Abstract
Internal hernias are a rare but morbid complication following Roux-en-Y gastric bypass surgery. The incorporation of Brolin’s anti-obstruction stitch has historically demonstrated a significant reduction in the incidence of internal hernias following Roux-en-Y gastric bypass. We present an ironic and unique case of a patient with small bowel herniation into a defect between Brolin’s stitch and the stapled closed common enterotomy of the jejunojejunostomy and technical considerations to decrease internal hernias at this site in the future.
Keywords: internal hernia, Brolin’s stitch, anti-obstruction stitch, Roux-en-Y gastric bypass, bariatric surgery
Introduction
The Roux-en-Y gastric bypass (RNYGB) has become one of the most performed bariatric procedures and has led to significant post-operative weight loss and reduction in comorbid conditions in patients suffering from obesity [1, 2]. Internal hernias are a rare but potentially fatal complication following laparoscopic RNYGB surgery with an incidence of 1–10% and a mortality of nearly 50% if bowel strangulation is present [3–5]. As previously described, surgically-created mesenteric defects serve as common sites for bowel herniation, with those involving the transverse mesocolon, Peterson’s space and Brolin’s space being the most common following RNYGB [6, 7]. The routine closure of these spaces has significantly reduced rates of internal hernias by approximately 70% [8].
The ‘anti-obstruction stitch’ or ‘Brolin’s stitch’ is another technique that was historically implemented to reduce rates of internal herniation due to kinking at the level of the jejunojejunal (JJ) anastomosis and involves fixing the common channel (CC) immediately distal to the anastomosis to the stapled end of the biliopancreatic (BP) limb via a seromuscular stitch [9]. This case report details the management of a patient with an unfortunate incident of internal herniation of the distal CC through the defect created by the Brolin’s stitch and the stapled closure of the enterotomy resulting from the creation of the JJ anastomosis.
Case result
The patient is a 34-year-old female with a pre-operative BMI of 40 mg/m2 who presented with acute onset (<24 hours) epigastric pain, nausea and dry heaves approximately 1 month following an uncomplicated laparoscopic retrogastric/retrocolic RNYGB with concomitant hiatal hernia repair and cholecystectomy. On arrival, she was hemodynamically stable with a softly distended and tender but non-peritoneal upper abdomen. Lab work including WBC and lactate were unremarkable. Computed tomography (CT) imaging revealed a dilated remnant stomach, BP limb and roux limb with a patent JJ anastomosis but a decompressed CC with concern for an internal hernia (Fig. 1).
Figure 1.
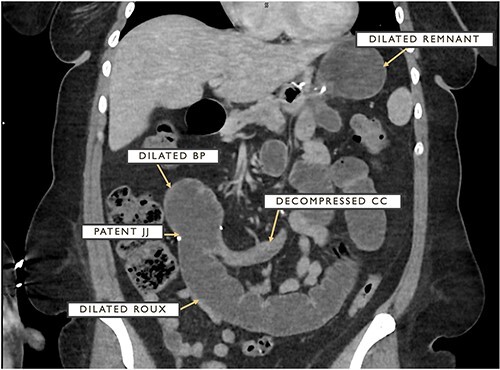
CT cross-section demonstrating dilated remnant stomach, BP limb and roux limb as well as a patent JJ anastomosis with a distally decompressed CC.
The patient underwent an urgent diagnostic laparoscopy with a noted herniation of the CC in between a 2-cm defect from the Brolin stitch and the stapled closed common enterotomy of the jejunojejunostomy. The anatomic landmarks and site of herniation are depicted in a different patient in Fig. 2. This herniated bowel was carefully and successfully reduced laparoscopically with subsequent visible decompression of previously dilated roux and BP limbs and remnant stomach. The defect was carefully closed with two simple-interrupted stitches with care taken not to narrow the JJ anastomosis or CC outflow. Further suction decompression of the bowel was completed by intentional enterotomies involving the BP and roux limbs that were then inconsequentially stapled, excised and removed. Her hospital course was complicated by an ileus requiring the placement of a decompressive remnant gastrostomy tube by interventional radiology on post-operative day 2. Following the resolution of her ileus, this remnant gastrostomy tube was clamped around the clock and her diet was slowly advanced. The patient was discharged uneventfully on post-operative day 5 with good pain control and diet tolerance.
Figure 2.
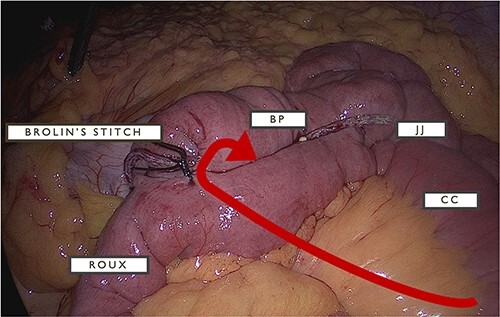
The arrow depicts the location of defect enabling herniation of CC between JJ anastomosis and Brolin’s stitch with relative locations for BP and roux limbs.
Discussion
The placement of the Brolin stitch was shown to resolve obstruction at the JJ due to kinking of the bowel at this location in nearly 1400 consecutive patients [10]. Despite this technical improvement, we encountered an ironic case of small bowel herniation between this stitch and the JJ anastomosis. We predict that rates of internal hernias at this site can be reduced with the careful and intentional placement of the Brolin stitch such that the distance to the JJ staple line is minimized. If the defect is large during the index operation, the placement of another simple interrupted seromuscular bite of the BP limb and CC can help reduce the risk of herniation into this space.
Contributor Information
Krishna Patel, Department of General Surgery, OhioHealth Riverside Methodist Hospital, Columbus, OH 43214, USA.
Vinnie Serapiglia, Department of General Surgery, OhioHealth Riverside Methodist Hospital, Columbus, OH 43214, USA.
Anthony N Rizzo, Department of General Surgery, OhioHealth Riverside Methodist Hospital, Columbus, OH 43214, USA.
Jaya Varre, Department of General Surgery, OhioHealth Riverside Methodist Hospital, Columbus, OH 43214, USA.
Thomas Sonnanstine, Department of General Surgery, OhioHealth Riverside Methodist Hospital, Columbus, OH 43214, USA.
Conflict of interest statement
None declared.
Funding
None declared.
References
- 1. Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the Fourth IFSO Global Registry Report 2018. Obes Surg 2019;29:782–95. [DOI] [PubMed] [Google Scholar]
- 2. Mitchell BG, Gupta N. Roux-En-Y Gastric Bypass. Treasure Island (FL): StatPearls Publishing; 2023. [PubMed]
- 3. Geubbels N, Lijftogt N, Fiocco M, et al. Meta-analysis of internal herniation after gastric bypass surgery. Br J Surg 2015;102:451–60. [DOI] [PubMed] [Google Scholar]
- 4. Ende V, Devas N, Zhang X, et al. Internal hernia trends following gastric bypass surgery. Surg Endosc Published online June 22 2023;37:7183–91. [DOI] [PubMed] [Google Scholar]
- 5. Merali HS, Miller CA, Erbay N, Ghosh A. Importance of CT in evaluating internal hernias after Roux-en-Y gastric bypass surgery. J Radiol Case Rep 2009;3:34–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Aghajani E, Nergaard BJ, Leifson BG, et al. The mesenteric defects in laparoscopic Roux-en-Y gastric bypass: 5 years follow-up of non-closure versus closure using the stapler technique. Surg Endosc 2017;31:3743–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Iannelli A, Facchiano E, Gugenheim J. Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg 2006;16:1265–71. [DOI] [PubMed] [Google Scholar]
- 8. Altieri MS, Carter J, Aminian A, et al. American Society for Metabolic and Bariatric Surgery literature review on prevention, diagnosis, and management of internal hernias after Roux-en-Y gastric bypass. Surg Obes Relat Dis 2023;19:763–71. [DOI] [PubMed] [Google Scholar]
- 9. Brolin RE. The antiobstruction stitch in stapled Roux-en-Y enteroenterostomy. Am J Surg 1995;169:355–7. [DOI] [PubMed] [Google Scholar]
- 10. Brolin R. How to perform an antiobstruction stitch. Bariatr Times 2011;8:8–9. [Google Scholar]


