Abstract
Background:
Lockdown was a unique experience that affected many aspects of life, particularly during the challenge of Ramadan fasting (RF). Studying this can increase understanding of the effects of lifestyle changes on quality of life (QoL) for children with type 1 diabetes (T1D) during RF.
Methods:
A cross-sectional study that assessed the effect of lockdown on lifestyle and QoL on fasting children living with T1D during Ramadan in the Middle East and North Africa region (2020-2021). We compared the child (self) and parent (proxy) reports using PEDQoL v3.0 disease specific questionnaire during lockdown and non-lockdown periods, and assessed correlations with lifestyle changes using regression and gap analyses.
Results:
A total of 998 reports from 499 children with T1D aged 8 to 18 years (study = 276, control = 223), and their parents during RF in lockdown and non-lockdown periods. Fathers were more involved in their children’s care during lockdown (P = .019). Patients had better compliance with treatment (P = .002), a reversed sleep pattern (P = .033), increased food intake (P ⩽ .001), and less exercise (P < .001). Children and parents perceived better QoL during lockdown (P ⩽.001) with no differences between their reports in “Diabetes Symptoms”, “Treatment Adherence,” and “Communication” domains. Self and proxy reports were different in all domains during non-lockdown (P = <.001-.009). In gap analysis, although not statistically significant, the gap was approximated between children’s and parents’ perceptions in all domains during lockdown.
Conclusion:
COVID-19 lockdown had a positive impact on QoL of children living with T1D during RF, possibly due to lifestyle changes and superior psychosocial family dynamics.
Keywords: COVID-19, lifestyle, lockdown, quality of life, Ramadan fasting, type 1 diabetes
Background
Health-related quality of life (HRQoL) represents an essential outcome measure of health in pediatric practice. 1 Improving quality of life (QoL) in chronic diseases has become an important subject for researchers in the recent decades. 2 There is a clear relationship between chronic diseases and reduction of QoL. Pediatric QoL disease specific questionnaires are increasingly used to identify children at-risk and applying early appropriate interventions. 3 Type 1 diabetes mellitus (T1D) is a known disease that negatively affect QoL and is related to multiple factors including severity of hypoglycemia, presence of complications, efficacy of self-management of diabetes, and acceptance of the disease. 4 Undoubtedly, understanding complications of the disease and improving the care delivered to children with T1D would reflect better on quality of life perceived by these children and their parents.4,5 The fasting month of Ramadan especially during COVID-19 was a good opportunity to revise the management of adolescents with type 1 diabetes, with a positive involvement of different family members in the child’s management.
Ramadan fasting (RF) has always posed a particular challenge, affecting QoL, in patients with T1D. Challenges include maintaining glycemic control, and sometimes, fasting for the first time in adolescents. 6 There are multiple shifts in lifestyle that occur during Ramadan including changes to mealtimes and sleep patterns. These have a direct effect on the body physiology that leads to disturbance in several homeostatic and hormonal processes.7,8 For example, shifting sleep timing during Ramadan will lead to changes in body temperature and cortisol level that affect blood glucose levels. 9 Because of that, fasting Muslim children and adolescents living with T1D are at risk of hypoglycemia, hyperglycemia, diabetic ketoacidosis, dehydration, and thrombosis during RF.10,11
During the COVID-19 pandemic, lockdown was an international experience. A complete lockdown was implemented as a preventative measure to stop the spread of the virus. A complete (restrictive) lockdown meant that people could not leave their house at all in the duration of the period of lockdown, that is, 24-hour lockdown. While a partial (less restrictive) lockdown meant that there was a time limit to the lockdown during the day, for example, 14 hours a day that allowed people to go grocery shopping or run errands during the day time. This was a unique experience which affected many aspects of life and subjected children in particular to a new adjustment of their schooling system as well as changes to social interactions and care received in children with chronic diseases. 12 Lockdown highlighted challenges experienced by families of children living with long term illnesses, including psychosocial challenges as well as difficulties with providing care to their young. Furthermore, lockdown resulted in restrictions to physical activities with RF resulting in added changes to sleep pattern and dietary intake. While lockdown resulted in many challenges for families it also held the potential for improving psychosocial bonding between family members - and especially for children living with T1D and their carers.
The aim of this study was to assess the impact of lockdown on lifestyle, diabetes management, and QoL in fasting children living with T1DM during RF in different Muslim countries in the Middle East and North Africa (MENA) regions.
Research Design and Methods
Study design and tools
This is a cross-sectional multicenter study, in which we compared the experience reported by patients fasting Ramadan during the complete lockdown period in 2020 (study group) to patients fasting Ramadan during non-lockdown (or partial lockdown, commonly in daytime hours) in 2021 (control group). The study was designed by a research group of the Arab Society of Pediatric Endocrinology (ASPED). Children living with T1D were enrolled from multiple centers in the MENA region. Participating countries included: Saudi Arabia, Kuwait, Oman, Bahrain, Sudan, Egypt, Palestine, and Jordan.
We assessed the lifestyle changes in Ramadan by asking questions about sleep pattern changes, dietary habits, indoor and outdoor exercise activities including night time special prayers in Ramadan (Tarawih prayer), hours spent on electronic devices and any major differences in lifestyle during current lockdown compared to non-locked time. We also assessed the effect of complete lockdown compared to non or partial lockdown on the perception of QoL and any possible relationship with changes in lifestyle. We used a validated Arabic version of a commonly used disease specific health related quality of life (HRQoL) questionnaire (PEDQoL) version 3.0 designated for children living with diabetes and their parents. 13 The questionnaire contained items clustered in 5 domains of QoL, these were (1) diabetes symptoms (2) treatment barriers, (3) treatment adherence, (4) worry, and (5) communication (Supplemental material). In addition, there were questions about demographics included age, gender, duration of diabetes, type of treatment; (conventional, multiple daily injection (MDI) therapy, or continuous subcutaneous insulin infusion (CSII)), parents’ level of education, socioeconomic status, the primary caregiver who most typically delivers injections, and compliance with treatment.
All families included in the study were approached by the research group by direct interview either in-person (while visiting the outpatient department) or via telephone interview (during the complete lockdown), where the questions were read out to children and the accompanying parent after obtaining verbal consent to participate in the study.
Study population
There were 2 groups of patients. The study group was recruited in 2020 and included participants from Saudi Arabia, Egypt, Oman, Bahrain and Kuwait who fasted Ramadan during the pandemic complete lockdown. The control group included participants from Egypt, Palestine, Jordan and Sudan was recruited in 2021 when the lockdown had been lifted, at least partially in the evening hours until dawn, in some countries.
The centers and institutions that participated in the study were: the Department of Pediatrics, King Abdullah Specialized Children’s Hospital, King Abdulaziz Medical City, National Guard Health Affairs, Riyadh, Saudi Arabia, Ain Shams University Children’s Hospital, Department of Pediatrics, Cairo, Egypt, Dasman Diabetes Institute, Kuwait University, Department of Pediatrics and Farwaniya Hospital, Department of Pediatrics, Kuwait, Sultan Qaboos University, Oman, Defense Force Royal Medical Services, Bahrain, The University of Jordan, Sudan Childhood Diabetes Center, Khartoum, and Makassed Hospital, Jerusalem, Palestine. Each center recruited between 50 and 60 patients for inclusion in either the study or control group (of note, Egypt recruited patients in both the study and control groups). Inclusion criteria were: Children and adolescents of 10 to 18 years of age living with T1D, patients diagnosed with T1D for more than 6 months, and observing fasting for at least 50% of the Ramadan month. Exclusion criteria included additional diagnoses with other autoimmune or chronic diseases, a recent diagnosis (<6 months) of diabetes, recent severe infections, or a learning difficulty or developmental delay which could impair the completion of questionnaires. A contribution of 50 to 60 patients per center from 8 MENA countries resulted in an estimated total sample size of 400 to 480 children living with T1D. Patients enrolled in the study and control groups were matched by age and gender.
Statistical analysis
A sample size of a minimal of 300 patients (Self) and parents (Proxy) reports (ie, 150 children’s responses and 150 parents’ responses to the QoL questionnaires) should be targeted to insure sufficient statistical power of the study (80%) with 95% confidence level of the results and a P-value of <.05 as significant. The statistical power was estimated based on the significant differences in QoL scores (the dependent variable) that ranges from 0 to 100 per item; where 0 = No problems and 100 = always problems. Using the recommended reversed scoring system: 0 QoL = always problems = very poor, 25 = mostly = poor, 50 = frequently = midway, 75 = some = acceptable but not the best, 100 = No reported problems = good QoL. Range of measurement was calculated as the percentage of scores at the extremes of scaling range determined as the maximum (ceiling effect) score and the minimum (floor effect) score to reflect on the best QoL and the cut point for poor QoL. A total score of 25 in each item of the 5 domains in the scoring system was considered to be the cut point for poor QoL.
Descriptive analysis described continuous data. Categorical variables were described using frequency and percentages. Mean and SD were used to describe parametric continuous variables and median (interquartile range for non-parametric continuous data). ANOVA tests were implemented for comparisons between self and proxy reports. For assessment of risk factors that might affect the QoL scores in children, spearman correlations and regression analyses were used. Paired t-test was used for comparisons within groups while independent t-test was used for comparison across groups. Multivariable regression analysis was used to compare quality of life scores across each lifestyle parameter individually. A P < .05 was considered statistically significant.
Results
The sample consisted of a total of 998 self (child) and proxy (parent) reports from 499 children with T1D. Data was collected from a study group (N = 276) and a control group (N = 223). The study and control groups were matched for age, gender, and parents’ level of education (Table1).
Table 1.
Demographics of participants and lifestyle changes in the study (Lockdown) and Control (Non-lockdown) groups.
| Lockdown | Non-lockdown | P-value | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Age (years) | |||||
| 8-12 | 93 | 33.7 | 94 | 42.2 | .052 |
| 13-18 | 183 | 66.3 | 129 | 57.8 | |
| Gender | |||||
| Male | 129 | 46.7 | 110 | 49.3 | .565 |
| Female | 147 | 53.3 | 113 | 50.7 | |
| Parents’ level of education | |||||
| Up to high school | 109 | 40.5 | 80 | 35.9 | .292 |
| University | 160 | 59.5 | 143 | 64.1 | |
| Accompanying parent | |||||
| Mother | 182 | 65.9 | 154 | 69.1 | <.001 |
| Father | 68 | 24.6 | 21 | 9.4 | |
| Both | 26 | 9.4 | 41 | 18.4 | |
| Other | 0 | 0.0 | 7 | 3.1 | |
| Main care-provider | |||||
| Child | 69 | 26.4 | 69 | 30.9 | .019 |
| Mother | 106 | 40.6 | 107 | 48.0 | |
| Father | 14 | 5.4 | 4 | 1.8 | |
| Other | 72 | 27.6 | 43 | 19.3 | |
| Total dose of insulin a | |||||
| Decreased | 91 | 57.2 | 126 | 57.5 | <.001 |
| Same | 34 | 21.4 | 75 | 34.2 | |
| Increased | 34 | 21.4 | 18 | 8.2 | |
| Injection delivered by a | |||||
| Child | 146 | 55.9 | 110 | 49.3 | <.001 |
| Mother | 28 | 10.7 | 80 | 35.9 | |
| Father and others | 87 | 33.3 | 33 | 14.8 | |
| Adherence to treatment a | |||||
| Poor | 40 | 14.9 | 56 | 25.1 | .004 |
| Average | 74 | 27.6 | 69 | 30.9 | |
| Good | 154 | 57.5 | 98 | 43.9 | |
| Is fasting Ramadan challenging? | |||||
| Yes | 132 | 48.7 | 173 | 85.2 | <.001 |
| No | 139 | 51.3 | 30 | 14.8 | |
| Sleep pattern | |||||
| Reverse sleep pattern | 238 | 86.5 | 177 | 79.4 | .033 |
| Normal sleep pattern | 37 | 13.5 | 46 | 20.6 | |
| Food contents and portion | |||||
| Increased portion = Carbs 90-100 g/meal | 147 | 58.8 | 147 | 66.5 | <.001 |
| Same, Carbs 60-75 g/meal | 64 | 25.6 | 72 | 32.6 | |
| Decreased portion, Carbs <60 g | 39 | 15.6 | 2 | 0.9 | |
| Number and timing of meals | |||||
| (Mean, SD) | 2.8 (0.4) | 2.3 (0.8) | <.001 | ||
| Hours spent on electronic devices | |||||
| (Mean, SD) | 6.1 (3.6) | 3.9 (2.2) | <.001 | ||
| Exercise | |||||
| No | 110 | 56.7 | 97 | 43.5 | <.001 |
| Tarawih prayer (mild intensity) | 8 | 4.1 | 44 | 19.7 | |
| Medium intensity | 35 | 18.0 | 30 | 13.5 | |
| High intensity | 41 | 21.1 | 52 | 23.3 | |
| Compliance with treatment | |||||
| Poor | 31 | 11.6 | 53 | 23.9 | .002 |
| Average | 76 | 28.4 | 56 | 25.2 | |
| Good | 161 | 60.1 | 113 | 50.9 | |
| Partial | 1 | 0.4 | 40 | 17.9 | |
Not reported by all patients.
Demographics
Children’s ages ranged between 8 and 18 years (Table 1). The majority of participants were females (study 53.3% vs control 50.7%). Accommodation type was included in the study. Open residential areas meant that children did not have any access to workout facility, whereas living in compounds gave some room to move around. The number of participants who live in open residential areas was comparable between study and control group, however, there were more patients living in compounds in the study group. There was a difference in the socioeconomic status between the groups, (P < .001) as 25.9% of study group reported high socioeconomic status as compared 8.5% in the control group.
Insulin regimen
As for insulin regimen, 92.8% of the control group reported MDI use as compared to the study group (81.8%; Table 1). Overall, children living with T1DM were more compliant with treatment during the lockdown period. Interestingly, greater adherence to insulin therapy was observed in the lockdown group (P-value .004). Dose of insulin is usually adjusted during Ramadan to accommodate the change in routine that occurs naturally with fasting and there was an increase in total daily dose of insulin in the lockdown group as compared to the control group (P < .001). There was also greater involvement of family members in insulin dose delivery in the lockdown group as compared to the control group. Fathers’ involvement was noted by assessing who was accompanying the child to their check-up or virtual follow up that was greater during lockdown (24.6%) as compared to non-lockdown (9.4%); P < .001). Also, fathers and other family members, but not their mothers, were the main care providers to these children in 33% during lockdown compared to 21% during non-lockdown period (P < .019).
Lifestyle changes
There were significant differences in lifestyle parameters during Ramadan between the lockdown and the non-lockdown groups (Table 1). They included in the lockdown group (as compared to the control group): worse reversed sleep pattern (P = .033) and an increased number of meals with lower carbohydrate consumption (P ⩽ .001). Better compliance with treatment was reported by the lockdown group (P = .002) as 60.1% of those in the lockdown group reported good compliance during lockdown as opposed to 50.9% in the non-lockdown group. A greater proportion of children in the lockdown group reported a significant lack of exercise (56.7%) as compared to those in the non-lockdown group (43.5%). Even Taraweh prayers were performed less in the study group as compared to the control group (P ⩽ .001). There was an increase in hours spent using electronic devices in the lockdown group (6.1 hours ± 3.6 SD) as compared to the non-lockdown group (3.9 hours ± 2.2 SD; P < .001). The number of meals was greater in the lockdown versus the control group (P < .001). The challenge of fasting Ramadan was considered to be lower in the lockdown group as compared to the control group (48.7% of patients reported RF to be challenging in the lockdown group as compared to 85.2% of patients during non-lockdown, P < .001).
QoL: Self versus proxy reports
Children and parents in the lockdown group perceived an overall better QoL in all domains compared to the control group (P ⩽ .001) (Table 2). There was no difference between child and parent perception of QoL during lockdown in “Diabetes Symptoms,” “Treatment Adherence,” or “Communication” domains. However, there was significant difference in their perception of QoL in all other domains during non-lockdown and in the “Treatment barriers” and “Worries” domains during lockdown (P values range from <.001 to .009).
Table 2.
Self and Proxy quality of life reports during lockdown and non-lockdown periods.
| Self-report | Proxy report | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lockdown | Non-lockdown | P-value | Lockdown | Non-lockdown | P-value | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Diabetes symptoms | 728.2 | 176.5 | 598.5 | 172.5 | <.001 | 727.8 | 193.8 | 569.0 | 159.0 | <.001 |
| Treatment barriers | 264.9 | 98.2 | 204.2 | 80.6 | <.001 | 248.4 | 100.0 | 172.7 | 62.8 | <.001 |
| Treatment adherence | 469.0 | 128.7 | 383.4 | 117.6 | <.001 | 450.8 | 133.3 | 390.5 | 112.5 | <.001 |
| Worry | 189.0 | 83.1 | 138.2 | 71.1 | <.001 | 172.5 | 93.3 | 95.4 | 60.0 | <.001 |
| Communication | 215.2 | 88.8 | 166.8 | 72.8 | <.001 | 216.6 | 85.5 | 179.3 | 67.2 | <.001 |
| Total aggregate | 1862.0 | 388.0 | 1491.0 | 366.0 | <.001 | 1815.0 | 403.0 | 1407.0 | 302.0 | <.001 |
Despite the significant variations in variables of lifestyle in the study and control groups, none of these variables had a significant individual effect when regressed against QoL scoring in self and proxy reports.
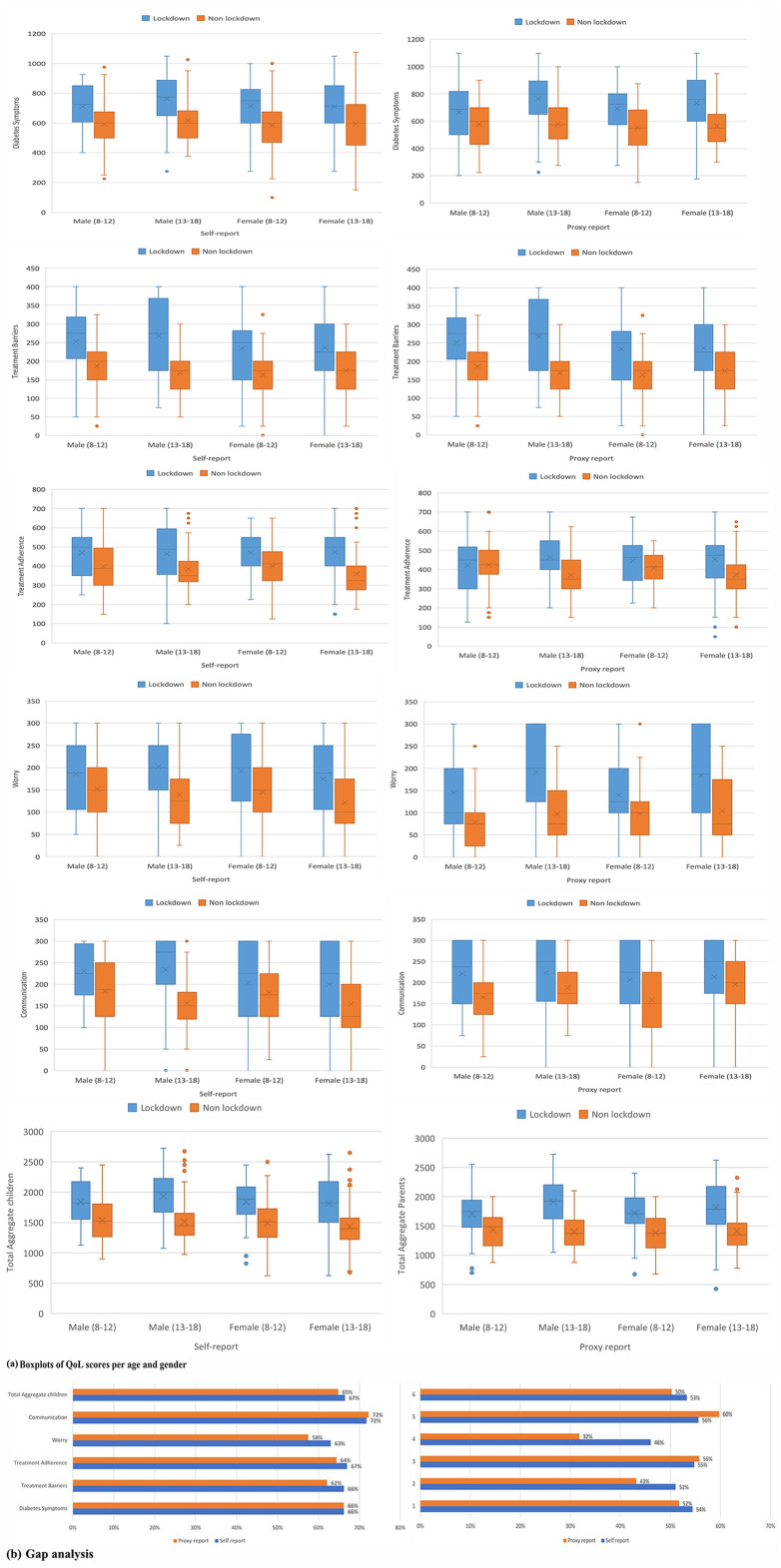
Lockdown versus non-lockdown
Using regression analysis, and focusing on self-report data, we found that group status (lockdown vs non-lockdown) predicted “Diabetes symptoms” and “Treatment adherence” domains as well as in total aggregate scores (Figure 1, Tables 2 and 3). The same was found for parent-report data (Table 3). Group status predicted QoL (aggregate score and all domains’ scores) in self and proxy reports—with a better QoL reported for the lockdown group. For the “worry” domain, and when focusing on parent-report, this effect was particularly pronounced in the older age group (13-18 years) in both genders (Figure 1). The male older age group (13-18 years) scored much better in the “Treatment barriers” domain during lockdown compared to other age group (Figure 1).
Figure 1.
(a) The differences in Qol scores per age and gender (b) gap analysis, between self and proxy reports during lockdown and non-lockdown periods.
Table 3.
Regression analyses of the overall changes in lifestyle against quality-of-life (QoL) scores in Self and Proxy reports.
| Parameter | Self report | Proxy report | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | P-value | 95% CI for B | B | P-value | 95% CI for B | |||||
| Upper | Lower | Upper | Lower | |||||||
| Total aggregate | Intercept | 1217.9 | <.001 | 714.5 | 1721.4 | Intercept | 864.9 | .001 | 367.4 | 1362.5 |
| Lockdown | 316.8 | <.001 | 213.1 | 420.5 | Lockdown | 279.3 | <.001 | 176.9 | 381.8 | |
| Non-lockdown (ref.) | 0.0 | . | . | . | Non-lockdown (ref.) | 0.0 | . | . | . | |
| Diabetes symptoms | Intercept | 634.5 | <.001 | 388.8 | 880.1 | Intercept | 429.7 | .001 | 181.2 | 678.2 |
| Lockdown | 108.4 | <.001 | 57.8 | 158.9 | Lockdown | 135.8 | <.001 | 84.6 | 187.0 | |
| Non-lockdown (ref.) | 0.0 | . | . | . | Non-lockdown (ref.) | 0.0 | . | . | . | |
| Treatment Barriers | Intercept | 95.2 | .142 | −32.0 | 222.3 | Intercept | 44.7 | .437 | −68.4 | 157.7 |
| Lockdown | 33.2 | .013 | 7.0 | 59.4 | Lockdown | 27.9 | .019 | 4.6 | 51.2 | |
| Non-lockdown (ref.) | 0.0 | . | . | . | Non-lockdown (ref.) | 0.0 | . | . | . | |
| Treatment adherence | Intercept | 359.8 | <.001 | 185.4 | 534.2 | Intercept | 285.6 | .002 | 109.4 | 461.8 |
| Lockdown | 101.5 | <.001 | 65.6 | 137.4 | Lockdown | 80.7 | <.001 | 44.4 | 117.0 | |
| Non-lockdown (ref.) | 0.0 | . | . | . | Non-lockdown (ref.) | 0.0 | . | . | . | |
| Worry | Intercept | 80.1 | .139 | −26.3 | 186.5 | Intercept | 14.7 | .762 | −80.4 | 109.8 |
| Lockdown | 18.6 | .096 | −3.3 | 40.5 | Lockdown | 5.7 | .569 | −13.9 | 25.3 | |
| Non-lockdown (ref.) | 0.0 | . | . | . | Non-lockdown (ref.) | 0.0 | . | . | . | |
| Communication | Intercept | 48.3 | .396 | −63.6 | 160.3 | Intercept | 92.7 | .075 | −9.5 | 194.9 |
| Lockdown | 55.2 | <.001 | 32.1 | 78.2 | Lockdown | 29.8 | .006 | 8.7 | 50.8 | |
| Non-lockdown (ref.) | 0 | . | . | . | Non-lockdown (ref.) | 0.0 | . | . | . | |
Using gap analysis to compare the variations in self and proxy reports in different domains, there was an approximation in the gap between children and parents’ perceptions in all domains during lockdown. However, that was not statistically significant (Figure 1).
Discussion
Risk of complications in children with T1D includes hypoglycemia and hyperglycemia. These complications are closely related to the changes that normally occurs in lifestyle during Ramadan including diet, exercise, and insulin requirement. COVID-19 lockdown was an additional burden on families with children and adolescents living with T1D. Having T1D is a risk factor for adverse outcomes during the COVID-19 lockdown. 14
The study group had faced a combination of 3 challenges, having type 1 diabetes, fasting Ramadan as well as being subjected to lockdown. Hence, it could be postulated that additional changes during the lockdown to lifestyle could pose further risks that can affect the outcome of these patient’s QoL.
The lockdown resulted in people staying at home and spending unprecedented amounts of time with their children. This global experience was novel and no similar periods have been studied to this extent. Undoubtedly, lockdown impacted the mental health on a societal level. 15 Children and adolescents are the most sensitive age groups to be affected by drastic changes in lifestyle. 15 Given that fasting Ramadan had always posed a challenge on children with T1D, we observed experiences while fasting during the month of Ramadan. Specifically, we compared lifestyle, QoL, and diabetes management (including diet, exercise, and insulin dosage) during RF in children and adolescents living with T1D who reported symptoms during complete lockdown period to those who reported symptoms during incomplete/partial lockdown (essentially referred to as non-lockdown) period.
Exercise
In general, outdoor activities improve the cognitive, physical, social, and emotional health of children. 16 Decreased physical activity is one of the lifestyle changes that has been observed during Ramadan among Muslim populations. 17 A recent paper have even discussed the fitness for work of an adult Muslim who fasts during Ramadan and adjustment of working hours to meet these needs. 18 There is a debate about the psychological effect of outdoor activities for type 1 DM patients, though it improves the general wellbeing and in some studies was proposed to have a therapeutic effect. The COVID-19 outbreak led to lockdown and limitations of this type of activities. 19
A central issue associated with spending prolonged hours a day at home is the lack of physical exercise which, was demonstrated in our control group. Lockdown, surprisingly did not affect exercise negatively. Although, it was thought that indoor activities versus outdoors would have negatively impact children’s QoL during lockdown time. Nevertheless, that was not the case in our cohort. Despite that there were more participants living in enclosed residential areas in the study group, there was no difference in outdoor activities reported between the groups. We propose that lack of exercise is an issue regardless of restrictions imposed by the compulsory lockdown. This is supported by the fact that subjects who lived in compounds, where there are facilities to use during lockdown, did not have a significant improvement in exercise practices.
Muslims perform prayers 5 times daily all year round and during Ramadan, additional prayers take place (called Taraweeh). These differ from regular daily prayers by being longer in duration and timed shortly after breaking the fast. Therefore, this activity is considered as an exercise of moderate intensity. We included Taraweeh as part of exercise. The prayers are usually preformed in groups at mosques. Understandably, therefore, Taraweeh prayers were less performed during the lockdown as compared to the control group in our cohort (<.001).
Screen time
Being confined to one space increased screen time. That in itself can contribute to psychological issues. 20 Studies have shown an increase in level of anxiety and depression with extended screen time and excessive use of internet and social media platforms. 21 As expected, screen time had inevitably increased during lockdown. However, the increase in hours spent on devices also included time spent studying from home which, theoretically, could have resulted in less psychosocial consequences as compared to the leisure use of devices.
Positive family dynamics
Some studies have found increased tension in households during lockdown due to the stress of quarantine. 22 However, we found improvement in family dynamics in the lockdown group as compared to the control group. This was evidenced by increased involvement in the care of patients during the lockdown. Comparing our 2 groups, we noted more involvement of fathers and other family members during the lockdown in the delivery of insulin injections. Many factors could have contributed to this improvement. First, we propose that increased time spent at home improved the communication and strengthened the ties between family members. Communication with parents increased and parents were perhaps more attentive to their children’s needs. Close supervision of the management of T1D by parents, increased family interactions and support from both parents and other members of the family to children living with T1D could have improved both children and parents’ perception of QoL during this new challenging experience of fasting of youngsters living with T1D.
In our study, we noticed more father involvement in patient’s care during the lockdown, as opposed to solely mothers being the primary care-providers in the control group. This change is favorable and would likely reduce the parenteral stress and burden of taking care of a child with a chronic condition such as T1D. 23 The positive effect of family involvement has been highlighted in the literature previously, and many studies have focused on improving health outcomes in children and adolescents living with type 1 diabetes via using family based interventions. 24
Effect on insulin
In our study, there was greater adherence to insulin therapy during the lockdown period and an increase in total daily dose of insulin in the lockdown group. This was consistent with an Italian study that found a significant increase in insulin boluses during COVID lockdown compared to non-lockdown in pre-school and school aged children. They proposed that during lockdown, more parental involvement led to that enhancement in metabolic effect. 25
Effect on quality of life
Superior QoL during RF was reported during the pandemic lockdown as compared to the control group. Improved dietary habits, better treatment compliance and adherence which, we attributed to more involvement of family members in supporting children and adolescents living with T1D through the stressful experience of RF. These changes that lockdown has brought on lifestyle, besides improvement in family interactions and greater support for children with T1D, have improved the QoL for these children and adolescents.
Despite the significant variations in some variables of lifestyle between the 2 groups, when QoL scores were regressed against these individual parameters, none of them had a significant impact on the QoL scoring in both children and parents’ reports. This indicates, that the significant overall and individual domains effects had resulted from them collectively in addition to the expected, but difficult to accurately measure, positive effects of family dynamics and social interactions that improved communication, adherence to treatment and reduced concerns about symptoms and acute and long-term complications.
The overall and individual domains’ QoL scores were consistently better during lockdown. That was more apparent in the older age group (13-18 years) in both genders and more specifically in the “Worry” domain in the proxy report. Probably parents may have felt that their children were less worried during lockdown as there were no outdoor activities and fewer commitments during fasting time in the lockdown. The male older age group (13-18 years) scored much better in the “Treatment barriers” domain during lockdown compared to other age groups probably with the help and support from other family members. This is the main group who typically shows the risk-taking behavior of missing insulin doses, though evidence to support this is sparse. 1 Also, the younger age (10-12 years) group is speculated to be still well-attached to parents and follows their guidance and instructions on management better than the older age (13-18 years) group during a new experience of RF. Although, there is no studies found in the literature to support this claim. Further research is needed to investigate why these trends may have been observed.
The lockdown imposed immense restrictions on social interactions. Schools closed down and contact with classmates, friends, and extended family varied in nature and was limited. That might have been isolating and was associated with depression and increased loneliness. 20 However, some children and adolescents living with T1D struggle with shame around peers with delivering injections. 26 That was no longer apparent in our study group and the worry domain was reduced as compared to the control group. Being close to parents and other family members during the lockdown period could have reduced the worries about potential hypoglycemic episodes during fasting hours and at the time of unattended outdoor activities that are popular among adolescents in Ramadan’s night-time.
Interestingly, there was a smaller gap between adolescents’ and parents’ perceptions of the QoL in children with T1D, in the lockdown group as compared to the non-lockdown group (although this difference was not statistically significant). One reason for this could be the alignment of experiences between children and their parents during lockdown. The gap between self-report and parent-report was greater in the older adolescent age group (13-18 years of age), as compared to the younger age-group. This could reflect different thinking styles during adolescents as compared to other developmental stages. 27 The neuronal sensitivity to motivational factors develops during adolescence, hence; teens compared to adults may possess novelty-seeking and risk-taking behaviors.28,29 Moreover, adolescents do not prefer to share their worries if that reflects a limitation in confidence or lacking experience. 30 Their decision making could also by influenced by peers or other emotions and social contexts.29,31This distinct behavior may frequently result in disagreement with parents in management of their diabetes. 30 Hence, a sustainable gap had remained between self and proxy reports of QoL in the 2 periods of our study, possibly due to different perspectives of parents and these adolescents, especially the older age group.
Study limitations
Our data reflected on a cohort from various MENA countries with multiple variations in socioeconomic status, dietary habits, and lockdown policies. Children and adolescents included in the study had different socioeconomic backgrounds. Some had the privilege to live in compounds where they had access to exercise facilities and experienced more freedom in mobility during the lockdown. Participants had different insulin regimens based on their income, with MDI mostly used with lower socioeconomic status. As we appreciate these differences and the effect they might have had, there was no way to adjust for it. Despite being from different groups of countries, most share similar cultures and rituals during Ramadan Fasting. However, there are some minor variations in food and eating habits/traditions between different countries in MENA region due to cultural differences, which was difficult to adjust for in our study. Due to variations in the extended lockdown time policy, we were unable to recruit the same patients during the non-lockdown/partial lockdown period.
Another challenge we faced during data collection was that the number of children who fasted for the first time was higher in the control group, hence; an increase in the percentage of incomplete RF (50%) in that group. It was also difficult to conclude whether the incomplete RF was because of facing more challenges or due to a decreased enthusiasm related to a belief of not reaching the appropriate age to complete RF. Although the patients were well matched in the 2 groups and changes in lifestyle between the groups were adjusted for, there could be some hidden unmeasured additional psychosocial factors related to parents/adolescents’ relationship in the 2 groups.
Furthermore, parental level of education, that was not assessed in our study, may be thought of as an important contributing factor that could affect the outcome of QoL in these children. However, because of variable participation from different family members in patients’ management during lockdown, this variable had possibly limited effect in that situation.
Conclusion
COVID-19 lockdown has restricted lifestyles of most people affected. However, the change in lifestyle experienced also provided great opportunities. By comparing patient groups recruited during and after the lockdown, we found that the lockdown group reported superior family dynamics, which were associated with a superior QoL in fasting Muslim children and adolescents living with T1D. The observations that were found in this study gave a positive impact of closer family interactions during the lockdown on the quality of life of children with type 1 diabetes. This could be implemented by diabetes treating teams via family-targeted programs to enhance the management of these children especially if implemented during the potentially stressful experience of Ramadan fasting. This holds true regardless of the challenges of COVID and associated lockdowns.
Supplemental Material
Supplemental material, sj-doc-1-end-10.1177_11795514231203907 for Lessons Learned From COVID-19 Lockdown: An ASPED/MENA Study on Lifestyle Changes and Quality of Life During Ramadan Fasting in Children and Adolescents Living With Type 1 Diabetes by Amir Babiker, Nancy Samir Elbarbary, Bothainah Alaqeel, Khalid Al Noaim, Saif Al Yaarubi, Dalia Al-Abdulrazzaq, Hessa Al-Kandari, Haya Alkhayyat, Rasha Odeh, Omer Babiker, Abdulsalam Abu-Libdeh, Amal Aljohani, Noof Al Abdul Salam, Fatima Al-Juailla, Emad Masuadi, Asma Deeb, Jill Weissberg-Benchell, Alice M. Gregory, Mohamed Hassanein and Ibrahim Al Alwan in Clinical Medicine Insights: Endocrinology and Diabetes
Supplemental material, sj-doc-2-end-10.1177_11795514231203907 for Lessons Learned From COVID-19 Lockdown: An ASPED/MENA Study on Lifestyle Changes and Quality of Life During Ramadan Fasting in Children and Adolescents Living With Type 1 Diabetes by Amir Babiker, Nancy Samir Elbarbary, Bothainah Alaqeel, Khalid Al Noaim, Saif Al Yaarubi, Dalia Al-Abdulrazzaq, Hessa Al-Kandari, Haya Alkhayyat, Rasha Odeh, Omer Babiker, Abdulsalam Abu-Libdeh, Amal Aljohani, Noof Al Abdul Salam, Fatima Al-Juailla, Emad Masuadi, Asma Deeb, Jill Weissberg-Benchell, Alice M. Gregory, Mohamed Hassanein and Ibrahim Al Alwan in Clinical Medicine Insights: Endocrinology and Diabetes
Supplemental material, sj-doc-3-end-10.1177_11795514231203907 for Lessons Learned From COVID-19 Lockdown: An ASPED/MENA Study on Lifestyle Changes and Quality of Life During Ramadan Fasting in Children and Adolescents Living With Type 1 Diabetes by Amir Babiker, Nancy Samir Elbarbary, Bothainah Alaqeel, Khalid Al Noaim, Saif Al Yaarubi, Dalia Al-Abdulrazzaq, Hessa Al-Kandari, Haya Alkhayyat, Rasha Odeh, Omer Babiker, Abdulsalam Abu-Libdeh, Amal Aljohani, Noof Al Abdul Salam, Fatima Al-Juailla, Emad Masuadi, Asma Deeb, Jill Weissberg-Benchell, Alice M. Gregory, Mohamed Hassanein and Ibrahim Al Alwan in Clinical Medicine Insights: Endocrinology and Diabetes
Supplemental material, sj-docx-4-end-10.1177_11795514231203907 for Lessons Learned From COVID-19 Lockdown: An ASPED/MENA Study on Lifestyle Changes and Quality of Life During Ramadan Fasting in Children and Adolescents Living With Type 1 Diabetes by Amir Babiker, Nancy Samir Elbarbary, Bothainah Alaqeel, Khalid Al Noaim, Saif Al Yaarubi, Dalia Al-Abdulrazzaq, Hessa Al-Kandari, Haya Alkhayyat, Rasha Odeh, Omer Babiker, Abdulsalam Abu-Libdeh, Amal Aljohani, Noof Al Abdul Salam, Fatima Al-Juailla, Emad Masuadi, Asma Deeb, Jill Weissberg-Benchell, Alice M. Gregory, Mohamed Hassanein and Ibrahim Al Alwan in Clinical Medicine Insights: Endocrinology and Diabetes
Acknowledgments
We wish to express our sincere appreciation to all the patients and their families for their participation and cooperation during the study period. From Kuwait, we would like to acknowledge the following: Dasman Diabetes Institute, Kuwait University, Dr. Doa Khalifa. Research assistants: Sarah Qabazard, Taibah Al-Qaisi, Fatima Al-Juailla, and Fouzeyah Othman. This paper’s guarantor is Dr. Amir Babiker.
Footnotes
ORCID iDs: Amir Babiker  https://orcid.org/0000-0001-7538-852X
https://orcid.org/0000-0001-7538-852X
Saif Al Yaarubi  https://orcid.org/0000-0003-0228-1304
https://orcid.org/0000-0003-0228-1304
Omer Babiker  https://orcid.org/0000-0002-8782-3813
https://orcid.org/0000-0002-8782-3813
Supplemental Material: Supplemental material for this article is available online.
Declarations
Ethics Approval and Consent to Participate: The Institutional Review Board (IRB) of King Abdullah International Medical Research Center (KAIMRC), Riyadh, Saudi Arabia had granted an approval of this (RC20/278/R) multicenter study (IRB approval number: H-01-R-005), followed by subsequent approvals by other ethical committees in the participating centers. Informed consent, as well as assent for all children aged 10 to 18 years, for participation in the study and publication of medical details and responses to questionnaires was also obtained from the parents of these patients.
Consent for publication: Not applicable.
Author Contributions: Amir Babiker: Conceptualization; Formal analysis; Methodology; Supervision; Writing—original draft; Writing—review & editing. Nancy Samir Elbarbary: Supervision; Data curation; Writing—original draft, Writing—review & editing. Bothainah Alaqeel: Data curation; Formal analysis; Methodology; Writing—original draft; Writing—review & editing. Khalid Al Noaim: Formal analysis; Data curation, Writing—review & editing. Saif Al Yaarubi: Investigation; Data curation; Writing—review & editing. Dalia Al-Abdulrazzaq: Investigation; Data curation; Writing—review & editing. Hessa Al-Kandari: Data curation; Writing—review & editing. Haya Alkhayyat: Investigation; Data curation; Writing—review & editing. Rasha Odeh: Investigation. Data curation; Writing—review & editing. Omer Babiker: Data curation; Investigation; Writing—review & editing. Abdulsalam Abu-Libdeh: Data curation; Investigation; Writing—review & editing. Amal Aljohani: Data curation; Writing—review & editing. Noof Al Abdul Salam: Data curation; Writing—review & editing. Fatima Al-Juailla: Data curation; Writing—review & editing. Emad Masuadi: Formal analysis; Methodology; Software; Writing—review & editing. Asma Deeb: Supervision; Writing—review & editing. Jill Weissberg-Benchell: Writing—review & editing. Alice M. Gregory: Writing—review & editing. Mohamed Hassanein: Writing—review & editing. Ibrahim Al Alwan: Conceptualization; Supervision; Writing—review & editing.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of Data and Materials: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1. Babiker A, Al Aqeel B, Marie S, et al. Quality of life and glycemic control in Saudi children with Type 1 diabetes at different developmental age groups. Clin Med Insights Endocrinol Diabetes. 2021. February 11;14;1179551421990678. doi: 10.1177/1179551421990678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. De Wit M, Delemarre-van de, Waal HA, Bokma JA, et al. Monitoring and discussing health-related quality of life in adolescents with type 1 diabetes improve psychosocial well-being: a randomized controlled trial. Diabetes Care. 2008;31:1521-1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Abdul-Rasoul M, AlOtaibi F, Abdulla A, et al. Quality of life of children and adolescents with type 1 diabetes in Kuwait. Med Princ Pract. 2013;22:379-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hagger V, Hendrieckx C, Sturt J, et al. Diabetes distress among adolescents with type 1 diabetes: a systematic review. Curr Diab Rep. 2016;16:1-14. [DOI] [PubMed] [Google Scholar]
- 5. Saoji N, Palta M, Young HN, et al. The relationship of type 1 diabetes self-management barriers to child and parent quality of life: a US cross-sectional study. Diabet Med. 2018;35:1523-1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. AlAlwan I, Al Banyan A. Effects of Ramadan fasting on children with type 1 diabetes. Int J Diabetes Mellit. 2010;2:127-129. [Google Scholar]
- 7. Beshyah S, Habeb A, Deeb A, Elbarbary N. Ramadan fasting and diabetes in adolescents and children: a narrative review. Ibnosina J Med Biomed Sci. 2019;11:47-56. [Google Scholar]
- 8. Fredheim S, Foli-Andersen P, Laerkholm G, et al. Adrenaline and cortisol levels are lower during nighttime than daytime hypoglycaemia in children with type 1 diabetes. Acta Paediatr. 2018;107:1759-1765. [DOI] [PubMed] [Google Scholar]
- 9. Reilly T, Waterhouse J. Altered sleep–wake cycles and food intake: the Ramadan model. Physiol Behav. 2007;90:219-228. [DOI] [PubMed] [Google Scholar]
- 10. Kaplan W, Afandi B. Blood glucose fluctuation during Ramadan fasting in adolescents with type 1 diabetes: findings of continuous glucose monitoring. Diabetes Care. 2015;38:e162-e163. [DOI] [PubMed] [Google Scholar]
- 11. Beshyah SA, Chowdhury TA, Ghouri N, Lakhdar AA. Risk of diabetic ketoacidosis during Ramadan fasting: a critical reappraisal. Diabetes Res Clin Pract. 2019;151:290-298. [DOI] [PubMed] [Google Scholar]
- 12. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912-920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Varni JW, Curtis BH, Abetz LN, et al. Content validity of the PedsQL™ 3.2 Diabetes Module in newly diagnosed patients with type 1 diabetes mellitus ages 8–45. Qual Life Res. 2013;22:2169-2181. [DOI] [PubMed] [Google Scholar]
- 14. Hassanein M, Alamoudi RM, Kallash M-A, et al. Ramadan fasting in people with type 1 diabetes during COVID-19 pandemic: the DaR Global survey. Diabetes Res Clin Pract. 2021;172:108626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Panchal U, Salazar de, Pablo G, Franco M, et al. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry. 2023;32:1151–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chaddock L, Voss MW, Kramer AF. Physical activity and fitness effects on cognition and brain health in children and older adults. Kinesiol Rev. 2012;1:37-45. [Google Scholar]
- 17. DeLang MD, Salamh PA, Chtourou H, et al. The effects of Ramadan intermittent fasting on football players and implications for domestic football Leagues over the next decade: a systematic review. Sports Med. 2022;52:585–600. [DOI] [PubMed] [Google Scholar]
- 18. Deen M, Moothadeth A, Waqar S, et al. Fasting during Ramadan and fitness for work implications. Occup Med. 2022;72:154-156. [DOI] [PubMed] [Google Scholar]
- 19. Chen P, Mao L, Nassis GP, et al. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J Sport Heal Sci. 2020;9:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Singh S, Roy D, Sinha K, et al. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. 2020;293:113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Woods HC, Scott H. # Sleepyteens: Social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem. J Adolesc. 2016;51:41-49. [DOI] [PubMed] [Google Scholar]
- 22. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180:817-818. [DOI] [PubMed] [Google Scholar]
- 23. Aldubayee M, Mohamud S, Almadani KA, et al. Parental levels of stress managing a child diagnosed with type 1 diabetes in Riyadh: a cross sectional study. BMC Psychiatry. 2020;20:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Feldman MA, Anderson LM, Shapiro JB, et al. Family-based interventions targeting improvements in health and family outcomes of children and adolescents with type 1 diabetes: a systematic review. Curr Diab Rep. 2018;18:15. [DOI] [PubMed] [Google Scholar]
- 25. Schiaffini R, Barbetti F, Rapini N, et al. School and pre-school children with type 1 diabetes during Covid-19 quarantine: the synergic effect of parental care and technology. Diabetes Res Clin Pract. 2020;166:108302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lu Y, Pyatak EA, Peters AL, et al. Patient perspectives on peer mentoring: type 1 diabetes management in adolescents and young adults. Diabetes Educ. 2015;41:59-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Van Duijvenvoorde ACK, van Hoorn J, Blankenstein NE. Risks and rewards in adolescent decision-making. Curr Opin Psychol. 2022;48:101457. [DOI] [PubMed] [Google Scholar]
- 28. Adriani W, Chiarotti F, Laviola G. Elevated novelty seeking and peculiar d-amphetamine sensitization in periadolescent mice compared with adult mice. Behav Neurosci. 1998;112:1152. [DOI] [PubMed] [Google Scholar]
- 29. Sturman DA, Mandell DR, Moghaddam B. Adolescents exhibit behavioral differences from adults during instrumental learning and extinction. Behav Neurosci. 2010;124:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schilling LS, Knafl KA, Grey M. Changing patterns of self-management in youth with type I diabetes. J Pediatr Nurs. 2006;21:412-424. [DOI] [PubMed] [Google Scholar]
- 31. Blakemore S-J, Robbins TW. Decision-making in the adolescent brain. Nat Neurosci. 2012;15:1184-1191. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-doc-1-end-10.1177_11795514231203907 for Lessons Learned From COVID-19 Lockdown: An ASPED/MENA Study on Lifestyle Changes and Quality of Life During Ramadan Fasting in Children and Adolescents Living With Type 1 Diabetes by Amir Babiker, Nancy Samir Elbarbary, Bothainah Alaqeel, Khalid Al Noaim, Saif Al Yaarubi, Dalia Al-Abdulrazzaq, Hessa Al-Kandari, Haya Alkhayyat, Rasha Odeh, Omer Babiker, Abdulsalam Abu-Libdeh, Amal Aljohani, Noof Al Abdul Salam, Fatima Al-Juailla, Emad Masuadi, Asma Deeb, Jill Weissberg-Benchell, Alice M. Gregory, Mohamed Hassanein and Ibrahim Al Alwan in Clinical Medicine Insights: Endocrinology and Diabetes
Supplemental material, sj-doc-2-end-10.1177_11795514231203907 for Lessons Learned From COVID-19 Lockdown: An ASPED/MENA Study on Lifestyle Changes and Quality of Life During Ramadan Fasting in Children and Adolescents Living With Type 1 Diabetes by Amir Babiker, Nancy Samir Elbarbary, Bothainah Alaqeel, Khalid Al Noaim, Saif Al Yaarubi, Dalia Al-Abdulrazzaq, Hessa Al-Kandari, Haya Alkhayyat, Rasha Odeh, Omer Babiker, Abdulsalam Abu-Libdeh, Amal Aljohani, Noof Al Abdul Salam, Fatima Al-Juailla, Emad Masuadi, Asma Deeb, Jill Weissberg-Benchell, Alice M. Gregory, Mohamed Hassanein and Ibrahim Al Alwan in Clinical Medicine Insights: Endocrinology and Diabetes
Supplemental material, sj-doc-3-end-10.1177_11795514231203907 for Lessons Learned From COVID-19 Lockdown: An ASPED/MENA Study on Lifestyle Changes and Quality of Life During Ramadan Fasting in Children and Adolescents Living With Type 1 Diabetes by Amir Babiker, Nancy Samir Elbarbary, Bothainah Alaqeel, Khalid Al Noaim, Saif Al Yaarubi, Dalia Al-Abdulrazzaq, Hessa Al-Kandari, Haya Alkhayyat, Rasha Odeh, Omer Babiker, Abdulsalam Abu-Libdeh, Amal Aljohani, Noof Al Abdul Salam, Fatima Al-Juailla, Emad Masuadi, Asma Deeb, Jill Weissberg-Benchell, Alice M. Gregory, Mohamed Hassanein and Ibrahim Al Alwan in Clinical Medicine Insights: Endocrinology and Diabetes
Supplemental material, sj-docx-4-end-10.1177_11795514231203907 for Lessons Learned From COVID-19 Lockdown: An ASPED/MENA Study on Lifestyle Changes and Quality of Life During Ramadan Fasting in Children and Adolescents Living With Type 1 Diabetes by Amir Babiker, Nancy Samir Elbarbary, Bothainah Alaqeel, Khalid Al Noaim, Saif Al Yaarubi, Dalia Al-Abdulrazzaq, Hessa Al-Kandari, Haya Alkhayyat, Rasha Odeh, Omer Babiker, Abdulsalam Abu-Libdeh, Amal Aljohani, Noof Al Abdul Salam, Fatima Al-Juailla, Emad Masuadi, Asma Deeb, Jill Weissberg-Benchell, Alice M. Gregory, Mohamed Hassanein and Ibrahim Al Alwan in Clinical Medicine Insights: Endocrinology and Diabetes