Abstract
Purpose of Review
The purpose of this review is to discuss the use of point-of-care ultrasound for sideline youth sports coverage.
Recent Findings
Participation in youth sports has been increasing, with trends that athletes are specializing earlier and competing at higher levels at younger ages (NSCH 2019, Fabricant 2013). Point-of-care ultrasound (POCUS) utilizes non-invasive imaging to diagnose and manage various musculoskeletal conditions ranging from traumatic injuries, such as fractures and intramuscular hematomas, to early screening for conditions such as asymptomatic knee lesions. Since it is well-tolerated by children and adolescents and allows for easy accessibility for sideline care, POCUS could provide a strong alternative to other imaging modalities such as x-ray and magnetic resonance imaging (MRI) as both have their limitations. Youth sideline sports coverage could be enhanced with immediate medical attention from ultrasound-trained medical professionals. On the sidelines of a traumatic injury, POCUS expedites patient care with immediate examination of acute injuries. In low resource and hard-to-reach locations such as a rural youth sporting event, it can be key in the triaging of injuries. As a supplement to a physical exam, the risk of a misdiagnosis is reduced, and a long, expensive trip to the hospital for unnecessary imaging studies may be avoided.
Summary
Ultrasound is a versatile, non-invasive, radiation-free imaging modality that serves as an accessible option for sideline coverage at youth sporting events. Ultrasound is well-tolerated by children and adolescents. It can be used to evaluate, diagnose, and manage a range of musculoskeletal conditions at the sidelines of youth sports.
Keywords: Musculoskeletal ultrasound, Point-of-care ultrasound (POCUS), Pediatric orthopedics, Sports medicine, Youth sports, Sideline coverage
Introduction
Ultrasound is a form of diagnostic imaging that evaluates structures within the body through the production and reception of sounds waves to produce an image. It is a non-invasive, radiation-free, accessible medical imaging modality that can be used in various clinical settings [1••]. Unlike other imaging modalities, ultrasound allows providers to perform dynamic exams with capability of evaluating tissues in multiple planes. Additionally, providers who utilize ultrasound can interact with patients and families during imaging, as well as easily compare contralateral side findings [1••].
Ultrasound as a diagnostic and procedural tool is becoming more of a standard of practice in sports medicine clinics. The American Medical Society for Sports Medicine (AMSSM) established a musculoskeletal ultrasound curriculum in 2010 for sports medicine fellows which was recently expanded [2••]. Sports ultrasound was termed in 2015 to recognize the significant role ultrasound holds in sports medicine clinic evaluations both musculoskeletal and non-musculoskeletal applications. In 2017, the Accreditation Council for Graduate Medical Education (ACGME) further reiterated the importance of sports ultrasound by adding ultrasound training into the core program requirements for all sports medicine fellowships. The implementation of this training ensures that fellows are properly educated and prepared to utilize sports ultrasound in their practice [2••].
To understand the role of ultrasound in youth sideline evaluations, one must first understand how ultrasound works. In addition to evaluating the cortex of bone, ultrasound produces high-resolution of ligaments, tendons, joints, and nerves—as long as they are not blocked by bone. Ultrasound has multiple different transducer attachments that allow for a broad evaluation. For sideline musculoskeletal usage, especially in youth, a high frequency linear transducer is most often used. Curvilinear transducers, which evaluate deeper structures with their low frequencies, are rarely needed given that youth athletes tend to have a smaller body habitus making visualization of deep structures possible with a high frequency transducer. Just like other imaging, ultrasound utilization is operator dependent. In order to be successful, proper training in ultrasound is required. When employed on the sideline, other factors should be considered specific to youth, including patient cooperation [1••] exposure of the affected area (i.e., uniforms or protective clothing may inhibit access) and having the proper equipment.
An emerging application of ultrasound is its role in diagnosing and managing pediatric musculoskeletal conditions. With its portability, low costs, and dynamitic testing abilities, it has become a topic of conversation as an application in sideline pediatric sports medicine. Implementation of portable ultrasound units on sidelines allows for immediate, high resolution imaging evaluation (Fig. 1). Ultrasound has been considered portable relative to radiographs and MRIs, but newer technology has led to ultrasound transducers connecting to a cellphone or tablet, even with wireless capabilities (Fig. 2). Ultrasound allows for optimized comfort of the patient in various positions for immediate investigation of the injury [3]. Although this is an emerging field with little scientific literature, sideline ultrasound use improves communication between the sports team, athletes, and families to prevent misinformation or delayed diagnoses [4, 5]. Sideline ultrasound use requires no insurance pre-authorization, while images can be saved and shared electronically with colleagues for instant consultation. Many don’t need reminding that MRI is the non-invasive “gold standard” for diagnosis of soft tissue, ligament, and tendon injuries, but obtaining these images is costly for patient families and requires extra time, not to mention the importance of remaining motionless during examination in a claustrophobic setting. Remaining motionless is challenging enough for adults, but even more challenging for youth. On the sidelines of a traumatic injury, POCUS expedites patient care with immediate examination of acute injuries [6]. In low resource and hard-to-reach locations such as a rural youth sporting event, it can be key in the triaging of injuries. As a supplement to a physical exam, the risk of a misdiagnosis is reduced, and a long, expensive trip to the hospital for unnecessary imaging studies may be avoided [7]. Additionally, Sideline ultrasound also carries a role in injury-prevention screenings and return to play evaluations, both of which can further benefit athletes and sports teams [6]. Therefore, the purpose of this paper is to summarize current literature and the clinical experience of the authors on point-of-care ultrasound in pediatric sports sideline coverage. This will be done by reviewing structures and providing ultrasound images that may be injured during a youth sports event that can be visualized with ultrasound.
Fig. 1.
Examples of different types of portable ultrasounds
Fig. 2.
Sports medicine physician doing a point-of-care sideline ultrasound using wireless ultrasound with smartphone application
Acute Injury
Muscle and Tendon Injuries
Ultrasound can be an excellent triaging tool for differential diagnoses such as muscular and tendon injuries. Although significant tendon injuries do occur in youth athletes, most commonly these consist of tendon strains or tendinitis [8]. When tendon tears do occur, they can be readily assessed on sideline ultrasound evaluation. Incomplete tears would appear as focal hypoechoic or anechoic defects in the tendon that do not extend to both surfaces of the tendon, often associated with some associated tendon thickening [9–11]. Full tears can be seen as full thickness disruptions with retraction of the torn edges and the presence of a hematoma [9] (Fig. 3).
Fig. 3.
Long axis view of Achilles tendon. Complete Achilles tendon tear. Notice hypoechoic defect (arrow) spanning the entire tendon. Able to visualize the proximal (left) and distal (right) ends of the tendon next to the defect
Ultrasound can also be very effective in identifying the severity of muscle injuries including tears and hematomas. Patterns such as an intramuscular collection of fluid can be seen in hematomas. These are often accompanied by a loss of normal muscle striation pattern. Partial muscle tears may also exhibit a hyperechoic halo around the area of injury without but lack the full thickness hypoechoic injury throughout the muscle seen in full tears. Full-thickness tears show complete discontinuity of muscle fibers with a hematoma and tendon retraction [12, 13] (Fig. 4a and b).
Fig. 4.
a Short axis view of anterior thigh. Thigh intramuscular hematoma. Notice large hypoechoic intramuscular lesion (arrow) without normal muscular striations signifying hematoma. Femur is deep to the hematoma. b Short axis view of anterior thigh. Healing thigh intramuscular hematoma. Notice significant decrease in hematoma and near complete restoration of normal muscular architecture
Ligament and Joint Injuries
Ultrasound can adequately visualize ligament injuries, especially the more superficial injuries. Although MRIs are considered the gold standard for ligament injuries, sideline ultrasound allows for quick visualization without the constriction of predetermined slice thicknesses. Ultrasound has been shown to accurately identify foot and ankle ligaments [14•, 15•], finger pulleys [16, 17], and joint collateral ligaments which has easy crossover to the sideline setting [18]. Not only can sideline ultrasound visualize these structures, but ultrasound allows to test for the function of a ligament by visualizing the joint gapping with stress testing [19]. See the images of a normal elbow UCL and the amount of ulnohumeral gapping compared to the image of the contralateral injured UCL with increased ulnohumeral gapping (Fig. 5a and b).
Fig. 5.
a Long axis view of ulnar collateral ligament. Normal appearing elbow UCL ligament (arrow) with medial epicondyle (ME). Notice humeroulnar joint space deep to UCL ligament. b Long axis view of ulnar collateral ligament. Elbow UCL tear (arrow). Notice hypoechoic signal spanning the entire UCL signifying complete UCL tear. Notice increased humeroulnar joint space deep to UCL ligament. ME, medial epicondyle
Although recent studies demonstrate that point-of-care ultrasound provides assistance in sideline diagnosis of ACL, PCL, and meniscal injuries [20•, 21••], this continues to be a point of study. Further studies have shown that ultrasound can identify direct and indirect findings of meniscal tear such as linear hypoechoic defects along the meniscus, a parameniscal cyst, or a joint effusion which could be seen secondary to meniscal tear [21••, 22]. However, identifying a joint effusion is within the capabilities of ultrasound and something that is learned on the fundamental level. Traumatic knee effusions in the youth population is likely one of four etiologies: intra-articular fracture, patellar instability, ACL tear, or isolated meniscal tear [23]. Looking for joint effusions applies to all joints which allows for screening acute intra-articular injury such as fracture [24] (Fig. 6).
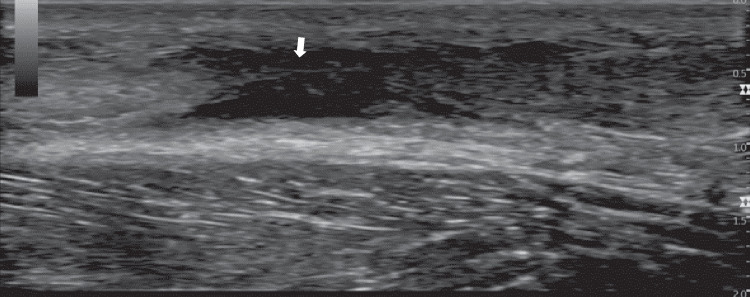
Fig. 6.
Long axis view of suprapatellar recess. Knee effusion. Notice fluid collection (arrow) within the suprapatellar bursa signifying knee effusion
When a shoulder dislocation occurs in an acute setting, ultrasound can be used to immediately identify the direction of dislocation. Anterior, lateral, and posterior views can be used to analyze the position of the head of the humerus relative to the glenoid. Thus, a reduction can be performed more accurately and can be confirmed immediately [25]. These same principles can aid in other joint dislocations (Fig. 7).
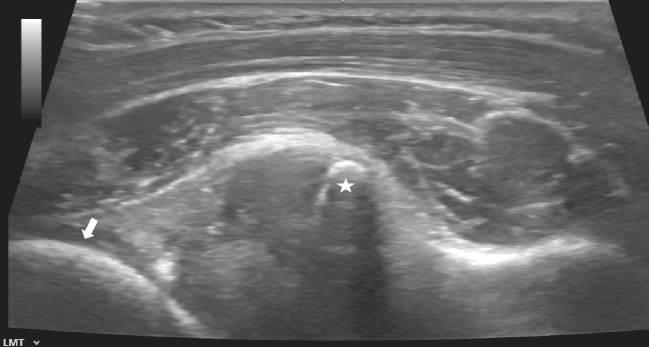
Fig. 7.
Axial view of posterior shoulder. Anterior shoulder dislocation. On this posterior shoulder view, notice humeral head (arrow) location relative to the glenoid (star)
Fractures
Since 1988, ultrasound has been documented as a tool to aid in the diagnosis and treatment of pediatric fractures [26, 27]. On ultrasound, fractures can be seen as disruptions of the cortex, often with anechoic or hypoechoic fluid collections that represent a hematoma at the fracture site [28] (Fig. 8). Avulsion fractures occur when a musculotendinous unit pulls off the piece of cartilage and/or bone. (Fig. 9). This is almost exclusively occurs in the pediatric and adolescent population [29] and can likewise be seen on ultrasound [30]. One can expect to find displacement of the apophyseal or epiphyseal cartilage which sometimes can have associated bone with it.
Fig. 8.
Long axis view of clavicle. Clavicle fracture. Notice disruption of clavicle cortex (arrow). Also notice surrounding hypoechoic structure signifying a hematoma
Fig. 9.
Sagittal view of anterior hip. Anterior inferior iliac spine (AIIS) avulsion fracture. Notice separation (arrow) of AIIS fragment (star) from the pelvis
Research has found ultrasound especially capable for evaluating fractures of the distal forearm and carpal bones with a sensitive, specificity, positive predictive value all above 90% with a negative predictive value of 83% [31]. This suggests that sideline ultrasound, in properly trained hands, can quickly and accurately assess for fractures in these areas. This is clinically helpful given the high fracture rate found in youth sports [32]. In the perspective of a medical provider providing sideline coverage, this tool for evaluating fractures can help with immediate triage. It can be key in assessing the stability of an extremity which can be combined with the physical assessment of functionality to guide return to play decisions [33–35].
Focused Assessment with Sonography for Trauma (FAST)
Furthermore, there are many non-musculoskeletal applications of sideline ultrasound which demonstrate the spectrum of sideline ultrasound versatility and relevance. Emergencies requiring immediate care, ultrasound protocols such as focused assessment with sonography for trauma (FAST) can diagnose conditions such as pulmonary edema on the sidelines of open-water sports and internal organ injury demonstrating that ultrasound does have capabilities to evaluate for internal organ injury [36–38]. However, these non-musculoskeletal applications of sideline ultrasound are outside the scope of this musculoskeletal review journal.
Screening
Ultrasound can be utilized on the sideline or in the training room as a screening method. Studies in young athletes across multiple sports screened for tendon changes in asymptomatic athletes [21••, 39•]. Some studies suggest that they may be at risk of developing symptoms related to tendinopathy [40••, 41]. Preliminary studies have also been performed to evaluate and screen for osteochondral abnormalities of joints. This is visualized as irregularity of the normal articular cartilage and subchondral bone of the joint (Fig. 10).
Fig. 10.
Sagittal view of femoral condyle. Femoral condyle osteochondral lesion. White arrow demonstrates area of loss of normal contour of articular surface
Conclusion
The purpose of this review was to assess the usefulness of point-of-care ultrasound for evaluating pediatric musculoskeletal injuries on the sideline. The portability, radiation-free, non-invasive, and dynamic nature of ultrasound makes it an excellent candidate for sideline use [1••, 42]. Although there is limited literature on ultrasound in the pediatric athlete population, the data supports the feasibility of POCUS for youth sideline athletes as a productive alternative to MRI in immediate care settings.
On the sideline, there is a wide range of injuries that can be seen in an acute setting. MRIs and radiographs remain the gold standard in imaging sports injuries; however, both have significant drawbacks that US can reduce.
Ultrasound does not expose patients to radiation, produces instant results, and allows for contralateral comparison as a component of the evaluation [43]. Sideline POCUS can diagnose fractures [31], joint injuries [25, 44], muscle and tendon injuries [9], and foot, ankle, and collateral ligament injuries [14•, 15•, 19]. As soon as injury is determined, a decision on an athlete’s ability to return to play can be made [45].
Ultrasound has also been shown to be used as a screening tool for assessing the risk for future injuries in a handful of conditions and will likely play a bigger role for screening other conditions in the future [21••, 39•, 41, 46, 47].
Drawbacks to ultrasound include the training required to adequately and confidently utilize it. While some injuries may be easily seen, some require more experience. Increased ultrasound training is being implemented into sports medicine leading to more providers possessing a higher ultrasound proficiency [2••]. Technology allows for almost instantly transmissioned images remotely for imaging consultation [48••]. This provides a role for ultrasound use in low-resource settings or when less-experienced providers seek aid in interpretation. As US technology and proficiency continues to improve, these limitations will continue to be mitigated.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jacob C. Jones, Email: Jacob.jones@tsrh.org
Cassidy Schultz, Email: Cassidy.schultz@tsrh.org.
Caroline Podvin, Email: Caroline.Podvin@tsrh.org.
David Mikhail, Email: David.Mikhail@utsouthwestern.edu.
Luke C. Radel, Email: radel.luke@mayo.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.•• de Borja C, Watkins R, Woolridge T. Common ultrasound applications for pediatric musculoskeletal conditions. Curr Rev Musculoskelet Med. 2022;15(6):447–55. 10.1007/s12178-022-09788-x. Case-based study that summarizes the use of ultrasound for diagnosis and management of common pediatric musculoskeletal conditions. [DOI] [PMC free article] [PubMed]
- 2.Hall MM, et al. American Medical Society for Sports Medicine sports ultrasound curriculum for sports medicine fellowships. Br J Sports Med. 2022;56(3):127–137. doi: 10.1136/bjsports-2021-103915. [DOI] [PubMed] [Google Scholar]
- 3.Takundwa P, Chen L, Malik RN. Evaluation of hip pain and management of toxic synovitis in the ultrasound era. Pediatr Emerg Care. 2021;37(1):34–38. doi: 10.1097/PEC.0000000000002314. [DOI] [PubMed] [Google Scholar]
- 4.Fukushima Y, et al. A review and proposed rationale for the use of ultrasonography as a diagnostic modality in the identification of bone stress injuries. J Ultrasound Med. 2018;37(10):2297–2307. doi: 10.1002/jum.14588. [DOI] [PubMed] [Google Scholar]
- 5.Guillodo Y, Saraux A. Soccer World Cup 2010: Evaluation of portable ultrasonography for diagnosing musculoskeletal injuries. J de Traumatologie du Sport. 2013;30(4):240–243. doi: 10.1016/j.jts.2013.10.002. [DOI] [Google Scholar]
- 6.Sofka CM. Ultrasound in sports medicine. Semin Musculoskelet Radiol. 2004;8(1):17–27. doi: 10.1055/s-2004-823012. [DOI] [PubMed] [Google Scholar]
- 7.Nowak MR, et al. Snowboarding injuries: a review of the literature and an analysis of the potential use of portable ultrasound for mountainside diagnostics. Curr Rev Musculoskelet Med. 2009;2(1):25–29. doi: 10.1007/s12178-008-9040-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zbojniewicz AM, et al. Rotator cuff tears in children and adolescents: experience at a large pediatric hospital. Pediatr Radiol. 2014;44(6):729–737. doi: 10.1007/s00247-014-2875-6. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed R, Nazarian LN. Overview of musculoskeletal sonography. Ultrasound Q. 2010;26(1):27–35. doi: 10.1097/RUQ.0b013e3181ce43ed. [DOI] [PubMed] [Google Scholar]
- 10.Cibulas A, et al. Acute Shoulder Injury. Radiol Clin North Am. 2019;57(5):883–896. doi: 10.1016/j.rcl.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Jacobson JA. Musculoskeletal ultrasound: focused impact on MRI. AJR Am J Roentgenol. 2009;193(3):619–627. doi: 10.2214/AJR.09.2841. [DOI] [PubMed] [Google Scholar]
- 12.Blankenbaker DG, Tuite MJ. Temporal changes of muscle injury. Semin Musculoskelet Radiol. 2010;14(2):176–193. doi: 10.1055/s-0030-1253159. [DOI] [PubMed] [Google Scholar]
- 13.Connell DA, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183(4):975–984. doi: 10.2214/ajr.183.4.1830975. [DOI] [PubMed] [Google Scholar]
- 14.Baltes TPA, et al. Diagnostic value of ultrasonography in acute lateral and syndesmotic ligamentous ankle injuries. Eur Radiol. 2021;31(4):2610–2620. doi: 10.1007/s00330-020-07305-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zaottini F, et al. Ultrasound imaging guide for assessment of the intrinsic ligaments stabilizing the subtalar and midtarsal joints. Semin Musculoskelet Radiol. 2020;24(2):113–124. doi: 10.1055/s-0040-1710066. [DOI] [PubMed] [Google Scholar]
- 16.Lutter C, Tischer T, Schöffl VR. Olympic competition climbing: the beginning of a new era-a narrative review. Br J Sports Med. 2021;55(15):857–864. doi: 10.1136/bjsports-2020-102035. [DOI] [PubMed] [Google Scholar]
- 17.Miro PH, et al. Finger flexor pulley injuries in rock climbers. Wilderness Environ Med. 2021;32(2):247–258. doi: 10.1016/j.wem.2021.01.011. [DOI] [PubMed] [Google Scholar]
- 18.Lueders DR, et al. Optimal elbow angle for sonographic visualization of the ulnar collateral ligament. Pm r. 2015;7(9):970–977. doi: 10.1016/j.pmrj.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 19.Kissenberth MJ, et al. Professional pitchers display differences in UCL morphology and elbow gapping during moving valgus stress testing after UCL reconstruction. Orthop J Sports Med. 2021;9(11):23259671211035734. doi: 10.1177/23259671211035734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmadi O, et al. Role of point-of-care ultrasonography (POCUS) in the diagnosing of acute medial meniscus injury of knee joint. Ultrasound J. 2022;14(1):7. doi: 10.1186/s13089-021-00256-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ho CS, et al. On-site ultrasound screens out asymptomatic knee lesions in elite adolescent male basketball players. Int J Med Sci. 2022;19(13):1856–1863. doi: 10.7150/ijms.72299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xia XP, Chen HL, Zhou B. Ultrasonography for meniscal injuries in knee joint: a systematic review and meta-analysis. J Sports Med Phys Fitness. 2016;56(10):1179–1187. [PubMed] [Google Scholar]
- 23.Abbasi D, et al. MRI findings in adolescent patients with acute traumatic knee hemarthrosis. J Pediatr Orthop. 2012;32(8):760–764. doi: 10.1097/BPO.0b013e3182648d45. [DOI] [PubMed] [Google Scholar]
- 24.Scheier E, et al. Children with elbow injuries and sonographic elevated posterior fat pad but no identifiable posterior fat pad on lateral radiographs: a case series. J Ultrasound Med. 2023;42(7):1617–1624. doi: 10.1002/jum.16173. [DOI] [PubMed] [Google Scholar]
- 25.Gleeson T, Blehar D. Point-of-care ultrasound in trauma. Semin Ultrasound CT MR. 2018;39(4):374–383. doi: 10.1053/j.sult.2018.03.007. [DOI] [PubMed] [Google Scholar]
- 26.Nicholson LT, Skaggs DL. Proximal radius fractures in children. J Am Acad Orthop Surg. 2019;27(19):e876–e886. doi: 10.5435/JAAOS-D-18-00204. [DOI] [PubMed] [Google Scholar]
- 27.Tsou PY, et al. Diagnostic accuracy of ultrasound for upper extremity fractures in children: a systematic review and meta-analysis. Am J Emerg Med. 2021;44:383–394. doi: 10.1016/j.ajem.2020.04.071. [DOI] [PubMed] [Google Scholar]
- 28.Neill E, Degesys NF, Graglia S. SONO case series: point-of-care ultrasound for fracture diagnosis. Emerg Med J. 2021;38(11):855–857. doi: 10.1136/emermed-2020-210446. [DOI] [PubMed] [Google Scholar]
- 29.Ferraro SL, et al. Acute pelvic and hip apophyseal avulsion fractures in adolescents: a summary of 719 cases. J Pediatr Orthop. 2023;43(4):204–210. doi: 10.1097/BPO.0000000000002355. [DOI] [PubMed] [Google Scholar]
- 30.Albtoush OM, et al. Avulsion injuries of the pelvis and hip. Rofo. 2020;192(5):431–440. doi: 10.1055/a-1082-1598. [DOI] [PubMed] [Google Scholar]
- 31.Oguz AB, et al. The efficiency of bedside ultrasonography in patients with wrist injury and comparison with other radiological imaging methods: a prospective study. Am J Emerg Med. 2017;35(6):855–859. doi: 10.1016/j.ajem.2017.01.043. [DOI] [PubMed] [Google Scholar]
- 32.Shanmugam C, Maffulli N. Sports injuries in children. Br Med Bull. 2008;86:33–57. doi: 10.1093/bmb/ldn001. [DOI] [PubMed] [Google Scholar]
- 33.Cummings DL, Leggit JC, Quinlan JD. Point-of-care ultrasound in the management of acute shoulder injury. Curr Sports Med Rep. 2016;15(6):423–425. doi: 10.1249/JSR.0000000000000316. [DOI] [PubMed] [Google Scholar]
- 34.Gumina S, Carbone S, Postacchini F. Occult fractures of the greater tuberosity of the humerus. Int Orthop. 2009;33(1):171–174. doi: 10.1007/s00264-007-0512-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patten RM, et al. Nondisplaced fractures of the greater tuberosity of the humerus: sonographic detection. Radiology. 1992;182(1):201–204. doi: 10.1148/radiology.182.1.1727282. [DOI] [PubMed] [Google Scholar]
- 36.Hårdstedt M, et al. Swimming-induced pulmonary edema: diagnostic criteria validated by lung ultrasound. Chest. 2020;158(4):1586–1595. doi: 10.1016/j.chest.2020.04.028. [DOI] [PubMed] [Google Scholar]
- 37.Montoya J, et al. From FAST to E-FAST: an overview of the evolution of ultrasound-based traumatic injury assessment. Eur J Trauma Emerg Surg. 2016;42(2):119–126. doi: 10.1007/s00068-015-0512-1. [DOI] [PubMed] [Google Scholar]
- 38.Wilson MH, et al. Stroke at high altitude diagnosed in the field using portable ultrasound. Wilderness Environ Med. 2011;22(1):54–57. doi: 10.1016/j.wem.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 39.Comin J, et al. The prevalence and clinical significance of sonographic tendon abnormalities in asymptomatic ballet dancers: a 24-month longitudinal study. Br J Sports Med. 2013;47(2):89–92. doi: 10.1136/bjsports-2012-091303. [DOI] [PubMed] [Google Scholar]
- 40.Benitez CL, Daniels B, Colvin AC. Point-of-care radiology service at the US Open Tennis Championships. Skeletal Radiol. 2022;51(12):2257–2261. doi: 10.1007/s00256-022-04128-z. [DOI] [PubMed] [Google Scholar]
- 41.Cook JL, et al. Prospective imaging study of asymptomatic patellar tendinopathy in elite junior basketball players. J Ultrasound Med. 2000;19(7):473–479. doi: 10.7863/jum.2000.19.7.473. [DOI] [PubMed] [Google Scholar]
- 42.Hryhorczuk AL, Restrepo R, Lee EY. Pediatric musculoskeletal ultrasound: practical imaging approach. AJR Am J Roentgenol. 2016;206(5):W62–72. doi: 10.2214/AJR.15.15858. [DOI] [PubMed] [Google Scholar]
- 43.Weil N, et al. Imaging of pediatric lower limb sports injuries. Semin Musculoskelet Radiol. 2021;25(1):123–136. doi: 10.1055/s-0041-1725076. [DOI] [PubMed] [Google Scholar]
- 44.Secko MA, et al. Musculoskeletal ultrasonography to diagnose dislocated shoulders: a prospective cohort. Ann Emerg Med. 2020;76(2):119–128. doi: 10.1016/j.annemergmed.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 45.Monseau AJ, et al. Point-of-care ultrasound diagnosis of tennis leg. Clin Pract Cases Emerg Med. 2019;3(1):36–39. doi: 10.5811/cpcem.2018.11.41022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Simpson M, et al. Effectiveness of non-surgical interventions for rotator cuff calcific tendinopathy: a systematic review. J Rehabil Med. 2020;52(10):jrm00119. doi: 10.2340/16501977-2725. [DOI] [PubMed] [Google Scholar]
- 47.Yu Q, et al. An imaging-based artificial intelligence model for non-invasive grading of hepatic venous pressure gradient in cirrhotic portal hypertension. Cell Rep Med. 2022;3(3):100563. doi: 10.1016/j.xcrm.2022.100563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rigamonti L, et al. An augmented reality device for remote supervision of ultrasound examinations in international exercise science projects: usability study. J Med Internet Res. 2021;23(10):e28767. doi: 10.2196/28767. [DOI] [PMC free article] [PubMed] [Google Scholar]