Abstract
OBJECTIVES:
Mean arterial hypotension between 55 and 65 mm Hg could be tolerated safely in the absence of tissue hypoperfusion, but the consequences on fluid balance and kidney function remain unknown.
DESIGN:
During a 1-year period, we retrospectively collected data of consecutive septic patients admitted for sepsis with a mean arterial pressure (MAP) less than 65 mm Hg despite fluid resuscitation.
SETTING:
Medical 18-bed ICU in a tertiary teaching hospital.
PATIENTS:
Septic patients with a MAP less than 65 mm Hg despite initial resuscitation.
INTERVENTIONS:
In our ICU, MAP between 55 and 65 mm Hg was tolerated in the absence of peripheral hypoperfusion (permissive hypotension) or corrected using norepinephrine (septic shock group) when peripheral tissue hypoperfusion was present.
MEASUREMENTS AND MAIN RESULTS:
Ninety-four consecutive septic patients were included, 15 in the permissive hypotension group and 79 in the septic shock group. Median age was 66 years (57–77 yr) and 42% were women. The main sources of infection were respiratory (45%) and abdominal (18%). Severity was more important in septic shock group with higher Sequential Organ Failure Assessment score (7 [5–10] vs. 4 [1–6]; p < 0.0001), more frequent organ support therapy and ultimately higher mortality (38 vs. 0%; p < 0.01). The total volume of crystalloids infused before ICU admission was not different between groups (1930 ± 250 vs. 1850 ± 150 mL; p = 0.40). Within the 6 first hours of ICU stay, patients in the permissive hypotension group received less fluids (530 ± 170 vs. 1100 ± 110 mL; p = 0.03) and had higher urinary output (1.4 mL [0.88–2.34 mL] vs. 0.47 mL/kg/hr [0.08–1.25 mL/kg/hr]; p < 0.001). In addition, kidney injury evaluated using KDIGO score was lower in the permissive hypotension group at 48 hours (0 hr [0–1 hr] vs. 1 hr [0–2 hr]; p < 0.05).
CONCLUSIONS:
In septic patients without clinical peripheral hypoperfusion, mean arterial hypotension between 55 and 65 mm Hg could be tolerated safely without vasopressor infusion and was not associated with excessive fluid administration or kidney damage.
Keywords: fluid management, kidney function, permissive hypotension, sepsis, tissue perfusion
KEY POINTS
Question: In septic patients, the optimal resuscitation target for mean arterial pressure (MAP) remains controversial. Bedside tissue perfusion analysis could be helpful to guide MAP target.
Findings: In this cohort study of septic patients, we showed that tolerating mean arterial hypotension between 55 and 65 mm Hg in the absence of peripheral hypoperfusion was safe and had no deleterious impact neither on fluid balance nor on kidney functions.
Meanings: Peripheral tissue perfusion could be helpful to personalize hemodynamic management of septic patients.
Sepsis is a common condition in ICUs and is responsible for high morbidity and mortality (1). During the golden hours of resuscitation, several key therapeutic steps must be achieved, including antibiotic administration, source control, and associated with fluid administration in the presence of tissue hypoperfusion (2). International guidelines also recommend using norepinephrine to maintain a mean arterial pressure (MAP) higher than 65 mm Hg despite no strong available evidence supporting this threshold. Asfar et al (3) reported that targeting a MAP at 80–85 mm Hg in septic shock patients did not improve mortality compared with a 65–70 mm Hg target but found a benefit on kidney damage, specifically in patients with chronic hypertension. Conversely, a more recent study in old patients with sepsis showed that tolerating a mean arterial hypotension at 60 mm Hg was safe and even improved the outcome of patients with hypertension (4). Overall, a one-size-fits-all MAP target in septic shock patients should be reconsidered and a more individualized approach proposed. In our ICU, as recommended by international guidelines, tissue perfusion is evaluated routinely and particularly used for the therapeutic management of patients suffering from infection-related acute circulatory failure. Peripheral tissue perfusion is a reliable marker of microvascular blood flow (5) but does not tightly correlate with macrohemodynamic variables, such as cardiac output or arterial pressure (6). We have previously shown in sepsis patients without peripheral tissue hypoperfusion that permissive arterial hypotension (55 < MAP < 65 mm Hg) could be tolerated safely (7) with no in-ICU supplemental mortality and a reduced length of stay. However, the impact of permissive hypotension on fluid balance and kidney functions remains unknown.
The aim of this study was to compare the volume of fluid infused and kidney injury parameters in both permissive and nonpermissive groups during the first 48 hours of ICU admission.
METHODS
During a 1-year period, we collected the data of consecutive septic patients admitted in our tertiary ICU with a MAP less than 65 mm Hg despite prior fluid resuscitation. Kidney injury was evaluated using plasma creatinine levels, urinary output, and the Kidney Disease Improval Global Outcomes (KDIGO) classification. Global ICU management was consistent with international sepsis guidelines, except for the MAP target. In our ICU, the decision to tolerate arterial hypotension (55 < MAP < 65 mm Hg) or not was taken routinely by the clinician in charge of the patient and based on biological and clinical parameters of tissue perfusion and the quality of source control. MAP between 55 and 65 mm Hg was tolerated in the absence of tissue hypoperfusion defined by preserved consciousness AND mottling score equal to 0 AND arterial lactate level less than 2 mmol/L after resuscitation. Infection source control requires drainage of infected abscess, surgical debridement of necrotic infected tissue, and removal of infected prosthetic or surgery to remove a focus of infection and restore organ function (e.g., peritonitis). In accordance with French law regarding retrospective monocenter study, no institutional review board review was necessary. All patients received information that data extracted from their medical charts could be used for research purposes. The database followed Methodology of Reference-004 and was declared to the Commission Nationale de l'Informatique et des Libertés (N° 2229819).
Categorical and quantitative variables were reported as n (%), medians (interquartile range), and mean ± sd according to the distribution. Comparisons between groups were made using chi-square or Fisher exact tests for categorical variables, and Mann-Whitney U test for continuous variables. Tests were two-tailed, with an α level of 0.05. Statistical analyses were done using GraphPad-Prism-6 software (San Diego, CA).
RESULTS
From January to December 2019, 94 consecutive septic patients with MAP less than 65 mm Hg despite initial fluid resuscitation were included. Median age was 66 years (57–77 yr) with 40 women (42%). The main sources of infection were respiratory (45%) and abdominal (18%). Arterial hypotension lower than 65 mm Hg was tolerated in 15 patients (permissive hypotension), whereas 79 patients received norepinephrine infusion to maintain a MAP greater than 65 mm Hg. Patients with permissive hypotension had preserved consciousness and lower arterial lactate levels compared with the septic shock group at baseline (1.7 mmol/L [1.1–2.9 mmol/L] vs. 4 mmol/L [2.7–6.7 mmol/L]; p < 0.001) and after initial resuscitation (1.1 mmol/L [0.9–1.8 mmol/L] vs. 2.5 mmol/L [1.4–3.9 mmol/L]; p < 0.001) (Table 1). No mottling was observed in the permissive group, whereas 24% of septic group had mottling around the knee (median score 0 [0–3]). As expected, the severity of septic shock patients was more important with higher Simplified Acute Physiology Score II (60 [45–86] vs. 45 [27–46]; p = 0.0001) and higher Sequential Organ Failure Assessment score (7 [5–10] vs. 4 [1–6]; p < 0.0001). Organ support therapy was more frequently used in the septic shock group, such as invasive mechanical ventilation (71% vs. 0%; p < 0.0001) and hemodialysis (20% vs. 0%; p = 0.06) (Table 1). Finally, 30 patients in the septic shock group died during their ICU stay (38%) but none in the permissive hypotension group.
TABLE 1.
General Characteristics of Studied Population
| Patients’ Characteristics, n (%) or Median (IQR) | Permissive Hypotension, n = 15 | Septic Shock, n = 79 | p |
|---|---|---|---|
| Age | 59 (50–73) | 67 (57–78) | 0.22 |
| Body mass index (kg/m2) | 24 (20–27) | 24 (20–28) | 0.85 |
| Male gender | 11 (73) | 43 (54) | 0.17 |
| Simplified Acute Physiology Score 2 | 45 (27–46) | 60 (45–86) | < 0.001 |
| Comorbidities | |||
| Diabetes | 4 (27) | 18 (23) | |
| Hypertension | 4 (27) | 33 (42) | |
| Cardiovascular disease | 7 (47) | 29 (32) | |
| Smokers | 3 (21) | 18 (24) | |
| Cirrhosis | 0 | 6 (7) | |
| Infection sources | |||
| Lung | 4 (27) | 38 (43) | |
| Abdominal | 4 (27) | 13 (15) | |
| Urinary tract infection | 1 (6) | 15 (17) | |
| Catheters | 2 (13) | 0 | |
| Others | 4 (27) | 20 (23) | |
| Organ support therapy | |||
| Vasopressor infusion | 0 | 79 (100) | < 0.001 |
| Invasive mechanical ventilation | 0 | 56 (71) | < 0.001 |
| Renal replacement therapy | 0 | 16 (20) | 0.06 |
| Biologics | |||
| Leucocytes (Giga/L) | 11 (7–15) | 8 (3–17) | 0.51 |
| Hemoglobin (g/dL) | 10 (8–13) | 12 (10–13) | 0.08 |
| Platelets (Giga/L) | 176 (98–259) | 142 (80–229) | 0.40 |
| Serum creatinine (µmol/L) | 139 (84–189) | 125 (94–207) | 0.65 |
| Procalcitonin (ng/mL) | 16 (3–41) | 13 (4–49) | 0.80 |
| Bicarbonate (mmol/L) | 21 (19–24) | 19 (14–23) | 0.12 |
| Arterial lactate (mmol/L)# | 1.7 (1.1–2.9) | 4 (2.7–6.7) | < 0.001 |
| Protidemia (g/L) | 59 (54–64) | 58 (49–67) | 0.6 |
| Arterial lactate (mmol/L) | |||
| Baseline | 1.7 (1.1–2.9) | 4.0 (2.7–6.7) | < 0.001 |
| After initial resuscitation | 1.1 (0.9–1.8) | 2.5 (1.4–3.9) | < 0.001 |
| Outcome | |||
| Death in ICU | 0 | 30 (38) | 0.004 |
| Death in hospital | 1 (6) | 35 (44) | 0.006 |
| LOS in ICU, da | 3 (2–5) | 7 (4–14) | < 0.001 |
| LOS in hospital, d | 13 (6–39) | 13 (5–37) | 0.80 |
IQR = interquartile range, LOS = length of stay.
Among survivors after 24 hr in ICU. Nonparametric test.
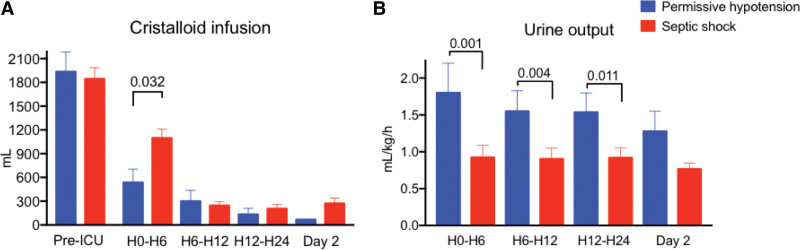
In the permissive group, arterial hypotension (admission MAP at 60 mm Hg [56–64 mm Hg]) recovered within the first days after ICU admission (24 hr: 69 mm Hg [60–72 mm Hg] and 48 hr: 77 mm Hg [70–81 mm Hg]). In the septic shock group, patients received norepinephrine to increase MAP from 61 mm Hg (56–64 mm Hg) at ICU admission to 69 mm Hg (64–76 mm Hg) at 6 hours with a median dose of 0.7 µg/kg/min (0.3–1.5 µg/kg/min), 72 mm Hg (66–80 mm Hg) at 24 hours, and 75 mm Hg (68–81 mm Hg) at 48 hours (Supplementary Table 1, http://links.lww.com/CCX/B261). The total volume of crystalloids infused before ICU admission was not different between groups (1930 ± 250 vs. 1850 ± 150 mL; p = 0.40) but during the first 6 hours of ICU stay, patients in the permissive hypotension group received less fluids (530 ± 170 vs. 1100 ± 110 mL; p = 0.03) (Fig. 1A). At inclusion, plasma creatinine level was not different between groups (139 µmol/L [84–189 µmol/L] vs. 125 µmol/L [94–207 µmol/L]; p = 0.65). However, in the permissive hypotension group, urinary output was higher during the first 24 hours of ICU stay (Fig. 1B) and kidney injury evaluated using Kidney Disease Improval Global Outcomes score was lower at 48 hours (0 hr [0–1 hr] vs. 1 hr [0–2 hr]; p < 0.05) (Supplementary Table 1, http://links.lww.com/CCX/B261).
Figure 1.
Global fluid balance in 2 groups. A, Mean crystalloid volume infusion during the first 48 hr in ICU. B, Mean urine output during the first 48 hr of management in ICU. Nonparametric test.
DISCUSSION
In this observational study, we showed that a strategy of permissive hypotension applied on selected septic patients without peripheral tissue hypoperfusion was not associated with excessive fluid administration or kidney injury. We suggest that an individualized hemodynamic approach could be used in septic patients with well tolerated arterial hypotension between 55 and 65 mm Hg, as defined by the absence of bedside evaluated tissue hypoperfusion (absence of mottling, preserved consciousness and low arterial lactate levels). The imbalance in admission characteristics between groups highlights that such a management strategy is possible only in selected septic patients, when source control seems optimal, and bedside evaluation of tissue perfusion is satisfactory.
We specifically investigated fluid volume because previous works have identified that fluid overload is associated with poor outcome (8). In the FENICE survey, intensivists declared that arterial hypotension is one of the main indications to infuse fluids in critically ill patients. In our study, patients in the permissive group received less fluid than septic shock group, whose MAP was maintained higher than 65 mm Hg with norepinephrine, highlighting that peripheral perfusion evaluation has been implemented in our therapeutic strategy. In a proof-of-concept study, Jansen et al (9) previously reported a significant reduction of fluid volume when resuscitation was guided by peripheral tissue perfusion parameters. In the seminal work by Hernandez et al (10), the authors also showed that a strategy based on capillary refill time monitoring is associated with reduced fluid volume infusion and decreased organ support therapy when compared to a strategy based on lactate clearance.
We also investigated the impact of hypotension lower than 65 mm Hg on kidney damage because the relationship between MAP target and kidney function is still a matter of debate. Some observational studies reported that high MAP is associated with better kidney function (11), whereas others did not find such relationship (12). In the SEPSISPAM trial, hemodialysis was less frequently used in the high MAP target patients with chronic hypertension (3). However, in another randomized trial, Lamontagne et al (4) did not confirm this benefit and even found better outcomes in hypertensive patients whose MAP target was 60–65 mm Hg. Here, we found that despite arterial hypotension of less than 65 mm Hg, urinary output was preserved in the permissive hypotension group and kidney injury recovered quickly. Such observations suggest that endogenous compensatory mechanisms regulating volemia or vasomotor tone are elicited in permissive hypotension patients to maintain kidney perfusion. We hypothesize that the absence of mechanical ventilation or sedative drugs is important for such compensatory mechanisms to be preserved (13). The generalizability of our strategy must be validated in larger cohorts, especially in patients under mechanical ventilation receiving vasodilating drugs.
CONCLUSIONS
In this observational work, we found that MAP between 55 and 65 mm Hg in septic patients could be tolerated safely in the absence of clinical peripheral hypoperfusion and was not associated with excessive fluid administration or kidney injury. These data pave the way for future interventional trials integrating tissue perfusion in MAP targets for septic patients.
ACKNOWLEDGMENTS
We are indebted to Rozenn Leboursicaud for her help in data extraction.
Supplementary Material
Footnotes
The authors have disclosed that they do not have any potential conflicts of interest.
Drs. Lavillegrand, Blum, Gabarre, Bonny, and Ait-Oufella were involved in acquisitions of data. Drs. Lavillegrand, Blum, Urbina, Guidet, and Ait-Oufella were involved in drafting of the article. Drs. Lavillegrand, Blum, and Ait-Oufella were involved in statistical analysis. All authors were involved in study concept and design and critical revision of article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
REFERENCES
- 1.Dupuis C, Bouadma L, Ruckly S, et al. : Sepsis and septic shock in France: Incidences, outcomes and costs of care. Ann Intensive Care 2020; 10:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Evans L, Rhodes A, Alhazzani W, et al. : Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Crit Care Med 2021; 49:e1063–e1143 [DOI] [PubMed] [Google Scholar]
- 3.Asfar P, Meziani F, Hamel JF, et al. ; SEPSISPAM Investigators: High versus low blood-pressure target in patients with septic shock. N Engl J Med 2014; 370:1583–1593 [DOI] [PubMed] [Google Scholar]
- 4.Lamontagne F, Richards-Belle A, Thomas K, et al. ; 65 trial investigators: Effect of reduced exposure to vasopressors on 90-day mortality in older critically ill patients with vasodilatory hypotension: A randomized clinical trial. JAMA 2020; 323:938–949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang W, Xiang H, Hu C, et al. : Association of sublingual microcirculation parameters and capillary refill time in the early phase of ICU admission. Crit Care Med 2023; 51:913–923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunser MW, Takala J, Brunauer A, et al. : Re-thinking resuscitation: Leaving blood pressure cosmetics behind and moving forward to permissive hypotension and a tissue perfusion-based approach. Crit Care 2013; 17:326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lavillegrand JR, Dumas G, Bige N, et al. : Should we treat mild hypotension in septic patients in the absence of peripheral tissue hypoperfusion? Intensive Care Med 2018; 44:1593–1594 [DOI] [PubMed] [Google Scholar]
- 8.Messmer AS, Zingg C, Muller M, et al. : Fluid overload and mortality in adult critical care patients-a systematic review and meta-analysis of observational studies. Crit Care Med 2020; 48:1862–1870 [DOI] [PubMed] [Google Scholar]
- 9.Jansen TC, van Bommel J, Schoonderbeek FJ, et al. ; LACTATE study group: Early lactate-guided therapy in intensive care unit patients: A multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med 2010; 182:752–761 [DOI] [PubMed] [Google Scholar]
- 10.Hernandez G, Ospina-Tascon GA, Damiani LP, et al. ; The ANDROMEDA SHOCK Investigators and the Latin America Intensive Care Network (LIVEN): Effect of a resuscitation strategy targeting peripheral perfusion status vs serum lactate levels on 28-day mortality among patients with septic shock: The ANDROMEDA-SHOCK randomized clinical trial. JAMA 2019; 321:654–664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Badin J, Boulain T, Ehrmann S, et al. : Relation between mean arterial pressure and renal function in the early phase of shock: A prospective, explorative cohort study. Crit Care 2011; 15:R135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bourgoin A, Leone M, Delmas A, et al. : Increasing mean arterial pressure in patients with septic shock: Effects on oxygen variables and renal function. Crit Care Med 2005; 33:780–786 [DOI] [PubMed] [Google Scholar]
- 13.Lamblin V, Favory R, Boulo M, et al. : Microcirculatory alterations induced by sedation in intensive care patients. Effects of midazolam alone and in association with sufentanil. Crit Care 2006; 10:R176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.