Abstract
Background
Workplace wellbeing programs can be beneficial but range widely in approach. A group coaching model offers numerous benefits.
Objective
To evaluate feasibility of group coaching for employees during COVID-19.
Methods
Employees (n = 29) at a university and university hospital underwent a 12-week group coaching program. Measurements of feasibility -- including enrollment, attendance at sessions goal attainment and satisfaction -- and exploratory outcomes including perceived physical and mental health and stress were administered at beginning, middle, and end of the program, plus 2 follow-ups.
Results
Twenty-six of the 29 program enrollees (96% women; 65% university employees) opted to complete surveys at 1 or more time points, and 9 individuals completed surveys at all 5 time points. Median attendance was 9 sessions. Participants opted to focus on movement, nutrition and mind/body goals and all participants reported making progress toward their goal during the program. Exploratory wellness outcomes showed meaningful improvements in perceived physical and mental health and reduced stress during the program, with return to near baseline 12 weeks after program completion. Perceptions of workplace wellness culture varied by employer.
Conclusion
Despite pandemic-related disruptions to life, work, and health, online group coaching is feasible and acceptable to participants. The program should be replicated to evaluate whether the improvements in exploratory wellness outcomes observed during the program are statistically significant. The apparent return to baseline levels by 24 weeks suggests that post-program maintenance support may be helpful.
Keywords: health coaching, employee wellbeing, behavioral change, wellness coaching, group coaching, wellness
Introduction
Background
Today, individuals spend nearly a quarter of the hours in a week working. 1 As more attention is brought to overall health and wellbeing, the work setting is an important environment to consider. An individual’s physical environment, including an organization or institution they are a part of, has a strong influence on their health and wellbeing. 2
Promoting wellbeing in the workplace can benefit employees’ physical and mental health, job satisfaction, motivation, leadership, and job-related stress. Although the evidence is mixed, employers may benefit through higher employee retention rates, productivity, and profits.3-5 Particularly in academic and health care settings, improvements in the wellbeing of employees can have secondary positive influences on the whole environment. 4 An industry-led study of best practices has identified that a whole person approach to wellness is needed in the workplace. 6
One whole person approach is Health and Wellness Coaching. This emerging health care field has already shown benefits for improving lifestyle-related health conditions and increasing self-efficacy. 7 Health and Wellness Coaching uses person-centered strategies such as motivational interviewing and goal-setting strategies to empower people to lead healthy lifestyles, increase self-awareness, and adopt effective self-management strategies. While most Health and Wellness Coaching research has been conducted on individual coaching, group health and wellness coaching provides camaraderie and accountability and facilitates peer-to-peer learning.7,8 Virtual group coaching may be especially impactful during times of global upheaval such as the COVID-19 pandemic, when in-person contact with others was greatly reduced.
National Board Certification for Health and Wellness Coaches educational and professional standards focus on individual coaching 9 ; however we wanted to study a group program as there has been a call for more research in this area. 7 With a lack of national standardization for group health and wellness coaching, our research team sought a novel program with demonstrated effectiveness in health promotion to use as a model for our group coaching program for employees. Our institution adapted the Open Source Wellness (OSW) group coaching model to an employee wellness setting. This model has been described as a “Behavioral Pharmacy” or an experimental program that uses a group approach, including small group coaching, to help people fill their behavioral prescriptions (ie, participant-chosen goals and actions). 10 The OSW model uses a four-part prescription: MOVE (physical activity), NOURISH (healthy meals), CONNECT (social support), and BE (stress reduction) to promote behavior changes for improved health and wellness, and has shown significant positive outcomes in individuals with chronic health conditions. 10 This model has yet to be studied in employee wellness.
The purpose of this study was to evaluate the feasibility of the OSW group coaching program, as adapted to a workplace environment, and its impact on physical and emotional wellness. We also explored the extent to which employees perceived their workplace to foster a culture of wellness.
Methods
Setting and Intervention
Employee Wellness departments at an American East Coast university and its affiliated medical center sent email blasts to employees and posted registration links on their websites for the employee coaching program. The program offered rolling admissions on the first Tuesday of each month. The 12-week virtual program, modeled after OSW, was led by Nationally Board Certified Health and Wellness Coaches and co-facilitated by students in the university’s Integrative Health and Wellness Coaching certificate program. We adapted the OSW program to make it relevant to employee wellness instead of health care environment. For example, the lessons were targeted toward an employee population instead of a clinical population with topics such as setting boundaries at work. The fundamental underpinnings of the OSW model remained intact. The OSW group coaching program was grounded in our wellness philosophy, depicted in Figure 1, which emphasizes the interconnectedness of 9 domains of health: mind and body, movement, nutrition, environment, relationships, personal development, spirituality, sleep and rest, and work life balance. As in OSW, participants were encouraged to connect with their peers following a community as medicine philosophy and set weekly prescriptions for themselves. Each one-hour weekly online session started with the employees all together for 25 minutes focusing on social connection, which included a 10-minute movement activity, a brief mindfulness exercise, and a lesson related to 1 of the domains of health identified on our Wheel of Health. Employees then went into breakout rooms with a coach and a student coach for 30 minutes of small group discussion and goal setting. Participants could choose more than 1 goal to focus on. The last 5 minutes of the session everyone returned to the large group space for final affirmations and gratitudes.
Figure 1.
The Wheel of Health represents the interconnectedness of the 9 domains of health used in our conceptual model. Used with permission from Osher Center for Integrative Health at the University of Vermont.
Measures
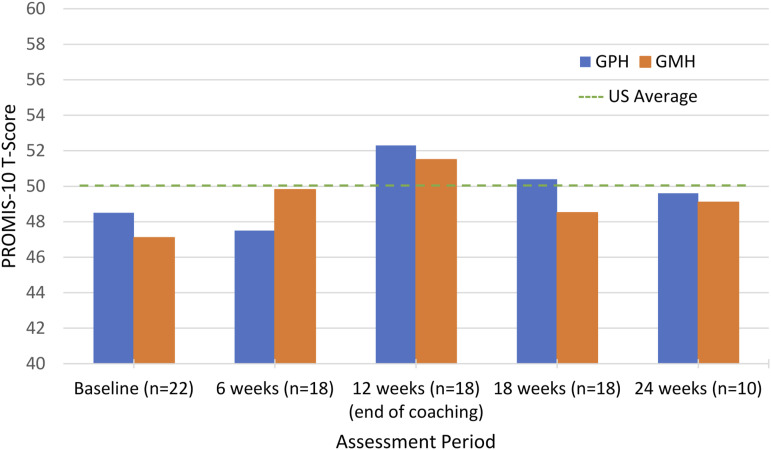
Demographic questions were assessed at the first survey. An additional set of surveys was administered at each timepoint and included the measures below. Self-reported physical and mental health was assessed using the Patient-Reported Outcomes Measurement Information System 10 (PROMIS-10) global physical health (GPH) and global mental health (GMH) scales. 11 The PROMIS-10 is scored using T-scores with a mean of 50 representing the average score for the US general population and standard deviation of 10. The higher the score, the better the health. Changes in T-scores of 2-6 points are considered meaningful by 1 standard. 12 Alternatively, by a different standard, changes are considered meaningful if they are greater than .5 standard deviation, ie, 6 T-score points on the PROMIS-10.13,14
Perceived stress was measured using the Perceived Stress Scale 4 (PSS-4); 15 Each of the 4 items is scored on a scale of 0-4. PSS-4 scores range between 0-16 with high scores indicating more stress. Burnout was measured using a 2-item burnout questionnaire. 16 Goal attainment was assessed using a Goal Attainment Scaling (GAS) 17 that was modified for self-report of “how much progress have you made on your goal?” Response options were “getting worse,” “almost no progress,” “a little progress,” “some progress,” “a lot of progress,” and “goal reached or almost reached.” Satisfaction/feasibility questions designed specifically for this program had response options of “Not at All,” “Somewhat,” or “Very” with an open comment option. In addition, 1 question assessed institutional support for/culture of wellness at program completion (“I believe my university/medical center has a culture and environment that promotes health and wellness for its staff,”) and 2 additional questions were added as proxies for institutional support: “I was given time off from work to attend,” and “I attended on my own time,” with response options of Yes, No and Unsure.
Procedure
Participants were invited to participate in the research by email at the time of registration and verbally at the first session. Participation in the research involved completing online surveys. The baseline survey had to be completed before the start of the second session. Participants were invited to complete additional surveys at 6 weeks, 12 weeks (end of the program), 18 weeks, and 24 weeks (12 weeks after completion of the program). The additional surveys were each left open for 1 week.
Attendance at 1 or more coaching sessions was set as the inclusion criterion so we could get feedback from all enrollees regardless of their attendance. Surveys were collected and managed using REDCap electronic data capture tools. Participants were invited to complete surveys for each timepoint independently; they were not asked to enroll in a longitudinal study at the start of the program. No compensation was provided for completing the surveys. This study was deemed exempt from review by the University Institutional Review Board because it was a program assessment.
Statistical Methods
Descriptive analyses were conducted using Microsoft Excel.
Results
Participant Characteristics
Mean age was 49 and all but 1 participant was female. Participants were employed by the University (n = 17; 65%) or Medical Center (n = 9; 35%), predominantly in staff positions (n = 17; 65%) but also as administrators (n = 4; 15%), health care practitioners (n = 3; 12%), and faculty (n = 1; 4%). One respondent did not specify their employment category.
Feasibility
Enrollment
Of 32 program enrollees, 3 no-showed leaving 29 remaining who were eligible to complete surveys. Twenty-six chose to complete online surveys at 1 or more timepoints. Twenty-seven participants began the program in September and 2 began in October.
Survey Completion Rates
Completion rates varied by employer and timepoint, as illustrated in Table 1. At 6 weeks, 2 participants completed only the PROMIS (the first survey in the set) so the response rate was lower for the remaining surveys in that set. The response rate was much lower at the 24-week time point, which corresponded to 12 weeks after completion of the active coaching period and fell during the university’s semester break. Nine participants completed surveys at all 5 timepoints.
Table 1.
Number and Percent of Completed Surveys at Each Time Point, by Institution.
| Timepoint | Responses to PROMIS-10 Survey n (%) | Responses to all Other Instruments n (%) | ||||
|---|---|---|---|---|---|---|
| University n = 17 | Hospital n = 9 | All n = 26 | University n = 17 | Hospital n = 9 | All n = 26 | |
| Baseline | 14 (82%) | 8 (89%) | 22 (85%) | 14 (82%) | 8 (89%) | 22 (85%) |
| 6 weeks | 12 (71%) | 6 (67%) | 18 (69%) | 10 (59%) | 6 (67%) | 16 (62%) |
| 12 weeks | 10 (59%) | 8 (89%) | 18 (69%) | 10 (59%) | 8 (89%) | 18 (69%) |
| 18 weeks | 13 (76%) | 5 (56%) | 18 (69%) | 13 (76%) | 5 (56%) | 18 (69%) |
| 24 weeks | 4 (24%) | 6 (67%) | 10 (38%) | 4 (24%) | 6 (67%) | 10 (38%) |
Attendance at Sessions
Session attendance ranged from 1 to 11 sessions (median = 9, IQR 7-10; skewness -1.1). As shown in Table 2, 22 (85%) participants attended 6 or more sessions, and over half of the participants attended 9 or more sessions.
Table 2.
Attendance at Group Coaching Sessions.
| Number of Sessions Attended, out of 12 | Number (%) of Participants Attending that Number of Sessions | Cumulative Attendance |
|---|---|---|
| 1 | 1 (4%) | 26 (100%) |
| 2 | 2 (8%) | 25 (96%) |
| 3 | 0 (0%) | 23 (88%) |
| 4 | 1 (4%) | 23 (88%) |
| 5 | 0 (0%) | 22 (85%) |
| 6 | 2 (8%) | 22 (85%) |
| 7 | 4 (15%) | 20 (76%) |
| 8 | 2 (8%) | 16 (61%) |
| 9 | 5 (19%) | 14 (53%) |
| 10 | 5 (19%) | 9 (34%) |
| 11 | 4 (15%) | 4 (15%) |
| 12 | 0 (0%) | 0 (0%) |
Note. Cumulative attendance means the number (%) of participants attending that number of sessions or more.
Acceptability
Of 9 domains of health included in our conceptual model (Figure 1), movement, nutrition, and mind/body were the most frequently selected focus areas. Respondents to the 12-week survey were very (n = 14; 78%) or somewhat (n = 4; 22%) satisfied with the program content and all 18 (100%) were satisfied with facilitator effectiveness. These participants thought the program was very (n = 10; 56%) or somewhat (n = 8; 44%) beneficial for achieving health-improvement goals, they were very (n = 10; 56%) or somewhat (n = 8; 44%) confident they would maintain their changes, and 94% of participants would recommend the program to peers. In the words of 1 participant, “I feel like the program helps with overall awareness of health and I like the goals as a focus for what I'm working on. I'm not sure the goal itself was what I achieved. I think the program really helped with building resilience and motivation to keep moving toward my goal.” All participants reported making at least a little progress toward their self-identified goal during the program. Respondents to the 12-week survey stated they made “at little progress” to “a lot of progress” on their goal, but no respondent had “reached or almost reached” their goal. Of the 10 respondents to the 24-week assessment, 1 participant reported they had achieved their original goal, 7 reported making “a little progress” or higher, and 2 individuals indicated they were “getting worse.”
Exploratory Wellness Outcomes
PROMIS-10 GPH T-scores at baseline for the group averaged 48.1 for respondents who completed the initial survey. PROMIS-10 GPH T-scores at 12 weeks for the group averaged 52.3 for respondents who completed the 12-week survey. PROMS-10 GPH scores at 24-week follow up for the group averaged 49.6 for respondents to the 24-week survey.
PROMIS-10 GMH scores at baseline averaged 47.4 for respondents to the initial survey. PROMIS-10 GMH scores at 12 weeks for the group averaged 54.5 for respondents to the 12-week survey. PROMIS-10 GMH scores at 24-week follow up for the group averaged 49.1 for respondents to the 24-week survey. Figure 2 shows GPH and GMH scores against the US general population.
Figure 2.
Exploratory patient reported outcomes measurement system – 10 (PROMIS-10) T-scores for global physical health and global mental health as assessed at initial, 6-week, 12-week, 18-week, and 24-week time points. The 12-week assessment corresponds to the end of the group coaching sessions. The dashed line indicates the US average T-score of 50. GPH = Global physical health; GMH = Global mental health.
Group average PSS-4 scores declined from 5.14 in the initial survey to 3.72 at 12 weeks, then increased to 4.5 at 24 weeks. See Supplementary Figure.
Responses to feeling burnt out at work ranged from every day to never. Approximately 40% responded either “a few times a year or less” or “once a month or less” at each of the 5 time points and a maximum of 25% at any of the 5 time points said they felt burnt out at work a few times a week or more. On all 5 surveys, responses to feeling callous toward people ranged from “a few times a week” (<6% of respondents) to “never” (25%–60% of respondents). There were no discernable trends over time.
Responses to the wellness culture items assessed at the 12-week survey showed institutional differences (see supplemental material). All 8 (100%) medical center employees said their workplace has a culture and environment that promotes health and wellness for its staff, yet only 3 (38%) were given some time off from work to attend this midweek noon time program and 5 (63%) said they attended at least partially on their own time. In contrast, just 6 (60%) of university employees said their workplace has a culture and environment that promotes health and wellness for its staff. Most (90%) university employees said they attended at least partly on their own time.
Discussion
Summary of the Program
This novel effort to adapt the OSW model from a health care to a workplace setting successfully enrolled and retained employees during the time of a global pandemic when most employees were working from home. The pandemic required us to conduct the program entirely online instead of the in-person format we had planned and which we suspect would have improved the engagement of participants. However, by offering the program virtually, we increased accessibility to all employees. It was difficult to predict at the outset what attendance to a virtual program would be like, due to its novelty. Half of the participants attended 9 or more of the 12 scheduled sessions and only 3 participants attended fewer than 4 sessions. These results are promising for the future of online employee health and wellness programming. Participants, predominantly women in staff positions at a university and university medical center who were in generally good health at baseline, were satisfied with the program content, facilitators, and behavior-change outcomes and said they would recommend the program to peers.
Results of the behavior-change and wellbeing targets of the program were mixed. While all participants reported they had made progress toward their goals, none had reached their goal by the end of the 12-week program. By 12 weeks after the program completed, 1 had fully achieved their goal but 2 indicated they were doing worse. Very low goal attainment could be due to the program not emphasizing the attainment of a single goal clearly enough as an outcome. Our client centered process allowed employees to change their goals over the course of the 12-week program making it difficult to know how to respond to the survey question that read “Thinking about the SMART goal you set for yourself, please rate your present status.” Our survey question was not able to capture the changes in goals that were observed. It is also possible that the rolling enrollment process interfered with goal attainment. New employees could enter the program at the beginning of the second month of the program. This is the OSW model which allows individuals who missed the first enrollment to join without waiting a full 12 weeks for a new session to start. Also, the overlap of current and new participants in OSW is thought to promote a group culture. 10 In our experience, rolling enrollment posed a challenge in that new people were being added each month which resulted in variation of the lessons each person heard and at what time points in the process. It also presented scheduling challenges in an academic environment that is focused on semester-length activities.
Regarding the exploratory wellness outcomes of perceived stress, physical health and mental health, we did see changes to group averages both during and after the program. However, this study was not powered for inferential analysis and is not an outcomes study. Burnout did not appear to change in any systematic way over the course of the program or follow-up period, possibly due to a floor effect because we did not specifically recruit employees known to have burnout.
There were differences between the 2 organizations in perceived culture of wellness. Employee cultures are modifiable, as demonstrated in a Veterans Administration employee well-being program that resulted in lower turnover rates, decreased burnout rates, and higher employee motivation on the job. 4 Investment in a high-quality employee well-being program can benefit employees and the organization overall.
An important facilitator of our successful implementation of this employee program was the leadership support we had from the university Provost, who is a strong supporter of wellness initiatives. In addition, the employee wellness departments at both institutions financially supported the program operation. Notably, both employee wellness programs receive funding from their medical health insurance provider.
Limitations
This pre-post-follow up evaluation did not include a control group so it’s possible that the gains observed in this program are due to external factors such as secular trends, regression to the mean, social desirability or even the opportunity to have a break in one’s workday. However, it’s also possible that secular trends diminished our ability to observe gains in functioning and wellbeing because the program coincided with the exacerbation of the Omicron variant of the COVID-19 pandemic. Data from the National Center for Health Statistics indicate that this time period was associated with increased anxiety and depression. 18 Therefore, the finding that group average wellness measures improved during this time and then decreased afterwards suggests that an appropriately-powered outcomes study measuring the effects of this program on stress reduction and perceived physical and mental health is warranted.
Another limitation to this study was that we did not require participants to complete surveys or even to commit to completing the entire set of surveys when they enrolled. Instead, participants were independently invited to complete a survey at each of the 5 time points. Reminders were sent but no compensation or incentive was offered resulting in variation in the number of people completing the surveys at each time point. The 24-week assessment was particularly low and limits what can be interpreted about the follow up data. We suspect that if this study had been designed as a longitudinal experimental trial in which participants consented at the outset to completing 5 sets of surveys over time, we might have had higher and more consistent response rates. A third limitation was the small sample size. We marketed the program through employee wellness and campus-wide emails and we recruited for the research through direct email to program participants. This approach yielded a sample that was small, mostly women, and mostly classified as staff (vs faculty, health care provider, or administrator), which limits the ability to translate findings to other populations and suggests that a different programmatic strategy may be necessary to attract other types of employees. A fourth limitation is that the program did not require participants to identify and maintain focus on 1 specific goal. While setting goals and checking-in on goals (accountability) are foundational elements of health and wellness coaching in general and in this program, our methodology allowed participants to change their goals throughout the program, making it difficult for them to respond to the survey question regarding goal attainment. The authors recommend future programming emphasizes goal attainment and the survey question be worded to capture if someone has changed their goal during the program.
Conclusions and Implications
We demonstrated that it is feasible to translate the OSW group coaching model to the employee wellness setting, and to conduct the program virtually instead of in-person, as originally planned. Employees were satisfied with the program content and would refer a colleague. Our observational wellness outcomes were promising and suggest future research is warranted to assess short- and long-term impact on health, wellbeing, and behavior. Future programs should consider program modifications and adjunct programming to sustain accountability and maintain attention to participants’ long-term goals. Future developers of programs should consider the fundamental question of whether recruitment should specifically target individuals with existing health conditions or concerns such as burnout -- who have room to change in areas of mental and physical health -- vs people who are already well and join programs to make more subtle improvements in their wellbeing that are less observable. Demonstrating change in symptoms among those with pre-existing conditions might be an important goal to justify ongoing funding for these programs, whereas a more inclusive program might be preferable for employers seeking to promote an organizational culture of wellness that could have longer and more widespread benefits for the organization. Future researchers should strive to identify the optimal design, duration, target population and recruitment strategies of an employee wellbeing program that promotes health for all.
Supplemental Material
Supplemental Material for Employee Group Coaching Program for University and Hospital Employees During COVID-19: A Feasibility Study by Karen Westervelt, Gail L. Rose, Scott Avery, Alisha Celley, Josh Cho, Rory Donoghue, and Brennan Goodrich in Global Advances in Integrative Medicine and Health
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Internal funding.
Supplemental Material: Supplemental material for this article is available online
ORCID iD
Gail L. Rose https://orcid.org/0000-0003-4997-401X
References
- 1.Giattino C, Ortiz-Ospina E, Roser M. Working hours. Our World Data, 2020. Published online. https://ourworldindata.org/working-hours. Accessed May 4, 2022 [Google Scholar]
- 2.Pronk N, Kleinman DV, Goekler SF, Ochiai E, Blakey C, Brewer KH. Promoting health and well-being in healthy people 2030. J Public Health Manag Pract. 2020;27:S242-S248. Publish Ahead of Print. doi: 10.1097/PHH.0000000000001254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lowensteyn I, Berberian V, Belisle P, DaCosta D, Joseph L, Grover SA. The measurable benefits of a workplace wellness program in Canada: results after one year. J Occup Environ Med. 2018;60(3):211-216. doi: 10.1097/JOM.0000000000001240 [DOI] [PubMed] [Google Scholar]
- 4.Reddy KP, Schult TM, Whitehead AM, Bokhour BG. Veterans health administration’s whole health system of care: supporting the health, well-being, and resiliency of employees. Glob Adv Health Med. 2021;10:216495612110226. doi: 10.1177/21649561211022698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Song Z, Baicker K. Effect of a workplace wellness program on employee health and economic outcomes: a randomized clinical trial. JAMA. 2019;321(15):1491. doi: 10.1001/jama.2019.3307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Yoder, Steven V, Purcell J. Workplace Wellness Best Practices Study 2022: Special Report. Wilmington, DE: Returns on Wellbeing Institute; 2022. https://returnsonwellbeing.com/best-practices-study-2022/. Accessed October 18, 2022. [Google Scholar]
- 7.Sforzo GA, Kaye MP, Harenberg S, et al. Compendium of health and wellness coaching: 2019 addendum. Am J Lifestyle Med. 2020;14(2):155-168. doi: 10.1177/1559827619850489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Armstrong C, Wolever RQ, Manning L, et al. Group health coaching: strengths, challenges, and next steps. Glob Adv Health Med. 2013;2(3):95-102. doi: 10.7453/gahmj.2013.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Board of Health and Wellness Coaching . https://nbhwc.org/become-an-approved-training-program/. Accessed October 18, 2022.
- 10.Emmert-Aronson B, Grill KB, Trivedi Z, Markle EA, Chen S. Group medical visits 2.0: the open Source wellness behavioral pharmacy model. J Altern Complement Med. 2019;25(10):1026-1034. doi: 10.1089/acm.2019.0079. [DOI] [PubMed] [Google Scholar]
- 11.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18(7):873-880. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Terwee CB, Peipert JD, Chapman R, et al. Minimal important change (MIC): a conceptual clarification and systematic review of MIC estimates of PROMIS measures. Qual Life Res. 2021;30(10):2729-2754. doi: 10.1007/s11136-021-02925-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beaton DE. Simple as possible? Or too simple? Possible limits to the universality of the one half standard deviation. Med Care. 2003;41(5):593-596. doi: 10.1097/01.MLR.0000064706.35861.B4. [DOI] [PubMed] [Google Scholar]
- 14.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582-592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 15.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 16.Li-Sauerwine S, Rebillot K, Melamed M, Addo N, Lin M. A 2-question summative score correlates with the maslach burnout inventory. West J Emerg Med. 2020;21(3):610-617. doi: 10.5811/westjem.2020.2.45139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goal attainment scale . Shirley ryan abilitylab, 2020. Published July 1, 2020. https://www.sralab.org/rehabilitation-measures/goal-attainment-scale
- 18.National Center for Health Statistics . Anxiety and Depression: Household Pulse Survey. Atlanta, GA, US: Center for Disease Control and Prevention. https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm. Accessed October 18, 2022. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Employee Group Coaching Program for University and Hospital Employees During COVID-19: A Feasibility Study by Karen Westervelt, Gail L. Rose, Scott Avery, Alisha Celley, Josh Cho, Rory Donoghue, and Brennan Goodrich in Global Advances in Integrative Medicine and Health