SUMMARY
Spontaneous subarachnoid hemorrhage (SAH) can occur unexpectedly and independently of the classic risk factors. Several different factors could affect intracranial aneurysm (IA) rupture, such as morphological and hemodynamic factors. The aim of this study was to establish the potential association of meteorological data such as temperature, atmospheric pressure, and humidity, and the onset of clinical symptoms preceding hospital admission of patients with acute SAH due to IA rupture. This retrospective study included 130 consecutive patients admitted for non-traumatic SAH with a determinable onset of SAH symptoms. The effects of meteorological parameters of atmospheric pressure, ambient temperature, and relative air humidity on the day of acute SAH onset and 24 hours prior to the onset of symptoms were recorded and analyzed in each patient. Spearman rank correlation analysis was used to assess the risks of incident SAH on the basis of daily meteorological data. Seasonal incidence of acute SAH showed the peak incidence in winter and a trough in summer, with monthly incidence peak in January and December. The circadian rhythm analysis showed the peak incidence of SAH in the forenoon, followed by the evening. Acute SAH incidence showed moderate positive association with daily atmospheric pressure (p<0.05), while no association was found with ambient temperature and relative air humidity. Our results suggested no significant association of changes in ambient temperature and relative humidity with the risk of SAH. Increases in atmospheric pressure were weakly associated with a higher SAH risk. Additional studies are needed to establish in detail both meteorological and morphological factors important to predict IA rupture and SAH.
Key words: Meteorological variables, Subarachnoid hemorrhages, Intracranial aneurysms
Introduction
Spontaneous subarachnoid hemorrhage (SAH) is a major condition with the annual incidence of approximately 91 per 100 000. The vast majority of SAH cases, around 85%, are caused by intracranial aneurysm (IA) rupture, which is one of the most serious complications associated with aneurysms. Morbidity and mortality of aneurysmal SAH remain high (1, 2). Approximately one-third of all patients suffering from SAH do not survive the first month after initial incident, while half of the survivors remain disabled (1, 3). Although case fatality of SAH from a ruptured IA has decreased over the last decades, further decrease will not be easy to achieve because of the considerable proportion of patients who die before reaching the hospital. In order to create strategies to prevent SAH, detailed insight in the risk factors analysis and the pathophysiology of IA rupture is necessary (4, 5).
Therefore, it is critical to understand the risk factors associated with this disease. The mechanisms underlying IA development and the factors associated with IA rupture are not yet fully understood. Several environmental risk factors for IA rupture resulting in SAH are gender, age, region, high blood pressure, smoking, high alcohol intake, female sex, and a family history of IA (5-12). The mentioned factors discriminate poorly between high and low risk aneurysms, and most SAH occur unexpectedly and independently of these risk factors. In addition, other, extensive studies analyzed morphological factors and differences between ruptured and unruptured IA, such as the size, shape, the neck, etc., as well as hemodynamic factors (13-17).
Furthermore, it was previously suggested and discussed that an additional possible risk factor of IA rupture and SAH could be seasonal or meteorological factors; some studies found that meteorological changes were associated with an increased incidence of SAH (18-26), whereas others report absence of such association (27-31). When observing and analyzing the data presented, the associations that have been observed appear to be conflicting. Even a recent meta-analysis was not able to determine the association between meteorological factors and SAH due to heterogeneity of data from previously published studies (5). One of the main uncertainties was whether the relations observed between meteorological factors and SAH incidence were chance findings, or the lack of association in negative studies was caused by too small numbers of included patients to detect the association. Furthermore, published results vary greatly depending on geography, climate, and study design. Therefore, evidence regarding the impact of meteorological factors on the SAH incidence remains a matter of debate.
The aim of this study was to establish the potential association of meteorological data such as temperature, atmospheric pressure, and humidity, and the onset of clinical symptoms preceding hospital admission of patients with acute SAH due to IA rupture. Determining the weather-related risk of SAH can help in IA rupture prediction and improve population health.
Patients and Methods
This retrospective study was conducted at the Department of Neurosurgery and Department of Neurointerventional Radiology, Sestre milosrdnice University Hospital Center, Zagreb, Croatia, from January 1, 2016 till June 1, 2021, with an area coverage of around 200 km. The study included 130 consecutive patients, 87 female and 43 male. Patient data were collected and analyzed from hospital electronic medical records including the patients discharged from the hospital with a diagnosis of SAH (I60.x, International Classification of Diseases, 10th Revision).
Available patient-related medical data including clinical, laboratory and neuroradiological reports were individually analyzed to identify patients diagnosed and treated due to acute SAH. Diagnosis of SAH was confirmed in all included patients using computerized tomography angiography. Additional data obtained from patient files included age, sex, date of onset of symptoms and date of aneurysm rupture and hospital admission, aneurysmal size, the World Federation of Neurological Surgeons grading score for subarachnoid hemorrhage (WFNS) and Fisher grading. Exclusion criteria were as follows: incomplete or inaccessible patient data, history of head trauma of at least 48 hours prior to the onset of clinical symptoms, indeterminable time of clinical symptom onset, and admission due to the reason other than acute SAH.
In addition, geographical location, above sea level and time of symptom onset were recorded for each individual patient. Data on weather conditions and indicators were obtained from the Croatian Meteorological and Hydrological Service (https://meteo.hr/). The following meteorological parameters on the day of acute SAH onset and 24 hours prior to the onset of symptoms in each patient were recorded: daily maximum, minimum and mean ambient temperatures (°C), daily mean relative humidity (%), and daily mean atmospheric pressure (hPa). Changes in these meteorological parameters were calculated as differences between the day of and day before the onset of acute SAH. All data were checked for accuracy by two independent researchers.
Statistical data analysis was performed using MedCalc Statistical Software version 12.5.0 (MedCalc Software, Ostend, Belgium; https://www.medcalc.org). Distribution was assessed by the Kolmogorov-Smirnov test, while χ2-test was used for qualitative variables. The associations between meteorological parameters and various patient data were assessed by Pearson correlation coefficient or Spearman’s rank correlation. The level of statistical significance was set at p<0.05.
Results
Between January 1, 2016 and January 1, 2021, a total of 130 consecutive patients (87 female and 43 male) were included in the study. Patient characteristics are shown in Table 1. The mean age of all patients was 51.51±12.97 years, with 57.91±14.05 in female and 52.01±13.17 in male patients. The highest incidence of aneurysms was recorded in the middle cerebral artery (34/130, 26.15%), followed by the anterior communicating artery (26/130, 20.00%) (Table 1). The rupture rates for aneurysm sizes <7 mm were 68/130 (52.31%), >7 mm 45/130 (34.61%) and undetermined 17/130 (13.07%) (Table 1). The WFNS SAH and Fisher grading were determined in all included patients (Table 1).
Table 1. Patient characteristics.
| Summary statistics | n | % |
|---|---|---|
| Total patients | 130 | 100 |
| Sex | ||
| Female | 87 | 67 |
| Male | 43 | 33 |
| Age, years (mean ± SD) | 51.51±12.97 | |
| Female | 57.91±14.05 | |
| Male | 52.01±13.17 | |
| Location of ruptured IA | ||
| ICA | 15 | 11.53 |
| MCA | 34 | 26.15 |
| ACA | 16 | 12.30 |
| PCA | 3 | 2.30 |
| ACoA | 26 | 20.00 |
| PCoA | 11 | 8.46 |
| VBA | 3 | 2.30 |
| Other | 22 | 16.92 |
| Size of ruptured IA | ||
| ≤7mm | 68 | 52.31 |
| ≥7mm | 45 | 34.61 |
| Undetermined | 17 | 13.07 |
| WFNS | ||
| 1-2 | 84 | 64.62 |
| 3-5 | 46 | 35.38 |
| Fisher grading | ||
| 1-3 (no intracerebral or intraventricular clots) | 48 | 36.92 |
| 4 (intracerebral or intraventricular clots) | 82 | 63.08 |
IA = intracranial aneurysm; ACA = anterior cerebral artery; AcoA = anterior communicating artery; ICA = internal carotid artery; MCA = middle cerebral artery; PCA = posterior cerebral artery; PCoA = posterior communicating artery; VBA = vertebrobasilar artery; WFNS = World Federation of Neurological Surgeons subarachnoid hemorrhage grading.
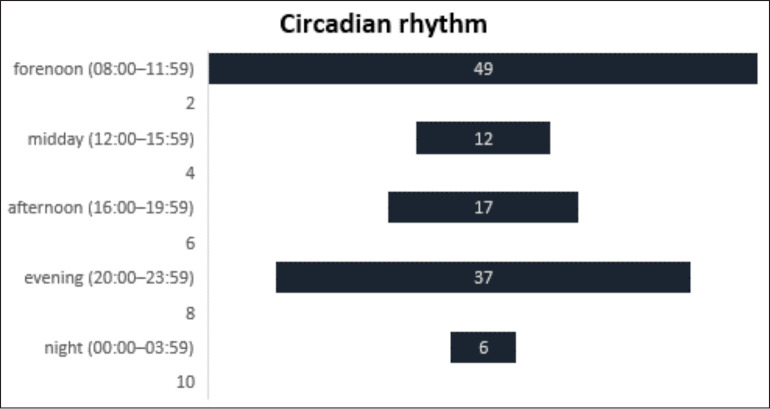
We presented data according to months and seasons (winter, spring, summer and fall); additionally, circadian rhythm was analyzed according to the time of acute SAH onset on the basis of the following six 4-hour periods: morning (04:00-07:59), forenoon (08:00-11:59), midday (12:00-15:59), afternoon (16:00-19:59), evening (20:00-23:59), and night (00:00-03:59). Total acute SAH incidence according to seasons, months and time at onset is shown in Table 2.
Table 2. Month, season and circadian rhythm analysis.
| Month analysis, n | Season analysis, n | Circadian rhythm analysis, n | |||
|---|---|---|---|---|---|
| January | 21 | Winter | 50 | Morning (04:00-07:59) | 9 |
| February | 11 | ||||
| March | 10 | Spring | 24 | Forenoon (08:00-11:59) | 49 |
| April | 6 | ||||
| May | 8 | Midday (12:00-15:59) | 12 | ||
| June | 6 | Summer | 21 | ||
| July | 9 | Afternoon (16:00-19:59) | 17 | ||
| August | 6 | ||||
| September | 15 | Fall | 35 | Evening (20:00-23:59) | 37 |
| October | 7 | ||||
| November | 13 | Night (00:00-03:59) | 6 | ||
| December | 18 | Winter | 50 | ||
The peak monthly incidence was in December (18/130) and January (21/130), and the trough monthly incidence was in April, June and August (6/130). The seasonal incidence peaked in winter (December to February, 50/130) and exhibited a trough in summer (June to August, 21/130; p<0.05). The peak incidence of SAH was recorded in the forenoon (08:00-11:59; 49/130), followed by the evening (20:00-23:59; 37/130), whereas the trough was at night (00:00-03:59; 6/130; p<0.05).
Daily mean temperature (r=0.026, p<0.58), daily maximum temperature (r=0.18, p<0.98), and daily minimum temperature (r=0.21, p<0.12) showed no association with daily SAH incidence, and so did not daily mean relative humidity either (r=0.18, p=0.21). Meanwhile, daily mean atmospheric pressure yielded a moderate positive association with acute SAH incidence (r=0.048, p<0.05).
Next, daily fluctuations in temperature and fluctuations on the day of acute SAH onset and 24 hours prior to the onset of symptoms in each patient showed no association between the incidence of SAH and fluctuations in the factors analyzed.
Discussion
In our study, we aimed to establish the potential association of meteorological data such as temperature, atmospheric pressure and humidity, and the onset of clinical symptoms preceding hospital admission of patients with acute SAH due to IA rupture. The effects of meteorological changes on IA rupture and consequential SAH remain a matter of debate because of the inconsistent findings of studies evaluating the relationship between different weather conditions and SAH incidence.
The peak seasonal and monthly incidence of SAH was highest in winter (January and February), and lowest in spring (April) and summer (June and August) (Fig. 1). Furthermore, circadian rhythm analysis showed the peak incidence of SAH to be significantly higher in the forenoon (37.69%), followed by the evening (28.46%), whereas the trough was at night (4.61%) (Fig. 2).
Fig. 1.
Seasonal incidence of acute subarachnoid hemorrhage showing the peak incidence in winter (December to February) and a trough in summer (June to August). Monthly incidence peaked in January and December, and the trough monthly incidence was in April, June and August.
Fig. 2.
Circadian rhythm analysis showed the peak incidence of subarachnoid hemorrhage in the forenoon (08:00-11:59; 49/130), followed by the evening (20:00-23:59; 37/130), whereas the trough was at night (00:00-03:59; 6/130; p<0.05).
Additionally, daily mean temperature, daily maximum temperature and daily minimum temperature showed no association with daily SAH incidence, and so did not the mean relative humidity either, while daily mean atmospheric pressure yielded a moderate positive association with acute SAH incidence and hospital admission for ruptured IAs. Meanwhile, daily fluctuations in temperature and relative humidity, as well as fluctuations on the day of acute SAH onset and 24 hours prior to the onset of symptoms showed no association between the incidence of SAH and fluctuations in the factors analyzed.
Low SAH incidence in summer, as observed in our study, has also been reported elsewhere (5, 32). The phenomenon was previously explained by meteorological determinants and the physiological processes they influence. On the contrary, the higher SAH incidence during winter could be explained by various factors. Lower temperatures during winter induce peripheral vasoconstriction leading to increased blood and pulse pressure. High blood pressure is an established risk factor for SAH (32). The mentioned cascade, especially under abrupt temperature changes, may produce wall deformity and increase friction and shear stress on the IA (5, 19, 26, 33). In addition, physiological responses to cold during winter, such as increases in platelet and red cell counts, increased sympathetic nerve activity, decreased factor VIII, antithrombin III and platelet aggregation, increased fibrinolytic activity, etc., should be taken into account (5, 33). Furthermore, cold weather leads to altered human behavioral response such as smoking indoors, increased alcohol intake, decreased physical exercise, etc. (5, 26).
Although previous studies have reported that temperature changes may increase the SAH incidence (19, 21, 22, 24-26), our results showed no association between temperature changes and SAH incidence. Regarding association between atmospheric change in pressure, these data are inconclusive and controversial. Increased SAH risk has been reported in correlation with increasing atmospheric pressure in different geographical regions (34-40), while other studies report on an increased SAH risk associated with decreased atmospheric pressure (41) or even absence of association (25, 27). There is a significant number of published papers showing some kind of association between atmospheric pressure change and SAH incidence, probably because papers with negative results are rarely published, as pointed previously (31). Furthermore, several authors speculate that atmospheric pressure may affect blood or intracranial pressure, leading to possible IA rupture (40, 42). Still, at this time, there is no satisfactory explanation for the association between atmospheric pressure changes and SAH.
In only a few studies did humidity correlate with SAH incidence (23, 27). There are no studies that confirm correlation of precipitation and IA rupture. In this study, we did not take into account sunlight exposure. Currently, there are several papers regarding this parameter that show clinical meaningfulness, albeit contradictory (23, 43).
Since more factors influence SAH incidence and IA rupture, we have to mention hemodynamic changes that may cause morphological changes and thus play an important role in the occurrence, development and rupture of IA (44, 45). Furthermore, the effect of the combination of meteorological factors, hemodynamic changes and aneurysm morphology on the prediction of IA rupture has not been in depth investigated. Very few studies combined morphological parameters of IA and meteorological variables, indicating that some IA that were not considered likely to rupture may rupture easily in high-risk meteorological conditions (26).
This study had several limitations that should be considered. First, this was a retrospective study. Second, the meteorological data assessed in this study were limited. For the meteorological factors included (temperature, atmospheric pressure, and humidity), values were measured three times a day, i.e., at 7 a.m. and 2 and 9 p.m.; daily mean values were also included in the analysis. This may have weakened assessments of the complexity of meteorological changes. Future studies with large samples and abundant meteorological data will be necessary to overcome these limitations. Finally, our study did not include 6%-14% of patients who died of SAH before reaching the hospital, which could have resulted in underrepresentation of patients with the most severe bleedings (46). Additionally, we acknowledge the possibility that patients with less severe bleedings were also underrepresented as these patients often present with minor symptoms and are misdiagnosed in approximately 10% of cases (47).
Conclusion
The results presented in this study suggest no significant association between changes of ambient temperature and relative humidity and SAH incidence. In addition, increases in atmospheric pressure were weakly associated with a higher SAH incidence, but the significance of this result remains unclear. Further studies are needed to establish in detail the possible association between meteorological factors in combination with other previously described risk factors, as well as morphological and hemodynamic factors important to predict IA rupture and SAH.
References
- 1.Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2(1):43–53. 10.1016/S1474-4422(03)00266-7 [DOI] [PubMed] [Google Scholar]
- 2.Macdonald RL, Schweizer TA. Spontaneous subarachnoid haemorrhage. Lancet. 2017;389(10069):655–66. 10.1016/S0140-6736(16)30668-7 [DOI] [PubMed] [Google Scholar]
- 3.Hackett ML, Anderson CS. Health outcomes 1 year after subarachnoid hemorrhage: an international population-based study. The Australian Cooperative Research on Subarachnoid Hemorrhage Study Group. Neurology. 2000;55(5):658–62. 10.1212/WNL.55.5.658 [DOI] [PubMed] [Google Scholar]
- 4.de Rooij NK, Linn FH, van der Plas JA, Algra A, Rinkel GJ. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry. 2007;78(12):1365–72. 10.1136/jnnp.2007.117655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Steenhuijsen Piters WA, Algra A, van den Broek MF, Dorhout Mees SM, Rinkel GJ. Seasonal and meteorological determinants of aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J Neurol. 2013;260(2):614–9. 10.1007/s00415-012-6687-z [DOI] [PubMed] [Google Scholar]
- 6.van Gijn J, Rinkel GJ. Subarachnoid haemorrhage: diagnosis, causes and management. Brain. 2001;124(Pt 2):249–78. 10.1093/brain/124.2.249 [DOI] [PubMed] [Google Scholar]
- 7.Qureshi AI, Suri MF, Yahia AM, et al. Risk factors for subarachnoid hemorrhage. Neurosurgery. 2001;49(3):607–12. 10.1097/00006123-200109000-00014 [DOI] [PubMed] [Google Scholar]
- 8.Broderick JP, Viscoli CM, Brott T, et al. Major risk factors for aneurysmal subarachnoid hemorrhage in the young are modifiable. Stroke. 2003;34(6):1375–81. 10.1161/01.STR.0000074572.91827.F4 [DOI] [PubMed] [Google Scholar]
- 9.Sandvei MS, Romundstad PR, Müller TB, Vatten L, Vik A. Risk factors for aneurysmal subarachnoid hemorrhage in a prospective population study: the HUNT study in Norway. Stroke. 2009;40(6):1958–62. 10.1161/STROKEAHA.108.539544 [DOI] [PubMed] [Google Scholar]
- 10.Korja M, Silventoinen K, Laatikainen T, Jousilahti P, Salomaa V, Hernesniemi J, et al. Risk factors and their combined effects on the incidence rate of subarachnoid hemorrhage – a population-based cohort study. PLoS One. 2013;8(9):e73760. 10.1371/journal.pone.0073760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Can A, Castro VM, Ozdemir YH, Dagen S, Yu S, Dligach D, Finan S, Gainer V, Shadick NA, Murphy S, Cai T, Savova G, Dammers R, Weiss ST, Du R. Association of intracranial aneurysm rupture with smoking duration, intensity, and cessation. Neurology. 2017:26;89(13):1408-15. doi: 10.1212/WNL.0000000000004419. 10.1212/WNL.0000000000004419 [DOI] [PMC free article] [PubMed]
- 12.Figueredo LF, Camila Pedraza-Ciro M, Sebastian Lopez-McCormick J, Javier Rueda-Esteban R, Armando Mejía-Cordovez J. Aneurysmal subarachnoid hemorrhage associated with small aneurysms in smokers and women: a retrospective analysis. World Neurosurg X. 2019;4:100038. 10.1016/j.wnsx.2019.100038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsukawa H, Uemura A, Fujii M, Kamo M, Takahashi O, Sumiyoshi S. Morphological and clinical risk factors for the rupture of anterior communicating artery aneurysms. J Neurosurg. 2013;118(5):978–83. 10.3171/2012.11.JNS121210 [DOI] [PubMed] [Google Scholar]
- 14.Li M, Jiang Z, Yu H, Hong T. Size ratio: a morphological factor predictive of the rupture of cerebral aneurysm? Can J Neurol Sci. 2013;40(3):366–71. 10.1017/S0317167100014323 [DOI] [PubMed] [Google Scholar]
- 15.Long Y, Zhong J, Yu H, Yan H, Zhuo Z, Meng Q, et al. A scaling aneurysm model-based approach to assessing the role of flow pattern and energy loss in aneurysm rupture prediction. J Transl Med. 2015. September 22;13:311. 10.1186/s12967-015-0673-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou G, Zhu Y, Yin Y, Su M, Li M. Association of wall shear stress with intracranial aneurysm rupture: systematic review and meta-analysis. Sci Rep. 2017:13;7(1):5331. doi: 10.1038/s41598-017-05886-w. 10.1038/s41598-017-05886-w [DOI] [PMC free article] [PubMed]
- 17.Cai W, Hu C, Gong J, Lan Q. Anterior communicating artery aneurysm morphology and the risk of rupture. World Neurosurg. 2018;109:119–26. 10.1016/j.wneu.2017.09.118 [DOI] [PubMed] [Google Scholar]
- 18.Rosenørn J, Rønde F, Eskesen V, Schmidt K. Seasonal variation of aneurysmal subarachnoid haemorrhage. Acta Neurochir (Wien). 1988;93(1-2):24–7. 10.1007/BF01409898 [DOI] [PubMed] [Google Scholar]
- 19.Gill RS, Hambridge HL, Schneider EB, Hanff T, Tamargo RJ, Nyquist P. Falling temperature and colder weather are associated with an increased risk of aneurysmal subarachnoid hemorrhage. World Neurosurg. 2013;79(1):136–42. 10.1016/j.wneu.2012.06.020 [DOI] [PubMed] [Google Scholar]
- 20.Jeong TS, Park CW, Yoo CJ, Kim EY, Kim YB, Kim WK. Association between the daily temperature range and occurrence of spontaneous intracerebral hemorrhage. J Cerebrovasc Endovasc Neurosurg. 2013;15(3):152–7. 10.7461/jcen.2013.15.3.152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neidert MC, Sprenger M, Wernli H, Burkhardt JK, Krayenbühl N, Bozinov O, Regli L, Woernle CM. Meteorological influences on the incidence of aneurysmal subarachnoid hemorrhage – a single center study of 511 patients. PLoS One. 2013:2;8(12):e81621. doi: 10.1371/journal.pone.0081621. 10.1371/journal.pone.0081621 [DOI] [PMC free article] [PubMed]
- 22.Miranpuri AS, Aktüre E, Baggott CD, Miranpuri A, Uluç K, Güneş VE, et al. Demographic, circadian, and climatic factors in non-aneurysmal versus aneurysmal subarachnoid hemorrhage. Clin Neurol Neurosurg. 2013;115(3):298–303. 10.1016/j.clineuro.2012.05.039 [DOI] [PubMed] [Google Scholar]
- 23.Lai PM, Dasenbrock H, Du R. The association between meteorological parameters and aneurysmal subarachnoid hemorrhage: a nationwide analysis. PLoS One. 2014:13;9(11):e112961. doi: 10.1371/journal.pone.0112961. 10.1371/journal.pone.0112961 [DOI] [PMC free article] [PubMed]
- 24.Lee S, Guth M. Associations between temperature and hospital admissions for subarachnoid hemorrhage in Korea. Int J Environ Res Public Health. 2017:21;14(4):449. doi: 10.3390/ijerph14040449. 10.3390/ijerph14040449 [DOI] [PMC free article] [PubMed]
- 25.Tarnoki AD, Turker A, Tarnoki DL, Iyisoy MS, Szilagyi BK, Duong H, Miskolczi L. Relationship between weather conditions and admissions for ischemic stroke and subarachnoid hemorrhage. Croat Med J. 2017:28;58(1):56-62. doi: 10.3325/cmj.2017.58.56. 10.3325/cmj.2017.58.56 [DOI] [PMC free article] [PubMed]
- 26.Li M, Hu S, Yu N, Zhang Y, Luo M. Association between meteorological factors and the rupture of intracranial aneurysms. J Am Heart Assoc. 2019:3;8(17):e012205. doi: 10.1161/JAHA.119.012205. 10.1161/JAHA.119.012205 [DOI] [PMC free article] [PubMed]
- 27.Hughes MA, Grover PJ, Butler CR, Elwell VA, Mendoza ND. A 5-year retrospective study assessing the association between seasonal and meteorological change and incidence of aneurysmal subarachnoid haemorrhage. Br J Neurosurg. 2010;24(4):396–400. 10.3109/02688697.2010.499154 [DOI] [PubMed] [Google Scholar]
- 28.Cowperthwaite MC, Burnett MG. The association between weather and spontaneous subarachnoid hemorrhage: an analysis of 155 US hospitals. Neurosurgery. 2011;68(1):132–8. 10.1227/NEU.0b013e3181fe23a1 [DOI] [PubMed] [Google Scholar]
- 29.Ishikawa K, Niwa M, Tanaka T. Difference of intensity and disparity in impact of climate on several vascular diseases. Heart Vessels. 2012;27(1):1–9. 10.1007/s00380-011-0206-5 [DOI] [PubMed] [Google Scholar]
- 30.Han MH, Yi HJ, Ko Y, Kim YS, Lee YJ. Association between hemorrhagic stroke occurrence and meteorological factors and pollutants. BMC Neurol. 2016. May 4;16:59. 10.1186/s12883-016-0579-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kockler M, Schlattmann P, Walther M, Hagemann G, Becker PN, Rosahl S, et al. Weather conditions associated with subarachnoid hemorrhage: a multicenter case-crossover study. BMC Neurol. 2021;21(1):283. 10.1186/s12883-021-02312-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Feigin VL, Anderson CS, Rodgers A, Bennett DA. Subarachnoid haemorrhage occurrence exhibits a temporal pattern – evidence from meta-analysis. Eur J Neurol. 2002;9(5):511–6. 10.1046/j.1468-1331.2002.00455.x [DOI] [PubMed] [Google Scholar]
- 33.Gill JS, Davies P, Gill SK, Beevers DG. Wind-chill and the seasonal variation of cerebrovascular disease. J Clin Epidemiol. 1988;41(3):225–30. 10.1016/0895-4356(88)90125-4 [DOI] [PubMed] [Google Scholar]
- 34.Chyatte D, Chen TL, Bronstein K, Brass LM. Seasonal fluctuation in the incidence of intracranial aneurysm rupture and its relationship to changing climatic conditions. J Neurosurg. 1994;81(4):525–30. 10.3171/jns.1994.81.4.0525 [DOI] [PubMed] [Google Scholar]
- 35.Landers AT, Narotam PK, Govender ST, van Dellen JR. The effect of changes in barometric pressure on the risk of rupture of intracranial aneurysms. Br J Neurosurg. 1997;11(3):191–5. 10.1080/02688699746230 [DOI] [PubMed] [Google Scholar]
- 36.Nakaguchi H, Matsuno A, Teraoka A. Prediction of the incidence of spontaneous intracerebral hemorrhage from meteorological data. Int J Biometeorol. 2008;52(4):323–9. 10.1007/s00484-007-0128-1 [DOI] [PubMed] [Google Scholar]
- 37.Kim HJ, Kim JH, Kim DR, Kang HI, Moon BG, Kim JS. Age and meteorological factors in the occurrence of spontaneous intracerebral hemorrhage in a metropolitan city. J Cerebrovasc Endovasc Neurosurg. 2014;16(3):209–15. 10.7461/jcen.2014.16.3.209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Donkelaar CE, Potgieser ARE, Groen H, Foumani M, Abdulrahman H, Sluijter R, et al. Atmospheric pressure variation is a delayed trigger for aneurysmal subarachnoid hemorrhage. World Neurosurg. 2018;112:e783–90. 10.1016/j.wneu.2018.01.155 [DOI] [PubMed] [Google Scholar]
- 39.Huang Q, Lin SW, Hu WP, Li HY, Yao PS, Sun Y, et al. Meteorological variation is a predisposing factor for aneurysmal subarachnoid hemorrhage: a 5-year multicenter study in Fuzhou, China. World Neurosurg. 2019;132:e687–95. 10.1016/j.wneu.2019.08.048 [DOI] [PubMed] [Google Scholar]
- 40.Patrice T, Rozec B, Desal H, Blanloeil Y. Oceanic meteorological conditions influence incidence of aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2017;26(7):1573–81. 10.1016/j.jstrokecerebrovasdis.2017.02.031 [DOI] [PubMed] [Google Scholar]
- 41.Hori A, Hashizume M, Tsuda Y, Tsukahara T, Nomiyama T. Effects of weather variability and air pollutants on emergency admissions for cardiovascular and cerebrovascular diseases. Int J Environ Health Res. 2012;22(5):416–30. 10.1080/09603123.2011.650155 [DOI] [PubMed] [Google Scholar]
- 42.Herbowski L. The major influence of the atmosphere on intracranial pressure: an observational study. Int J Biometeorol. 2017;61(1):181–8. 10.1007/s00484-016-1202-3 [DOI] [PubMed] [Google Scholar]
- 43.Stienen MN, Smoll NR, Battaglia M, Schatlo B, Woernle CM, Fung C, et al. Swiss SOS study group . Intracranial aneurysm rupture is predicted by measures of solar activity. World Neurosurg. 2015;83(4):588–95. 10.1016/j.wneu.2014.12.021 [DOI] [PubMed] [Google Scholar]
- 44.Jamous MA, Nagahiro S, Kitazato KT, Tamura T, Aziz HA, Shono M, et al. Endothelial injury and inflammatory response induced by hemodynamic changes preceding intracranial aneurysm formation: experimental study in rats. J Neurosurg. 2007;107(2):405–11. 10.3171/JNS-07/08/0405 [DOI] [PubMed] [Google Scholar]
- 45.Xiang J, Natarajan SK, Tremmel M, Ma D, Mocco J, Hopkins LN, et al. Hemodynamic-morphologic discriminants for intracranial aneurysm rupture. Stroke. 2011;42(1):144–52. 10.1161/STROKEAHA.110.592923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lindekleiv HM, Njølstad I, Ingebrigtsen T, Mathiesen EB. Incidence of aneurysmal subarachnoid hemorrhage in Norway, 1999-2007. Acta Neurol Scand. 2011;123(1):34–40. 10.1111/j.1600-0404.2010.01336.x [DOI] [PubMed] [Google Scholar]
- 47.Kowalski RG, Claassen J, Kreiter KT, Bates JE, Ostapkovich ND, Connolly ES, Mayer SA. Initial misdiagnosis and outcome after subarachnoid hemorrhage. JAMA. 2004:18;291(7):866-9. doi: 10.1001/jama.291.7.866. 10.1001/jama.291.7.866 [DOI] [PubMed]