Abstract
Key Clinical Message
Accidental displacement of mandibular third molars or their roots into neighboring anatomical spaces, notably the submandibular region, during extraction, is a rare but significant complication. Comprehensive preoperative assessment, meticulous surgical techniques, and precise radiographic imaging play pivotal roles in successful management. Adhering to established protocols is imperative to mitigate potential complications and ensure optimal outcomes.
Abstract
In this report, we emphasize the critical importance of comprehensive preoperative preparation to tailor surgical approaches and techniques in accordance with recognized surgical principles. Oral and maxillofacial surgery often involves the extraction of impacted lower third molars, a common surgical procedure. However, this procedure can present potential complications such as hemorrhage, tissue damage, infection, alveolar osteitis, paresthesia, and mandible dislocation. Unintentional displacement of a mandibular third molar or its root fragments into adjacent anatomical areas, such as the maxillary sinus or submandibular space, is a rare intra‐operative exodontia complication that is seldom documented. A 44‐year‐old male patient presented with complaints of pain, discomfort, and limited mouth opening. He had previously attempted to have a tooth extracted, but the procedure resulted in a misplaced tooth. A painful, indurated swelling was observed at the patient's left mandibular angle. Radiographic analyses revealed a radiopaque lesion resembling the third molar tooth root. Utilizing orthopantomography and CT images, the misplaced root in the left submandibular region was accurately located. The tooth was successfully extracted following the elevation of a lingual flap. The patient was prescribed antibiotics and painkillers for 7 days, and he reported an uneventful recovery with no complications on the eighth postoperative day. Accidental displacement of lower third molars or root fragments into neighboring anatomical areas is a rare but potentially concerning complication. Common sites of displacement include the submandibular, sublingual, and pterygomandibular spaces. Risk factors for displacement encompass improper use of surgical instruments and variations in patient anatomical characteristics. The ease of extraction can be influenced by various factors, including the degree of impaction, root structure, and dental inclination. Recommended screening examinations include panoramic radiography, intraoral periapical (PA) radiography, and occlusal radiography. Precise diagnosis and localization necessitate radiographic assessments such as CT scans and panoramic radiography. Postoperative care involves administering analgesics, antibiotics, suturing, wound irrigation, and managing potential complications like swelling, discomfort, infection, and nerve damage. Accidental displacement of lower third molars or their roots into the submandibular region is an infrequent yet potential complication. Thorough case assessment and adherence to established protocols for appropriate access, judicious bone removal, and avoiding excessive force are imperative for clinicians in the field of oral and maxillofacial surgery.
Keywords: case report, mandibular, submandibular space, third molar displacement, third molar displacement
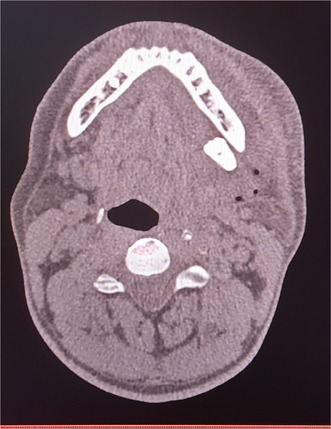
Axial Computed Tomography scan showing high‐density area showing displaced molar in the left submandibular region.
1. INTRODUCTION
Impacted extraction of the lower third molar is a widely practiced surgical procedure within the specialized field of oral and maxillofacial surgery. This intricate intervention carries inherent intra‐ and post‐operative complications including but not limited to hemorrhage, damage to adjacent soft tissues, infection, alveolar osteitis, paresthesia of the lingual or inferior alveolar nerve, and dislocation of the mandible. Among these well‐described complications, another well‐known, yet scarcely‐reported intra‐operative complication of exodontia is the accidental displacement of a mandibular third molar or its root fragments into adjacent anatomic spaces such as the maxillary sinus or submandibular space. 1 , 2 , 3 The displacement usually occurs as a result of excessive force, inadequate clinical and radiographic examination/assessment, inappropriate surgical technique, and/or a patient's unique anatomical characteristics. 2 , 4 In this report, we present the case of an accidentally displaced mandibular third molar in the submandibular space and emphasize the need for adequate preoperative planning for an individualized approach and the blending of surgical techniques in accordance with established surgical principles.
2. CASE PRESENTATION
A male patient, aged 44, presented to our hospital with complaints of pain, discomfort while swallowing, and difficulty in mouth opening. His medical history revealed that a general dentist had made an unsuccessful attempt to extract an impacted third molar from the mandible under local anesthesia a week prior. During the procedure, the tooth was displaced. Upon clinical examination, the patient exhibited a painful and hardened swelling in the left mandibular angle. The patient's mouth could only open up to 11 mm, and there were no evident signs of lip or tongue abnormal sensations. Other than that, the patient's medical records did not contribute any relevant information.
To conduct a thorough radiographic assessment, computed tomography (CT), panoramic radiography, and intraoral periapical radiography were employed (see Figures 1 and 2). Panoramic radiographs revealed a radiopaque lesion resembling the appearance of the root of the third molar. Further evaluation through CT scans identified a dense area indicating the placement of the root fragment in the left submandibular region. The misplaced root's precise location in the submandibular area was determined through meticulous analysis of the orthopantomography (OPG) and CT scans. After discussing the surgical process, potential risks, and obtaining the patient's consent, it was agreed to proceed with the surgery under local anesthesia.
FIGURE 1.

Preoperative orthopantomogram showing displaced molar in the left submandibular region.
FIGURE 2.

Axial Computed Tomography scan showing high‐density area.
During the surgical procedure (see Figure 3), a combination of 4% carticaine and adrenaline was administered through injections to provide anesthesia and block the inferior alveolar, lingual, and long buccal nerves. Under the effect of the local anesthetic, the patient's mouth opening angle was manually extended, and through palpation, the displaced fragment of the molar was identified to be deeply located in the submandibular area. To access the fragment, a lingual flap was raised medially up to the first premolar and connected distally with a buccal flap that was raised from the mandibular first molar to the external oblique ridge. With appropriate lighting and the aid of an extra‐oral finger, the root fragment became visible, and the lingual flap was carefully reflected up to the submandibular area. A curette was utilized to extract the molar by pulling it outward (see Figure 4). Following the procedure, the wound was treated with normal saline, and the flaps were closed using 3–0 Vicryl sutures (see Figure 5). The patient was prescribed a course of antibiotics and analgesics for 7 days. On the eighth day after the surgery, the patient reported no issues of concern and indicated a satisfactory recovery. The sutures were subsequently removed.
FIGURE 3.

Intra‐operative view of the surgical site.
FIGURE 4.

Retrieved molar fragment after surgery.
FIGURE 5.

Sutured surgical site using Vicryl 3–0 sutures.
3. DISCUSSION
Accidental displacement of lower third molars or their root fragments into adjacent anatomical spaces is a rare, yet possible complication. 5 The most frequent locations for an impacted mandibular third molar fragment to dislodge are the sublingual, submandibular, and pterygomandibular spaces. 6 Many times, efforts to remove the fragment without sufficient vision and the necessary surgical abilities might lead to the displacement of the tooth or root fragment deep into the nearby spaces. 5 Factors such as improper use of the surgical instruments, and patient anatomical features can further increase the risk of displacement, such as lingually located teeth or deeply impacted molars. 3 , 7 A lingual plate fracture or perforation during extraction, in addition to excessive pressure exerted with the elevators, can cause the root to extend deeper into anatomical areas. 5 The presenting signs and symptoms of a misplaced root in a patient depend on its size, position, and the presence of infection. 6 They may range from asymptomatic instances to accounts of discomfort, edema, and mandibular trismus. 4 Patients have been seen with a history of swelling in the right angulus area along with facial asymmetry, and restriction in mouth opening. This leads to issues in speaking and swallowing, due to a restricted range of motion of the mandible in all planes. 5 In roughly 1% of third molar procedures, complications consist of discomfort, dry socket, edema, paresthesia of the lingual or inferior alveolar nerve, hemorrhage, and infection. 6 Hence, before initiating removal, an extensive treatment strategy should be created to reduce the chance of problems. If a dental component is neglected for a long time, there may be an allergic reaction to the foreign body in addition to a risk of infection in the neck spaces. 3 Few surgeons choose to put off surgery for a few weeks so that fibrosis can take place and firmly anchor the tooth. 8 However, postponing removal for more than 24 h may cause an inflammatory reaction that can cause excruciating pain, swelling, trismus, infection, and additional root relocation or root fracture into deep regions, resulting in a reaction similar to that of a foreign body. 6 This infection may have a direct impact on the occupants of the space, particularly those in the posterior compartment, such as interaction with cranial nerves 9–12, erosion of the carotid artery and its branches, and thrombosis of the internal jugular vein. 9
The clinical complication of third molar displacement should be duly taken into consideration during the process of mandibular third molar extraction. 10 Retrieving a lost tooth fragment in the submandibular region can be challenging, and it is considered a rare complication of extraction that is difficult to anticipate. 8 Several factors should be taken into account which may influence the level of difficulty such surgical procedures might present. The level of impaction refers to the depth of the tooth within the jawbone and its proximity to adjacent structures. The more deeply impacted the tooth, the more challenging the extraction becomes, as it may require extensive bone removal and potentially involve nearby nerves and blood vessels. 11 The root format plays a role in the ease of extraction as well. Dilacerated or curved roots can make the extraction more difficult, requiring careful manipulation and potential sectioning of the tooth. 12 A tooth with a severe forward tilt can cause a horizontal impaction, which is harder to remove than a mesioangular impaction and more challenging to extract due to limited access and potential obstruction by adjacent teeth or bone. 13 So, higher levels of impaction, complex root morphology, increased dental inclination, etc. may make extractions more challenging and significantly affect the surgical approach.
Panoramic radiography, also known as orthopantomography (PAN), is the most frequently recommended screening examination 14 as it captures a wide‐angle image of the entire oral and maxillofacial region while Intraoral periapical (PA) radiography focuses on capturing detailed views of individual teeth and their surrounding structures. Occlusal radiography focuses on the bite and occlusal surfaces, aiding in evaluating tooth development and identifying abnormalities. While panoramic radiographs have shown higher overall accuracy, occlusal radiographs have demonstrated greater precision. 15 However, these 2D modalities can miss certain 3D anatomical alterations and potential overlap of anatomical structures may obscure the region of interest. That is where cone beam computed tomography (CBCT) offers a more detailed assessment of teeth and the surrounding alveolar anatomy 16 allowing for precise evaluations of dental and skeletal structures. An accurate diagnosis of the displaced tooth fragment's location is crucial for successful retrieval. In this case, radiographic evaluation played a vital role. Panoramic radiography and CT scans provided detailed images showing the radiopaque lesion. The combination of orthopantomography (OPG) and CT scans allowed for precise localization of the displaced fragment. While radiographs and tomography images are valuable for seeking the exact localization of the displaced fragment, a bimanual examination is helpful in locating tooth fragments. 17 By carefully palpating the affected area, the dental surgeon can ascertain the depth and position of the fragment within the submandibular region. This tactile feedback enhances the surgeon's ability to plan the surgical approach and minimize the risk of further displacement during extraction.
In cases of displaced root fragments following unsuccessful third molar extraction, surgical as well as conservative treatments are available depending on the clinical presentation and patient factors. When the root fragments are small and located deep within tissues without any signs of infection, surgical removal may not be necessary if patients do not experience any symptoms. But regular clinical and radiographic follow‐ups should be performed to monitor the stability and potential complications associated with the retained fragment. 4 It is commonly recommended to postpone the surgery for a few weeks to allow for fibrosis and the establishment of a stable tooth position. However, it is important to consider that delaying the intervention may heighten the risk of infection and potentially result in complications like foreign body reactions or further migration of the dislodged tooth. 18 The primary surgical approach for removing tooth fragments is typically intraoral. However, in certain cases, an extraoral or combined intraoral/extraoral technique may be preferred. This is particularly true when the displaced fragment is located in challenging areas such as the lateral pharyngeal or deep cervical space. In rare instances, a sagittal split approach to the mandibular angle has even been described for the removal of a displaced third molar. 10 In this case, a lingual flap was raised medially up to the first premolar, and a buccal flap was raised from the mandibular first molar to the external oblique ridge. The displaced molar fragment was visualized, extracted using a curette, and the wound was irrigated and closed with sutures.
The postoperative care consisted of irrigating the wound with normal saline, suturing the incision, and administering a 1‐week course of antibiotics and analgesics. It is important to note that tooth extraction in cases like these can lead to various sequelae and complications, including pain, swelling, infection, and nerve injury. Among these, swelling and pain are the most commonly reported complications. Additionally, certain cases may experience paraesthesia (abnormal sensations) and hemorrhage. In a previous study, it was found that several factors such as the presence of a large and/or bulbous root, ankylosis (fusion of tooth to bone), and deep impaction significantly contributed to the occurrence of complications. Figure 6 summarizes the management of mandibular third molar displacement.
FIGURE 6.
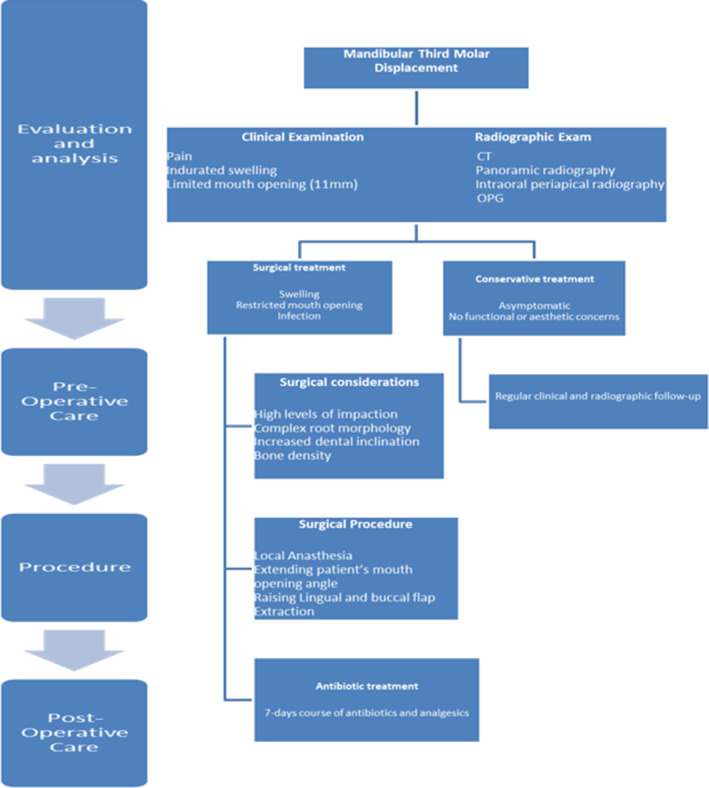
Summary of the management of mandibular third molar displacement. 19
4. CONCLUSION
An uncommon but possible complication is the accidental displacement of lower third molars or their root pieces into the submandibular region. Since this rare incidence occurs due to the negligence of the dentist, it is essential that every third molar extraction case should be thoroughly assessed beforehand and dentists doing these extractions should adhere to the usual guidelines for good access, sensible bone removal, and avoid using too much power. Dentists with insufficient training who attempt to remove teeth can lead to complications like displacement of teeth into different spaces. Such complications should be managed by experienced oral and maxillofacial surgeons with adequate technical skills and knowledge.
AUTHOR CONTRIBUTIONS
Abdullah Nadeem: Conceptualization; data curation; formal analysis; methodology; project administration; writing – original draft; writing – review and editing. Laiba Imran Vohra: Conceptualization; data curation; formal analysis; project administration; writing – original draft; writing – review and editing. Areeba Ahsan: Conceptualization; data curation; formal analysis; methodology. Hasan Mushahid: Supervision; validation; writing – original draft; writing – review and editing. Rabeea Tariq: Resources; software; visualization; writing – original draft; writing – review and editing. Mahima Rizwan: Writing – original draft; writing – review and editing. Maryam Gul: Writing – original draft; writing – review and editing. Nahid Raufi: Funding acquisition.
CONFLICT OF INTEREST STATEMENT
There are no conflicts of interest.
ETHICAL APPROVAL
Not applicable.
PATIENT CONSENT STATEMENT
Not applicable.
CLINICAL TRIAL REGISTRATION
Not applicable.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENTS
None.
Nadeem A, Vohra LI, Ahsan A, et al. A rare case of mandibular third molar displaced into submandibular space: A complication of mandibular third molar extraction. Clin Case Rep. 2023;11:e8101. doi: 10.1002/ccr3.8101
DATA AVAILABILITY STATEMENT
Not applicable.
REFERENCES
- 1. Bouloux GF, Steed MB, Perciaccante VJ. Complications of third molar surgery. Oral Maxillofac Surg Clin North Am. 2007;19(1):117‐128. doi: 10.1016/j.coms.2006.11.013 [DOI] [PubMed] [Google Scholar]
- 2. Goldberg MH, Nemarich AN, Marco WP. Complications after mandibular third molar surgery: a statistical analysis of 500 consecutive procedures in private practice. J Am Dent Assoc. 1985;111(2):277‐279. doi: 10.14219/jada.archive.1985.0098 [DOI] [PubMed] [Google Scholar]
- 3. Oliveira MMM, da Franca AR, de Souza DD, da Silva BA, Carvalho DDC. Third molar displacement into submandibular space. Case Rep Dent. 2019;2019:1‐3. doi: 10.1155/2019/6137868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aznar‐Arasa LFRGEC. Iatrogenic displacement of lower third molar roots into the sublingual space: report of 6 cases. J Oral Maxillofac Surg. 2012;70:e107‐e115. [DOI] [PubMed] [Google Scholar]
- 5. Kose I, Koparal M, Günes N, et al. Displaced lower third molar tooth into the submandibular space: two case reports. J Nat Sci Biol Med. 2014;5(2):482‐484. doi: 10.4103/0976-9668.136274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jolly SS, Rattan V, Rai SK. Intraoral management of displaced root into submandibular space under local anaesthesia –a case report and review of literature. Saudi Dent J. 2014;26(4):181‐184. doi: 10.1016/J.SDENTJ.2014.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nusrath MA, Banks RJ. Unrecognised displacement of mandibular molar root into the submandibular space. Br Dent J. 2010;209(6):279‐280. doi: 10.1038/sj.bdj.2010.816 [DOI] [PubMed] [Google Scholar]
- 8. Kamburoglu K, Kursun S, Oztas B. Submandibular displacement of a mandibular third molar root during extraction: a case report. Cases J. 2010;3(1):8. doi: 10.1186/1757-1626-3-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kasatwar A, Bhola N, Borle R, Rajanikanth K. Displacement of lower third molar into the lateral pharyngeal space in a case of mandibular angle fracture: an unusual complication. Contemp Clin Dent. 2016;7(2):229‐231. doi: 10.4103/0976-237X.183046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alexoudi VA, Tatsis D, Zamani K, Zelkas D, Paraskevopoulos K, Vaxtsevanos K. Iatrogenic displacement of impacted mandibular third molars or their roots into adjacent soft tissues and spaces: a report of three cases. Natl J Maxillofac Surg. 2020;11(2):275‐279. doi: 10.4103/njms.NJMS_95_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhang Y, Chen X, Zhou Z, et al. Effects of impacted lower third molar extraction on periodontal tissue of the adjacent second molar. Ther Clin Risk Manag. 2021;17:235‐247. doi: 10.2147/TCRM.S298147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Benton PN, Chang P. Oral surgery, Extraction Of Roots. Vol 9. StatPearls ; 2023. https://www.ncbi.nlm.nih.gov/books/NBK589696/ [PubMed] [Google Scholar]
- 13. Farish SE, Bouloux GF. General technique of third molar removal. Oral Maxillofac Surg Clin North Am. 2007;19(1):23‐43. doi: 10.1016/j.coms.2006.11.012 [DOI] [PubMed] [Google Scholar]
- 14. Izzetti R, Nisi M, Aringhieri G, Crocetti L, Graziani F, Nardi C. Basic knowledge and new advances in panoramic radiography imaging techniques: a narrative review on what dentists and radiologists should know. Appl Sci. 2021;11(17):7858. doi: 10.3390/app11177858 [DOI] [Google Scholar]
- 15. Kim JH, Aoki EM, Cortes ARG, Abdala‐Júnior R, Asaumi J, Arita ES. Comparison of the diagnostic performance of panoramic and occlusal radiographs in detecting submandibular sialoliths. Imaging Sci Dent. 2016;46(2):87‐92. doi: 10.5624/isd.2016.46.2.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lo Giudice R, Nicita F, Puleio F, et al. Accuracy of periapical radiography and CBCT in endodontic evaluation. Int J Dent. 2018;2018:1‐7. doi: 10.1155/2018/2514243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chattopadhyay A, Hossain M, Chatterjee A, Hussain M, Barman S, Raha A. Intraoral management of latrogenic tooth displacement: a report of two cases and a brief review of literature. Contemp Clin Dent. 2021;12(2):187‐190. doi: 10.4103/ccd.ccd_384_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Solanki R, Khangwal M, Kumar D, Goel M. Retrieval of mandibular third molar tooth accidentally displaced in submandibular space: series of two cases. Indian J Dent. 2016;7(2):105‐108. doi: 10.4103/0975-962X.184653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chubb DWR, Kang B, Tong N. Accidental displacement of mandibular third molars into the submandibular space–two case reports, a suggested surgical approach and management algorithm. J Stomatol Oral Maxillofac Surg. 2021;122(2):203‐207. doi: 10.1016/j.jormas.2020.08.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


