Summary
Background
The dual impacts of a warming climate and population ageing lead to an increasing kidney disease prevalence, highlighting the importance of quantifying the burden of kidney disease (BoKD) attributable to high temperature, yet studies on this subject are limited. The study aims to quantify the BoKD attributable to high temperatures in Australia across all states and territories, and project future BoKD under climatic, population and adaptation scenarios.
Methods
Data on disability-adjusted-life-years (DALYs) due to kidney disease, including years of life lost (YLL), and years lived with disability (YLD), were collected during 2003–2018 (baseline) across all states and territories in Australia. The temperature-response association was estimated using a meta-regression model. Future temperature projections were calculated using eight downscaled climate models to estimate changes in attributable BoKD centred around 2030s and 2050s, under two greenhouse gas emissions scenarios (RCP4.5 and RCP8.5), while considering changes in population size and age structure, and human adaptation to climate change.
Findings
Over the baseline (2003–2018), high-temperature contributed to 2.7% (Standard Deviation: 0.4%) of the observed BoKD in Australia. The future population attributable fraction and the attributable BoKD, projected using RCP4.5 and RCP8.5, showed a gradually increasing trend when assuming no human adaptation. Future projections were most strongly influenced by the population change, with the high temperature-related BoKD increasing by 18.4–67.4% compared to the baseline under constant population and by 100.2–291.2% when accounting for changes in population size and age structure. However, when human adaptation was adopted (from no to partial to full), the high temperature-related BoKD became smaller.
Interpretation
It is expected that increasing high temperature exposure will substantially contribute to higher BoKD across Australia, underscoring the urgent need for public health interventions to mitigate the negative health impacts of a warming climate on BoKD.
Funding
Australian Research Council Discovery Program.
Keywords: High temperature, Climate change, Kidney disease, Attributable risk, Burden of disease
Research in context.
Evidence before this study
Previous epidemiologic studies have documented the association between high temperature and kidney disease. However, evidence for the burden of kidney disease (BoKD) attributable to high temperature remains limited. We searched PubMed, Scopus, and Google Scholar for studies published in English until April 2023, that explore the high temperature-related burden of kidney disease, and projections under future climate change. We used a combination of search terms, including “temperature”, “climate change”, “weather” AND “kidney disease”, “renal disease” AND “mortality”, “morbidity”, “attributable burden”, “attributable risk”, “projection”, “prediction”. Among the limited studies quantifying the high temperature-attributable burden of disease, most have only examined mortality to quantify the years of life lost (YLL) associated with high temperature. However, the inclusion of morbidity indicator i.e., years lived with disability (YLD), is particularly important for estimating the BoKD. The BoKD attributable to high temperature has not been examined at the regional level in a country, including both fatal (YLL) and non-fatal (YLD) indicators.
Added value of this study
This study is the first globally to provide a national overview of BoKD attributable to high temperature, including both YLL and YLD in the context of future climate change and population shifts in size and age distribution. Our projection incorporates future temperatures from eight climate models under two representative concentration pathways (RCP4.5 and RCP8.5), while accounting for changes in population and scenarios of human adaptations until the middle of the 21st century. We modelled the variation in the exposure-response relationship between high temperature and kidney disease in each of the 2310 statistical level 2 areas covering the whole of Australia and calculated the theoretical minimum risk exposure distribution (TMRED). We then computed the high temperature-related population attributable fraction and the attributable BoKD, as measured in disability-adjusted life years (DALYs). We found that during the baseline period between 2003 and 2018, high temperature contributed to 2.7% (SD: 0.4%) of the observed BoKD in Australia, resulting in an average annual loss of 1446.8 years of healthy life or 6.4 DALYs per million population. Our projections suggest that future temperature will correspond to steady increases in BoKD in Australia across all scenarios examined, except for full (100%) adaptation with no population change. When assuming no human adaptation, we observed a gradually increasing trend in the high temperature-related BoKD using RCP4.5 and RCP8.5 climate scenarios. This rise was primarily influenced by the expected changes in population. For instance, under a higher-emission RCP8.5 scenario, the high temperature-attributable BoKD is projected to increase approximately four times (5660.4 DALYs) compared to the baseline level (1446.8 DALYs) by 2050. Of this, population increase accounted for the greater proportion (3238.4 DALYs, 77%), with the remaining 23% attributed to an increase in future high temperature exposure. Moreover, we found that the jurisdiction with a warmer climate i.e., the Northern Territory, had the highest rate of high temperature-attributable BoKD in both the baseline and future periods (2030s and 2050s).
Implications of all the available evidence
This study provides a comprehensive picture of the BoKD attributable to high temperature in all jurisdictions across Australia, which will help extend our understanding of the health impacts of high temperature and aid in policy-making to reduce the future BoKD caused by the warming climate. The disparate geographical patterns of attributable BoKD found in our study suggest that geographically specific adaptation actions need to be strengthened to maximize the effectiveness of reducing future BoKD in the context of warming climates.
Introduction
Kidney disease is a growing global public health concern, responsible for 41.8 million disability-adjusted life years (DALY) in 2019, and 2.2% of global burden.1 Prevalence increased by 16% from 2010 to 2019, unlike other non-communicable diseases with declining age-standardized death and DALYs rates.1 With the aging population, there will inevitably be a greater number of people with, or at risk of, kidney disease.2 Characterized by progressive damage to the kidneys, reduced filtration function, and removal of protein/albumin from blood into urine, kidney disease increases the risk of other disease such as cardiovascular diseases, hypertension, and COVID-19, thereby impacting worldwide mortality and morbidity.3 In Australia, the burden of kidney disease (BoKD) accounted for 1.5% of Australia’s total disease burden in 2022.4
High ambient temperature is a known risk factor for kidney disease and can worsen its occurrence.5 Recurrent dehydration due to sweating is reported as a cause of chronic kidney disease (CKD) in people exposed to high temperature, and the decreased extracellular fluid and blood flow to the kidneys may lead to renal failure.6 CKD contributed to 11% of Australia’s deaths in 2020.7 Acute renal failure can also occur due to high temperature-associated dehydration.6
Australia is vulnerable to climate change, with an increase in frequency, magnitude, and duration of heatwaves and extreme high temperature.8 With an aging population and rising temperatures, heat-induced kidney diseases are expected to increase, posing a significant threat to population health and a cause for concern from health experts.9 Despite established evidence linking high temperature with kidney disease-related mortality and morbidity,5,6 no previous research has estimated the high temperature-attributable fatal and non-fatal BoKD,10,11 nor projected future BoKD in the context of climatic and population changes, and adaptation.
Accordingly, this study estimates the observed and projected BoKD attributable to high temperature in Australia, using the national burden of disease database,4 as measured in DALYs, incorporating years of life lost (YLL) and years lived with disability (YLD) in different regions. In addition, we assessed the future high temperature-attributable BoKD, considering a range of climatic, population, and adaptation scenarios. Results from this study will help to guide region-specific climate adaptation strategies and healthcare resource allocation for kidney disease.
Methods
Study overview
We conducted this analysis across the whole of Australia, comprising six states (New South Wales, Queensland, Victoria, Western Australia, South Australia, Tasmania) and two territories (Australian Capital Territory, Northern Territory). We used Australian Statistical Areas Level 2 (SA2, n = 2310) as spatial areas, which were defined based on the 2016 census and cover the entire country. SA2s represent communities of 3000–25,000 people.12
The BoKD attributed to high temperature was calculated for 2003–2018 (baseline, hereafter referred to simply as “2010s”) and compared to future periods centred around 2030s (2016–2045) and 2050s (2036–2065) in each Australian jurisdiction. In our projections, we used a 30-year period based on the latest climate projections by the Commonwealth Scientific and Industrial Research Organization (CSIRO).13 This allows for a better estimation of long-term trends in temperature and attributable fractions, as recommended by the World Meteorological Organization.14,15 We projected these trends for every combination of (1) two scenarios of change in population size and age structure; (2) two climate change scenarios; and (3) three levels of adaptation to high temperature exposure (no, partial and full), as described below. More details on the analytical framework is provided in our recent publication.16
Data sources
We acquired the age-specific annual Australian BoKD (YLL and YLD) data from the Australian Institute of Health and Welfare (AIHW) for four reference years (2003, 2011, 2015, 2018),4 and estimated missing values between years using ordinary least-squares regression for linear interpolation based on the trend of BoKD.17
Mean temperature distributions for each SA2 during the baseline period was obtained as the average of maximum and minimum temperatures from daily high-resolution (0.05°) gridded temperature observations.18 We obtained gridded climate projections (approximately 5 km × 5 km) data using eight climate models, as detailed in the Couples Model Inter-comparison Project,13 under two greenhouse gas emissions scenarios (Representative Concentration Pathway, RCP4.5 and 8.5),19 and averaged the projections of future daily mean temperature in each SA2 area.
We obtained baseline and projected population data (population size and age structures) from the Australian Bureau of Statistics (ABS) for each jurisdiction.20,21 We chose ‘series B’ for the main analysis, which reflects current trends in migration, fertility and life expectancy. Sensitivity analysis was conducted using ‘Series A’ (increased migration, fertility and life expectancy) and ‘Series C’ (decreased migration, fertility and life expectancy) projections (Supplementary Table S1).22
Estimation of exposure-response curves and thresholds
Following our recent methodological framework publication,16 we first published a global systematic review to obtain the relative risks (RR) between high (mean) temperature and kidney disease.5 We calculated the RR associated with each 1 °C increment in mean temperature, and collected location-specific predictors (Köppen–Geiger climate classification,23 continent, latitude, longitude, GDP per capita, annual mean temperature, and annual mean relative humidity)5 that may explain the heterogeneity in the associations across locations.11,24 Next, we built a meta-regression model using the relevant RR and the aforementioned location-specific meta-predictors. The model regression and comparison results are summarized in Supplementary Table S2. Based on the fitted model and the predictors, we predicted the RR for each Australian SA2 per 1 °C increase in mean temperature.5,11
As per previous research,25 the most frequent temperature (MFT) and the minimum mortality temperature (MMT) are similar, and the MFT-MMT association remains constant after controlling for predictors including GDP per capita, annual mean temperature and latitude. Given this, the MFT was selected as a surrogate for the theoretical minimum risk exposure distribution (TMRED) in our analyses i.e., temperature at which the risk of kidney disease would be the lowest, for each Australian SA2. Accordingly, we calculated the annual MFT during the baseline (2003–2018) within the 54th–92nd percentile temperature range in each SA2. While this range may not cover all exposures, it has been reported to cover 95% of the minimum mortality percentile in an international study covering 30 countries in six continents across the world.25 Given the heat-dominant J-shaped relationship between temperature and health in most parts of Australia,26 we assumed a log-linear monotonic increase of RR for kidney disease per 1 °C increase in average temperature beyond the threshold in each SA2.5 We conservatively assumed that the exposure-response relationship estimated on the current temperature range would not increase in the future for the projection.19 In addition, we conducted sensitively analysis using nonlinear functional forms (quadratic and cubic) to examine the exposure-response relationship.
Additionally, we explored three assumptions of human adaptation to increasing high temperature: no adaptation, full adaptation, and partial adaptation.27,28 The no adaptation scenario used the baseline TMREDs (the annual MFT calculated using the baseline climate data), while the full adaptation scenario (100%) used TMREDs calculated from future projected climate data, assuming the threshold for minimum risk exposure rises as people adapt to higher temperatures.27,28 The partial adaptation scenario assumed 50% adaptation, using the mean of the no and full adaptation TMREDs. Supplementary Fig. S1 shows the differences in TMREDs assumed in each climatic and adaptation scenario over time, compared to the baseline TMREDs per SA2. Sensitivity analysis was conducted to assess the assumptions made in the modelling and calculation.
Population attributable fraction and attributable burden
We calculated the annual high temperature-related BoKD for each SA2 by determining the population exposure to daily mean temperatures exceeding the TMRED value.16 Specifically, by using location-specific exposure-response relationships along with observed and projected mean temperatures, we computed the population fraction of BoKD attributable to high temperature in baseline, and future periods (2030s and 2050s), respectively.16
Using population data from each SA2 for each time period, we calculated the location-specific DALYs (YLLs and YLDs) according to their proportion of the state/territory and national population. Particularly, we considered the expected changes in the population size, age structure and the associated BoKD, and scenario where the population remains constant. Next, we multiplied the annual location-specific population attributable fraction (PAF) by its corresponding YLDs and YLLs to obtain the annual high temperature-attributable BoKD in each SA2 area in 2010s, 2030s and 2050s. Finally, we estimated the attributable BoKD for the future periods compared to baseline, and evaluated the fraction of additional BoKD under different combinations of climatic, population and adaptation scenarios.29
Uncertainty and sensitivity analysis
We considered various factors that may contribute to uncertainties in the estimation of PAFs and the high temperature attributable BoKD during each step of our analysis. These factors included (1) the use of different models to estimate the effect sizes, (2) alternative TMREDs, (3) eight climate change models under two RCPs, and (4) effects of aging populations and human adaptation under different population projections.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Summary statistics
Supplementary Table S3 shows the estimates of annual average DALYs across jurisdictions in the baseline period (2003–2018). The national annual average years of healthy life lost for kidney diseases was 52,654 (age-standardized DALY rates of 219 DALYs per 100,000 population), the fatal burden (YLLs) representing 74.6% of the total BoKD, and the non-fatal burden 25.4%. The Northern Territory (NT) had the highest total burden rate due to kidney disease (age-standardized DALY rates of 810.4 per 100,000 population) which was approximately four times as high as the national average during the baseline period.
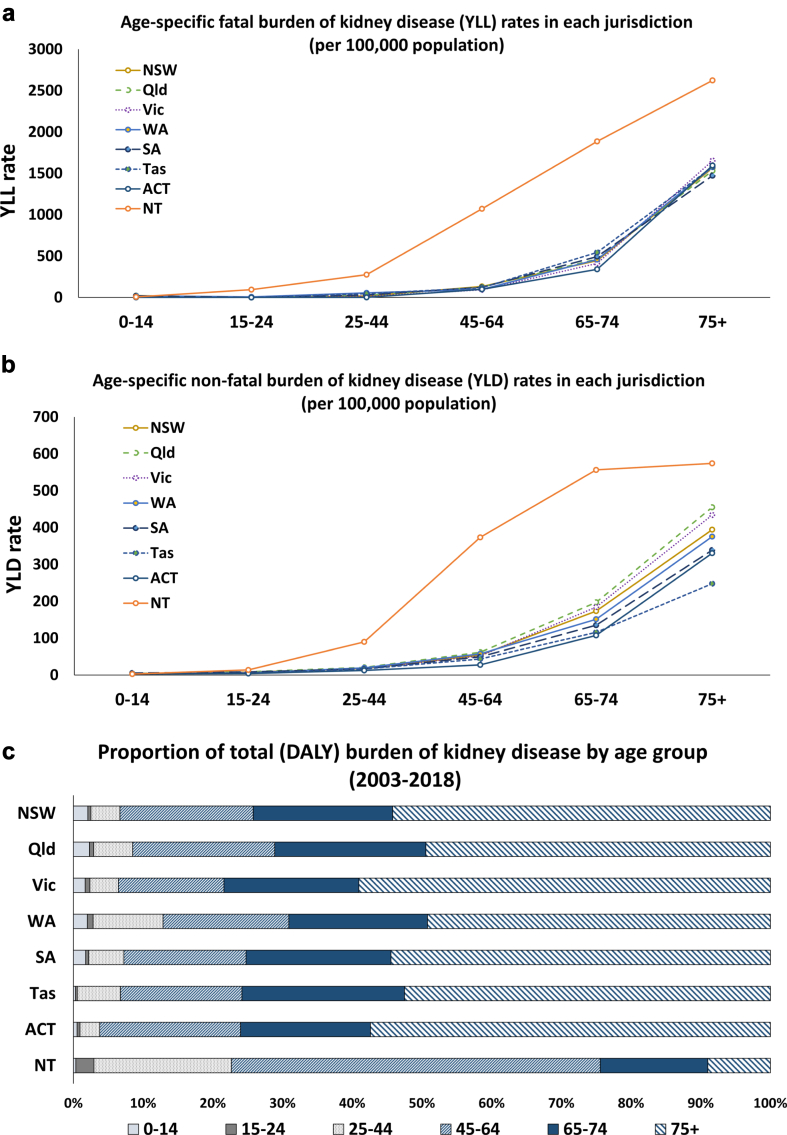
Fig. 1 shows the rates (per 100,000 population) and the proportion (%) of fatal and non-fatal BoKD by age group for each state and territory (see Supplementary Fig. S2 for the DALY rates). A similar trend is observed across all jurisdictions, where the rates of fatal and non-fatal BoKD exhibit an upward trajectory alongside increasing age (Fig. 1a and b). Notably, compared to other jurisdiction, rates were higher in the NT from age >15 years, with the gap increasing from the age of 25 onwards. Furthermore, the NT had a higher proportion of total BoKD occurring in the younger age group than in the older population (Fig. 1c), with 76% among individuals aged 0–64 years and 24% in those aged 65 years and over, unlike other jurisdictions (Supplementary Fig. S6).
Fig. 1.
Comparison of fatal and non-fatal burden of kidney disease by age groups and jurisdictions. a) fatal rates between age groups, b) non-fatal rates between age groups, and c) relative proportion of the total burden (%).
Estimated high temperature attributable burden of kidney disease during baseline
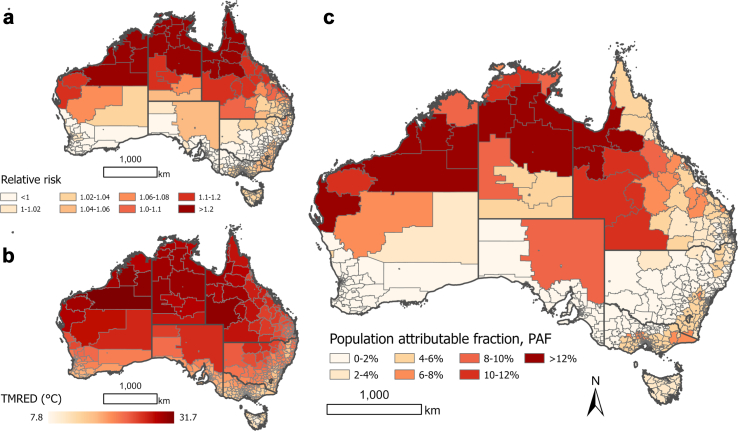
The geographic distribution of RR per unit (1 °C) increase in high temperature for kidney disease at the SA2 level is shown in Fig. 2, along with the corresponding TMREDs defining high temperature exposure and PAFs (which demonstrate the proportion of the BoKD per SA2 area that can be attributed to exposure to high temperature, compared to an alternative ideal exposure scenario). It can be seen that the risk of kidney disease increases with high temperatures in most regions, with the estimated location-specific TMREDs ranging from 7.8 to 31.7 °C. Higher RRs, TMREDs and PAFs are observed in warmer regions closer to the equator.
Fig. 2.
Spatial distribution of a) the relative risk per 1 °C increment in mean temperature, b) the theoretical minimum risk exposure distributions, TMREDs (°C), and c) population attributable fraction (PAF) of kidney disease due to high temperatures exposure, by the statistical areas level 2 (SA2) within each state and territory in Australia, averaged across the baseline period (2003–2018).
Nationally, high temperature was responsible for 2.7% of the BoKD, with the attributable DALYs totalling 1,447, comprising 1070 YLLs and 377 YLDs from 2003 to 2018 (Table 1). While NT (9.0%) and Australian Capital Territory (ACT) (5.3%) had the highest attributable BoKD, the NT had by far the highest rate (56.1 DALYs per 100,000 population), which was over nine times the national average (6.4 DALYs per 100,000 population). Supplementary Fig. S3 displays the geographical variation in the rate of high temperature-attributable BoKD in Australia.
Table 1.
Annual mean temperature (range) and burden of kidney disease (BoKD) attributable to high temperatures, by state and territory in Australia, 2003–2018.
| State/Territory | Tmean (range) | Attributable YLLs (SD) | Attributable YLDs (SD) | Attributable DALYs (SD) | % of attributable DALYs (SD) | Attributable DALYs rate, per 100,000 personsa (SD) |
|---|---|---|---|---|---|---|
| NSW | 17.6 (6.5–33.2) | 106.3 (29.7) | 35.5 (11.7) | 141.9 (40.9) | 0.8 (0.2) | 1.9 (0.5) |
| Qld | 21.5 (10.0–33.5) | 308.9 (116.7) | 119.6 (42.7) | 428.6 (158.4) | 4.2 (0.9) | 9.6 (2.9) |
| Vic | 15.0 (4.4–34.5) | 422.0 (116.3) | 151.5 (33.5) | 573.4 (148.8) | 4.4 (0.7) | 10.2 (2.0) |
| WA | 18.9 (7.8–34.3) | 68.5 (23.6) | 21.7 (4.8) | 90.2 (28.2) | 1.8 (0.2) | 3.8 (0.9) |
| SA | 16.7 (6.0–36.8) | 13.4 (2.4) | 3.9 (0.8) | 17.3 (3.1) | 0.4 (0.05) | 1.1 (0.2) |
| Tas | 12.1 (2.3–28.9) | 29.9 (8.3) | 6.6 (2.0) | 36.6 (10.3) | 2.9 (0.5) | 7.2 (1.9) |
| ACT | 13.8 (0.6–30.4) | 22.7 (5.8) | 6.5 (2.0) | 29.2 (7.6) | 5.3 (1.0) | 7.9 (1.7) |
| NT | 26.8 (15.7–33.6) | 98.4 (40.5) | 31.4 (13.4) | 129.8 (83.8) | 9.0 (2.2) | 56.1 (20.3) |
| Australia | 17.9 (6.7–33.6) | 1070.1 (313.7) | 376.7 (96.4) | 1446.8 (408.3) | 2.7 (0.4) | 6.4 (1.4) |
Tmean, mean temperature. NSW, New South Wales. Qld, Queensland. Vic, Victoria. WA, Western Australia. SA, South Australia. Tas, Tasmania. ACT, Australian Capital Territory. NT, Northern Territory.
Averaged total across periods, and standard deviation (SD).
Estimated projection of future high temperature attributable burden of kidney disease
Mean temperatures are projected to increase across Australia by 2050s relative to 2010s, with greater increases under the higher greenhouse gas emissions RCP8.5 scenario, compared to the RCP4.5 scenario. In 2050s, this difference is more pronounced than in 2030s (see Supplementary data, Supplementary Table S3). The geographical representation of the mean temperature anomalies over each future period is provided in Supplementary Fig. S3. Supplementary Table S3 shows the estimated population size for each state and territory under the series B projection, with Supplementary Fig. S4 illustrating the trends for all three population projection series. Additionally, in accordance with an ageing population, the proportion of the population aged 65 and over in each jurisdiction is projected to increase from 7.5–19.7% in 2018 to 11.2–27.0% by 2065 under series B (Supplementary Fig. S5).
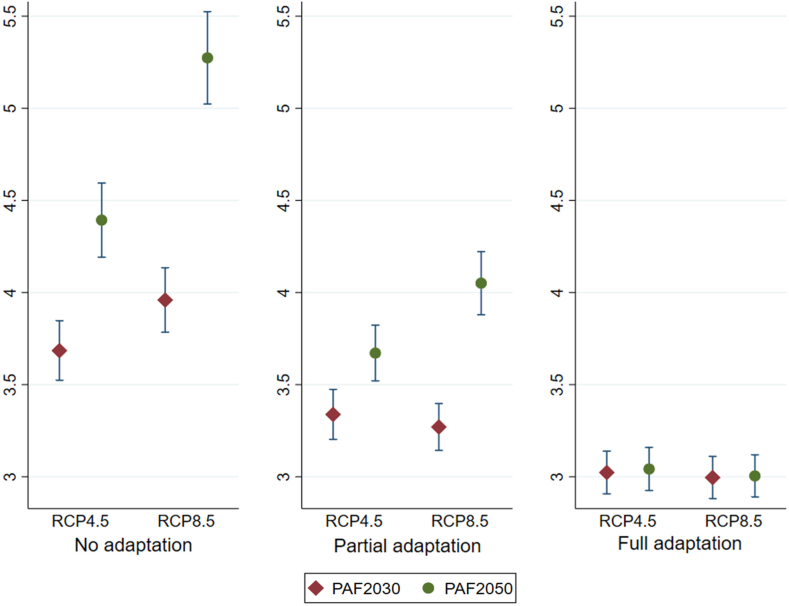
Fig. 3 shows the mean across SA2s of the projected population attributable fractions (PAFs) of high temperature attributable BoKD during 2030s and 2050s for three adaptation scenarios under RCP4.5 and RCP8.5. As expected, we observed a gradually increasing trend of PAFs over time across climate scenarios, with higher PAFs for each centred period under RCP8.5 than the RCP4.5 scenario, when assuming no human adaptation. The annual average PAFs were reduced when human adaptation (from 0% to 100% adaptation) was considered, ranging from 1.4% lower under RCP4.5 and 2.3% lower under RCP8.5 by 2050s. The differences in estimated PAFs per each State and Territory are displayed in Supplementary Fig. S7.
Fig. 3.
Comparisons of population attributable fractions (PAF) of high temperature attributable burden of kidney disease (BoKD) for future period centred on 2030 and 2050 (mean and 95% confidence interval), under two representative concentration pathways (RCP4.5 and RCP8.5), and scenarios of human adaptation to climate change (none, partial, full).
Table 2 provides a summary of the estimated BoKD attributed to high temperatures, along with the projected increase in the proportion of high temperature-related BoKD during the 2030s and 2050s, compared to the baseline. These estimates are provided for each state and territory under RCP4.5 and RCP8.5, and three adaptation scenarios. The proportion of the total BoKD attributable to high temperature and the share of this additional attributable BoKD are provided in Supplementary Tables S4 and S5, respectively.
Table 2.
Projected high temperature-attributable burden of kidney disease for future periods centred on 2030, and 2050 (annual average number of disability-adjusted life years (DALYs)), and the projected percentage change (%) compared to the baseline (2003–2018), under scenarios of constant population and medium population growth, adaptation to climate change (none, partial, full), and two representative concentration pathways (RCP4.5, RCP8.5). Estimates are the mean across eight climate models.
| RCPs | State/territory | Projected burden of kidney disease attributable to high temperature, DALYs (%)a |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Constant population |
Medium population growth (Series B projection) |
||||||||||||
| No adaptation |
Partial adaptation |
Full adaptation |
No adaptation |
Partial adaptation |
Full adaptation |
||||||||
| 2030 | 2050 | 2030 | 2050 | 2030 | 2050 | 2030 | 2050 | 2030 | 2050 | 2030 | 2050 | ||
| 4.5 | NSW | 165.7 (16.8%) | 192.5 (35.7%) | 155.6 (9.7%) | 168.2 (18.5%) | 147.2 (3.8%) | 146.1 (2.9%) | 257.2 (81.3%) | 397.4 (180.1%) | 242.0 (70.6%) | 347.8 (145.2%) | 229.1 (61.5%) | 302.2 (113.0%) |
| Qld | 552.2 (28.9%) | 682.3 (59.2%) | 474.2 (10.6%) | 537.9 (25.5%) | 404.8 (−5.5%) | 407.8 (−4.8%) | 978.0 (128.2%) | 1671.2 (290.0%) | 839.6 (95.9%) | 1319.3 (207.8%) | 717.7 (67.5%) | 1000.9 (133.6%) | |
| Vic | 584.2 (1.9%) | 651.8 (13.7%) | 584.9 (2.0%) | 621.7 (8.4%) | 588.1 (2.6%) | 590.7 (3.0%) | 1010.0 (76.1%) | 1610.0 (180.8%) | 1011.2 (76.3%) | 1537.1 (168.0%) | 1017.8 (77.5%) | 1460.4 (154.7%) | |
| WA | 102.9 (14.2%) | 114.9 (27.5%) | 93.6 (3.8%) | 99.0 (9.8%) | 87.7 (−2.7%) | 86.4 (−4.2%) | 178.0 (97.4%) | 283.9 (214.8%) | 161.4 (79.0%) | 244.3 (171.0%) | 151.5 (68.0%) | 213.0 (136.3%) | |
| SA | 17.9 (3.4%) | 19.3 (11.7%) | 17.5 (1.7%) | 18.2 (5.6%) | 17.2 (−0.4%) | 17.3 (−0.04%) | 25.4 (47.2%) | 33.0 (91.0%) | 25.0 (44.8%) | 31.2 (80.6%) | 24.5 (42.0%) | 29.5 (71.1%) | |
| Tas | 37.7 (3.1%) | 44.6 (22.0%) | 34.9 (−4.4%) | 38.3 (4.7%) | 33.0 (−9.8%) | 33.5 (−8.3%) | 57.6 (57.6%) | 78.2 (114.0%) | 53.4 (46.2%) | 67.2 (83.8%) | 50.5 (38.1%) | 58.9 (61.0%) | |
| ACT | 31.0 (6.0%) | 35.0 (19.9%) | 31.2 (7.0%) | 33.5 (14.7%) | 31.0 (6.1%) | 32.3 (10.7%) | 61.0 (108.6%) | 98.9 (238.7%) | 61.3 (110.1%) | 94.6 (224.0%) | 60.7 (108.0%) | 91.1 (212.0%) | |
| NT | 221.1 (70.4% | 292.7 (125.5%) | 174.9 (34.8%) | 200.4 (54.4%) | 127.6 (−1.7%) | 128.0 (−1.3%) | 329.0 (153.5%) | 586.4 (351.9%) | 259.8 (100.2%) | 399.1 (207.5%) | 188.5 (45.2%) | 253.8 (95.6%) | |
| National | 1712.6 (18.4%) | 2033.1 (40.5%) | 1566.9 (8.3%) | 1717.2 (18.7%) | 1436.6 (−0.7%) | 1422.0 (−0.3%) | 2896.1 (100.2%) | 4759.1 (228.9%) | 2653.7 (83.4%) | 4040.7 (179.3%) | 2440.2 (68.7%) | 3409.9 (135.7%) | |
| 8.5 | NSW | 175.5 (23.7%) | 230.3 (62.3%) | 155.9 (9.9%) | 184.7 (30.2%) | 146.6 (3.3%) | 145.5 (2.6%) | 272.4 (92.0%) | 475.2 (234.9%) | 242.4 (70.9%) | 381.6 (168.9%) | 228.2 (60.8%) | 301.3 (112.4%) |
| Qld | 618.9 (44.4%) | 852.5 (98.9%) | 466.7 (8.9%) | 612.5 (42.9%) | 402.6 (−6.1%) | 405.7 (−5.3%) | 1094.9 (155.5%) | 2085.4 (386.6%) | 826.6 (92.9%) | 1500.5 (250.1%) | 714.2 (66.6%) | 995.8 (132.3%) | |
| Vic | 605.0 (5.5%) | 729.7 (27.2%) | 597.4 (4.2%) | 653.3 (13.9%) | 585.8 (2.1%) | 580.6 (1.2%) | 1046.3 (82.5%) | 1801.6 (214.2%) | 1034.1 (80.3%) | 1615.1 (181.7%) | 1014.5 (76.9%) | 1435.7 (150.4%) | |
| WA | 104.5 (15.9%) | 135.4 (50.2%) | 90.6 (0.5%) | 108.4 (20.2%) | 86.6 (−4.0%) | 86.4 (−4.2%) | 180.5 (100.2%) | 333.2 (269.5%) | 156.3 (73.3%) | 267.1 (196.3%) | 149.2 (65.5%) | 213.3 (136.5%) | |
| SA | 18.4 (6.5%) | 21.3 (23.5%) | 17.6 (2.2%) | 19.1 (10.9%) | 17.2 (−0.2%) | 17.2 (−0.3%) | 26.2 (51.6%) | 36.5 (111.2%) | 25.2 (45.7%) | 32.7 (89.7%) | 24.6 (42.3%) | 29.5 (70.6%) | |
| Tas | 40.1 (9.6%) | 49.4 (35.0%) | 35.1 (−4.1%) | 40.5 (10.7%) | 32.8 (−10.1) | 33.7 (−7.9%) | 61.3 (67.7%) | 86.6 (137.0%) | 53.7 (46.9%) | 71.1 (94.4%) | 50.3 (37.7%) | 59.1 (61.7%) | |
| ACT | 32.3 (10.5%) | 41.0 (40.4%) | 31.5 (8.0%) | 36.0 (23.2%) | 30.8 (5.6%) | 30.9 (5.9%) | 63.6 (117.7%) | 115.9 (296.8%) | 61.9 (112.1%) | 101.5 (247.7%) | 60.5 (107.1%) | 87.6 (199.9%) | |
| NT | 241.9 (86.4%) | 362.4 (179.3%) | 149.5 (15.2%) | 231.2 (78.2%) | 122.3 (−5.8%) | 124.8 (−3.9%) | 360.7 (177.9%) | 726.0 (459.4%) | 221.2 (70.4%) | 460.5 (254.8%) | 180.1 (38.7%) | 247.6 (90.8%) | |
| National | 1836.6 (26.9%) | 2422.0 (67.4%) | 1544.2 (6.7%) | 1885.6 (30.3%) | 1424.7 (−1.5%) | 1424.8 (−1.5%) | 3105.8 (114.7%) | 5660.4 (291.2%) | 2621.3 (81.3%) | 4430.2 (206.2) | 2421.4 (67.4%) | 3369.8 (132.9%) | |
The bold numbers indicate over 200% increases of the projected percentage change (%) relative to the baseline value.
NSW, New South Wales; Qld, Queensland; Vic, Victoria; WA, Western Australia; SA, South Australia; Tas, Tasmania; ACT, Australian Capital Territory; NT, Northern Territory.
Annual average value across periods.
Climate change
Given the mean temperature is expected to increase over time across Australia (Supplementary Fig. S4), we observed a gradual increase in the high temperature attributable BoKD from the 2030s to the 2050s, as expected. Additionally, under the assumption of no human adaptation, we found higher estimates of attributable BoKD under RCP8.5 compared to those under RCP4.5, with an increase ranging between 7.2% (1712.6 DALYs versus 1836.6 DALYs in 2030s) and 19.1% (4759.1 DALYs versus 5660.4 DALYs in 2050s), depending on the scenario of changes in population (Table 2). In addition, variations were observed between different jurisdictions in Australia. Jurisdictions with relatively higher proportions of BoKD attributable to high temperature (NT and ACT) also exhibited greater proportions of increased attributable burden in future projections compared to the national average (Table 1 and Supplementary Table S4), with the NT had the highest attributable BoKD rate (Supplementary Table S6).
Changes in population
Our findings indicate that future population growth and aging have a more substantial impact on the increase in high temperature-attributable BoKD than the influence of rising temperature due to climate change. For example, when comparing scenarios with constant population against those with future population changes, we observed that the high temperature attributable BoKD is projected to increase by 69% (from 1712.6 DALYs to 2896.1 DALYs under RCP4.5, and from 1836.6 DALYs to 3105.8 DALYs under RCP8.5) in the 2030s and more than double in the 2050s (Table 2). In addition, we assessed the contribution of changes in population size and age structure to the additional high temperature-related BoKD compared to the baseline, and found that the changes in population account for an increase of more than 80% of the projected high temperature attributable BoKD across all scenarios (Supplementary Table S5).
Human adaptation
The assumption of human adaptation has led to substantial variations in projections of future exposure of high temperature. For instance, when accounting for changes in the future population under the high-emission RCP8.5 scenario, the projected percentage increase in high temperature-attributable BoKD more than halved. It moved from 291.2% (15.1 DALYs per 100,000 population) under no adaptation, to 132.9% (10.8 DALYs per 100,000) under full adaptation scenario by the 2050s (Table 2 and Supplementary Table S4). In additional, we observed different effects in magnitude between jurisdictions when assuming human adaptations. Specifically, NT was found to be more sensitive to the assumptions of human adaptation, resulting in a larger decrease in the estimated high temperature-related BoKD. Similar patterns were observed in other jurisdictions, albeit with smaller magnitudes (Table 2 and Supplementary Table S4). Supplementary Fig. S8 depicts the geographical variation in the high temperature-related DALY rate for kidney disease, with higher rates and greater magnitudes observed in the northern and warmer regions of Australia.
Sensitivity analyses
Several sensitivity analyses confirmed the robustness of our results despite variations in the modelling choices during the baseline and future periods. These included alternative TMREDs, exposure periods, predictors, functional forms of exposure-response associations (linear/non-linear), climate projection models, and population projection scenarios (Supplementary Tables S7 and S8).
Discussion
The present study quantified the observed and future BoKD attributable to high temperatures in Australia using a comparative risk assessment and a nationwide dataset that included YLL and YLD. We used contemporary analytical techniques that considered local climates and exposure-response associations covering over 2000 geographically distinct areas, and accounted for variations in BoKD due to changes in population size and ageing. The investigation found that 2.7% of the BoKD in Australia during the baseline period (2003–2018) can be attributed to high temperature (Table 1). A gradually increasing trend is predicted due to the rising temperature over time (holding all other factors constant), with the attributable fraction increasing to 3.8% and 4.6% by 2050 under RCP4.5 and RCP8.5, respectively (Supplementary Table S4). Our projection accounting for changes in population size and age structure underscores the critical role of demographic factors in shaping the future BoKD attributable to high temperature in a warming climate (Table 2). In addition, the assumption of human adaptation to future climate change resulted in a substantial reduction in the projected BoKD attributable to high temperature, but it still remained higher than that of the baseline period in the majority of scenarios examined.
We observed spatial heterogeneity in the profile of BoKD and the impacts associated with high temperature. Regions with warmer climates, particularly the northern and central regions in Australia, had high temperature-related risks and PAFs (Fig. 2), and are projected to experience stronger impacts from future rising temperatures (Supplementary Fig. S4). Previous studies have documented that people living in hotter climates are more at risk of high temperature-induced kidney diseases.30 In both the baseline and projected periods, the rate of BoKD attributable to high temperature is significantly higher in the Northern Territory (NT) when compared to the national average (Table 1, Table 2). Within the NT, the SA2 areas in the northern and warmer region exhibit the highest rates of attribution (Supplementary Fig. S3 and S8). Factors contributing to the higher BoKD rates in the NT include higher baseline rates, heat vulnerability, living conditions, infrastructure problems, social and behavioural factors.22,31,32 This highlights the role that social determinants play in the impacts of climate change on local area populations.33 Notably, the high underlying rates of kidney disease in the Indigenous population, which has a younger age profile due to high fertility but low life expectancies, may also play a significant role in the higher proportion of BoKD in the younger age group in the NT (Fig. 1).32 This result emphasizes the disproportionate effects of increasing high temperature exposure on the lives of minoritized and Indigenous communities within Australia,33 and suggests that localized interventions that take regional characteristics into account may be beneficial in improving resilience to future climate change.
A thorough understanding of the health burden associated with high temperatures is critical for monitoring population health, prioritizing resources, and optimizing planning to prepare for the anticipated warming climate. While much previous research has only examined fatal burden (YLLs) to quantify the attributable burden of disease,10,11,34 our study incorporates both fatal and non-fatal burdens, providing a more comprehensive and precise picture.7,35 When examining only the fatal burden, our estimation of the annual average proportion of high temperature-attributable YLLs for kidney disease is largely comparable to the estimate provided by the Global Burden of Diseases (GBD) study for Australia. Specifically, during the baseline period (2003–2018), we found an annual proportion of 2.7%, compared with the GBD estimate of 2.5%.10 However, given the different purposes of international and local studies - the former to facilitate international comparisons and the latter to match resources and priorities to regional levels - local studies using national administrative and linked data are considered to have higher flexibility to meet local needs.16,35
Our projections indicate that the high temperature-induced BoKD is expected to increase in future decades, with hotter regions being the most affected, particularly under the high emission scenario (RCP8.5).29,36 Notably, our projections account for future adaptation, population growth, and aging, indicating that the projected increase in BoKD due to a warming climate will not be offset by adaptation. As Australia is projected to be one of the developed nations most vulnerable to the effects of climate change,8 our findings underscore the pressing need for additional mitigation measures to reduce greenhouse gas emissions, as well as proactive measures to better prepare Australia for the challenges ahead.
The findings of this study have unique strengths. It is the first international investigation to quantify both fatal and non-fatal BoKD that can be attributed to high temperature exposure at a national level. Previous studies have primarily focused on the fatal burden associated with all-cause mortality, while mechanisms underlying temperature-related health outcomes are diverse and disease-specific, and there have been many chronic kidney disease cases which have not been considered in such studies.29,36 Our analysis incorporated various sources of uncertainty, including exposure-response associations modelling, the projected future temperatures by the eight climate models, changes in population age structures and two projection series. This allowed us to comprehensively capture possible uncertainty. The set of sensitivity analyses highlights the robustness of our findings against the assumptions made. Additionally, we provided a detailed assessment of the baseline and projected BoKD attributable to high temperature in each of the jurisdictions, thereby enabling the development of more instructive heat health planning strategies that are tailored to the needs and challenges of each jurisdiction.
Limitations of our research must be acknowledged. We utilized linear interpolation to fill in missing values between years, assuming a constant rate of change between observed data points, which may not accurately reflect the underly trends of BoKD. Nevertheless, this method is often chosen for its simplicity and compatibility with historical data, allowing for the continuation of established methodologies.17,37 Given the lack of health information and future population projection in each SA2 level, we utilized the BoKD estimates and population projections obtained at the state and national levels, and then applied a downscaling method based on population distribution to estimate the BoKD and projected population at the SA2 level.36 This may result in overestimation or underestimation of the true values in certain regions, and therefore, the data should be interpreted with caution. In addition, a meta-regression model was built to predict the associated exposure-response relationship, using effect estimates obtained from international literature and location-specific meta-predictors (Supplementary Table S2). Although the predictors were found to explain most of the heterogeneity in the temperature-health relationship across locations,11 we were not able to account for other possible effect modifiers (e.g., age, sex and social and behavioural factors). The assumption involved in our future projections utilize the current estimates of exposure-response relationships, and as such does not take into unknown patterns and magnitudes of temperature-health associations that may occur in the future.19 Therefore, the reported estimates should be interpreted as potential impacts under well-defined but hypothetical scenarios.38 This study explored the future projection of attributable BoKD under the assumption of constant economic conditions in Australia, where economic development is relatively high.39
In order to reflect the attenuation of the adverse impact of high temperature on health,40 we assumed that human adaptation would occur as threshold temperature (TMRED) increases. Our approach to adaptation considers that regions experiencing greater shifts in future temperature distributions will also experience greater changes in human adaptation. Instead of assuming that all regions will adapt by a fixed absolute increase in TMRED (e.g., 0.2 °C per decade),41 we determine the magnitude of the shift on the exposure-response curve based on the climate and human adaptation scenarios we adopted (Supplementary Fig. S1). This approach allows for a more nuanced representation of how different regions may adapt to the changing climate, involving physiological, behavioural, and technological adaptations.27 However, the extent to which adaptation to high temperature will continue in Australia remains uncertain. Future studies are needed to more comprehensively assess the complex aspects incorporating measures of both physiological and socioeconomic adaptation, which can be strongly influence by within-community variation (built environment, education, and income).33,42 In addition, this study focused on the impact of high temperature exposure defined as the annual number of days where the daily mean temperature exceeded the TMREDs (MFT within the 54th to 92nd percentile range of mean temperature). It is worth noting that our assumption of the similarity in the TMRED and MFT may not hold true in all contexts and population, and therefore may introduced bias in some cases. However, the results of our sensitivity analysis using alternative TMREDs justified our decision to use MFTs (Supplementary Tables S7 and S8). In addition, in some regions of Australia, such as Tasmania, due to its geographic location, the TMRED can be as low as 7.8 °C, and above this temperature may not be typically perceived as ‘high’. Given these limitations, future studies are warranted to explore the entire spectrum of temperatures to obtain a more comprehensive understanding of their impact on human health.
In conclusion, our study reveals that future rising temperature will lead to an increase in high temperature-related BoKD in Australia, especially under the RCP8.5 scenario, and this effect will be amplified with the population growth and aging. These findings have important implications for public health interventions, emphasizing the need to focus on reducing attributable BoKD in the Northern Territory. Adaptation strategies should consider these factors to effectively reduce future BoKD in a warming climate.
Contributors
J.L., B.V., A.H., and P.B. conceived of the presented idea. J.L. conducted the analysis and wrote the first draft. B.V. and K.D. helped to design the analytical strategy and to interpret the findings. All authors critically revised the paper for intellectual content and approved the final version of the manuscript.
Data sharing statement
This manuscript makes use of data collected from the Australian Institute of Health and Welfare (AIHW), an official health data custodian in Australian; therefore, no original data is available for sharing due to confidentiality.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
The authors state no relevant conflicts of interest.
Acknowledgements
J.L. is supported by the Adelaide University China Fee Scholarships (The China Scholarship Council). This project is part of an Australian Research Council Discovery Program project (DP200102571 ‘awarded to PB’).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100916.
Appendix ASupplementary data
References
- 1.Vos T., Lim S.S., Abbafati C., et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tonelli M., Riella M. Chronic kidney disease and the ageing population. Lancet. 2014;383(9925):1278–1279. doi: 10.1016/S0140-6736(14)60155-0. [DOI] [PubMed] [Google Scholar]
- 3.La Porta E., Baiardi P., Fassina L., et al. The role of kidney dysfunction in COVID-19 and the influence of age. Sci Rep. 2022;12(1):8650. doi: 10.1038/s41598-022-12652-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Australian Institute of Health and Welfare Australian burden of disease study 2022. 2022. https://www.aihw.gov.au/reports/burden-of-disease/australian-burden-of-disease-study-2022/contents/summary
- 5.Liu J., Varghese B.M., Hansen A., et al. Hot weather as a risk factor for kidney disease outcomes: a systematic review and meta-analysis of epidemiological evidence. Sci Total Environ. 2021;801 doi: 10.1016/j.scitotenv.2021.149806. [DOI] [PubMed] [Google Scholar]
- 6.Borg M., Bi P., Nitschke M., Williams S., McDonald S. The impact of daily temperature on renal disease incidence: an ecological study. Environ Health. 2017;16(1):114. doi: 10.1186/s12940-017-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Australian Institute of Health and Welfare Chronic kidney disease: Australian facts. 2023. https://www.aihw.gov.au/reports/chronic-kidney-disease/chronic-kidney-disease/contents/summary
- 8.Trancoso R., Syktus J., Toombs N., Ahrens D., Wong K.K.H., Pozza R.D. Heatwaves intensification in Australia: a consistent trajectory across past, present and future. Sci Total Environ. 2020;742 doi: 10.1016/j.scitotenv.2020.140521. [DOI] [PubMed] [Google Scholar]
- 9.Barraclough K.A., Blashki G.A., Holt S.G., Agar J.W.M. Climate change and kidney disease—threats and opportunities. Kidney Int. 2017;92(3):526–530. doi: 10.1016/j.kint.2017.03.047. [DOI] [PubMed] [Google Scholar]
- 10.Burkart K.G., Brauer M., Aravkin A.Y., et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality: a two-part modelling approach applied to the Global Burden of Disease Study. Lancet. 2021;398(10301):685–697. doi: 10.1016/S0140-6736(21)01700-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao Q., Guo Y.L.Y., Ye T., et al. Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. Lancet Planet Health. 2021;5(7):e415–e425. doi: 10.1016/S2542-5196(21)00081-4. [DOI] [PubMed] [Google Scholar]
- 12.Australian Bureau of Statistics Australian statistical geography standard (ASGS): volume 1. Main structure and greater capital city statistical areas. 2016. https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/1270.0.55.001Main+Features10018July2016?OpenDocument
- 13.Commonwealth Science Industrial Research Organisation (CSIRO) Climate change in Australia. http://www.climatechangeinaustralia.gov.au/en/obtain-data/download-datasets/#ARD
- 14.World Meteorological Organization (WMO) WMO guidelines on the calculation of climate normals. 2017. https://library.wmo.int/doc_num.php?explnum_id=4166
- 15.Martínez-Solanas È., Quijal-Zamorano M., Achebak H., et al. Projections of temperature-attributable mortality in Europe: a time series analysis of 147 contiguous regions in 16 countries. Lancet Planet Health. 2021;5(7):e446–e454. doi: 10.1016/S2542-5196(21)00150-9. [DOI] [PubMed] [Google Scholar]
- 16.Liu J., Hansen A., Varghese B.M., et al. Estimating the burden of disease attributable to high ambient temperature across climate zones: methodological framework with a case study. Int J Epidemiol. 2022;52:783–795. doi: 10.1093/ije/dyac229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang G. Missing data filling method based on linear interpolation and lightgbm. J Phys Conf Ser. 2021;1754(1) doi: 10.1088/1742-6596/1754/1/012187. [DOI] [Google Scholar]
- 18.Scientific Information for Land Owners Australian climate data from 1889 to yesterday. https://www.longpaddock.qld.gov.au/silo/gridded-data/
- 19.Vicedo-Cabrera A.M., Sera F., Gasparrini A. Hands-on tutorial on a modeling framework for projections of climate change impacts on health. Epidemiology. 2019;30(3):321–329. doi: 10.1097/EDE.0000000000000982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Australian Bureau of Statistics (ABS) National, state and territory population. https://www.abs.gov.au/statistics/people/population/national-state-and-territory-454population/jun-2021#data-download
- 21.Australian Bureau of Statistics Population projections, Australia, 2017 (base)-2066. https://www.abs.gov.au/AUSSTATS/abs@.nsf/mf/3222.0
- 22.Wijnen A., Bishop K., Joshy G., Zhang Y., Banks E., Paige E. Observed and predicted premature mortality in Australia due to non-communicable diseases: a population-based study examining progress towards the WHO 25X25 goal. BMC Med. 2022;20(1):57. doi: 10.1186/s12916-022-02253-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beck H.E., Zimmermann N.E., McVicar T.R., Vergopolan N., Berg A., Wood E.F. Present and future Köppen-Geiger climate classification maps at 1-km resolution. Sci Data. 2018;5(1) doi: 10.1038/sdata.2018.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ross M.E., Vicedo-Cabrera A.M., Kopp R.E., et al. Assessment of the combination of temperature and relative humidity on kidney stone presentations. Environ Res. 2018;162:97–105. doi: 10.1016/j.envres.2017.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yin Q., Wang J., Ren Z., Li J., Guo Y. Mapping the increased minimum mortality temperatures in the context of global climate change. Nat Commun. 2019;10(1):4640. doi: 10.1038/s41467-019-12663-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Longden T. The impact of temperature on mortality across different climate zones. Clim Change. 2019;157(2):221–242. doi: 10.1007/s10584-019-02519-1. [DOI] [Google Scholar]
- 27.Anderson G.B., Oleson K.W., Jones B., Peng R.D. Projected trends in high-mortality heatwaves under different scenarios of climate, population, and adaptation in 82 US communities. Clim Change. 2018;146(3–4):455–470. doi: 10.1007/s10584-016-1779-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang B., Li G., Ma Y., Pan X. Projection of temperature-related mortality due to cardiovascular disease in beijing under different climate change, population, and adaptation scenarios. Environ Res. 2018;162:152–159. doi: 10.1016/j.envres.2017.12.027. [DOI] [PubMed] [Google Scholar]
- 29.Weinberger K.R., Haykin L., Eliot M.N., Schwartz J.D., Gasparrini A., Wellenius G.A. Projected temperature-related deaths in ten large U.S. metropolitan areas under different climate change scenarios. Environ Int. 2017;107(July):196–204. doi: 10.1016/j.envint.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lu P., Miao J., Feng S., et al. Temporal variations of the association between summer season heat exposure and hospitalizations for renal diseases in Queensland, Australia, 1995–2016. Environ Res Lett. 2022;17(6) doi: 10.1088/1748-9326/ac72b8. [DOI] [Google Scholar]
- 31.Schwartzkopff K.M., Kelly J., Potter C. Review of kidney health among aboriginal and torres strait Islander people. Aust Indig Health. 2020;20(4):3–4. [Google Scholar]
- 32.Hoy W.E. Kidney disease in aboriginal Australians: a perspective from the northern territory. Clin Kidney J. 2014;7(6):524–530. doi: 10.1093/ckj/sfu109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deivanayagam T.A., English S., Hickel J., et al. Envisioning environmental equity: climate change, health, and racial justice. Lancet. 2023;402(10395):64–78. doi: 10.1016/S0140-6736(23)00919-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cheng J., Xu Z., Bambrick H., Su H., Tong S., Hu W. Impacts of exposure to ambient temperature on burden of disease: a systematic review of epidemiological evidence. Int J Biometeorol. 2019;63(8):1099–1115. doi: 10.1007/s00484-019-01716-y. [DOI] [PubMed] [Google Scholar]
- 35.Zhao C., Choi C., Laws P., et al. Value of a national burden-of-disease study: a comparison of estimates between the Australian burden of disease study 2015 and the global burden of disease study 2017. Int J Epidemiol. 2022;51(2):668–678. doi: 10.1093/ije/dyab093. [DOI] [PubMed] [Google Scholar]
- 36.Yang J., Zhou M., Ren Z., et al. Projecting heat-related excess mortality under climate change scenarios in China. Nat Commun. 2021;12(1):1039. doi: 10.1038/s41467-021-21305-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Australian Institute of Health and Welfare . 2021. Australian burden of disease study: methods and supplementary material 2018. [DOI] [Google Scholar]
- 38.Gasparrini A., Guo Y.L.Y., Sera F., et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health. 2017;1(9):e360–e367. doi: 10.1016/S2542-5196(17)30156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dong W., Liu Z., Liao H., Tang Q., Li X. New climate and socio-economic scenarios for assessing global human health challenges due to heat risk. Clim Change. 2015;130(4):505–518. doi: 10.1007/s10584-015-1372-8. [DOI] [Google Scholar]
- 40.Schwartz J.D., Lee M., Kinney P.L., et al. Projections of temperature-attributable premature deaths in 209 U.S. cities using a cluster-based Poisson approach. Environ Health. 2015;14(1):85. doi: 10.1186/s12940-015-0071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dong S., Wang C., Han Z., Wang Q. Projecting impacts of temperature and population changes on respiratory disease mortality in Yancheng. Phys Chem Earth Parts A/B/C. 2020;117 doi: 10.1016/j.pce.2020.102867. [DOI] [Google Scholar]
- 42.Rai M., Breitner S., Wolf K., Peters A., Schneider A., Chen K. Future temperature-related mortality considering physiological and socioeconomic adaptation: a modelling framework. Lancet Planet Health. 2022;6(10):e784–e792. doi: 10.1016/S2542-5196(22)00195-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.