Abstract
Background
Hearing loss leads to increased irritability and disengagement in social activities and conversations, which may impact quality of life. Dental professionals are at risk of developing hearing loss through daily exposure to noise from a wide range of equipment that produces significantly high decibels and noise frequencies.
Aims
The aim of this systematic review was to investigate the risk of hearing loss in dental professionals, including dentists, dental specialists, dental hygienists and dental assistants.
Methods
This review was conducted following the Cochrane Handbook for Systematic Reviews. PubMed, Scopus, Embase, Cochrane, Science Direct, Google Scholar and ProQuest were searched up to March 2023. Seventeen of 416 studies met the inclusion criteria. Quality assessment was performed according to the Newcastle–Ottawa Scale for cohort and case–control studies, and a modified version of this tool for cross-sectional studies.
Results
The majority of included studies (82%) found a positive association with hearing loss for dentists and dental specialists, with years of clinical experience identified as a prominent risk factor. Dental hygienists and dental assistants were less commonly reported in the literature. Difference between the left and right ears was found in 71% of studies, with the left ear more affected in both dentists and dental assistants due to proximity to the noise-inducing equipment.
Conclusions
Dental professionals are at risk of hearing loss in their workplace, especially linked to years of clinical experience, which highlights the need for prevention and appropriate ear-protective devices.
A systematic review was conducted to summarize the risk of hearing loss in dental professionals due to exposure to noise-inducing equipment. The results show a clear association with hearing loss in dentists and dental specialists, with years of clinical experience identified as a prominent risk factor. The left ear seems to be more affected due to proximity to the noise-inducing equipment.
Key learning points.
What is already known about this subject:
Exposure to noise exceeding 85 dB for over 8 h a day may lead to adverse effects on the human ear and can lead to conditions such as noise-induced hearing loss.
Tinnitus, a condition where an individual experiences a ringing, hissing and sizzling sensation without an external stimulus present, may arise from noise-induced hearing loss.
Dental professionals are at risk of developing noise-induced hearing loss since they are exposed to a wide range of equipment in their work environment that produces significantly high decibels and frequencies of noise.
What this study adds:
A positive association between noise in the dental workplace and hearing loss was found in dentists and dental specialists, with the left ear more affected, due to proximity to the noise-inducing equipment.
Results for gender and hours of exposure per day showed no association with hearing loss.
Future research should investigate the association between noise-induced hearing loss and dental specialists in more detail; the viability of hearing protection targeted towards the ear most at risk; noise levels produced by specific dental equipment; and comparisons between new and old dental equipment.
What impact this may have on practice or policy:
The results from this review highlight the need for prevention and appropriate protective devices to mitigate the implications of noise-induced hearing loss in the dental workplace.
Digital noise excluding headphones that excludes environmental noise, but allows the passage of the human voice, should be considered for the dental environment.
Introduction
Noise, measured in decibels (dB), is a stimulus that is perceived through the hearing of the individual and is characterized by the frequency and level of sound [1]. According to the USA’s National Institute on Deafness and Other Communication Disorders (NIDCD), exposure to long or repeated noise exceeding 85 dBA may lead to adverse effects on the human ear [2]. The Occupational Safety and Health Administration (OSHA) further recommends a hearing conservation programme should this exposure exceed an 8-h time-weighted average [3]. The NIDCD describes noise-induced hearing loss (NIHL) as damage to the sensitive structures in the inner ear, caused by both loud and long-lasting sounds [2]. NIHL occurs when sensory cells present in the cochlea are damaged and killed through aggravated noise exposure; they are then unable to regenerate and are eventually replaced by scar tissue, which then results in hearing loss [4]. NIHL should be distinguished from presbycusis, which is age-related hearing loss, usually affecting both ears, due to changes in the middle ear and the nerve pathways from the ear to the brain [5]. Tinnitus, a condition where an individual experiences a constant or intermittent ringing, hissing and sizzling sensation without an external stimulus present, may arise from NIHL [6]. Persistent tinnitus can become chronic, which may require therapy, drugs and hearing aids [7]. Hearing loss leads to increased irritability and disengagement in social activities and conversations, which may be a barrier to the development or management of relationships and affect quality of life [8]. NIHL also leads to an increase in sleep disorders, headaches, heart disease and tinnitus [1].
Dental professionals are at risk of developing NIHL since they are exposed to a wide range of equipment in their work environment that produces significantly high dB and frequencies of noise [9]. Some of these include high-volume excavators, air turbine handpieces, ultrasonic scalers, amalgamators and sterilization equipment [10]. Sound levels of this equipment, often used in combination, were found to vary between 60–99 [1] and 52–92 dBA [9] in studies conducted in two dental schools. A study in four dental practices found that ultrasonic scalers were the only equipment to exceed 85 dBA [10].
The literature reports conflicting results on whether noise in the dental environment results in hearing loss [11]. This systematic review investigated NIHL in dental professionals, including dentists, dental specialists, dental hygienists and dental assistants.
Methods
This systematic review did not require ethics approval; the protocol was registered on PROSPERO (CRD42022298641). The Cochrane Handbook for Systematic Reviews was used to conduct this study [12]. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement was used for reporting this review [13].
The Population–Exposure–Comparison–Outcome framework guided the controlled terminology and Medical Subject Headings (MeSH) keywords for the search strategy [14]. Population: dentists, dental specialists, dental hygienists and dental assistants; Exposure: noise levels and frequency; Comparison: no or a lower noise level; and Outcome: NIHL.
Eligibility criteria included (i) observational studies (cohort, case–control and cross-sectional); (ii) peer-reviewed journals; (iii) published in English and (iv) dentists, dental specialists, dental hygienists and dental assistants. Exclusion criteria included (i) case reports, case series, pilot studies, letters/editorials and opinion-based studies; literature reviews and qualitative surveys; experimental and in vivo studies; (ii) non-clinical dental personnel (dental technicians and dental receptionists); and (iii) papers published before 1990. Dental technicians were excluded as it is advised that they use protective devices for their ears [10], whereas clinicians do not since they need to communicate with patients.
A search was undertaken in March 2022 in PubMed, Scopus, Embase, Cochrane, Science Direct, Google Scholar and ProQuest. The search was repeated in March 2023 to ensure the inclusion of any newly published articles. A manual search of bibliographies of the included articles was conducted to identify other relevant articles. Table 1 presents the search strategy. Independent screening of titles and abstracts was done by five reviewers (A.C., E.M., G.T., J.H. and OM). Discrepancies and disagreements were resolved through consensus. A Cohen’s kappa value of 0.85 was set as the level of agreement [15]. Full-text analyses were performed independently by four reviewers (E.M., J.H., O.M. and G.T.) following the removal of duplicates. A record was kept for the reasons for exclusion.
Table 1.
Search strategy
| # | Search terms |
|---|---|
| #1 | dent* OR ‘dental hygienist’ OR ‘dental assistant’ OR ‘oral health therapist’ |
| #2 | ‘hearing impair*’ OR ‘hearing loss’ OR ‘hearing issues’ OR deafness OR ‘partial hearing’ OR ‘deaf*’ OR tinnitus OR ‘noise induced hearing loss’ OR ‘noise-induced hearing loss’ OR NIHL OR ringing OR ‘occupational hearing loss’ OR ‘transitory hypoacusis’ |
| #3 | ‘ultrasonic scaler’ OR ‘ultrasonic instrument’ OR ‘ultrasonic equipment’ OR ‘ultrasonic cleaner’ |
| #4 | ‘dent* handpiece’ OR ‘dent* drill’ OR ‘dent* air turbine handpiece’ OR ‘air turbine handpiece’ |
| #5 | ‘dent* technician equipment’ OR ‘dent* technician instruments’ OR ‘dent* laboratory equipment’ |
| #6 | ‘high volume suction’ OR ‘high volume evacuator’ OR ‘dental suction’ OR suction |
| #7 | risk* OR impact OR effect OR influence OR hazard |
| #8 | #1 AND #2 AND #3 AND #4 AND #5 AND #6 AND #7 |
The Newcastle–Ottawa Scale (NOS) was used for quality assessment of cohort and case–control studies [16], and a modified version for cross-sectional studies [17]. NOS evaluates selection, exposure and comparability with a maximum score of 9 for cohort and case–control studies, and a maximum score of 10 for cross-sectional studies. A score equal to or less than 5 indicates a high risk of bias, 6–7 a medium risk, and 8 or higher a low risk of bias. Two reviewers independently rated and compared the scores for each study (O.M. and G.T.). A third reviewer (A.C.) resolved any disagreements.
Two reviewers (J.H. and E.R.) extracted the data independently according to the Cochrane Handbook for Systematic Reviews [12]. This included study type and details (author, year, and publication and country), sample size, age of participants, statistical analysis, audiometric tests used and the direction of association of the investigated variables. Accuracy of information was checked by two reviewers (J.H. and E.R.). Data extraction was repeated to resolve any discrepancies.
Due to the heterogeneity of the statistical analysis and reporting of results of the included papers, presentation of results for the type of oral health professional and demographic/environmental variables associated with hearing impairment was either indicated as direct (+) or none (0). The number of studies with these respective associations, divided by the number of studies reporting on the respective variable, was expressed as a percentage. This was only calculated if four or more studies reported on a specific variable.
Results
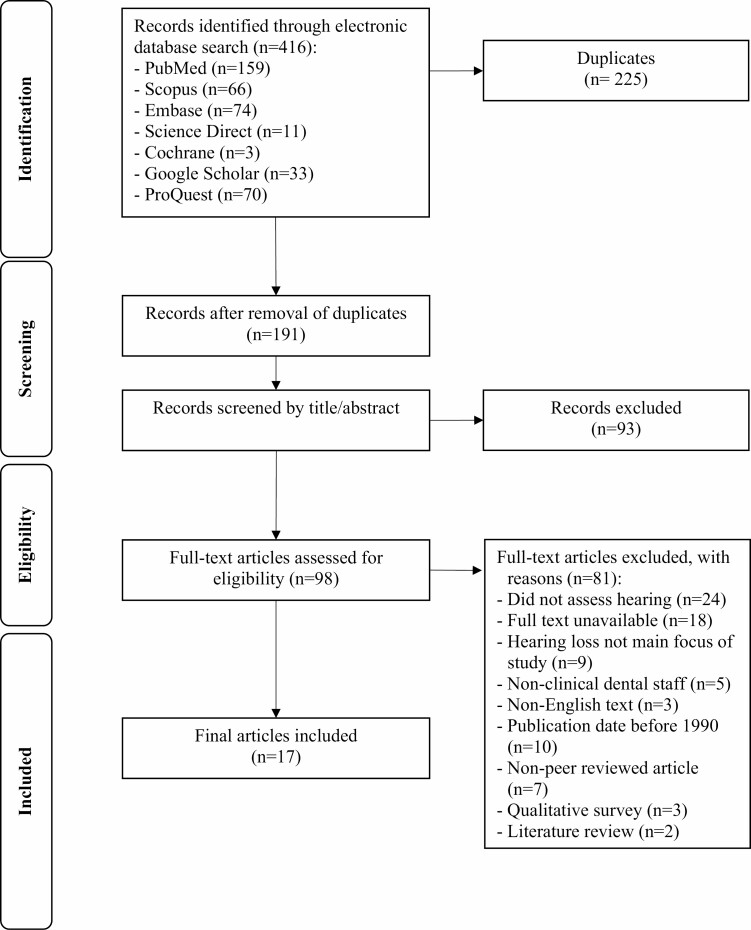
Figure 1 shows the PRISMA flowchart for the selection of studies. The initial search identified 416 records. After the removal of duplicates and screening by title/abstract, 98 records remained for full-text review. This led to another 81 records being excluded with reasons, resulting in 17 records eligible for review and data extraction.
Figure 1.
PRISMA flowchart.
All variables in this systematic review were strictly quantitative, with the inclusion of questionnaire data only if it was subjected to statistical analysis to eliminate subjective perceptions of hearing loss. Supplementary Table 1 presents the characteristics of the included studies. One was a cohort (6%), 6 were case–control (35%) and the remaining 10 were cross-sectional studies (59%), conducted in 13 different countries. Participants’ hearing was measured through either a single or combination of audiometric tests, predominantly as pure tone audiometry, acoustic impedance, otoacoustic emission, distortion product otoacoustic emission and/or tympanometry. The statistical significance of the association between hearing loss and oral health professionals, demographic and environmental variables, was determined by conducting various bivariate or multivariate analyses. Most studies included dentists, dental specialists and/or dental assistants. Dental hygienists were included in one [18], and dental students in two studies [19,20]. Results for dental students were excluded as learning environments tend to have higher volumes of noise due to a large volume of students operating concurrently in large clinics [21,22]. The majority of studies found statistically significant hearing loss at high frequencies between 3 and 6 kHz [23–26].
Table 2 presents the quality assessment of the included studies. All studies had either a low (n = 14) or medium (n = 3) risk of bias. Of the 10 cross-sectional studies, 8 [20,23,26–31] had a low, and the remaining 2 [18,25] had a medium risk of bias, both of which did not mention blind testing. Only three studies did not account for confounding variables [11,25,27].
Table 2.
Quality assessment of included studies
| Author | Selection | Comparability | Outcome | Total score (Max: 9) (risk) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Is the case definition adequate? | Representiveness of the cases | Selection of controls | Definition of controls | The subjects in different outcome groups are comparable, based on the study design or analysis | Confounding factors controlled | Ascertainment of exposure | Same method of ascertainment for cases and control | Non-response rate | ||
| Cohort studies (n = 1) | ||||||||||
| Gijbels et al. [33] | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 (low) |
| Case–control studies (n = 6) | ||||||||||
| Ahmed et al. [32]. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 (low) |
| Al‐Omoush et al. [19] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 (low) |
| Dierickx et al. [11] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 7 (medium) |
| Gonçalves et al. [34] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 (low) |
| Gurbuz et al. [24] | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 7 (medium) |
| Khaimook et al. [35] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 (low) |
| Author | Selection | Comparability | Outcome | Total score (Max. 10) (risk) | ||||||
| Representative-ness of sample | Sample size | Non-respondents | Ascertainment of exposure | The subjects in different outcome groups are comparable, based on the study design or analysis. | Confounding factors controlled | Assessment of outcome | Statistical test | |||
| Cross-sectional studies (n = 10) | ||||||||||
| Alabdulwahhab et al. [27] | 1 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 8 (low) | |
| Al-Rawi et al. [23] | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 1 | 8 (low) | |
| Chopra et al. [28] | 1 | 1 | 1 | 2 | 1 | 1 | 2 | 1 | 10 (low) | |
| Daud et al. [29] | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 1 | 8 (low) | |
| Gabrielle et al. [30] | 1 | 1 | 0 | 2 | 1 | 1 | 2 | 0 | 8 (low) | |
| Lopes et al. [25] | 1 | 1 | 1 | 2 | 1 | 0 | 0 | 1 | 7 (medium) | |
| Shetty et al. [31] | 1 | 1 | 1 | 2 | 1 | 1 | 2 | 1 | 10 (low) | |
| Theodoroff and Folmer [20] | 1 | 1 | 0 | 2 | 1 | 1 | 2 | 1 | 9 (low) | |
| Willershausen et al. [26]. | 1 | 1 | 0 | 2 | 1 | 1 | 2 | 1 | 9 (low) | |
| Wilson et al. [18] | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 1 | 7 (medium) | |
Table 3 presents the percentage of studies with either a direct (+) or no (0) association of the variable with NIHL included in this review. This was calculated from the results presented in Supplementary Table 1. Nine of the 11 studies (82%) found a direct association with hearing loss for dentists [20,24–26,28,32–35]. All five studies including dental specialists also indicated a direct association with hearing loss [23,25,27,30,31]. Two out of four studies (50%) reported a direct association between dental assistants and hearing loss [19,25].
Table 3.
The association of type of oral health professional and demographic/environmental variables with NIHL
| Studies assessing the risk variablea (n) | Direct association with hearing loss, n (%) | No association with hearing loss, n (%) | |
|---|---|---|---|
| Type of oral health professional | |||
| Dentist | 11 | 9 (82) | 2 (18) |
| Dental specialists | 5 | 5 (100) | 0 (0) |
| Dental assistants | 4 | 2 (50) | 2 (50) |
| Demographic and environmental variables | |||
| Difference between ears | 14 | 10 (71) | 4 (29) |
| Years of clinical experience | 11 | 9 (82) | 2 (18) |
| Age | 8 | 6 (75) | 2 (25) |
| Gender | 5 | 1 (20) (males) | 4 (80) |
| Hours of exposure per day | 4 | 1 (25) | 3 (75) |
aCalculations were only performed if four or more of the included studies (n = 17) reported on the variable.
The difference between the left and right ears was investigated in 14 studies, 10 of which (71%) reported a difference in hearing loss [19,20,23,25,27,28,31–34]. Years of clinical experience were reported in 11 studies. Nine (82%) found a direct association with hearing loss [11,20,23,24,30,31,33–35]. For gender, only one of five studies (20%) found a direct association with hearing loss reported for males [23]. Three of four studies (75%) found no association for hours of exposure per day [30,31,35].
Discussion
Current literature shows no consensus on whether dental professionals are at risk of NIHL. The aim of this systematic review was to ascertain whether dental professionals, including dentists, dental specialists, dental hygienists and dental assistants, are at risk of hearing loss due to noise exposure in their work environment. A direct association with hearing loss in dentists and dental specialists was found in this review, combined with a difference between the left and right ears. Years of clinical experience were the most important demographic/environmental variable.
A strength of this review was the inclusion of observational studies with objective audiometric testing only, with pure tone audiometry reported in all included studies. As a result, all included studies had either a low (82%) or medium (18%) risk of bias. Further strengths were that similar results were reported from 13 different countries across the 17 included papers. Selection bias and associated publication bias were minimized by searching seven different databases, as well as implementing a duplicate screening strategy by independent reviewers.
A limitation of this review is that the majority of includes studies (59%) were cross-sectional, which in general does not provide good evidence since there is no temporal association. Heterogeneity of the statistical analysis and reporting of results of the included papers prevented a meta-analysis. Further limitations are that three studies did not account for confounding variables, and no studies reported on the impact of hearing loss on dental professionals’ quality of life. Although five studies reported on hearing loss in dental specialists, they were included in the study population with dentists [23,27,30]. Two studies specified the specialities included [25,31]. Another limitation was that only one of these drew comparisons, with one test indicating inner ear dysfunction in paediatric specialists, most likely due to cumulative noises of dental equipment and cries of babies and children [31]. A qualitative study concluded that prosthodontists were more significantly associated with hearing loss when compared to other specialities such as periodontology, dental surgery, paedodontics and orthodontics due to the regular use of equipment emitting louder noise, placing them at a higher risk of hearing loss when compared to other specialists [36].
The finding from this review is that significant hearing loss occurs at high frequencies between 3 and 6 kHz [23–26], especially since background noise of frequencies above 3 kHz plays a crucial role in localization and comprehension of speech [37].
Whereas clear associations with noise and hearing loss were found for dentists and dental specialists, this was inconclusive for dental assistants. A possible reason is that the average noise exposure for assistants was 6.6 h [29], which is less than the 8-h limit recommended by OSHA [3].
The majority of studies reported that the left ear was more affected by hearing loss in both dentists and specialists [23,27,28,32,33], most likely due to the left ear being closer to the noise-inducing equipment held by right-handed clinicians [33]. The left ear was also found to be more affected in dental assistants since it was closer to high-volume excavators and other equipment [19]. In contrast, two studies reported increased hearing loss in the right ear for both dentists and dental assistants [25,34], whereas equal hearing loss was reported in both ears in another study [20].
NIHL occurs with years of clinical experience. There is consensus in the literature that NIHL becomes apparent from 10 years or more of clinical experience [23,26,31,33,34]. Similarly, a significant correlation was found between sensorineural hearing loss and a work tenure of 15 years [35].
Age showed a positive association with NIHL in six out of eight studies (75%) [18,22,25,29,30,34], especially after the age of 40 [19,20,23,30,31,33–35]. Since presbycusis usually occurs from the age of 50 [30,31,35], results from this review for age should be considered in light of presbycusis as a confounding variable.
Hours of exposure per day showed no association with hearing loss. This variable is complex as the results are reliant on self-reported estimates due to the difficulty of measuring the exact duration of exposure [38]. Only one study found an association between the duration of exposure and hearing loss, where exposure to intensive noise-producing devices was significant at an average of 4 h per day [19]. The NIDCD advises the louder the noise, the shorter amount of time it takes to induce hearing loss [2]. This contrasts another recommendation which suggests exposure to noise levels over 85 dBA for 8 h is responsible for NIHL [9,36].
Future research should investigate the association between NIHL and dental specialists in more detail, the viability of hearing protection targeted towards the ear most at risk, noise levels produced by specific dental equipment, and comparisons between new/well-maintained versus old and poorly maintained dental equipment.
Conclusions from this review highlight the need for prevention and appropriate ear-protective devices to mitigate the implications of NIHL in the dental workplace [39]. Digital noise excluding headphones that excludes environmental noise, but allows the passage of the human voice, should be considered for the dental environment.
Supplementary Material
Contributor Information
J C Hartland, School of Medicine and Dentistry, Griffith University, Gold Coast, Queensland 4222, Australia.
G Tejada, School of Medicine and Dentistry, Griffith University, Gold Coast, Queensland 4222, Australia.
E J Riedel, School of Medicine and Dentistry, Griffith University, Gold Coast, Queensland 4222, Australia.
A H-L Chen, School of Medicine and Dentistry, Griffith University, Gold Coast, Queensland 4222, Australia.
O Mascarenhas, School of Medicine and Dentistry, Griffith University, Gold Coast, Queensland 4222, Australia.
J Kroon, School of Medicine and Dentistry, Griffith University, Gold Coast, Queensland 4222, Australia.
Funding
None declared.
Competing interests
None declared.
References
- 1. Sampaio Fernandes JC, Carvalho APO, Gallas M, Vaz P, Matos PA.. Noise levels in dental schools. Eur J Dent Educ 2006;10:32–37. [DOI] [PubMed] [Google Scholar]
- 2. National Institute on Deafness and Other Communication Disorders. Noise-Induced Hearing Loss. Bethesda, MD: National Institutes of Health, 2014. Accessed on 27 June 2022. [Google Scholar]
- 3. Occupational Safety and Health Administration. Occupational Noise Exposure. Washington, DC: US Department of Labor, n.d. Accessed on 27 June 2022. [Google Scholar]
- 4. Cheng AG, Cunningham LL, Rubel EW.. Mechanisms of hair cell death and protection. Curr Opin Otolaryngol Head Neck Surg 2005;13:343–348. [DOI] [PubMed] [Google Scholar]
- 5. National Institute on Deafness and Other Communication Disorders. Age-Related Hearing Loss (Presbycusis). Bethesda, MD: National Institutes of Health, 2023. Accessed on 4 April 2023. [Google Scholar]
- 6. Baguley D, McFerran D, Hall D.. Tinnitus. Lancet 2013;382:1600–1607. [DOI] [PubMed] [Google Scholar]
- 7. Coles RR, Hallam RS.. Tinnitus and its management. Br Med Bull 1987;43:983–998. [DOI] [PubMed] [Google Scholar]
- 8. Ramsey R, Greenough J, Breeze J.. Noise-induced hearing loss in the military dental setting: a UK legislative perspective. BMJ Mil Health 2020;166:e53–e56. [DOI] [PubMed] [Google Scholar]
- 9. Qsaibati ML, Ibrahim O.. Noise levels of dental equipment used in dental college of Damascus University. Dent Res J 2014;11:624–630. [PMC free article] [PubMed] [Google Scholar]
- 10. Setcos JC, Mahyuddin A.. Noise levels encountered in dental clinical and laboratory practice. Int J Prosthodont 1998;11:150–157. [PubMed] [Google Scholar]
- 11. Dierickx M, Verschraegen S, Wierinck E, Willems G, van Wieringen A.. Noise disturbance and potential hearing loss due to exposure of dental equipment in flemish dentists. Int J Environ Res Public Health 2021;18:5617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions, version 6.3 (updated February 2022). London, UK: Cochrane, 2022. Accessed on 23 April 2022. [Google Scholar]
- 13. Page MJ, McKenzie JE, Bossuyt PMet al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Morgan RL, Whaley P, Thayer KA, Schunemann HJ.. Identifying the PECO: A framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ Int 2018;121:1027–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 2012;22:276–282. [PMC free article] [PubMed] [Google Scholar]
- 16. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Ottawa, Ontario: Ottawa Hospital Research Institute, 2000. Accessed on 23 January 2022. [Google Scholar]
- 17. Modesti PA, Reboldi G, Cappuccio FPet al.; ESH Working Group on CV Risk in Low Resource Settings. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One 2016;11:e0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wilson JD, Darby ML, Tolle SL, Sever JC.. Effects of occupational ultrasonic noise exposure on hearing of dental hygienists: a pilot study. J Dent Hyg 2002;76:262–269. [PubMed] [Google Scholar]
- 19. Al-Omoush SA, Abdul-Baqi KJ, Zuriekat M, Alsoleihat F, Elmanaseer WR, Jamani KD.. Assessment of occupational noise-related hearing impairment among dental health personnel. J Occup Health 2020;62:e12093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Theodoroff SM, Folmer RL.. Hearing loss associated with long-term exposure to high-speed dental handpieces. Gen Dent 2015;63:71–76. [PubMed] [Google Scholar]
- 21. Amine M, Aljalil Z, Redwane A, Delfag I, Lahby I, Bennani A.. Assessment of noise levels of equipment used in the practical dental teaching activities. Int J Dent 2021;2021:6642560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yousuf A, Ganta S, Nagaraj Aet al. Acoustic noise levels of dental equipments and its association with fear and annoyance levels among patients attending different dental clinic setups in Jaipur, India. J Clin Diagn Res 2014;8:ZC29–ZC34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Al-Rawi NH, Al Nuaimi AS, Sadiqi Aet al. Occupational noise-induced hearing loss among dental professionals. Quintessence Int 2019;50:245–250. [DOI] [PubMed] [Google Scholar]
- 24. Gurbuz MK, Çatli T, Cingi C, Yaz A, Bal C.. Occupational safety threats among dental personnel and related risk factors. J Craniofac Surg 2013;24:e599–e602. [DOI] [PubMed] [Google Scholar]
- 25. Lopes AC, De Melo ADP, Santos CC.. A study of the high-frequency hearing thresholds of dentistry professionals. Int Arch Otorhinolaryngol 2012;16:226–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Willershausen B, Callaway A, Wolf TGet al. Hearing assessment in dental practitioners and other academic professionals from an urban setting. Head Face Med 2014;10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Alabdulwahhab BM, Alduraiby RI, Ahmed MAet al. Hearing loss and its association with occupational noise exposure among Saudi dentists: a cross-sectional study. BDJ Open 2016;2:16006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chopra A, Thomas BS, Mohan K, Sivaraman K.. Auditory and nonauditory effects of ultrasonic scaler use and its role in the development of permanent hearing loss. Oral Health Prev Dent 2016;14:493–500. [DOI] [PubMed] [Google Scholar]
- 29. Daud MKM, Noh NFM, Sidek DS, Abd Rahman N, Abd Rani N, Zakaria MN.. Screening of dental staff nurses for noise induced hearing loss. B-ENT 2011;7:245–249. [PubMed] [Google Scholar]
- 30. Gabrielle M, Susilawati S, Mahdiani S.. Hearing threshold and noise exposure of dentists at Padjadjaran University Dental Hospital in Bandung. J Int Dent Med Res 2020;13:1151–1155. [Google Scholar]
- 31. Shetty R, Shoukath S, Shetty SK, Dandekeri S, Shetty NHG, Ragher M.. Hearing assessment of dental personnel: a cross-sectional exploratory study. J Pharm Bioallied Sci 2020;12:488–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ahmed NA, Ummar F, Girishraj G, Sameer KM.. Noise induced hearing loss in dental professionals: an audiometric analysis of dental professionals. IOSR J Dent Med Sci 2013;11:29–31. [Google Scholar]
- 33. Gijbels F, Jacobs R, Princen K, Nackaerts O, Debruyne F.. Potential occupational health problems for dentists in Flanders, Belgium. Clin Oral Investig 2006;10:8–16. [DOI] [PubMed] [Google Scholar]
- 34. Gonçalves CG, Santos L, Lobato D, Ribas A, Lacerda ABM, Marques J.. Characterization of hearing thresholds from 500 to 16,000 Hz in dentists: a comparative study. Int Arch Otorhinolaryngol 2015;19:156–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Khaimook W, Suksamae P, Choosong T, Chayarpham S, Tantisarasart R.. The prevalence of noise-induced occupational hearing loss in dentistry personnel. Workplace Health Saf 2014;62:357–360. [DOI] [PubMed] [Google Scholar]
- 36. Messano GA, Petti S.. General dental practitioners and hearing impairment. J Dent 2012;40:821–828. [DOI] [PubMed] [Google Scholar]
- 37. Moore BCJ. A review of the perceptual effects of hearing loss for frequencies above 3 kHz. Int J Audiol 2016;55:707–714. [DOI] [PubMed] [Google Scholar]
- 38. Akesson I, Balogh I, Skerfving S.. Self-reported and measured time of vibration exposure at ultrasonic scaling in dental hygienists. Appl Ergon 2001;32:47–51. [DOI] [PubMed] [Google Scholar]
- 39. Mohan KM, Chopra A, Guddattu V, Singh S, Upasana K.. Should dentists mandatorily wear ear protection device to prevent occupational noise-induced hearing loss? A randomized case-control study. J Int Soc Prev Community Dent 2022;12:513–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.