Abstract
Introduction
Obstruction of the lacrimal drainage represents a common ophthalmologic issue. The blockage may interest any level of the lacrimal drainage pathway, and it is important to find the site of obstruction to plan the most appropriate treatment. In this study, findings from magnetic resonance (MR) dacryocystography were compared with findings from endoscopic and surgical procedures to evaluate the accuracy of MR dacryocystography in localizing the site of nasolacrimal duct obstruction.
Methods
We enrolled twenty-one patients with clinical suspicion of nasolacrimal duct obstruction who underwent dacryoendoscopy and surgery. MR dacryocystography was performed with a heavily T2-weighted fast spin echo sequence in the coronal planes. Before the MRI was performed, a sterile 0.9% NaCl solution was administered into both conjunctival sacs. For each examination, two independent readers (with 8 and 10 years of experience in head and neck imaging) evaluated both heavily 3D space T2-weighted and STIR sequences.
Results
Stenosis/obstruction of nasolacrimal duct or lacrimal sac was diagnosed in all 21 patients who underwent MRI dacryocystography. In particular, the site of the obstruction was classified as lacrimal sac in 12 (57%) patients, nasolacrimal duct in 6 (29%) patients, and canaliculi in 3 (14%) patients by both readers. By comparison with the evidence resulting from the endoscopy, there were differences between MRI dacryocystography and dacryoendoscopy in the evaluation of the obstruction’s site in three patients, with an overall accuracy of 85.7%.
Conclusion
MR dacryocystography allows a non-invasive evaluation of the lacrimal drainage pathway, valid for the planning of the most appropriate treatment.
Keywords: MR dacryocystography, lacrimal sac, dacryocystitis, lacrimal drainage pathway, magnetic resonance imaging
Introduction
The function of the nasolacrimal apparatus is the supply of moisturization and lubrication of the cornea and the conjunctiva. 1 Obstruction of the lacrimal drainage can manifest with epiphora and eye discharge and represents a common ophthalmologic issue. The cause of obstruction can affect any level of the lacrimal drainage pathway 2 as a result of idiopathic inflammation, fibrosis, or scarring of the nasolacrimal duct.3,4
Another possibility is represented by functional obstructions. Functional obstructions are an underdiagnosed entity, consisting of the manifestation of epiphora in the presence of a patent lacrimal pathway and the absence of alternative possible etiology. Functional abnormalities of the lacrimal system have been poorly defined and include functional block, physiologic dysfunction, and functional acquired epiphora; however, functional nasolacrimal duct obstruction (FNLDO) is the most commonly used terminology.5–8
Few authors have defined FNLDO to include partial obstructions; 8 however, this would be misleading because the issue is anatomical rather than functional. Before labeling a case as functional, it is critical to rule out other causes of epiphora. Upper or lower lacrimal system functional issues can occur. It is known that altered outflow dynamics without anatomical narrowing in the upper system occur in older patients (mean age 57–64 years) with a high incidence of bilaterality (86%): 9 these findings support the hypothesis of decreasing efficiency of the lacrimal pump due to an age-related weakening of the orbicularis oculi.
Because functional epiphora is an exclusion diagnosis, a careful slit-lamp examination, lacrimal irrigation, and probing should be performed to rule out a number of potential causes of epiphora. Nasal endoscopy can sometimes reveal nasal causes of functional epiphoras, such as rhinitis.
Traditional methods of treating the obstructions involved surgical external dacryocystorhinostomy, a very effective but invasive procedure that frequently required general anesthesia and could result in the formation of facial scar tissue. 10 In recent years, endoscopic dacryocystorhinostomy has been developed as a less invasive treatment. 11 Moreover, micro-invasive therapies such as balloon dilation and nasolacrimal polyurethane stent placement have been used with successful results.12,13
Proper imaging is essential to confirm the diagnosis and assess the exact level of the obstruction to plan the most appropriate treatment.4,14 However, it might be challenging to accurately pinpoint the location and degree of stenosis/obstruction while evaluating the nasolacrimal duct. 14
Lacrimal drainage can be studied using different imaging modalities. Traditionally, dacryocystography has been used to exclude areas of narrowing or stenosis. 8 Digital subtraction dacryocystography was once the standard gold method, but it has gradually been replaced by computed tomography dacryocystography. 15 Also this technique, however, has some drawbacks, including the use of ionizing radiation, the need for canaliculus cannulation, and the lack of information on the surrounding soft tissues due to low-contrast resolution.16,17 Cone beam CT dacryocystography has been proposed as a valid alternative due to the low radiation exposure.18,19
Dacryoscintigraphy technique is used to define the dynamic level of outflow delay if the lacrimal system is patent. 8
Magnetic resonance (MR) dacryocystography with or without gadolinium administration has been increasingly used, as it does not involve ionizing radiation exposure, allows the identification of lacrimal drainage pathway obstruction and its level, and is characterized by a high-contrast resolution.19,21
Dynamic MR examinations through the execution of time-resolved angiography with interleaved stochastic trajectories (TWIST) 22 or dynamic recalled three-dimensional spoiled gradient (3DSPGR) 23 sequence demonstrated their ability to visualize real-time contrast flow through the lacrimal drainage system, from the lacrimal sac to nasolacrimal duct and finally inferior meatus, providing functional information.
To avoid the contrast injection into the lacrimal puncta, topical contrast instillation has been proposed by some authors20,21; however, this type of gadolinium administration is still off-label.
An alternative is represented by non-contrast MR dacryocystography, a MR technique based on acquiring heavily T2-weighted sequences to enhance static and slowing moving fluids, with suppression of the tissue background signal.24,25 Because fluid-filled lacrimal drainage pathway components have long longitudinal and transverse relaxation times, they show high signal intensity on T2-weighted images.14,24 This acquisition modality can also benefit from the acquisition of other standard orbital sequences for the assessment of periorbital soft tissue and retro-orbital components. 25
Few data on non-contrast MR dacryocystography have been described in the literature;14,24,26 therefore, we aim at reporting our experience with this technique.
Materials and methods
This study has been approved by our Institutional Review Board and conducted in accordance with the Declaration of Helsinki and its later amendments. Patients provided their consent to the examinations and use of their anonymized data and images.
Acquisition technique
We performed the examinations on a 1.5-Tesla magnet (Avantofit, Siemens Healthineers, Erlangen, Germany); the gradient system operates with a maximum gradient strength of 45 mT/m/ms and a slew rate of 200 mT/m. The patients were placed on the scanner table in a supine position, head first, using supports when needed to keep the patient’s head as firm as possible. The patients were instructed to stay still.
Sterile 0.9% NaCl solution was administered into both conjunctival sacs, two drops per eye, 4 times at 1 min intervals with patients in a sitting position and with the head hyperextended. The patients were then asked to lie down on the MR table in a supine position, and another two drops were topically administered before a 20-channel head and neck coil was placed.
Magnetic resonance dacryocystography was performed with a 3D space heavily T2-weighted fast spin-echo sequence in the coronal plane and a 3D space coronal Short Time Inversion Recovery (STIR). The acquisition parameters are listed in Table 1.
Table 1.
Acquisition parameters.
| t2_space_stir_cor_p2_iso | t2_ space_cor_p2_trig_320_iso | |
|---|---|---|
| Bandwidth | 744 Hz/Px | 367 Hz/Px |
| FoV read | 200 mm | 230 mm |
| FoV phase | 166.7 mm (83%) | 230 mm (100%) |
| Matrix | 192 × 192 | 152 × 192 |
| Flip angle | 140 | — |
| Averages | 3 | 4 |
| Concatenations | 1 | 1 |
| Voxel size | 1 × 1 × 1 mm | 1.2 × 1.2 × 1.2 mm |
| Slice thickness | 1.00 mm | 1.20 mm |
| Slice gap | 0 mm | 0 mm |
| TR | 3800 | 2500 |
| TE | 213 | 705 |
| Time of acquisition | 3.19 min | 5.34 min |
STIR: Short Time Inversion Recovery; FOV: Field of View; TR: Repetition Time; TE: Echo Time.
Patients
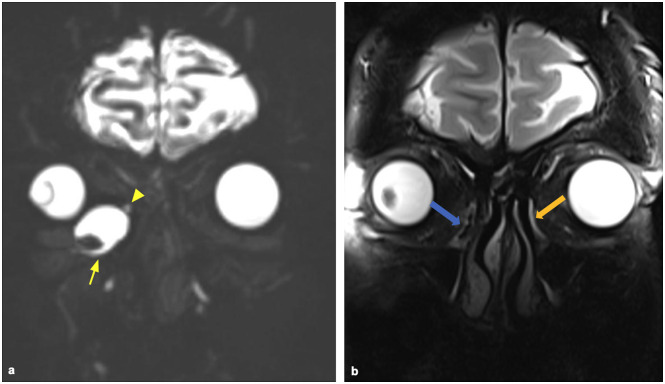
The technique was first tested on three healthy volunteers (Figure 1) and then performed on patients referred by otorhinolaryngologists with clinical suspicion of nasolacrimal duct or lacrimal sac obstruction, with epiphora and recurrent dacryocystitis being the most common clinical presentations.
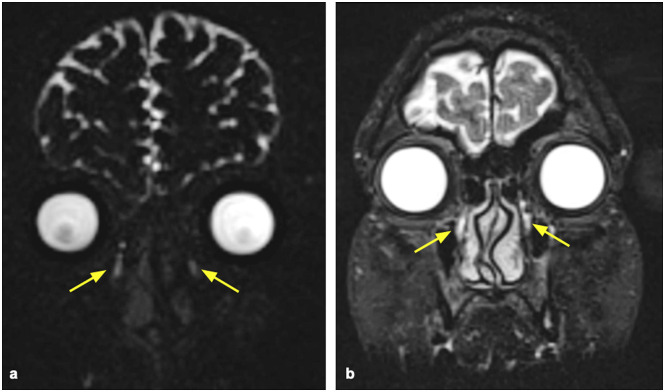
Figure 1.
Images obtained in a healthy volunteer: heavily T2-weighted 3D coronal sequence (a) and 3D coronal STIR (b) showing fluid-filled nasolacrimal ducts with normal caliber (yellow arrows). No signs of dilated lacrimal sacs.
All patients had been previously evaluated by an ophthalmologist for a clinical evaluation to exclude potential cause of functional stenosis.
From January 2021 to March 2022, consecutive patients who underwent MR dacryocystography were included in the study. Dacryoendoscopy and subsequent surgical procedures were then performed on each patient and used as the gold standard for comparison.
Patients with neoplasm-related nasolacrimal duct obstruction or previously submitted to dacryocystorhinostomy were excluded.
Image evaluation
Magnetic resonance images were sent to our Picture and Archiving Communication System and reconstructed in the axial and coronal planes and with the maximum intensity projection (MIP) algorithm.
For each examination, two independent readers (with 8 and 10 years of experience in head and neck imaging) evaluated both heavily T2-weighted and STIR sequences to assess the following findings: the visibility of the superior and inferior canaliculi on the right and left side, the dilatation of the lacrimal sac, and the presence of fluid content in the lacrimal ducts, if partial or complete.
Then, each reader, blind to any clinical findings, determined the site of the obstruction, classified as located into the lacrimal sac, nasolacrimal duct, and canaliculi.
Stenosis or obstruction at the lacrimal sac was hypothesized when an incomplete filling of the sac was depicted, or when the lacrimal sac was dilated without any recognizable fluid components in the whole nasolacrimal duct.
Stenosis or obstruction of the nasolacrimal duct was assumed in the case of partial or absent fluid filling of the nasolacrimal duct. Stenosis of the canaliculus was diagnosed in the case of dilatation of one or more canaliculus without fluid in the lacrimal sac and nasolacrimal duct.
The findings of MR dacryocystography were then compared with the results of the dacryoendoscopy and the surgical procedures for the positional diagnosis of the obstruction.
Inter-reader agreement on the positional diagnosis of the obstruction was assessed through Cohen’s k calculation. The interpretation of κ values was considered poor agreement for values < 0.20, fair agreement for values between 0.21 and 0.40, moderate agreement for values between 0.41 and 0.60, good agreement for values between 0.61 and 0.80, and excellent agreement for values > 0.80.
Results
Twenty one patients were enrolled in our study. We had no complications during MRI procedures, and no patients complained of any discomfort after the administration of sterile 0.9% NaCl solution into both conjunctival sacs.
We observed lacrimal sac dilatation in 8/21 (38%) patients on the right and on 10 patients (48%) on the left side; the presence of fluid content in the nasolacrimal ducts was seen in 15 patients (71%) on the right side and in 9 patients (43%) on the left side; and the superior and inferior canaliculi were visible in 11 patients (52%) on the right side and 14 patients (67%) on the left side.
The site of the obstruction was classified as located in the lacrimal sac in 12 (57%) patients, nasolacrimal duct in 6 (29%) patients, and canaliculi in 3 (14%) patients (Figures 2–5).
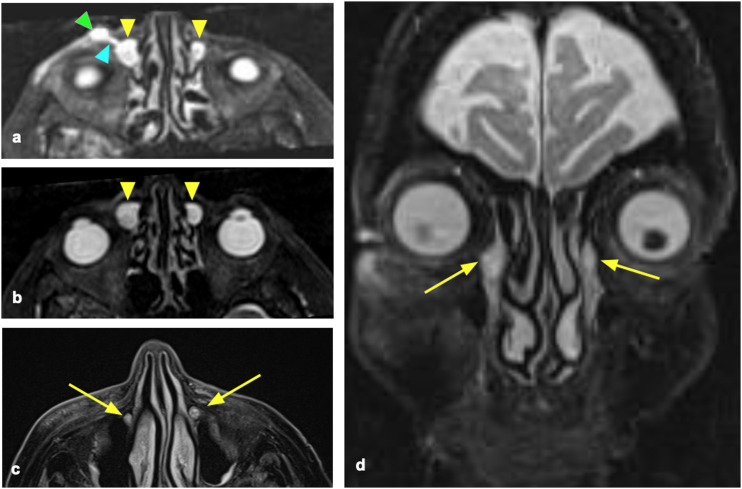
Figure 3.
73-year-old female patient affected by bilateral recurrent dacryocystitis. Axial (a, b, c) and coronal (d) reconstructions of the STIR images. Bilateral dilatation of the lacrimal sacs (a, b) (yellow arrowheads). The right lacrimal ducts present a fistulization (light blue arrowhead) with subcutaneous fluid collection (green arrowhead) (a). Both nasolacrimal ducts are filled with fluid (c, d, yellow arrows). The stenosis was diagnosed as located in the lacrimal sac and confirmed by endoscopy.
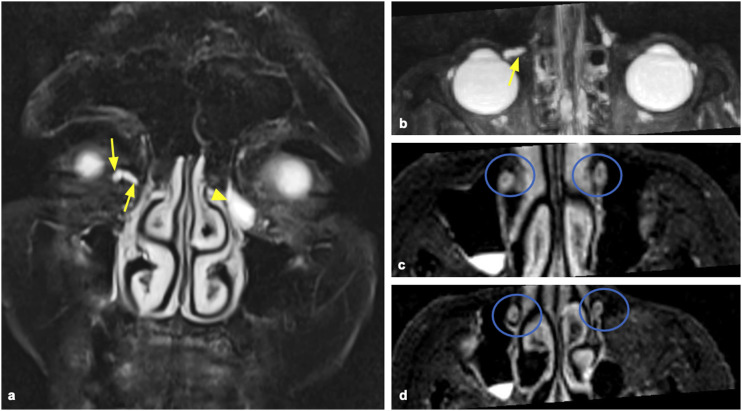
Figure 4.
Coronal MIP reconstruction of the heavily T2-weighted 3D coronal sequence (a) and axial MIP reconstruction of the heavily T2-weighted 3D coronal sequence (b) show stenosis of the common right canaliculus, with retro dilation of the common and inferior canaliculi (yellow arrows). Contralateral dilatation of the lacrimal sac (yellow arrowhead). Axial reconstructions of the 3D STIR sequence (c, d) show bilateral empty lacrimal ducts (blue circles). The patient was diagnosed as having stenosis located at the right common canaliculus and stenosis located at the left lacrimal sac.
Figure 2.
65-year-old female patient affected by right recurrent dacryocystitis. The T2-weighted image (a) showed a dilated lacrimal sac (arrowhead), with mild dilation of the inferior and superior canaliculi (white arrows). Axial (b, d) and coronal (c) reconstructions of the STIR images. In (b) the dilatation of the lacrimal sac is detectable (arrowhead). The left nasolacrimal duct is regularly filled with fluid (c, orange arrow), whereas the right nasolacrimal duct is empty (blue arrow): this finding is also visible in (d), where the axial image shows the fluid content of the left nasolacrimal duct (orange circle), whereas the left one is empty (blue circle). The obstruction was diagnosed in the nasolacrimal duct and confirmed by the endoscopy.
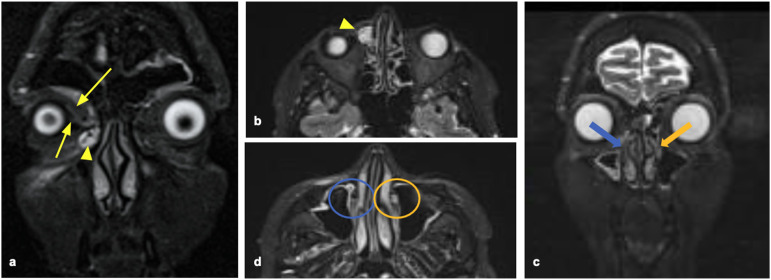
Figure 5.
A 42-year-old patient with recurrent episodes of right dacryocystitis. (a) Huge distension of the right lacrimal sac (yellow arrow), with evidence of stenosis (yellow arrowhead) at the level with the conjunction to the nasolacrimal duct. (b) Shows that the right duct is empty (blue arrow), whereas the left one is filled with fluid (orange arrow). In Supplementary Materials, we uploaded the video of the surgical procedure.
Analysis of inter-reader agreement demonstrated a κ value of 0.945, indicating an excellent agreement.
Compared with the evidence resulting from the endoscopy, the accuracy was 85.7%: there were differences between MRI dacryocystography and dacryoendoscopy in the evaluation of the obstruction site in two patients. In two of them, the site of obstruction was assumed to be the nasolacrimal duct while the endoscopy diagnosed it in the lacrimal sac. In the third patient, instead, the endoscopy identified the obstruction site at the nasolacrimal duct while it was assumed to be at canaliculi with MRI.
Afterward, 16 patients were treated with dacryocystorhinostomy and five patients with balloon dilatation or stent placement. There were no discrepancies between the site of the obstruction assessed with endoscopy and the conclusive diagnosis after surgery.
Analysis of inter-reader agreement demonstrated a κ value of 0.93, indicating an excellent agreement.
Discussion
Mini-invasive therapy, such as endonasal endoscopic dacryocystorhinostomy, stenosis dilatation with a balloon, and stent positioning, has recently advanced in the treatment of lacrimal drainage pathways. These therapies are well-tolerated by patients,12,13 but they require precise preoperative assessment of the stenosis level, the so-called “positional diagnosis.”
Due to the high radiation sensitivity of the lens, diagnostic modalities without any ionizing radiation exposure are preferred. 27
Since the introduction of MR dacryocystography with the administration of diluted gadolinium solution by Goldberg et al. 28 administered as eye drops, some studies with different imaging parameters and sequences, with topical administration of gadolinium or saline solutions, demonstrated that this technique provides detailed information about the nasolacrimal system without risks associated with cannulation and could be a useful method for the identification of nasolacrimal duct obstruction. 24
Comparing the cannulation method, the topical administration method is favored: following topical application, capillary action, muscle contraction, and blinking force the diluted contrast medium—like tears—into the nasolacrimal duct, 29 without any forced dilatation of the lacrimal drainage system and discomfort related to cannulation.14,30
The topical instillation of diluted gadolinium solution is usually well-tolerated, but it still represents an off-label use.21,28,30–32
Saline solution has a lower viscosity than diluted gadolinium, thus allowing a more physiological examination, causing less irritation in the mucosal structures and no discomfort or adverse effects, 8 as also demonstrated in our study.
Non-contrast MR dacryocystography uses stationary or slow-moving fluids into the lacrimal drainage pathway as a contrast medium through the acquisition of heavily T2-weighted images, where they show high-signal intensity, resulting in hydrographic sequences. 25
Our study demonstrated the high accuracy of non-contrast MR dacryocystography in the detection of the level of the lacrimal drainage pathway obstruction. Our results are in line with the study performed by Higashi et al. 14 who demonstrated that this imaging technique correctly diagnosed the stenosis at the canalicular level in 9/9 patients (100%) and correctly diagnosed the stenosis at the lacrimal sac in 87.5% of patients, with an overall accuracy in identifying the obstruction in 84% of the cases.
Another study, including 13 healthy volunteers and 31 patients, investigated the use of 2D and 3D impulse recovery-single-shot fast spin-echo after topical administration of saline solution to acquire non-contrast MR dacryocystography. The authors observed 100% sensitivity and 63.6% specificity for detecting the site of obstruction. 24
Other studies analyzed a variation of non-contrast MR dacryocystography involving the administration of the saline solution through cannulation20,27 and acquisition of axial and coronal T2-weighted half Fourier Single Shot Fast Spin Echo sequences with TR/TE 4000/600-1000. The findings observed at MR dacryocystography corresponded to that of conventional dacryocystography.
Cubuk et al. 27 proposed an MR dacryocystography technique based on the cannulation of the inferior puncta with the injection of 7 mL of saline and 3 mL 0.5% lidocaine with the acquisition of a fat-saturated T2 weighted single-shot turbo spin-echo sequence in the coronal plane, which was repeated 25 times for 3 min with 7 s interval to obtain dynamic images. The authors demonstrated 100% agreement with this technique with the result of conventional dacryocystography and observed no local or systemic side effects.
Only one study in the literature 33 compared the image quality of examinations performed with topical administration of saline and gadolinium solution drops: the authors reported the presence of artifacts due to the susceptibility effect in the images obtained after the administration of gadolinium.
Another study 20 compared the accuracy of non-contrast MR dacryocystography obtained with true fast imaging with steady-state precession T2-weighted images with T1-weighted fat-saturated images acquired after the cannulation of the lacrimal inferior canaliculus and injection of diluted contrast medium in the detection of the exact level of obstruction in patients with epiphora. Non-contrast MR was able to detect the site of obstruction in all cases, whereas enhanced MR wrongly diagnosed the site of obstruction in 10%; unenhanced MR dacryocystography was therefore found to be more accurate than enhanced MRI dacryocystography with a statistically significant difference. Moreover, as the authors emphasized, non-contrast MR dacryocystography was cheaper and easier to perform.
No study that investigated MR dacryocystography with the administration of saline solution reported any side effects related to its use.
Non-enhanced MR dacryocystography has some advantages over other imaging modalities for studying the lacrimal drainage pathway.
First, it uses no ionizing radiation. As the lens is one of the most susceptible tissues to ionizing radiation, its exposure to radiation should be avoided, also considering that the radiation exposure to the eye lens in conventional dacryocystography has been estimated to be 2.7 mG. 34 Second, it does not require local anesthesia, or cannulation of the punctum, therefore eliminating the risk of iatrogenic trauma on the punctum. Third, no injection of viscous contrast media is required, thus avoiding the risk of local or system side effects 19 reducing the timing and costs of the examination. 27
The main disadvantage is that since it is a static technique it does not provide any information on the transit of contrast media. Even if we are able to work with a slice thickness of 1 mm, images are affected by a discrete amount of noise.
This is a preliminary study with a limited case series. We only considered the presence/absence of stenosis without further characterizing them as partial or complete. Wider studies with the comparison with other imaging techniques and a wider population are needed to validate the usefulness of non-contrast MR dacryocystography and to optimize the acquisition technique. The comparison between images acquired pre- and post-saline administration could be also useful to further investigate the acquisition technique.
We did not include in our case series any case of functional epiphora, as the patients were previously evaluated and investigated by both ophthalmology and ENT surgeons and were sent to the execution of the MR examination for suspected stenosis.
In conclusion, MR dacryocystography allows a non-invasive evaluation of the lacrimal drainage pathway and identification of the level of obstruction/stenosis, enabling the planning of the most appropriate treatment.
Supplemental Material
Video 1.
Video 2.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was acquired before performing the examination.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Maurizio Cè https://orcid.org/0000-0002-8906-5665
Michaela Cellina https://orcid.org/0000-0002-7401-1971
References
- 1.Jones L. Anatomy of the tear system. Int Ophthalmol Clin 1973; 13(1): 3–22. DOI: 10.1097/00004397-197301310-00003 [DOI] [PubMed] [Google Scholar]
- 2.Weber A, Rodriguez-DeVelasquez A, Lucarelli M, et al. Normal anatomy and lesions of the lacrimal sac and duct: evaluated by dacryocystography, computed tomography, and MR imaging. Neuroimag Clin N Am 1996; 6: 199–217. [PubMed] [Google Scholar]
- 3.Sasaki T, Sugiyama K, Yuuko N. Nasolacrimal duct obstruction classified by dacryoendoscopy and treated with inferior meatal dacryorhinotomy. Part I: positional diagnosis of primary nasolacrimal duct obstruction with dacryoendoscope. Am J Ophthalmol 2005; 140(6): 1065–1070. DOI: 10.1016/j.ajo.2005.07.038 [DOI] [PubMed] [Google Scholar]
- 4.Cellina M, Cè M, Irmici G, et al. Nontraumatic orbital emergencies: a pictorial essay - CT and MRI features for an imaging findings-based approach. Emerg Radiol 2022; 29: 769–780. DOI: 10.1007/s10140-022-02047-z [DOI] [PubMed] [Google Scholar]
- 5.Chan W, Malhotra R, Kakizaki H, et al. Perspective: what does the term functional mean in the context of epiphora? Clin experiment Ophthalmol 2012; 40: 749–755. [DOI] [PubMed] [Google Scholar]
- 6.Montanara A, Ciabattoni P, Rizzo P. Stenoses and functional disorders of the lacrimal drainage apparatus. Radiological examination. Surv Ophthalmol 1979; 23: 249–258. [DOI] [PubMed] [Google Scholar]
- 7.Moscato EE, Dolmetsch AM, Silkiss RZ, et al. Silicone intubation for the treatment of epiphora in adults with presumed functional nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg 2012; 28: 35–39. [DOI] [PubMed] [Google Scholar]
- 8.Conway ST. Evaluation and management of “functional” nasolacrimal blockage: results of a survey of the American society of ophthalmic plastic and reconstructive surgery. Ophthal Plast Reconstr Surg 1994; 10: 185–187. [PubMed] [Google Scholar]
- 9.Cheung LM, Francis IC, Stapleton F, et al. Symptoms assessment in patients with functional and primary acquired nasolacrimal duct obstruction before and after a successful dacryocystorhinostomy surgery: a prospective study. Br J Ophthalmol 2007; 91: 1671–1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mandeville JTH, Woog JJ. Obstruction of the lacrimal drainage system. Curr Opin Ophtalmol 2002; 13: 303–309. DOI: 10.1097/01.ICU.0000029098.93308 [DOI] [PubMed] [Google Scholar]
- 11.Strong EB. Endoscopic dacryocystorhinostomy. Craniomaxillofac Trauma Reconstr 2013; 6: 67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ilgit ET, Yüksel D, Unal M, et al. Transluminal balloon dilatation of the lacrimal drainage system for the treatment of epiphora. Am J Roentgenol 1995; 165(6): 1517–1524. DOI: 10.2214/ajr.165.6.7484599 [DOI] [PubMed] [Google Scholar]
- 13.Ilgit ET, Onal B, Coskun B. Interventional radiology in the lacrimal drainage system. Eur J Radiol 2005; 55: 331–339. DOI: 10.1016/j.ejrad.2005.03.006 [DOI] [PubMed] [Google Scholar]
- 14.Higashi H, Tamada T, Mizukawa K, et al. MR dacryocystography: comparison with dacryoendoscopy in positional diagnosis of nasolacrimal duct obstruction. Radiol Med 2016; 121(7): 580–587. DOI: 10.1007/s11547-016-0632-7 [DOI] [PubMed] [Google Scholar]
- 15.Singh S, Ali MJ, Paulsen F. Dacryocystography: from theory to current practice. Ann Anat 2019; 224: 33–40. DOI: 10.1016/j.aanat.2019.03.009 [DOI] [PubMed] [Google Scholar]
- 16.Massoud TF, Whittet HB. CT-dacryocystography for nasolacrimal duct obstruction following paranasal sinus surgery. Br J Radiol 1993; 66(783): 223–237. DOI: 10.1259/0007-1285-66-783-223 [DOI] [PubMed] [Google Scholar]
- 17.Chen Z, Wang P, Du L, et al. Potential of dosage reduction of cone - beam CT dacryocystography in healthy volunteers by decreasing tube current. Jpn J Radiol 2020; 39: 233–239. DOI: 10.1007/s11604-020-01058-5 [DOI] [PubMed] [Google Scholar]
- 18.Chen Z, Wang J. Diagnostic capability and radiation dose of cone beam CT dacryocystography in different scanning fields of view in healthy volunteers. Radiol Med 2020: 668: 47–54. DOI: 10.1007/s11547-020-01227-6 [DOI] [PubMed] [Google Scholar]
- 19.Hoffmann K, Hosten N, Anders N, et al. High-resolution conjunctival contrast-enhanced MRI dacryocystography. Neuroradiology 1999; 41(3): 208–213. DOI: 10.1007/s002340050737 [DOI] [PubMed] [Google Scholar]
- 20.Somma F, Fabio A, Nicola T. Magnetic resonance imaging in the pre-operative evaluation of obstructive epiphora : true - FISP and VIBE vs gadolinium. Radiol Med 2017; 122(2): 123–130. DOI: 10.1007/s11547-016-0696-4 [DOI] [PubMed] [Google Scholar]
- 21.Coskun B, Ilgit E, Onal B, et al. MR dacryocystography in the evaluation of patients with obstructive epiphora treated by means of interventional radiologic procedures. Am J Neuroradiol 2012; 33(1): 141–147. DOI: 10.3174/ajnr.A2889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sia PI, Curragh D, Patel S, et al. Time-resolved three-dimensional technique for dynamic magnetic resonance dacryocystography. Clin Exp Ophthalmol 2019; 47(9): 1131–1137. [DOI] [PubMed] [Google Scholar]
- 23.Singh S, Dhull A, Selva D, et al. Tear transit time evaluation using real-time technique for dynamic MR dacryocystography. Orbit 2021; 40(1): 34–38. [DOI] [PubMed] [Google Scholar]
- 24.Jing Z, Lang C, Qiu-xia W, et al. High-spatial-resolution isotropic three-dimensional fast-recovery fast spin-echo magnetic resonance dacryocystography combined with topical administration of sterile saline solution. Eur J Radiol 2013; 82(9): 1546–1551. DOI: 10.1016/j.ejrad.2013.04.013 [DOI] [PubMed] [Google Scholar]
- 25.Cellina M, Martinenghi C, Panzeri M, et al. Noncontrast MR lymphography in secondary lower limb lymphedema. J Magn Reson Imaging 2021; 53(2): 458–466. DOI: 10.1002/jmri.27328 [DOI] [PubMed] [Google Scholar]
- 26.Takehara Y, Isoda H, Kurihashi K, et al. Dynamic MR dacryocystography: a new method for evaluating nasolacrimal duct obstructions. Am J Roentgenol 2000; 175(2): 469–473. DOI: 10.2214/ajr.175.2.1750469 [DOI] [PubMed] [Google Scholar]
- 27.Cubuk R, Tasali N, Aydin S, et al. Dynamic MR dacryocystography in patients with epiphora. Eur J Radiol 2010; 73(2): 230–233. [DOI] [PubMed] [Google Scholar]
- 28.Goldberg R, Heinz G, Chiu L. Gadolinium magnetic resonance imaging dacryocystography. Am J Ophthalmol 1993; 115: 738–741. [DOI] [PubMed] [Google Scholar]
- 29.Caldemeyer K, Stockberger SJ, Broderick L. Topical contrast-enhanced CT and MR dacryocystography: imaging the lacrimal drainage apparatus of healthy volunteers. Am J Roentgenol 1998; 171: 1501–1504. [DOI] [PubMed] [Google Scholar]
- 30.Karagülle T, Zileliog G, Erden A. Nasolacrimal system: evaluation with gadolinium-enhanced MR dacryocystography with a three-dimensional fast spoiled gradient-recalled technique. Eur Radiol 2002; 12(9): 2343–2348. DOI: 10.1007/s00330-001-1258-1 [DOI] [PubMed] [Google Scholar]
- 31.Amrith S, Goh PS, Wang S. Tear flow dynamics in the human nasolacrimal ducts — a pilot study using dynamic magnetic resonance imaging. Graefes Arch Clin Exp Ophthalmol 2005; 243(2): 127–131. DOI: 10.1007/s00417-004-1045-1 [DOI] [PubMed] [Google Scholar]
- 32.Manfrè L, De Maria M, Todaro E, et al. MR dacryocystography: comparison with dacryocystography and CT dacryocystography. Am J Neuroradiol 2000; 21(6): 1145–1150. [PMC free article] [PubMed] [Google Scholar]
- 33.Yoshikawa T, Hirota S, Sugimura K. Topical contrast-enhanced magnetic resonance dacryocystography. Radiat Med 2000; 18(6): 355–362. [PubMed] [Google Scholar]
- 34.Galloway J, Kavic T, Raflo G. Digital subtraction macrodacryocystography. A new method of lacrimal system imaging. Ophthalmology 1984; 91(8): 956–962. DOI: 10.1016/s0161-6420(84)34220-8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video 1.
Video 2.