Abstract
Background
The incidence of correctional surgery for adult spinal deformity (ASD) has increased significantly over the past 2 decades. Pelvic incidence, an angular measurement, is the gold standard pelvic parameter and is used to classify spinal shapes into Roussouly types. Current literature states that restoration of the spine to its original Roussouly classification optimizes outcomes. We propose a new pelvic parameter, pelvic index, as a length measurement to complement pelvic incidence in more accurately characterizing Roussouly types.
Methods
This study is a retrospective evaluation of sagittal spinal radiographs of 208 patients who were assessed by a single fellowship trained orthopedic spine surgeon between January and December 2020. Measurements included pelvic incidence, sacroacetabular distance, and L5 vertebral height. Pelvic index was calculated as the ratio of sacroacetabular distance to L5 height. Each spine was also classified into one of the Roussouly types: 1, 2, 3 anteverted pelvis (AP), 3, or 4. The 2 pelvic parameters were compared between groups to assess their ability to differentiate between Roussouly types.
Results
Of the 208 patients included, 103 (49.5%) were female and 105 (50.5%) were male. The mean pelvic incidence was 54.9 ± 12.3° and the mean pelvic index was 3.99 ± 0.38. The difference in mean pelvic index was statistically significant between types 1 and 2 (0.15; p=.046) and between types 1 and 3 AP (0.19; p=.029). It was not statistically significant between types 3 and 4 (0.05; p=.251). However, in terms of pelvic incidence, the mean difference was statistically significant only between types 3 and 4 (10.4; p<.001).
Conclusions
Pelvic index is the ratio of the sacroacetabular distance to the height of the L5 vertebra. In conjunction with pelvic incidence, pelvic index can help to distinguish between Roussouly types 1 and 2 and between types 1 and 3 AP, the low-pelvic incidence types.
Keywords: Pelvic incidence, Adult spinal deformity, Roussouly, Pelvic parameter, Pelvic index, Scoliosis, Reconstructive surgery
Background
Adult spinal deformity (ASD) arises from various etiologies that lead to abnormal curvature of the spine in the coronal or sagittal plane. The progression of this abnormal curvature may be accelerated due to age-related factors such as pre-existing deformity or osteoporosis [1]. With increasing life expectancy and a growing elderly population, spinal deformity is estimated to affect approximately 27.5 million elderly individuals [2]. The incidence of spinal correction surgery for ASD has also increased significantly in the past 2 decades [3]. Additionally, there has been substantial growth in surgical complexity, with increased numbers of long-segment fusions and 3-column osteotomies [2].
The standard imaging protocol for evaluation of ASD comprises standing full-length 36 posteroanterior and lateral radiographs [4]. The Cobb angle is determined from posteroanterior radiographs to assess spinal curvature in the coronal plane [5]. Pelvic parameters are determined from lateral radiographs to assess for sagittal spinal alignment [4]. Current literature states that sagittal spinal alignment is an important parameter to consider when planning corrective surgery for ASD. Restoring the spinopelvic balance back to its original alignment, based on Roussouly classification, optimizes functional outcomes and decrease rates of complication [6], [7], [8], [9].
The Roussouly sagittal classification is divided into 5 types. Types 1 and 2 have a sacral slope <35°, differing by the apex of the lumbar lordosis (L5 for Type 1 and L4 for Type 2). Type 3 anteverted pelvis (AP) has a low pelvic incidence despite having a sacral slope >35°. Type 3 has a sacral slope between 35° and 45°, with an apex of lumbar lordosis at the center of the L4 vertebral body, and is considered to be a well-balanced spine. The type 4 Roussouly spines have a sacral slope greater than 45° with an apex of lumbar lordosis at the L3 vertebral body or higher, and is associated with a higher pelvic incidence [10].
The pelvis is key in sagittal balance for maintaining stability and alignment, as the pelvis allows for transfer of weight from the trunk to the lower extremities [6]. Pelvic incidence is the gold standard pelvic parameter for characterizing the pelvis in relation to sagittal spinal curves. Other established pelvic parameters include pelvic tilt and sacral slope. The current classification of spinal shape into Roussouly type is based on pelvic incidence [8,9]. However, the pelvic incidence only defines an angular relationship; pelvic tilt and sacral slope also only serve as angular measurements. Therefore, the addition of a standardized length measurement may contribute to enhanced characterization of the spinopelvic relationship. The use of a length measurement would add a second dimension in characterizing the 2-dimensional space seen on lateral radiographs.
The purpose of this study was to propose a new pelvic parameter, the pelvic index—based on sacroacetabular distance and L5 vertebral height—to assess sagittal spinal alignment based on Roussouly classification. We hypothesize that the pelvic index, used in conjunction with pelvic incidence, will allow for better characterization of Roussouly types in evaluating spinal shape than pelvic index alone.
Methods
This retrospective study included patients from 1 fellowship trained orthopedic spine surgeon between January 2020 and December 2020. Deidentified sagittal spinal radiographs were accessed through our institution's Picture Archive and Communications System (PACS). This study was deemed exempt from approval by our University's Institutional Review Board, as no identifiable patient information was accessed.
Patients with history of prior spinal correction surgery, which may be evidenced by visible hardware, were excluded from the study. In such patients, sometimes it is not possible to determine the original sagittal profile. The patients included in the study did not have obvious deformity concerning such measurements taken. For patients with multiple sagittal spinal radiographs performed in the study period, only the first radiograph was included in the study. All measurements were performed by 2 observers, using the measurement tools within PACS. Measurements included sacroacetabular distance, L5 vertebral height, and pelvic incidence.
A total of 217 patients were initially included in this study, of which 9 were excluded for presence of visible hardware. Of the remaining 208 patients, 103 (49.5%) were female and 105 (50.5%) were male.
The sacroacetabular distance was measured as the distance between the midpoint of the sacral endplate to the midpoint between the center of the femoral heads. The midpoints of the sacral endplate and between femoral heads were established by bisecting a line drawn over the sacral endplate and across the centers of the femoral heads, respectively. L5 vertebral height was measured vertically through the center of the L5 vertebral body. The pelvic index was calculated as the ratio of sacroacetabular distance to L5 height. Pelvic incidence was measured as the angle between a line perpendicular to the midpoint of the sacral endplate to a line connecting this point to a midpoint between the femoral heads (Fig. 1) [11]. Sagittal spinal alignment was determined by classifying each radiograph as Roussouly type 1 to 4 [12]. All measurements were performed by 2 observers.
Fig. 1.
Examples of pelvic parameter measurements for each Roussouly type shown in blue: A (L5 height), B (sacroacetabular distance), C (pelvic incidence). The yellow line indicates the inflection point between kyphosis and lordosis.
The mean pelvic incidence and pelvic index values for each Roussouly type were compared using independent sample t tests. Logistic regression was used to assess the likelihood of pelvic index predicting Roussouly type. All statistical analyses were conducted using SPSS Software version 26.0 (IBM Corp.). Odds ratios (OR) were reported with 95% confidence intervals (CI). The level of statistical significance was set at p<.05.
Results
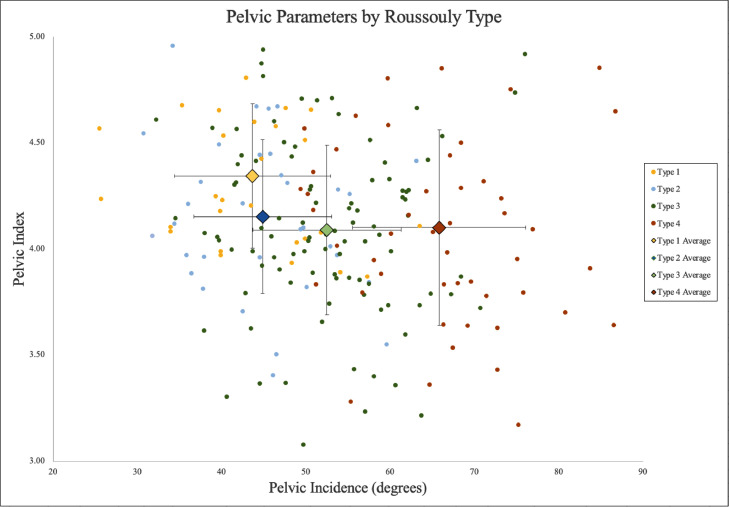
Across the entire cohort, the mean pelvic incidence was 54.9 ± 12.3° and the mean pelvic index was 3.99 ± 0.38. The sagittal spinal alignment of each patient was grouped based on Roussouly classification: 29 (13.9%) were classified as type 1, 33 (15.9%) were classified as type 2, 19 (9.1%) were classified as type 3 AP, 78 (37.5%) were classified as type 3, and 49 (23.6%) were classified as type 4 (Table 1). Pelvic index values were plotted as a function of pelvic incidence on a scatterplot (Fig. 2). The mean pelvic parameter values for each Roussouly type were also plotted on the scatterplot.
Table 1.
Mean values of pelvic incidence and pelvic index grouped by Roussouly type.
| Roussouly type | Number | Percent | Mean pelvic incidence (°) | Mean pelvic index |
|---|---|---|---|---|
| Total | 208 | – | 54.9 ± 12.3 | 3.99 ± 0.38 |
| 1 | 29 | 13.9% | 44.8 ± 9.4 | 4.22 ± 0.33 |
| 2 | 33 | 15.9% | 46.5 ± 9.0 | 4.07 ± 0.33 |
| 3 AP | 19 | 9.1% | 47.5 ± 6.8 | 4.03 ± 0.33 |
| 3 | 78 | 37.5% | 56.6 ± 9.4 | 3.93 ± 0.38 |
| 4 | 49 | 23.6% | 67.0 ± 10.0 | 3.88 ± 0.40 |
Fig. 2.
Scatterplot of pelvic parameters grouped by Roussouly type: type 1 (yellow), type 2 (blue), type 3 (green), type 4 (red). The average pelvic parameter values of each Roussouly type are plotted as well, with error bars indicating standard deviation.
The mean values for pelvic incidence and pelvic index by Roussouly classification are summarized in Table 1. These means were compared between Roussouly types based on low-incidence (types 1 vs. 2, 1 vs. 3 AP, 2 vs. 3 AP) and high-incidence (types 3 and 4) (Table 2). The difference in mean pelvic index was statistically significant between types 1 and 2 (0.15; p=.046) and between types 1 and 3 AP (0.19; p=.029). There was no statistically significant difference in mean pelvic index between types 2 and 3 AP (0.04; p=.321) and between types 3 and 4 (0.05; p=.251). However, in terms of pelvic incidence, the mean difference was statistically significant between types 3 and 4 (10.4; p<.001).
Table 2.
Comparison of mean pelvic parameter values based on low and high-incidence.
| Pelvic incidence (°) |
Pelvic index |
|||
|---|---|---|---|---|
| Roussouly type | Mean difference | p-value | Mean difference | p-value |
| 1 vs. 2 | 2.3 | .245 | 0.15 | .046 |
| 1 vs. 3 AP | 2.7 | .141 | 0.19 | .029 |
| 2 vs. 3 AP | 1.1 | .322 | 0.04 | .321 |
| 3 vs. 4 | 10.4 | <.001 | 0.05 | .251 |
Bold p-values indicate statistical significance with p<.05.
Inter-rater reliability for pelvic index was measured using Pearson's correlation coefficient and Cronbach's alpha (Table 3). Pelvic index had a Pearson's coefficient of 0.812 and Cronbach's alpha of 0.892, indicating good reliability.
Table 3.
Inter-rater reliability coefficients for pelvic index measurements.
| Measurement | Pearson | Cronbach's alpha |
|---|---|---|
| L5 height | 0.581 | 0.734 |
| Sacroacetabular distance | 0.881 | 0.936 |
| Pelvic index | 0.812 | 0.892 |
Discussion
This study introduces the pelvic index as a novel pelvic parameter for characterizing the spinopelvic relationship. The pelvic index was measured for a cohort of 208 patients to determine if pelvic index can provide better Roussouly characterization of spinal shape, when used in conjunction with pelvic incidence. Our findings demonstrate that pelvic index can potentially assist in distinguishing between Roussouly types with low pelvic incidence, between types 1 and 2 and between 1 and 3 AP. Further, our study demonstrates that pelvic incidence alone can effectively differentiate between the high pelvic incidence groups, types 3 and 4.
Adult spinal deformity represents a spectrum of spinal diseases that range from progressive conditions of adolescence, multilevel degenerative disc disease with subsequent global deformity, post-traumatic deformity, among several others. These diseases are increasingly important to characterize and understand as the average age of the global population increases, with increased proportion of the population being composed of older-age individuals. In patients aged 65 and older, the prevalence of spinal deformity has been estimated to be 32% to 68% [13]. Using the United States alone as an example, it is estimated by 2060 that roughly a quarter of Americans will be older than 65. With respect to the high prevalence and impending global demographic shifts, there is a strong need to better understand and characterize spinal deformity.
Parameters that are routinely used to evaluate the sagittal spinopelvic relationship include pelvic incidence, pelvic tilt, and sacral slope. While these metrics are helpful in evaluating the spine in the sagittal plane, they can be misleading when used in isolation. For example, in the asymptomatic population, pelvic incidence itself has variability without any clear mechanistic explanation. Importantly, the pelvic incidence is considered to be fixed after the cessation of growth, which further highlights the limited use of these metrics in isolation [10].
The Roussouly sagittal classification is divided into types 1 to 4. With the understanding that Roussouly Type 3 is considered a “normal” spine, some surgeons have proposed using it as a sagittal alignment goal when surgically treating adult spinal deformities. A retrospective study showed that there were similar rates of revision surgery required when Roussouly spine shape achieved and not achieved, but also showed after controlling for confounders that there was a 5-fold increase in mechanical failure of constructs when Roussouly spine shape was not achieved [14]. While this may highlight the importance of achieving Roussouly alignment in corrective surgery, the similar rate of revision surgeries elucidates factors that are not explained by restoration of Roussouly type alone [14].
We introduce the pelvic index as a second measurement to define the spinopelvic relationship in 2-dimensional space. The pelvic index is the ratio of the sacroacetabular distance to the L5 vertebral height. The pelvic index, a ratio utilizing length measurements, will allow for better characterization of 2-dimensional space when combined with an angular measurement. The length measurement is necessary, as the degree of pelvic offset can vary for the same angle of pelvic incidence. In effect, we are using the polar coordinate system to characterize the spinopelvic relationship, with the midpoint of the sacral endplate as our reference. Polar coordinates have previously been used for effectively describing geometry and deformation of the heart on magnetic resonance imaging [15].
In our study, we reported an overall mean pelvic incidence of 54.9°. This is consistent with previous studies that have reported mean pelvic incidences of 51.4°, 51.9°, and 53.1° [16], [17], [18]. We reported a mean overall pelvic index of 3.99. Although we propose using the L5 vertebra to standardize the pelvic index, there is insufficient evidence to show that this is necessarily the best method. Regardless, we used L5 because it is the vertebral level that is closest in proximity to our reference point on the sacral endplate. As Roussouly types can be classified based on low-grade and high-grade pelvic incidence, our study focused on differentiating between Roussouly types within these groups [19].
Among the low incidence group (types 1 vs. 2, 1 vs. 3 AP), we found no statistically significant difference between the means of pelvic incidence. However, we found a statistically significant difference between the means of pelvic index. Among the high incidence group (types 3 and 4), we found a statistically significant difference between pelvic incidence, but not between pelvic index. These findings suggest that pelvic incidence alone may not be enough to distinguish between Roussouly types 1 and 2. The means of pelvic index for type 1, 2, and 3 AP were 4.22, 4.07, and 4.03, respectively. This suggests that patients with low pelvic incidence and high pelvic index are more like to be Roussouly type 1, and patients with low pelvic incidence and low pelvic index are more likely to be type 2. Between Roussouly types 3 and 4, there is enough variation in pelvic incidence to distinguish the 2 types.
There are a few limitations of this study due to the nature of the investigation. Previous studies that were done to establish pelvic incidence and Roussouly types included asymptomatic adult volunteers [10]. Our study was also limited to an older, symptomatic patient population with varying degrees of preexisting spinal deformities. As this study was conducted during the height of the COVID-19 pandemic, public health guidelines and restrictions limited the number of patients that could be seen in the office. This may have led to more severe pathology to present to the office more so than milder pathology, for concerns of health. Further studies are needed to evaluate the pelvic index in asymptomatic adults of various ages, with a greater sample size to better evaluate the efficacy of the pelvic index in distinguishing between Roussouly types. Further investigation would also benefit from utilizing an age and gender matched cohort to explore differences between symptomatic and asymptomatic patients in vertebral body height. As this study was conducted solely on PACS, sub analysis for other variables including ethnicity or BMI could not be conducted. We also acknowledge that there are potential variabilities in L5 height, especially the concavity of the lower endplate [20]. L5 vertebral body was chosen as a result of its proximity to the other pelvic parameters; along with a matched cohort, as mentioned prior, comparing multiple lumbar vertebral body heights for uniformity should be explored. Inter-rater reliability of these measurements will also have to be analyzed. We primarily had 2 observes record the measurements, but having more observers would help determine inter-rater reliability.
Conclusion
To our knowledge, this is the first study to propose a new pelvic parameter based on length. This parameter is to be used in conjunction with pelvic incidence and more accurately determine a person's specific Roussouly type, which would assist in optimizing patient outcomes.
Our newly proposed pelvic parameter, pelvic index, is the ratio of the sacroacetabular distance to the height of the L5 vertebra. Pelvic index is a length measurement that can be used with pelvic incidence, an angular measurement, to better characterize the 2-dimensional plane provided in a sagittal spinal radiograph. In conjunction with pelvic incidence, pelvic index can help to distinguish between Roussouly types 1 and 2 and between types 1 and 3 AP, which are all low-pelvic incidence types. We believe, in addition to pelvic index, this measure will aid in better characterization of patients into the Roussouly types during preoperative planning of corrective surgery for adult spinal deformity, which would then aid in yielding optimized outcomes postoperatively.
Funding
No funding was disclosed by the author(s).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
None.
Footnotes
IRB APPROVAL: Stony Brook University ORC, IRB ID: IRB2020-00208.
FDA device/drug status: Not applicable.
Author disclosures: JUA: Nothing to disclose. KL: Nothing to disclose. RB: Nothing to disclose. AG: Nothing to disclose. DEK: Nothing to disclose. NAP: Nothing to disclose.
References
- 1.Good CR, Auerbach JD, O'Leary PT, Schuler TC. Adult spine deformity. Curr Rev Musculoskelet Med. 2011;4(4):159–167. doi: 10.1007/s12178-011-9101-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Safaee MM, Ames CP, Smith JS. Epidemiology and socioeconomic trends in adult spinal deformity care. Neurosurgery. 2019;87(1):25–32. doi: 10.1093/neuros/nyz454. [DOI] [PubMed] [Google Scholar]
- 3.Zygourakis CC, Liu CY, Keefe M, et al. Analysis of national rates, cost, and sources of cost variation in adult spinal deformity. Neurosurgery. 2018;82(3):378–387. doi: 10.1093/neuros/nyx218. [DOI] [PubMed] [Google Scholar]
- 4.Dagdia L, Kokabu T, Ito M. Classification of adult spinal deformity: review of current concepts and future directions. Spine Surg Relat Res. 2018;3(1):17–26. doi: 10.22603/ssrr.2017-0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Langensiepen S, Semler O, Sobottke R, et al. Measuring procedures to determine the Cobb angle in idiopathic scoliosis: a systematic review. Eur Spine J. 2013;22(11):2360–2371. doi: 10.1007/s00586-013-2693-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheung J. The importance of sagittal balance in adult scoliosis surgery. Ann Transl Med. 2020;8 doi: 10.21037/atm.2019.10.19. 35-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pizones J, Moreno-Manzanaro L, Sánchez Pérez-Grueso FJ, et al. Restoring the ideal Roussouly sagittal profile in adult scoliosis surgery decreases the risk of mechanical complications. Eur Spine J. 2020;29(1):54–62. doi: 10.1007/s00586-019-06176-x. [DOI] [PubMed] [Google Scholar]
- 8.Sebaaly A, Gehrchen M, Silvestre C, et al. Mechanical complications in adult spinal deformity and the effect of restoring the spinal shapes according to the Roussouly classification: a multicentric study. Eur Spine J. 2020;29(4):904–913. doi: 10.1007/s00586-019-06253-1. [DOI] [PubMed] [Google Scholar]
- 9.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34(17):1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 10.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976). 2005;30(3):346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 11.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laouissat F, Sebaaly A, Gehrchen M, Roussouly P. Classification of normal sagittal spine alignment: refounding the Roussouly classification. Eur Spine J. 2018;27(8):2002–2011. doi: 10.1007/s00586-017-5111-x. [DOI] [PubMed] [Google Scholar]
- 13.Diebo BG, Shah NV, Boachie-Adjei O, et al. Adult spinal deformity. Lancet. 2019;394(10193):160–172. doi: 10.1016/s0140-6736(19)31125-0. [DOI] [PubMed] [Google Scholar]
- 14.Bari TJ, Hansen LV, Gehrchen M. Surgical correction of adult spinal deformity in accordance to the Roussouly classification: effect on postoperative mechanical complications. Spine Deform. 2020;8(5):1027–1037. doi: 10.1007/s43390-020-00112-6. [DOI] [PubMed] [Google Scholar]
- 15.Nasiraei-Moghaddam A, Finn JP. Tagging of cardiac magnetic resonance images in the polar coordinate system: physical principles and practical implementation. Magn Reson Med. 2014;71(5):1750–1759. doi: 10.1002/mrm.24839. [DOI] [PubMed] [Google Scholar]
- 16.Boulay C, Tardieu C, Hecquet J, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15(4):415–422. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Le Huec JC, Aunoble S, Philippe L, Nicolas P. Pelvic parameters: origin and significance. Eur Spine J. 2011;20(suppl 5):564–571. doi: 10.1007/s00586-011-1940-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fallatah SM, Altijani AM, Alharbi AA, Bourgleh SM, Bassi MM. How do pelvic parameters correlate with postoperative outcomes when the parameters are not measured preoperatively in patients undergoing instrumented lumbar fusion? Cureus. 2021;13(8):e16885. doi: 10.7759/cureus.16885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J. 2011;20(suppl 5):609–618. doi: 10.1007/s00586-011-1928-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lakshmanan P, Purushothaman B, Dvorak V, Schratt W, Thambiraj S, Boszczyk M. Sagittal endplate morphology of the lower lumbar spine. Eur Spine J. 2012;21(suppl 2):S160–S164. doi: 10.1007/s00586-012-2168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]