted. |
| Ellies and Hawker17 | 1993 | The prevalence of altered sensation associated with implant surgery | International Journal of Oral & Maxillofacial Implants | Retrospective questionnaire analysis | 112 | 64 women, 36 men; mean age 57 y | Mandible | Altered sensation was reported by 36%, with 23% of them having transient changes and 13% experiencing permanent changes | Restrospective questionnaire | Numbness/ paresthesia was the most common complaint in almost all patients. | 5-year data collected |
| Ellies16 | 1992 | Altered sensation following mandibular implant surgery: A retrospective study | Journal of Prosthetic Dentistry | Retrospective questionnaire study | 226 | NA | Mandible | 37% reported altered sensations, with 28% having transient sensory changes and 8% reporting long-term sensory changes; higher changes were reported in women. | Questionnaire study; 80% responded | NA | 27 (13%) patients experienced altered sensation within 3 mo, and 17 (8%) patients experienced persistent changes more than 3 mo |
IASP = International Association for the Study of Pain; ICHD = International Classification of Headache Disorders; PTTN = painful posttraumatic neuropathy; SIG-OFP = Special Interest Group of Orofacial Pain; TNWP = trigeminal neuropathy without pain.
Table 3.
Prospective Research Articles
| Author | Year | Title | Journal | Study design | Enrolled subjects for dental implant surgeries/implants, n |
Gender/age | Location | Subjects with altered sensation |
Test(s) performed | Symptoms | Duration of symptoms |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hartmann et al67 | 2017 | Neurophysiological changes associated with implant placement | Clinical Oral Implants Research | Prospective with follow-up of 9 y | 33/NA | 17 men, 16 women; median 58 y (28–80 y) | Maxilla, mandible | 1 | Mechanical and thermal QST on implant vs control side at chin and lower lip | Abnormal sensory responses to touch coexisting with numbness and temperature algesia | Followed up for 9 y; 1 patient presented late for initial evaluation; loss in MDT and VDT, with a gain in sensitization for pain were experienced by 1 patient for 9 y |
| Vazquez et al38 | 2008 | Efficacy of panoramic radiographs in the preoperative planning of posterior mandibular implants: A prospective clinical study of 1,527 consecutively treated patients | Clinical Oral Implants Research | Prospective clinical study of 1,527 consecutively treated patients | 1,527/2,584 consecutively placed | 890 women and 637 men; aged from 17 to 86 y (mean age 53 y) | Posterior segment of the completely edentulous mandible | 2 | A panoramic radiograph was the only preoperative imaging technique used to determine the incidence of altered mental nerve sensation after implant placement in the posterior segment of the mandible. | Temporary paresthesia | Lasted 3 and 6 wk; resolved spontaneously |
| Abarca et al69 | 2006 | Neurosensory disturbances after immediate loading of implants in the anterior mandible: An initial questionnaire approach followed by a psychophysical assessment | Clinical Oral Investigations | Prospective study to assess past and present neurosensory disturbances using a questionnaire and a psychophysical approach in patients treated with three immediate loaded implants in edentulous anterior mandible | 65/NA | 30 women, 35 men/30–84 y | Anterior mandible; all of them treated with 3 immediately loaded implants | 58 completed the questionnaire; 19 (33%) reported neurosensory disturbance after surgery; of these, 11 patients had less than 3 mo of disturbance, and the remaining 8 still complained of neurosensory disturbance | Questionnaire and psychophysical testing: 2-point discrimination test, light touch, thermal sensitivity | Most common sites affected: inferior lip, gingiva, chin Symptoms: numbness (9 patients), followed by cutting, beating, itching (2 patients) | Sensory disturbance lasted for 8 and 21 mo for the 8 patients. |
| Kubilius et al70 | 2004 | Traumatic damage to the inferior alveolar nerve sustained in course of dental implantation. Possibility of prevention | Stomatologija | Prospective; tactile and pain sensitivity thresholds determined during first 2 d of implantation, then 7, 14, 28, 45, 60, 90 d, followed by 1 to 2 y | 383/11,152 | 137 women, 246 men | Mandible | 68 (17.755%) suffered from inferior alveolar nerve damage after dental implant placement | Sensographic method used to detect tactile and pain sensitivity thresholds | 38 (9.92%) with mild IAN transient damage had predominant paresthesia; 27 (7.05%) with moderate IAN transient damage exhibited paresthesia; 3 (0.78%) with severe persistent IAN damage experienced hyperesthesia | Follow-up to 45 d postoperation and follow-up to 2 y |
| El-Sheikh et al71 | 2003 | Changes in passive tactile sensibility associated with dental implants following their placement | International Journal of Oral & Maxillofacial Implants | Prospective study to investigate the changes in passive tactile sensibility for a period of 3 mo following implant surgery | 5/10 (2 each) | 2 women, 3 men/56–78 y | Anterior mandible | NA | Measurement of force applied with a custom device | Significant increase in passive tactile sensitivity during 3 mo in subjects treated with immediate loading of implants | Follow-up to 3 mo after surgery |
| Walton72 | 2000 | Altered sensation associated with implants in the anterior mandible: A prospective study | Journal of Prosthetic Dentistry | Prospective study; objective and subjective tests performed before implant surgery and at planned intervals for 12 mo following surgery | 75/NA | 47 women, 28 men/40–87 y | Anterior mandible | 24% reported altered sensation in anterior mandible in the short term; with only 1% reporting changes 1 y after surgery | Objective and subjective tests | Numbness and tingling of lower lip | Follow-up to 12 mo after surgery |
| Bartling et al18 | 1999 | The incidence of altered sensation of the mental nerve after mandibular implant placement | Journal of Oral & Maxillofacial Surgery | Prospective study to determine the incidence of altered sensation; neurologic testing followed up until 6 mo, or later until the altered sensation resolved after the implant surgery | 94/405 | 43 women, 51 men | Mandible | 8 patients (8.5%) reported altered sensation in the postoperative visit | Subjective assessment and neurologic testing | Paresthesia, anesthesia Most of these patients had a large number of implants placed, but the altered sensations returned to normal in all of them by 121 d following implant placement. | Follow-up to 6 mo after surgery |
| Wismeijer et al73 | 1997 | Patients’ perception of sensory disturbances of the mental nerve before and after implant surgery: A prospective study of 110 patients | British Journal of Oral & Maxillofacial Surgery | Prospective randomized controlled clinical trial: Patient perception of sensation of lower lip before surgery, 10 d later, and 16 mo after implant surgery | 110/NA | 76 women, 34 men; 30–80 y | Mandible | Considering a 3-mm safety margin around the mental foramen, the study still showed 7% sensory disturbance in the lower lip | Questionnaire | 26 (25%) had altered sensation of lower lip before surgical procedure; 11 (11%) at 10 d, and 10 (10%) had altered sensation of lower lip 16 mo following surgery | Follow -to 16 mo postsurgery |
| Higuchi et al15 | 1995 | Implant survival rates in partially edentulous patients: A 3-year prospective multicenter study | Journal of Oral and Maxillofacial Surgery | Prospective study | 139/460 | NA/15–80 y | Maxilla, mandible | NA | Questionnaire, 80% responded | 4% paresthesia of inferior alveolar nerve was reported | Follow-up to 5 y |
| Johns et al74 | 1992 | A multicenter study of overdentures supported by Brånemark implants | The International Journal of Oral & Maxillofacial Implants | Prospective study with 9 clinical centers with 1-y follow-up | 133/117 in maxilla, 393 in mandible | 59 women, 74 men/ 32–75 y | Maxilla, mandible | NA | Multicenter study involving 9 clinical centers, clinical and radiologic exams | 19 patients suffered from paresthesia after mandibular implant surgery; 16 of these recovered by the time of prosthesis placement | In 1 patient, paresthesia still existed 1 y later. |
| Kiyak et al76 | 1990 | The psychological impact of osseointegrated dental implants | The International Journal of Oral & Maxillofacial Implants | Prospective longitudinal questionnaire study; assessed before and after until 18 mo after surgery | 39, but a total of 27 completed the study/NA | 79.5% women, 19.5% men; 36–78 y | NA | 4.3% experienced facial paresthesia at first-stage surgery; later, 43.5% reported experience at second stage, but none reported persistent sensory changes | Questionnaire | Paresthesia | Follow-up to 14–18 mo |
| van Steenberge et al77 | 1990 | The applicability of osseointegrated oral implants in the rehabilitation of partial edentulism: A prospective multicenter study on 558 fixtures | The International Journal of Oral & Maxillofacial Implants | Prospective study with 9 clinical centers; with follow-up visits after 1 wk, 1 mo, 6 mo, and 12 mo; patients will be evaluated after 24, 36, 48, and 60 mo following prosthesis placement | 154/558; 68 in maxilla, 91 in mandible (521 completed the study) | NA/15–80 y | Maxilla, mandible | 16 patients complained of transient paresthesia of lower lip; 1 year after prosthesis placement, 6 patients still complained of persistent paresthesia | Clinical exam | Paresthesia of the lower lip | Follow-up to 12 mo; then later to 60 mo after prosthesis placement |
QST = quantitative sensory testing; IAN = inferior alveolar nerve; MDT = mechanical detection threshold; VDT = vibration detection threshold.
Table 4.
Case Reports and Case Series
| Author | Year | Title | Journal | Enrolled subjects for dental implant surgeries |
Gender | Age | Tooth number(s) restored, (number of implants) |
Symptoms | Duration post injury | Pain level (0–10 VAS) |
|---|---|---|---|---|---|---|---|---|---|---|
| Politis et al40 | 2017 | Report of neuropathic pain after dental implant placement: A case series | International Journal of Oral & Maxillofacial Implants | 26 | NA | NA | Mandibles of 18 patients, 6 received regular implants and 2 received a zygomatic implant in the maxilla | 17 developed pain due to implant placement, 9 developed pain with unknown cause | 12 mo | NA |
| Devine et al41 | 2016 | Chronic post-surgical pain following the placement of dental implants in the maxilla: A case series | European Journal of Oral Implantology | 10 | 9 women, 1 man | Average 55.4 y | 6 patients had single implants placed, 4 had multiple implants | Onset of pain was immediate in 9 patients with constant pain | NA | Pain intensity ranged from 2 to 9 (average 5.6) |
| Du Toit et al78 | 2015 | Implant injury case series and review of the literature part 1: Inferior alveolar nerve injury | Journal of Oral Implantology | 4 | Woman Woman Woman Man |
42 yr 33 y 27 y 43 y |
29, 30 (2) 29, 30 (2) 29, 30 (2) 29, 30 (2) |
Paresthesia Anesthesia Paresthesia Paresthesia |
8 wk NA 3 mo 12 mo |
NA |
| Givol et al79 | 2013 | Inferior alveolar neurosensory deficiency associated with placement of dental implants | Journal of Periodontology | 92 | 58 women | 27–89 y | NA | NA | More than 5 y | Pain level not available |
| Mourào et al80 | 2013 | Role of homeopathy in post-surgical dental implants paresthesia–A case report | Journal of Case Studies in Homeopathy | 1 | Man | 63 y | 18, 24, 25 (3) | Paresthesia | 12 mo | 3 |
| Wright81 | 2011 | Persistent dysesthesia following dental implant placement: A treatment report of 2 cases | Implant Dentistry | 2 | Man Woman |
56 y 66 y |
14 (1) 24 (4) |
Dysesthesia Dysesthesia |
28 mo 36 mo |
3 7 |
| Stamatin et al82 | 2011 | Post-implant neurological complications in the horizontal mandibular arch | International Journal of Medical Dentistry | 27 | Woman Woman |
54 y 44 y |
21 (1) 21 (1) |
Paresthesia Paresthesia |
NA | Disappeared after 6 wk Disappeared after 3 wk |
| Al-Ouf and Salti83 | 2011 | Post-insertion pain in region of mandibular dental implants: A case report | Implant Dentistry | 1 | Woman | 27 y | 19, 20 (2) | Dysesthesia | NA | Implant removal reduced pain |
| Yoon et al84 | 2010 | Use of botulinum toxin type A injection for neuropathic pain after trigeminal nerve injury | Pain Medicine | 1 | Woman | 62 y | 23, 24, 25, 26 (4) | Dysesthesia, allodynia, paresthesia | 2 mo | NA |
| Rodriguez-Lozano et al85 | 2010 | Neuropathic orofacial pain after dental implant placement: Review of the literature and case report | Oral Surgery, Oral Medicine, Oral Pathology Oral Radiology, & Endodontics | 1 | Woman | 62 y | Maxilla (8) | Dysesthesia, allodynia | 8 mo | NA |
| Leckel et al86 | 2009 | Neuropathic pain resulting from implant placement: Case report and diagnostic conclusions | Journal of Oral Rehabilitation | 1 | Man | 56 y | 19, 20 (2) | Dysesthesia | 17 mo | Pain free after removal of one implant |
| Khawaja and Renton87 | 2009 | Case studies on implant removal influencing the resolution of inferior alveolar nerve injury | British Dental Journal | 4 | Woman Woman Woman Woman |
55 y 56 y 46 y 39 y |
30 (2) Mandibular quadrant of partial denture 19 (1) Mandibular left and right quadrants for a mandiblar implant partial denture 20 (1) 29 (1) |
Paresthesia of lower lip and chin Paresthesia Paresthesia, mechanical allodynia, dysesthesia Paresthesia, mechanical allodynia Paresthesia of right lower lip |
Numbness immediately after surgery until implant was removed 18 h after surgery; one of the implants was removed 24 h postsurgery; implant removed 2 days later; implant removed 4 days later | Decrease in symptoms 3 mo later Decrease in symptoms at 2-mo follow-up No improvement in symptoms at 3-mo follow-up No improvement |
| Liang et al88 | 2008 | Neurovascular disturbance associated with implant placement in the anterior mandible and its surgical implications: Literature review including report of a case | Chinese Journal of Dental Research | 1 | Woman | 61 y | Mandibular arch (4) | Paresthesia, dysesthesia | NA | NA |
| Elian et al89 | 2005 | Unexpected return of sensation following 4.5 years of paresthesia: Case report | Implant Dentistry | 1 | Man | 34 y | 19, 20, 29, 30 (4) | Paresthesia | NA | Pain reduced after implant removal |
| Flanagan90 | 2002 | Delayed onset of altered sensation following dental implant placement and mental block local anesthesia: A case report | Implant Dentistry | 1 | Woman | 45 y | 20 (1) | Paresthesia | Pain started 4 mo after surgery | Pain free 17 mo later |
| Gregg14 | 2000 | Neuropathic complications of mandibular implant surgery: Review and case presentation | Annals of the Royal Australasian College of Dental Surgeons | 2 | Woman Man |
45 y 50 y |
Right mandibular body (2) Mandible |
Paresthesia Dysesthesia, mechanical allodynia, hyperalgesia |
3 mo to more than 1 y 1 y |
NA |
| *Kim et al91 | 2013 | Clinical outcome of conservative treatment of injured inferior alveolar nerve during dental implant placement | Journal of the Korean Association of Oral and Maxillofacial Surgeons | 64 | 35 women 29 men |
NA | Posterior mandible | 6 anesthesia 28 hypoesthesia and paresthesia 17 hypoesthesia 13 dysesthesia | 3 had transient sensory changes, whereas 54 had persistent sensory changes | NA |
| *Juodzbalys et al45 | 2013 | Inferior alveolar nerve injury associated with implant surgery | Clinical Oral Implants Research | 16 | 8 women 8 men |
36–65 y | Right and left premolar, molar region in the mandible | 5 hyperalgesia 11 hypoalgesia |
More than 3 mo for 11 subjects | NA |
| *Renton et al39 | 2012 | Post-implant neuropathy of the trigeminal nerve. A case series | British Dental Journal | 30 | 20 women 10 men |
26–80 y | Mandibular second premolar, molar | Paresthesia in 47% of cases; mechanical/,thermal allodynia 30%; anesthesia 40% Functional disabilities: Kissing 54%, speech 46%, eating, drinking, brushing teeth due to pain 30% Recurrent lip biting 23% Dribbling 33% Psychologic problems 30% |
NA | NA |
| *Tay and Zuniga94 | 2007 | Clinical characteristics of trigeminal nerve injury referrals to a university center | The International Journal of Oral & Maxillofacial Surgery | 59 patients included in the study, but only 7 (11%) were related to implant procedures | 5 women, 2 men | 17–27 y | NA | 7 patients had at least one functionality problem; 3 mild sensory impairment; 2 moderate; 2 with no deficit | NA | NA |
| *Libersa et al95 | 2007 | Neurosensory disturbances of the inferior alveolar nerve: A retrospective study of complaints in 10 years | Journal of Oral & Maxillofacial Surgery | 382 subjects were included, and 12 were related to dental implant placement | Prospective longitudinal questionnaire study; assessed before, after up to 18 mo after surgery | NA | IAN | 3 (1%) were transient; 9 (12%) with permanent neurosensory disturbances | NA | NA |
| *Hillerup96 | 2007 | Iatrogenic injury to oral branches of the trigeminal nerve: Records of 449 cases | Clinical Oral Investigations | 449 | NA | 16–83 y | Implant surgery, 16 out of 449 iatrogenic injuries (3.6%) included in the study | Paresthesia Allodynia | NA | NA |
| *Chaushu et al98 | 2002 | Medicolegal aspects of altered sensation following implant placement in the mandible | The International Journal of Oral & Maxillofacial Implants | 16 | 12 women, 4 men | 28–67 y | Mandibular: 2 premolar, 1 molar | Lip and chin; all 16 patients had persistent sensory changes | NA | NA |
IAN = inferior alveolar nerve; VAS = visual analog scale.
Data Analysis
Variable and poor reporting of data is seen in the diverse group of included articles. Any variability among studies in a review is termed heterogeneity.28 The considerable variation in results due to inconsistent methodology may be misleading. However, the following were performed:
Counts and rates calculation of counting the number of symptoms that each individual experienced
Time-to-event data that analyzes the time until an event occurs
Quantitative data analysis by data tabulation
Narrative assessment of results
Results
The quantitative results of retrospective articles (n = 7) are described in Table 5. Transient sensory changes were symptoms noticed immediately or within a week of implant placement. Persistent sensory changes lasted for more than 3 months. Common characteristics observed in retrospective studies were:
Table 5.
Retrospective Articles Analysis Results
| Study | Enrolled subjects for dental implant surgeries, n |
Transient sensory changes, n (%) |
Persistent sensory changes, n (%) |
|---|---|---|---|
| Vázquez-Delgado et al10 | 1,012 | 0 (0) | 5 (0.49) |
| Scarano et al63 | 1,065 | 23 (2.16) | 2 (0.19) |
| Deppe et al64 | 48 | 2 (4.16) | 0 (0) |
| KÜtÜk et al65 | 55 | 10 (18.18) | 5 (9.09) |
| Kwon et al66 | 47 | 21 (44.68) | 2 (4.26) |
| Ellies16 | 212 | 61 (28.77) | 17 (8.02) |
| Ellies and Hawker17 | 87 | 16 (18.39) | 4 (4.60) |
| Total | 2,526 | 133 (5.27) | 35 (1.39) |
The most common location of the implant was the posterior mandible (n = 5), followed by the anterior region, from canine to canine (n = 1).
The nerve most damaged was the inferior alveolar nerve (n = 4), followed by the mandibular incisive nerve (n = 1).
There was a female sex predominance, although no data were available on the male to female ratio. Age data were also not available.
The most common symptoms reported were paresthesia and dysesthesia, though the percentage was not available.
Out of the 7 articles, the study design of 3 was questionnaire-type research with yes or no responses or multiple choices, and 2 were clinical tests with subjective and objective evaluations to assess the neurosensory function. The clinical exam included tests to evaluate the detection threshold, detection perception, thermal detection, pinprick, and two-point discrimination. One of them also included radiographic assessment using CT scans.
The quantitative results of prospective articles (n = 13) are described in Table 6. Common characteristics of subjects in the prospective articles were:
Table 6.
Prospective Articles Analysis Results
| Study | Enrolled subjects for dental implant surgeries, n |
Transient sensory changes, n (%) |
Persistent sensory changes, n (%) |
|---|---|---|---|
| Hartmann et al67 | 33 | 0 (0) | 1 (3.03) |
| Vazquez et al38 | 1,527 | 2 (0.13) | 0 (0) |
| Abarca et al69 | 58 | 11 (18.97) | 8 (13.79) |
| Kubilius et al70 | 383 | 65 (16.97) | 3 (0.78) |
| El-Sheikh et al71 | 5 | 5 (100) | 0 (0) |
| Walton72 | 75 | 18 (24) | 1 (1.33) |
| Bartling et al18 | 94 | 8 (8.51) | 0 (0) |
| Wismeijer et al73 | 110 | 11 (10) | 10 (9.09) |
| Higuchi et al15 | 139 | 6 (4.32) | 6 (4.32) |
| Johns et al74 | 133 | 19 (14.28) | 1 (0.75) |
| Kiyak et al76 | 39 | 2 (5.12) | 0 (0) |
| van Steenberghe et al77 | 154 | 16 (10.39) | 6 (3.90) |
| Total | 2,750 | 163 (5.93) | 36 (1.31) |
The most common location was the posterior mandible, and the inferior alveolar nerve was the most common nerve damaged. Three articles reported sensory changes after placement of implants in the anterior mandible (138 subjects), with the mandibular incisor nerve being the most commonly damaged.
The sex and age data of patients who developed neuropathy were not available.
The most common symptoms reported were paresthesia and hyperesthesia, but the percentages were not available. Additionally, the sensory changes were not listed in all articles.
The common sites where neuropathy was reported were the inferior lip, gingiva, and chin.
Sensory changes in case reports and case series (n = 20) are reported in Table 7. Common characteristics observed in these 336 patients (8 patients described individually, and 328 described as part of a case series) were:
Table 7.
Case Series and Case Reports Analysis Results
| Study | Enrolled subjects for dental implant surgeries, n |
Transient sensory changes, n (%) |
Persistent sensory changes, n (%) |
|---|---|---|---|
| Politis et al40 | 26 | 2 (7.69) | 24 (92.30) |
| Devine et al41 | 10 | 0 (0) | 10 (100) |
| Du Toit et al78 | 4 | 0 (0) | 4 (100) |
| Givol et al79 | 92 | 0 (0) | 92 (100) |
| Mourào et al80 | 1 | 0 (0) | 1 (100) |
| Wright81 | 2 | 0 (0) | 2 (100) |
| Stamatin et al82 | 27 | 2 (7.40) | 0 (0) |
| Al-Ouf and Salti83 | 1 | 1 (100) | 0 (0) |
| Yoon et al84 | 1 | 0 (0) | 1 (100) |
| Rodriguez-Lozano et al85 | 1 | 0 (0) | 1 (100) |
| Leckel et al86 | 1 | 0 (0) | 1 (100) |
| Khawaja and Renton87 | 4 | 1 (25) | 3 (75) |
| Liang et al88 | 1 | 0 (0) | 1 (100) |
| Elian et al89 | 1 | 0 (0) | 1 (100) |
| Flanagan90 | 1 | 0 (0) | 1 (100) |
| Gregg14 | 2 | 0 (0) | 2 (100) |
| Kim et al91 | 64 | 3 (5.26) | 54 (94.74) |
| Juodzbalys et al45 | 16 | 5 (31.25) | 11 (68.75) |
| Renton et al39 | 30 | 3 (10) | 27 (90) |
| Tay and Zuniga94 | 7 | 0 (0) | 7 (100) |
| Libersa et al95 | 12 | 3 (25) | 9 (75) |
| Hillerup96 | 16 | 0 (0) | 16 (100) |
| Chaushu et al98 | 16 | 0 (0) | 16 (100) |
| Total | 336 | 20 (5.95) | 284 (84.52) |
The most affected region was the mandibular posterior region. The inferior alveolar nerve (IAN) was the most affected.
Women (70.83%) were primarily affected, with an age range from 17 to 83 years (mean 58 years).
The most common symptom was paresthesia (75%).
Immediate removal of implants within 24 hours led to improvement in symptoms when compared to delay in removal or treatment.
An association was found between pain and number of implants, but the evaluation was only at the 1-week postoperative follow-up. The pain was present but insignificant in a 2-year follow-up study. The study design of the prospective articles included questionnaire-type (n = 5), pain scale (visual analog scale [VAS], n = 1) and clinical examination (neurosensory testing, n = 7). A few articles with questionnaires also had clinical test evaluations as part of their examinations. Therefore, the data of both retrospective and prospective studies were combined to assess the incidence of sensory changes after dental implant placement (Table 8).
Table 8.
Sensory Changes in Subjects Due to Implant Placement
| Study design | Enrolled subjects for dental implant surgeries, n |
Transient sensory changes, n (%) |
Persistent sensory changes, n (%) |
|---|---|---|---|
| Retrospective | 2,526 | 133 (5.27) | 35 (1.39) |
| Prospective | 2,750 | 163 (5.93) | 36 (1.31) |
| Case reports and case series | 336 | 20 (5.95) | 284 (84.52) |
| Total | 5,612 | 316 (5.63) | 355 (6.33) |
Discussion
There are many articles in the literature related to pain following dental implant placement in patients, but there are very few that specifically mention sensory changes such as paresthesia, hypoesthesia, dysesthesia, numbness, tingling, etc. These sensory changes could be either transient or persistent.11,19,29
The present scoping review identified a total of 72 articles, of which 30 were literature reviews, 7 were retrospective, 12 were prospective, and 23 were case reports and case series on sensory changes after dental implant placement in patients. Of the 30 literature reviews, the included articles were on sensory changes related to dental implant placement and on risk factors, complications, and techniques to manage and avoid them.
Iatrogenic mishaps may occur, as with any other surgical procedures. Clinicians should be cautious, and a better understanding of the anatomy of vital structures around implants is necessary. Ultimately, it is prudent not to use specific locations that have high potential risks for nerve injury.
Mastering technical and safety (eg, implant drill stops) procedures for placing implants are important.30 Pain due to local anesthetic, direct impingement of the implant on the nerves, overdrilling the osteotomy site, and partial or complete nerve transaction are iatrogenic mishaps that can be avoided with drill stops, experience, and training.31 Moreover, treatment planning with radiographs or cone beam tomograms should be recommended to ensure nerves are completely separated from the dental implant using the smallest field of view necessary so that the radiation exposure is minimal.32,33 If the mandibular canal cannot be seen on a panoramic radiograph, a cone beam tomogram should be taken to verify its location. However, if such scenarios occur, it was observed that early treatment interventions, either by removal of implant or medications, lead to a better prognosis. Also, most sensory alterations found in this review with the prospective and retrospective articles were reported prior to 2005. Since then, many technologic advancements have been implemented in the field of dental implantology, such as implant placement with the help of computer guidance or augmented reality.34,35 Hence, iatrogenic failures and nerve damage can be limited.
To manage nerve damage successfully, it is vital to be able to evaluate the extent of nerve damage and the risk factors associated with it as early as possible. Clinicians performing surgical procedures should familiarize themselves with a neurosensory examination that requires no special equipment. Follow-up radiographs and evaluations are mandatory to detect any changes, as early treatment intervention is helpful to resolve neurosensory disturbances after dental implant placement.30,36
Timely and early referral to an orofacial pain specialist for noninvasive management is the responsibility of a clinician treating neurosensory trauma cases after implant placement. It is reported that delayed reporting of pain and/or sensory alterations by patients, the poorer the chances for the sensations to return to normal. A better prognosis was observed in a group of patients with early visits to the clinic and with implants placed with a safety margin of at least 2 mm from the IAN.37,38 The factors that influence the final results are the distance from the implant to the IAN canal and the surgeon’s immediate management, such as implant removal, decompression, and medication.30 These steps ensure the quality of life of the patient is maintained.
In this review, the incidence of transient neurosensory changes was observed in 5.27% and persistent neurosensory changes in 1.39% of the subjects in retrospective studies; moreover, the incidence of transient neurosensory changes was observed in 5.93% and persistent neurosensory changes in 1.31% of the subjects in prospective cohort studies. The incidence of transient neurosensory changes was observed in 5.95% and persistent neurosensory changes in 84.52% of the subjects enrolled in case reports and case series (Table 8). Including the case series and case reports in calculating the incidence could skew the average percentage, as these cases were chosen for publication due to the presence of sensory disturbances after implant surgery, but it was decided to include them in this scoping review, as this information was available in the literature. It is also important to note that, in this scoping review, it was not possible to distinguish between sensory changes related to frank axonal damage and sensory changes following implant placement without evidence of neural damage, and this should be addressed in future studies.
It was found that the mandibular premolar and molar regions were commonly affected areas due to the complex anatomy in this region, which is similar to the findings of Renton et al39 on common implant positions associated with inferior alveolar nerve injury. In addition, more implants were placed in the mandible than in the maxilla, which is in accordance with the previous literature.39,40 In this review, women more commonly developed sensory alterations when compared to men, possibly due to various reasons, such as: women visit their health care providers more than men; the prevalence of chronic pain disorders is greater in women than in men; and there could be complex interactions of factors, such as the influence of sex hormones, differences in coping strategies, etc.39,41
The present results are based on low-quality research. Most of the research articles included were questionnaire-based and are thus solely dependent on the patients’ subjective responses, so the results may not be accurate, especially as patients may be incapable of differentiating and describing the exact symptoms. The report of incidence numbers is based on a diverse group of studies; therefore, the reported incidence is likely biased in many ways and should be interpreted with caution.
In the prospective research articles, follow-up evaluations with neurosensory testing and clinical examinations were limited, mainly for a week or two. Long-term evaluation is necessary for accurate results. Furthermore, data were not available in most of the studies regarding number of implants placed, gender distribution, or specific symptoms of patients.
As can be seen, there was no standardized methodology used, which illustrates wide heterogeneity. The data for persistent pain were insufficient, and cohort studies examining persistent pain after dental implant placement could not be found.
This scoping review reports the incidence of transient and persistent sensory changes related to dental implant placement. As this review has identified gaps in knowledge, it is hoped that the results may assist in informed decision-making for health care providers (clinicians), researchers, and patients.
Conclusions
Even though the results are based on research that is not of particularly high quality, this study found that the incidence of transient (less than 3 months) sensory changes after dental implant placement is approximately 5.63%, and the incidence of persistent (more than 3 months) sensory changes after dental implant placement is approximately 6.33%.
Nerve injuries in relation to dental implants are impactful, can be persistent, and are often life-changing for patients. Dental implant treatment is, by nature, an elective procedure, and thus these injuries are avoidable if proper treatment planning is followed and if referral to the respective specialist to manage these injuries is timely. The present authors suggest more prospective controlled trials with surgical control and a long-term follow-up to assess persistent pain and neurosensory testing (preferably quantitative sensory testing) on every visit.
Key Findings
The incidence of transient sensory changes after dental implant placement is approximately 5.63%.
The incidence of persistent sensory changes after dental implant placement is approximately 6.33%.
These injuries may be avoidable if proper treatment planning is followed and referral to the respective specialist to manage these injuries is timely.
Acknowledgments
Author contributions: Dr Sowmya Ananthan led this scoping review and was responsible for managing the project and drafting the manuscript and mentored Dr Jaiswal. Dr Amey G. Patil assisted in conducting this review, and made substantial contributions in gathering and analyzing important data and formatting the tables and references. Dr Deepika Jaiswal conducted the initial review and assisted with data extraction. Dr Cibele Nasri-Heir mentored Dr Jaiswal and performed a critical review of the manuscript. Dr Gary M. Heir provided critical project advice and reviewed the manuscript. Dr Rafael Benoliel conceived and guided the research project and provided critical comments on the final draft and provided final approval before publishing.
The authors gratefully acknowledge the assistance of Ms Yingting Zhang, the Research Services Librarian at the Robert Wood Johnson Library of the Health Sciences and Adjunct Assistant Professor in the Department of Medicine of the Robert Wood Johnson Medical School at Rutgers University, for her critical comments of the review.
This study presents independent research funded by the Center for Temporomandibular Disorders and Orofacial Pain, Department of Diagnostic Sciences at Rutgers School of Dental Medicine. The views and opinions expressed by authors in this manuscript are those of the authors and do not necessarily reflect those of the funding source.
The authors report no conflicts of interest.
Funding Statement
This study presents independent research funded by the Center for Temporomandibular Disorders and Orofacial Pain, Department of Diagnostic Sciences at Rutgers School of Dental Medicine. The views and opinions expressed by authors in this manuscript are those of the authors and do not necessarily reflect those of the funding source.
References
- Hong DGK, Oh JH. Recent advances in dental implants. Maxillofac Plast Reconstr Surg. 2017;39:33. doi: 10.1186/s40902-017-0132-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alghamdi HS, Jansen JA. The development and future of dental implants. Dent Mater J. 2020;39:167–172. doi: 10.4012/dmj.2019-140. [DOI] [PubMed] [Google Scholar]
- Beschnidt SM, Cacaci C, Dedeoglu K, et al. Implant success and survival rates in daily dental practice: 5-year results of a non-interventional study using CAMLOG SCREW-LINE implants with or without platform-switching abutments. Int J Implant Dent. 2018;4:33. doi: 10.1186/s40729-018-0145-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti PCR, Bonjardim LR, Stuginski-Barbosa J, Costa YM, Svensson P. Pain complications of oral implants: Is that an issue? J Oral Rehabil. 2021;48:195–206. doi: 10.1111/joor.13112. [DOI] [PubMed] [Google Scholar]
- Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90:121–132. doi: 10.1016/S0022-3913(03)00212-9. [DOI] [PubMed] [Google Scholar]
- Goodacre CJ, Kan JY, Rungcharassaeng K. Clinical complications of osseointegrated implants. J Prosthet Dent. 1999;81:537–552. doi: 10.1016/s0022-3913(99)70208-8. [DOI] [PubMed] [Google Scholar]
- Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002;29(suppl 3):197–212. doi: 10.1034/j.1600-051x.29.s3.12.x. [DOI] [PubMed] [Google Scholar]
- Greenstein G, Cavallaro J, Romanos G, Tarnow D. Clinical recommendations for avoiding and managing surgical complications associated with implant dentistry: A review. J Periodontol. 2008;79:1317–1329. doi: 10.1902/jop.2008.070067. [DOI] [PubMed] [Google Scholar]
- Lamas Pelayo J, Peñarrocha Diago M, Martí Bowen E, Peñarrocha Diago M. Intraoperative complications during oral implantology. Med Oral Patol Oral Cir Bucal. 2008;13:e239–e243. [PubMed] [Google Scholar]
- Vázquez-Delgado E, Viaplana-Gutiérrez M, Figueiredo R, Renton T, Gay-Escoda C, Valmaseda-Castellón E. Prevalence of neuropathic pain and sensory alterations after dental implant placement in a university-based oral surgery department: A retrospective cohort study. Gerodontology. 2018;35:117–122. doi: 10.1111/ger.12326. [DOI] [PubMed] [Google Scholar]
- Benoliel R, Kahn J, Eliav E. Peripheral painful traumatic trigeminal neuropathies. Oral Dis. 2012;18:317–332. doi: 10.1111/j.1601-0825.2011.01883.x. [DOI] [PubMed] [Google Scholar]
- Dao TT, Mellor A. Sensory disturbances associated with implant surgery. Int J Prosthodont. 1998;11:462–469. [PubMed] [Google Scholar]
- Eliav E, Herzberg U, Ruda M, Bennett GJ. Neuropathic pain from an experimental neuritis of the rat sciatic nerve. Pain. 1999;83:169–182. doi: 10.1016/s0304-3959(99)00102-5. [DOI] [PubMed] [Google Scholar]
- Gregg JM. Neuropathic complications of mandibular implant surgery: review and case presentations. Ann R Australas Coll Dent Surg. 2000;15:176–180. [PubMed] [Google Scholar]
- Higuchi KW, Folmer T, Kultje C. Implant survival rates in partially edentulous patients: A 3-year prospective multicenter study. J Oral Maxillofac Surg. 1995;53:264–268. doi: 10.1016/0278-2391(95)90222-8. [DOI] [PubMed] [Google Scholar]
- Ellies LG. Altered sensation following mandibular implant surgery: A retrospective study. J Prosthet Dent. 1992;68:664–671. doi: 10.1016/0022-3913(92)90384-m. [DOI] [PubMed] [Google Scholar]
- Ellies LG, Hawker PB. The prevalence of altered sensation associated with implant surgery. Int J Oral Maxillofac Implants. 1993;8:674–679. [PubMed] [Google Scholar]
- Bartling R, Freeman K, Kraut RA. The incidence of altered sensation of the mental nerve after mandibular implant placement. J Oral Maxillofac Surg. 1999;57:1408–1412. doi: 10.1016/s0278-2391(99)90720-6. [DOI] [PubMed] [Google Scholar]
- Al-Sabbagh M, Okeson JP, Khalaf MW, Bhavsar I. Persistent pain and neurosensory disturbance after dental implant surgery: Pathophysiology, etiology, and diagnosis. Dent Clin North Am. 2015;59:131–142. doi: 10.1016/j.cden.2014.08.004. [DOI] [PubMed] [Google Scholar]
- Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Social Res Methodol. 2005;8:19–32. [Google Scholar]
- Armstrong R, Hall BJ, Doyle J, Waters E. Cochrane update. ‘Scoping the scope’ of a cochrane review. J Public Health (Oxf) 2011;33:147–150. doi: 10.1093/pubmed/fdr015. [DOI] [PubMed] [Google Scholar]
- Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sucharew H, Macaluso M. Progress notes: Methods for research evidence synthesis: The scoping review approach. J Hosp Med. 2019;14:416–418. doi: 10.12788/jhm.3248. [DOI] [PubMed] [Google Scholar]
- Nugraha B, Gutenbrunner C, Barke A, et al. The IASP classification of chronic pain for ICD-11: Functioning properties of chronic pain. Pain. 2019;160:88–94. doi: 10.1097/j.pain.0000000000001433. [DOI] [PubMed] [Google Scholar]
- Lin CS, Wu SY, Huang HY, Lai YL. Systematic review and meta-analysis on incidence of altered sensation of mandibular implant surgery. PloS One. 2016;11:e0154082. doi: 10.1371/journal.pone.0154082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Hoboken, NJ: John Wiley & Sons; 2011. [Google Scholar]
- Muller E, Ríos Calvo MP. Pain and dental implantology: Sensory quantification and affective aspects. Part I: At the private dental office. Implant Dent. 2001;10:14–22. doi: 10.1097/00008505-200101000-00007. [DOI] [PubMed] [Google Scholar]
- Juodzbalys G, Wang HL, Sabalys G. Injury of the inferior alveolar nerve during implant placement: A literature review. J Oral Maxillofac Res. 2011;2:e1. doi: 10.5037/jomr.2011.2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenstein G, Greenstein B, Desai RN. Using drill stops on twist drills to promote safety and efficiency when creating osteotomies for dental implants. J Am Dent Assoc. 2014;145:371–375. doi: 10.14219/jada.2014.10. [DOI] [PubMed] [Google Scholar]
- American Dental Association Council on Scientific Affairs. The use of cone-beam computed tomography in dentistry: an advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2012;143:899–902. doi: 10.14219/jada.archive.2012.0295. [DOI] [PubMed] [Google Scholar]
- Tyndall DA, Price JB, Tetradis S, et al. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:817–826. doi: 10.1016/j.oooo.2012.03.005. [DOI] [PubMed] [Google Scholar]
- Kwon HB, Park YS, Han JS. Augmented reality in dentistry: A current perspective. Acta Odontol Scand. 2018;76:497–503. doi: 10.1080/00016357.2018.1441437. [DOI] [PubMed] [Google Scholar]
- Mozer PS. Accuracy and deviation analysis of static and robotic guided implant surgery: A case study. Int J Oral Maxillofac Implants. 2020;35:e86–e90. doi: 10.11607/jomi.8231. [DOI] [PubMed] [Google Scholar]
- Misch CE, Resnik R. Mandibular nerve neurosensory impairment after dental implant surgery: Management and protocol. Implant Dent. 2010;19:378–386. doi: 10.1097/ID.0b013e3181effa92. [DOI] [PubMed] [Google Scholar]
- Padmanabhan H, Kumar AV, Shivashankar K. Incidence of neurosensory disturbance in mandibular implant surgery - a meta-analysis. J Indian Prosthodont Soc. 2020;20:17–26. doi: 10.4103/jips.jips_373_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vazquez L, Saulacic N, Belser U, Bernard JP. Efficacy of panoramic radiographs in the preoperative planning of posterior mandibular implants: A prospective clinical study of 1527 consecutively treated patients. Clin Oral Implants Res. 2008;19:81–85. doi: 10.1111/j.1600-0501.2007.01402.x. [DOI] [PubMed] [Google Scholar]
- Renton T, Dawood A, Shah A, Searson L, Yilmaz Z. Post-implant neuropathy of the trigeminal nerve. A case series. Br Dent J. 2012;212:e17. doi: 10.1038/sj.bdj.2012.497. [DOI] [PubMed] [Google Scholar]
- Politis C, Agbaje J, Van Hevele J, et al. Report of neuropathic pain after dental implant placement: A case series. Int J Oral Maxillofac Implants. 2017;32:439–444. doi: 10.11607/jomi.5241. [DOI] [PubMed] [Google Scholar]
- Devine M, Taylor S, Renton T. Chronic post-surgical pain following the placement of dental implants in the maxilla: A case series. Eur J Oral Implantol. 2016;9(suppl 1):179–186. [PubMed] [Google Scholar]
- Carter E, Yilmaz Z, Devine M, Renton T. An update on the causes, assessment and management of third division sensory trigeminal neuropathies. Br Dent J. 2016;220:627–635. doi: 10.1038/sj.bdj.2016.444. [DOI] [PubMed] [Google Scholar]
- Jacobs R, Quirynen M, Bornstein MM. Neurovascular disturbances after implant surgery. Periodontol 2000. 2014;66:188–202. doi: 10.1111/prd.12050. [DOI] [PubMed] [Google Scholar]
- Dannan A. Traumatic injury of the inferior alveolar nerve after dental implant surgery: A literature review. Int J Dent Sci. 2013;12:1–7. [Google Scholar]
- Juodzbalys G, Wang HL, Sabalys G, Sidlauskas A, Galindo-Moreno P. Inferior alveolar nerve injury associated with implant surgery. Clin Oral Implants Res. 2013;24:183–190. doi: 10.1111/j.1600-0501.2011.02314.x. [DOI] [PubMed] [Google Scholar]
- Renton T. Oral surgery: Part 4. Minimising and managing nerve injuries and other complications. Br Dent J. 2013;215:393–399. doi: 10.1038/sj.bdj.2013.993. [DOI] [PubMed] [Google Scholar]
- Tinastepe N, Oral K. Neuropathic pain after dental treatment. Agri. 2013;25:1–6. doi: 10.5505/agri.2013.55477. [DOI] [PubMed] [Google Scholar]
- Greenwood M, Corbett I. Dental Emergencies. Chichester: John Wiley & Sons; 2012. [Google Scholar]
- Palma-Carrió C, Balaguer-Martínez J, Peñarrocha-Oltra D, Peñarrocha-Diago M. Irritative and sensory disturbances in oral implantology. Literature review. Med Oral Patol Oral Cir Bucal. 2011;16:e1043–e1046. doi: 10.4317/medoral.17125. [DOI] [PubMed] [Google Scholar]
- Siqueira JTT, Siqueira SRDT. Persistent pain, sensory abnormalities, nervous injury and loss of implant after dental implant surgery: Clinical approach suggestion. Revista Dor. 2011;12:172–181. [Google Scholar]
- Sánchez Garcés MA, Escoda-Francolí J, Gay-Escoda C. Implant complications. In: Turkyilmaz I, editor. Implant Dentistry. The Most Promising Discipline of Dentistry. InTech Open; 2011. pp. 369–396. [Google Scholar]
- Kim SG. Clinical complications of dental implants. In: Turkyilmaz I, editor. Implant Dentistry. A Rapidly Evolving Practice. InTech Open; 2011. doi: 10.5772/17262. [Google Scholar]
- Alhassani AA, AlGhamdi AST. Inferior alveolar nerve injury in implant dentistry: Diagnosis, causes, prevention, and management. J Oral Implantol. 2010;36:401–407. doi: 10.1563/AAID-JOI-D-09-00059. [DOI] [PubMed] [Google Scholar]
- Moore PA, Haas DA. Paresthesias in dentistry. Dent Clin North Am. 2010;54:715–730. doi: 10.1016/j.cden.2010.06.016. [DOI] [PubMed] [Google Scholar]
- Renton T. Prevention of iatrogenic inferior alveolar nerve injuries in relation to dental procedures. Dent Update. 2010;37:350–352. 354–356, 358–360. doi: 10.12968/denu.2010.37.6.350. passim. [DOI] [PubMed] [Google Scholar]
- Misch K, Wang HL. Implant surgery complications: Etiology and treatment. Implant Dent. 2008;17:159–168. doi: 10.1097/ID.0b013e3181752f61. [DOI] [PubMed] [Google Scholar]
- Peñarrocha M, Cervelló MA, Martí E, Bagán JV. Trigeminal neuropathy. Oral Dis. 2007;13:141–150. doi: 10.1111/j.1601-0825.2006.01356.x. [DOI] [PubMed] [Google Scholar]
- Greenstein G, Tarnow D. The mental foramen and nerve: Clinical and anatomical factors related to dental implant placement: A literature review. J Periodontol. 2006;77:1933–1943. doi: 10.1902/jop.2006.060197. [DOI] [PubMed] [Google Scholar]
- Hegedus F, Diecidue RJ. Trigeminal nerve injuries after mandibular implant placement–practical knowledge for clinicians. Int J Oral Maxillofac Implants. 2006;21:111–116. [PubMed] [Google Scholar]
- Worthington P. Injury to the inferior alveolar nerve during implant placement: A formula for protection of the patient and clinician. Int J Oral Maxillofac Implants. 2004;19:731–734. [PubMed] [Google Scholar]
- Mraiwa N, Jacobs R, Steenberghe D, Quirynen M. Clinical assessment and surgical implications of anatomic challenges in the anterior mandible. Clin Implant Dent Relat Res. 2003;5:219–225. doi: 10.1111/j.1708-8208.2003.tb00204.x. [DOI] [PubMed] [Google Scholar]
- Vallerand WP. Peripheral trigeminal nerve injuries. N Y State Dent J. 1992;58:27–30. [PubMed] [Google Scholar]
- Scarano A, Sinjari B, Murmura G, Lorusso F. Neurosensory disturbance of the inferior alveolar nerve after 3025 implant placements. Implant Dent. 2017;26:735–743. doi: 10.1097/ID.0000000000000651. [DOI] [PubMed] [Google Scholar]
- Deppe H, Mücke T, Wagenpfeil S, Kesting M, Linsenmeyer E, Tölle T. Trigeminal nerve injuries after mandibular oral surgery in a university outpatient setting–a retrospective analysis of 1,559 cases. Clin Oral Investig. 2015;19:149–157. doi: 10.1007/s00784-014-1222-5. [DOI] [PubMed] [Google Scholar]
- Kütük N, Demirbaş AE, Gönen ZB, et al. Anterior mandibular zone safe for implants. J Craniofac Surg. 2013;24:e405–e408. doi: 10.1097/SCS.0b013e318292c7d5. [DOI] [PubMed] [Google Scholar]
- Kwon TG, Kim SY, Kim JB. The prevalence of sensory disturbance after implant surgery—Retrospective survey of implant practitioners. J Korean Assoc Oral Maxillofac Surg. 2004;30:339–344. [Google Scholar]
- Hartmann A, Welte-Jzyk C, Seiler M, Daubländer M. Neurophysiological changes associated with implant placement. Clin Oral Implants Res. 2017;28:576–581. doi: 10.1111/clr.12837. [DOI] [PubMed] [Google Scholar]
- Al-Khabbaz AK, Griffin TJ, Al-Shammari KF. Assessment of pain associated with the surgical placement of dental implants. J Periodontol. 2007;78:239–246. doi: 10.1902/jop.2007.060032. [DOI] [PubMed] [Google Scholar]
- Abarca M, van Steenberghe D, Malevez C, De Ridder J, Jacobs R. Neurosensory disturbances after immediate loading of implants in the anterior mandible: an initial questionnaire approach followed by a psychophysical assessment. Clin Oral Investig. 2006;10:269–277. doi: 10.1007/s00784-006-0065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubilius R, Sabalys G, Juodzbalys G, Gedrimas V. Traumatic damage to the inferior alveolar nerve sustained in course of dental implantation. Possibility of prevention. Stomatologija. 2004;6:106–110. [Google Scholar]
- El-Sheikh AM, Hobkirk JA, Howell PG, Gilthorpe MS. Changes in passive tactile sensibility associated with dental implants following their placement. Int J Oral Maxillofac Implants. 2003;18:266–272. [PubMed] [Google Scholar]
- Walton JN. Altered sensation associated with implants in the anterior mandible: A prospective study. J Prosthet Dent. 2000;83:443–449. doi: 10.1016/s0022-3913(00)70039-4. [DOI] [PubMed] [Google Scholar]
- Wismeijer D, van Waas MA, Vermeeren JI, Kalk W. Patients’ perception of sensory disturbances of the mental nerve before and after implant surgery: a prospective study of 110 patients. Br J Oral Maxillofac Surg. 1997;35:254–259. doi: 10.1016/s0266-4356(97)90043-7. [DOI] [PubMed] [Google Scholar]
- Johns RB, Jemt T, Heath MR, et al. A multicenter study of overdentures supported by Brånemark implants. Int J Oral Maxillofac Implants. 1992;7:513–522. [PubMed] [Google Scholar]
- Astrand P, Borg K, Gunne J, Olsson M. Combination of natural teeth and osseointegrated implants as prosthesis abutments: A 2-year longitudinal study. Int J Oral Maxillofac Implants. 1991;6:305–312. [PubMed] [Google Scholar]
- Kiyak HA, Beach BH, Worthington P, Taylor T, Bolender C, Evans J. The psychological impact of osseointegrated dental implants. Int J Oral Maxillofac Implants. 1990;5:61–69. [PubMed] [Google Scholar]
- van Steenberghe D, Lekholm U, Bolender C, et al. The applicability of osseointegrated oral implants in the rehabilitation of partial edentulism: A prospective multicenter study on 558 fixtures. Int J Oral Maxillofac Implants. 1990;5:272–281. [PubMed] [Google Scholar]
- Du Toit J, Gluckman H, Gamil R, Renton T. Implant injury case series and review of the literature part 1: Inferior alveolar nerve injury. J Oral Implantol. 2015;41:e144–e151. doi: 10.1563/aaid-joi-D-14-00022. [DOI] [PubMed] [Google Scholar]
- Givol N, Peleg O, Yarom N, Blinder D, Lazarovici TS. Inferior alveolar neurosensory deficiency associated with placement of dental implants. J Periodontol. 2013;84:495–501. doi: 10.1902/jop.2012.110599. [DOI] [PubMed] [Google Scholar]
- Mourào L, Moutinho H, Canabarro A. Role of homeopathy in post-surgical dental implants paresthesia—A case report. J Case Stud Homeopathy. 2013;1:6–10. [Google Scholar]
- Wright EF. Persistent dysesthesia following dental implant placement: A treatment report of 2 cases. Implant Dent. 2011;20:20–26. doi: 10.1097/ID.0b013e31820968b5. [DOI] [PubMed] [Google Scholar]
- Stamatin O, Voroneanu M, Stelea C. Post-Implant neurological complications in the horizontal mandibular arch. International J Med Dent. 2011;2:197–201. [Google Scholar]
- Al-Ouf K, Salti L. Postinsertion pain in region of mandibular dental implants: A case report. Implant Dent. 2011;20:27–31. doi: 10.1097/ID.0b013e3182096c94. [DOI] [PubMed] [Google Scholar]
- Yoon SH, Merrill RL, Choi JH, Kim ST. Use of botulinum toxin type A injection for neuropathic pain after trigeminal nerve injury. Pain Med. 2010;11:630–632. doi: 10.1111/j.1526-4637.2010.00801.x. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Lozano FJ, Sanchez-Pérez A, Moya-Villaescusa MJ, Rodríguez-Lozano A, Sáez-Yuguero MR. Neuropathic orofacial pain after dental implant placement: Review of the literature and case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e8–e12. doi: 10.1016/j.tripleo.2009.12.004. [DOI] [PubMed] [Google Scholar]
- Leckel M, Kress B, Schmitter M. Neuropathic pain resulting from implant placement: Case report and diagnostic conclusions. J Oral Rehabil. 2009;36:543–546. doi: 10.1111/j.1365-2842.2009.01950.x. [DOI] [PubMed] [Google Scholar]
- Khawaja N, Renton T. Case studies on implant removal influencing the resolution of inferior alveolar nerve injury. Br Dent J. 2009;206:365–370. doi: 10.1038/sj.bdj.2009.258. [DOI] [PubMed] [Google Scholar]
- Liang X, Lambrichts I, Corpas L, et al. Neurovascular disturbance associated with implant placement in the anterior mandible and its surgical implications: Literature review including report of a case. Chinese J Dent Res. 2008;11:56–64. [Google Scholar]
- Elian N, Mitsias M, Eskow R, et al. Unexpected return of sensation following 4.5 years of paresthesia: Case report. Implant Dent. 2005;14:364–370. doi: 10.1097/01.id.0000190252.60779.ae. [DOI] [PubMed] [Google Scholar]
- Flanagan D. Delayed onset of altered sensation following dental implant placement and mental block local anesthesia: A case report. Implant Dent. 2002;11:324–330. doi: 10.1097/00008505-200211040-00010. [DOI] [PubMed] [Google Scholar]
- Kim YT, Pang KM, Jung HJ, Kim SM, Kim MJ, Lee JH. Clinical outcome of conservative treatment of injured inferior alveolar nerve during dental implant placement. J Korean Assoc Oral Maxillofac Surg. 2013;39:127–133. doi: 10.5125/jkaoms.2013.39.3.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peñarrocha M, Peñarrocha D, Bagán JV, Peñarrocha M. Post-traumatic trigeminal neuropathy. A study of 63 cases. Med Oral Patol Oral Cir Bucal. 2012;17:e297–e300. doi: 10.4317/medoral.17401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renton T, Yilmaz Z. Profiling of patients presenting with posttraumatic neuropathy of the trigeminal nerve. J Orofac Pain. 2011;25:333. [PubMed] [Google Scholar]
- Tay AB, Zuniga JR. Clinical characteristics of trigeminal nerve injury referrals to a university centre. Int J Oral Maxillofac Surg. 2007;36:922–927. doi: 10.1016/j.ijom.2007.03.012. [DOI] [PubMed] [Google Scholar]
- Libersa P, Savignat M, Tonnel A. Neurosensory disturbances of the inferior alveolar nerve: A retrospective study of complaints in a 10-year period. J Oral Maxillofac Surg. 2007;65:1486–1489. doi: 10.1016/j.joms.2007.03.023. [DOI] [PubMed] [Google Scholar]
- Hillerup S. Iatrogenic injury to oral branches of the trigeminal nerve: Records of 449 cases. Clin Oral Investig. 2007;11:133–142. doi: 10.1007/s00784-006-0089-5. [DOI] [PubMed] [Google Scholar]
- Caissie R, Goulet J, Fortin M, Morielli D. Iatrogenic paresthesia in the third division of the trigeminal nerve: 12 years of clinical experience. J Can Dent Assoc. 2005;71:185–190. [PubMed] [Google Scholar]
- Chaushu G, Taicher S, Halamish-Shani T, Givol N. Medicolegal aspects of altered sensation following implant placement in the mandible. Int J Oral Maxillofac Implants. 2002;17:413–415. [PubMed] [Google Scholar]