Abstract
Purpose
To summarize adverse healthcare outcomes experienced by older adults with multimorbidity and barriers perceived by stakeholders regarding the healthcare systems primarily designed to address individual health conditions. Healthcare elements that aim to provide coordinated, continuous, and comprehensive services for this population were also identified.
Patients and Methods
We applied the methodology framework developed by Arksey and O’Malley to guide the review. The three-step search strategy was used to identify relevant English reviews that focused on adverse healthcare outcomes and barriers encountered by older adults with multimorbidity and other stakeholders regarding the single-disease-focused healthcare systems, as well as those concentrated on healthcare elements that aim to provide coordinated, continuous, and comprehensive services for older adults with multimorbidity. Five electronic databases, including PubMed/Medline, CINAHL, Web of Science Core Collection, Cochrane Library, and Embase, were systematically searched from database inception to February 2022. A standardized table was used to extract data. Thematic analysis was then conducted under the guidance of the Rainbow Model of Integrated Care and the Chronic Care Model.
Results
Twenty reviews were included in this study. Therapeutic competitions, high healthcare service utilization, and high healthcare costs were three adverse healthcare outcomes experienced by patients. Both patients and healthcare professionals faced various barriers. Other stakeholders, including informal caregivers, healthcare managers, and policymakers, also perceived several barriers. Numerous healthcare elements were identified that may contribute to optimized services. The elements most frequently mentioned included the implementation of shared decision-making, comprehensive geriatric assessments, and individual care plans.
Conclusion
This study conducted a comprehensive overview of the current knowledge related to healthcare for older adults with multimorbidity. In the future, it is necessary to develop more coordinated, continuous, and comprehensive healthcare service delivery models based on the healthcare needs of older adults with multimorbidity and the specific characteristics of different countries.
Keywords: multiple chronic conditions, aging, healthcare service delivery, long-term care, review
Introduction
The success of 20th-century public health, medicine, and economic and social development brings an increase in longevity in high-income countries (HIC) and low- and middle-income (LMIC) countries.1,2 Today, most people can expect to live into their sixties and beyond.2 In China, the population over 60 years has reached 264 million based on the results of the Seventh National Census.3 In the United States, more than 10,000 people turn 65 years every day.4 Between 2015 and 2050, the proportion of the world’s population over 60 years will nearly double from 12% to 22%.2 However, increased longevity also brings a health challenge – an explosion in the prevalence of multimorbidity, referring to the co-existence of two or more chronic conditions in the same individual.5 Over the past decades, people with multimorbidity have become the norm rather than the exception.6,7 Although multimorbidity is not a problem only for older adults, its prevalence is much higher in the older age group than in the young and middle-aged groups, with 65% of adults aged 65–84 years and 82% of adults over 85 years affected.6
Due to the aging process and consequent nutritional and physical degeneration, older adults are inclined to suffer from more chronic conditions, disease–disease competitions, and disease-drug competitions, leading to a high prevalence of adverse drug reactions, high healthcare services utilization and costs, declined functional status and health-related quality of life, frail, disability, and even premature death.8–11 Insufficient social support and age-friendly e-health technologies further increase their treatment burdens.12,13 Thus, healthcare for older adults with multimorbidity has become one of the most important issues facing the healthcare system across the world.
However, the healthcare systems that were primarily designed to address individual health conditions fail to provide older adults with multimorbidity coordinated, continuous, and comprehensive services. This is because our healthcare systems were developed historically to provide rapid, specialized, and efficient responses to any acute conditions and communicable diseases.14–17 The roles of patients with acute conditions and their informal caregivers were always passive, and there was little urgency to develop patient self-management skills, follow-up programs, and long-term care during the short clinical course.14 Nevertheless, this is not the case for chronic conditions which are long-term, may leave residual disability, require special training of the patient for rehabilitation, or may be expected to require a long period of supervision, observation, or care. Meanwhile, the heterogeneity and complexity of people with multimorbidity and polypharmacy render single-disease-focused guidelines often inadequate and complicate clinical decision-making.15,18 As a result, this population has to access, navigate, and cope with different healthcare services delivered by different professionals and settings to secure eligibility for services, which will further increase their burden of treatment and threaten their health and the healthcare system’s sustainability.15 Thus, the global healthcare systems must continue to reform to optimize experiences, improve clinical outcomes, reduce healthcare costs for older adults with multimorbidity and regain the work-life balance for healthcare professionals.19
Several reviews have contributed to summarizing the evidence base of healthcare for older adults with multimorbidity. Aggarwal et al conducted a study focusing on the management of polypharmacy within this particular population, 20 while Sendall et al summarized the essential components of transitional care.21 Another study by Søgaard et al synthesized the effects of patient involvement.22 Furthermore, multiple reviews explored the barriers and facilitators of healthcare for this population,23 as well as adverse healthcare outcomes.24 However, these reviews are not enough to provide broader and more detailed guidance for clinical and health policy decisions based on the following reasons:
they focused on different facets of healthcare, such as barriers,23 facilitators,23 adverse consequences,24 and healthcare elements;25,26
they focused on different research subjects, such as patients’ self-management,22 and healthcare professionals’ decision-making and interdisciplinary team;25,27
they included different types of primary studies, such as randomized controlled trials,26,28 cross-sectional studies,24 and focus group interviews.23
Thus, a scoping review of reviews method was selected as the most appropriate methodology in this study to conduct a comprehensive overview of the current state of knowledge regarding the healthcare for older adults with multimorbidity.29 The primary objective of this study was to systematically identify, summarize, and map the healthcare elements aimed to provide coordinated, continuous, and comprehensive services for older adults with multimorbidity from the current healthcare models and programs; healthcare elements can also be facilitators of the coordinated, continuous, and comprehensive services from the perspectives of stakeholders. Adverse healthcare outcomes experienced by older adults with multimorbidity and barriers perceived by stakeholders regarding the healthcare systems that were primarily designed to address individual chronic conditions were also summarized in this study.
Materials and Methods
Study Design
According to the Canadian Institutes of Health Research, scoping reviews are defined as exploratory projects that systematically map the literature available on a topic, identifying key concepts, theories, sources of evidence, and gaps in the research.30 In this present study, a scoping review of reviews was selected as the most appropriate methodology for the following three reasons: (1) a scoping review is appropriate to assess and understand the breadth and depth of the knowledge in a given field and to identify, map, report, or discuss the characteristics or concepts in that field, which is consistent with our study objectives; (2) a scoping review is particularly helpful when the types of evidence sources are complex and heterogeneous and include different study designs (eg, quantitative, qualitative, and mix-methods); and (3) a review of reviews is a rational advancement in analyzing and synthesizing a large and wide-ranging body of literature.29
The five-stage methodology framework developed by Arksey and O’Malley and advanced by Levac, Colquhoun, and O’Brien was used to guide this study.31,32 The updated methodological guidance for the conduct of scoping reviews proposed by the Joanna Briggs Institute (JBI) was also incorporated in this study.30 The optional consultation with experts was not performed as this step will be integrated into stakeholder interviews and Delphi panels when developing a new healthcare model for older adults with multimorbidity in the future. As scoping reviews focus largely on providing an overview of the existing evidence regardless of quality, an assessment of methodological limitations or risk of bias of the evidence included in this study was generally not performed.30,31
The study protocol was registered in OSF Preregistration (DOI 10.17605/OSF.IO/3MXSA). This study was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) extension for scoping reviews.33
Stage 1: Identifying the Research Question
Three research questions consistent with the objectives of this study were identified:
What are the adverse healthcare outcomes experienced by older adults with multimorbidity regarding the healthcare systems that were primarily designed to address individual chronic conditions?
What are the barriers perceived by various stakeholders (eg, patients, informal caregivers, healthcare professionals, healthcare managers, and policymakers) regarding the healthcare systems that were primarily designed to address individual chronic conditions?
What healthcare elements have been included in healthcare models, implemented in healthcare programs, or purposed as facilitators from the perspective of stakeholders to provide coordinated, continuous, and comprehensive services for older adults with multimorbidity?
Stage 2: Identifying Relevant Studies
Eligibility Criteria
Table 1 presents the study eligibility criteria based on PCCs (Population, Concept, Context, and study design/types of evidence resources) elements.30 In accordance with Arksey and O’Malley’s framework and recommendations from Levac and his colleagues,31,32 we used an iterative approach to discuss and modify these eligibility criteria during the review process.
Table 1.
Eligibility Criteria
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Population |
|
|
| Concept |
|
(1) The study focused on healthcare services for one of the multiple chronic conditions (considering the objective of this study was to address multimorbidity in a non-disease-specific way); or (2) epidemiological or physiological study related to multimorbidity. |
| Context | The contexts of interest were not limited and included all types of settings such as homes, communities, primary healthcare settings, hospitals, long-term care settings, etc. | —— |
| Study design | All types of literature reviews. | —— |
Search Strategy
The three-step search strategy recommended by JBI was utilized by two independent reviewers under the guidance of an expert librarian.30,34,35 The first step was an initial limited search of two online databases: PubMed/Medline and CINAHL. This initial search was then followed by an analysis of the text words contained in the title and abstract of retrieved articles and of the index terms used to describe the articles. A second search using all identified keywords across all included databases: PubMed/Medline, CINAHL (through EBSCO platform), Web of Science Core Collection, Cochrane Library, and Embase was conducted with limits to English articles published from database inception to February 2022. The search terms used in Web of Science Core Collection were listed in Supplementary Table 1 (Supplementary File). Grey literature databases were not searched in this study for the following reasons: (1) this study is a scoping review of reviews, which included review articles rather than original studies (the most common types of grey literature) and (2) grey literature databases (eg, Canadian Agency for Drugs and Technologies in Health Grey Matters tool, ClinicalTrials.gov, OpenGrey, Science.gov, and WorldCat) were searched by several included reviews.26,36 Thirdly, the reference lists of all included articles were manually searched to augment the coverage.
Stage 3: Study Selection
Two independent reviewers performed the initial screening of all titles and abstracts and then evaluated all potentially relevant articles based on full-text reviews. This process was piloted on the first 50 potentially relevant articles to ensure the clarification of eligibility criteria, ensure the homogenization of the study selection process between two reviewers, and reduce the chance of errors and bias. Any discrepancies regarding study inclusion were adjudicated by discussion, and if needed, in consultation with the senior author.
Stage 4: Charting the Data
To ensure transparency and clarity in the data extraction process, a standardized charting table was developed and used to extract the data including title, first author’s family name, publication year, country, study characteristics (purpose, population, sample size if applicable, methodology, and concept), and key findings related to the research objective(s). To reduce the chance of errors and bias, the standardized table was piloted with these two reviewers on at least three included articles to ensure that all necessary data was extracted appropriately. Any discrepancies regarding the extracted data were resolved by discussion, and if needed, in consultation with the senior author.
Stage 5: Collecting, Summarizing, and Reporting the Results
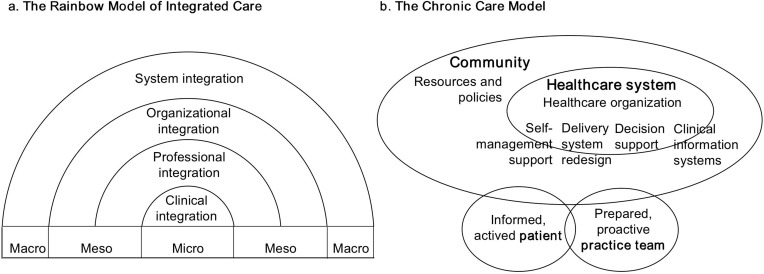
Considering elements of healthcare for older adults with multimorbidity are multifaceted because of the heterogeneous nature of diseases, a review of healthcare elements can be challenging as there is currently no formal methodology for the synthesis of data from included studies.37 To overcome this problem, theoretical frameworks could be applied to organize and make sense of the data extracted. In this scoping review of reviews, the Rainbow Model of Integrated Care and Chronic Care Model were used.14,38
The Rainbow Model of Integrated Care was developed through the literature review, a series of Delphi panels, and expert discussions at international conferences. It describes dimensions that play inter-connected roles on the macro- (system integration), meso- (organizational and professional integration), and micro-level (clinical integration) that facilitate the integration between different levels within a healthcare system.38
The Chronic Care Model developed by Wagner et al is a guide to chronic disease management.14 It provides six interrelated healthcare components: self-management support, clinical information systems, delivery system redesign, decision support, healthcare organization, and community resources and policies, and can promote system reform in which informed, motivated patients interact with prepared, proactive healthcare professionals and organizations. Applying these two theoretical frameworks (Figure 1) can offer a systematic approach to analyzing and synthesizing healthcare elements.
Figure 1.
Visual representation of the Rainbow Model of Integrated Care and the Chronic Care Model.
Deductive thematic synthesis was used to code key excerpts of extracted data.39 Two independent reviewers firstly coded the findings of included studies line-by-line, then organized these “free codes” into descriptive themes (key elements of healthcare), and mapped these “key elements” onto six “healthcare components” proposed by the Chronic Care Model and three “healthcare levels” proposed by the Rainbow Model of Integrated Care. To enhance the rigor of the synthesis process and the trustworthiness of the findings, after the initial synthesis process was completed, two reviewers then met to discuss and the consensus was finally reached through iterative discussions by the research team.
Results
Study Selection and Characteristics of Included Studies
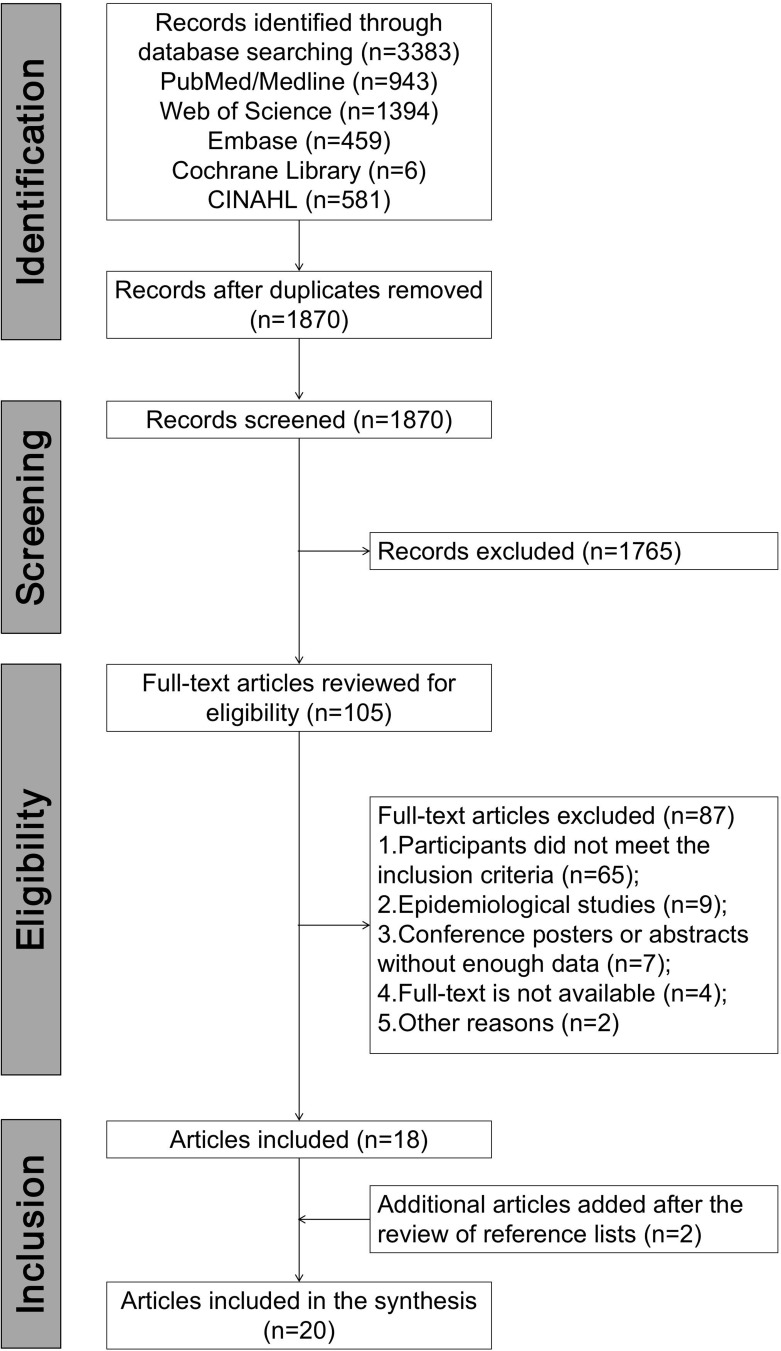
The study selection process is summarized in Figure 2 using a Preferred Reporting Items for Systematic Reviews and Meta-Analysis flow diagram. The initial search yielded 1870 records after the removal of duplicates. After title and abstract screening and full-text review, 18 studies were included, and another two studies were added through reference lists review. A total of 20 studies were included for data extraction and synthesis. The type of these studies includes systematic review, systematic search and review, literature review, meta-analysis, scoping review, and realist review. Descriptions and methods of these reviews have been summarized by Grant & Booth.40 There were three studies conducting additional expert discussions and/or stakeholder interviews. The basic characteristics of included reviews are summarized in Table 2, and the detailed information on these reviews is listed in Supplementary Table 2 (Supplementary File). The reviews originated from 10 countries, with the majority from the USA. Sixty percent of the included studies were published from 2018 to 2022.
Figure 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis flow diagram.
Table 2.
Basic Characteristics of Included Studies (n=20)
| Characteristics | Frequency Count (%) | |
|---|---|---|
| Study type | Systematic review | 7 (35.0) |
| Systematic search and review | 4 (20.0) | |
| Literature review | 4 (20.0) | |
| Meta-analysis | 2 (10.0) | |
| Scoping review | 2 (10.0) | |
| Realist review | 1 (5.0) | |
| Publication year | 2008–2012 | 3 (15.0) |
| 2013–2017 | 5 (25.0) | |
| 2018–2022 | 12 (60.0) | |
| Country | Europe | 9 (45.0) |
| USA and Canada | 7 (35.0) | |
| Asia | 3 (15.0) | |
| Australia | 1 (5.0) |
Adverse Healthcare Outcomes
Three adverse healthcare outcomes related to the healthcare systems that were primarily designed to address individual health conditions were identified from the included systematic review and literature review.24,41 The type of primary studies included in these reviews was mainly observational studies. These reviews found that older adults with multimorbidity were more likely to have therapeutic competition, high healthcare service utilization, and high healthcare costs.
Healthcare Barriers
Twenty-one barriers related to the healthcare systems that were primarily designed to address individual health conditions were identified from the included systematic reviews,12,23,42 systematic searches and reviews,20,27 literature reviews,41,43,44 and realistic review.25 The types of primary studies included in these reviews were quantitative, qualitative, and mixed-method studies. They included seven barriers (33.3%) encountered by patients, one barrier (4.8%) encountered by informal caregivers, seven barriers (33.3%) encountered by healthcare professionals, four barriers (19.0%) encountered by healthcare managers, and two barriers (9.5%) encountered by policymakers. The detailed descriptions of these barriers are outlined in Table 3.
Table 3.
Barriers Regarding the Healthcare Systems That Were Primarily Designed to Address Individual Health Conditions from the Perspective of Stakeholders
| Stakeholders | Barriers |
|---|---|
| Patients | Disease and treatment burdens |
| Lack of communication skills with healthcare professionals | |
| Lack of knowledge, skills, and confidence in self-management | |
| Conflicting information from healthcare professionals of different disciplines and settings | |
| Insufficient information adaptation of healthcare professionals based on patients’ needs and capacities | |
| Insufficient social support | |
| Preferring a passive role in the process of healthcare | |
| Informal caregivers | Lack of knowledge, skills, and confidence in providing informal care |
| Healthcare professionals | Insufficient evidence base |
| Insufficient awareness of shared decision-making with patients and informal caregivers | |
| Lack of knowledge, skills, and confidence in addressing multimorbidity | |
| Lack of communication skills with patients, informal caregivers, and other professionals | |
| Low medical adherence of patients | |
| Conflicting priorities, preferences, and goals on decision-making among two or more informal caregivers | |
| Heavy workloads | |
| Healthcare managers | Fragmented and poorly coordinated healthcare system |
| Insufficient human resources | |
| Insufficient information and communication technology support | |
| Lack of appropriate quality metrics designed for patient-centered, coordinated, and continuous healthcare | |
| Policymakers | Lack of efficient and sustainable reimbursement and payment mechanisms |
| Insufficient chronic care resources and health inequality |
Healthcare Elements
Twenty-six healthcare elements that aim to provide coordinated, continuous, and comprehensive services for older adults with multimorbidity were identified from the included systematic review,12,22,23,25,42 systematic searches and reviews,20,21,27,45 literature review,41,43,46 meta-analyses,26,28 scoping reviews,36,47 and realistic review.25 The types of primary studies included in these reviews were quantitative, qualitative, and mixed-method studies. The detailed descriptions of these elements are outlined in Table 4.
Table 4.
Healthcare Elements Aim to Provide Coordinated, Continuous, and Comprehensive Services for Older Adults with Multimorbidity
| Levels of Care | Components of Care | Elements of Care | Aims/Descriptions |
|---|---|---|---|
| Micro-level of care | Self-management support | Trustful and respectful professional-patient | Through careful listening and efficient communication, trustful and respectful professional-patient relationships can be established for the delivery of population and/or individual healthcare. |
| Active engagement of patient(s) | Healthcare professionals transfer the accountability for healthcare to patients, encourage patients to engage in the whole healthcare process, and ensure that patients are active partners in healthcare instead of passive recipients. | ||
| Active engagement of informal caregiver(s) | Recognition and support of the important role played by spouses, adult children, and other informal caregivers is necessary due to the limited consciousness and mobility of some patients. Informal caregivers should be involved in decision-making, care planning, transitions between different healthcare settings, and patient self-monitoring and self-management at home. Meanwhile, informal caregivers’ needs, quality of life, and burden of caregiving should also be considered as they may have health problems themselves. | ||
| Tailored information support | Healthcare professionals provide patients with tailored information, including disease process, signs and symptoms, healthy behaviors, medication effects, adverse drug reactions, efficient communication skills, self-monitoring methods, and use of health services, through face-to-face and telephone consultation, in-person education either individually or part of a group or community, and written, audio-visual or online materials. All information provided to patients should be tailored to their needs and capacities and kept out of medical terms. | ||
| Accessible and timely contact options | Healthcare professionals and emergency teams are accessible by telephone and/or e-health tools and can provide timely consultation, education, monitoring, outpatient and inpatient appointment, and emergency services to patients. | ||
| Meso-level of care | Delivery system redesign | Comprehensive geriatric assessment | Regular, comprehensive, and interdisciplinary geriatric assessment during patients’ first visit and subsequent health-related events should be conducted to update patients’ sociodemographic and health-related information. Sociodemographic information includes patients’ age, sex, marital status, primary informal caregiver(s), income, medicare insurance, and other details. Health-related information includes patients’ physical and mental health, living environment, unhealthy lifestyles, functional status, health-related quality of life, healthcare service utilization, healthcare costs, disease and treatment burdens, healthcare needs, priorities, preferences, goals, health literacy, medications’ names, doses, frequency, approaches, and so on. Multiple methods can be used to gather the above information such as electronic health records reviews, standardized questionnaires, patient surveys in healthcare settings or their homes, and direct observations. |
| Risk identification and prediction | Following the completion of a comprehensive geriatric assessment, patients’ risk identification and prediction should be conducted to identify potential complications and determine the appropriate level of healthcare required. | ||
| Individual care plan | To address patients’ multiple health conditions at the same time, an individual care plan should be created, implemented, and monitored by interdisciplinary teams based on the results of a comprehensive geriatric assessment. After each comprehensive geriatric assessment of patients, their individual care plans should be reviewed and modified to address patients’ evolving health problems, needs, priorities, preferences, and goals. Any changes of the individual care plan should be shared within interdisciplinary teams, patients, and informal caregivers. Printed or online care plans shared with patients may further improve their adherence. | ||
| Interdisciplinary team | The interdisciplinary team includes different practitioners (general practitioner, nurse, pharmacist, social worker, physiotherapist, occupational therapist, dietitian, rehabilitation therapist, and so on), different specialties (geriatrics, internal medicine, cardiology, oncology, psychiatry, and so on), and different levels of healthcare (primary healthcare, outpatient specialized care, hospitals, emergency department, and so on). The roles, responsibilities, and accountabilities of team members are highly clarified. | ||
| Case manager | The case manager is a trained healthcare professional serving as a point of contact for the patient and each healthcare professional involved in the healthcare process to ease communication, enhance effectiveness, reduce care fragmentation, and facilitate continuity of care and transitions across care settings. | ||
| Primary decision-maker | The role of a primary decision-maker is important when making a patient’s overall care decisions. | ||
| Decision support | Evidence-based practice | Disease-specific guidelines should be used with considerations of the heterogeneous nature and therapeutic competition of multimorbidity, and be applied together with healthcare professionals’ clinical expertise and patients’ preferences. Guidelines for multimorbidity are urgently needed. Clinical pathways and computerized decision support systems are tools to support evidence-based practice. | |
| Professional training | The focus of professional training should be primarily on prominent members of interdisciplinary teams, particularly on experts or specialists who administer regular and vital care or treatment to patients. The following knowledge and skills should be provided: screening and identification of multimorbid patients, comprehensive geriatric assessment, drug-disease and drug-drug interactions, adverse drug reactions and solutions, shared decision-making and goal-setting methods, design and implementation of individual care plans, working effectively as a team, efficient communication skills, critical appraisal and implementation of evidence-based knowledge, and health education. | ||
| Shared decision-making | The interdisciplinary teams take into account various factors such as patients’ healthcare goals, preferences, and prognosis, as well as the complexity and feasibility of treatment when making clinical decisions. Additionally, they strive to ensure the active engagement of patients and their informal caregivers during the decision-making process. Patients’ goals refer to personal health and life outcomes that patients hope to achieve through their healthcare. Patients’ preferences refer to what patients are able and willing to do to achieve their goals as well as the time, inconvenience, discomfort, and money in completing these tasks. Patients’ prognoses refer to their remaining life expectancy, functional status, quality of life, and so on. | ||
| Consultation system to experts outside of the interdisciplinary teams | Incorporating the participation of external experts, such as medical specialists and advanced practice nurses, offers the advantage of ensuring the continuity of individualized care plans while allowing a high level of professional input. | ||
| Clinic information systems | Uniform coding of health conditions | Patients’ health problems, patient-reported outcomes, healthcare utilization, and other concepts such as patient preferences, should be standardized through uniform coding and consistent definitions to promote information-sharing between different healthcare professionals and settings. | |
| Electronic health records system | Healthcare professionals keep track of patients’ medical histories, diagnoses, symptoms, medications, needs, priorities, preferences, goals, and other important information and record this information in the electronic health records system to promote information-sharing. Patients and their informal caregivers can obtain this information through patient portals. | ||
| Information-sharing | With the permission of patients, electronic health records should be shared among patients, informal caregivers, and healthcare professionals across different disciplines, organizations, and levels of healthcare. Data ownership and protection also need to be considered in this process. | ||
| E-health tools | The use of e-health tools, specifically patient-operated technologies, offers numerous benefits regarding healthcare. These tools empower patients to send information to healthcare professionals and schedule appointments, while also enabling healthcare professionals to view, monitor, and respond to this information. As a result, e-health tools have the potential to enhance in-person visits, particularly for patients who reside in remote areas, lack social support, or have limited mobility. They also contribute to increased access to interdisciplinary resources, improved self-management for patients, and enhanced monitoring of clinical indicators by healthcare professionals. Assistive technologies such as medication-taking reminders and ePrescription services are also helpful. | ||
| Healthcare organization | Human resource management | To achieve sustainable development, it is essential to have suitable human resources and visitation time for healthcare professionals. This allows them to establish close relationships with patients and their informal caregivers and implement personalized care plans at the organizational level. | |
| Supportive leadership and environment | Supportive leadership should promote the adoption of new healthcare models, management methodologies, and information and communication technologies. It should be prepared for change, ensure transparency within the organization, and establish clear accountability. Additionally, supportive leadership should create opportunities, allocate sufficient time, and provide healthcare professionals with value-based financial incentives. A supportive environment, on the other hand, pertains to the culture within the healthcare setting. This culture should embrace shared philosophies, values, and visions, such as patient-centeredness, collaboration, coordination, and caution. Furthermore, the establishment of effective communication channels promotes collaboration, coordination, and the development of mutual trust and respect among professionals from diverse disciplines. | ||
| Quality tracing and continuous improvement | Healthcare organizations should formulate suitable quality metrics with the aim of evaluating the efficacy of various treatments, interventions, and healthcare services provided to patients. Additionally, these metrics could serve as a basis for carrying out continuous enhancements in clinical practices, supported by robust evidence. | ||
| Organization collaboration | The collaboration between healthcare organizations across different levels is essential in reducing care fragmentation and achieving continuity of care. To achieve these goals, it is imperative to establish both fully integrated formal alliances and informal cooperation agreements. | ||
| Macro-level of care | Community resources and policies | Health education and promotion programs | Communities provide health education and promotion programs with the engagement of trained volunteers regularly, such as nutrition and exercise programs, peer-support programs, adult daycare centers, and psychosocial consultations. |
| Available and accessible healthcare resources | Governments should construct more infrastructure in public health and long-term care areas to ensure the availability and accessibility of health and social care resources (eg, accessible waiting time, reasonable travel times, wheelchair accessible points, and so one). | ||
| Innovative reimbursement and payment mechanisms | National or regional government subsidies and private investments are necessary for the reimbursement of costs in health and social care. Moreover, the current payment mechanisms used by both public and private medical insurers, which rely on fee-for-service payments, do not adequately support the additional services offered by emerging healthcare models. Therefore, it is crucial to explore and implement various blended payment mechanisms, such as fee-for-value payment systems that consider patients’ outcomes to ensure the sustainability of the healthcare system. |
Discussion
This study is a comprehensive overview of the current state of knowledge regarding healthcare for older adults with multimorbidity. Through a systematic search of previously published reviews, a total of three adverse healthcare outcomes experienced by patients, 21 barriers perceived by stakeholders, and 26 elements contributing to more coordinated, continuous, and comprehensive healthcare services were summarized.
Most care for older adults with multimorbidity is coordinated from patients’ self-management, informal caregivers’ home-based care, and healthcare professionals’ primary and acute care. The results of this study indicate that a wide range of adverse healthcare outcomes and barriers were encountered by stakeholders during these processes, which may be attributed to the following reasons: (1) older adults with multimorbidity are usually required to manage complex regimens, in particular medications;48 (2) informal caregivers of older adults with multimorbidity are more likely to encounter various difficulties; for example, practical challenges related to managing patients’ multiple appointments, examinations, and medications;49 (3) disease-specific clinical guidelines are not fully applicable for addressing multimorbidity;50 (4) the single-disease-focused and poorly coordinated healthcare systems often deliver fragmented services for multimorbid patients; for example, healthcare professionals typically prioritizing the most pressing problem that the patient is experiencing rather than providing person-centered healthcare;14,15 and (5) health-related policy has not adequately involved to provide person-centered and value-based care; for example, the reform of payment mechanism from fee-for-service to fee-for-value, which emphasizes the quality of services and outcomes of patients.51
To address both acute episodic illness and chronic conditions of this particular population, the coordination of care needs to be reconfigured. Skou et al proposed that three key areas related to providing healthcare services for patients with multimorbidity need to be considered, including targeting the appropriate patients and addressing their priorities, including their caregivers; supporting self-management and healthy behaviors; and delivering health and social care with a focus on interdisciplinary care and professional expertise.49 An umbrella review that aimed to clarify what is a comprehensive geriatric assessment found that the main beneficiaries of comprehensive geriatric assessment are older adults with acute illness.52 However, a random controlled trial with a follow-up period of 24 months (n=382) reported that outpatient comprehensive geriatric assessments may delay the progression of frailty and may contribute to the improvement of frail patients in older adults with multimorbidity,53 suggesting potential benefits of comprehensive geriatric assessments for not only older adults with acute conditions but also multiple chronic conditions, and that comprehensive geriatric assessment may be one of the interventions that aim to identify the older adults with multimorbidity, elicit their health problems, need, and priorities, and contribute to the development of an integrated care plan. Although this study enumerates the contents that should be included in comprehensive geriatric assessment, there is currently no standardized tool available.
Regarding the concept of self-management, Skou et al considered that it may not entirely match the lived experience of older adults with multimorbidity: they frequently receive care from informal caregivers and are more likely to do so as their health worsens.49 However, there are several randomized controlled trials that demonstrated the effectiveness of community-based or nurse-led interventions in enhancing the self-management among older adults with multimorbidity,48,54 suggesting that active engagement of both patients and their informal caregivers plays an essential role in the whole process of healthcare. In addition, this present study also summarized other elements that contribute to patients’ self-management, such as professional–patient relationship and tailored information offered by healthcare professionals. In this study, we also highlight that as informal caregivers may have health problems themselves, their needs, quality of life, and burden of caregiving should also be considered by healthcare professionals.
An increasingly aging population with multiple chronic health conditions requiring the healthcare of multiple specialists, increased specialization in healthcare and each specialist focusing on a narrow aspect of their field, and an expanding body of medical knowledge are important factors that have contributed to the increasing need for interdisciplinary teams in healthcare, especially for geriatric medicine.55 Differing from the concept of a “multidisciplinary team”, an interdisciplinary team is not just a group of experts implementing treatments or other services on a patient separately. Members of an interdisciplinary team complement one another’s expertise and actively coordinate to conduct comprehensive geriatric assessments, develop and implement individual care plans, and work toward shared goals.55 In this study, case managers and primary decision-makers are summarized as two important roles within interdisciplinary teams to ease the communication between patients, informal caregivers, and professionals, to reduce care fragmentation and ensure care continuity, to avoid conflict information provided by multiple healthcare professionals and even conflict clinical decisions, and to realize coordinated and person-centered healthcare. Future research should be designed based on the characteristics of healthcare systems in different countries and regions and establish interdisciplinary teams to validate their effectiveness in managing older adults with multimorbidity. Moreover, the implementation of interdisciplinary teams cannot be separated from educational reform. Education, training, and workforce plans that typically consider each healthcare profession in isolation cannot meet the complex healthcare needs of older adults with multimorbidity.
Furthermore, the primary concept behind the additional healthcare elements summarized in this study is to deliver a coordinated, continuous, comprehensive, and patient-centered healthcare services for older adults with multimorbidity. For example, the establishment of an inter-operated electronic health record system that connects different healthcare organizations and levels will facilitate information sharing and the implementation of interdisciplinary teams. The reform of the medical payment and reimbursement mechanism is also beneficial for healthcare professionals to provide integrated and coordinated services guided by patient outcomes and health.
Strengthens and Limitations
The strengths of this study include our broad eligibility criteria concerning the phenomena of interest and the design and methods of included studies. Since doing the right things to optimize healthcare for older adults with multimorbidity is determined not only by evidence-based practice but also by the needs of stakeholders and the models of service,46 the value of systematic reviews and meta-analyses assessing the effectiveness of healthcare programs and interventions is limited. Thus, a scoping review of reviews was used in this study to synthesize the current state of knowledge related to healthcare barriers, adverse consequences, programs, interventions, models, and elements comprehensively, and provide broader and detailed guidance for clinical and health policy decisions. Quantitative and qualitative findings helped to assess the current healthcare system from the stakeholders’ perspectives.
This study also has several limitations. Firstly, we chose to perform a scoping review of reviews to further synthesize a large body of literature. This means, all primary studies were not screened to capture information missing in the review articles, which resulted in some missing information (eg, the countries where the primary studies were carried out) and limited further possible analyses. Additionally, the same primary study may be included in more than one review. However, since this is not a systematic review trying to establish precise effects, this was not considered problematic. Second, the healthcare elements identified in this study are not all evaluated through rigorous randomized controlled trials. Therefore, the level of evidence provided by this study is lower than that of a systematic review of randomized controlled trials. Third, quality assessments were not conducted in this study as scoping reviews focus largely on providing an overview of the existing evidence regardless of quality.29,30 Fourth, we searched a limited number of electronic databases, and only articles written in English were included. Thus, we may miss some studies in specific populations. Finally, grey literature databases were not searched in this study as the most common types of grey literature are abstracts and unpublished data, which do not meet our eligibility criteria.
Implications for Further Practice and Research
After summarizing a wide range healthcare elements in this study, it is necessary to explore the healthcare needs of older adults with multimorbidity based on these elements. It is also important to assess whether demographic, health-related, or sociocultural characteristics of individuals could impact the healthcare needs of this particular population. Following the findings from needs assessments, intervention strategies should be further formulated with the aim of addressing their unmet healthcare needs.
Conclusion
This study is the first scoping review to provide a comprehensive overview of the current state of knowledge related to healthcare for older adults with multimorbidity. In the future, it is necessary to develop more coordinated, continuous, and comprehensive healthcare service delivery models based on the healthcare needs of older adults with multimorbidity and the specific characteristics of different countries.
Funding Statement
This study was funded by National Social Science Foundation [20BGL275].
Disclosure
Jingjie Wu and Hui Zhang are co-first authors for this study. The authors report no conflicts of interest in this work.
References
- 1.Salisbury C. Multimorbidity: redesigning health care for people who use it. Lancet. 2012;380(9836):7–9. doi: 10.1016/S0140-6736(12)60482-6 [DOI] [PubMed] [Google Scholar]
- 2.United Nations (UN). World population aging report; 2019. Available from https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Report.pdf. Accessed October 10, 2023.
- 3.National Bureau of Statistics of China. Bulletin of the seventh national census; 2021. Available from http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/qgrkpcgb/202106/t20210628_1818824.html. Accessed October 10, 2023.
- 4.U.S. Department of Health & Human Services. Aging; 2022. Available from https://www.hhs.gov/aging/index.html. Accessed October 10, 2023.
- 5.National Institute for Health and Care Excellence (NICE). Multimorbidity: clinical assessment and management; 2016. Available from https://www.nice.org.uk/guidance/ng56. Accessed October 10, 2023.
- 6.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 7.Zhang L, Sun F, Li Y, Tang Z, Ma L. Multimorbidity in community-dwelling older adults in Beijing: prevalence and trends, 2004–2017. J Nutr Health Aging. 2021;25(1):116–119. doi: 10.1007/s12603-020-1467-4 [DOI] [PubMed] [Google Scholar]
- 8.Hanlon P, Nicholl BI, Jani BD, Lee D, McQueenie R, Mair FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493 737 UK Biobank participants. Lancet Public Health. 2018;3(7):e323–e332. doi: 10.1016/S2468-2667(18)30091-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li HW, Lee WJ, Lin MH, et al. Quality of life among community-dwelling middle-aged and older adults: function matters more than multimorbidity. Arch Gerontol Geriatr. 2021;95:104423. doi: 10.1016/j.archger.2021.104423 [DOI] [PubMed] [Google Scholar]
- 10.Marengoni A, Akugizibwe R, Vetrano DL, et al. Patterns of multimorbidity and risk of disability in community-dwelling older persons. Aging Clin Exp Res. 2021;33(2):457–462. doi: 10.1007/s40520-020-01773-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nunes BP, Flores TR, Mielke GI, Thumé E, Facchini LA. Multimorbidity and mortality in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2016;67:130–138. doi: 10.1016/j.archger.2016.07.008 [DOI] [PubMed] [Google Scholar]
- 12.Boye LK, Mogensen CB, Mechlenborg T, Waldorff FB, Andersen PT. Older multimorbid patients’ experiences on integration of services: a systematic review. BMC Health Serv Res. 2019;19(1):795. doi: 10.1186/s12913-019-4644-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson KC, Gould MK, Krishnan JA, et al. An official American Thoracic Society workshop report. A framework for addressing multimorbidity in clinical practice guidelines for pulmonary disease, critical illness, and sleep disorders. Ann Am Thorac Soc. 2016;13(3):S12–S21. doi: 10.1513/AnnalsATS.201601-007ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff. 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64 [DOI] [PubMed] [Google Scholar]
- 15.Mair FS, May CR. Thinking about the burden of treatment. BMJ. 2014;349(4):g6680. doi: 10.1136/bmj.g6680 [DOI] [PubMed] [Google Scholar]
- 16.Yip W, Fu H, Chen AT, et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet. 2019;394(10204):1192–1204. doi: 10.1016/S0140-6736(19)32136-1 [DOI] [PubMed] [Google Scholar]
- 17.Feng Z, Glinskaya E, Chen H, et al. Long-term care system for older adults in China: policy landscape, challenges, and future prospects. Lancet. 2020;396(10259):1362–1372. doi: 10.1016/S0140-6736(20)32136-X [DOI] [PubMed] [Google Scholar]
- 18.Guthrie B, Payne K, Alderson P, McMurdo ME, Mercer SW. Adapting clinical guidelines to take account of multimorbidity. BMJ. 2012;345(1):e6341. doi: 10.1136/bmj.e6341 [DOI] [PubMed] [Google Scholar]
- 19.Bachynsky N. Implications for policy: the Triple AIM, Quadruple AIM, and interprofessional collaboration. Nurs Forum. 2020;55(1):54–64. doi: 10.1111/nuf.12382 [DOI] [PubMed] [Google Scholar]
- 20.Aggarwal P, Woolford SJ, Patel HP. Multi-morbidity and polypharmacy in older people: challenges and opportunities for clinical practice. Geriatrics. 2020;5(4):85. doi: 10.3390/geriatrics5040085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sendall M, McCosker L, Crossley K, Bonner A. A structured review of chronic care model components supporting transition between healthcare service delivery types for older people with multiple chronic diseases. Health Inf Manag. 2017;46(2):58–68. doi: 10.1177/1833358316681687 [DOI] [PubMed] [Google Scholar]
- 22.Søgaard MB, Andresen K, Kristiansen M. Systematic review of patient-engagement interventions: potentials for enhancing person-centred care for older patients with multimorbidity. BMJ Open. 2021;11(12):e048558. doi: 10.1136/bmjopen-2020-048558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pel-Littel RE, Snaterse M, Teppich NM, et al. Barriers and facilitators for shared decision making in older patients with multiple chronic conditions: a systematic review. BMC Geriatr. 2021;21(1):112. doi: 10.1186/s12877-021-02050-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lehnert T, Heider D, Leicht H, et al. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68(4):387–420. doi: 10.1177/1077558711399580 [DOI] [PubMed] [Google Scholar]
- 25.Kastner M, Hayden L, Wong G, et al. Underlying mechanisms of complex interventions addressing the care of older adults with multimorbidity: a realist review. BMJ Open. 2019;9(4):e025009. doi: 10.1136/bmjopen-2018-025009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kastner M, Cardoso R, Lai Y, et al. Effectiveness of interventions for managing multiple high-burden chronic diseases in older adults: a systematic review and meta-analysis. CMAJ. 2018;190(34):E1004–E1012. doi: 10.1503/cmaj.171391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American Geriatrics Society Expert Panel on Person-Centered Care. Person-centered care: a definition and essential elements. J Am Geriatr Soc. 2016;64(1):15–18. doi: 10.1111/jgs.13866 [DOI] [PubMed] [Google Scholar]
- 28.Yang C, Zhu S, Lee DTF, Chair SY. Interventions for improving medication adherence in community-dwelling older people with multimorbidity: a systematic review and meta-analysis. Int J Nurs Stud. 2022;126:104154. doi: 10.1016/j.ijnurstu.2021.104154 [DOI] [PubMed] [Google Scholar]
- 29.Schultz A, Goertzen L, Rothney J, et al. A scoping approach to systematically review published reviews: adaptations and recommendations. Res Synth Methods. 2018;9(1):116–123. doi: 10.1002/jrsm.1272 [DOI] [PubMed] [Google Scholar]
- 30.Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement. 2021;19(1):3–10. doi: 10.1097/XEB.0000000000000277 [DOI] [PubMed] [Google Scholar]
- 31.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 32.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. doi: 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and Explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 34.Aromataris E, Riitano D. Constructing a search strategy and searching for evidence. A guide to the literature search for aSystematic review. Am J Nurs. 2014;114(5):49–56. doi: 10.1097/01.NAJ.0000446779.99522.f6 [DOI] [PubMed] [Google Scholar]
- 35.The Joanna Briggs Institute. The Joanna Briggs institute reviewers’ manual 2015 methodology for JBI scoping reviews; 2015. Available from https://nursing.lsuhsc.edu/JBI/docs/ReviewersManuals/Scoping-.pdf. Accessed October 10, 2023.
- 36.Lee JQ, Ying K, Lun P, et al. Intervention elements to reduce inappropriate prescribing for older adults with multimorbidity receiving outpatient care: a scoping review. BMJ Open. 2020;10(8):e039543. doi: 10.1136/bmjopen-2020-039543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new medical research council guidance. Int J Nurs Stud. 2013;50(5):587–592. doi: 10.1016/j.ijnurstu.2012.09.010 [DOI] [PubMed] [Google Scholar]
- 38.Nurjono M, Valentijn PP, Bautista MA, Wei LY, Vrijhoef HJ. A prospective validation study of a rainbow model of integrated care measurement tool in Singapore. Int J Integr Care. 2016;16(1):1. doi: 10.5334/ijic.2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45. doi: 10.1186/1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108. doi: 10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- 41.Kim DH, Rich MW. Patient-centred care of older adults with cardiovascular disease and multiple chronic conditions. Can J Cardiol. 2016;32(9):1097–1107. doi: 10.1016/j.cjca.2016.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eriksen CU, Kyriakidis S, Christensen LD, et al. Medication-related experiences of patients with polypharmacy: a systematic review of qualitative studies. BMJ Open. 2020;10(9):e036158. doi: 10.1136/bmjopen-2019-036158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lavan AH, Gallagher PF, O’Mahony D. Methods to reduce prescribing errors in elderly patients with multimorbidity. Clin Interv Aging. 2016;11:857–866. doi: 10.2147/CIA.S80280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tinetti ME, Esterson J, Ferris R, Posner P, Blaum CS. Patient Priority-Directed Decision Making and Care for Older Adults with Multiple Chronic Conditions. Clin Geriatr Med. 2016;32(2):261–275. doi: 10.1016/j.cger.2016.01.012 [DOI] [PubMed] [Google Scholar]
- 45.Guiding principles for the care of older adults with multimorbidity: an approach for clinicians. Guiding principles for the care of older adults with multimorbidity: an approach for clinicians: American Geriatrics Society expert panel on the care of older adults with multimorbidity. J Am Geriatr Soc. 2012;60(10):E1–E25. doi: 10.1111/j.1532-5415.2012.04188.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ouellet GM, Ouellet JA, Tinetti ME. Principle of rational prescribing and deprescribing in older adults with multiple chronic conditions. Ther Adv Drug Saf. 2018;9(11):639–652. doi: 10.1177/2042098618791371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lun P, Law F, Ho E, et al. Optimising prescribing practices in older adults with multimorbidity: a scoping review of guidelines. BMJ Open. 2021;11(12):e049072. doi: 10.1136/bmjopen-2021-049072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang C, Lee DTF, Wang X, Chair SY. Effects of a nurse-led medication self-management intervention on medication adherence and health outcomes in older people with multimorbidity: a randomised controlled trial. Int J Nurs Stud. 2022;134:104314. doi: 10.1016/j.ijnurstu.2022.104314 [DOI] [PubMed] [Google Scholar]
- 49.Skou ST, Mair FS, Fortin M, et al. Multimorbidity. Nat Rev Dis Primers. 2022;8(1):48. doi: 10.1038/s41572-022-00376-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gray M. Value based healthcare. BMJ. 2017;356:j437. doi: 10.1136/bmj.j437 [DOI] [PubMed] [Google Scholar]
- 51.Lemak CH, Nahra TA, Cohen GR, et al. Michigan’s fee-for-value physician incentive program reduces spending and improves quality in primary care. Health Aff. 2015;34(4):645–652. doi: 10.1377/hlthaff.2014.0426 [DOI] [PubMed] [Google Scholar]
- 52.Parker SG, McCue P, Phelps K, et al. What is Comprehensive Geriatric Assessment (CGA)? An umbrella review. Age Ageing. 2018;47(1):149–155. doi: 10.1093/ageing/afx166 [DOI] [PubMed] [Google Scholar]
- 53.Mazya AL, Garvin P, Ekdahl AW. Outpatient comprehensive geriatric assessment: effects on frailty and mortality in old people with multimorbidity and high health care utilization. Aging Clin Exp Res. 2019;31(4):519–525. doi: 10.1007/s40520-018-1004-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Markle-Reid M, Ploeg J, Fraser KD, et al. Community program improves quality of life and self-management in older adults with diabetes mellitus and comorbidity. J Am Geriatr Soc. 2018;66(2):263–273. doi: 10.1111/jgs.15173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.What is an interdisciplinary team? Definition, importance and advantages; 2023. Available from https://www.indeed.com/career-advice/finding-a-job/interdisciplinary-team. Accessed October 10, 2023.