Abstract
Purpose of Review
First metatarsophalangeal joint sprains or turf toe (TT) injuries occur secondary to forceful hyperextension of the great toe. TT injuries are common among athletes, especially those participating in football, soccer, basketball, dancing, and wrestling. This review summarizes the current treatment modalities, rehabilitation protocols, and return-to-play criteria, as well as performance outcomes of patients who have sustained TT injuries.
Recent Findings
Less than 2% of TT injuries require surgery, but those that do are typically grade III injuries with damage to the MTP joint, evidence of bony injury, or severe instability. Rehabilitation protocols following non-operative management consist of 3 phases lasting up to 10 weeks, whereas protocols following operative management consist of 4 phases lasting up 20 weeks. Athletes with low-grade injuries typically achieve their prior level of performance. However, among athletes with higher grade injuries, treated both non-operatively and operatively, about 70% are expected to maintain their level of performance.
Summary
The treatment protocol, return-to-play criteria, and overall performance outcomes for TT injuries depend on the severity and classification of the initial sprain. For grade I injuries, players may return to play once they experience minimal to no pain with normal weightbearing, traditionally after 3–5 days. For grade II injuries, or partial tears, players typically lose 2–4 weeks of play and may need additional support with taping when returning to play. For grade III injuries, or complete disruption of the plantar plate, athletes lose 4–6 weeks or more depending upon treatment strategy.
Keywords: Turf toe, First metatarsophalangeal (MTP) joint, Hallux rigidus, Return to play, Rehabilitation, Postoperative performance
Introduction
Turf toe (TT), or sprains of the first metatarsophalangeal (MTP) joint, are most commonly sustained from forceful hyperextension of the great toe and lead to an impairment in athletes’ overall agility and abilities to push-off, accelerate, and cut [1, 2]. Although football players have the highest incidence of TT injuries, this pathology is also common in soccer, basketball, tennis, dancing, volleyball and wrestling athletes [3]. The incidence of TT injuries has increased following the widespread use of artificial turf, which is more rigid, and which places more strain on players’ feet. If severe, neglected, or improperly diagnosed, these injuries can lead to long-term sequelae, including loss of push-off strength, decreased athletic performance, joint stiffness, pain, arthrosis and joint deformity [4]. This review summarizes the current treatment modalities, rehabilitation protocols following each modality, return-to-play (RTP) criteria, and performance outcomes of patients that have sustained TT injuries.
Anatomy and Biomechanics
The first MTP joint functions as a hinge and sliding joint. Four bones, nine ligaments, and three muscular attachments comprise the first MTP joint. There is little bony stability due to the shallow articulation between the convex metatarsal head and the concave base of the proximal phalanx [5]. Therefore, the capsuloligamentous soft tissue structures surrounding the first MTP joint account for the majority of its stability [1]. In particular, the plantar plate, comprised of a thickening of the joint capsule, is the strongest stabilizer [5].
Mechanism of Injury
TT injuries are sustained after hyperextension of the plantar capsule, which results in a sprain of the capsuloligamentous structures that provide stability to the first MTP. The most common mechanism of injury occurs when an athlete’s foot is planted with the heel off the ground, and the great toe is hyper-dorsiflexed (Fig. 1) [6]. Additionally, excessive valgus stress during push-off can also cause damage to the capsule surrounding the first MTP. Other mechanisms occur when the great toe is jammed towards the front of an athletic shoe while stopping short [1, 2].
Fig. 1.

Axial loading of the foot in equinus, resulting in hallux MTP joint hyper-dorsiflexion injury (turf toe)
Classification
Although first described by Clanton and Ford in 1994 [7], the Anderson criteria has become the standard for TT classification. The Anderson criteria uses physical exam and radiographic findings to differentiate TT injuries into three categories (Table 1) [8]. Grade 1 injuries involve an acute sprain without any bony pathology or joint instability. Patients with grade 1 injuries are typically able to weight bear and have normal range of motion (ROM). Partial tear injuries to the plantar structures comprise grade 2 injuries. These patients have restricted ROM and difficulty bearing weight secondary to pain. Grade 3 injuries are the most severe, constituting a complete tear of the plantar structures with disruption of the plantar capsule or plate. There may be evidence of sesamoid bone migration on exam or radiographs. There will be frank instability of the first MTP joint along with hallux flexion weakness, decreased ROM, difficulty weight bearing, and significant ecchymosis and swelling.
Table 1.
Classification, treatment, and RTP for turf toe injuries
| Grade | Description/findings | Treatment | RTP |
|---|---|---|---|
| I |
• Acute sprain of the plantar structures • Localized swelling • Minimal ecchymosis • Lack of obvious hallux valgus deformity • Negative Lachman test • Sesamoid to proximal phalanx distance of 2 mm on hallux dorsiflexion |
Symptomatic |
• Return as tolerated • May need taping* on return to play • RTP criteria: minimal to no pain with weight bearing/normal plantar pressure |
| II |
• Partial tear of the plantar structures • Moderate swelling • Restricted motion due to pain |
Walking boot with crutches as needed for 2-4 weeks |
• Loss of playing time for up to 2 weeks • May need taping* on return to play • RTP criteria: achieve pre-injury level of performance during practice |
| III |
• Complete disruption of the plantar structures • Significant swelling/ecchymosis • Hallux flexion weakness • Frank instability of MTP joint • Sesamoid fracture |
Long-term immobilization in boot or cast, surgical reconstruction |
• Loss of playing time for at least 4–6 weeks, possibly up to 10 to 16 weeks depending on sport and position** • Likely to need taping on return to play • RTP criteria: 50 to 60 degree arc of painless first MTP motion |
Epidemiology
In a cross-sectional analysis of all NCAA athletes competing in fifteen different sports from 2009 to 2015, turf toe was the fourth most common foot injury (behind foot/toe contusion, midfoot injury, and plantar fascia injury), with an incidence of 0.040 per 1000 athlete-exposures [3]. The greatest incidence of turf toe injuries was observed among football players, followed by basketball and European football (i.e., soccer) players. A separate analysis of NCAA Injury Surveillance System data spanning over 10 years across twenty-five sports demonstrated that TT was the most common foot injury overall, comprising 11.5% of documented injuries [11]. Among intercollegiate American football players, there was an 11% incidence of TT injury or first MTP dislocation [12]. The estimated incidence is several fold higher at the professional level. Between 30 and 45% of professional American football players claim that they have experienced a TT injury [6, 13], with over 80% of those injuries occurring on artificial turf [6]. Researchers proposed that this is the result of a combination of rigid synthetic surfaces and lighter, more flexible shoes, causing hyperextension injuries [14].
However, with the advent of newer generations of artificial turf, the rates of TT injuries are decreasing [15–17]. First introduced in 1960, first-generation artificial turf, commonly known as AstroturfTM, has short grass fibers padded into a carpet over concrete. With the goal of reducing stiffness, second-generation artificial turf used thicker grass fibers (22–25 mm), a rubber base, and/or sand fillings. Third-generation turf was originally designed for soccer fields, with longer fibers (50–60 mm) and a sand and/or rubber infill [18].
Studies of professional soccer players have shown that third-generation turf has similar injury rates seen on normal grass [16, 17].
Risk Factors
Several studies agree that certain risk factors can predispose athletes to TT injuries. In particular, an analysis of NCAA football injuries found that TT injuries were 13.7 times more likely to occur in games compared to practices or scrimmages [15], which is higher than the 8- to 9-fold difference in injury rates noted for all NCAA football injuries [19]. Interestingly, there was no significant difference in injury rate between home and away games [15]. Athletes that play at the Division I level for football were more likely to be injured compared to Division II and III players [15]. As mentioned earlier, artificial surfaces have been associated with up to an 85% increased risk of TT injury compared to grass [15].
Specific athlete positions are predisposed to TT injuries. Running backs, quarterbacks, and wide receivers comprised over 50% of players with TT injuries, followed by defensive tackles [15]. Athletes with increased weight were more likely to be injured, as well as those with prior 1st MTP injury [13].
Additionally, athletes wearing shoes with increased toe box flexibility and fewer cleats (i.e., the rubber-sole, multi-cleat shoe) are more susceptible to TT injuries [6]. Risk factors for TT injuries are summarized in Table 2.
Table 2.
Risk factors for turf toe injury
| • Games > practice |
| • Division I football > Division II or III |
| • Artificial surfaces |
|
• Football positions most susceptible: ○ Offensive players: running backs, quarterbacks, wide receivers ○ Defensive players: defensive tackles |
| • Increased athlete weight |
| • Prior first MTP injury |
| • Increased shoe toe box flexibility |
| • Decreased number of cleats |
| • Increased foot pronation |
Initial Management and Workup
Sideline Management
Initial sideline management when a TT injury is suspected is crucial to determine whether a player should be held from play. If any evidence of instability is detected on physical exam, the player should refrain from playing for the rest of the game or practice [21]. Instability should be evaluated by gently passing the toe through full range of motion and assessing specifically for loss of resistance to dorsiflexion [22]. Applying gentle varus and valgus stress on the joint will allow the examiner to determine collateral ligament integrity. Strength of great toe dorsiflexion and plantarflexion should be evaluated to assess potential injury to flexor or extensor tendons. Additional physical exam maneuvers should assess for crepitus, indicating a potential fracture, and the presence of first MTP joint dislocation or subluxation. If a dislocation is obvious, and immediate imaging is not available at the sports facility, a closed reduction should be attempted to avoid a delay in joint realignment [21]. After the closed reduction is performed, the player’s MTP joint stability should be assessed with a dorsal-plantar drawer test (i.e., Lachman’s test), as this may influence the player’s injury management [21]. During this maneuver, the second toe is grasped between the thumb and index finger, while the MTP joint is stressed in a dorsal direction. Increased mobility of the first MTP joint results in a positive drawer sign and indicates joint instability [23].
Radiographic Workup
After appropriate initial sideline management, radiographic imaging is necessary to evaluate the extent of the injury and determine treatment options. The most crucial radiographs include weight-bearing anteroposterior (AP) and lateral views, as well as non-weight-bearing oblique views of the foot [21, 24]. If pain allows, weight-bearing images should be completed with 100% of the weight on the injured foot rather than spread equally between both feet. AP radiographs should include both the injured and contralateral hallux MTP joints, as this allows for better evaluation of asymmetry and may help in identifying subtle sesamoid migration.
Besides a sign of an obvious sesamoid fracture, bony flecks may also indicate capsular avulsion, sesamoid diastasis, or sesamoid retraction [21]. Specifically, proximal migration of one or both of the sesamoids suggests plantar plate rupture (Fig. 2) [25]. Additionally, the presence of an intra-articular loose body may be indicative of a compressive fracture of the metatarsal head [26]. Any evidence of bony pathology increases the severity of the injury, resulting in grade II or grade III classification, and may necessitate a longer loss of playing time and potential surgery.
Fig. 2.
Anteroposterior (A) and lateral (B) weightbearing radiographs of turf toe injury in the left foot with subtle proximal migration of the lateral sesamoid (arrow) and mild subluxation of the 1st MTP joint (notched arrowhead) compared to the uninjured foot. (Image courtesy of Dr. Clifford Jeng, Mercy Medical Center)
Magnetic resonance imaging (MRI) may provide further insight regarding the degree of soft tissue injury and is particularly useful when considering any surgical intervention. Both coronal and sagittal views are useful as they can demonstrate injuries to the flexor hallucis longus tendon and capsular injury (including the plantar plate and sesamoid collateral ligaments), respectively [24, 26]. Coronal sequencing is best for identifying metatarsophalangeal ligament tears. Visualization of bone marrow edema and injuries to the joint surface such as an osteochondral lesion or an intra-articular loose body are also possible with MRI [8, 21]. MRI is most appropriate for high-performance athletes in whom a lower threshold of suspicion for soft tissue injury is indicated, for grade II or III injuries when tendon/ligament involvement is likely, and when planning operative intervention [9, 21].
Treatment Options
Non-operative Treatment
All grade I and II TT injuries that do not meet clear surgical indications (Table 3) should be initially managed with rest, ice, compression, and elevation (RICE). Patients should refrain from athletic activities until pain resolves. Anti-inflammatory medications can help reduce initial swelling and pain. Ice should be applied to the area for the three days following injury, at a recommended frequency of three times daily for up to 20 min at a time. After the first 72 h, contrast baths alternating between cold and warm temperatures can also be utilized [26]. Compression of the injured extremity can be accomplished using gauze and tape forefoot dressings. In cases with significant swelling, compression wraps must be monitored closely, as there is a risk of circulation restriction. Concomitant elevation of the foot can further reduce swelling [26]. Patients may benefit from wearing shoes with stiff or rocker-bottom soles to limit motion in the acute post-injury period.
Table 3.
Surgical indications of turf toe injuries
| Acute presentation |
| • Proximal migration of one or both sesamoids (i.e., sesamoid retraction) |
| • Diastasis of bipartite sesamoid |
| • Symptomatic nonunion of fractured sesamoid |
| • Disruption of distal plantar plate attachment |
| • Dorsal plantar instability of the hallux |
| • Traumatic angular deformity of the hallux |
| • Vertical instability (positive Lachman’s test of hallux) |
| • MTP joint disruption (i.e., loose bodies, chondral injuries) |
| • Failed conservative management |
| Chronic presentation |
| • Symptomatic degeneration of MTP joint |
| • Chronic synovitis |
| • Hallux rigidus |
With more severe TT injuries (e.g., grade III injuries), there may be unrecognized subluxation or dislocation with spontaneous reduction. While this may be challenging to detect on physical exam alone, joint laxity (e.g., positive Lachman’s test) indicating injury to the capsuloligamentous structures may suggest a spontaneous instability event; the most reliable clue would likely be a patient who reports feeling the toe pop “out of place” or “back into place.” If joint subluxation or dislocation is suspected to have occurred, the injured extremity can be temporarily immobilized in a short-leg cast, controlled ankle movement (CAM) walker boot, or cast shoe with the hallux MTP joint in slight plantarflexion to allow soft tissue rest. Patients should remain non-weightbearing, with gradual progression of weightbearing with pain resolution [7, 26]. While the decision to discontinue immobilization should be primarily guided by symptoms, it is recommended to immobilize grade II injuries for up to 2 weeks and grade III injuries for up to 6 weeks (Table 4).
Table 4.
Rehabilitation protocol following non-operative treatment of turf toe injuries
| Phase (timeline) | Goals of care | Recommendations |
|---|---|---|
|
Phase 1 (0–2 weeks) |
• Acute pain control • Decrease swelling • Maintain ROM, avoid stiffness |
• Anti-inflammatory medication, RICE • Electrical stimulation (e.g., TENS) • Toe extension/flexion strengthening (e.g., toe crunches, short foot exercises, aquatic exercises) • Joint mobilizations • Limited weightbearing • Tape toe spica, graphite/carbon fiber insole, stiff-sole shoe • Short leg cast, CAM boot, cast shoe (Grades II–III) |
|
Phase 2 (2-6 weeks) |
• Increase weightbearing • Increase strength/ROM • Normalize gait |
• Advance strengthening exercises • Continue joint mobilizations • Stability exercises (e.g., core, ankle, and hips) • Gait training • Tape toe spica, graphite/carbon fiber insole, stiff-sole shoe • Short leg cast, CAM boot, cast shoe (Grade III) |
|
Phase 3 (6-10 weeks) |
• Improve proprioception, balance, endurance, and conditioning • Return to athletic activities |
• Treadmill jogging/running, aqua jogging, single-leg squats, ladder drills, and circuit training • Straight-line running (Grade III) • Cutting drills (Grades I-II) • Tape toe spica, graphite/carbon fiber insole, stiff-sole shoe |
Operative Treatment
Less than 2% of TT injuries require operative intervention; these are usually grade III injuries [11, 15]. Indications for surgical repair in patients with acute and chronic presentations are displayed in Table 3.
Primary repair of the plantar capsuloligamentous complex can be accomplished if sufficient tissue remains attached to the base of the phalanx. This is typically done via a medial approach to the plantar foot or a J incision, where the medial incision is extended horizontally across the first MTP flexion crease. A capsulotomy is then performed, extending longitudinally from the metatarsal neck to the mid-phalanx, thereby allowing visualization of the metatarsosesamoidal compartment [29]. For better access to the lateral plantar plate, a two-incision technique can be utilized. This involves a plantar-lateral or dorsal midline incision over the first MTP in addition to the medial incision [10]. More recently, arthroscopic techniques have emerged using three portals placed dorsomedial, dorsolateral, and direct medial relative to the extensor hallucis longus tendon [30]. While open repair techniques offer improved visualization of the plantar plate and allow for greater control over suture placement, they also involve more soft tissue trauma which theoretically increases the risk of delayed wound healing, infection, and MTP joint stiffness. However, we are not aware of any studies directly comparing open versus arthroscopic approaches for TT repair. In patients with an isolated distal capsular disruption, direct end-to-end repair of the capsule and adjacent soft tissue structures with nonabsorbable sutures is typically sufficient to restore joint stability. If the tissue is inadequate for primary repair, the plantar plate may be advanced by placing suture anchors or drill holes in the proximal phalanx (Fig. 3) [29]. Complete ruptures must be addressed early, as delayed repair can be complicated by scarring and retraction of the proximal plantar plate due to pull of the flexor hallucis tendon [4, 31].
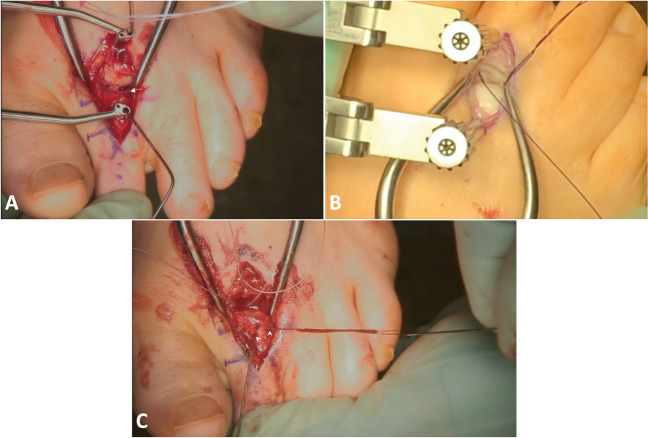
Fig. 3.
Dorsal midline incision with Weil osteotomy and distraction of the metatarsal and proximal phalanx allows for direct visualization of the plantar plate (A, arrow). Suture anchors placed through the plantar plate (B) and passed through dorsomedial and dorsolateral drill tunnels in the proximal phalanx (C, arrowheads) allow for advancement of the plantar plate. (Image courtesy of Dr. Paul Talusan, University of Michigan)
In patients with concomitant injuries, such as sesamoid fractures and/or traumatic hallux valgus, further procedures may be indicated. Intractable sesamoid pain secondary to bursitis, plantar keratosis, or plantar exostosis can benefit from resection of the plantar 50% of the sesamoid [10]. Associated sesamoid fractures that fail conservative management can be addressed with internal fixation or more commonly, partial or total sesamoidectomy. An extraarticular approach is preferred because it allows repair of the flexor hallucis brevis after sesamoid excision. When possible, the larger pole of the fractured sesamoid is preserved, and the remaining fragment is removed [10]. In cases where a total sesamoidectomy is indicated, abductor hallucis longus tendon transfers into the void left by the removed sesamoid can augment postoperative joint stability and flexion strength [4, 31]. If both sesamoids are symptomatic, staged medial and lateral sesamoidectomies may be performed, with the second procedure performed 1 year after the index surgery to reduce the risk of a cock-up deformity (persistent extension of the first MTP joint) [32, 33]. Bone grafting of sesamoid non-unions has demonstrated success for athletes where the loss of push-off strength associated with sesamoidectomy can be detrimental [34].
For patients with TT injury–associated traumatic hallux valgus, a formal bunionectomy can be pursued at the same time as repair. The modified McBride procedure has demonstrated success in these patients, where adductor tendon release, medial eminence resection, and medial capsular tightening can balance the forces acting on the MTP joint [8, 31, 35]. This also minimizes the risk of progressive hallux valgus deformity that can develop following a medial total sesamoidectomy [10].
In patients with persistent disability, joint debridement may reduce symptoms and allow continued participation in sports activities.
Rehabilitation Protocols
Following Non-operative Treatment
Individualized rehabilitation protocols should be guided by pain and swelling. Generally, rehabilitation of first MTP joint injuries can be divided into three phases (Table 4) [27]. The goals of the first phase (0–2 weeks) are to control acute pain and swelling and early ROM to avoid later joint stiffness. Pain management can be accomplished through anti-inflammatory medication, RICE, or electrical stimulation modalities (e.g., transcutaneous electrical nerve stimulation, or TENS). Once initial pain and swelling have subsided, the patient can gradually start strengthening exercises to restore toe extension and flexion (e.g., toe crunches, short foot exercises, aquatic exercises), with addition of joint mobilization as tolerated to reduce pain and increase ROM [9, 28]. At this point, weightbearing is typically limited to walking for grade II injuries, whereas some grade I injuries may be ready to return to practice as soon as symptoms allow.
The goals of the second phase (2–6 weeks) are to gradually increase weightbearing, increase strength and ROM, and normalize gait [27]. Strengthening exercises and joint mobilization should be advanced as tolerated without exacerbating pain. Exercises for the core, ankle, and hips focusing on stability and gait training can also be incorporated.
Limiting dorsiflexion of the injured toe during the early phases of rehabilitation is of principle importance to prevent re-injury and provide comfort. For lower grade injuries, this can be accomplished simply with a tape toe spica, although this is not recommended acutely due to risk of compromising circulation [22, 26, 28]. Alternatively, the patient can switch to footwear with a stiffer sole or utilize an insertable, rigid forefoot insole (e.g., graphite or carbon fiber) with sufficient protection of the great toe, such as with a Morton’s extension (Fig. 4). For grade III injuries with suspected joint subluxation or dislocation, stricter immobilization in a short-leg cast, CAM walker boot, or cast shoe is indicated.
Fig. 4.

Morton’s extension shoe insert (inferior view) protects against excessive dorsiflexion of the great toe by providing a rigid base under the 1st MTP joint
The third phase (6–10 weeks) is aimed at improving proprioception, balance, endurance, and conditioning with the goal of transitioning patients back to athletic activities. Progression to full weight bearing and eventual return to sport should be gradual and once again guided by pain and swelling. The athlete should not return to play until they are able to walk and jog without a limp [26]. The exact time frame may vary between patients based on injury severity and individual pain tolerance. While most grade I and some grade II injuries may be ready for higher impact exercises earlier than 6 weeks, rehabilitation should not be rushed for those that are still limited by pain or swelling. Conservative alternatives to sport include treadmill jogging/running, aqua jogging, single-leg squats, ladder drills, and circuit training [27]. Premature return to full activity without adequate healing can lead to permanently decreased ROM and early osteoarthritis [10]. For patients with grade III injuries, activity should initially be restricted to straight-line running only; cutting drills should be withheld until the patient can perform straight-line runs at full speed without pain [26]. It is also important to continue use of stiff-soled footwear as the athlete begins returning to sport.
Post-operative Rehabilitation
Postoperative rehabilitation of high-grade TT injuries treated surgically can be divided into four phases (Table 5). The primary goals of the first phase (4–6 weeks) are immobilization and structural support, as well as pain control and wound maintenance [4, 26]. Immediately following surgery, a toe spica should be applied with 5 to 10 degrees of plantar flexion to protect against excessive dorsiflexion. The method and duration of immobilization depend on the extent of disruption to the MTP musculoligamentous capsule, provider preference, and patient compliance. A CAM boot should be worn for 8 weeks in cases of partial rupture and 12 weeks in cases of full rupture [26]. For convenience and hygiene, a removable bunion splint with plantar restraints can be worn at night in place of the daytime splint or CAM boot [4]. In cases of traumatic hallux valgus, the toe should also be maintained in slight varus to protect the repair [36]. The patient must remain non-weightbearing during the first 4 to 6 weeks [36, 37]. To reduce stiffness and prevent later arthrofibrosis (e.g., sesamoid adhesions), gentle passive mobilization of the injured toe under supervision is recommended after approximately 1 week [8, 38–40]. These passive ranging exercises should only be performed once incisions are healed. The patient should also be encouraged to perform additional exercises to strengthen other muscle groups and maintain cardiovascular fitness during this phase, so long as they do not involve the injured foot (e.g., core exercises, upper body exercises).
Table 5.
Rehabilitation protocol following operative treatment of turf toe injuries
| Phase (timeline) | Goals of care | Recommendations |
|---|---|---|
| Phase 1 (4–6 weeks postop) |
• Immobilization • Structural support • Pain control • Wound maintenance |
• Icing, electrical stimulation (e.g., TENS) • Non-weightbearing • Daytime — short leg cast, CAM boot, cast shoe (8 weeks for partial rupture, 12 weeks for full rupture) • Nighttime — removable bunion splint • Joint mobilizations under supervision (>1 week) • Exercise other muscle groups (e.g., core, upper body) • Wound checks and suture removal |
| Phase 2 (6–10 weeks) |
• Progressive weightbearing • Improve strength/ROM • Normalize gait |
• Icing, electrical stimulation (e.g., TENS) • Short leg cast, CAM boot, cast shoe (8 weeks for partial rupture, 12 weeks for full rupture) • Protected weightbearing only (tape toe spica, graphite/carbon fiber insole, stiff-sole shoe) • Shoe with wide toe box (full rupture injuries) • Gait training (crutch-assisted or unassisted) • Aerobic exercises with reduced MTP joint load (e.g., biking, aquatic exercises) • Strengthen other muscle groups (e.g., core, hips, ankles, and foot intrinsics) |
| Phase 3 (10–12 weeks) |
• Advance through structured physical rehabilitation • Improve strength/ROM • Re-conditioning • Preparation for return to sports practice |
• Tape toe spica, graphite/carbon fiber insole, stiff-sole shoe • Agility and stability training with progressive loading of MTP joint (e.g., lunges, single leg squats, treadmill jogging, elliptical, ladder drills, box jumps) • Avoid running/sprinting |
| Phase 4 (12–20 weeks) |
• Advanced agility re-conditioning • Preparation for return to full contact sport |
• Tape toe spica, graphite/carbon fiber insole, stiff-sole shoe • Sports-specific drills and exercises • Straight-line running • Multidirectional planting/cutting movements (once running is pain-free) • Return to play (>3 months) |
The goals of the second phase (6–10 weeks) are to improve strength and ROM, progressively bear weight, and normalize gait. Pain and swelling can be concomitantly managed with icing or electrical stimulation modalities (e.g., transcutaneous electrical nerve stimulation, or TENS). At this stage, protected weightbearing with modified footwear is permitted. A stiff-soled shoe, turf-toe plate, carbon fiber insert, or insole with Morton’s extension will prevent excessive dorsiflexion of the injured MTP joint [8]. Tape toe spica may still be used if needed for comfort. Use of protected footwear should be continued for at least 6 months after surgery to reduce the risk of reinjury [26]. For full rupture injuries, the athlete should additionally transition to a shoe with a wide toe box [26]. Gait training can be either assisted (with crutches) or unassisted; this should be guided by pain. It is appropriate to perform aerobic exercises with reduced load bearing on the MTP joint (e.g., biking, aquatic exercises) at this stage, while specific conditioning should focus on strengthening the core, hips, ankles, and foot intrinsics.
Phase three (10–12 weeks) is characterized by advancement through structured physical rehabilitation without return to athletic activity. The goals are continued improvement of strength/ROM, re-conditioning, and preparation for return to sports practice [27]. Progression through this stage should be guided primarily by pain and swelling. The patient should continue use of tape toe spica and rigid insole footwear/inserts to limit excessive dorsiflexion. More advancement movements focusing on agility and stability which place greater load on the MTP joint are permitted (e.g., lunges, single leg squats, treadmill jogging, elliptical, ladder drills, box jumps). Starting with simpler exercises (i.e., exercises which primarily increase loadbearing), the patient should follow a stepwise progression, being essentially pain- and swelling-free before moving to more challenging exercises (i.e., exercises which involve cutting movements or explosive jumping movements). Running/sprinting should still generally be avoided.
The player may return to practice at 3 months postoperatively [26]. This constitutes phase four (12–20 weeks) of the recovery protocol, which focuses on advanced agility re-conditioning, sports-specific drills and exercises, and preparation for return to full contact sport [27]. Most players are not cleared for full RTP by 12 weeks, and initial involvement should be limited to practice only. Again, progression should be guided primarily by pain and swelling. Continued use of modified footwear and/or insertable rigid insoles is recommended. Running is encouraged as tolerated. Once straight-line running can be performed without pain, multidirectional planting and cutting movements are permitted. The player should be able to tolerate essentially all exercises in practice without pain or swelling before being allowed to return to full-contact play.
Return-to-Play and Functional Outcomes
The effect of TT injuries on athletic participation should not be underestimated. Though players with low-grade injuries often respond well to conservative rehabilitation efforts, chronic or severe injuries may be career ending [41, 42]. To put this in perspective, ankle sprains have a 4-fold higher prevalence among football players, but 1st MTP joint injuries still account for more missed games and 60% as many missed practices [20]. A systematic review of 65 patients found that the median RTP time for patients treated nonoperatively was 5.85 weeks (range, 3.00–8.70 weeks) compared with 14.70 weeks (range, 6.00–156.43 weeks) for patients treated surgically [43].
Prompt treatment of TT injuries is essential to minimize long-term complications and achieve successful functional outcomes. Those that are left untreated can lead to permanent MTP joint pain and stiffness, loss of push-off strength, degenerative changes and osteoarthritis, and diminished athletic performance [7, 13, 31, 44]. For athletes who are improperly diagnosed or return to play too early, late sequelae include claw-toe or cock-up toe deformities, progressive hallux valgus, hallux rigidus, and longitudinal tears of the flexor hallucis longus tendon [10]. Late surgical reconstruction may be necessary. However, delayed surgery is made difficult by scarring, contractures, and bony deformities. Up to 50% of athletes may experience persistent pain and stiffness at long-term follow-up [45].
Following Non-operative Treatment
Grade I and II injuries are rarely season-ending (3.0%) or career-ending (1.5%), and functional prognosis is generally favorable [11]. At least one study of NFL athletes has found that 100% of high-grade injuries treated nonoperatively also resume play, though only 78% were able to achieve their prior level of performance [46]. RTP criteria are dictated by both subjective pain levels and objective ROM measurements of the 1st MTP joint. Generally, athletes may resume full activity when full weightbearing, sprinting, and cutting exercises produce minimal pain, and the great toe is able to achieve a 50° to 60° arc of painless motion [4].
Following a grade I injury, low-impact activities can be resumed as tolerated, typically once swelling resolves in 3 to 5 days. Athletes with these injuries are frequently able to continue practicing and competing right away with the aid of shoe inserts and taping to minimize MTP dorsiflexion [8, 10, 28]. Data from the NCAA Injury Surveillance System demonstrates that the average time lost from play due to non-season-ending TT injuries is only 3.3 days among all athletes and only 10 days for football players specifically [3, 15].
Grade II injuries often require longer healing. Some sources suggest permitting athletes to return to play as early as 2 to 4 weeks [21, 22, 26]. However, a systematic review by Hainsworth et al. [47] found that for grade II injuries managed conservatively, time to RTP ranged from 3 to 24 weeks. Lindsey et al. [46] similarly reported that the mean RTP time for patients with high-grade injuries treated nonoperatively was 75.8 days, or nearly 11 weeks. The loss of playing time also depends heavily upon the demands of the patient’s desired activity, including type of sport, level of performance (amateur versus professional), and player’s specific position (i.e., runners and sprinters may require longer recovery) [44, 47]. Interestingly, professional athletes resume play significantly sooner than high school and collegiate athletes, possibly owing to more intensive and dedicated rehabilitation efforts [43].
Long-term implications for pain and other patient-reported outcomes following conservative management of low-grade TT injuries are unclear. In a series of 10 patients with grade I or II pathology, there was significant improvement in AOFAS Hallux scores (51 to 84, p < .001) following treatment [48], although 2 patients (20%) with grade II injuries did not resume their previous activities. There is also an 11% risk of recurrence after low-grade injuries [11]. Nevertheless, athletic performance (as measured by power ratings) among NFL players who return from TT injuries is statistically comparable to uninjured controls as well as to their own pre-injury performance [46, 49, 50], though this may not necessarily hold true for high-grade injuries.
Following Operative Treatment
Unlike low-grade TT injuries, grade III injuries have a much greater potential to be season- (36%) or career-ending (16%) [11]. Open repair of the plantar soft tissue capsule is preferred in these cases, and additional sesamoidectomy and/or abductor hallucis transfer may be indicated for concomitant sesamoid fractures. Recovery duration, likelihood of return to sport, and long-term functional outcomes vary widely based on individual player characteristics, as well as injury severity and chronicity. Of those patients undergoing operative treatment, 71–90% are expected to resume pre-injury activity [30, 35, 44, 47, 48, 51], although the level of performance may suffer in as many as 73% [46]. Coaches and training staff can generally expect a 2- to 4-month rehabilitation window before the player is able to participate in games, although more complicated injuries may further delay recovery [26, 27, 30, 35, 46, 47, 51].
In a study of 19 professional athletes who underwent operative treatment for turf toe injuries, Covell et al. [35] reported that 14 (75%) ultimately returned to their sport, while the remaining players retired after surgery or could only return to a lower level of play. Of those 14 who returned to professional-level play, 5 retired shortly afterwards. This included 4 NFL players, one of whom played for 6 seasons before retiring, one for 3 seasons, one for 2 seasons, and one for 1 season plus the subsequent preseason. The fifth was a collegiate football player who competed for 1 full season before retiring. Nine players remained active in their respective leagues, with one playing for 8 years post-injury, two for 3 years, three for 2 years, two for 1 year, and one for 6 months. RTP time was available for 7 patients and averaged 3.4 months (range, 2–4 months) [35]. Three additional athletes were able to return for the beginning of their subsequent season without missing time. One player missed the first 5 games of the season before returning.
While complications following surgical repair of first MTP joint injuries are uncommon, they can substantially delay RTP and may lead to long-term functional impairment or pain. In the cohort published by Covell et al. [35], one patient experienced flexor hallucis longus tendinitis, one had a longer than expected recovery (although ultimately recovered fully), and one patient who underwent concomitant second toe procedure developed pain and contracture which resolved after surgical debridement. Anderson et al. [44] reported on 9 collegiate and professional athletes who underwent operative treatment for grade 3 injuries with evidence of proximal sesamoid migration and plantar plate disruption. Seven (78%) returned to full activity with minimal pain. One patient developed severe progressive degenerative joint disease, and one had persistent pain upon toe push-off in spite of satisfactory MTP joint stability. Smith et al. [51] reported that at average follow-up of 27.5 months, re-operation was required for only 1 in 15 patients (6.6%) with sesamoid pathology due to persistent pain with plantarflexion and swelling. Importantly, there is a 17% risk of recurrence after high-grade injuries [11].
Injury chronicity and delay in seeking care may also play a role in determining post-operative functional outcomes. Of the 7 players who were able to recall a specific injury date in the study by Covell et al. [35], the mean time from injury to surgery was 4.5 months (range, 1–8 months), with 6 other players reporting progressing great toe pain for at least 1 year prior to presentation. In Smith et al. [51], ten of 15 patients underwent surgery within 6 weeks of their injury, whereas the remaining five experienced an average time delay to treatment of >23 weeks (range, 0.75–36 weeks). Husebye et al. [30] found that the median delay to surgery for uncomplicated grade III injuries without sesamoid migration was 20 months (range, 2–38 months). Although none of these studies have specifically investigated the relationship between injury chronicity and functional outcomes, it is generally accepted that delaying treatment increases the risk for long-term joint disease.
Functional outcomes among athletes who do return to high-level activity after operative treatment are generally favorable. In the study by Smith et al. [51], average AOFAS Hallux score at final follow-up was 91.3 (range, 82–100), and average visual analog scale (VAS) pain score for the toe was 0.7 at rest and 0.8 with physical activity. Husebye et al. [30] reported that at final physical follow-up (median 12 months), 1 (10%) patient had reduced skin sensation, 7 (70%) had minor reduced ROM at the first MTPJ, and 5 of 7 (71%) had persistent subtle valgus deformity. Median patient-reported MOxFQ subscores at 29 months were walking/standing, 2 (range, 0–54); pain, 10 (range, 0–40), social interaction, 0 (range, 0–38), and total score, 6 (range, 0–41). Median VAS pain was 0 (range, 0–2). In a cohort of 14 patients treated operatively by Nery et al. [48], AOFAS Hallux scores improved significantly after surgery (36 to 81, p < .001), although only 10 players (71%) were able to resume their respective sports.
Conclusions
The treatment protocol, RTP criteria, and overall performance outcomes for TT injuries depend on the severity and classification of the initial sprain. For grade I injuries, players may return to play once they either experience minimal to no pain with normal weightbearing, sprinting, and cutting or they achieve a 50 to 60° arc of painless motion, usually after 3–5 days. For grade II injuries, or partial tears, players typically lose 2–4 weeks of play and may need additional support with taping when returning to play. For grade III injuries, or complete disruption of the plantar plate, athletes lose 4–6 weeks or more depending upon treatment. Less than 2% of TT injuries require surgery but those that do are typically grade III injuries with damage to the MTP joint, evidence of bony injury, or severe instability. Rehabilitation protocols for injuries managed non-operatively consist of 3 phases and may last up to 10 weeks. For TT injuries managed operatively, rehabilitation protocols consist of 4 phases and may last up 20 weeks. Without prompt treatment of TT injuries, players can have permanent MTP joint pain and stiffness, loss of push-off strength, degenerative changes and osteoarthritis, and diminished athletic performance. Athletes with low-grader injuries can expect to resume play and achieve their prior level of performance. However, among athletes with higher grade injuries, both treated non-operatively and operatively, about 70% are expected to maintain their level of performance.
Acknowledgements
The authors would like to thank and acknowledge Clifford Jeng, M.D. (Mercy Medical Center) and Paul Talusan, M.D. (University of Michigan), for generously contributing radiographic and intraoperative images.
Declarations
Conflict of Interest
Arjun Gupta, Priya Singh, Amy Xu, Rachel Bronheim, and Claire McDanieal declare that they have no conflict of interest. Amiethab Aiyer has the following disclosures: American Orthopaedic Foot and Ankle Society (board or committee member); Bioventus (paid consultant); Delee and Drez Orthopaedic Sports Medicine — Elsevier (publishing royalties, financial, or material support); Journal of Bone and Joint Surgery — British (editorial or governing board); KCI (paid consultant); Miller’s Review of Orthopaedics — Elsevier (publishing royalties, financial, or material support); Novastep (paid consultant); Smith and Nephew (paid consultant); Vilex (paid consultant)
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Arjun Gupta, Email: agupt114@jhmi.edu.
Priya K. Singh, Email: psingh34@jhmi.edu
Amy L. Xu, Email: amyxu@jhmi.edu
Rachel S. Bronheim, Email: rbronhe1@jhmi.edu
Claire M. McDaniel, Email: cmcdan11@jhmi.edu
Amiethab A. Aiyer, Email: aaiyer2@jhmi.edu
References
- 1.Childs SG. The pathogenesis and biomechanics of turf toe. Orthop Nurs. 2006;25(4):276. doi: 10.1097/00006416-200607000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Frimenko RE, Lievers B, Coughlin MJ, Anderson RB, Crandall JR, Kent RW. Etiology and biomechanics of first metatarsophalangeal joint sprains (turf toe) in athletes. Crit Rev Biomed Eng. 2012;40(1). 10.1615/CritRevBiomedEng.v40.i1.30. [DOI] [PubMed]
- 3.Lievers WB, Goggins KA, Adamic P. Epidemiology of foot injuries using National Collegiate Athletic Association data from the 2009–2010 through 2014–2015 seasons. J Athl Train. 2020;55(2):181–187. doi: 10.4085/1062-6050-560-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chiou D, Stupay KL, Waryasz G. Turf toe review. Foot Ankle Spec. 2020;13(2):161–168. doi: 10.1177/1938640019857794. [DOI] [PubMed] [Google Scholar]
- 5.Aran F, Ponnarasu S, Scott AT. Turf Toe. StatPearls Publishing; 2022. Accessed February 9, 2023. https://www.ncbi.nlm.nih.gov/books/NBK507810/. [PubMed]
- 6.Rodeo SA, O’Brien S, Warren RF, Barnes R, Wickiewicz TL, Dillingham MF. Turf-toe: an analysis of metatarsophalangeal joint sprains in professional football players. Am J Sports Med. 1990;18(3):280–285. doi: 10.1177/036354659001800311. [DOI] [PubMed] [Google Scholar]
- 7.Clanton TO, Ford JJ. Turf toe injury. Clin Sports Med. 1994;13(4):731–741. doi: 10.1016/S0278-5919(20)30282-9. [DOI] [PubMed] [Google Scholar]
- 8.McCormick JJ, Anderson RB. Turf toe: anatomy, diagnosis, and treatment. Sports Health. 2010;2(6):487–494. doi: 10.1177/1941738110386681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson RB, Hunt KJ, McCormick JJ. Management of common sports-related injuries about the foot and ankle. J Am Acad Orthop Surg. 2010;18(9):546–556. doi: 10.5435/00124635-201009000-00006. [DOI] [PubMed] [Google Scholar]
- 10.McCormick JJ, Anderson RB. The great toe: failed turf toe, chronic turf toe, and complicated sesamoid injuries. Foot Ankle Clin. 2009;14(2):135–150. doi: 10.1016/j.fcl.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Chan JJ, Geller JS, Chen KK, et al. Epidemiology of severe foot injuries in US collegiate athletes. Orthop J Sports Med. 2021;9(4):23259671211001132. doi: 10.1177/23259671211001131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaplan LD, Jost PW, Honkamp N, Norwig J, West R, Bradley JP. Incidence and variance of foot and ankle injuries in elite college football players. Am J Orthop Belle Mead NJ. 2011;40(1):40–44. [PubMed] [Google Scholar]
- 13.Brophy RH, Gamradt SC, Ellis SJ, et al. Effect of turf toe on foot contact pressures in professional American football players. Foot Ankle Int. 2009;30(5):405–409. doi: 10.3113/FAI-2009-0405. [DOI] [PubMed] [Google Scholar]
- 14.Bowers KD, Martin RB. Turf-toe: a shoe-surface related football injury. Med Sci Sports. 1976;8(2):81–83. [PubMed] [Google Scholar]
- 15.George E, Harris AHS, Dragoo JL, Hunt KJ. Incidence and risk factors for turf toe injuries in intercollegiate football: data from the National Collegiate Athletic Association Injury Surveillance System. Foot Ankle Int. 2014;35(2):108–115. doi: 10.1177/1071100713514038. [DOI] [PubMed] [Google Scholar]
- 16.Soligard T, Bahr R, Andersen TE. Injury risk on artificial turf and grass in youth tournament football. Scand J Med Sci Sports. 2012;22(3):356–361. doi: 10.1111/j.1600-0838.2010.01174.x. [DOI] [PubMed] [Google Scholar]
- 17.Bjørneboe J, Bahr R, Andersen TE. Risk of injury on third-generation artificial turf in Norwegian professional football. Br J Sports Med. 2010;44(11):794–798. doi: 10.1136/bjsm.2010.073783. [DOI] [PubMed] [Google Scholar]
- 18.Taylor SA, Fabricant PD, Khair MM, Haleem AM, Drakos MC. A review of synthetic playing surfaces, the shoe-surface interface, and lower extremity injuries in athletes. Phys Sportsmed. 2012;40(4):66–72. doi: 10.3810/psm.2012.11.1989. [DOI] [PubMed] [Google Scholar]
- 19.Powell JW, Dompier TP. Analysis of injury rates and treatment patterns for time-loss and non-time-loss injuries among collegiate student-athletes. J Athl Train. 2004;39(1):56–70. [PMC free article] [PubMed] [Google Scholar]
- 20.Coker TP, Arnold JA, Weber DL. Traumatic lesions of the metatarsophalangeal joint of the great toe in athletes. Am J Sports Med. 1978;6(6):326–334. doi: 10.1177/036354657800600604. [DOI] [PubMed] [Google Scholar]
- 21.Davis WA, Yagnik GP. In-season management of acute and subacute sports foot injuries. Foot Ankle Clin. 2021;26(1):187–203. doi: 10.1016/j.fcl.2020.12.001. [DOI] [PubMed] [Google Scholar]
- 22.Hunt KJ, McCormick JJ, Anderson RB. Management of forefoot injuries in the athlete. Oper Tech Sports Med. 2010;18(1):34–45. doi: 10.1053/j.otsm.2009.12.001. [DOI] [Google Scholar]
- 23.Coughlin M, Baumfeld D, Nery C. Second MTP joint instability: grading of the deformity and description of surgical repair of capsular insufficiency. Phys Sportsmed. 2011;39:132–141. doi: 10.3810/psm.2011.09.1929. [DOI] [PubMed] [Google Scholar]
- 24.Linklater JM. Imaging of sports injuries in the foot. AJR Am J Roentgenol. 2012;199(3):500–508. doi: 10.2214/AJR.12.8547. [DOI] [PubMed] [Google Scholar]
- 25.Prieskorn D, Graves SC, Smith RA. Morphometric analysis of the plantar plate apparatus of the first metatarsophalangeal joint. Foot Ankle. 1993;14(4):204–207. doi: 10.1177/107110079301400405. [DOI] [PubMed] [Google Scholar]
- 26.Coughlin MJ, Kemp TJ, Hirose CB. Turf toe: soft tissue and osteocartilaginous injury to the first metatarsophalangeal joint. Phys Sportsmed. 2010;38(1):91–100. doi: 10.3810/psm.2010.04.1766. [DOI] [PubMed] [Google Scholar]
- 27.Faltus J, Mullenix K, Moorman CT, Beatty K, Easley ME. Case series of first metatarsophalangeal joint injuries in division 1 college athletes. Sports Health. 2014;6(6):519–526. doi: 10.1177/1941738114527546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chinn L, Hertel J. Rehabilitation of ankle and foot injuries in athletes. Clin Sports Med. 2010;29(1):157–167. doi: 10.1016/j.csm.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Doty JF, Coughlin MJ. Turf toe repair: a technical note. Foot Ankle Spec. 2013;6(6):452–456. doi: 10.1177/1938640013507107. [DOI] [PubMed] [Google Scholar]
- 30.Husebye EE, Stødle AH. Arthroscopic repair of chronic plantar plate tears of the first metatarsophalangeal joint: a new surgical technique with patient outcomes. Orthop J Sports Med. 2022;10(12):23259671221137560. doi: 10.1177/23259671221137558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Drakos MC, Fiore R, Murphy C, DiGiovanni CW. Plantar-plate disruptions: “the severe turf-toe injury”. Three cases in contact athletes. J Athl Train. 2015;50(5):553–560. doi: 10.4085/1062-6050-49.6.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aper RL, Saltzman CL, Brown TD. The effect of hallux sesamoid resection on the effective moment of the flexor hallucis brevis. Foot Ankle Int. 1994;15(9):462–470. doi: 10.1177/107110079401500902. [DOI] [PubMed] [Google Scholar]
- 33.Aper RL, Saltzman CL, Brown TD. The effect of hallux sesamoid excision on the flexor hallucis longus moment arm. Clin Orthop. 1996;325:209–217. doi: 10.1097/00003086-199604000-00025. [DOI] [PubMed] [Google Scholar]
- 34.Anderson RB, McBryde AM. Autogenous bone grafting of hallux sesamoid nonunions. Foot Ankle Int. 1997;18(5):293–296. doi: 10.1177/107110079701800509. [DOI] [PubMed] [Google Scholar]
- 35.Covell DJ, Lareau CR, Anderson RB. Operative treatment of traumatic Hallux Valgus in elite athletes. Foot Ankle Int. 2017;38(6):590–595. doi: 10.1177/1071100717697961. [DOI] [PubMed] [Google Scholar]
- 36.McCormick JJ, Anderson RB. Rehabilitation following turf toe injury and plantar plate repair. Clin Sports Med. 2010;29(2):313–323. doi: 10.1016/j.csm.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 37.Marchetti DC, Chang A, Ferrari M, Clanton TO. Turf toe: 40 years later and still a problem. Oper Tech Sports Med. 2017;25(2):99–107. doi: 10.1053/j.otsm.2017.03.001. [DOI] [Google Scholar]
- 38.York PJ, Wydra FB, Hunt KJ. Injuries to the great toe. Curr Rev Musculoskelet Med. 2017;10(1):104–112. doi: 10.1007/s12178-017-9390-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hong CC, Pearce CJ, Ballal MS, Calder JDF. Management of sports injuries of the foot and ankle: an update. Bone Jt J. 2016;98-B(10):1299–1311. doi: 10.1302/0301-620X.98B10.37896. [DOI] [PubMed] [Google Scholar]
- 40.Hsu AR, Anderson RB. Foot and ankle injuries in American football. Am J Orthop Belle Mead NJ. 2016;45(6):358–367. [PubMed] [Google Scholar]
- 41.Lieber J. Turf Toe: The NFL’s Most Pesky Agony of Da Feet. Sports Illustrated Vault | SI.com. Accessed March 12, 2023. https://vault.si.com/vault/1988/12/12/turf-toe-the-nfls-most-pesky-agony-of-da-feet.
- 42.Underwood J. Just An Awful Toll. Sports illustrated cvault | SI.com. Accessed March 12, 2023. https://vault.si.com/vault/1985/08/12/just-an-awful-toll.
- 43.Vopat ML, Hassan M, Poppe T, et al. Return to sport after turf toe injuries: a systematic review and meta-analysis. Orthop J Sports Med. 2019;7(10):2325967119875133. doi: 10.1177/2325967119875133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Anderson RB. Turf toe injuries of the hallux metatarsophalangeal joint. Tech Foot Ankle Surg. 2002;1(2):102. doi: 10.1097/00132587-200212000-00004. [DOI] [Google Scholar]
- 45.Clanton TO, Butler JE, Eggert A. Injuries to the metatarsophalangeal joints in athletes. Foot Ankle. 1986;7(3):162–176. doi: 10.1177/107110078600700306. [DOI] [PubMed] [Google Scholar]
- 46.Lindsey BB, Bakshi NK, Walton DM, Holmes JR, Talusan PG. Return to play following high-grade turf toe injuries in National Football League athletes. Foot Ankle Orthop. 2020;5(4). 10.1177/2473011420S00055.
- 47.Hainsworth L, McKinley J. 15 The management of turf toe — a systematic review. Br J Sports Med. 2017;51(Suppl 2):A7–A8. doi: 10.1136/bjsports-2017-098966.19. [DOI] [Google Scholar]
- 48.Nery C, Fonseca LF, Gonçalves JP, et al. First MTP joint instability — expanding the concept of “turf-toe” injuries. Foot Ankle Surg Off J Eur Soc Foot Ankle Surg. 2020;26(1):47–53. doi: 10.1016/j.fas.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 49.Madi NS, Parekh TJ, Parekh SG. Outcome of turf toe injuries in NFL players. J Foot Ankle Surg Off Publ Am Coll Foot Ankle Surg. 2023;62(1):115–119. doi: 10.1053/j.jfas.2022.05.008. [DOI] [PubMed] [Google Scholar]
- 50.Tran A, Kappa J, Smith E, et al. The effect of turf toe injuries on player performance in the National Football League. Iowa Orthop J. 2019;39(2):35–39. [PMC free article] [PubMed] [Google Scholar]
- 51.Smith K, Waldrop N. Operative outcomes of grade 3 turf toe injuries in competitive football players. Foot Ankle Int. 2018;39(9):1076–1081. doi: 10.1177/1071100718775967. [DOI] [PubMed] [Google Scholar]